Abstract
OBJECTIVE
Pediatric hypertension affects 2% to 5% of children and adolescents in the United States and is frequently undertreated. The increasing prevalence of pediatric hypertension and worsening physician shortage create difficulties in closing this treatment gap. Physician-pharmacist collaborations have been shown to improve patient outcomes in adult patients. Our aim was to demonstrate a similar benefit for pediatric hypertension.
METHODS
Pediatric patients whose hypertension was managed at a single pediatric cardiology clinic from January 2020 to December 2021 were enrolled in collaborative drug therapy management (CDTM). Patients whose hypertension was managed in the same clinic from January 2018 to December 2019 were used as a comparison group. The primary outcomes were achievement of at-goal blood pressure at 3, 6, and 12 months and time to control of hypertension. Secondary outcomes were appointment adherence and serious adverse events.
RESULTS
A total of 151 patients were included in the CDTM group, and 115 patients were included in the traditional care group. Of those, 100 CDTM patients and 78 traditional care patients were assessed for the primary outcome. Fifty-four (54%) CDTM patients and 28 (36%) traditional care patients achieved at-goal blood pressure at 12 months (OR, 2.09; 95% CI, 1.14–3.85). Appointment non-adherence was 9.4% for CDTM and 16% for traditional care (OR, 0.54; 95% CI, 0.35–0.82). Adverse events were similar between groups.
CONCLUSIONS
CDTM increased rates of at-goal blood pressure without increased adverse events. Physician-pharmacist collaboration may improve treatment of hypertension in pediatric patients.
Keywords: drug therapy, hypertension, pediatrics
Introduction
Pediatric hypertension affects 2% to 5% of children and adolescents in the United States and is frequently underdiagnosed and undertreated.1–6 A study by Shapiro et al2 found that as many as two-thirds of pediatric patients are not screened for hypertension at clinic visits. Kaelber et al4 found that only 23% of patients who meet criteria for hypertension are diagnosed with hypertension, and only 5.6% of diagnosed patients are treated. Patients with pediatric hypertension are frequently referred to cardiology or nephrology subspecialists for workup and treatment.1 However, the Association of American Medical Colleges predicts a shortage of 9300 to 17,800 medical specialists including pediatric subspecialists by 2033, and rural communities may have fewer than 20% the number of general pediatricians and specialists per capita as urban communities.7,8 Rural patients also report statistically significantly lower appointment adherence and lower-quality patient-provider communication on quality of care surveys.9 Data show that the prevalence of pediatric obesity is increasing in the United States, the so-called obesity epidemic, and obesity is strongly linked to primary hypertension in pediatric patients.3,10,11 As the care gap for children and adolescents with hypertension widens, and as hypertension and elevated blood pressure in pediatric patients most likely contributes to cardiovascular disease in adults, there is a need to improve drug therapy management for pediatric hypertension.
Pharmacists engaged in ambulatory care clinics extend ambulatory care services, reduce the burden on overloaded physicians, and decrease costs.12–14 Physicians respond well to pharmacists in ambulatory care settings and pharmacists can improve outcomes for patients and practices.13–15 Although the benefit of deploying pharmacists in ambulatory care settings has been demonstrated, the pharmacist's role in these settings is still being defined, including pediatric settings, where there is no standard practice model.16,17 The objective of this study was to determine if pharmacist-physician collaborative drug therapy management (CDTM) could improve rates of blood pressure control in a pediatric hypertension clinic.
Methods
This study was a controlled trial of physician-pharmacist CDTM versus traditional care. We intended to determine if CDTM for pediatric hypertension is non-inferior to traditional care.
Participants. Participants were patients at a pediatric cardiology clinic in Northeast Louisiana with 2 pediatric cardiologists. To be included in the study, patients needed to be aged 4 to 20 years at enrollment and have a diagnosis of elevated blood pressure or primary or secondary hypertension as defined in the 2017 pediatric hypertension guidelines.1 Patients who were pregnant or had physical preclusion to routine blood pressure measurement, such as patients with missing limbs or abnormal vasculature, were excluded. Patients in the CDTM group provided consent or assent as appropriate for age. We were not able to conduct the consent/assent process in languages other than English, so to respect patient autonomy and rights, patients who could not speak English or did not have a caregiver able to speak English were excluded from the study. Non–English-speaking patients were not excluded from the CDTM service.
