Abstract
Medicaid eligibility expansion, though not directly applicable to children, has been associated with improved access to care in children with cancer, but associations with overall survival are unknown. Data for children ages 0 to 14 years diagnosed with cancer from 2011 to 2018 were queried from central cancer registries data covering cancer diagnoses from 40 states as part of the Centers for Disease Control and Prevention’s National Program of Cancer Registries. Difference-in-differences analyses were used to compare changes in 2-year survival from 2011-2013 to 2015-2018 in Medicaid expansion relative to nonexpansion states. In adjusted analyses, there was a 1.50 percentage point (95% confidence interval = 0.37 to 2.64) increase in 2-year overall survival after 2014 in expansion relative to nonexpansion states, particularly for those living in the lowest county income quartile (difference-in-differences = 5.12 percentage point, 95% confidence interval = 2.59 to 7.65). Medicaid expansion may improve cancer outcomes for children with cancer.
The Patient Protection and Affordable Care Act (ACA), passed in 2010 and largely enacted in 2014, included expanding Medicaid eligibility to adults with incomes of no more than 138% of the federal poverty level (1). As of July 2022, 39 states (including Washington, DC) adopted Medicaid expansion, and 12 did not (2). Although not directed specifically at increasing Medicaid coverage in children, expansion is associated with increased Medicaid uptake and slightly decreased uninsured rates in children, including those with cancer (3,4). These findings may be at least partially attributed to “welcome mat” effects, where eligible but previously uninsured children become enrolled in Medicaid or the Children’s Health Insurance Program because of gains in parental coverage eligibility or other ACA-mediated factors (3,4).
Medicaid expansion has positively affected cancer survival and mortality in adults (5-9); however, its effect on childhood cancer survival has not been reported. Our objective was to examine whether there is early evidence for an expansion-associated impact on childhood cancer survival.
Data for children ages 0 to 14 years diagnosed with cancer from 2011 to 2018 were queried from data covering cancer diagnoses from 40 states as part of the Centers for Disease Control and Prevention’s National Program of Cancer Registries (Supplementary Table 1, available online) (10). The primary outcome was 2-year overall survival, which was integrated into our analyses via the pseudo-observation method (11). The 2-year endpoint was selected to be similar to the median follow-up time (21 months for individuals diagnosed post-ACA). Other oncologic endpoints were not available. We used difference-in-differences (DID) analyses to compare changes in 2-year survival from 2011-2013 to 2015-2018 between children residing in states expanding Medicaid by 2014 vs states not expanding Medicaid within the study period (Supplementary Methods, available online) (12). The year 2014 was excluded as a washout and phase-in period. States expanding Medicaid from 2015 to 2018 were excluded from our main analyses but were included in a sensitivity analysis (Supplementary Table 1, available online). Analyses were adjusted for state and year fixed effects and covariates including age, race, ethnicity, sex, metropolitan residence, and cancer type, which were selected a priori because of associations with health-care access and cancer outcomes. Individuals missing covariate information were excluded from the analyses. Because several states had limited Medicaid expansions from 2010 to 2011 (13), we conducted a sensitivity analysis adjusting for early Medicaid expansion status, including 2009 to 2018 data. Because the expansions could lead to earlier diagnosis resulting in improved prognosis (6,14), stage at diagnosis was not included as a covariate in our main analyses but was included in a sensitivity analysis. Analyses were conducted overall and by sociodemographic subgroups and cancer type. We hypothesized that historically socioeconomically disadvantaged subgroups and those with tumors more amenable to early detection and/or treatment would be most affected by the expansions (15). The parallel trends assumption for DID analyses was assessed by visually assessing temporal trends and by testing for differential changes in survival between expansion and nonexpansion states over the pre-expansion period (Supplementary Methods, available online) (12). The trends were satisfactorily similar for all analyses unless noted (Supplementary Table 2, available online).
