Abstract
Objective
We tested if automated Personalized Self-Awareness Feedback (PSAF) from an online survey or in-person Peer Resilience Champion support (PRC) reduced emotional exhaustion among hospital workers during the COVID-19 pandemic.
Method
Among a single cohort of participating staff from one hospital organization, each intervention was evaluated against a control condition with repeated measures of emotional exhaustion at quarterly intervals for 18 months. PSAF was tested in a randomized controlled trial compared to a no-feedback condition. PRC was tested in a group-randomized stepped-wedge design, comparing individual-level emotional exhaustion before and after availability of the intervention. Main and interactive effects on emotional exhaustion were tested in a linear mixed model.
Results
Among 538 staff, there was a small but significant beneficial effect of PSAF over time (p = .01); the difference at individual timepoints was only significant at timepoint three (month six). The effect of PRC over time was non-significant with a trend in the opposite direction to a treatment effect (p = .06).
Conclusions
In a longitudinal assessment, automated feedback about psychological characteristics buffered emotional exhaustion significantly at six months, whereas in-person peer support did not. Providing automated feedback is not resource-intensive and merits further investigation as a method of support.
Keywords: Burnout, E-intervention, COVID-19, Healthcare workers, Peer support
1. Background
In the two years following the declaration of a COVID-19 pandemic by the World Health Organization [1], healthcare workers experienced extraordinarily stressful work conditions, which increased psychological distress, burnout, and other mental health challenges [2]. Contributors to healthcare workers' stress included increased patient acuity, understaffing, exposure to the virus, increased overtime, reassignment to unfamiliar roles, moral distress, and uncertainty about infectious risks and precautions [3].
Many healthcare organizations implemented ad hoc support resources for their staff during the pandemic [4,5] in addition to existing resources. Understandably, the ability of healthcare organizations to formally evaluate these interventions has been limited. A wide range of interventions have been reported thus far, including online or app-based stress management interventions [6,7], a video aimed to increase treatment-seeking [8], expressive writing [9], and various stress reduction interventions [10,11]. While several interventions have been evaluated using validated outcome measures, many of these have not been compared to control conditions [[12], [13], [14], [15], [16], [17]]. Of those studies which have reported comparison conditions, some have not employed randomization [6], had a small number of participants (e.g. 〈100) [9,10], and had short periods of follow-up (e.g. one month or less) [[7], [8], [9],11]. Randomized controlled trials of interventions for hospital-based staff, evaluated in larger cohorts and over longer periods of time are needed.
In our hospital, staff support during the COVID-19 pandemic included many resources which varied in their intensity and focus [18]. Some resources were available to individuals upon their request, including assessment and sometimes treatment through the Employee Assistance Program, or the Department of Psychiatry. Other support resources targeted the entire organization including (i) timely, transparent, responsive communications about extraordinary circumstances, procedures, policies and their rationale, (ii) pre-existing organizational resources to support well-being, safety and quality improvement, and (iii) pandemic-specific online resources (information, links to internal and external support resources, stress and coping educational resources, and a question-and-answer function). Additionally, resources were available that targeted groups of staff in response to specific demands. These included on-demand in-service huddles for clinical units after extraordinary events (typically facilitated by the unit manager and appropriate experts from, for example, infection control), and support from “coaches” (mental health professionals) assigned to specific units who attended rounds and work with teams and team leaders to provide support [[19], [20], [21]].
Evidence from prior infectious outbreaks indicates that support can increase resilience in HCWs. In particular, during H1N1 influenza pandemic preparation, computer-based interactive learning targeting interpersonal sources of stress (isolation, interpersonal conflict, stigma, blame) reduced interpersonal problems and increased self-efficacy, which is confidence in managing professionals' pandemic responsibilities [22]. In-person interactive team-based learning co-facilitated by peers and a mental health nurse increased participants' confidence in their pandemic preparation [23]. Indeed, approaches to reducing psychological burden in healthcare workers have often incorporated peer support although the evaluation of these intervention has not been robust [24].
The current project aimed to evaluate two types of support provided to hospital staff during the COVID-19 pandemic in addition to the range of supportive resources described above: automated personalized self-awareness feedback (PSAF) provided at intervals through a longitudinal online survey, and support from Peer Resilience Champions (PRC), provided both virtually and in-person. For each intervention we implemented a randomized, controlled evaluation of the effect of the intervention on emotional exhaustion, a dimension of burnout, over eighteen months.
2. Methods
The study took place at two sites of Sinai Health, an urban acute care teaching hospital and a rehabilitation hospital with a combined staff of over 6000, in Toronto, Canada. The trial was conducted according to the Consolidated Statements of Reporting Trials (CONSORT) guidelines and was registered on clinical trials.gov (CT04373382).
2.1. Study design
Two interventions were tested: personalized self-awareness feedback from psychological surveys self-administered at intervals (the PSAF intervention), and the availability of in-person peer support by Peer Resilience Champions (the PRC intervention). The participants in each trial were the same: professional staff, employees, volunteers, and learners (for brevity: “staff”) who completed a longitudinal survey at 3-month intervals (T1 to T7) over eighteen months. The assessment method for each trial was also the same: a measure of the emotional exhaustion dimension of professional burnout repeated at each survey time-point.
-
a.