Comparisons. Patients were enrolled in the CDTM group prospectively from January 2020 through December 2021. Patients were seen and diagnosed by 1 of 2 supervising cardiologists and referred to the pharmacist for CDTM. CDTM visits were placed on the pharmacist's schedule, which had 20 hours/week available for appointments. During visits, the pharmacist could counsel about medications and therapeutic lifestyle choices such as diet and exercise, issue prescription orders and laboratory orders by way of a protocol based on the 2017 pediatric hypertension guidelines, and order follow-up visits (Figure 1).1 The pharmacist also issued oscillometric blood pressure devices for home blood pressure monitoring at no cost to patients and taught proper use to patients and caregivers. Patients aged 13 years and older who were capable of home blood pressure monitoring were invited to schedule virtual visits after their first visit with the pharmacist.
Figure 1.
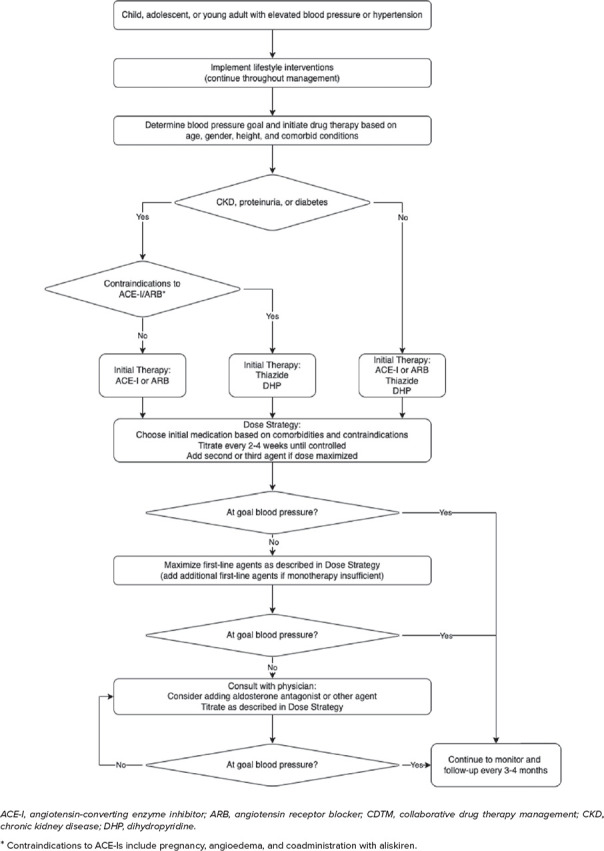
CDTM treatment algorithm.
Patients with hypertension who were seen in the clinic between January 2018 and December 2019 were retrospectively included in the traditional care group. Traditional care patients were managed by the pediatric cardiologists with or without assistance from nurse practitioners or physician assistants. Traditional care patients did not have the option for telemedicine, nor were they issued home blood pressure monitors.
Outcomes. The primary outcomes were the proportion of patients at goal blood pressure at 3, 6, and 12 months and time to control (TTC) of blood pressure. Goal blood pressure was defined as in-clinic blood pressure <95th percentile for age, sex, and height in children or <130/80 mm Hg in adolescents. Time to control was defined as days until achievement of goal blood pressure, provided goal blood pressure was maintained through the end of the study period. The start date for all primary outcomes was the first visit with above-goal blood pressure. Secondary outcomes included appointment adherence and a composite of serious adverse drug events and hypertension-related unanticipated health care encounters. All appointments with any provider or service in the cardiology clinic were counted for adherence outcomes, but if a patient had multiple appointments on the same day, such as an echocardiogram and a provider visit, this was counted only once.
Statistical Methods. All categorical outcomes were assessed with chi-square statistics with a non-inferiority margin of 20% (δ = 0.2). TTC was assessed by using a Kaplan-Meier estimate. With an alpha of 0.05, we determined that we would need 324 patients for 90% power to establish non-inferiority. All patients who met inclusion criteria, attended at least 2 visits with the pharmacist (CDTM) or physician (traditional care), and were followed up for at least 3 months were included in the intention-to-treat (ITT) analysis. ITT patients who had at least 1 visit with above-goal blood pressure were included in the modified intention-to-treat (mITT) analysis. The mITT population was used for assessments of blood pressure control. The ITT population was used for assessments of adherence and safety. All statistical analyses were performed by using R in the RStudio environment.18,19 Assessment was conducted with group assignments blinded.