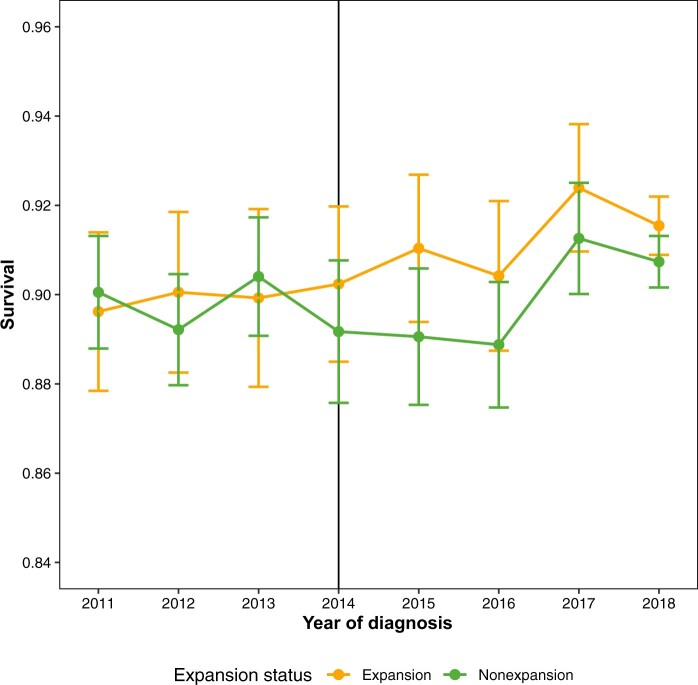
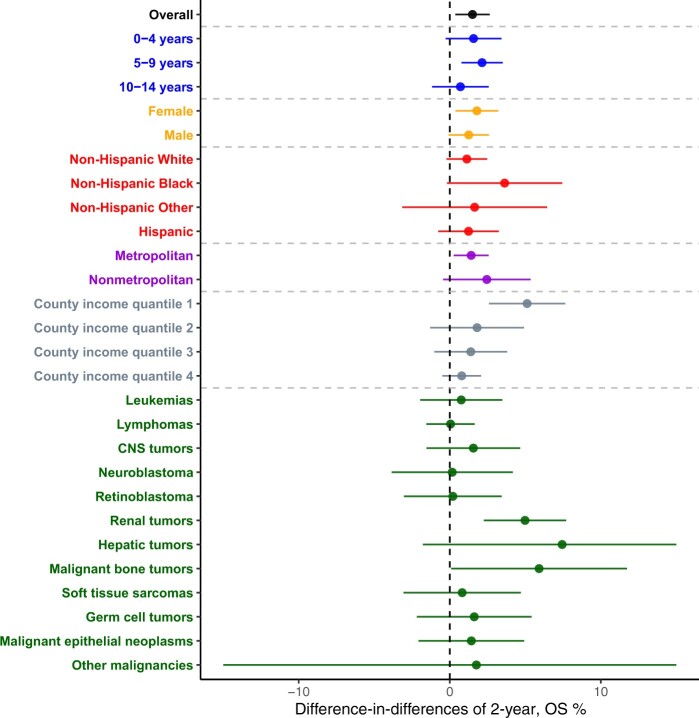
A total of 46 850 children diagnosed between 2011 and 2018 were included (Supplementary Table 3, Supplementary Figure 1, available online). For all cancers combined, there was a statistically significant increase in 2-year overall survival from pre- to post-expansion in expansion (89.9%-91.3%) vs nonexpansion (89.9%-89.9%) states (DID = 1.50 percentage points, 95% confidence interval [CI] = 0.37 to 2.64). The most notable expansion-associated increases in overall survival were in those living in the lowest quartile of county income (DID = 5.12%, 95% CI = 2.59 to 7.65) and with malignant bone tumors (DID = 5.91 percentage points, 95% CI = 0.09 to 11.73). Statistically non-significant expansion-associated increases in overall survival were also observed in non-Hispanic Black children (DID = 3.63 percentage points, 95% CI = -0.19 to 7.45) (Figures 1 and 2; Supplementary Table 4, Supplementary Figures 2 and 3, available online). Sensitivity analyses produced similar results (Supplementary Results, Supplementary Table 5, available online).
Figure 1.
Temporal trends in 2-year overall survival by state Medicaid expansion status (Central Brain Tumor Registry of the United States: data provided by the Center for Disease Control and Prevention’s National Program of Cancer Registries, 2011-2018).
Figure 2.
Difference-in-differences estimates of the expansion-associated change in 2-year overall survival (CBTRUS: data provided by the Center for Disease Control and Prevention’s National Program of Cancer Registries, 2011-2018). Point estimates and 95% confidence intervals reflect the adjusted difference-in-differences estimates of expansion-associated changes in 2-year overall survival for the overall cohort or given subgroup. Positive (>0) values reflect increased 2-year overall survival associated with Medicaid expansion. CNS = central nervous system; OS = overall survival.
In summary, we found evidence for an expansion-associated increase in overall survival for children with cancer in expansion relative to nonexpansion states, particularly for those living in lower income areas and with bone tumors. Although the relative increase was small, it translates to an additional 200 children alive at 2 years following their cancer diagnosis.
These results may be explained in part by “welcome mat” effects, where Medicaid-eligible children became enrolled from an increased awareness by their guardian(s), perhaps because of greater outreach in expansion states and reductions in application burden (3). The observations that lower socioeconomic status groups, including residents of low-income counties and possibly non-Hispanic Black children, had expansion-related survival improvements are plausible given that expansion policies targeted low-income populations.
