Abstract
Background:
Hypothermic young infants presenting to the Emergency Department (ED) are at risk for serious bacterial infections (SBI), however there is no consensus temperature to prompt evaluation for SBI among these children. We sought to statistically derive a temperature threshold to guide detection of SBI in hypothermic young infants presenting to the ED.
Methods:
We performed a cross-sectional study of infants ≤90 days old presenting to four academic pediatric EDs from January 2015 through December 2019 with a rectal temperature of ≤36.4°C. Our primary outcomes were SBI, defined as urinary tract infection (UTI), bacteremia, and/or bacterial meningitis, and invasive bacterial infections (IBI, limited to bacteremia and/or bacterial meningitis). We constructed receiver operating characteristic (ROC) curves to evaluate an optimally derived cutpoint for minimum ED temperature and presence of SBI or IBI.
Results:
We included 3,376 infants, of whom SBI were found in 62 (1.8%) and IBI in 16 (0.5%). The most common infection identified was Escherichia coli UTI. Overall cohort minimum median temperature was 36.2°C (IQR 36.0–36.4°C). Patients with SBI and IBI had lower median temperatures, 35.8°C (IQR 35.8–36.3°C) and 35.4°C (IQR 35.7–36.3°C) respectively, compared to those without corresponding infections (both P<0.05). Using an outcome of SBI, the area under the ROC curve (AUROC) was 61.0% (95% CI 54.1–67.9%). At a cutpoint of 36.2°C, sensitivity was 59.7% and specificity was 59.2%. When using an outcome of IBI, the AUROC was 65.9% (95% CI 51.1–80.6%). Using a cutpoint of 36.1°C in this model resulted in a sensitivity of 68.8% and specificity of 60.1%.
Conclusion:
Young infants with SBI and IBI presented with lower temperatures than infants without infections. However, there was no temperature threshold to reliably identify SBI or IBI. Further research incorporating clinical and laboratory parameters, in addition to temperature, may help to improve risk stratification for these vulnerable patients.
Keywords: serious bacterial infections, hypothermia, temperature threshold, invasive bacterial infections
Introduction:
Temperature instability is a known risk factor for the presence of serious bacterial infections (SBI) among young infants presenting to the emergency department (ED) [1–7]. Through decades of research efforts to identify risk factors for SBI among febrile infants, the American College of Emergency Physicians and the American Academy of Pediatrics have established consensus policy guidelines for evaluating and managing young febrile infants in the ED [6,8]. In contrast, robust multicenter literature on hypothermic infants is lacking. Studies evaluating hypothermic infants are limited to single-center or administrative data sources [1–5]. Postulated reasons for hypothermia in the setting of overwhelming infection have included an altered regulatory response, increased catabolism, inflammatory activation in response to bacterial pyrogens, and endothelial dysfunction [9–13].
A unique challenge in investigating the association of SBI among hypothermic infants lies in the lack of a universally accepted temperature threshold to define hypothermia in this population. The World Health Organization (WHO) categorizes hypothermia in newborns as severe (<32 °C), moderate (32.0 to 35.9 °C), and mild (36.0 to 36.4 °C) [14]. In contrast, the International Pediatric Sepsis Consensus Conference uses <36.0°C among their criteria for the systemic inflammatory response syndrome [15]. Illustrative of this challenge, recently published single-center studies investigating the association between hypothermia and sepsis have used a variety of thresholds to define hypothermia in young children, ranging from 36.0 to 36.4°C [1–4]. These varying cutoffs limit the ability to translate research findings into improved clinical practice.
A statistically derived threshold to define hypothermia would enable clinicians to identify patients at increased risk for SBI more accurately, avoid unnecessary diagnostic testing, and standardize future research. We therefore sought to describe the prevalence of SBI and optimal temperature to define hypothermia among young infants presenting to the ED.
Methods:
Study design and setting.
We conducted a multicenter retrospective cross-sectional study of infants ≤90 days old presenting to one of four academic pediatric EDs from January 2015 to December 2019. We included encounters of patients with measured rectal temperatures ≤36.4°C in the ED, consistent with the most conservative threshold for hypothermia as suggested by the WHO [14]. We retained the first eligible encounter per patient. Data were abstracted electronically from each participating site and uploaded to the secure, web-based Research Electronic Data Capture (REDCap) tool [16] at Northwestern University, Chicago, IL, USA. Approval was granted from each participating site’s Institutional Review Board.
Outcome measures.