Results
One hundred fifty-six patients were screened for inclusion in the CDTM group. Of those patients screened, 151 were included. Reasons for exclusion included not providing or withdrawing consent (3) or not having a caregiver who speaks English (2). In the traditional care group, 115 patients were screened and all 115 met inclusion criteria. Of all patients included, 125 (CDTM) and 79 (traditional) were included in the ITT analysis, and 100 (CDTM) and 78 (traditional) were included in the mITT analysis (Figures 2 and 3). Baseline characteristics were similar between groups (Table 1).
Figure 2.
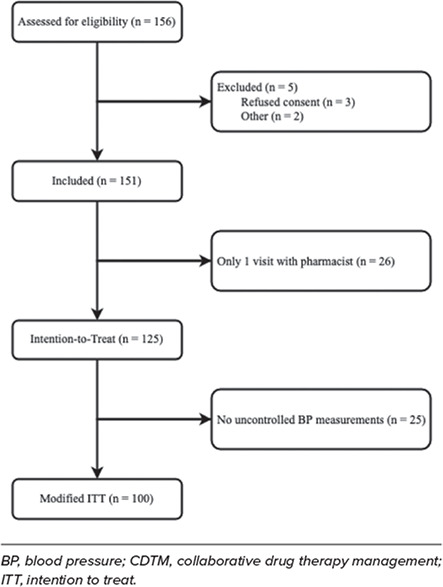
Patient flowchart for patients in the CDTM (prospective) group.
Figure 3.
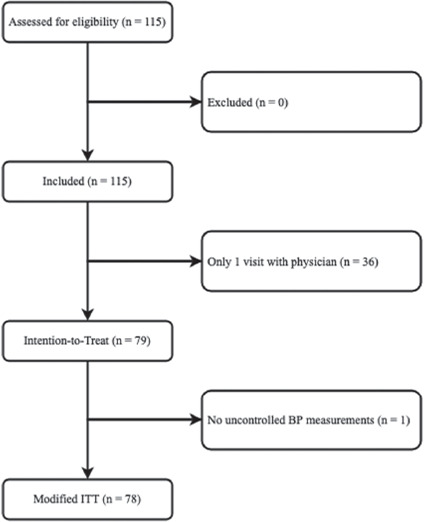
Patient flowchart for patients in the traditional care (retrospective) group.
Table 1.
Baseline Characteristics
| CDTM | Traditional | p | |
|---|---|---|---|
| Age, mean ± SD, yr | 12.4 ± 3.5 | 12.6 ± 3.5 | 0.67 |
| Age 4–12, n (%) | 57 (46) | 36 (46) | >0.99 |
| Age 13–17, n (%) | 66 (53) | 37 (47) | 0.41 |
| Age 18–20, n (%) | 2 (2) | 6 (8) | 0.03 |
| SBP, median (IQR), percentile* | 95 (88–98) | 97 (92–99) | 0.06 |
| DBP, median (IQR), percentile* | 89 (74–96) | 78 (50–94) | 0.01 |
| BMI, mean ± SD, kg/m2 | 28.7 ± 7.8 | 28.8 ± 7.8 | 0.91 |
| BMI, median (IQR), percentile† | 97 (90–99) | 97 (88.5–99) | 0.67 |
| Obese, n (%) | 83 (66) | 51 (65) | 0.79 |
| Severely obese, n (%) | 52 (42) | 30 (38) | 0.61 |
| Height, median (IQR), percentile† | 86 (60–98) | 82 (56–96.5) | 0.37 |
BMI, body mass index; CDTM, collaborative drug therapy management; DBP, diastolic blood pressure; SBP, systolic blood pressure
* Percentile for age, height, and sex.
† Percentile for age.
Primary Outcomes. Achievement of at-goal blood pressure at 12 months was statistically significantly higher in the CDTM group, occurring in 54 (54%) patients in the CDTM group compared with 28 (36%) in the traditional care group (OR, 2.09; 95% CI, 1.14–3.85; p = 0.016) (Table 2). This difference also existed at 6 months (OR, 2.21; 95% CI, 1.18–4.12; p = 0.012) and at 3 months (OR, 2.92; 95% CI, 1.44–5.91; p = 0.002). Median TTC was 44 days shorter in the CDTM group (63.5 days; IQR, 36.75–129.75) than in the traditional care group (107.5 days; IQR, 58.25–249) (p = 0.026) (Figure 4).
