Abstract
Background
During 4 months of the severe acute respiratory coronavirus 2 (SARS-CoV-2) pandemic, nurses in a pediatric emergency department (ED) used surgical and clear face masks in triage. This study aimed to find out if the type of face mask influenced children’s reports of pain.
Methods
A retrospective cross-sectional analysis of the pain scores of all patients aged 3–15 years who visited the ED during the 4-month period was performed. Multivariate regression was used to control for the potential confounders of demographics, diagnosis (medical, trauma), nurse experience, ED time of arrival, and triage acuity level. Self-reports of pain ≥1/10 and pain ≥4/10 were the dependent variables.
Results
Overall, 3,069 children attended the ED during the study period. Triage nurses wore surgical and clear face masks in 2,337 and 732 nurse-patient encounters, respectively. The two types of face masks were used in similar proportions of nurse-patient encounters. Compared with the clear face mask, wearing a surgical face mask was associated with a lower likelihood of reporting pain ≥1/10, and a lower likelihood of reporting pain ≥4/10; [adjusted odds ratio (aOR) =0.68; 95% confidence interval (CI): 0.56–0.82], and (aOR =0.71; 95% CI: 0.58–0.86), respectively.
Conclusions
The findings suggest that the type of face mask used by the nurse influenced the report of pain. This study provides preliminary evidence that covered face masks worn by healthcare providers might have a negative impact on the child’s report of pain.
Keywords: Pain, self-report, face mask, triage, severe acute respiratory coronavirus 2 (SARS-CoV-2)
Highlight box.
Key findings
• The study examined the association between the type of face mask worn by triage nurses and the pain reported by children. We found that the surgical face mask was associated with a lower likelihood of reporting pain than the clear face mask.
What is known and what is new?
• During 4 months of the SARS-CoV-2 pandemic, nurses in a pediatric ED used surgical and clear face masks in triage.
• Compared with the clear face mask, wearing a surgical face mask was associated with a lower likelihood of reporting any pain (score ≥1/10), and reporting significant pain (score ≥4/10).
What is the implication, and what should change now?
• Study findings suggest that in the presence of covered face masks, children might under-report their pain level.
Introduction
Effective communication is a vital necessity in building therapeutic relationships between healthcare providers and children (1). Since the emergence of the severe acute respiratory coronavirus 2 (SARS-CoV-2) pandemic, physicians and nurses have been required to wear medical face masks that cover their lower faces during routine activities (2). However, covering the lower part of the face with a mask, especially a mouth, might influence nonverbal communication of emotions by affecting the ability to infer sentiment from facial expressions (3). This may be particularly important in the pediatric emergency department (ED), where the environment is stressful for children (1,4). Previous studies reported that surgical face masks worn by adults may have a significant effect on children’s emotion recognition accuracy (5-7). Currently, no study has examined the possible effect of the type of face mask worn by healthcare providers on the pain reported by children.
During a 4-month period of the SARS-CoV-2 pandemic, nurses in a pediatric ED of a tertiary medical center in Israel used surgical (standard covered) or clear face masks in triage, throughout the whole shift. The present study sought to find out if the type of face mask influenced children’s reports of pain. We present the following article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-511/rc).
Methods
Setting, study design, and participants
This cross-sectional study was conducted in the pediatric ED of Rambam Health Care Campus, a tertiary care center in Haifa, Israel. Analysis of the triage pain scores of all patients aged 3–15 years who visited the pediatric ED during a 4-month period was performed. Patients with special healthcare needs and patients who needed immediate intervention (triage acuity level 1) were excluded from the analysis. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Ethics Committee of Rambam Health Care Campus (No. D-0348-21). Patient informed consent was not required due to the observational design of the study.
Study instruments and assessment
Between February 1 and May 31, 2021, as part of assessing nurses’ satisfaction with face masks, triage nurses were asked to wear surgical face masks or clear face masks throughout the whole shift. Nurses wore clear and surgical face masks, alternately, every other shift. The clear mask is Food and Drug Administration (FDA)-cleared as a class II surgical mask that meets the American Society for Testing and Materials Level 3 standards (8,9).