Our prior results showed expansion-associated increases in Medicaid and/or Children’s Health Insurance Program coverage and reductions in privately insured and uninsured childhood cancer patients in association with expansion (4). The ACA has been associated with reductions in out-of-pocket expenses for medical care in families (16), which may result in increases in access to care that could ultimately affect outcomes (17). Given similar results in a sensitivity analysis adjusting for stage at diagnosis, stage changes are likely not an important contributor to the changes in survival.
A key strength of these data is the large size. However, only two years of follow-up may be insufficient to fully capture policy effects on disease outcomes. Additionally, not all states were included, earlier detection could result in lead-time bias, power may be insufficient for some cancer types, and we lacked information on potential Medicaid expansion–associated changes in treatment patterns. Furthermore, it is unclear whether changing sample composition, such as an increase in children of lower socioeconomic status, contributed to the present findings. Finally, DID analyses assume parallel trends in the outcome in the absence of expansion and common shocks between the state groups (12). Although changes in survival were similar between state groups over time in the pre-ACA period, it is impossible to directly test these assumptions; hence, factors beyond Medicaid expansion could also contribute to our findings, precluding causal inference.
In conclusion, in an early analysis of Medicaid expansion, we found evidence for improvements in overall survival in children with cancer.
Supplementary Material
Acknowledgements
The CBTRUS data were provided through an agreement with the Centers for Disease Control and Prevention’s National Program of Cancer Registries. In addition, CBTRUS used data from the research data files of the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program. Contents are solely the responsibility of the authors and do not necessarily represent the official views of the CDC or the NCI.
The funder/sponsor did not participate in the work.
A portion of this work was presented at the American Society of Clinical Oncology (ASCO) 2022 Annual Meeting, June 4, 2022, Chicago, IL.
Contributor Information
Justin M Barnes, Department of Radiation Oncology, Washington University School of Medicine in St. Louis, St. Louis, MO, USA.
Corey Neff, Department of Neurosurgery, Duke University School of Medicine, Durham, NC, USA; Central Brain Tumor Registry of the United States, Hinsdale, IL, USA.
Xuesong Han, Surveillance & Health Equity Science, American Cancer Society, Atlanta, GA, USA.
Carol Kruchko, Central Brain Tumor Registry of the United States, Hinsdale, IL, USA.
Jill S Barnholtz-Sloan, Central Brain Tumor Registry of the United States, Hinsdale, IL, USA; Center for Biomedical Informatics & Information Technology and Division of Cancer Epidemiology and Genetics, National Cancer Institute, Bethesda, MD, USA.
Quinn T Ostrom, Department of Neurosurgery, Duke University School of Medicine, Durham, NC, USA; Central Brain Tumor Registry of the United States, Hinsdale, IL, USA; The Preston Robert Tisch Brain Tumor Center, Duke University School of Medicine, Durham, NC, USA; Duke Cancer Institute, Duke University Medical Center, Durham, NC, USA.
Kimberly J Johnson, Brown School, Washington University in St. Louis, St. Louis, MO, USA.
Data availability
No new data were analyzed in support of this research. The data analyzed included data from the Central Brain Tumor Registry of the United States (CBTRUS), which were provided through an agreement with the Centers for Disease Control’s National Program of Cancer Registries. In addition, CBTRUS used data from the research data files of the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program.
Author contributions
Jill S. Barnholtz-Sloan, PhD (Data curation; Writing—review & editing), Quinn T. Ostrom, PhD, MPH (Conceptualization; Methodology; Supervision; Writing—review & editing), Kimberly J. Johnson, PhD, MPH (Conceptualization; Methodology; Supervision; Visualization; Writing—original draft; Writing—review & editing), Carol Kruckko, BA (Data curation; Writing—review & editing), Justin Michael Barnes, MD, MS (Conceptualization; Formal analysis; Methodology; Visualization; Writing—original draft; Writing—review & editing), Corey Neff, MPH (Data curation; Formal analysis; Methodology; Writing—review & editing), and Xuesong Han, PhD (Methodology; Writing—review & editing)
Funding
Funding for CBTRUS was provided by the Centers for Disease Control and Prevention (CDC) under Contract No. 75D30119C06056 Amendment/Modification No: 0002, the American Brain Tumor Association, Novocure, the Musella Foundation for Brain Tumor Research & Information, National Brain Tumor Society, the Pediatric Brain Tumor Foundation, The Sontag Foundation, the Uncle Kory Foundation, the Zelda Dorin Tetenbaum Memorial Fund, as well as private and in-kind donations. The research services of JSB-S were provided by the Division of Cancer Epidemiology and Genetics of the NCI.