Table 2.
Primary Outcomes: At-Goal Blood Pressure at 3, 6, and 12 Months and Time to Control of Hypertension
| CDTM (N = 100) | Traditional (N = 78) | OR (95% CI) | |
|---|---|---|---|
| Outcome | |||
| At-goal blood pressure | |||
| 12 mo | 54 (54%) | 28 (36%) | 2.09 (1.14–3.85) |
| 6 mo | 48 (48%) | 23 (29%) | 2.21 (1.18–4.12) |
| 3 mo | 39 (39%) | 14 (18%) | 2.92 (1.44–5.91) |
Figure 4.
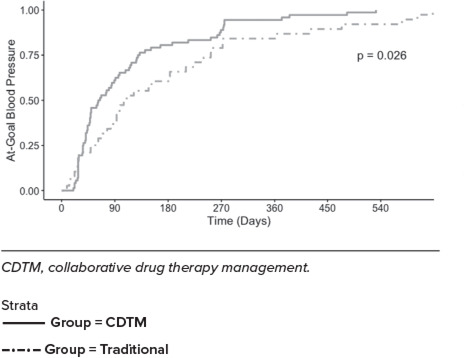
Kaplan-Meier graph for time to control of hypertension.
Safety Outcomes. One patient in each group experienced possible angioedema while taking lisinopril. Both patients' symptoms resolved after discontinuing lisinopril. Two patients in the CDTM group and 1 patient in the traditional care group were referred to acute care for observation following elevated blood pressure measurements. All 3 patients' blood pressure resolved during observation. No other study-related serious adverse events or unanticipated health care encounters were reported.
Appointment Adherence. In the CDTM group, 35 (28%) patients had at least 1 “no show” missed appointment, compared with 23 (29%) in the traditional care group (OR, 0.95; p = 0.86). There were a total of 58 (9%) no show appointments for CDTM patients, compared with 45 (16%) no show appointments for traditional care patients (p < 0.01) (Table 3).
Table 3.
Secondary Outcomes: Missed Appointments
| CDTM | Traditional | OR (95% CI) | |
|---|---|---|---|
| Outcome | |||
| Patients with ≥1 “no show” | 35/125 (28%) | 23/79 (29%) | 0.95 (0.51–1.8) |
| “No show” appointments | 58/620 (9.4%) | 45/280 (16%) | 0.54 (0.35–0.82) |
CDTM, collaborative drug therapy management
Medication Usage. Drug choice was similar between groups, except that patients in the CDTM group were more likely to receive angiotensin receptor blockers (ARBs) (p = 0.03) (Table 4). This reflects the success of challenging some CDTM patients on ARBs who did not tolerate angiotensin-converting enzyme inhibitors (ACE-Is).20
Table 4.
Medication Usage
| CDTM, % | Traditional, % | p | |
|---|---|---|---|
| ACE-I or ARB* | 73 | 61 | 0.13 |
| ACE-I | 62 | 57 | 0.37 |
| ARB | 14 | 4 | 0.03 |
| Aldosterone antagonist | 1 | 0 | - |
| Alpha agonist | 11 | 5 | 0.22 |
| Amiloride | 2 | 0 | - |
| Beta blocker | 13 | 23 | 0.11 |
| Calcium channel blocker (dihydropyridine) | 28 | 33 | 0.52 |
| Calcium channel blocker (non-dihydropyridine) | 1 | 1 | 0.94 |
| Thiazide-like antihypertensive | 27 | 16 | 0.08 |
ACE-I, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; CDTM, collaborative drug therapy management
* Some patients received both an ACE-I and ARB at different times in their therapy (no patients received an ACE-I and ARB concomitantly).
Discussion
In this study, we improved drug therapy management in hypertensive pediatric patients through use of a pharmacist-physician collaboration. Our primary outcomes, at-goal blood pressure at 12 months and TTC of blood pressure, both met statistical criteria for non-inferiority and superiority of CDTM. The number needed to treat was 6 patients enrolled for 12 months in CDTM to achieve 1 additional controlled hypertension case. This mirrors similar results found when deploying clinical pharmacists in adult settings, where pharmacist collaborators with the ability to issue prescription orders improve rates of at-goal blood pressure by as much as double traditional care.13,21–24 The results of this study provide another mechanism to improve the nationwide low rates of successful treatment for pediatric hypertension.25–31
We expected telemedicine to improve appointment adherence by reducing travel time and time away from home, work, and school for patients and caregivers. While telemedicine was underused, our missed appointment rate was still lower in the CDTM group. In both groups, patients were called after missed appointments to reschedule, by a nurse for traditional care and by the pharmacist for CDTM. It is possible that the novelty of the clinic motivated patients to keep CDTM appointments, or else the increased frequency of visits made it easier for CDTM patients to remember their appointment times.