PSAF Trial
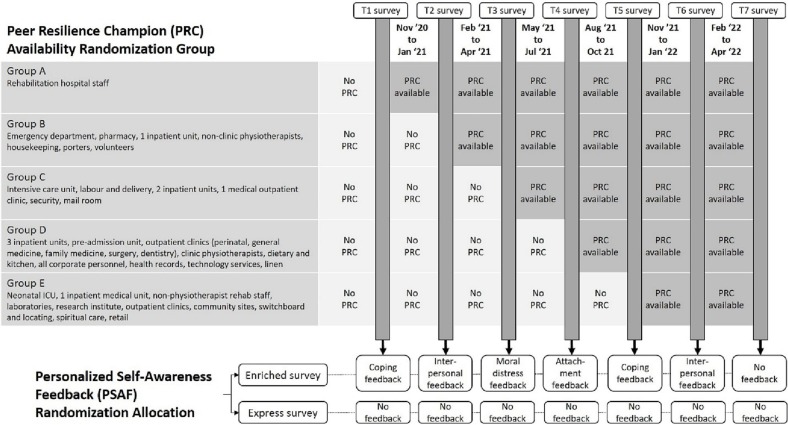
For the PSAF trial, participants were randomized (1:1) into two versions of the survey using an online randomizer in blocks of eight. The PSAF version of the survey (“enriched”) included psychological measures which varied between time points that were used to provide personalized feedback. The measures used for feedback were scored automatically, facilitating personalized feedback to the participant about coping style (T1, T5), interpersonal problems (T2, T6), moral distress (T3), and attachment style (T4) (Fig. 1 ). The control version of the survey (“express”) did not include these intervention instruments and did not provide feedback. Both versions of the survey measured emotional exhaustion and a short battery of measures not reported here (psychological distress, sleep quality, pandemic-self-efficacy). Participants were not blind to whether they received feedback.
-
b.
PRC Trial
Fig. 1.
Designs of two simultaneous trials: stepped wedge department-level randomization of availablity of Peer Resilience Champions, evaluated with measures at seven time points, and individual randomization of survey participants to personalized self-awareness feedback or no feedback conditions.
The PRC intervention was available to all staff with the timing of onset of availability randomly determined using a stepped-wedge design. The intervention exposure is described as “availability” because staff were not obligated to attend PRC sessions. Randomization of the time of availability of PRC was facilitated by assigning clinical units and departments to five randomization groups. To balance randomization group composition, the following procedure was followed. First, units were categorized by acuity: high acuity (e.g., ICU, emergency department), other patient care, or non-patient care. Within acuity categories, units were assigned to randomization groups to balance the number of participants and the proportion of occupation types within groups as much as possible and to minimize unintended early participant exposure to PRC interventions (e.g., by assigning geographically or organizationally related units to the same group). The order of availability of PRC intervention was then determined using an online randomization tool, and the groups were labelled A (first) to E (fifth). The start of the availability of PRC coincided with the end of survey time-points (Fig. 1), such that PRC was available to staff of Group A after the T1 survey was completed, Group B after T2, etc. Staff attending PRC sessions were not obligated to complete the longitudinal survey. Staff were not blind to whether PRC was available. Staff who did participate in the longitudinal survey provided information about their unit, department and occupational role such that they could be identified as a member of one of the five PRC groups. This facilitated comparison of emotional exhaustion, prior to and after the availability of the PRC intervention for each survey participant.
2.2. Survey participants
Staff were invited via posters in high-traffic areas of the hospital and emails (e.g. hospital updates, newsletters, and communications from managers) to participate in a longitudinal survey, distributed quarterly starting in fall 2020 until spring 2022. Those younger than 18 years were excluded. All survey participants provided informed consent. Surveys were completed using an online software (Alchemer, Louisville, CO) that is compliant with jurisdictional privacy standards in Ontario, Canada. Participants received a gift card at the end of each completed survey (~$20 CAD value). This study received approval from the Sinai Health Research Ethics Board (20–0084-E).
2.3. Evaluation instrument
Burnout was measured with the emotional exhaustion scale of the Maslach Burnout Inventory: Human Services Survey for Medical Personnel [25], which includes nine items scored from 0 to 6, for a potential score of 0 to 54. Cronbach's alpha ranged from 0.94 to 0.96 across time points.
2.4. The personalized self-awareness feedback (PSAF) intervention
The enriched survey provided personalized feedback about coping behaviors, interpersonal problems, moral distress, and attachment style (Fig. 1), based on the relevant scores. Feedback, authored by the investigators, consisted of a few sentences that summarized what had been self-reported plus a gently phrased suggestion about possible changes to consider. Cut-off scores to select feedback statements were based on a prior study [26], using validated cut-offs when available. The method of providing feedback and the full text of all feedback statements are provided in Supplementary File 1.
2.5. Personalized feedback instruments
Coping behaviors were measured with the Brief COPE, a 28-item instrument [27], with the pandemic designated as the stressful event. Brief COPE items are measured on a Likert-like scale [[1], [2], [3], [4]]. The instrument yields fourteen subscales (Cronbach's alpha at T1, T5): active coping (0.74, 0.76), using instrumental support (0.78, 0.79), planning (0.68, 0.77), self-distraction (0.49, 0.62), using emotional support (0.70, 0.82), positive reframing (0.66, 0.79), humor (0.83, 0.85), acceptance (0.68, 67), religion (0.85, 0.89), denial (0.79, 0.66), substance use (0.95, 0.94), behavioral disengagement (0.66, 0.65), venting (0.53, 0.58) and self-blame (0.70, 0.65). To align with PRC teaching, two items were created to measure coping via purpose and values (“I have been trying to live according to my values,” “I have been paying attention to the things that give me a sense of purpose” (0.60, 0.65).
Interpersonal problems were assessed with the Inventory of Interpersonal Problems-32 [28]. Eight four-item subscales (each item scored 1 to 8) are theoretically arranged on a circumplex such that they consist of four sets of opposites: domineering/controlling vs. nonassertive, vindictive/self-centered vs. overly accommodating, cold/distant vs. self-sacrificing, socially inhibited vs. intrusive/needy. Cronbach's alpha for the subscales ranged from 0.72 to 0.93.
