Abstract
Objective:
Metabolic syndrome (MetS) is associated with common mental health conditions. Using cross-sectional data from the observational Hispanic Community Health Study / Study of Latinos (HCHS/SOL), this study examined the relationship between MetS and depression and anxiety in addition to testing moderating effects of gender and Hispanic heritage subgroups.
Methods:
Participants included 13,496 Hispanic Americans aged 18–74 (59% women, mean age 46.59 ± 13.65) from seven heritage subgroups. Depression was measured using the Center for Epidemiologic Studies Depression 10-item scale, and anxiety was assessed using the State-Trait Anxiety Inventory 10-item scale. A 3-level categorical variable was developed to assess the combined influence of depression and anxiety. The dependent variable is dichotomous, delineating the presence or absence of MetS as defined by the National Cholesterol Education Program Third Adult Treatment Panel. Logistic regression and Hayes’ PROCESS macro assessed these relationships and the moderating effects of gender-heritage subgroups.
Results:
Results suggest depression (p< .001) and anxiety (p< .001) were associated with an increased likelihood of MetS. Puerto Ricans had the highest, and South Americans had the lowest, levels of depression and anxiety. Gender moderated the relationship between mental health and MetS, with women having a significant increase in the probability of MetS with depression (p< .001), anxiety (p< .001), or both (p< .001).
Conclusion:
Elevated symptoms of depression and anxiety are associated with the presence of MetS in US Hispanic subgroups. Gender-heritage differences are present among the study variables. Strategies to manage psychological well-being must be employed to optimize cardiometabolic health in US Hispanics.
Keywords: metabolic syndrome, Hispanic subgroups, depression, anxiety
1. Introduction
Metabolic syndrome (MetS) is a cluster of cardiometabolic characteristics that predispose an individual to morbidities such as cardiovascular disease (CVD) and type 2 diabetes (T2DM). These conditions partly develop from the body’s inflammatory response, which degrades endothelial tissue and disrupts metabolic processes such as glucose and fat regulation (Lett et al., 2004; Pasquali et al., 2006). Identifying MetS before such chronic conditions develop provides a critical opportunity to delay or detour disease by initiating pharmacological interventions and promoting healthy behaviors. Expert groups, including the World Health Organization, the European Group for the Study of Insulin Resistance, the International Diabetes Foundation, and the National Cholesterol Education Program Third Adult Treatment Panel (NCEP ATP III), agree that obesity, insulin resistance, dyslipidemia, and hypertension are core components of MetS; however, each organization uses different clusters to diagnose MetS (Alberti et al., 2006). The NCEP-ATP III, recommended for clinical use in the US and therefore used in this study, defines MetS as having three of the following five criteria, including elevated fasting blood glucose, hypertension, elevated triglycerides, low high-density lipoprotein cholesterol, and increased waist circumference (Alberti et al., 2006; Cassells & Haffner, 2006).
Common mental health conditions such as depression and anxiety have been consistently linked with MetS and the resultant conditions T2DM and CVD (Lett et al., 2004; Moradi et al., 2021; Pan et al., 2012; Renn et al., 2011; Smith et al., 2018; Tang et al., 2017). Depression and anxiety are posited to increase the risk for incident MetS via systemic inflammation and dysregulation of the hypothalamic–pituitary–adrenal (HPA) axis and the autonomic nervous system, which may lead to increased waist circumference, hyperlipidemia, insulin resistance, and cardiac changes (Brunner et al., 2002; Lett et al., 2004; Van Reedt Dortland et al., 2010). Moreover, depression and anxiety make self-care and adopting healthy behaviors difficult, which is essential to prevent or manage MetS. Such a behavioral pathway includes poor treatment adherence and an increased likelihood of poor diet, smoking, alcohol use, and sedentary behavior (Liu et al., 2017; Young-Hyman et al., 2017).
US Hispanic/Latino populations (hereafter referred to as Hispanics) face disparities related to the development of MetS as a result of complex genetic and cultural factors, in addition to structural and societal determinants of health such as poverty and access to care (Aguayo-Mazzucato et al., 2019). When compared to other non-Hispanic populations, Hispanics in the US typically have higher obesity rates, dyslipidemia, elevated blood pressure, and a greater propensity toward glucose dysregulation, all contributing to MetS prevalence rate (Allison et al., 2008; Burroughs Peña et al., 2018; Heiss et al., 2014). These conditions impart devastating consequences, with CVD and T2DM among the top five leading causes of death among US Hispanics (Mozaffarian et al., 2016). From 2011–2016, MetS prevalence in the US was similar among Hispanics (36.3%) and non-Hispanic Whites (36.0%) and was not significantly different across gender; yet the prevalence increased most among young adults ages 20–39, women, and Hispanics (Hirode & Wong, 2020). Among American adults in the age ranges of 18–29 and 50–69, Mexican American men and women also demonstrated higher MetS prevalence relative to their non-Hispanic White and non-Hispanic Black counterparts (Moore et al., 2017). This finding was further corroborated with data from the National Health and Nutrition Examination Survey (NHANES). Between 1999–2018, certain US adult subgroups had a significant upward trend in MetS prevalence, with 40.64% of Mexican Americans meeting NCEP-ATP III criteria for MetS by 2018 (Yang et al., 2022).
Hispanics have a high prevalence of lifestyle and psychological risk factors that may contribute to MetS development and progression. Yet, the association between MetS and mental health in such communities is sorely understudied. In a recent US national opt-in survey, Hispanic adults report having 59% more depressive symptoms than non-Hispanic Whites during the early months of the COVID-19 pandemic, associated in part with higher levels of psychosocial stressors related to social determinants of health (McKnight-Eily et al., 2021). Hispanic men and women who report depression and anxiety symptoms are associated with increased CVD risk (Castañeda et al., 2015). However, data suggest differences in the link between mental health and cardiometabolic disease among Hispanic subgroups. Elevated stress levels independently predicted risk for MetS in Mexicans and Puerto Ricans but not for Dominicans, Central, or South Americans (Ortiz et al., 2015). Finally, although understudied in Hispanic samples, gender differences and inconsistencies in the relationship between MetS and mental health suggest the need for further study. Compared to men with similar symptomatology, women with depressive and anxiety symptoms are at an increased risk of developing MetS (Butnoriene et al., 2015; Kim et al., 2015).
Disaggregated data on Hispanic subgroups are essential to comprehend and potentially prevent or better manage the differences in health outcomes among individuals from diverse Hispanic backgrounds (Daviglus et al., 2012). Data from the National Center for Health Statistics indicated that each Hispanic subgroup, including Mexicans and Cubans, had higher reports of severe psychological distress than all non-Hispanic persons; Puerto Rican adults were almost twice as likely as Central and South Americans to have severe psychological distress (Lucas et al., 2016). Racial/ethnic discrimination, nativity, immigration status, English proficiency, length of time living in the US, family cultural conflict, and processes of racialization contribute to poor mental health conditions in Hispanics (Figuereo & Calvo, 2022). One study indicated that Hispanics born in the US had higher anxiety and depression than those who had immigrated to the US, suggesting that foreign nativity may have a protective influence against psychiatric disorders (Alegría et al., 2008). Similarly, Cook et al. (2009) found that Hispanic individuals living in the US for ten years or longer had a higher risk of psychiatric disorders such as depression than those who recently immigrated.
Our understanding of the association between mental health and chronic illness among US Hispanics is limited, in part because there have been few attempts to disaggregate this heterogeneous population into distinct heritage subgroups. Current literature often overlooks this heterogeneity by examining Mexican Americans only, including small percentages of Hispanics, or by not specifying heritage background, lumping all Hispanics into one category (Heiss et al., 2014; Sorlie et al., 2010). This study examined the relationship between MetS and mental health conditions among diverse Hispanic gender-heritage subgroups to begin to better understand these disparities. Gender-heritage differences among study variables were evaluated to describe the mental health characteristics of this sample. Early detection and treatment of depression and anxiety may detour or decrease the severity of MetS and its sequelae. Lifestyle factors, such as tobacco smoking, alcohol use, and physical activity can impact the relationship between mental health and MetS; therefore, they are included in the analysis. These aims guided the following hypotheses. Hypothesis 1: Depression and anxiety will be associated with MetS, controlling for age, gender, and Hispanic heritage subgroup membership, smoking, alcohol use, physical activity, whether US-born, and years lived in the US. Hypothesis 2: Gender and Hispanic heritage group membership will moderate the association between mental health (depression and anxiety) and MetS, controlling for age, smoking, alcohol use, physical activity, whether US-born, and years lived in the US.
