Video
Endoscopic full-thickness resection of a GI stromal tumor lesion arising in the rectum’s muscularis propria.
GI stromal tumors (GISTs) are characterized as the most common subset of mesenchymal neoplasms arising in the subepithelial of the GI tract. While subepithelial tumors (SETs) are recognized as asymptomatic and clinically insignificant, other SETs, including GISTs, are neoplastic or can potentially progress to malignancy.1 Therefore, it is important to determine the diagnosis and predict a prognosis. However, the diagnosis of GISTs may be delayed because of their vague symptomatic presentation.2 While bite-on-bite biopsy has low diagnostic accuracy, the current standard procedure of EUS fine-needle biopsy (FNB) has better accuracy in making a tissue diagnosis for subepithelial lesions and can diagnose metastasis for neighboring lymphadenopathy.3 Yet, EUS-FNB may not necessarily provide sufficient tissue to make a pathological determination regarding high-risk features. The choice of intervention type for subepithelial rectal lesion will depend on the location of the lesion. In a female patient with a subepithelial lesion at the anterior rectal wall, a transanal surgical approach will be the preferred intervention because of the thin rectovaginal septum and the risk of rectovaginal fistula development after endoscopic surgery.4 A lesion on the posterior wall can be treated safely with the endoscopic approach. Recently, a new procedure has been developed to resect SETs: endoscopic full-thickness resection (EFTR). Here we present EFTR of a lesion arising in the rectum's muscularis propria (MP) (Video 1, available online at www.videogie.org).
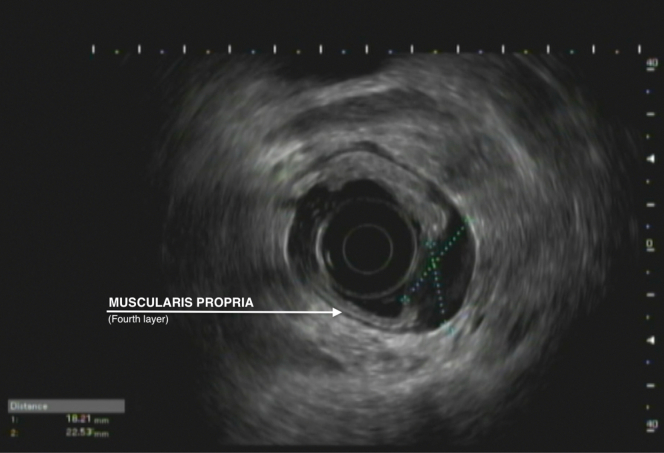
A 54-year-old woman underwent a screening colonoscopy, during which a posterior rectal submucosal mass was observed. Tissue collected by a 25-gauge FNB was inadequate for histopathological diagnosis, and thus, the patient was referred. We performed a repeat rectal EUS, which showed a 23- × 18- × 15-mm hypoechoic fourth-layer mass arising from the MP (Figs. 1 and 2). As previous FNAs were nondiagnostic, and there was no mitotic index suggesting a high-risk lesion, our multidisciplinary tumor board decided to proceed with EFTR given the posterior rectal location with potential diagnostic and curative purposes in mind. After the patient consulted with our oncology team, EFTR was carried out.
Figure 1.
US view showing 23- × 18- × 15-mm rectal submucosal lesion.
Figure 2.
Endoscopic view showing rectal submucosal lesion.
While the patient was under general anesthesia, EFTR was carried out with endoscopic carbon dioxide insufflation. A single-channel gastroscope (EG-760Z; Fujifilm, Tokyo, Japan) with a transparent hood attachment was used in conjunction with an endoscopic submucosal dissection knife (DualKnife J; Fujifilm, Tokyo, Japan) for incision and dissection.
After creating a generous circumferential thermal marking with the distal cap attached to the endoscope, gel-based pigmented fluid submucosal dynamic injections (ORISE; Boston Scientific, Boston, Mass, USA) were performed to expand the submucosal space. A short retractable electrocautery needle extending from the ceramic base guided the mucosal incision of the submucosa until the mass was no longer readily visible. Once the mass was exposed to the level of the muscularis mucosa, a traction wire suture loop (ProdiGI Wire; Medtronic, Dublin, Ireland) was affixed above the distal side of the lesion with a built-in clip. The free loop is then grasped with a secondary clip and attached to the proximal rectal wall. The traction wire pulls on the mass, proximally exposing dissection planes (Fig. 3). As the mass was dissected, it retracted upward and away from the scope, further exposing the subepithelial space until it was freed from the rectal wall. When dissection was complete, it was possible to appreciate the abundant perirectal fat in the absence of the mucosa and MP (Fig. 4). Full-thickness closure from left to right was obtained with a dual-channel endoscope with a fixed suturing device. Full inspection showed complete full-thickness closure with an approximation of the mucosa (Figs. 5 and 6). The histopathologic assessment showed R0 resection with features typical of a GIST and negative peripheral and deep margins. The subtype of this GIST was determined to have the least malignancy, which goes well for this patient. After the 3.5-hour procedure, the patient was administered ciprofloxacin 400 mg intravenously and was observed in the hospital for 2 nights. The patient recovered well and was discharged without any postoperative challenges. Colonoscopy and EUS were performed 4 months postresection with no evidence of recurrence.