At the end of the 4-month period, nurses were asked to complete a 5-item questionnaire to score their satisfaction with the surgical mask and the clear mask, using a five-point Likert Scale (“the face mask was comfortable to use”; 1—strongly disagree, 2—disagree, 3—neither agree nor disagree, 4—agree, 5—strongly agree).
Pain assessment protocol in triage
The triage nurse is responsible for pain assessment and treatment of any child admitted to the pediatric ED. The Wong-Baker FACES Pain Rating Scale is used to assess pain in children aged 3–7 years. The child is presented with a selection of six faces expressing different degrees of distress and then points to the face that best represents his/her pain level (10). In children aged 8–15 years, the visual analog scale is used. This scale consists of a 10 cm horizontal line, anchored by the word descriptors: none, annoying, uncomfortable, and worst imaginable pain. The child points to the level of pain that best represents his/her level of pain. After providing an explanation of the scale, the triage nurse asks the child to mark the level of pain that represents his/her current state of pain (11). The two pain assessment scales have been shown to be reliable and valid measures for use with children (12).
Data collection
All patients seen have their episode of care recorded in a patient data management system (‘Prometheus’, integrated electronic medical records system, Haifa, Israel). The Prometheus is a computerized mandatory working tool for all physicians, nursing staff, and any pediatric ED healthcare personnel. It contains any data collected in real-time by the triage nurses, including vital signs, triage category level, and pain scores. Based on Prometheus, the Information Technology department of the hospital developed a business intelligence information system (BIIS) that provides reporting and analytical functions across multiple datasets. The BIIS enables the automatic extraction of patient data from electronic medical records according to criteria set by researchers (13). During the study period (March to May 2021), the type of face mask worn by the triage nurse (surgical or clear) was recorded in the Prometheus.
In addition to the type of face mask worn by the nurse, other known factors associated with pain assessment in triage were extracted from the BIIS for each patient: demographics (age, sex), diagnosis (medical or trauma), time of arrival (07:01–15:00, 15:01–23:00, 23:01–07:00), triage acuity level (2–5 based on triage criteria: level 2—patient requires evaluation and care within 15 min, level 3—patient requires evaluation and care within 30 min, level 4—patient requires evaluation and care within 60 min, level 5—patient requires evaluation and care within 120 min), and triage nurse experience (<5, 6–10, >11 years) (13-18).
Statistical analysis
An independent t-test was used to compare the mean age between groups, and the Chi-square test was used for the comparison of proportions between groups. The Mann-Whitney nonparametric test was used for the comparison of the ‘satisfaction with the face mask’ between groups. Pain scores were analyzed with SPSS 21 version (SPSS-IBM, Chicago, IL, USA). Multivariate regression analysis was performed to control for the potential confounders of demographics, diagnosis (medical, trauma), nurse experience, time of arrival, and triage acuity level. Self-report of pain ≥1/10 and pain ≥4/10 were the dependent variables for the purpose of this study.
Results
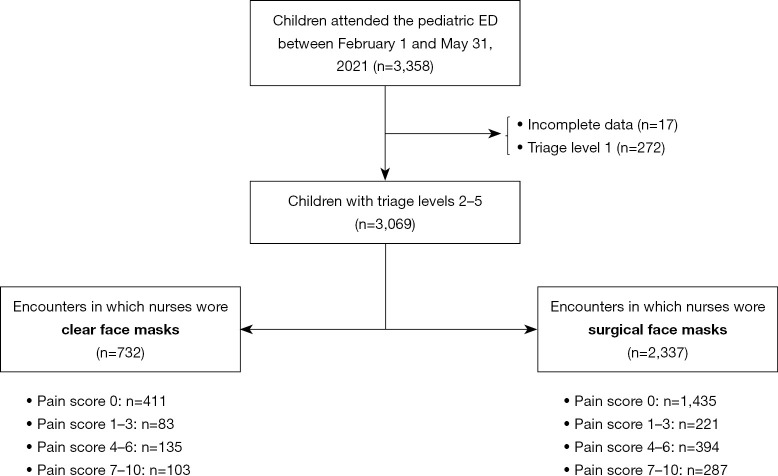
Overall, 3,358 children attended the pediatric ED during this period. Complete data were available for 3,069 patients with triage levels 2–5 (Figure 1). Fifteen nurses wore surgical and clear face masks in triage in 2,337 and 732 nurse-patient encounters, respectively. Nurses used the two types of face masks in similar proportions of patient encounters and had similar satisfaction scores with each type of face mask (Table 1).