Our primary outcomes of interest were SBI and invasive bacterial infection (IBI). SBI was defined as presence of culture-positive bacteremia, bacterial meningitis, and/or urinary tract infection (UTI). IBI was limited to culture-positive bacteremia and/or bacterial meningitis. We used previously delineated criteria for classifying true and false positives from prior multicenter research on febrile infants [17]. For bacteremia and bacterial meningitis, growth of multiple bacteria or those not commonly pathogenic (e.g., diphtheroids, Lactobacillus, coagulase-negative staphylococci, Corynebacteria) were considered contaminants. UTI was defined using as ≥1000 colony forming units (CFU) per mL from urine culture obtained via suprapubic aspiration, ≥50,000 CFU/mL from catheterization, or 10,000–49,999 CFU/mL from catheterization with a positive urinalysis (presence of leukocyte esterase, nitrite, or >5 WBC per high-power field) [18]. Primary site investigators individually assessed indeterminate cultures for inclusion after reviewing medical records, and consensus decisions were made with the input of all members after review. We reported baseline demographic information, proportions of patients with complaints of hypothermia and International Classification of Diseases (ICD), 9th or 10th revision, diagnosis code for hypothermia [5].
Data analysis.
We compared the demographic categories and the minimum temperature among patients with SBI or IBI to those without infections using the chi-square test. We analyzed temperature in isolation without including other clinical or laboratory parameters, e.g., prematurity and co-existing conditions that often affect ED physicians’ decisions to pursue testing for infections. We selected this approach because, in practice, the decision to initiate testing for serious infections in febrile infants is frequently decided in the context of temperature alone [19]. We constructed receiver operating characteristic (ROC) curves for each outcome of interest and calculated the area under the ROC curve (AUROC). We then determined a cutoff value for hypothermic temperature by optimizing sensitivity and specificity along the ROC curve using the Euclidean distance method. We described accuracy as follows: AUC <70% as poor, 70–80% as fair, 80–90% as good, and >90% as excellent. To more discretely evaluate the diagnostic accuracy of differing temperature cutoffs more discretely for SBI and IBI, we reported the sensitivity, specificity, positive and negative predictive values, and positive and negative likelihood ratios using varying definitions of hypothermia from 34.9 to 36.3°C in 0.2°C bands. We performed a sensitivity analysis limited to the subset of children who had a blood culture obtained. Analyses were performed using R, version 4.1.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Study subject characteristics.
We included 3,376 infants. Among these, 53.1% were male, and 1,926 (57.0%) were younger than 30 days old (median age 22.0 days, IQR 6–51). Seventy (2.1%) infants had a chief complaint of hypothermia, and 287 (8.5%) had a relevant ICD-9 or 10 diagnosis code for hypothermia [5]. There were no significant age subgroup differences between infants with SBI and without SBI. The overall median minimum temperature was 36.2 °C (IQR 36.0–36.4°C). Among included patients, 934 (27.7%) had a blood culture, 832 (24.6%) had a urine culture, and 481 (14.2%) had a CSF culture done during their ED encounter. In patients with SBI, 64.5% received antibiotics in the ED. Similarly, 62.5% of patients with IBI received antibiotics in the ED. Demographics, overall and stratified based on SBI and IBI, are presented in Table 1.
Table 1:
Patient characteristics overall and stratified by serious bacterial infection (SBI) and invasive bacterial infection (IBI).
| Total N = 3376 | SBI N = 62 | Without SBI N = 3314 | P | IBI N = 16 | Without IBI N = 3360 | P | |
|---|---|---|---|---|---|---|---|
| Sex, male, n (%) | 1791 (53.1) | 32 (51.6) | 1759 (53.1) | 0.90 | 8 (50.0) | 1783 (53.1) | 0.81 |
| Age, n (%) | 0.86 | 0.37 | |||||
| ≤30 days old | 1942 (57.5) | 34 (54.8) | 1908 (57.6) | 12 (75.0) | 1930 (57.4) | ||
| 31–60 days old | 843 (25.0) | 17 (27.4) | 826 (24.9) | 3 (18.8) | 840 (25.0) | ||
| 61–90 days old | 591 (17.5) | 11 (17.7) | 580 (17.5) | 1 (6.3) | 590 (17.6) | ||
| Race, n (%) | 0.05 | 0.83 | |||||
| White | 2010 (59.5) | 31 (50.0) | 1979 (59.7) | 10 (62.5) | 2000 (59.5) | ||
| Black | 527 (15.6) | 7 (11.3) | 520 (15.7) | 3 (18.8) | 524 (15.6) | ||
| Other | 839 (24.9) | 24 (38.7) | 815 (24.6) | 3 (18.8) | 836 (24.9) | ||
| Presenting season, n (%) | 0.39 | 0.81 | |||||
| Spring (April - June) | 724 (21.4) | 13 (21.0) | 711 (21.5) | 2 (12.5) | 722 (21.5) | ||
| Summer (July – September) | 738 (21.9) | 19 (30.6) | 719 (21.7) | 3 (18.8) | 735 (21.9) | ||
| Fall (October – December) | 1028 (30.5) | 15 (24.2) | 1013 (30.6) | 6 (37.5) | 1022 (30.4) | ||
| Winter (January - March) | 886 (26.2) | 15 (24.2) | 871 (26.3) | 5 (31.3) | 881 (26.2) | ||
| Chief complaint of hypothermia | 70 (2.1) | 1 (1.6) | 69 (2.1) | 1 | 1 (6.3) | 69 (2.1) | 0.29 |
| ICD-9/10 code for hypothermia | 287 (8.5) | 7 (11.3) | 280 (8.4) | 0.36 | 4 (25.0) | 283 (8.4) | 0.04 |
| Received antibiotics | 572 (16.9) | 40 (64.5) | 532 (16.1) | <0.01 | 10 (62.5) | 562 (16.7) | <0.01 |
Comparisons made through chi square tests
Abbreviations: ICD, International Classification of Diseases.