2. Methods
The current study follows the Strengthening the Reporting of Observations Studies in Epidemiology (STROBE) guidelines for reporting observational studies (von Elm et al., 2007). Secondary analysis of cross-sectional data from the observational Hispanic Community Health Study / Study of Latinos (HCHS/SOL) examined the above hypotheses.
2.1. Participants
2.1.1. The Larger Sample: HCHS/SOL
The HCHS/SOL is a multicenter, community-based cohort study representing 16,415 individuals who self-identified as Hispanic/Latino, aged 18–74 years, and lived in four US communities (the Bronx, Chicago, Miami, or San Diego). Participants were recruited using a two-staged randomization process of geographically clustered blocks and households within each block. Individuals within the selected households that agreed to participate underwent a physical exam, blood draw, and answered questionnaires in English or Spanish. The first visit was conducted from 2008–2011; the second from 2014–2017; the third and final visit is currently in process. All participants provided written consent. The other details about the sample design and participant selection have been previously described (Sorlie et al., 2010).
2.1.2. The Current Study Sample
The data from the first visit were used for the current study. Inclusion criteria for this sample included participants with available data that differentiated them into MetS categories, including known medication history, anthropometric measurements, fasting blood draw, and blood pressure measurements. Participants excluded were those who did not complete the two-part psychological well-being survey, those with missing data required to classify them into the MetS categories, and those with missing gender identification. Sociodemographic and clinical characteristics of the current study sample (N = 13,496) are presented in Table 1.
Table 1.
Sample Sociodemographic and Clinical Characteristics for the Total Study Sample
| Variable | n (%) or M (SD) | Median | IQR |
|---|---|---|---|
|
| |||
| Age | 45.95 (13.94) | 48.00 | 20.00 |
| Years lived in US | 22.52 (15.35) | 20.00 | 22.00 |
| Gender | |||
| Women | 7,990 (59) | ||
| Men | 5,506 (41) | ||
| Hispanic heritage subgroup | |||
| Mexican | 4.984 (37) | ||
| Puerto Rican | 2,313 (17) | ||
| Cuban | 2,156 (16) | ||
| Central American | 1,454 (11) | ||
| Dominican | 1,238 (9) | ||
| South American | 895 (7) | ||
| ME/O | 431 (3) | ||
| US-born | |||
| Not US-born (50 US states) | 11,074 (82) | ||
| US-bom (50 US states) | 2,410 (18) | ||
| Education | |||
| No HS or GED | 4,326 (32) | ||
| At most HS or GED | 2,965 (22) | ||
| Greater than HS or GED | 4,290 (32) | ||
| Income | |||
| Less than 10,000 | 1,662 (12) | ||
| 10,001–20,000 | 3,450 (26) | ||
| 20,001–40,000 | 3,554 (26) | ||
| 40,001–75,000 | 1,430 (11) | ||
| More than 75,000 | 477 (4) | ||
| Cigarette pack years | |||
| 0 years | 8,105 (60) | ||
| >0 <10 years | 2,838 (21) | ||
| 10+ years | 2,260 (17) | ||
| Alcohol use | |||
| None | 7,042 (52) | ||
| Low level use | 5,735 (43) | ||
| High level use | 711 (5) | ||
| Physical activity | |||
| Low activity | 6,053 (45) | ||
| Moderate activity | 5,945 (44) | ||
| High activity | 1,449 (11) | ||
| Metabolic Syndrome | |||
| Yes | 5,230 (39) | ||
| No | 8,266 (61) | ||
| CESD-10 | 7.38 (6.17) | 6.00 | 8.00 |
| STAI-10 | 17.26 (5.88) | 16.00 | 9.00 |
| Mental health status | |||
| Depression and anxiety | 1,970 (15) | ||
| Depression or anxiety | 2,570 (19) | ||
| Neither | 8,956 (66) | ||
Note. N = 13,496. The proportion of missing data was pack years (2%), education (14%), and income (22%), <1% for all other variables. ME/O = multiple or other Hispanic ethnicities, US = United States, referring to 50 states and Washington, DC, exclusive of territories, HS = high school, GED = general education degree. CESD-10 = Center for Epidemiologic Studies Depression 10-item scale; STAI-10 = State-Trait Anxiety Inventory 10-item scale.
2.2. Measurements
2.2.1. Metabolic Syndrome
The primary outcome was the absence or presence of MetS, based on the NCEP-ATP III criteria. MetS is defined as having three of the following five criteria, including elevated fasting blood glucose (≥ 100 mg/dL), hypertension (blood pressure ≥ 130 mmHg systolic and ≥ 85 mmHg diastolic), elevated triglycerides (≥ 150 mg/dL), low high-density lipoprotein cholesterol (< 40 mg/dL for men and < 50 mg/dL for women), and increased waist circumference (> 102 cm or 40.2 inches in men and > 88 cm or 34.6 inches in women. Based on these criteria, participants were assigned to one of two groups using a dichotomous variable of 1 = no MetS (having two or fewer of the qualifying criteria) or 2 = presence of MetS. The group without MetS was used as the reference group.
2.2.2. Depression and Anxiety
The HCHS/SOL assessed mental health via two 10-item questionnaires that were available in English, Spanish, and could be read aloud to the participant (LaVange et al., 2010). The Center for Epidemiologic Studies Depression 10-item (CESD-10) scale has a possible total score ranging from 0–30, with higher scores indicating more significant depressive symptoms during the past week (Radloff, 1977). Participants responded to the ten items using a 4-point Likert scale [0 = rarely or none of the time (<1 day), 1 = some or a little of the time (1–2 days), 2 = occasionally or a moderate amount of time (3–4 days), and 3 = all of the time (5–7 days)]. Of the ten items, two were reverse coded. If one or two items were missing, the CESD-10 score equals the weighted average of the response items. An example of an item is: I was bothered by things that usually don’t bother me. The CESD-10 summary score was used as a continuous variable to indicate depression. The CESD-10 has been validated across age, gender, and race; high internal consistency has been reported, with an average Cronbach’s α coefficient between .85 to .90 and test-retest reliability across Hispanic subgroups with Pearson’s correlations from r = .42 to r = .78 (González, P. et al., 2017). The internal consistency in a subsample of the HCHS/SOL was α = 0.82 (Camacho et al., 2015).
The State-Trait Anxiety Inventory (STAI) is a tool used to measure transient and enduring anxiety levels (Spielberger et al., 1983). Internal consistency coefficients for the STAI range from .86 to .95 with test-retest reliability coefficients ranging from .65 to .89 (American Psychological Association, 2011). The HCSC/SOL used an abbreviated version of the STAI by selecting 10 items (STAI-10). Participants respond to each item of the STAI-10 using a 4- point Likert scale to describe how they generally feel (1 = almost never, 2 = sometimes, 3 = often, and 4 = always). An example of an item is: I feel nervous and restless. Of the ten items, three were reverse coded. If one or two items were missing, the STAI-10 equals the weighted average of the response items. STAI-10 total scores were a continuous variable ranging from 10–40, with higher scores indicating greater anxiety. The STAI has a coefficient α reliability estimate of .80 in Spanish and .84 in English (Castañeda et al., 2015). The internal consistency in a subsample of the HCHS/SOL was α = 0.81 (Camacho et al., 2015).
In addition to these individual scales for depression and anxiety, we also created a new 3-level categorical variable to address the multicollinearity of the continuous CESD-10 and STAI-10 scores and capture concurrent depression and anxiety (1 = concurrent depression and anxiety, 2 = either depression or anxiety, 3 = neither). Previous research informed the cut-off scores for depression and anxiety (Björgvinsson et al., 2013; Zsido et al., 2020). A score of ten or higher on the CESD-10 was suggestive of depression; a score of 23 or higher suggested anxiety.
2.2.3. Other Factors
The covariates included in these analyses were cigarette-pack years, alcohol consumption level, physical activity level, age (in years), whether US born, and total years lived in the US, exclusive of territories. These variables were all collected by the HCSC/SOL using self-report questionnaires. To measure cigarette pack-years, we created a 3-level categorical variable (0 = zero years; 1 = > 0 and < 10 years; 2 = 10+ years). Pack-years are the total number of years smoked, multiplied by the average number of cigarettes smoked per day, and then divided by twenty. To measure alcohol consumption, a 3-level categorical variable, delineated by the National Institute on Alcohol Abuse and Alcoholism, was used [0 = no current use, 1 = low level use (females = < 7 drinks/week, males = < 14 drinks/week) 2 = high level use (females, = 7+ drinks/week, males = 14+ drinks/week)]. Physical activity was collected using the Global Physical Activity Questionnaire (including activity from work, transportation, and leisure time) and delineated into a 3-categorical variable (0 = low, 1 = moderate, 2 = high).