Moral distress was measured with the Measure of Moral Distress for Healthcare Providers [29], a 27-item scale which measures moral distress at the patient, system, and team levels. Each item scored for frequency (0 to 4) and for how distressing it is (0 = none, 4 = very distressing). The product of these two scores for each item is summed (total score 0–432, Cronbach's alpha = 0.98).
Adult attachment style was measured with an abbreviation of the Experience in Close Relationships, the ECR-M16. The ECR-M16 is 16-item measure of individuals' attachment orientations to close others, which has been validated in cancer patients [30]. The ECR-M16 includes eight items measuring attachment anxiety (Cronbach's alpha = 0.88) and eight measuring attachment avoidance (Cronbach's alpha = 0.80).
2.6. The peer resilience champion (PRC) intervention
Two PRCs provided in-person interventions. One PRC (a social worker) worked full-time throughout the trial and was the sole provider of the PRC intervention during blocks 1–3 of the stepped wedge. Following the T4 survey, a half-time PRC (a Masters candidate in counselling psychotherapy) provided additional support during the blocks 4–6.
The PRCs were oriented using a manual (Supplementary File 2), which described the concepts of resilience, mental health challenges that healthcare workers had experienced in previous infectious outbreaks, characteristics of the normal stress response and of burnout, and modifiable contributors to stress responses, burnout, and resilience. The manual emphasized the value of interpersonal support, developing reflective function, cautious facilitation of emotional expression with consent, advocacy, psychological safety, and principals of organizational resilience. Examples of skills-based activities for relaxation, and attention to personal meaning and values were described. The interventions that were provided ranged broadly and included identifying challenges, validating participants' responses, teaching stress and relaxation skills, leading values-based and gratitude exercises, discussing readings, assisting with resource navigation, and advocacy to managers and leaders. The PRCs were encouraged to develop further resources and exercises to adapt to local needs (for example, team-building exercises and craft activities were introduced by PRCs in response to requests). The principal investigator, research coordinator and PRC(s) met weekly for discussion and supervision of the iteratively developing role.
2.7. Sample size
The a priori target sample size was calculated for the PRC study which was expected to require a larger sample than the PSAF study. Based on previous research [31], we assumed 30.4% of staff would have high burnout at baseline and a drop in this rate ≥ 9.4% would be meaningful. Five clusters of 200 staff would be sufficient to detect this drop with an intra-cluster correlation coefficient congruent with previous studies (80% power, alpha level 0.05).
2.8. Analysis
Descriptive statistics were calculated for all variables of interest. Continuous measures were summarized using means and standard deviations whereas categorical measures were summarized using counts and percentages. The main outcome, emotional exhaustion, was analyzed as a continuous variable rather than as a rate of high scores to maximize statistical power. Linear mixed models were run on emotional exhaustion, with subject as a random effect. The models included (i) main effects of PRC exposure, time, PSAF allocation, (ii) main effects of co-variates known to be associated with emotional exhaustion: education [32,33] and occupation type [34,35], as well as (iii) a priori hypothesized interactions between PRC exposure, time, and PSAF allocation. Non-significant interaction terms were removed, and the models rerun to improve the precision of the parameter estimates for the main effects. Post-hoc, the proportion of participants with high emotional exhaustion (score ≥ 27 [36]) in intervention and control groups was used to illustrate the magnitude of significant effects. Analyses were carried out using SAS Version 9.4 (SAS Institute, Cary, NC, USA) or IBM SPSS Statistics 28 (Armonk, New York).
3. Results
3.1. Demographics of full cohort
Of 1038 respondents to the invitation to participate, 884 met inclusion criteria and consented to participate during the recruitment phase. Of these, 538 (61%) completed the first survey (T1, conducted September 21–November 15, 2020) which included the baseline measure of emotional exhaustion. These 538 formed the cohort for further follow-up. The characteristics of the 538 survey participants are described in Table 1 . Participants were predominantly female (78.4%), about half with professional or graduate degrees (50.2%), and about half white (51.7%). Occupation type was fairly evenly distributed between nurses and nursing students (24.9%), other health professionals and their trainees (29.0%), other personnel with patient contact (16.7%), and other personnel without patient contact (29.4%).
Table 1.
Demographics for 538 survey participants.