Figure 1.
Study flow chart. ED, emergency department.
Table 1. Patients’ and nurses’ characteristics.
| Variable | Encounters in which nurses wore clear face masks (n=732) | Encounters in which nurses wore surgical face masks (n=2,337) | P value |
|---|---|---|---|
| Patient age, mean ± SD, years | 9.6±4.6 | 10.1±4.6 | 0.275 |
| Patient sex, n (%) | 0.815 | ||
| Male | 458 (62.6) | 1,451 (62.1) | |
| Female | 274 (37.4) | 886 (37.9) | |
| Diagnosis, n (%) | 0.643 | ||
| Trauma | 293 (40.0) | 958 (41.0) | |
| Medical | 439 (60.0) | 1,379 (59.0) | |
| 24-hour time of arrival, n (%) | <0.05 | ||
| 07:01–15:00 | 292 (40.0) | 700 (29.9) | |
| 15:01–23:00 | 343 (46.8) | 1,226 (52.5) | |
| 23:01–07:00 | 97 (13.2) | 411 (17.6) | |
| Triage acuity level*, n (%) | <0.05 | ||
| 2 | 53 (7.2) | 309 (13.4) | |
| 3 | 381 (52.0) | 1,247 (53.3) | |
| 4 | 276 (37.8) | 707 (30.2) | |
| 5 | 22 (3.0) | 74 (3.2) | |
| Nurse experience, n (%) | <0.05 | ||
| <5 years | 517 (70.6) | 1,719 (73.6) | |
| 5–10 years | 167 (22.8) | 384 (16.4) | |
| >10 years | 48 (6.6) | 234 (10.0) | |
| Pain score, n (%) | 0.796 | ||
| 0 | 411 (56.1) | 1,435 (61.4) | |
| 1–3 | 83 (11.4) | 221 (9.4) | |
| 4–6 | 135 (18.4) | 394 (16.9) | |
| 7–10 | 103 (14.1) | 287 (12.3) | |
| Nurses’ face mask use, n (%) | |||
| Nurse 1 | 87 (11.9) | 328 (14.0) | 0.069 |
| Nurse 2 | 118 (16.2) | 392 (16.8) | 0.339 |
| Nurse 3 | 90 (13.1) | 316 (13.5) | 0.196 |
| Nurse 4 | 53 (7.3) | 201 (8.6) | 0.122 |
| Nurse 5 | 54 (7.4) | 145 (6.2) | 0.130 |
| Nurse 6 | 42 (5.8) | 168 (7.2) | 0.087 |
| Nurse 7 | 95 (13.0) | 280 (12.0) | 0.236 |
| Nurse 8 | 27 (3.8) | 76 (3.2) | 0.284 |
| Nurse 9 | 39 (5.3) | 107 (4.6) | 0.203 |
| Nurse 10 | 29 (4.0) | 113 (4.8) | 0.163 |
| Nurse 11 | 29 (4.0) | 66 (2.8) | 0.060 |
| Nurse 12 | 21 (2.7) | 60 (2.6) | 0.328 |
| Nurse 13 | 21 (2.7) | 46 (2.0) | 0.072 |
| Nurse 14 | 14 (1.9) | 21 (0.9) | 0.012 |
| Nurse 15 | 7 (0.9) | 18 (0.8) | 0.312 |
| Nurses’ satisfaction of wearing a face mask, median [IQR] | Clear face mask: 4 [2–4] | Surgical face mask: 4 [1–5] | 0.952 |
*, based on the PaedCTAS. Level 1—patient requires immediate evaluation and care, level 2—patient requires evaluation and care within 15 min, level 3—patient requires evaluation and care within 30 min, level 4—patient requires evaluation and care within 60 min, and level 5—patient requires evaluation and care within 120 min. Patients who receive triage level 1 were excluded from the study. n, number of patients; SD, standard deviation; IQR, interquartile range; PaedCTAS, Paediatric Canadian Triage Acuity Scale.