Dichotomous variables included gender (0 = women; 1= men) and whether the participant was born in the US (0 = not US-born, 1 = US-born), excluding US territories. Heritage subgroups were measured using a 7-level categorical variable (0 = Dominican, 1 = Central American, 2 = Cuban, 3 = Puerto Rican, 4 = South American, 5 = multiple or other Hispanic heritage, 6 = Mexican). Mexicans were selected as the reference group due to their large sample size and because they are the most common Hispanic heritage subgroup in the US and represented in the literature. Education and income were also considered covariates but were not used in the final analyses as they were nonsignificant and did not alter the model results (results not shown).
2.3. Statistical Analyses
All data analyses were conducted using IBM SPSS software (version 28). Frequencies and percentages were obtained for categorical variables; mean and standard deviations were obtained for continuous variables. Gender-heritage differences were evaluated for each study variable. Chi-square tests assessed differences in MetS. Independent t-tests and one-way analysis of variance (ANOVA) models evaluated group differences in age, years lived in the US, and depression and anxiety scale scores. Post hoc analysis confirmed group differences. The Games-Howell procedure was employed due to unequal population variances in heritage background.
Logistic regression tested Hypothesis 1. CESD-10 scores and STAI-10 scores were tested separately. Due to the multicollinearity of the mental health variables, they were not added to the model simultaneously during the initial analysis. Instead, we further tested the overall association of mental health with MetS using the combined categorical variable (mental health status: 1 = concurrent depression and anxiety, 2 = either depression or anxiety, 3 = neither). Lifestyle variables of smoking, alcohol use, and physical activity, along with demographic variables of age, gender, Hispanic group heritage, US-born, and years lived in the US, were added to each model. Unadjusted parameter estimates were also obtained for all predictor variables. Adding depression, anxiety, and mental health status to the analytical model significantly improved the goodness of fit over the null model (results not shown). The analytical models including depression, anxiety, and mental health status have a receiver operating characteristic (ROC) curve of .70, .70, and .70, respectively. The current study sample size (N = 13,496) provided an observed 99% power to detect an association at the .05 alpha level for each logistic regression analysis. PROCESS macro for SPSS, version 4.1, Model 2 tested Hypothesis 2 (Hayes, 2013). Two-way interactions were assessed to determine whether gender and heritage subgroup membership moderated the effects of the mental health variables and MetS, controlling for demographic variables.
3. Results
3.1. Sociodemographic Characteristics of the Study Sample
Descriptive statistics for the study sample are presented in Table 1. The participants were 13,496 Hispanic Americans aged 18–74 (59% women, mean age 46.59 ± 13.65) self-identifying in one of seven distinct heritage subgroups. Gender and Hispanic heritage subgroup differences among age, years lived in the US, depression and anxiety scores, and MetS are presented in Table 2. Women had significantly higher depression, p < .001, and anxiety, p < .001, and MetS, p < .001, than men. One-way ANOVAs revealed heritage subgroup differences among age, p < .001; years lived in the US, p < .001; depression, p < .001; and anxiety scores, p < .001 (Table 2). Post hoc analyses using the Games-Howell procedure indicated that the mean depression scores (M = 9.15, SD = 6.56) and anxiety scores (M = 18.56, SD = 6.39) were significantly higher for Puerto Ricans than any other heritage group. Puerto Ricans also had the highest prevalence of MetS (45%) compared to South Americans (31%).
Table 2.
Gender and Heritage Differences in the absence or presence of MetS
| Variable | Age | Years lived in US | CESD-10 | STAI-10 | MetS n (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| M (SD) | P value | M (SD) | P value | M (SD) | P value | M (SD) | P value | Yes | No | P value | |
|
| |||||||||||
| Gender | |||||||||||
| Women | 46.59 (13.65) | <.001 | 22.32 (15.41) | .41 | 8.26 (6.54) | <.001 | 18.02 (6.20) | <.001 | 3,273 (41) | 4,717 (59) | <.001 |
| Men | 45.02 (14.28) | 22.81 (15.25) | 6.11 (5.34) | 16.20 (5.22) | 1,957 (36) | 3,549 (64) | |||||
| Hispanic heritage subgroup | |||||||||||
| Dominican | 45.15 (14.46) | <.001 | 18.79 (11.38) | <.001 | 7.35 (6.12) | <.001 | 17.08 (5.65) | <.001 | 417 (34) | 821 (66) | <.001 |
| C. American | 44.61 (13.36) | 16.31 (10.50) | 7.11 (6.08) | 16.69 (5.66) | 554 (38) | 900 (62) | |||||
| Cuban | 49.02 (13.11) | 14.27 (13.07) | 7.48 (6.74) | 16.71 (5.97) | 925 (43) | 1,231 (57) | |||||
| Mexican | 44.68 (13.80) | 22.81 (14.15) | 6.69 (5.60) | 17.24 (5.64) | 1,880 (38) | 3,104 (62) | |||||
| Puerto Rican | 48.18 (14.14) | 37.36 (14.72) | 9.15 (6.56) | 18.56 (6.39) | 1,030 (45) | 1,283 (55) | |||||
| S. American | 46.41 (13.33) | 15.86 (11.20) | 6.67 (5.92) | 16.44 (5.62) | 273 (31) | 622 (69) | |||||
| ME/O | 39.15 (14.97) | 26.09 (15.02) | 7.67 (6.31) | 17.13 (5.75) | 142 (33) | 289 (67) | |||||
Note. N = 13,496. CESD-10 = Center for Epidemiologic Studies Depression 10-item scale; STAI-10 = State-Trait Anxiety Inventory 10-item scale. C. American = Central American, S. American = South American, ME/O = Multiple or more than one Hispanic heritage. MetS = metabolic syndrome. Gender differences were tested with Independent t-tests; heritage subgroup differences were tested with one-way ANOVA. Gender and heritage differences were tested with Chi-square tests.
3.2. Hypothesis 1: Mental Health Symptoms Associated with MetS in Hispanic Subgroups
Depression (OR = 1.01, p < .001) and anxiety (OR = 1.01, p < .001) were each associated with the presence of MetS (Table 3). Table 4 presents additional analysis using the categorical mental health status variable. In this model, concurrent depression and anxiety were significantly associated with MetS (OR = 1.30, p < .001).
Table 3.
Binary Logistic Regression Analysis of the Presence or Absence of MetS for those with Depression and Anxiety Separately
| Variable | Depression | Anxiety | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| B (SE) | Wald X2 | OR (95%) | P value | B (SE) | Wald X2 | OR (95%) | P value | |
|
| ||||||||
| Depression | .01 (.00) | 13.94 | 1.01 (1.01-1.02) | <.001 | -- | -- | -- | |
| Anxiety | -- | -- | -- | .01 (.00) | 13.61 | 1.01 (1.01–1.02) | < .001 | |
| Age | .05 (.00) | 722.62 | 1.05 (1.05–1.06) | <.001 | .05 (.00) | 729.59 | 1.05 (1.05–1.06) | < .001 |
| Years lived in US | .00 (.00) | .28 | 1.00 (.99–1.00) | .59 | .01 (.00) | .39 | 1.00 (.99–1.01) | .53 |
| Gender (Reference group: men) | ||||||||
| Women | .09 (.04) | 4.05 | 1.09 (1.00–1.19) | .04 | .09 (.04) | 4.57 | 1.10 (1.01–1.19) | .03 |
| Heritage background (Reference group: Mexican) | ||||||||
| Dominican | −.22 (.07) | 9.15 | .80 (.70–.93) | .002 | −.21 (.07) | 8.36 | .81 (.70–.94) | .004 |
| C. American | .01 (.07) | .01 | 1.01 (.88–1.15) | .93 | .02 (.07) | .07 | 1.02 (.89–1.16) | .79 |
| Cuban | −.01 (.06) | .07 | .99 (.84–1.11) | .80 | .00 (.06) | .00 | 1.00 (.89–1.13) | .99 |
| Puerto Rican | .05 (.06) | .56 | 1.05 (.93–1.18) | .46 | .06 (.06) | .83 | 1.06 (.94–1.19) | .36 |
| S. American | −.43 (.08) | 25.41 | .65 (.55–.77) | < .001 | −.41 (.08) | 24.10 | .66 (.56–.78) | < .001 |
| ME/O | .02 (.12) | .02 | 1.02 (.80–1.29) | .83 | .03 (.12) | .07 | 1.03 (.82–1.31) | .79 |
| Alcohol Use (Reference group: no use) | ||||||||
| Low level use | −.26 | 39.91 | .77 (.71–84) | < .001 | −.26 (.04) | 39.83 | .77 (.71–84) | < .001 |
| High level use | −.09 (.09) | 1.03 | .91 (.76–1.09) | .31 | −.09 (.09) | 1.00 | .91 (.76-1.09) | .32 |
| Cigarette Pack Years (Reference group: none) | ||||||||
| > 0, < 10 years | .07 | 1.81 | 1.07 (.97–1.18) | .18 | .07 (.05) | 1.98 | 1.07 (.97–1.18) | .16 |
| 10+ years | .07 (.06) | 1.80 | 1.08 (.97–1.20) | .18 | .07 (.06) | 1.86 | 1.08 (.97–1.20) | .17 |
| Activity (Reference group: low level activity) | ||||||||
| Moderate level | −.20 (.04) | 24.62 | .82 (.75–.89) | < .001 | −.20 (.04) | 24.54 | .82 (.75–.89) | < .001 |
| High level | −.27 (.07) | 14.90 | .76 (.66–.87) | < .001 | −.27 (.04) | 14.43 | .77 (.67–.88) | < .001 |
| US-born (Reference group: born in US) | ||||||||
| Not US-born | −.09 (.07) | 1.45 | .92 (.80–1.05) | .23 | −.08 (.07) | 1.41 | .92 (.80–1.06) | .24 |
Note. N = 13,496. MetS = metabolic syndrome, C. American = Central American, S. American = South American, ME/O = Multiple or more than one Hispanic heritage. Reference group for the dependent variable is no MetS.