| Demographic | N (%), mean ± SD |
|---|---|
| Occupation Type | |
| Nursing | 134 (24.9) |
| Other clinical professions | 156 (29.0) |
| Other clinical personnel | 90 (16.7) |
| Non-clinical personnel | 158 (29.4) |
| Gender (missing 1) | |
| Female | 422 (78.4) |
| Male | 85 (15.8) |
| Other/prefer not to say | 30 (5.6) |
| Education | |
| High School | 13 (2.4) |
| College diploma | 79 (14.7) |
| Undergraduate degree | 176 (32.7) |
| Professional/Graduate degree | 270 (50.2) |
| Ethnic Group (missing 1) | |
| African/Black | 30 (5.6) |
| Asian | 148 (27.5) |
| East Indian | 35 (6.5) |
| European/White | 278 (51.7) |
| Hispanic | 15 (2.8) |
| Other/Mixed/Multiple | 31 (5.8) |
| Age (years) | 38.5 ± 11.9 |
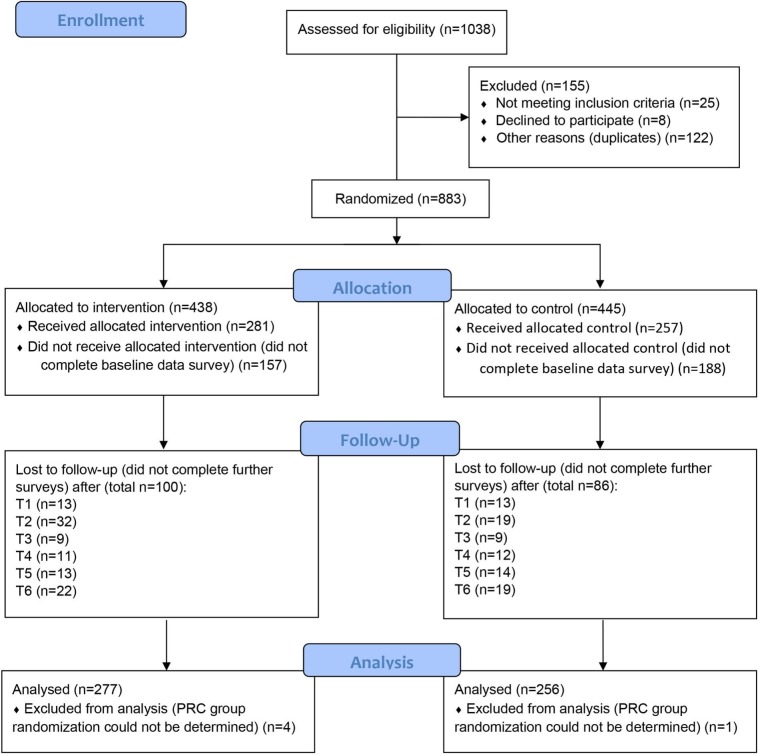
The number of survey participants assigned to each PSAF condition, and the number lost to follow-up at each time-point is provided in the CONSORT diagram (Fig. 2 ). Regarding the intention to treat, there was no significant difference between those were randomized and received interventions and those who were lost to follow-up with respect to occupation group (Χ2 = 0.7, p = .89), gender (male/female) (Χ2 = 1.8, p = .18), education (Χ2 = 2.8, p = .44), or ethnicity (White/non-White) (Χ2 = 1.2, p = .27).
Fig. 2.
CONSORT flow diagram for Personalized Self-Awareness Feedback (PSAF) intervention.
3.2. PSAF comparison groups
Two-hundred and fifty-seven participants were randomized to the express (no feedback) version of the survey and 281 to the enriched (feedback) version. Comparison between these intervention and control groups revealed no significant difference in gender, age, occupation type, or ethnicity (Supplementary File 3). PSAF groups did not differ in emotional exhaustion at baseline (express: 25.0 ± 12.3, enriched: 25.2 ± 12.5, F = 0.0, p = .88).
3.3. PRC comparison groups
Over the course of the intervention, PRCs met with 61 groups across two hospital sites, providing over 1100 sessions. A CONSORT diagram for the PRC trial is not possible because it is not known how many staff in the units assigned to each randomization group attended PRC sessions, nor how many of those who attended sessions participated in the survey. The characteristics of study participants compared by the PRC group to which their unit or department was assigned is provided in Supplementary File 4. Notably, there were significant differences in occupation type (F = 124.8, p < .0001) between groups, related to differences in the types of units and departments assigned to each group. PRC groups did not differ in emotional exhaustion at baseline (Group A: 24.3 ± 11.1, Group B: 27.6 ± 14.6, Group C: 25.9 ± 13.9, Group D: 26.5 ± 13.0, Group E: 23.2 ± 11.2, F = 2.126, p = .08).
3.4. Analysis
Details of the analysis of main and interaction effects of study variables on emotional exhaustion over the course of the survey's seven time points is provided in Supplementary File 5. The full model shows significant main effects of time (F = 14.7, p < .0001) and occupation type (F = 7.9, p < .0001) as well as a significant interaction of PSAF assignment and time (F = 3.2, p = .005). In the final model, clearly non-significant interactions were removed, and the models rerun, to improve the precision of the parameter estimates for the main effect terms, while the near-significant interaction of PRC intervention and time in the full model (F = 2.5, p = .06) was retained. The results of the final model confirm significant main effects of time (F = 14.9, p < .0001) and occupation type (F = 7.8, p < .0001) as well as a significant interaction of PSAF assignment and time (F = 2.8, p = .01). The interaction of PRC intervention and time remain non-significant in the final model (F = 2.5, p = .06).
3.5. Post hoc testing
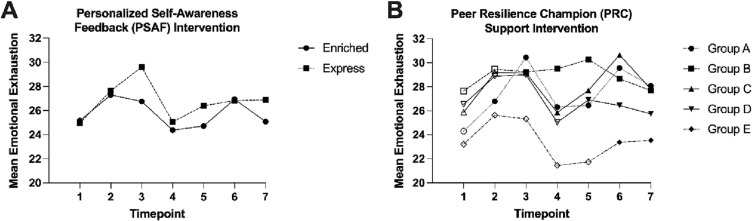
Post hoc testing of the difference in emotional exhaustion over time between the groups randomized to the enriched (PSAF) or express (no feedback) surveys, revealed significantly lower emotional exhaustion in the group who received PSAF at T3 and nonsignificant trends in the same direction at T2, T4, T5, and T7 (Supplementary Table 5). However, a linear mixed model testing the slope of change over time by allocation category for participants who did and did not receive PSAF did not find the difference in slopes to be statistically significant. The longitudinal pattern of emotional exhaustion at each time point by PSAF allocation group is illustrated in Fig. 3 , Panel A.
Fig. 3.
Trends in emotional exhaustion over time in groups randomized with respect to survey feedback (Panel A) and Peer Resilience Champion availability (Panel B).