Outcomes.
Sixty-two (1.8%) infants had an SBI and 16 (0.5%) had an IBI. Isolated UTI encompassed 74.2% of all SBI, with 6.1% of UTI associated with concomitant bacteremia. The most common organisms associated with SBI were Escherichia coli (62%), followed by Enterococcus species (16%) and Group B streptococcus (8%) (Table 2).
Table 2:
Serious bacterial infections (SBI) identified in the study cohort, organized by infection type
| SBI Type and Organisms | Number |
|---|---|
| Meningitis with or without bacteremia (n=4) | |
| Group B Streptococcus | 1 |
| Enterococcus faecalis | 1 |
| Staphylococcus aureus | 1 |
| Escherichia coli | 1 |
| Isolated bacteremia (n=9) | |
| Group B Streptococcus | 4 |
| Enterococcus faecalis | 2 |
| Staphylococcus aureus | 1 |
| Streptococcus pneumoniae | 1 |
| Pseudomonas aeruginosa | 1 |
| Bacteremia with UTI (n=3) | |
| Escherichia coli | 3 |
| Isolated UTI (n=46) | |
| Escherichia coli | 35 |
| Enterococcus species | 7 |
| Staphylococcus aureus | 2 |
| Klebsiella species | 1 |
| Enterobacter aerogenes | 1 |
Abbreviations: SBI, serious bacterial infections; UTI, urinary tract infection
Temperature threshold identification.
Among infants with SBI, the median temperature was 35.8°C (IQR 35.8–36.3°C), which was significantly lower than the median temperature among those without SBI (36.0°C; IQR 36.0–36.4°C; p=<0.01). A similar finding was noted for IBI: among infants with IBI, the median temperature was 35.4 °C (IQR 35.7–36.3°C) compared to the median temperature of 36.0 °C (IQR 36.0–36.4°C; p=0.03) among those without IBI.
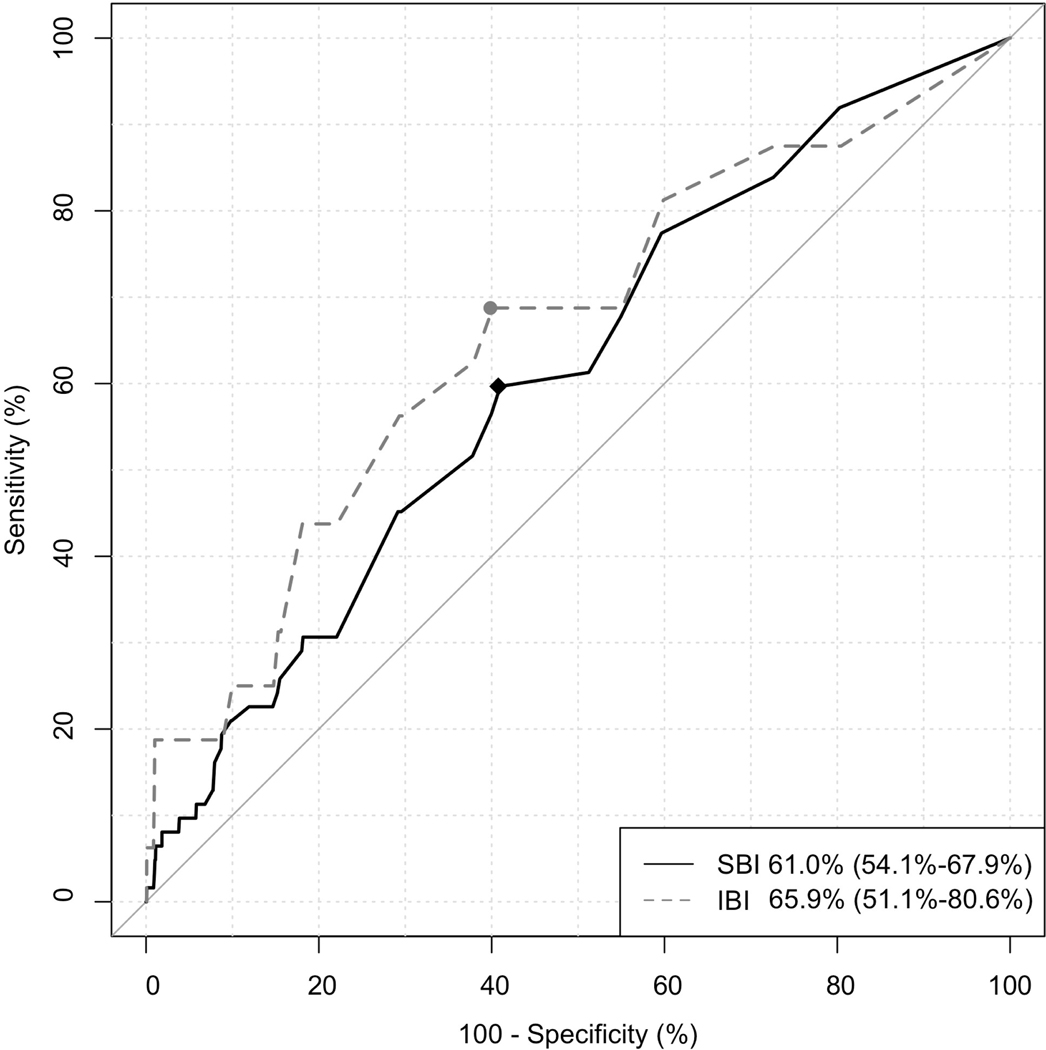
The AUROC for both outcomes demonstrated poor discrimination. When evaluating the performance of temperature with an outcome of SBI, the AUROC was 61.0% (95% CI 54.1–67.9%). The optimally selected cutoff of 36.2°C resulted in a sensitivity of 59.7% and specificity of 59.2%. For IBI, the AUROC was 65.9% (95% CI 51.1–80.6%). A cutoff temperature of 36.1°C resulted in a sensitivity of 68.8% and specificity of 60.1% (Figure). Analysis of sensitivity and specificity in 0.2°C intervals from 36.3 to 34.9°C demonstrated substantial tradeoffs between sensitivity and specificity in detecting SBI and IBI at all cutoffs (Table 3).
Figure:
Receiver operator curve of temperature with outcomes of serious bacterial infection (SBI) and invasive bacterial infection (IBI). Points in the figure represent the optimally selected thresholds.
Table 3:
Diagnostic performance of serious bacterial infection (SBI) and invasive bacterial infection (IBI) identification in 0.2 °C bands. Numbers in parenthesis represent 95% confidence intervals
| Outcome: SBI | ||||||
|---|---|---|---|---|---|---|
| Sensitivity | Specificity | PPV | NPV | LR+ | LR− | |
| ≤36.3 °C | 83.9 (72.3–92.0) | 27.4 (25.9–29.0) | 2.1 (1.6–2.8) | 98.9 (98.0–99.5) | 1.2 (1.0–1.3) | 0.6 (0.3–1) |