Table 4.
Binary Logistic Regression Analysis of the Presence or Absence of MetS in Mental Health Conditions
| Variable | B (SE) | Wald x2 | OR (95%) | p value |
|---|---|---|---|---|
|
| ||||
| Mental Health Status (Reference group: neither) | ||||
| Depression and anxiety | .27 (.06) | 22.80 | 1.30 (1.17–1.45) | < .001 |
| Depression or anxiety | .06 (.05) | 1.39 | 1.06 (.96–1.17) | .24 |
| Age | .05 (.00) | 724.56 | 1.05 (1.05–1.06) | < .001 |
| Years lived in US | .00 (.00) | .26 | 1.00 (.99–1.00) | .61 |
| Gender (Reference group: men) | ||||
| Women | .09 (.04) | 3.99 | 1.09 (1.00–1.19) | .046 |
| Hispanic heritage subgroup (Reference group: Mexican) | ||||
| Dominican | −.22 (.07) | 8.73 | .81 (.70-.93) | .003 |
| C. American | .01 (.07) | .02 | 1.01 (.89–1.15) | .88 |
| Cuban | −.01 (.06) | .03 | .99 (.88–1.11) | .86 |
| Puerto Rican | .05 (.06) | .55 | 1.05 (.93–1.18) | .46 |
| S. American | −.42 (.08) | 25.26 | .65 (.56–.77) | < .001 |
| ME/O | −.02 (.12) | .03 | 1.02 (.81–1.29) | .87 |
| Alcohol Use (Reference group: no use) | ||||
| Low level use | −.26 (.04) | 38.98 | .77 (.71–84) | < .001 |
| High Level use | −.10 (.09) | 1.07 | .91 (.76–1.09) | .30 |
| Cigarette Pack Years (Reference group: none) | ||||
| > 0, < 10 years | .07 (.05) | 1.76 | 1.07 (.97–1.18) | .19 |
| 10+ years | .07 (.06) | 1.07 | 1.07 (.96–1.19) | .20 |
| Activity (Reference group: low level activity) | ||||
| Moderate Activity | −.20 (.04) | 24.35 | .82 (.76–.89) | < .001 |
| High Activity | −.27 (.07) | 14.63 | .76 (.67–.88) | < .001 |
| US-born (Reference group: born in the US) | ||||
| Not born in US | −.09 (.07) | 1.54 | .92 (.80–1.05) | .22 |
Note. N = 13,496. MetS = metabolic syndrome. C. American = Central American, S. American = South American, ME/O = Multiple or more than one Hispanic heritage. Reference group for the dependent variable is no MetS.
Gender, heritage subgroup, age, alcohol use, cigarette pack years, activity level, whether US-born, and years lived in the US were added to the model as covariates (Table 3). Compared to men, women were more likely to be classified as having MetS in both the model including depression (OR = 1.09, p = .04) and anxiety (OR = 1.10, p = .03). Compared to Mexicans, Dominicans and South Americans were less likely to evidence an association between depression (OR = 0.80, p = .002, OR = 0.65, p < .001) and anxiety (OR = 0.81, p = .004, OR = 0.66, p < .001), respectively, with MetS. US-born and years lived in the US were not significant in either model. The covariate results in the mental health status and MetS analyses were similar, as presented in Table 4. Univariate logistic regression analysis of the presence or absence of MetS in mental health conditions and other factors are presented in Table 5.
Table 5.
Univariate Logistic Regression Analysis of the Presence or Absence of MetS in Mental Health Conditions and Other Factors
| Variable | B (SE) | Wald x2 | OR (95%) | p value |
|---|---|---|---|---|
|
| ||||
| Depression | .02 (.00) | 64.26 | 1.02 (1.02–1.03) | < .001 |
| Anxiety | .02 (.00) | 26.29 | 1.02 (1.01–1.02) | < .001 |
| Mental health status (Reference group: neither) | ||||
| Depression and anxiety | .40 (.05) | 64.76 | 1.50 (1.36–1.65) | < .001 |
| Depression or anxiety | .21 (.05) | 21.13 | 1.23 (1.13–1.35) | < .001 |
| Age | .05 (.00) | 1299.42 | 1.06 (1.05–1.06) | < .001 |
| Years lived in US | .02 (.00) | 257.12 | 1.02 (1.02–1.02) | < .001 |
| Gender (Reference group: men) | ||||
| Women | .23 (.04) | 40.30 | 1.26 (1.17–1.35) | < .001 |
| Hispanic heritage subgroup (Reference group: Mexican) | ||||
| Dominican | −.18 (.07) | 6.93 | .84 (.74–.96) | .008 |
| C. American | .02 (.06) | .07 | 1.02 (.90–1.15) | .79 |
| Cuban | .22 (.05) | 16.92 | 1.24 (1.12–1.38) | < .001 |
| Puerto Rican | .28 (.05) | 30.49 | 1.33 (1.20–1.47) | < .001 |
| S. American | −.32 (.08) | 16.93 | .73 (.62–.85) | < .001 |
| ME/O | −.21 (.11) | 3.85 | .81 (.66–1.00) | .050 |
| Alcohol Use (Reference group: no use) | ||||
| Low level use | −.44 (.04) | 143.90 | .64 (.60–.69) | < .001 |
| High Level use | −.38 (.09) | 21.48 | .68 (.58–.80) | < .001 |
| Cigarette Pack Years (Reference group: none) | ||||
| > 0, < 10 years | .01 (.05) | .02 | 1.00 (.92–1.10) | .90 |
| 10+ years | .47 (.05) | 93.80 | 1.59 (1.45–1.75) | < .001 |
| Activity (Reference group: low level activity) | ||||
| Moderate Activity | −.35 (.04) | 86.83 | .71 (.45–.58) | < .001 |
| High Activity | −.68 (.06) | 112.68 | .51 (.66–.76) | < .001 |
| US-born (Reference group: born in the US) | ||||
| Not born in US | .45 (.05) | 85.17 | 1.56 (1.42–1.72) | < .001 |
Note. N = 13,496. MetS = metabolic syndrome. C. American = Central American, S. American = South American, ME/O = Multiple or more than one Hispanic heritage. Reference group for the dependent variable is no MetS.
3.3. Hypothesis 2: Moderation Analysis in Hispanic Subgroups
Using the PROCESS macro, a two-way interaction between each gender and heritage subgroup membership and each CESD-10, STAI-10, and the 3-level mental health status variable were added to the logistic regression models. Moderation effects were identified for gender in the relationship between depression and MetS [R2 = .19, F(18, 13,415) = 172.60, p < .001] and anxiety and MetS [R2 = .19, F(18, 13,415) = 171.95, p < .001]. Moderation analysis conducted with the mental health status variable also demonstrated significant results for gender, moderating the relationship between mental health status and MetS [R2 = .19, F(26, 13,407) = 120.25, p < .001]. As presented in Figure 2, women with higher CESD-10 or higher STAI-10 scores had a stronger association with MetS than men. Women who had either depression or anxiety, or a combination of both, also had a stronger association with MetS. Heritage subgroup moderation results were not significant. Complete results from Hypothesis 2 analyses were not presented as the significance of CESD-10, STAI-10, and the mental health status variables were unchanged after the interaction terms were added to the logistic regression.