Note: For panel B, open markers indicate survey time-points prior to availability of the PRC intervention and filled markers indicate survey time-points after availability of the intervention.
Post hoc testing of the near-significant effect of the interaction of PRC availability and time was also conducted in case it is informative for future research. Comparison of emotional exhaustion between groups having or not yet having PRC availability at individual timepoints (Supplementary Table 5) revealed a non-significant trend toward greater emotional exhaustion in the post-PRC availability group at T4 and T5. The longitudinal pattern of emotional exhaustion over time is illustrated in Fig. 3, Panel B. Inspection of this figure indicates complex changes in emotional exhaustion over time. There is no indication of any trend toward the effectiveness of the PRC intervention, and a non-significant indication of a trend in the opposite direction.
4. Discussion
Supports for the mental health of healthcare workers during prolonged, extraordinary occupational stress are greatly needed and yet it is challenging to test their effectiveness in the complex environment of healthcare organizations, especially during a crisis. During the COVID-19 pandemic, this complexity has been amplified by large fluctuations in emotional exhaustion over time, related to waves of hospitalized cases [37]. This study demonstrates that in this environment, recurrent, brief personalized feedback about psychological variables buffered the impact of stressors on emotional exhaustion. On the other hand, we found no evidence that the availability of a hospital-wide peer support intervention buffered emotional exhaustion.
The effectiveness of PSAF is consistent with previous evidence that modest psychological feedback can influence behavior change [38]. In addition, automated feedback of psychological variables was one component of a computerized, interactive learning intervention that previously showed significant psychological benefits in preparation for an H1N1 pandemic [22]. Possible mechanisms by which personalized feedback could influence mental health include the value of self-awareness and self-reflection, the experience of validation, or the utility of specific suggestions. It is noteworthy that despite a significant buffering effect of PSAF, levels of emotional exhaustion continued to fluctuate substantially over time (Fig. 3), in a temporal pattern which corresponds with local fluctuations in COVID-19 case rates [37]. It is also important that the PSAF intervention varied in its effectiveness at different points, with a difference between intervention groups at specific timepoints being significant only at T3. There was no significant overall difference in the slopes of emotional exhaustion by time between the PSAF and no feedback groups, which suggests the benefits of PSAF were limited. This variation in effectiveness may have been the result of dynamically changing occupational stressors or could relate to differences in the effectiveness of specific aspects of feedback (for example the T3 measure followed feedback about interpersonal problems at T2). Overall, a relatively small effect of this intervention with fluctuation over time is consistent with the suggestion that individual-level interventions are at best partially effective in buffering the impact of severe societal and organization-level stressors [3].
Evidence for effectiveness of PSAF may be important to future efforts to mitigate healthcare workers' occupational stress. Importantly, the difference found in emotional exhaustion between PSAF intervention and control groups was clinically meaningful but not large. However, the cost of providing automated feedback using a survey platform is relatively low and availability depends only on internet access. Thus, the potential of PSAF for scale and spread is high. Further research could address the optimal dose and frequency and determine if PSAF provides benefit under non-pandemic conditions. As a low-cost, easy-access intervention with significant benefits on an outcome, burnout, which is common and need not indicate the presence of mental disorder, an intervention like PSAF could be considered in an early phase of a stepped care approach to supporting healthcare workers, with more intensive resources reserved for those with greater needs.
This study provided no evidence that the availability of in-person peer support reduces emotional exhaustion. Discussion of this finding requires attention to both the intervention and the method of evaluation. With respect to the intervention, PRC support combined many elements of staff support and was applied adaptively, contextualized to local contexts. While such an approach is justified under the circumstances of a dynamic stressor with varied impacts over time and by local context, in a research context this adaptability creates uncertainty regarding the potential effectiveness of any of its elements. It also important that a total PRC workforce of 1.5 full-time equivalent Peer Champions is a small resource in the context of a 6000-employee organization. Peer Resilience Champions received frequent, spontaneous positive feedback from participants, which suggests the intervention was valued. With respect to the evaluation strategy, the stepped-wedge study design has limitations. First, evaluation via repeated staff surveys could only evaluate the effects of PRC availability, not participation in PRC sessions, because it is not known how many of the survey responders also participated in PRC sessions. Second, grouping of clinical units for stepped wedge assignment may result in significant differences in the composition of comparison groups, as occurred this study with differences between-group with respect to occupation type. Baseline differences are accounted for statistically in our analysis but were not eliminated by study design, which would have facilitated a more robust comparison. The third limitation is the dynamic nature of the both the stressor and the intervention; it is likely that the Peer Champions developed greater skills in this support work over the course of their work and may have emphasized different resources or tasks at different times. Bearing these limitations in mind, while this study finds no evidence of the effectiveness of peer support, neither is it sufficient to demonstrate that peer support is ineffective.
Finally, since the effect of PRC availability over time was near-significant (p = .06), we considered if the result was due to a lack of statistical power. Indeed, recruitment to the survey did not meet the targets established by the initial sample size calculation (200 staff members per group), which we attribute to the challenges of recruiting hospital staff to participate in research in the context of a pandemic. However, the trend in post-hoc testing was not in the direction of a potentially effective intervention (pre-intervention slope of emotional exhaustion was in the direction of improvement, whereas the post-intervention slope of emotional exhaustion was flat). Therefore, we do not think the null result is due to a lack of power.
This study has a number of strengths. Compared to other reported studies of healthcare worker support during the pandemic, the sample size is larger and the length of follow-up longer. The PSAF intervention is based on previous work [22], and so the consistency of findings adds confidence in the current result. The population recruited included all types of occupations, volunteers, and learners in a hospital setting, which is broader and more representative than previous studies of specific healthcare professions, such as physicians and nurses.