Triage acuity level 2 increased the likelihood of reporting pain ≥1/10 and pain ≥4/10; [adjusted odds ratio (aOR) =2.27; 95% confidence interval (CI): 1.90–2.70], and (aOR =2.15; 95% CI: 1.63–2.84), respectively (Table 2). Compared with medical diagnosis, trauma diagnosis increased the likelihood of reporting pain ≥1/10 and pain ≥4/10; (aOR =1.97; 95% CI: 1.67–2.31), and (aOR =1.68; 95% CI: 1.41–1.99), respectively (Table 2).
Table 2. Results of multivariate regression analyses of factors affecting children’s self-report of pain in triage.
| Variable | Pain score ≥1 | Pain score ≥4 | |||||
|---|---|---|---|---|---|---|---|
| aOR | 95% CI | P value | aOR | 95% CI | P value | ||
| Older age | 1.15 | (1.13–1.17) | <0.0001 | 1.15 | (1.12–1.16) | <0.0001 | |
| Patient sex | |||||||
| Female | Reference | – | – | Reference | – | – | |
| Male | 1.05 | (0.89–1.24) | 0.53 | 1.1 | (0.93–1.31) | 0.27 | |
| Triage acuity level* | |||||||
| 5 | Reference | – | – | Reference | – | – | |
| 3–4 | 2.01 | (1.54–2.62) | <0.0001 | 2.09 | (1.73–2.51) | <0.0001 | |
| 2 | 2.27 | (1.90–2.70) | <0.0001 | 2.15 | (1.63–2.84) | <0.0001 | |
| 24-hour time of arrival | |||||||
| 07:01–15:00 | Reference | – | – | Reference | – | – | |
| 15:01–23:00 | 1.12 | (0.94–1.34) | 0.19 | 1.02 | (0.85–1.20) | 0.79 | |
| 23:01–07:00 | 1.06 | (0.84–1.35) | 0.64 | 1.14 | (0.89–1.46) | 0.30 | |
| Medical | Reference | – | – | Reference | – | – | |
| Trauma | 1.97 | (1.67–2.31) | <0.0001 | 1.68 | (1.41–1.99) | <0.0001 | |
| Nurse experience | |||||||
| More than 10 years | Reference | – | – | Reference | – | – | |
| 5–10 years | 1.03 | (0.79–1.35) | 0.82 | 1.07 | (0.79–1.43) | 0.62 | |
| Less than 5 years | 1.12 | (0.95–1.26) | 0.86 | 1.14 | (0.93–1.34) | 0.76 | |
| Nurse’s face mask | |||||||
| Clear | Reference | – | – | Reference | – | – | |
| Surgical | 0.68 | (0.56–0.82) | <0.001 | 0.71 | (0.58–0.86) | <0.001 | |
*, based on the PaedCTAS. Level 1—patient requires immediate evaluation and care, level 2—patient requires evaluation and care within 15 min, level 3—patient requires evaluation and care within 30 min, level 4—patient requires evaluation and care within 60 min, and level 5—patient requires evaluation and care within 120 min. Patients who receive triage level 1 were excluded from the study. aOR, adjusted odds ratio; CI, confidence interval; PaedCTAS, Paediatric Canadian Triage Acuity Scale.
Compared with the clear face mask, wearing a surgical face mask had a lower likelihood of reporting pain ≥1/10, and a lower likelihood of reporting pain ≥4/10; (aOR =0.68; 95% CI: 0.56–0.82), and (aOR =0.71; 95% CI: 0.58–0.86), respectively.