4. Discussion
The current study examined the association of depression and anxiety and MetS, as well as the association between overall mental health (depression and anxiety combined) with MetS among US Hispanic subgroups. In addition, this study assessed potential gender-heritage subgroup moderation of these relationships. Hypothesis 1 was partially supported in that higher depression and anxiety scores were each associated with an increased cardiometabolic risk as evidenced by the presence of MetS. The combined presence of depression and anxiety was similarly associated with MetS. These findings suggest an association between mental health and physical health across diverse Hispanic subgroups.
These findings are consistent with other studies identifying an association between mental health conditions and MetS (Pan et al., 2012; Shinkov et al., 2018; Tang et al., 2017). Previous data suggests that inactivity, tobacco smoking, alcohol abuse, and poor diet quality are associated with depression in the US and could compound metabolic risk associated with depression (Castañeda et al., 2015; Goldbacher et al., 2009; Liu et al., 2017). Although the association between anxiety and MetS is inconsistent in the literature, accumulating evidence supports this connection (Tang et al., 2017). Concurrent depression and anxiety results were each associated with the presence of MetS. The presence of both depression and anxiety increased the likelihood of someone being classifies as having MetS (OR = 1.30, risk ratio = 1.10). Similar to depression, anxiety is associated with HPA dysregulation and inflammation, which are known to be significant contributors in the development of MetS (Pasquali et al., 2006; Powers et al., 2016). Further, medications used to treat anxiety and depression have adverse effects including weight gain, dyslipidemia, and glucose dysregulation compounding the risk and progression of MetS (Corruble et al., 2015; Van Reedt Dortland et al., 2010).
Hypothesis 2 was partially supported in that gender moderated the relationship between mental health status and MetS. Gender moderation on the association of depression, anxiety, and concurrent depression and anxiety with MetS demonstrates that as the burden of mental health symptoms increase, the likelihood of MetS increases more sharply in women than in men. These results underscore the relationship between depression and anxiety on physiologic health in women. Although depression and anxiety are associated with MetS in studies of men (Powers et al., 2016; Shinkov et al., 2018), previous findings largely support the increased physiologic impact of depression and anxiety in women (Butnoriene et al., 2015; Goldbacher et al., 2009; Kim et al., 2015; Shinkov et al., 2018). MetS, depression, and anxiety were predictors of greater 10-year mortality in women but not in men (Butnoriene et al., 2015). Taken together, these findings emphasize psychological and behavioral health as a critical component of holistic, or whole person health (National Center for Complementary and Integrative Health, 2021). Best practices use a biopsychosocial perspective to assess and conceptualize interplay between various medical, psychological, and sociocultural factors, such as the link between mental health and MetS, in patients or research participants. The corresponding movement towards integrated primary care (Funderburk et al., 2021) is pivotal in assessing and addressing behavioral and psychological contributions to physical health. Likewise, a newer ―reverse integrated care‖ model is emerging that situates primary care in traditionally specialized mental health care settings (Maragakis et al., 2016). Both models acknowledge the link between mental (e.g., depression, anxiety) and physical (e.g., MetS) health.
Despite our findings of a moderating effect by gender, the rest of Hypothesis 2 was not supported in that Hispanic heritage subgroup membership did not moderate these relationships. The lack of moderation by heritage subgroups could indicate the uniform relevance of mental health on MetS across the subgroups or that the other demographic variables (e.g., ethnic differences within these nationalities) in the model covaried with depression and anxiety. Although the heritage subgroup moderation results were not significant, Puerto Ricans had the highest mean scores of both depression and anxiety scores among all Hispanic heritage subgroups. Supporting a similar pattern, according to national survey data, Puerto Ricans had the highest prevalence of 12-month and lifetime major depression among various US heritage groups, including non-Hispanic Whites, African Americans, Chinese, Mexican Americans, Cubans, and Black Caribbeans (González et al., 2010). Understanding such differences among Hispanic subgroups deserves further attention. Various factors, such as the psychological consequences of US colonization in Puerto Rico (Capielo Rosario et al., 2019) to the cultural syndrome of ataque de nervios, an expression of distress among Hispanic subgroups that is similar to anxiety or panic (Moitra et al., 2018), may play a significant role in the prevalence of anxiety symptomatology among Hispanic individuals in comparison to non-Hispanic Whites. Conversely, South Americans had the lowest mean scores of depression and anxiety and a significantly lower risk of being in each of the MetS subgroups. Further research is warranted to investigate protective factors among diverse heritage subgroups.
Health promotion implications derived from our findings include physiological, psychological, and sociocultural components. Lifestyle interventions aimed at the reduction of MetS-related risk factors include reduction of smoking and heavy alcohol use, promotion of a healthy diet, increased physical activity, and weight reduction (Allison et al., 2008; Daviglus et al., 2012). Recent guidelines from the American Diabetes Association recommend individualized nutrition counseling to promote potentially beneficial diet patterns, including Mediterranean-style, low-carbohydrate eating, the dietary approaches to stop hypertension (DASH) diet, and plant-based diets, as well as 150 minutes/week of moderate-intensity workouts to prevent or delay T2DM (ElSayed et al., 2023). Behavioral interventions and pharmacological adherence can aid in the reduction of lipid levels, blood pressure, and glycemic control. Cognitive behavioral therapy and other evidence-based psychotherapies can help manage or reduce symptoms of depression and anxiety while improving quality of life and well-being; indeed, managing these psychological symptoms may help improve physical health and support health behavioral change, such as exercise (Lu et al., 2021). However, engaging a patient in health behavior change necessitates clinicians consider complex social determinants of individual health.
Reducing the incidence and prevalence of MetS may be more complex for Latina women than for other patient groups as they face unique barriers in seeking care and maintaining health in the US. There is limited data on the most effective and culturally-responsive health promotion strategies for Hispanic women. Care providers must assess and understand cultural practices and strengths that can best support whole-person health for this underserved and vulnerable population. Inclusion of sociocultural practices and values–such as centering familism (familisimo), personal relationships (personalismo), respect (respecto), and kindness (simpatia; Garcia, 2016) in care–may promote adherence to health promotion strategies and optimize health. One way to support Latinas is to support their agency and encourage acculturation into Western healthcare in a way that they direct; for example, integrating components of the new culture while maintaining traditions from their own culture, which has been shown to promote psychological well-being (Buckingham & Suarez-Pedraza, 2019). Folk practices, herbal remedies, and other alternative therapies can often be safely integrated into conventional treatments (Juckett, 2013).
5. Study Limitations and Directions for Future Research
This study used a cross-sectional design, created from the HCHS/SOL’s first phase in an observational cohort from four urban centers across the US. This design permits inferences of association but not directionality, prediction, and causality. Potential recall or other response bias may be a limitation in this study, as the questionnaires were all self-reported. This cohort is not from a nationally representative sample, nor does it explore rural populations with distinct psychological and health care needs; therefore, these findings cannot be translated across US communities. Rather, the selected communities are diverse, with high concentrations of Hispanic subgroups yielding the opportunity to explore cardiometabolic risk factors with significant breadth (Sorlie et al., 2010). The data used for this study is from the initial phase of HCHS/SOL data collection (2008–2011). While dated, it is still the most recent data to fill the knowledge gap of the relationship between mental health conditions and MetS among Hispanic/Latino heritage subgroups in the US. While prevalence estimates of specific conditions may vary, there is no indication that the pathophysiology of mental health conditions and their relationship to MetS change over time. However, it builds on the extant literature by exploring granularity in US Hispanic heritage subgroups. Recommendations for future research include longitudinal design with subsequent visits of the HCHS-SOL study to examine the direction of influence and causation.
This study is limited to discussing the relationships of current mental health status and MetS in Hispanic populations, as we did not assess the effect of psychiatric medication and biological markers. Prospective studies are needed to confirm the potential causal effect of depression and anxiety on the development of MetS. Investigating MetS-related and psychiatric medication use could be essential for future research in understanding the pathophysiological overlap between MetS and mental health. Finally, the concept of acculturation includes lifestyle and attitudinal changes due to living in a non-native culture; it is one potential cultural determinant of health that also requires examination while investigating disease patterns. However, variables to adequately describe acculturation were not available in this dataset. Further investigation of the influence of acculturation on psychological symptoms and health outcomes is recommended.