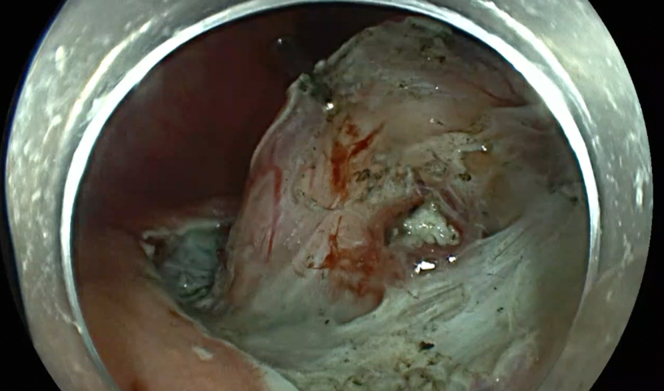
Figure 3.
Endoscopic view showing dissection plane, perirectal fat, and muscle using a retraction device.
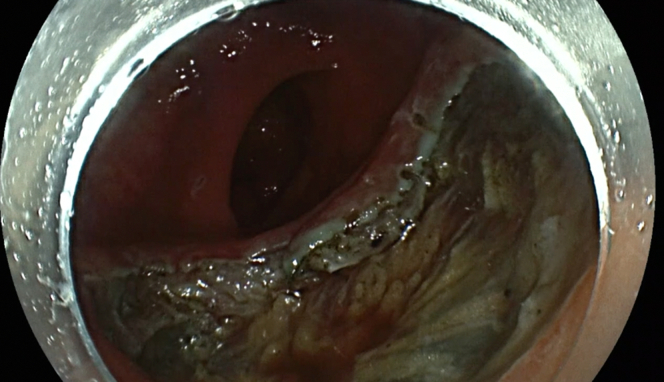
Figure 4.
Endoscopic view showing exposed mesorectum after resection.
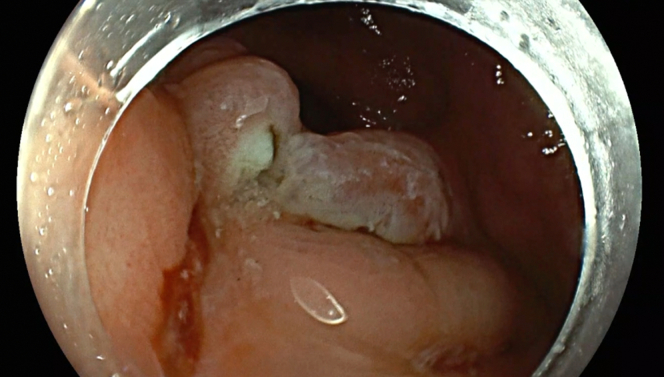
Figure 5.
Endoscopic view showing full-thickness closure with approximation of the mucosa.
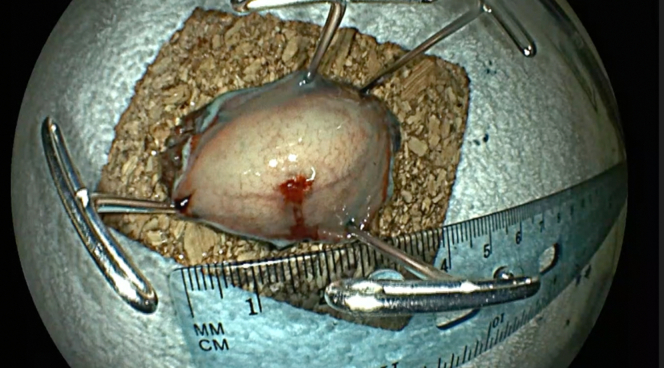
Figure 6.
Pinned-down submucosal lesion.
Alternative treatments include transanal minimally invasive, which may carry greater patient morbidity. Another alternative is the use of an EFTR device, which will be limited in the rectum because of its size, location, and depth of mass, especially by the limited mobility of the rectal wall. Therefore, for a well-identified rectal submucosal mass, EFTR offers a safe and minimally invasive option for resectioning lesions originating in the MP, such as GISTs (Video 1, available online at www.videogie.org).
Disclosure
The authors disclosed no financial relationships.
Supplementary data
Endoscopic full-thickness resection of a GI stromal tumor lesion arising in the rectum's muscularis propria.
References
- 1.Cho J.W., Korean ESD Study Group Current guidelines in the management of upper gastrointestinal subepithelial tumors. Clin Endosc. 2016;49:235–240. doi: 10.5946/ce.2015.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stamatakos M., Douzinas E., Stefanaki C., et al. Gastrointestinal stromal tumor. World J Surg Oncol. 2009;7:61. doi: 10.1186/1477-7819-7-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Han J., Cho J., Song J., Yang M., Lee Y., Ju M. Endoscopic subserosal dissection for gastric tumors: 18 cases in a single center. Surg Endosc. 2022;36:8039–8046. doi: 10.1007/s00464-022-09229-3. [DOI] [PubMed] [Google Scholar]
- 4.Kumar S., Coronel M.A., Romero L.G., Coronel E.S., Ge P.S. Full-thickness resection: troubleshooting, tips, and tricks for success in the colorectum. VideoGIE. 2022;7:201–204. doi: 10.1016/j.vgie.2022.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic full-thickness resection of a GI stromal tumor lesion arising in the rectum’s muscularis propria.
Endoscopic full-thickness resection of a GI stromal tumor lesion arising in the rectum's muscularis propria.