| ≤36.1 °C | 51.6 (38.6–64.5) | 62.2 (60.5–63.9) | 2.5 (1.7–3.5) | 98.6 (98.0–99.0) | 1.4 (1.1–1.7) | 0.8 (0.6–1) |
| ≤35.9 °C | 30.6 (19.6–43.7) | 78.3 (76.8–79.7) | 2.6 (1.6–4.0) | 98.4 (97.8–98.8) | 1.4 (1.0–2.1) | 0.9 (0.8–1) |
| ≤35.7 °C | 22.6 (12.9–35.0) | 87.4 (86.2–88.5) | 3.2 (1.8–5.4) | 98.4 (97.8–98.8) | 1.8 (1.1–2.9) | 0.9 (0.8–1) |
| ≤35.5 °C | 21.0 (11.7–33.2) | 90.2 (89.1–91.2) | 3.8 (2.1–6.5) | 98.4 (97.9–98.8) | 2.1 (1.3–3.5) | 0.9 (0.8–1) |
| ≤35.3 °C | 12.9 (5.7–23.9) | 92.3 (91.3–93.2) | 3.0 (1.3–5.9) | 98.3 (97.7–98.7) | 1.7 (0.9–3.2) | 1.0 (0.9–1) |
| ≤35.1 °C | 9.7 (3.6–19.9) | 94.2 (93.4–95.0) | 3.0 (1.1–6.5) | 98.2 (97.7–98.7) | 1.7 (0.8–3.6) | 1.0 (0.9–1) |
| ≤34.9 °C | 9.7 (3.6–19.9) | 95.7 (94.9–96.3) | 4.0 (1.5–8.5) | 98.3 (97.8–98.7) | 2.2 (1.0–4.8) | 0.9 (0.9–1) |
| Outcome: IBI | ||||||
| ≤36.3 °C | 87.5 (61.7–98.4) | 27.3 (25.8–28.8) | 0.6 (0.3–1.0) | 99.8 (99.2–100.0) | 1.2 (1.0–1.4) | 0.5 (0.1–1.7) |
| ≤36.1 °C | 62.5 (35.4–84.8) | 62.1 (60.4–63.7) | 0.8 (0.4–1.4) | 99.7 (99.4–99.9) | 1.6 (1.1–2.4) | 0.6 (0.3–1.1) |
| ≤35.9 °C | 43.8 (19.8–70.1) | 78.2 (76.8–79.6) | 0.9 (0.4–1.9) | 99.7 (99.4–99.8) | 2.0 (1.1–3.5) | 0.7 (0.5–1.1) |
| ≤35.7 °C | 25.0 (7.3–52.4) | 87.3 (86.1–88.4) | 0.9 (0.3–2.4) | 99.6 (99.3–99.8) | 2.0 (0.8–4.6) | 0.9 (0.6–1.1) |
| ≤35.5 °C | 25.0 (7.3–52.4) | 90.0 (89.0–91.0) | 1.2 (0.3–3.0) | 99.6 (99.3–99.8) | 2.5 (1.1–5.9) | 0.8 (0.6–1.1) |
| ≤35.3 °C | 18.8 (4–45.6) | 92.2 (91.3–93.1) | 1.1 (0.2–3.3) | 99.6 (99.3–99.8) | 2.4 (0.9–6.7) | 0.9 (0.7–1.1) |
| ≤35.1 °C | 18.8 (4–45.6) | 94.2 (93.4–95.0) | 1.5 (0.3–4.4) | 99.6 (99.3–99.8) | 3.2 (1.2–9.1) | 0.9 (0.7–1.1) |
| ≤34.9 °C | 18.8 (4–45.6) | 95.6 (94.9–96.3) | 2.0 (0.4–5.7) | 99.6 (99.3–99.8) | 4.3 (1.5–12) | 0.8 (0.7–1.1) |
Abbreviations: SBI, serious bacterial infections; IBI, invasive bacterial infections; PPV, positive predictive value; NPV, negative predictive value; LR+, positive likelihood ratio; LR-, negative likelihood ratio
In a sensitivity analysis, both the AUROC and metrics of diagnostic accuracy were poorer when inclusion was limited to the subset of infants who had a blood culture performed. The AUROCs were 51.8% (95% CI 44.5–59.1%) and 47.6% (95% CI 32.3–62.9%) when using respective outcomes of SBI and IBI, respectively (Table 4).
Table 4:
Diagnostic performance of serious bacterial infection (SBI) and invasive bacterial infection (IBI) identification in 0.2 °C bands. Numbers in parenthesis represent 95% confidence intervals
| Infants with a blood culture obtained (n=967) | ||||||
|---|---|---|---|---|---|---|
| Outcome: SBI (AUROC 51.8; 95% CI 44.5–59.1%) | ||||||
| Sensitivity | Specificity | PPV | NPV | LR+ | LR− | |
| ≤36.3 °C | 87.7 (76.3–94.9) | 18.0 (15.5–20.7) | 6.5 (4.9–8.5) | 95.8 (91.5–98.3) | 1.1 (1.0–1.2) | 0.7 (0.3–1.4) |