6. Conclusion
In summary, increased depression and anxiety are associated with MetS in US Hispanic gender-heritage subgroups and there are significant gender differences in these associations. Hispanic women with depression, anxiety, or both, face a higher likelihood of MetS compared to Hispanic men. Puerto Ricans had the highest levels of depression and anxiety, whereas South Americans had the lowest levels in each category. Concurrent depression and anxiety increase the likelihood of MetS. Early detection and treatment of depression and anxiety may decrease the severity of MetS and its sequelae. These findings necessitate initiating and reinforcing health-promoting behavioral interventions to reduce depression and anxiety and promote cardiometabolic health in US Hispanic populations.
Figure 1.
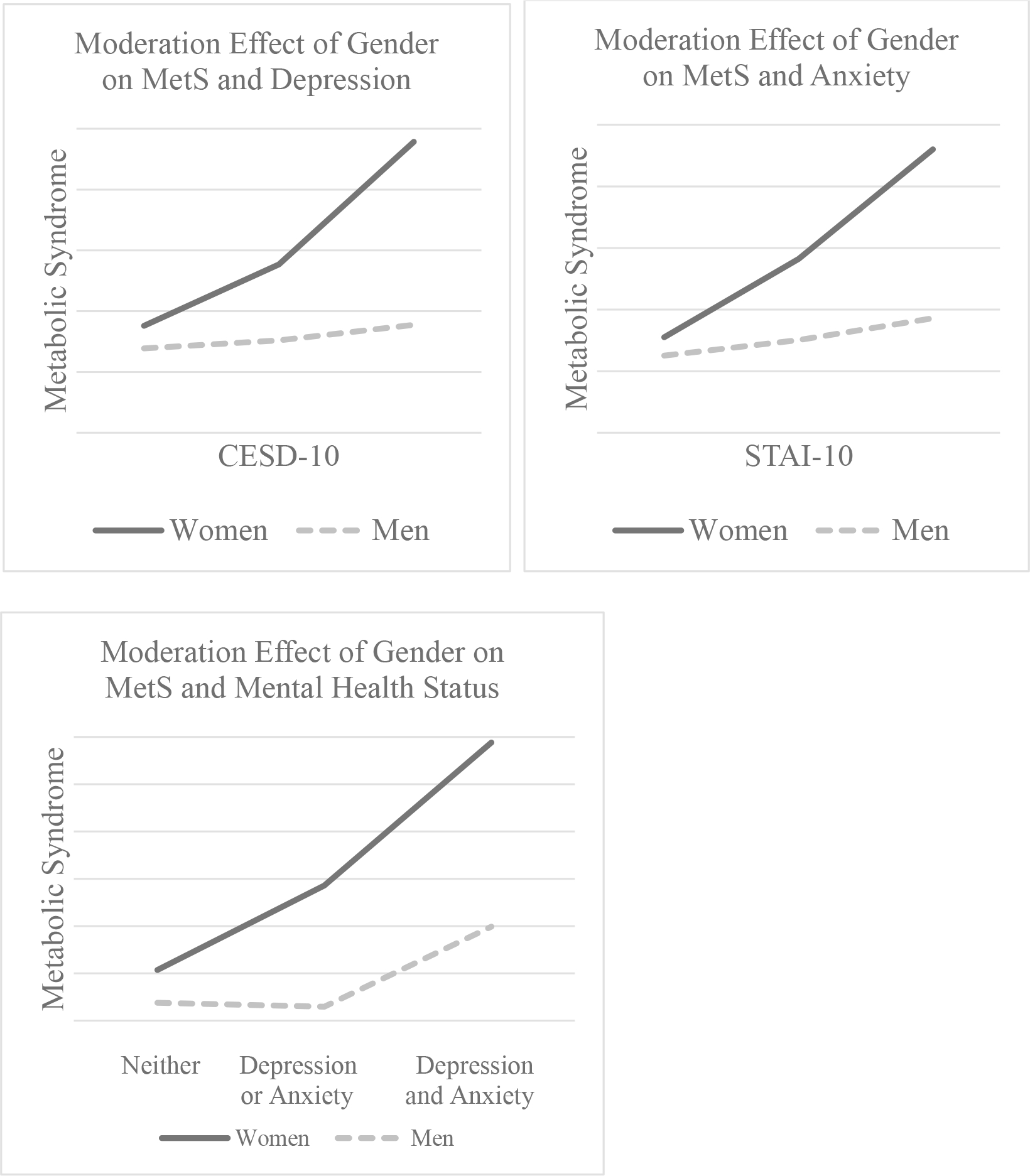
Moderation Effect of Gender on MetS and Mental Health Status
Highlights.
Anxiety increases the likelihood of metabolic syndrome (MetS) in Hispanic subgroups
Depression increases the likelihood of MetS in Hispanic subgroups
Gender moderates the relationship between mental health conditions and MetS
7. Acknowledgements
Acknowledgement of people
The authors thank the staff and participants of HCHS/SOL for their important contributions. A complete list of staff and investigators is also available on the study website http://www.cscc.unc.edu/hchs/
Funding
The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following Institutes/Centers/Offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: National Center on Minority Health and Health Disparities, the National Institute of Deafness and Other Communications Disorders, the National Institute of Dental and Craniofacial Research, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Neurological Disorders and Stroke, and the Office of Dietary Supplements.
Dr. Renn’s effort is supported in part by the National Institute of General Medical Sciences (grant P20 GM103440).
Footnotes
Declarations of Interest: none
Submission declaration and verification: The work described has not previously been published, nor is it under review elsewhere. This study is a secondary data analysis from Visit 1 of the Hispanic Community Health Study / Study of Latinos (HCHS/SOL). The larger study expands the literature on US Hispanic/Latino health by describing risk profiles contributing to cardiometabolic disease. The paper expands upon this goal with its unique study design.
Disclosure Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The authors had full access to the study data and took responsibility for the data’s integrity and the analyses’ accuracy. All authors have reviewed and approved the final manuscript. None of the authors had any financial or other conflicts of interest. This article does not contain any studies with animals performed by any of the authors.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Shannon L. Richard, 336 Blooming Sage Way, Sparks, NV 89441, 775-857-8692.
Brenna N. Renn, 4505 S Maryland Pky, Las Vegas, NV 89154.
Jinyoung Kim, 4505 S Maryland Pky, Las Vegas, NV 89154.
Dieu-My T. Tran, 4505 S Maryland Pky, Las Vegas, NV 89154.
Du Feng, 4505 S Maryland Pky, Las Vegas, NV 89154.
Data Statement:
Data is available upon request.