Pharmacotherapy choices were similar between groups. CDTM patients were more likely to receive a thiazide-like antihypertensive or renin-angiotensin-aldosterone system (RAAS) inhibitors, and traditional care patients were more likely to receive beta blockers, but these differences were not statistically significant. This difference can be explained by the pharmacist's protocol, which preferred first-line agents (thiazides, RAAS inhibitors, dihydropyridines) over second-line agents (including beta blockers). The only statistically significant difference was ARB use. During the study, 1 patient experienced dramatically improved blood pressure after switching from an ACE-I to an ARB.20 This resulted in the pharmacist's attempting the same switch in some other patients who were not at goal on dual therapy as an extra step before advancing to triple therapy or moving to second-line agents.
In addition to the clinical pharmacist's time, resources required for our practice model included physician time for protocol and collaborative care discussions; administrative support for credentialing, electronic medical record access, and scheduling; clinic staff support for rooming patients; clinic space; and home blood pressure monitors. In practice, the cost of home monitors may be transferred to some third-party payors or to patients. For this study, the most challenging resource was clinic space, as the examination rooms and other clinic space were shared by physicians, advanced practice providers, and the pharmacist.
Strengths of this study include a realistic, easy-to-replicate practice. We designed this practice to resemble typical pharmacist-provider clinics across the United States.32 The pharmacist's schedule was open for the entire 20 hours/week for patient appointments, which could be 30 minutes or 1 hour. Patient appointment slots were supposed to be long enough for the pharmacist to prepare to see the patient, conduct the visit, consult with the physician, if necessary, and write a progress note into the patient's chart—the pharmacist schedule was designed to closely emulate other provider schedules. Patient scheduling was managed mostly by clinic staff, so appointments could be added even when the pharmacist was not present. Finally, this is the first study in pediatric hypertension to report rates of control at short-term intervals.26
Our study also had some limitations. We originally intended for many of our CDTM patient encounters to occur via telemedicine. After the initial in-person visit to enroll patients and provide and teach patients to use a home blood pressure monitor, we expected eligible patients—those patients at least 13 years of age who could fit one of our home monitoring cuffs and demonstrate proper technique—would be managed mostly by telemedicine. This would have helped with the problem of clinic space and the need for patient rooms. However, telemedicine acceptance was low in our study patients. Early in the COVID-19 pandemic, our clinic encouraged telemedicine visits where possible. This might have reasonably catalyzed our telemedicine service, but only 7 patients chose to schedule and attend more than 1 telemedicine session during the entire duration of the study. Reasons for low acceptance of telemedicine are unknown.
As an additional limitation, only in-clinic blood pressure measurements were used in assessing outcomes, instead of gold standard ambulatory blood pressure monitoring. Home blood pressure logs for CDTM patients were reviewed and may have influenced provider decisions but were not used to assess study outcomes. Also, there are no home blood pressure monitors available in the United States that are validated for use in children.33 Because of this, we could not take full advantage of home blood pressure monitoring for patients aged 12 years and younger.
This article describes clinical outcomes associated with physician-pharmacist CDTM. We are planning a pharmacoeconomic analysis of the cost-effectiveness of our model, which may provide further justification for deploying a clinical pharmacist in similar settings. We also recognize the need for further research into telemedicine, specifically the reasons for low adoption of telemedicine, billing, and clinics covering multiple disease states.
Conclusion
This study describes a novel pediatric hypertension clinic using physician-pharmacist CDTM. We found that this approach improves rates of at-goal blood pressure, time to at-goal blood pressure, and appointment adherence without compromising patient safety. Physician-pharmacist collaboration is permitted in most US jurisdictions, so provided resources such as pharmacist time and clinic space can be allocated, our practice model could be reasonably emulated and improve patient management in a variety of settings.
Acknowledgments
Jeffery Evans of University of Louisiana Monroe and Nancy King of Ochsner Health for their assistance in setting up the clinical practice site. Preliminary results were presented at American Academy of Pediatrics AAP Experience on October 8, 2021.
