Abstract
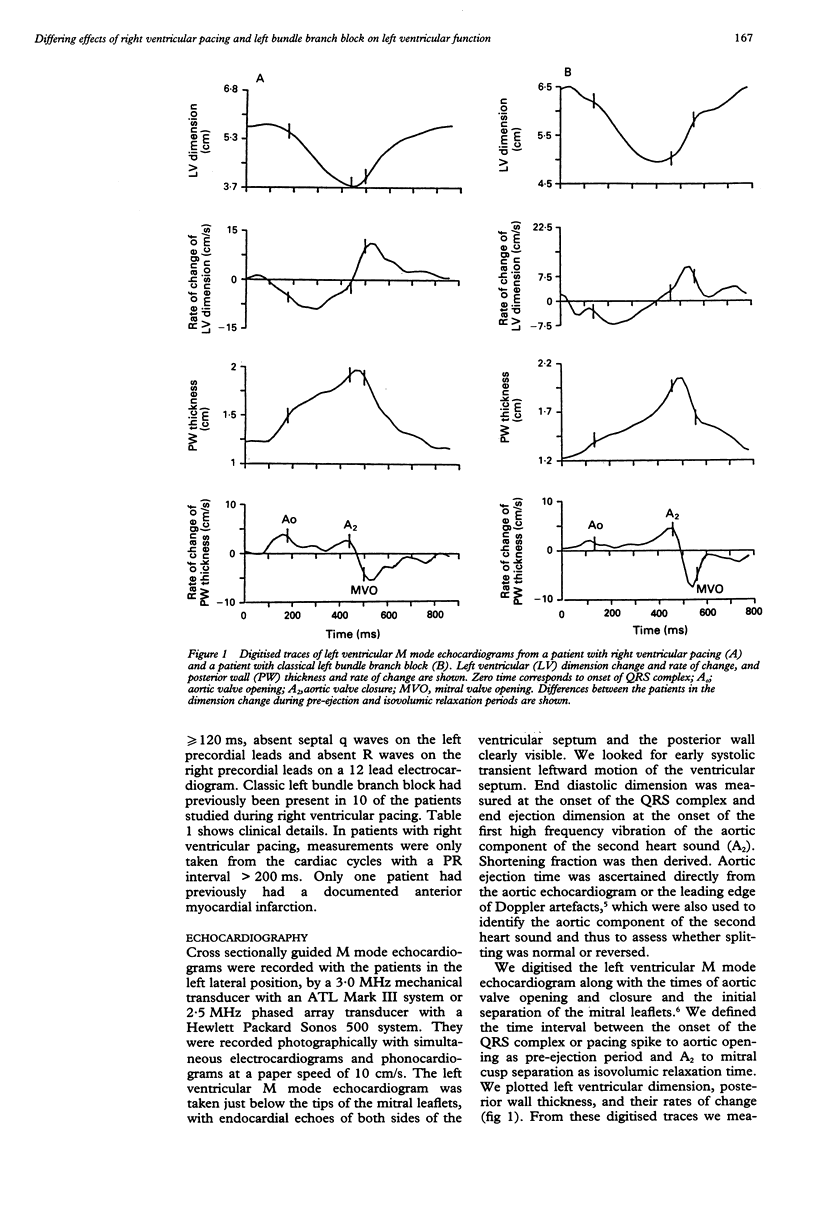
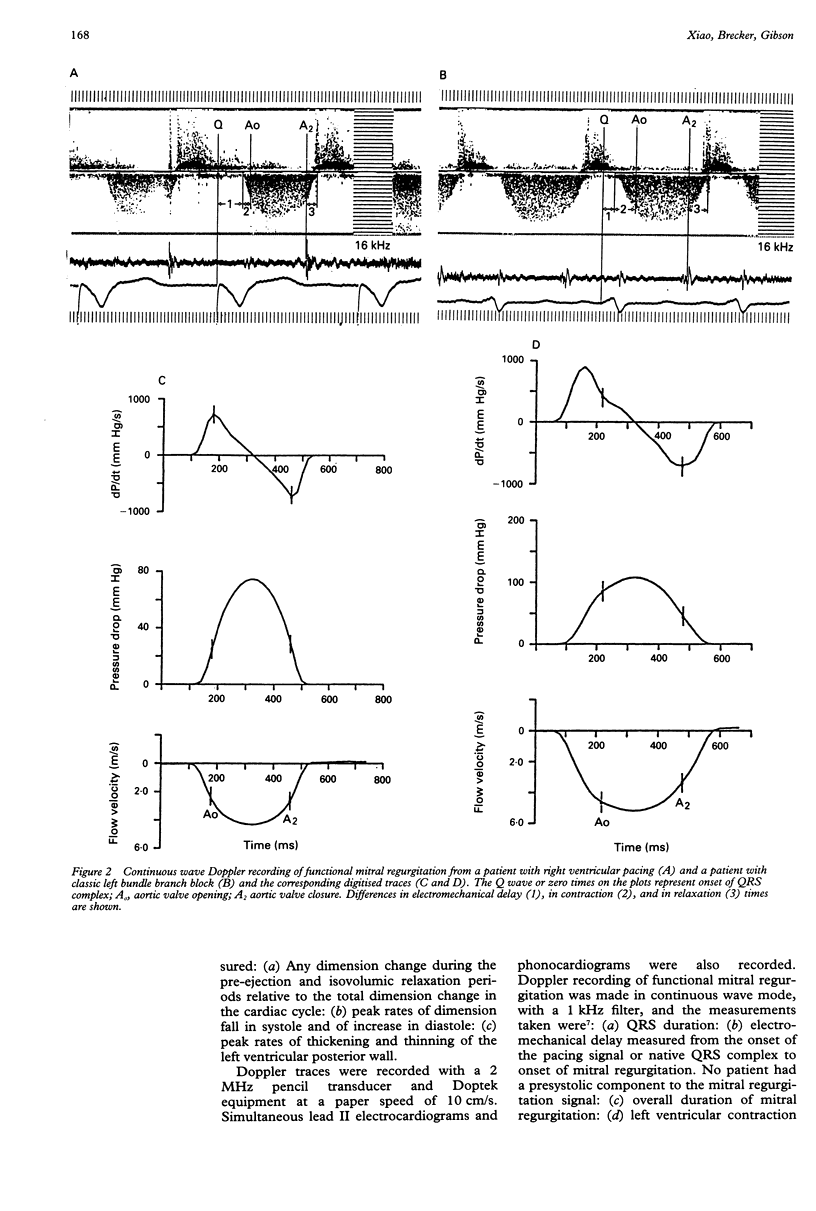
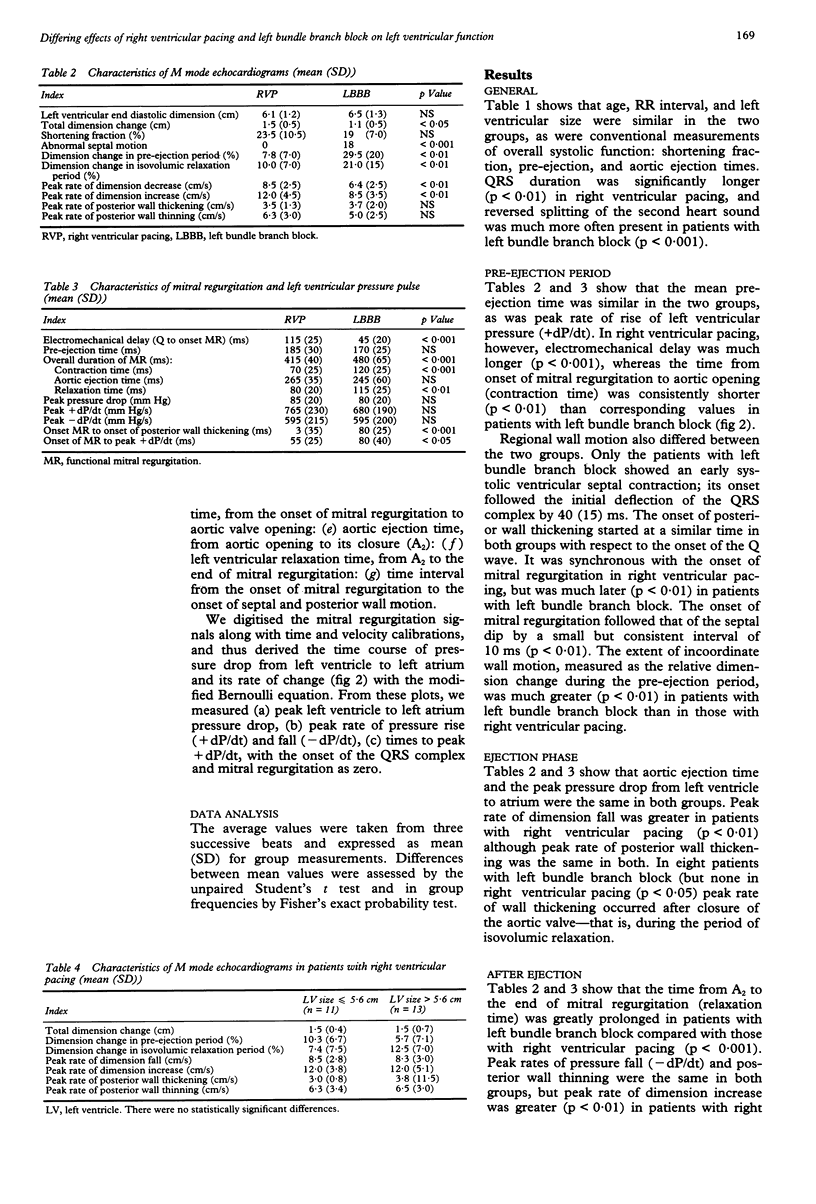
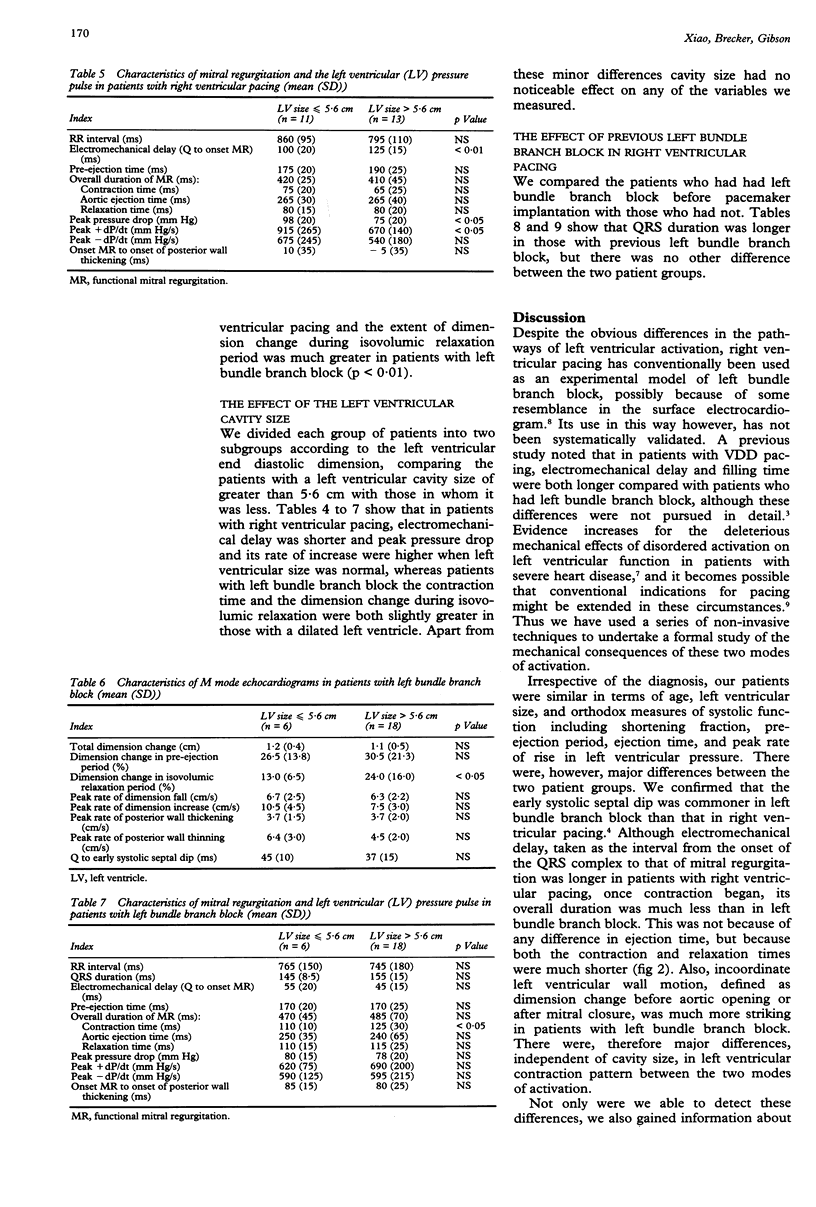
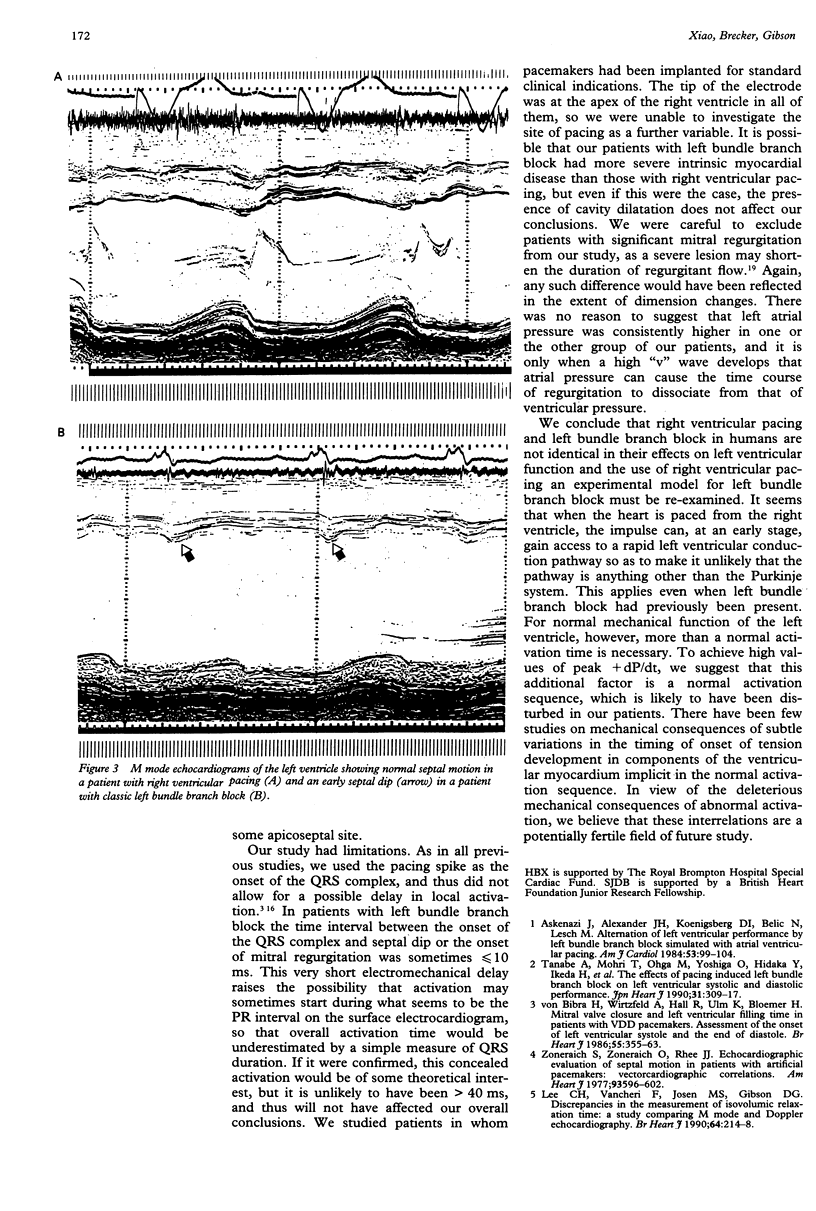
OBJECTIVE--To compare the different effects of right ventricular pacing and classic left bundle branch block on left ventricular function. DESIGN--Retrospective and prospective study of 48 patients by electrocardiography, and M mode, cross sectional, and Doppler echocardiography. SETTING--A tertiary cardiac referral centre. PATIENTS--48 patients (age range 21 to 89 years, 15 women), 24 with a VVI pacemaker implanted and 24 with classic left bundle branch block. Functional mitral regurgitation was present in all those with right ventricular pacing and 22 of those with left bundle branch block. RESULTS--Age, RR interval, and left ventricular size were similar in the two groups, as were conventional measurements of overall systolic function: shortening fraction and pre-ejection and aortic ejection times. In right ventricular pacing, however, QRS duration (p < 0.01) and electromechanical delay were much longer (p < 0.001), whereas the time intervals from onset of mitral regurgitation to aortic opening (contraction time) and from A 2 to the end of mitral regurgitation (relaxation time) were