References
- Aguayo-Mazzucato C, Diaque P, Hernandez S, Rosas S, Kostic A, & Caballero AE (2019). Understanding the growing epidemic of type 2 diabetes in the Hispanic population living in the United States. Diabetes/Metabolism Research and Reviews, 35(2), e3097–n/a. 10.1002/dmrr.3097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alberti K, Zimmet P, & Shaw J (2006). Metabolic syndrome-a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabetic Medicine, 23(5), 469–480. 10.1111/j.1464-5491.2006.01858.x [DOI] [PubMed] [Google Scholar]
- Alegría, Canino G, Shrout PE, Woo M, Duan N, Vila D, Torres M, Chen C, & Meng X-L (2008). Prevalence of Mental Illness in Immigrant and Non-Immigrant U.S. Latino Groups. The American Journal of Psychiatry, 165(3), 359–369. 10.1176/appi.ajp.2007.07040704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison MA, Budoff MJ, Wong ND, Blumenthal RS, Schreiner PJ, & Criqui MH (2008). Prevalence of and risk factors for subclinical cardiovascular disease in selected US Hispanic ethnic groups: the Multi-Ethnic Study of Atherosclerosis. American Journal of Epidemiology, 167(8), 962–969. 10.1093/aje/kwm402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association. (2011). The State-Trait Anxiety Inventory (STAI). American Psychological Association. https://www.apa.org/pi/about/publications/caregivers/practice-settings/assessment/tools/trait-state [Google Scholar]
- Björgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, & Aderka IM (2013). Psychometric Properties of the CES-D-10 in a Psychiatric Sample. Assessment (Odessa, Fla.), 20(4), 429–436. 10.1177/1073191113481998 [DOI] [PubMed] [Google Scholar]
- Brunner EJ, Hemingway H, Walker BR, Page M, Clarke P, Juneja M, Shipley MJ, Kumari M, Andrew R, Seckl JR, Papadopoulos A, Checkley S, Rumley A, Lowe GDO, Stansfeld SA, & Marmot MG (2002). Adrenocortical, Autonomic, and Inflammatory Causes of the Metabolic Syndrome: Nested Case-Control Study. Circulation, 106(21), 2659–2665. 10.1161/01.CIR.0000038364.26310.BD [DOI] [PubMed] [Google Scholar]
- Buckingham SL & Suarez-Pedraza MC (2019). “It has cost me a lot to adapt to here”: The Divergence of Real Acculturation From Ideal Acculturation Impacts Latinx Immigrants’ Psychosocial Wellbeing. American Journal of Orthopsychiatry, 89(4), 406–419. 10.1037/ort0000329 [DOI] [PubMed] [Google Scholar]
- Burroughs Peña M, Swett K, Schneiderman N, Spevack DM, Ponce SG, Talavera GA, Kansal MM, Daviglus ML, Cai J, Hurwitz BE, Llabre MM, & Rodriguez CJ (2018). Cardiac structure and function with and without metabolic syndrome: the Echocardiographic Study of Latinos (Echo-SOL). BMJ Open Diabetes Research & Care, 6(1), e000484. 10.1136/bmjdrc-2017-000484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butnoriene J, Bunevicius A, Saudargiene A, Nemeroff CB, Norkus A, Ciceniene V, & Bunevicius R (2015). Metabolic syndrome, major depression, generalized anxiety disorder, and ten-year all-cause and cardiovascular mortality in middle aged and elderly patients. International Journal of Cardiology, 190, 360–366. 10.1016/j.ijcard.2015.04.122 [DOI] [PubMed] [Google Scholar]
- Camacho Á, Gonzalez P, Buelna C, Emory KT, Talavera GA, Castañeda SF, Espinoza RA, Howard AG, Perreira KM, Isasi CR, Daviglus ML, & Roesch SC (2015). Anxious-depression among Hispanic/Latinos from different backgrounds: results from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Social Psychiatry and Psychiatric Epidemiology, 50(11), 1669–1677. 10.1007/s00127-015-1120-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capielo Rosario C, Schaefer A, Ballesteros J, Rentería R, & David EJR (2019). A Caballo Regalao no se le Mira el Colmillo: Colonial Mentality and Puerto Rican Depression. Journal of Counseling Psychology, 66(4), 396–408. 10.1037/cou0000347 [DOI] [PubMed] [Google Scholar]
- Cassells H, & Haffner S (2006). The Metabolic Syndrome: Risk Factors and Management. The Journal of Cardiovascular Nursing, 21(4), 306–313. 10.1097/00005082-200607000-00012 [DOI] [PubMed] [Google Scholar]
- Castañeda SF, Buelna C, Giacinto RE, Gallo LC, Sotres-Alvarez D, Gonzalez P, Fortmann AL, Wassertheil-Smoller S, Gellman MD, Giachello AL, & Talavera GA (2015). Cardiovascular disease risk factors and psychological distress among Hispanics/Latinos: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Preventive Medicine, 87, 144–150. 10.1016/j.ypmed.2016.02.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cena H, Fonte ML, & Turconi G (2011). Relationship between smoking and metabolic syndrome. Nutrition Reviews, 69(12), 745–753. 10.1111/j.1753-4887.2011.00446.x [DOI] [PubMed] [Google Scholar]
- Cook B, Alegria M, Lin JY, & Guo J (2009). Pathways and Correlates Connecting Latinos’ Mental Health With Exposure to the United States. American Journal of Public Health, 99(12), 2247–2254. 10.2105/AJPH.2008.137091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corruble E, El Asmar K, Trabado S, Verstuyft C, Falissard B, Colle R, Petit A, Gressier F, Brailly-Tabard S, Ferreri F, Lépine J, Haffen E, Polosan M, Bourrier C, Perlemuter G, Chanson P, Fève B, & Becquemont L (2015). Treating major depressive episodes with antidepressants can induce or worsen metabolic syndrome: results of the METADAP cohort. World Psychiatry, 14(3), 366–367. 10.1002/wps.20260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daviglus ML, Talavera GA, Avilés-Santa ML, Allison M, Cai J, Criqui MH, Gellman M, Giachello AL, Gouskova N, Kaplan RC, LaVange L, Penedo F, Perreira K, Pirzada A, Schneiderman N, Wassertheil-Smoller S, Sorlie PD, & Stamler J (2012). Prevalence of Major Cardiovascular Risk Factors and Cardiovascular Diseases Among Hispanic/Latino Individuals of Diverse Backgrounds in the United States. JAMA: the Journal of the American Medical Association, 308(17), 1775–1784. 10.1001/jama.2012.14517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, Collins BS, Hilliard ME, Isaacs D, Johnson EL, Kahan S, Khunti K, Leon J, Lyons SK, Perry ML, Prahalad P, Pratley RE, Seley JJ, Stanton RC, & Gabbay RA (2023). Prevention or Delay of Type 2 Diabetes and Associated Comorbidities: Standards of Care in Diabetes-2023. Diabetes Care, 46(Supplement_1), S41–S48. 10.2337/dc23-S003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Figuereo V & Calvo R (2022). Racialization and Psychological Distress among U.S. Latinxs. Journal of Racial and Ethnic Health Disparities, 9(3), 865–873. 10.1007/s40615-021-01026-3 [DOI] [PubMed] [Google Scholar]
- Funderburk JS, Polaha J, & Beehler GP (2021). What is the recipe for PCBH? Proposed resources, processes, and expected outcomes. Families Systems & Health, 39(4), 551–562. 10.1037/fsh0000669 [DOI] [PubMed] [Google Scholar]
- Garcia DS (2016). Evaluation of 3 Behavioral Theories for Application in Health Promotion Strategies for Hispanic Women. Advances in Nursing Science, 39(2), 165–180. 10.1097/ANS.0000000000000116 [DOI] [PubMed] [Google Scholar]
- Goldbacher EM, Bromberger J, & Matthews KA (2009). Lifetime history of major depression predicts the development of the metabolic syndrome in middle-aged women. Psychosomatic Medicine, 71(3), 266–272. 10.1097/PSY.0b013e318197a4d5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- González HM, Tarraf W, Whitfield KE, & Vega WA (2010). The epidemiology of major depression and ethnicity in the United States. Journal of Psychiatric Research, 44(15), 1043–1051. 10.1016/j.jpsychires.2010.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- González P, Nuñez A, Merz E, Brintz C, Weitzman O, Navas EL, Camacho A, Buelna C, Penedo FJ, Wassertheil-Smoller S, Perreira K, Isasi CR, Choca J, Talavera GA, & Gallo LC (2017). Measurement Properties of the Center for Epidemiologic Studies Depression Scale (CES-D 10): Findings From HCHS/SOL. Psychological Assessment, 29(4), 372–381. 10.1037/pas0000330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis. Guilford Press. [Google Scholar]
- Heiss G, Snyder ML, Loehr L, Aviles-Santa L, Yanping T, Schneiderman N, Llabre MM, Cowie C, Carnethon M, Kaplan R, Giachello A, & Gallo L (2014). Prevalence of metabolic syndrome among Hispanics/Latinos of diverse background: The Hispanic community health study/study of Latinos. Diabetes Care, 37(8), 2391–2399. 10.2337/dc13-2505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirode G, & Wong RJ (2020). Trends in the prevalence of metabolic syndrome in the United States, 2011–2016. Journal of the American Medical Association, 323(24), 2526–2528. 10.1001/jama.2020.4501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juckett G (2013). Caring for Latino Patients. American Family Physician, 87(1), 48–54. [PubMed] [Google Scholar]