ABBREVIATIONS
- ACE-I
angiotensin-converting enzyme inhibitor;
- ARB
angiotensin receptor blocker;
- CDTM
collaborative drug therapy management;
- COVID-19
coronavirus disease of 2019;
- ITT
intention to treat;
- mITT
modified intention to treat;
- RAAS
renin-angiotensin-aldosterone system;
- TTC
time to control
Footnotes
Disclosures. This research was funded by the Delta Health Care Services grant from the United States Department of Agriculture (Award 2018-18682). The authors declare no conflicts or financial interest in any product or service mentioned in the manuscript, including grants, equipment, medications, employment, gifts, and honoraria. Bryan Donald had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Ethical Approval and Informed Consent. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and have been approved by the institutional review boards at University of Louisiana Monroe and Ochsner Health. All patients aged 18 and older provided informed consent. All parents/caregivers of minor patients provided parent/caregiver permission; informed assent was obtained from all children aged 7 and older.
References
- 1.Flynn JT, Kaelber DC, Baker-Smith CM et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics . 2017;140(3):e20171904. doi: 10.1542/peds.2017-1904. [DOI] [PubMed] [Google Scholar]
- 2.Shapiro DJ, Hersh AL, Cabana MD et al. Hypertension screening during ambulatory pediatric visits in the United States, 2000-2009. Pediatrics . 2012;130(4):604–610. doi: 10.1542/peds.2011-3888. [DOI] [PubMed] [Google Scholar]
- 3.Hill KD, Li JS. Childhood hypertension: an underappreciated epidemic. Pediatrics . 2016;138(6) doi: 10.1542/peds.2016-2857. e20162857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaelber DC, Liu W, Ross M et al. Diagnosis and medication treatment of pediatric hypertension: a retrospective cohort study. Pediatrics . 2016;138(6):e20162195. doi: 10.1542/peds.2016-2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kharbanda EO, Asche SE, Sinaiko AR et al. Clinical decision support for recognition and management of hypertension: a randomized trial. Pediatrics . 2018;141(2):e20172954. doi: 10.1542/peds.2017-2954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flynn JT. Stability of blood pressure and diagnosis of hypertension in childhood. Pediatrics . 2020;146(4):e2020018481. doi: 10.1542/peds.2020-018481. [DOI] [PubMed] [Google Scholar]
- 7.Dall T, Reynolds R, Chakrabuarti R The complexities of physician supply and demand: projections from 2018 to 2033. Association of American Medical Colleges. 2020. Accessed May 2, 2022. https://www.aamc.org/system/files/2020-06/stratcomm-aamc-physician-workforce-projections-june-2020.pdf.
- 8.Rosenblatt RA. A view from the periphery—health care in rural America. N Engl J Med . 2004;351(11):1049–1051. doi: 10.1056/NEJMp048073. [DOI] [PubMed] [Google Scholar]
- 9.Stumetz KS, Yi-Frazier JP, Mitrovich C, Early KB. Quality of care in rural youth with type 1 diabetes: a cross-sectional pilot assessment. BMJ Open Diabetes Res Care . 2016;4(1):e000300. doi: 10.1136/bmjdrc-2016-000300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flynn J. The changing face of pediatric hypertension in the era of the childhood obesity epidemic. Pediatr Nephrol . 2013;28(7):1059–1066. doi: 10.1007/s00467-012-2344-0. [DOI] [PubMed] [Google Scholar]
- 11.Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic risks and severity of obesity in children and young adults. N Engl J Med . 2015;373(14):1307–1317. doi: 10.1056/NEJMoa1502821. [DOI] [PubMed] [Google Scholar]
- 12.Hartkopf KJ, Heimerl KM, McGowan KM, Arndt BG. Expansion and evaluation of pharmacist services in primary care. Pharmacy . 2020;8(124):124. doi: 10.3390/pharmacy8030124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hawes EM, Misita C, Burkhart JI et al. Prescribing pharmacists in the ambulatory care setting: experience at the University of North Carolina Medical Center. Am J Health Syst Pharm . 2016;73(18):1425–1433. doi: 10.2146/ajhp150771. [DOI] [PubMed] [Google Scholar]
- 14.Moreno G, Lonowski S, Fu J et al. Physician experiences with clinical pharmacists in primary care teams. J Am Pharm Assoc . 2017;57(6):686–691. doi: 10.1016/j.japh.2017.06.018. [DOI] [PubMed] [Google Scholar]
- 15.Schultz JL, Horner KE, McDanel DL et al. Comparing clinical outcomes of a pharmacist-managed diabetes clinic to usual physician-based care. J Pharm Pract . 2018;31(3):268–271. doi: 10.1177/0897190017710522. [DOI] [PubMed] [Google Scholar]
- 16.Jun JK. The role of pharmacy through collaborative practice in an ambulatory care clinic. Am J Lifestyle Med . 2019;13(3):275–281. doi: 10.1177/1559827617691721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lampkin SJ, Gildon B, Benavides S et al. Considerations for providing ambulatory pharmacy services for pediatric patients. J Pediatr Pharmacol Ther . 2018;23(1):4–17. doi: 10.5863/1551-6776-23.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.R Core Team R: a language and environment for statistical computing. R Foundation for Statistical Computing. 2022. Accessed April 26, 2022. https://www.R-project.org.