There are also several limitations. Given the wide array of support resources applied in our hospital during the pandemic, it is difficult to isolate the benefits of any particular one. The environmental stressor during this study was very changeable over time which complicates assessing interventions. The limitations of the study design to assess the PRC intervention are described in detail above. Recruitment for survey participation did not include a sampling procedure that would ensure a representative sample (although the sample which was recruited represented most occupational roles within the organization). The drop-out rate prior to providing baseline data was higher in people randomly assigned to PSAF than to the control condition. Since participants had no information about their assignment prior to providing baseline data, this difference is not related to the intervention, but could introduce bias. The study was conducted at two sites of a single healthcare organization. The lack of a strategy to ensure a representative sample and inclusion of a single hospital organization restrict our ability to draw conclusions about the generalizability of results. Job type was a strong correlate of emotional exhaustion and the composition of the work force with respect to job types is likely to differ across organizations.
In summary, this study reports on support interventions for hospital-based healthcare workers during the COVID-19 pandemic in a trial that is the largest and has the longest follow-up of any thus far reported to our knowledge. It provides evidence of a significant and meaningful effect of repeated, automated feedback of personal psychological characteristics to buffer the effects of extraordinary occupational stress on emotional exhaustion. This intervention shows promise for wider application in the future, pending replication in different settings and determination of optimal dose and frequency.
Funding sources
Canadian Institutes of Health Research (FRN OV7–170642) and the Chair in Health and Behaviour at Sinai Health (funded by Sinai Health Foundation and the Medical Psychiatry Alliance, University of Toronto).
CRediT authorship contribution statement
Robert G. Maunder: Funding acquisition, Conceptualization, Methodology, Writing – original draft, Writing – review & editing. Alex Kiss: Funding acquisition, Formal analysis, Writing – review & editing. Natalie Heeney: Data curation, Project administration, Writing – original draft, Writing – review & editing. Emma Wallwork: Investigation, Writing – review & editing. Jonathan J. Hunter: Conceptualization, Funding acquisition, Writing – review & editing. Jennie Johnstone: Funding acquisition, Writing – review & editing. Lesley Wiesenfeld: Supervision, Writing – review & editing. Lianne Jeffs: Funding acquisition, Writing – review & editing. Allison McGeer: Funding acquisition, Writing – review & editing. Kyla Lee: Visualization, Writing – review & editing. Carla Loftus: Funding acquisition, Writing – review & editing. Leanne Ginty: Project administration, Writing – review & editing. Kate Wilkinson: Funding acquisition, Writing – review & editing. Jane Merkley: Funding acquisition, Writing – review & editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.genhosppsych.2023.06.005.
Appendix A. Supplementary data
Supplementary material 1
Supplementary material 2
Supplementary material 3
Supplementary material 4
Supplementary material 5
Data availability
Data will be made available on request.
References
- 1.World Health Organization WHO Director-General's opening remarks at the media briefing on COVID-19 - 30 March 2020. [Internet] 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---30-march-2020 Available from:
- 2.Saragih I.D., Tonapa S.I., Saragih I.S., Advani S., Batubara S.O., Suarilah I., et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Int J Nurs Stud. 2021 Sep 1;121 doi: 10.1016/j.ijnurstu.2021.104002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maunder R.G., Heeney N.D., Strudwick G., Shin H.D., O'Neill B., Young N., et al. Burnout in Hospital-Based Healthcare Workers during COVID-19. 2021 Oct 7. https://covid19-sciencetable.ca/sciencebrief/burnout-in-hospital-based-healthcare-workers-during-covid-19 [cited 2021 Oct 24]; Available from:
- 4.Soklaridis S., Lin E., Lalani Y., Rodak T., Sockalingam S. Mental health interventions and supports during COVID- 19 and other medical pandemics: a rapid systematic review of the evidence. Gen Hosp Psychiatry. 2020 Sep 1;66:133–146. doi: 10.1016/j.genhosppsych.2020.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zaçe D., Hoxhaj I., Orfino A., Viteritti A.M., Janiri L., di Pietro M.L. Interventions to address mental health issues in healthcare workers during infectious disease outbreaks: a systematic review. J Psychiatr Res. 2021 Apr 1;136:319–333. doi: 10.1016/j.jpsychires.2021.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DeTore N.R., Sylvia L., Park E.R., Burke A., Levison J.H., Shannon A., et al. Promoting resilience in healthcare workers during the COVID-19 pandemic with a brief online intervention. J Psychiatr Res. 2022 Feb 1;146:228–233. doi: 10.1016/j.jpsychires.2021.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fiol-DeRoque M.A., Serrano-Ripoll M.J., Jiménez R., Zamanillo-Campos R., Yáñez-Juan A.M., Bennasar-Veny M., et al. A mobile phone-based intervention to reduce mental health problems in health care workers during the COVID-19 pandemic (PsyCovidApp): randomized controlled trial. JMIR Mhealth Uhealth [Internet] 2021 May 1;9(5) doi: 10.2196/27039. https://pubmed.ncbi.nlm.nih.gov/33909587/ [cited 2022 Oct 4]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Amsalem D., Lazarov A., Markowitz J.C., Smith T.E., Dixon L.B., Neria Y. Video intervention to increase treatment-seeking by healthcare workers during the COVID-19 pandemic: randomised controlled trial. Br J Psychiatry [Internet] 2022 Jan 4;220(1):14–20. doi: 10.1192/bjp.2021.54. https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/abs/video-intervention-to-increase-treatmentseeking-by-healthcare-workers-during-the-covid19-pandemic-randomised-controlled-trial/98D0062592FB590A01B8222CADC68B09 [cited 2022 Oct 4]. Available from: [DOI] [PubMed] [Google Scholar]