| ≤36.1 °C | 54.4 (40.7–67.6) | 41.4 (38.1–44.7) | 5.7 (3.9–8.0) | 93.3 (90.4–95.6) | 0.9 (0.7–1.2) | 1.1 (0.8–1.5) |
| ≤35.9 °C | 33.3 (21.4–47.1) | 55.0 (51.6–58.3) | 4.6 (2.8–7.1) | 92.7 (90.1–94.8) | 0.7 (0.5–1.1) | 1.2 (1.0–1.5) |
| ≤35.7 °C | 24.6 (14.1–37.8) | 69.0 (65.8–72.0) | 4.9 (2.7–8.1) | 93.4 (91.2–95.2) | 0.8 (0.5–1.3) | 1.1 (0.9–1.3) |
| ≤35.5 °C | 22.8 (12.7–35.8) | 74.8 (71.8–77.6) | 5.6 (3.0–9.3) | 93.7 (91.7–95.4) | 0.9 (0.6–1.5) | 1.0 (0.9–1.2) |
| ≤35.3 °C | 14.0 (6.3–25.8) | 80.0 (77.2–82.6) | 4.4 (1.9–8.4) | 93.5 (91.5–95.1) | 0.7 (0.4–1.4) | 1.1 (1.0–1.2) |
| ≤35.1 °C | 10.5 (4.0–21.5) | 85.1 (82.5–87.4) | 4.4 (1.6–9.3) | 93.6 (91.7–95.2) | 0.7 (0.3–1.5) | 1.1 (1.0–1.2) |
| ≤34.9 °C | 10.5 (4.0–21.5) | 88.8 (86.6–90.8) | 5.8 (2.1–12.1) | 93.9 (92.0–95.4) | 0.9 (0.4–2.1) | 1.0 (0.9–1.1) |
| Outcome: IBI (AUROC 47.6; 95% CI 32.3–62.9%) | ||||||
| ≤36.3 °C | 87.5 (61.7–98.4) | 17.8 (15.3–20.4) | 1.8 (1.0–3.0) | 98.8 (95.7–99.9) | 1.1 (0.9–1.3) | 0.7 (0.2–2.6) |
| ≤36.1 °C | 62.5 (35.4–84.8) | 41.7 (38.5–45) | 1.8 (0.9–3.3) | 98.5 (96.7–99.4) | 1.1 (0.7–1.6) | 0.9 (0.5–1.7) |
| ≤35.9 °C | 43.8 (19.8–70.1) | 55.7 (52.4–58.9) | 1.7 (0.7–3.5) | 98.3 (96.7–99.2) | 1.0 (0.6–1.7) | 1.0 (0.7–1.6) |
| ≤35.7 °C | 25 (7.3–52.4) | 69.3 (66.2–72.3) | 1.4 (0.4–3.5) | 98.1 (96.8–99) | 0.8 (0.3–1.9) | 1.1 (0.8–1.4) |
| ≤35.5 °C | 25 (7.3–52.4) | 74.9 (72.0–77.7) | 1.7 (0.5–4.3) | 98.3 (97.0–99.1) | 1.0 (0.4–2.3) | 1.0 (0.8–1.3) |
| ≤35.3 °C | 18.8 (4.0–45.6) | 80.4 (77.7–82.9) | 1.6 (0.3–4.7) | 98.3 (97.1–99.1) | 1.0 (0.3–2.7) | 1.0 (0.8–1.3) |
| ≤35.1 °C | 18.8 (4.0–45.6) | 85.4 (83–87.6) | 2.2 (0.5–6.3) | 98.4 (97.2–99.1) | 1.3 (0.5–3.6) | 1.0 (0.8–1.2) |
| ≤34.9 °C | 18.8 (4.0–45.6) | 89.0 (86.8–90.9) | 2.9 (0.6–8.2) | 98.4 (97.3–99.2) | 1.7 (0.6–4.8) | 0.9 (0.7–1.2) |
Abbreviations: SBI, serious bacterial infections; IBI, invasive bacterial infections; AUROC, area under the receiver operating characteristic curves; PPV, positive predictive value; NPV, negative predictive value; LR+, positive likelihood ratio; LR-, negative likelihood ratio
Discussion:
Using a multicenter retrospective dataset, we attempted to identify a clinically meaningful definition of hypothermia for use in risk stratification of infants <90 days of age. While there was a significant difference in the temperatures of patients with SBI or IBI compared to those without these infections, the AUROC demonstrated poor discriminatory capability. Furthermore, no temperature cutoff for hypothermia resulted in satisfactory diagnostic accuracy for clinical use. While a low temperature may be associated with infections in young infants, further research is required to identify risk factors associated with SBI.