- Kim EY, Kim SH, Ha K, Lee HJ, Yoon DH, & Ahn YM (2015). Depression trajectories and the association with metabolic adversities among the middle-aged adults. Journal of Affective Disorders, 188, 14–21. 10.1016/j.jad.2015.08.024 [DOI] [PubMed] [Google Scholar]
- LaVange LM, Kalsbeek WD, Sorlie PD, Avilés-Santa Larissa M.,, Kaplan RC, Barnhart Janice, Liu K, Giachello A, Lee DJ, Ryan J, Criqui Michael H., & Elder John P.. (2010). Sample Design and Cohort Selection in the Hispanic Community Health Study/Study of Latinos. Annals of Epidemiology, 20(8), 642–649. 10.1016/j.annepidem.2010.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lett HS, Blumenthal JA, Babyak MA, Sherwood A, Strauman T, Robins C, & Newman MF (2004). Depression as a Risk Factor for Coronary Artery Disease: Evidence, Mechanisms, and Treatment. Psychosomatic Medicine, 66(3), 305–315. 10.1097/01.psy.0000126207.43307.c0 [DOI] [PubMed] [Google Scholar]
- Liu Y, Ozodiegwu ID, Yu Y, Hess R, & Bie R (2017). An Association of Health Behaviors with Depression and Metabolic Risks: Data from 2007–2014 U.S. National Health and Nutrition Examination Survey. Journal of Affective Disorders, 217, 190–196. 10.1016/j.jad.2017.04.009 [DOI] [PubMed] [Google Scholar]
- Lu X, Yang D, Liang J, Xie G, Li X, Xu C, Liao H, Zhou H, Xu Z, Ye C, Chen H, Liang M, Shen Q, Sun T, Hu Y, Zhang W, & Ning Y (2021). Effectiveness of intervention program on the change of glycaemic control in diabetes with depression patients: A meta-analysis of randomized controlled studies. Primary Care Diabetes, 15(3), 428–434. 10.1016/j.pcd.2021.01.006 [DOI] [PubMed] [Google Scholar]
- Lucas JW, Freeman G, & Adams PF (2016). Health of Hispanic adults: United States, 2010–2014. (Report No. 251). Retrieved from https://www.cdc.gov/nchs/products/databriefs/db251.htm [PubMed] [Google Scholar]
- Maragakis A, Siddharthan R, RachBeisel J, & Snipes C (2016). Creating a ‗reverse’ integrated primary and mental healthcare clinic for those with serious mental illness. Primary Health Care Research & Development, 17(5), 421–427. 10.1017/S1463423615000523 [DOI] [PubMed] [Google Scholar]
- McKnight-Eily LR, Okoro CA, Strine TW, Verlenden J, Hollis ND, Njai R, Mitchell EW, Board A, Puddy R, & Thomas C (2021). Racial and Ethnic Disparities in the Prevalence of Stress and Worry, Mental Health Conditions, and Increased Substance Use Among Adults During the COVID-19 Pandemic - United States, April and May 2020. MMWR. Morbidity and Mortality Weekly Report, 70(5), 162–166. 10.15585/mmwr.mm7005a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moitra E, Duarte-Velez Y, Lewis-Fernández R, Weisberg RB, & Keller MB (2018). Examination of ataque de nervios and ataque de nervios like events in a diverse sample of adults with anxiety disorders. Depression and Anxiety, 35(12), 1190–1197. 10.1002/da.22853 [DOI] [PubMed] [Google Scholar]
- Moore JX, Chaudhary N, & Akinyemiju T (2017). Metabolic syndrome prevalence by race/ethnicity and sex in the United States, National Health and Nutrition Examination Survey, 1988–2012. Preventing Chronic Disease, 14, E24. 10.5888/pcd14.160287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moradi Y, Albatineh AN, Mahmoodi H, & Gheshlagh RG (2021). The relationship between depression and risk of metabolic syndrome: a meta-analysis of observational studies. Clinical Diabetes and Endocrinology, 7(1), 4. 10.1186/s40842-021-00117-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozaffarian D, Benjamin E, Go A, Arnett D, Blaha M, Cushman M, Das S, de Ferranti S, Després J, Fullerton H, Howard V, Huffman M, Isasi C, Jiménez M, Judd S, Kissela B, Lichtman J, Lisabeth L, Liu S, … Turner M (2016). Executive Summary: Heart Disease and Stroke Statistics—2016 Update: A Report From the American Heart Association. Circulation (New York, N.Y.), 133(4), 447–454. 10.1161/CIR.0000000000000366 [DOI] [PubMed] [Google Scholar]
- National Center for Complementary and Integrative Health. (2021). Whole Person Health: What you need to know. Retrieved September 17, 2022, from https://www.nccih.nih.gov/health/whole-person-health-what-you-need-to-know
- Ortiz MS, Myers HF, Dunkel Schetter C, Rodriguez CJ, & Seeman TE (2015). Psychosocial Predictors of Metabolic Syndrome among Latino Groups in the Multi-Ethnic Study of Atherosclerosis (MESA). PLoS ONE, 10(4), e0124517. 10.1371/journal.pone.0124517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan A, Keum N, Okereke OI, Sun Q, Kivimaki M, Rubin RR, & Hu FB (2012). Bidirectional Association Between Depression and Metabolic Syndrome: A systematic review and meta-analysis of epidemiological studies. Diabetes Care, 35(5), 1171–1180. 10.2337/dc11-2055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasquali R, Vicennati V, Cacciari M, & Uberto Pagotto. (2006). The Hypothalamic-Pituitary-Adrenal Axis Activity in Obesity and the Metabolic Syndrome. Annals of the New York Academy of Sciences, 1083(1), 111–128. 10.1196/annals.1367.009 [DOI] [PubMed] [Google Scholar]
- Powers SI, Laurent HK, Gunlicks-Stoessel M, Balaban S, & Bent E (2016). Depression and Anxiety Predict Sex-Specific Cortisol Responses to Interpersonal Stress. Psychoneuroendocrinology, 69, 172–179. 10.1016/j.psyneuen.2016.04.007 [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: A self-report depression scale for research in the general population. 10.1177/014662167700100306 [DOI]
- Renn BN, Feliciano L, & Segal DL (2011). The bidirectional relationship of depression and diabetes: A systematic review. Clinical Psychology Review, 31(8), 1239–1246. 10.1016/j.cpr.2011.08.001 [DOI] [PubMed] [Google Scholar]
- Shinkov A, Borissova A, Kovatcheva R, Vlahov J, Dakovska L, Atanassova I, & Petkova P (2018). Increased prevalence of depression and anxiety among subjects with metabolic syndrome and known type 2 diabetes mellitus - a population-based study. Postgraduate Medicine, 130(2), 251–257. 10.1080/00325481.2018.1410054 [DOI] [PubMed] [Google Scholar]
- Smith KJ, Deschênes SS, & Schmitz N (2018). Investigating the longitudinal association between diabetes and anxiety: a systematic review and meta-analysis. Diabetic Medicine, 35(6), 677–693. 10.1111/dme.13606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorlie PD, Avilés-Santa Larissa M., Wassertheil-Smoller S, Kaplan RC, Daviglus Martha L., Giachello AL, Schneiderman N, Raij L, Talavera G, Allison M, LaVange L, Chambless LE, & Heiss Gerardo. (2010). Design and Implementation of the Hispanic Community Health Study/Study of Latinos. Annals of Epidemiology, 20(8), 629–641. 10.1016/j.annepidem.2010.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene PR, Vagg PR, & Jacobs AG (1983). Manual for the State-Trait Anxiety Inventory (Form Y). Consulting Psychologists Press, Inc. [Google Scholar]
- Tang F, Wang G, & Lian Y (2017). Association between anxiety and metabolic syndrome: A systematic review and meta-analysis of epidemiological studies. Psychoneuroendocrinology, 77, 112–121. 10.1016/j.psyneuen.2016.11.025 [DOI] [PubMed] [Google Scholar]
- Vancampfort D, Hallgren M, Mugisha J, De Hert M, Probst M, Monsieur D, & Stubbs B (2016). The Prevalence of Metabolic Syndrome in Alcohol Use Disorders: A Systematic Review and Meta-analysis. Alcohol and Alcoholism (Oxford), 51(5), 515–521. 10.1093/alcalc/agw040 [DOI] [PubMed] [Google Scholar]
- Van Reedt Dortland A, Giltay EJ, Van Veen T, Zitman FG, & Penninx BWJH (2010). Metabolic syndrome abnormalities are associated with severity of anxiety and depression and with tricyclic antidepressant use. Acta Psychiatrica Scandinavica, 122(1), 30–39. 10.1111/j.1600-0447.2010.01565.x [DOI] [PubMed] [Google Scholar]
- von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, & Vandenbroucke JP (2007). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Bulletin of the World Health Organization, 85(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C, Jia X, Wang Y, Fan J, Zhao C, Yang Y, & Shi X (2022). Trends and influence factors in the prevalence, intervention, and control of metabolic syndrome among US adults, 1999–2018. BMC Geriatrics, 22(1), 979–979. 10.1186/s12877-022-03672-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young-Hyman D, de Groot M, Hill-Briggs F, Gonzalez JS, Hood K, & Peyrot M (2017). Erratum. Psychosocial Care for People With Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care 2016;39:2126–2140. Diabetes Care, 40(5), 726. 10.2337/dc17-er05 [DOI] [Google Scholar]
- Zsido AN, Teleki SA, Csokasi K, Rozsa S, & Bandi SA (2020). Development of the short version of the spielberger state—trait anxiety inventory. Psychiatry Research, 291, 113223. 10.1016/j.psychres.2020.113223 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available upon request.