- 9.Procaccia R., Segre G., Tamanza G., Manzoni G.M. Benefits of expressive writing on healthcare Workers’ psychological adjustment during the COVID-19 pandemic. Front Psychol. 2021 Feb 25;12:360. doi: 10.3389/fpsyg.2021.624176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dincer B., Inangil D. The effect of Emotional Freedom Techniques on nurses’ stress, anxiety, and burnout levels during the COVID-19 pandemic: A randomized controlled trial. Explore (NY) [Internet] 2021 Mar 1;17(2):109–114. doi: 10.1016/j.explore.2020.11.012. https://pubmed.ncbi.nlm.nih.gov/33293201/ [cited 2022 Oct 4]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vajpeyee M., Tiwari S., Jain K., Modi P., Bhandari P., Monga G., et al. 2021 Apr 5. Yoga and music intervention to reduce depression, anxiety, and stress during COVID-19 outbreak on healthcare workers. [cited 2022 Oct 4];68(4):798–807. Available from: [DOI] [PubMed] [Google Scholar]
- 12.Giordano F., Scarlata E., Baroni M., Gentile E., Puntillo F., Brienza N., et al. Receptive music therapy to reduce stress and improve wellbeing in Italian clinical staff involved in COVID-19 pandemic: a preliminary study. Arts Psychother. 2020 Sep 1;70 doi: 10.1016/j.aip.2020.101688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheung V.K.L., So E.H.K., Ng G.W.Y., So S.S., Hung J.L.K., Chia N.H. Investigating effects of healthcare simulation on personal strengths and organizational impacts for healthcare workers during COVID-19 pandemic: a cross-sectional study. Integr Med Res. 2020 Sep 1;9(3) doi: 10.1016/j.imr.2020.100476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheng W., Zhang F., Liu Z., Zhang H., Lyu Y., Xu H., et al. A psychological health support scheme for medical teams in COVID-19 outbreak and its effectiveness. Gen Psychiatr [Internet] 2020 Aug 30;33(5) doi: 10.1136/gpsych-2020-100288. https://pmc/articles/PMC7462042/ [cited 2022 Oct 4]. 100288. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ben-Arye E., Gressel O., Samuels N., et al. Complementary and integrative medicine intervention in front-line COVID-19 clinicians. BMJ Supportive & Palliative Care. 05 April 2022 doi: 10.1136/bmjspcare-2021-003333. Published Online First: [DOI] [PubMed] [Google Scholar]
- 16.Beverly E., Hommema L., Coates K., Duncan G., Gable B., Gutman T., et al. A tranquil virtual reality experience to reduce subjective stress among COVID-19 frontline healthcare workers. PLoS One [Internet] 2022 Feb 1;17(2) doi: 10.1371/journal.pone.0262703. e0262703. Available from:. [cited 2022 Oct 4] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yi-Frazier J.P., O’Donnell M.B., Adhikari E.A., Zhou C., Bradford M.C., Garcia-Perez S., et al. Assessment of resilience training for hospital employees in the era of COVID-19. JAMA Netw Open [Internet] 2022 Jul 1;5(7) doi: 10.1001/jamanetworkopen.2022.20677. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2793802 [cited 2022 Oct 4]. e2220677–e2220677. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jeffs L., Merkley J., Greenberg R., Ginty L., Amaral N., Maunder R., et al. An Academic Health Sciences Centre’s Strategy to Enhance Nurse Resilience and Psychological Safety. Nurs Leadersh (Tor Ont) [Internet] 2021;34(2):39–44. doi: 10.12927/cjnl.2021.26531. https://www.ncbi.nlm.nih.gov/pubmed/341972 2021/07/02. Available from: [DOI] [PubMed] [Google Scholar]
- 19.Rosen B., Preisman M., Hunter J., Maunder R. Applying Psychotherapeutic Principles to Bolster Resilience Among Health Care Workers During the COVID-19 Pandemic. Am J Psychother [Internet] 2020;73(4):144–148. doi: 10.1176/appi.psychotherapy.20200020. https://www.ncbi.nlm.nih.gov/pubmed/32985915 [DOI] [PubMed] [Google Scholar]
- 20.Rosen B., Preisman M., Read H., Chaukos D., Greenberg R.A., Jeffs L., et al. Resilience coaching for healthcare workers: Experiences of receiving collegial support during the COVID-19 pandemic. Gen Hosp Psychiatry [Internet] 2022;75:83–87. doi: 10.1016/j.genhosppsych.2022.02.003. https://pubmed.ncbi.nlm.nih.gov/35247687/ Mar 1 [cited 2022 Oct 4] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosen B., Preisman M., Read H., Chaukos D., Greenberg R.A., Jeffs L., et al. Providers’ perspectives on implementing resilience coaching for healthcare workers during the COVID-19 pandemic. BMC Health Serv Res. 2022;22(1) doi: 10.1186/s12913-022-08131-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maunder R.G., Lancee W.J., Mae R., Vincent L., Peladeau N., Beduz M.A., et al. Computer-assisted resilience training to prepare healthcare workers for pandemic influenza: A randomized trial of the optimal dose of training. BMC Health Serv Res [Internet] 2010;10(1):1–10. Mar 22 [cited 2021 Dec 21];Available from: https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-10-72. [DOI] [PMC free article] [PubMed]