Discussion
To treat pediatric pain adequately in the ED, proper assessment of the presence and severity of pain in triage is the first essential step. This study is the first to examine the association between the type of face mask worn by healthcare providers and the pain reported by children. The findings suggest that the type of face mask used by the triage nurse influenced the child's report of pain; wearing a surgical face mask was associated with lower odds of reporting pain compared to a clear face mask. These findings seem to suggest that in the presence of covered face masks, children might under-report their pain level. Since nonverbal communication between nurses and children has an important role in the self-report of pain, this could be a potential explanation for our observation (1,3,4).
Previous reports support our findings. Schneider et al. assessed the correct responses of healthy preschool children to pictures of adults displaying joy, anger, or sadness with and without a surgical face mask (5). Analysis of the mistakes made by the children revealed that up to one-quarter of the subjects confused anger and sadness and one-fifth of them answered joy for anger or sadness. The findings of Schneider et al. suggest that, if a face mask is used, the child’s ability to recognize emotions from facial expressions may sometimes be inaccurate. Bourke et al. found that surgical face masks worn by adults had a significant effect on the children’s emotion recognition accuracy. Masked angry faces were more easily recognized and masked happy and sad faces were less easily recognized (6). Similar findings were reported by Gori et al. who found that the use of a face mask influenced the ability to infer facial expressions at any age (7). The results of these studies stress the importance of recognizing information located in the lower face of the healthcare provider (5-7). A possible interpretation of our results is that the presence of a covered face mask influences the child’s perception of facial expressions, and might have a negative effect on nonverbal communication (3).
The regression model used in our study showed a significant influence on pain score for the variable of triage acuity level (Table 2). Since patients are categorized into a triage level based also on their pain assessment, this finding is not surprising (13,14). According to the regression model, older patients and patients with injuries had higher odds of reporting pain. Similar findings were previously reported in the setting of emergency care (13,18).
This single-center study has several limitations. Firstly, because of the lower number of clear face masks available for the study, there were fewer encounters in which the clear face masks were used compared to encounters in which the standard face masks were used (732 vs. 2,337). We believe that this limitation did not affect our results because the two types of face masks were used in similar proportions of patient encounters, and the nurses were equally satisfied with the two types of face masks (Table 1). Secondly, the study has the inherent limitation of a retrospective analysis, including dependence on the quality of documentation recording. The data were extracted using a BIIS; therefore, misinterpretation or abstractor bias had no impact. Thirdly, our cohort came from a single center where nurses are skilled in practicing analgesia. Therefore, our results may not apply to other institutions.
Conclusions
The findings of this pilot study suggest that the type of face mask used by the nurse influenced the report of pain. Although future studies are required to prospectively validate our findings, the study provides preliminary evidence that covered face masks worn by healthcare providers might have a negative impact on the child’s report of pain.
Supplementary
The article’s supplementary files as
Acknowledgments
The authors would like to thank the biostatistician, Mrs. Ronit Leiba, from the Quality-of-Care Unit, Rambam Health Care Campus, Haifa, Israel. Rambam Health Care Campus investigators (Dr. Itai Shavit, Dr. Najib Nasrallah, and Mrs. Oshra Levi) purchased the clear face mask (ClearMask, LLC) from TRADIS GAT Ltd. (Petach Tikva, Israel).
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Ethics Committee of Rambam Health Care Campus (No. D-0348-21). Patient informed consent was not required due to the observational design of the study.
Footnotes
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-22-511/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-22-511/dss
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-22-511/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-511/coif). The authors have no conflicts of interest to declare.