consistently shorter (p < 0.01) than corresponding values in patients with left bundle branch block. Reversed splitting of the second heart sound was much commoner in left bundle branch block (p < 0.02), and only these patients showed an early systolic ventricular septal contraction. Its onset followed the initial deflection of the QRS complex by 40(15) ms and preceded mitral regurgitation by a small but consistent interval of 10 ms (p < 0.01). The onset of posterior wall thickening was synchronous with the onset of mitral regurgitation in right ventricular pacing but much later (p < 0.01) in patients with left bundle branch block. The extent of incoordinate wall motion measure as relative dimension change during pre-ejection and isovolumic relaxation period was much greater (p < 0.01) in left bundle branch block. These major differences were not altered by left ventricular cavity size in either group, nor by the presence of previous left bundle branch block in patients who were subsequently paced. CONCLUSIONS--The left ventricle seems to be activated much more rapidly with right ventricular pacing than with left bundle branch block. This applies even when left bundle branch block is present before pacing. Electromechanical delay, contraction and relaxation times, and extent of incoordinate ventricular wall motion differ strikingly between the two conditions. The use of right ventricular pacing as an experimental model of left bundle branch block in humans must be re-examined.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Askenazi J., Alexander J. H., Koenigsberg D. I., Belic N., Lesch M. Alteration of left ventricular performance by left bundle branch block simulated with atrioventricular sequential pacing. Am J Cardiol. 1984 Jan 1;53(1):99–104. doi: 10.1016/0002-9149(84)90691-x. [DOI] [PubMed] [Google Scholar]
- Badke F. R., Boinay P., Covell J. W. Effects of ventricular pacing on regional left ventricular performance in the dog. Am J Physiol. 1980 Jun;238(6):H858–H867. doi: 10.1152/ajpheart.1980.238.6.H858. [DOI] [PubMed] [Google Scholar]
- Bargiggia G. S., Bertucci C., Recusani F., Raisaro A., de Servi S., Valdes-Cruz L. M., Sahn D. J., Tronconi L. A new method for estimating left ventricular dP/dt by continuous wave Doppler-echocardiography. Validation studies at cardiac catheterization. Circulation. 1989 Nov;80(5):1287–1292. doi: 10.1161/01.cir.80.5.1287. [DOI] [PubMed] [Google Scholar]
- Bedotto J. B., Grayburn P. A., Black W. H., Raya T. E., McBride W., Hsia H. H., Eichhorn E. J. Alterations in left ventricular relaxation during atrioventricular pacing in humans. J Am Coll Cardiol. 1990 Mar 1;15(3):658–664. doi: 10.1016/0735-1097(90)90642-3. [DOI] [PubMed] [Google Scholar]