- 23.Aiello A., Khayeri M.Y., Raja S., Peladeau N., Romano D., Leszcz M., et al. Resilience training for hospital workers in anticipation of an influenza pandemic. J Contin Educ Health Prof [Internet] 2011;31(1):15–20. doi: 10.1002/chp.20096. http://www.ncbi.nlm.nih.gov/pubmed/21425355 [DOI] [PubMed] [Google Scholar]
- 24.Anderson G.S., di Nota P.M., Groll D., Carleton R.N. Peer support and crisis-focused psychological interventions designed to mitigate post-traumatic stress injuries among public safety and frontline healthcare personnel: a systematic review. Int J Environ Res Public Health. 2020 Oct 20;17(20):7645. doi: 10.3390/ijerph17207645. https://www.mdpi.com/1660-4601/17/20/7645/htm [cited 2022 Oct 11]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maslach C., Jackson S., Leiter M. Consulting Psychologists Press; 1996. Maslach Burnout Inventory Manual [Internet]https://www.worldcat.org/title/maslach-burnout-inventory-manual/oclc/807246527 [cited 2021 Oct 20]. Available from: [Google Scholar]
- 26.Maunder R.G., Hunter J.J. An Internet Resource for Self-Assessment of Mental Health and Health Behavior: Development and Implementation of the Self-Assessment Kiosk. JMIR Ment Health [Internet] 2018;5(2):e39. doi: 10.2196/mental.9768. https://www.ncbi.nlm.nih.gov/pubmed/29769171 2018/05/18. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carver C.S., Scheier M.F., Weintraub J.K. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol [Internet] 1989;56(2):267–283. doi: 10.1037//0022-3514.56.2.267. https://www.researchgate.net/publication/20228888_Assessing_Coping_Strategies_A_Theoretically_Based_Approach [cited 2021 Dec 21]. Available from: [DOI] [PubMed] [Google Scholar]
- 28.Horowitz L.M., Rosenberg S.E., Baer B.A., Ureno G., Billasenor V.S. Inventory of interpersonal problems: psychometric properties and clinical applications. J Consult Clin Psychol. 1988;56:885–892. doi: 10.1037//0022-006x.56.6.885. [DOI] [PubMed] [Google Scholar]
- 29.Epstein E.G., Whitehead P.B., Prompahakul C., Thacker L.R., Hamric A.B. Enhancing understanding of moral distress: the measure of moral distress for health care professionals. AJOB Empir Bioeth [Internet] 2019/04/20;10(2):113–124. doi: 10.1080/23294515.2019.1586008. https://www.ncbi.nlm.nih.gov/pubmed/31002584 Available from: [DOI] [PubMed] [Google Scholar]
- 30.Lo C., Walsh A., Mikulincer M., Gagliese L., Zimmermann C., Rodin G. Measuring attachment security in patients with advanced cancer: psychometric properties of a modified and brief experiences in close relationships scale. Psychooncology. 2009;18(5):490–499. doi: 10.1002/pon.1417. [DOI] [PubMed] [Google Scholar]
- 31.Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S., et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12(12) doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Madhavappallil, Kohli V., Choi J. Correlates of job burnout among human services workers: implications for workforce retention. J Sociol Soc Welf [Internet] 2014;41 https://scholarworks.wmich.edu/jsswAvailableat:https://scholarworks.wmich.edu/jssw/vol41/iss4/5 [cited 2023 Mar 8]. Available from: [Google Scholar]
- 33.Soares J.J.F., Grossi G., Sundin Ö. Burnout among women: associations with demographic/socio-economic, work, life-style and health factors. Arch Womens Ment Health [Internet] 2007 Apr;10(2):61–71. doi: 10.1007/s00737-007-0170-3. https://pubmed.ncbi.nlm.nih.gov/17357826/ [cited 2023 Mar 8]. Available from: [DOI] [PubMed] [Google Scholar]
- 34.Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. Bmj [Internet] 2020/05/07;369 doi: 10.1136/bmj.m1642. https://www.ncbi.nlm.nih.gov/pubmed/32371466 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brooks S.K., Dunn R., Amlot R., Rubin G.J., Greenberg N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J Occup Environ Med [Internet] 2017/12/19;60(3):248–257. doi: 10.1097/JOM.0000000000001235. https://www.ncbi.nlm.nih.gov/pubmed/29252922 Available from: [DOI] [PubMed] [Google Scholar]
- 36.Rotenstein L.S., Torre M., Ramos M.A., Rosales R.C., Guille C., Sen S., et al. Prevalence of burnout among physicians: a systematic review. JAMA [Internet] 2018/10/17;320(11):1131–1150. doi: 10.1001/jama.2018.12777. https://www.ncbi.nlm.nih.gov/pubmed/30326495 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maunder R.G., Heeney N.D., Hunter J.J., Strudwick G., Jeffs L.P., Ginty L., et al. Trends in burnout and psychological distress in hospital staff over 12 months of the COVID-19 pandemic: a prospective longitudinal survey. Journal of Occupational Medicine and Toxicology 2022 17:1 [Internet] 2022;17(1):1–11. doi: 10.1186/s12995-022-00352-4. https://occup-med.biomedcentral.com/articles/10.1186/s12995-022-00352-4 May 25 [cited 2022 Jul 26]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Palfai T.P., Zisserson R., Saitz R. Using personalized feedback to reduce alcohol use among hazardous drinking college students: the moderating effect of alcohol-related negative consequences. Addict Behav [Internet] 2011/02/08;36(5):539–542. doi: 10.1016/j.addbeh.2011.01.005. https://www.ncbi.nlm.nih.gov/pubmed/21295919 Available from: [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 1
Supplementary material 2
Supplementary material 3
Supplementary material 4
Supplementary material 5
Data Availability Statement
Data will be made available on request.