- 19.Rstudio Team Rstudio: integrated development environment for R. Rstudio, PBC. 2022. Accessed April 26, 2022. http://www.rstudio.com.
- 20.Donald BJ, King TD, Phillips BL. Case report: improved blood pressure control after switching to an angiotensin receptor blocker from an angiotensin-converting enzyme inhibitor in an adolescent with hypertension. J Am Coll Clin Pharm . 2022;5(7):781. [Google Scholar]
- 21.Magid DJ, Olson KL, Billups SJ et al. A pharmacist-led, American Heart Association Heart360 web-enabled home blood pressure monitoring program. Circ Cardiovasc Qual Outcomes . 2013;6(2):157–163. doi: 10.1161/CIRCOUTCOMES.112.968172. [DOI] [PubMed] [Google Scholar]
- 22.Rothman RL, Malone R, Bryant B et al. A randomized trial of a primary care-based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes. Am J Med . 2005;118(3):276–284. doi: 10.1016/j.amjmed.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 23.Vivian EM. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy . 2002;22(12):1533–1540. doi: 10.1592/phco.22.17.1533.34127. [DOI] [PubMed] [Google Scholar]
- 24.Santschi V, Chiolero A, Colosimo AL et al. Improving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trials. J Am Heart Assoc . 2014;3(2):e000718. doi: 10.1161/JAHA.113.000718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yoon EY, Davis MM, Rocchini A et al. Medical management of children with primary hypertension by pediatric subspecialists. Pediatr Nephrol . 2009;24(1):147–153. doi: 10.1007/s00467-008-0970-3. [DOI] [PubMed] [Google Scholar]
- 26.Kaelber DC, Localio AR, Ross M et al. Persistent hypertension in children and adolescents: a 6-year cohort study. Pediatrics . 2020;146(4):e20193778. doi: 10.1542/peds.2019-3778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wühl E. Hypertension in childhood obesity. Acta Paediatr . 2019;108(1):37–43. doi: 10.1111/apa.14551. [DOI] [PubMed] [Google Scholar]
- 28.Shield JPH, Lynn R, Wan KC et al. Management and 1 year outcome for UK children with type 2 diabetes. Arch Dis Child . 2009;94(3):206–209. doi: 10.1136/adc.2008.143313. [DOI] [PubMed] [Google Scholar]
- 29.Wei C, Candler T, Crowne E, Hamilton-Shield JP. Interval outcomes of a lifestyle weight-loss intervention in early adolescence. Children (Basel) . 2018;5(6):E77. doi: 10.3390/children5060077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Urbina EM, Khoury PR, McCoy C et al. Cardiac and vascular consequences of pre-hypertension in youth. J Clin Hypertens . 2011;13(5):332–342. doi: 10.1111/j.1751-7176.2011.00471.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Samuel JP, Tyson JE, Green C et al. Treating hypertension in children with n-of-1 trials. Pediatrics . 2019;143(4):e20181818. doi: 10.1542/peds.2018-1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hill JD, Hill JM, Gentile NJ. A review of state pharmacist collaborative practice laws. Am J Health Syst Pharm . 2016;73(18):1467–1472. doi: 10.2146/ajhp160269. [DOI] [PubMed] [Google Scholar]
- 33.dabl Educational Trust Sphygmomanometers for self-measurement of blood pressure. Accessed July 28, 2021. www.dableducational.org/sphygmomanometers/devices_2_sbpm.html.