References
- 1.O’Neill KA. Kids speak: effective communication with the school-aged/adolescent patient. Pediatr Emerg Care 2002;18:137-40. 10.1097/00006565-200204000-00018 [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Advice on the use of masks in the context of COVID-19: interim guidance, 5 June 2020. Geneva: World Health Organization, 2020. Available online: https://apps.who.int/iris/handle/10665/332293
- 3.Marler H, Ditton A. “I’m smiling back at you”: Exploring the impact of mask wearing on communication in healthcare. Int J Lang Commun Disord 2021;56:205-14. 10.1111/1460-6984.12578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krauss BA, Krauss BS. Managing the Frightened Child. Ann Emerg Med 2019;74:30-5. 10.1016/j.annemergmed.2018.12.011 [DOI] [PubMed] [Google Scholar]
- 5.Schneider J, Sandoz V, Equey L, et al. The Role of Face Masks in the Recognition of Emotions by Preschool Children. JAMA Pediatr 2022;176:96-8. 10.1001/jamapediatrics.2021.4556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bourke L, Lingwood J, Gallagher-Mitchell T, et al. The effect of face mask wearing on language processing and emotion recognition in young children. J Exp Child Psychol 2023;226:105580. 10.1016/j.jecp.2022.105580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gori M, Schiatti L, Amadeo MB. Masking Emotions: Face Masks Impair How We Read Emotions. Front Psychol 2021;12:669432. 10.3389/fpsyg.2021.669432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.ClearMask, LLC. See the person, not the mask. Available online: https://www.theclearmask.com/
- 9.Kratzke IM, Rosenbaum ME, Cox C, et al. Effect of Clear vs Standard Covered Masks on Communication With Patients During Surgical Clinic Encounters: A Randomized Clinical Trial. JAMA Surg 2021;156:372-8. 10.1001/jamasurg.2021.0836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bieri D, Reeve RA, Champion DG, et al. The Faces Pain Scale for the self-assessment of the severity of pain experienced by children: development, initial validation, and preliminary investigation for ratio scale properties. Pain 1990;41:139-50. 10.1016/0304-3959(90)90018-9 [DOI] [PubMed] [Google Scholar]
- 11.Le May S, Ballard A, Khadra C, et al. Comparison of the psychometric properties of 3 pain scales used in the pediatric emergency department: Visual Analogue Scale, Faces Pain Scale-Revised, and Colour Analogue Scale. Pain 2018;159:1508-17. 10.1097/j.pain.0000000000001236 [DOI] [PubMed] [Google Scholar]
- 12.Huguet A, Stinson JN, McGrath PJ. Measurement of self-reported pain intensity in children and adolescents. J Psychosom Res 2010;68:329-36. 10.1016/j.jpsychores.2009.06.003 [DOI] [PubMed] [Google Scholar]
- 13.Shavit I, Hecht-Sagie L, Allon R, et al. Variables Associated With Administration of Nurse-initiated Analgesia in Pediatric Triage. Clin J Pain 2020;36:365-70. 10.1097/AJP.0000000000000813 [DOI] [PubMed] [Google Scholar]
- 14.Thomas D, Kircher J, Plint AC, et al. Pediatric Pain Management in the Emergency Department: The Triage Nurses’ Perspective. J Emerg Nurs 2015;41:407-13. 10.1016/j.jen.2015.02.012 [DOI] [PubMed] [Google Scholar]
- 15.Alexander J, Manno M. Underuse of analgesia in very young pediatric patients with isolated painful injuries. Ann Emerg Med 2003;41:617-22. 10.1067/mem.2003.138 [DOI] [PubMed] [Google Scholar]
- 16.Safdar B, Heins A, Homel P, et al. Impact of physician and patient gender on pain management in the emergency department—a multicenter study. Pain Med 2009;10:364-72. 10.1111/j.1526-4637.2008.00524.x [DOI] [PubMed] [Google Scholar]
- 17.Goldman RD, Narula N, Klein-Kremer A, et al. Predictors for opioid analgesia administration in children with abdominal pain presenting to the emergency department. Clin J Pain 2008;24:11-5. 10.1097/AJP.0b013e318156d921 [DOI] [PubMed] [Google Scholar]
- 18.Galinski M, Picco N, Hennequin B, et al. Out-of-hospital emergency medicine in pediatric patients: prevalence and management of pain. Am J Emerg Med 2011;29:1062-6. 10.1016/j.ajem.2010.06.031 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as