The lack of a clearly defined cutoff to identify SBI and IBI in this study of hypothermic infants presents a challenge in the use of a narrower temperature definition of hypothermia for the identification of these infections, which impacts clinicians’ decision to perform cultures or initiate empiric antimicrobial therapy. Only one-quarter of patients in our study had a blood culture confirmed. In this cohort, the diagnostic value of temperature to detect SBI was even lower. Furthermore, we found considerable proportions of patients without antibiotic treatment in cases of SBI and IBI, 35.5% and 37.5% respectively. These findings suggest that clinicians combine the presence of hypothermia with other clinical findings (such as age, prematurity, or ill appearance, which may each be independently associated with bacterial infections) to decide which infants require testing and treatment for suspected SBI. This is highlighted in a recent multicenter retrospective study that found high variability in the pediatric ED management of hypothermic infants, including blood tests in 74–95% and antibiotics administration in 56–92% of patients, further suggesting uncertainty in interpreting various clinical data in hypothermic infants [20].
One of the historical challenges in establishing an abnormal threshold for hypothermia is defining a lower end of normal temperature for infants. In published studies, there is a wide range of lower rectal temperatures for infants, from 35.9 to 36.6°C [21–24]. In a study of 691 well infants less than three months of age seen for routine visits, investigators found that rectal temperatures averaged 37.5 ± 0.3°C, varying particularly with age and season of presentation [24]. Other variables that affect body temperature include sleep [22, 25] and measurement site [26, 27]. Hence, a single temperature of ≤36.4°C may be insufficient to discriminate bacterial infections from other causes.
The proportion of infants identified with culture-confirmed SBI in this study (1.8%) is corroborated by previously published single-center studies, ranging from 1.6 to 2.9% [1–4]. Similar to epidemiologic trends identified in febrile infants over the past decade [7, 28] Escherichia coli, Enterococcus species, and Group B streptococcus were the most common pathogens in our cohort. Despite a considerable number of infants with UTI, few UTIs were associated with bacteremia, also comparable to previously published rates of bacteremia in febrile infants with UTI [22–23]. Our low proportion of infants who underwent sepsis evaluation (27%) is also consistent with data from other academic pediatric centers. Perry et al. reported that 25% of hypothermic infants underwent a sepsis evaluation [4]. Similarly, Kasmire et al. reported a 28.4% sepsis evaluation rate in hypothermic infants [1]. Understanding the prevalence and etiology of SBI among hypothermic infants can help direct future research into diagnostic evaluation, antimicrobial selection and resistance, and clinical outcomes.