- Bradley J. A., Gibson D. G. Assessment of the severity of mitral regurgitation from the dynamics of retrograde flow. Br Heart J. 1988 Aug;60(2):134–140. doi: 10.1136/hrt.60.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C., Rodriguez L., Guerrero J. L., Marshall S., Levine R. A., Weyman A. E., Thomas J. D. Noninvasive estimation of the instantaneous first derivative of left ventricular pressure using continuous-wave Doppler echocardiography. Circulation. 1991 Jun;83(6):2101–2110. doi: 10.1161/01.cir.83.6.2101. [DOI] [PubMed] [Google Scholar]
- Grines C. L., Bashore T. M., Boudoulas H., Olson S., Shafer P., Wooley C. F. Functional abnormalities in isolated left bundle branch block. The effect of interventricular asynchrony. Circulation. 1989 Apr;79(4):845–853. doi: 10.1161/01.cir.79.4.845. [DOI] [PubMed] [Google Scholar]
- Hochleitner M., Hörtnagl H., Ng C. K., Hörtnagl H., Gschnitzer F., Zechmann W. Usefulness of physiologic dual-chamber pacing in drug-resistant idiopathic dilated cardiomyopathy. Am J Cardiol. 1990 Jul 15;66(2):198–202. doi: 10.1016/0002-9149(90)90588-r. [DOI] [PubMed] [Google Scholar]