Conflicts of interest
The authors have no conflicts of interest to disclose.
References
- 1.U.S. Centers for Medicare & Medicaid Services. Affordable Care Act (ACA) - HealthCare.gov Glossary | HealthCare.gov. https://www.healthcare.gov/glossary/affordable-care-act/. Accessed February 15, 2023.
- 2.Kaiser Family Foundation. Status of State Medicaid Expansion Decisions: Interactive Map | KFF. https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/. Accessed February 15, 2023.
- 3. Hudson JL, Moriya AS.. Medicaid expansion for adults had measurable ‘welcome mat’ effects on their children. Health Aff. 2017;36(9):1643-1651. doi: 10.1377/hlthaff.2017.0347. [DOI] [PubMed] [Google Scholar]
- 4. Barnes JM, Barker AR, King AA, Johnson KJ.. Association of Medicaid expansion with insurance coverage among children with cancer. JAMA Pediatr. 2020;174(6):581-591. doi: 10.1001/jamapediatrics.2020.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Barnes JM, Johnson KJ, Adjei Boakye E, et al. Early Medicaid expansion and cancer mortality. J Natl Cancer Inst. 2021;113(12):1714-1722. doi: 10.1093/jnci/djab135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Han X, Zhao J, Yabroff KR, Johnson CJ, Jemal A.. Association between Medicaid expansion under the Affordable Care Act and survival among newly diagnosed cancer patients. J Natl Cancer Inst. 2022;114(8):1176-1185. doi: 10.1093/jnci/djac077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Liu Y, Colditz GA, Kozower BD, et al. Association of Medicaid expansion under the patient protection and Affordable Care Act with non–small cell lung cancer survival. JAMA Oncol. 2020;6(8):1289. doi: 10.1001/jamaoncol.2020.1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lam MB, Phelan J, Orav EJ, Jha AK, Keating NL.. Medicaid expansion and mortality among patients with breast, lung, and colorectal cancer. JAMA Netw Open. 2020;3(11):e2024366. doi: 10.1001/jamanetworkopen.2020.24366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ji X, Shi KS, Mertens AC, et al. Survival in young adults with cancer is associated with Medicaid expansion through the Affordable Care Act. J Clin Oncol. 2022;16:JCO2201742. doi:10.1200/J Clin Oncol.22.01742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention National Center for Health Statistics. National Program of Cancer Registries and Surveillance, Epidemiology, and End Results SEER*Stat Database: NPCR Survival Analytic File (2001-2018). United States Department of Health and Human Services, Centers for Disease Control and Prevention. Released June 2022. Based on the 2021 Submission.
- 11. Andersen PK, Pohar Perme M.. Pseudo-observations in survival analysis. Stat Methods Med Res. 2010;19(1):71-99. doi: 10.1177/0962280209105020. [DOI] [PubMed] [Google Scholar]
- 12. Dimick JB, Ryan AM.. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA J Am Med Assoc. 2014;312(22):2401-2402. doi: 10.1001/jama.2014. [DOI] [PubMed] [Google Scholar]
- 13. Sommers BD, Arntson E, Kenney GM, Epstein AM.. Lessons from early Medicaid expansions under health reform: interviews with Medicaid officials. Medicare Medicaid Res Rev. 2013;3(4):E1-E23. doi: 10.5600/mmrr.003.04.a02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Han X, Yabroff KR, Ward E, Brawley OW, Jemal A.. Comparison of insurance status and diagnosis stage among patients with newly diagnosed cancer before vs after implementation of the patient protection and affordable care act. JAMA Oncol. 2018;4(12):1713. doi: 10.1001/JAMAONCOL.2018.3467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Delavar A, Barnes JM, Wang X, Johnson KJ.. Associations between race/ethnicity and US childhood and adolescent cancer survival by treatment amenability. JAMA Pediatr. 2020;174(5):428. doi: 10.1001/JAMAPEDIATRICS.2019.6074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wisk LE, Peltz A, Galbraith AA.. Changes in health care–related financial burden for us families with children associated with the affordable care act. JAMA Pediatr. 2020;174(11):1032-1040. doi: 10.1001/jamapediatrics.2020.3973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Santacroce SJ, Kneipp SM.. A conceptual model of financial toxicity in pediatric oncology. J Pediatr Oncol Nurs. 2019;36(1):6-16. doi: 10.1177/1043454218810137. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No new data were analyzed in support of this research. The data analyzed included data from the Central Brain Tumor Registry of the United States (CBTRUS), which were provided through an agreement with the Centers for Disease Control’s National Program of Cancer Registries. In addition, CBTRUS used data from the research data files of the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program.