Decades of research on febrile infants has culminated in a national guideline that stratifies SBI risk and management by age, with clear association of SBI with younger age in febrile infants [6]. The relationship between age and SBI in hypothermic infants remains unclear. In single centered retrospective studies, Wood et al. found 8/9 (89%) and Kasmire et al. found 2/3 (67%) of hypothermic infants with SBI were <14 days old [1,2]. Others have suggested SBI in hypothermic infants may be associated with older age [3, 4]. A multicenter retrospective study using administrative data from 40 hospitals over 10 years showed no statistically significant association between age and rates of SBI [5]. Further investigation is needed to determine an infant’s degree of hypothermia with age to the risk of SBI in multivariable risk prediction models.
A minority of hypothermic infants in our cohort had an associated ICD 9/10 code for hypothermia or a chief complaint of hypothermia. While ICD codes have previously been shown to effectively identify febrile infants and UTI [31, 32], their accuracy in identifying hypothermic infants has not been investigated. Our data suggest future investigations in this population should not rely on ICD codes for cohort identification. In addition, hypothermic infants may have coexisting medical conditions that cause temperature dysregulation or present with other concerning symptoms with hypothermia as a secondary finding. Single-center studies have suggested kidney disease, cardiomyopathy, hyperbilirubinemia, metabolic disorders, hypoglycemia, and prematurity as potential risk factors for hypothermia [1–4], with a retrospective multicenter administrative database study suggesting hypothermic infants with complex chronic conditions confer a higher risk of SBI and mortality [5].
Our findings are subject to limitations. This was a retrospective study that utilized data from the electronic medical record. Even though our cohort contains hypothermic infants from four tertiary pediatric hospitals, the number of cases with SBI and IBI remained low, resulting in wider confidence intervals. Future multicenter research should focus on including a sufficiently large sample size of infants to identify other risk factors in screening for SBI and improve the diagnostic accuracy of various temperature thresholds in conjunction with other historical, physical examination, and laboratory attributes. While we utilized well-established criteria from a national febrile infant study to identify pathologic organisms from cultures [17], culture positivity is dependent on sample volume and possibly sample collection timing in relation to the temperature abnormality [33]. We did not analyze patients with reported temperatures ≤36.4°C at home but with temperatures >36.4°C in the ED, which can potentially indicate underestimate the number of patients with hypothermia and overestimate the rates of SBI, as some infants may have only had reported hypothermia before hospital arrival. Because our study was comprised of patients from tertiary academic centers, our results may not be generalizable to children presenting to other settings. Despite these limitations, our study provides important data suggesting that the decision to perform testing or provide antimicrobial therapy to hypothermic young infants should not be performed based on a single temperature cutoff value.
Conclusion
Infants with SBI and IBI have lower minimum temperatures compared to hypothermic infants without these infections. However, our study could not establish a clear hypothermia temperature threshold with satisfactory diagnostic accuracy for SBI or IBI based solely on temperature. Other factors (such as history and/or clinical appearance) may be essential in identifying infants at risk of these infections. Our findings highlight the importance of a uniform definition to guide future research on this vulnerable population. Future studies should focus on detailed clinical and laboratory data to better risk stratify hypothermic infants.
What is already known on this topic
Data from mostly single centers have suggested that hypothermic infants presenting to the ED are at risk for serious or invasive bacterial infections. Interpretation of these data are challenging because of the varying temperatures used to define hypothermia. No study has evaluated a statistically derived temperature threshold to detect serious bacterial infections in hypothermic young infants.
What this study adds
In this cross-sectional study of hypothermic infants presenting to four academic pediatric EDs, we could not establish a clear temperature threshold with satisfactory diagnostic accuracy for serious or invasive bacterial infections based solely on a minimum rectal temperature in the ED. Additional research using clinical and laboratory data are needed to better risk stratify hypothermic infants.
Acknowledgements:
We thank Norma-Jean Simon, MS (Data Analytics and Reporting, Ann and Robert H. Lurie Children’s Hospital of Chicago), Chiu-Mei Chen, MS (University of Michigan), Elaine James, DNP, MSN, RN-BC (WakeMed Health and Hospitals), and Kelly Huynh, MStat (University of Utah) for assistance with data acquisition.
Funding source:
S.R. is sponsored by PEDSnet (Department of Pediatrics, Ann and Robert H Lurie Children’s Hospital). REDCap is supported at Feinberg School of Medicine by the Northwestern University Clinical and Translational Science (NUCATS) Institute. Research reported in this publication was supported, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences, Grant Number UL1TR001422. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. All authors have no financial relationships relevant to this article to disclose.
Abbreviations:
- ED
Emergency Department
- SBI
serious bacterial infections
- IBI
invasive bacterial infections
- UTI
urinary tract infections
- ICD
international classification of diseases
- WHO
World Health Organization
Footnotes
Conflict of Interest: The authors have no conflicts of interest to disclose.