- Lee C. H., Vancheri F., Josen M. S., Gibson D. G. Discrepancies in the measurement of isovolumic relaxation time: a study comparing M mode and Doppler echocardiography. Br Heart J. 1990 Sep;64(3):214–218. doi: 10.1136/hrt.64.3.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald I. G. Echocardiographic demonstration of abnormal motion of the interventricular septum in left bundle branch block. Circulation. 1973 Aug;48(2):272–280. doi: 10.1161/01.cir.48.2.272. [DOI] [PubMed] [Google Scholar]
- Park R. C., Little W. C., O'Rourke R. A. Effect of alteration of left ventricular activation sequence on the left ventricular end-systolic pressure-volume relation in closed-chest dogs. Circ Res. 1985 Nov;57(5):706–717. doi: 10.1161/01.res.57.5.706. [DOI] [PubMed] [Google Scholar]
- Tanabe A., Mohri T., Ohga M., Yoshiga O., Hidaka Y., Ikeda H., Hiyamuta K., Koga Y., Toshima H. The effects of pacing-induced left bundle branch block on left ventricular systolic and diastolic performances. Jpn Heart J. 1990 May;31(3):309–317. doi: 10.1536/ihj.31.309. [DOI] [PubMed] [Google Scholar]
- Upton M. T., Gibson D. G. The study of left ventricular function from digitized echocardiograms. Prog Cardiovasc Dis. 1978 Mar-Apr;20(5):359–384. doi: 10.1016/0033-0620(78)90003-8. [DOI] [PubMed] [Google Scholar]
- Vassallo J. A., Cassidy D. M., Marchlinski F. E., Buxton A. E., Waxman H. L., Doherty J. U., Josephson M. E. Endocardial activation of left bundle branch block. Circulation. 1984 May;69(5):914–923. doi: 10.1161/01.cir.69.5.914. [DOI] [PubMed] [Google Scholar]
- Vassallo J. A., Cassidy D. M., Miller J. M., Buxton A. E., Marchlinski F. E., Josephson M. E. Left ventricular endocardial activation during right ventricular pacing: effect of underlying heart disease. J Am Coll Cardiol. 1986 Jun;7(6):1228–1233. doi: 10.1016/s0735-1097(86)80140-1. [DOI] [PubMed] [Google Scholar]
- Xiao H. B., Lee C. H., Gibson D. G. Effect of left bundle branch block on diastolic function in dilated cardiomyopathy. Br Heart J. 1991 Dec;66(6):443–447. doi: 10.1136/hrt.66.6.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoneraich S., Zoneraich O., Rhee J. J. Echocardiographic evaluation of septal motion in patients with artificial pacemakers: vectorcardiographic correlations. Am Heart J. 1977 May;93(5):596–602. doi: 10.1016/s0002-8703(77)80010-0. [DOI] [PubMed] [Google Scholar]
- von Bibra H., Wirtzfeld A., Hall R., Ulm K., Blömer H. Mitral valve closure and left ventricular filling time in patients with VDD pacemakers. Assessment of the onset of left ventricular systole and the end of diastole. Br Heart J. 1986 Apr;55(4):355–363. doi: 10.1136/hrt.55.4.355. [DOI] [PMC free article] [PubMed] [Google Scholar]