References
- 1.Kasmire KE, Vega C, Bennett NJ, Laurich VM. Hypothermia: A Sign of Sepsis in Young Infants in the Emergency Department?. Pediatr Emerg Care. 2021;37(3):e124–e128. doi: 10.1097/PEC.0000000000001539 [DOI] [PubMed] [Google Scholar]
- 2.Wood JK, Halvorson EE, Auriemma JR, et al. Clinical Characteristics and Health Outcomes of Neonates Reporting to the Emergency Department With Hypothermia. Hosp Pediatr. 2018;8(8):458–464. doi: 10.1542/hpeds.2017-0176 [DOI] [PubMed] [Google Scholar]
- 3.Ramgopal S, Walker LW, Vitale MA, Nowalk AJ. Factors associated with serious bacterial infections in infants ≤60 days with hypothermia in the emergency department. Am J Emerg Med. 2019;37(6):1139–1143. doi: 10.1016/j.ajem.2019.04.015 [DOI] [PubMed] [Google Scholar]
- 4.Perry MC, Yaeger SK, Noorbakhsh K, Cruz AT, Hickey RW. Hypothermia in Young Infants: Frequency and Yield of Sepsis Workup. Pediatr Emerg Care. 2021;37(8):e449–e455. doi: 10.1097/PEC.0000000000001674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramgopal S, Noorbakhsh KA, Pruitt CM, Aronson PL, Alpern ER, Hickey RW. Outcomes of Young Infants with Hypothermia Evaluated in the Emergency Department. J Pediatr. 2020;221:132–137.e2. doi: 10.1016/j.jpeds.2020.03.002 [DOI] [PubMed] [Google Scholar]
- 6.Pantell RH, Roberts KB, Adams WG, et al. Evaluation and Management of Well-Appearing Febrile Infants 8 to 60 Days Old [published correction appears in Pediatrics. 2021 Oct 29;:]. Pediatrics. 2021;148(2):e2021052228. doi: 10.1542/peds.2021-052228 [DOI] [PubMed] [Google Scholar]
- 7.Powell EC, Mahajan PV, Roosevelt G, et al. Epidemiology of Bacteremia in Febrile Infants Aged 60 Days and Younger. Ann Emerg Med. 2018;71(2):211–216. doi: 10.1016/j.annemergmed.2017.07.488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Pediatric Fever, Mace SE, Gemme SR, et al. Clinical Policy for Well-Appearing Infants and Children Younger Than 2 Years of Age Presenting to the Emergency Department With Fever [published correction appears in Ann Emerg Med. 2017 Nov;70(5):758]. Ann Emerg Med. 2016;67(5):625–639.e13. doi: 10.1016/j.annemergmed.2016.01.042 [DOI] [PubMed] [Google Scholar]
- 9.Marik PE, Zaloga GP. Hypothermia and cytokines in septic shock. Norasept II Study Investigators. North American study of the safety and efficacy of murine monoclonal antibody to tumor necrosis factor for the treatment of septic shock. Intensive Care Med. 2000;26(6):716–721. doi: 10.1007/s001340051237 [DOI] [PubMed] [Google Scholar]
- 10.Arons MM, Wheeler AP, Bernard GR, et al. Effects of ibuprofen on the physiology and survival of hypothermic sepsis. Ibuprofen in Sepsis Study Group. Crit Care Med. 1999;27(4):699–707. doi: 10.1097/00003246-199904000-00020 [DOI] [PubMed] [Google Scholar]
- 11.Drewry AM, Fuller BM, Skrupky LP, Hotchkiss RS. The presence of hypothermia within 24 hours of sepsis diagnosis predicts persistent lymphopenia. Crit Care Med. 2015;43(6):1165–1169. doi: 10.1097/CCM.0000000000000940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Romanovsky AA, Almeida MC, Aronoff DM, et al. Fever and hypothermia in systemic inflammation: recent discoveries and revisions. Front Biosci. 2005;10:2193–2216. Published 2005 Sep 1. doi: 10.2741/1690 [DOI] [PubMed] [Google Scholar]
- 13.Garami A, Steiner AA, Romanovsky AA. Fever and hypothermia in systemic inflammation. Handb Clin Neurol. 2018;157:565–597. doi: 10.1016/B978-0-444-64074-1.00034-3 [DOI] [PubMed] [Google Scholar]
- 14.Thermal protection of the newborn: A practical guide. World Health Organization. https://apps.who.int/iris/handle/10665/63986. Published January 1, 1997. Accessed January 2, 2022. [Google Scholar]
- 15.Goldstein B, Giroir B, Randolph A. International Consensus Conference on Pediatric S. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6:2–8. [DOI] [PubMed] [Google Scholar]
- 16.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics, 42(2), 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mahajan P, Kuppermann N, Mejias A, Suarez N, Chaussabel D, Casper TC, et al. Association of RNA biosignatures with bacterial infections in febrile infants aged 60 days or younger. JAMA 2016;316:846. doi: 10.1001/jama.2016.9207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mahajan P, Kuppermann N, Suarez N, et al. RNA transcriptional biosignature analysis for identifying febrile infants with serious bacterial infections in the emergency department: a feasibility study. Pediatr Emerg Care. 2015;31(1):1–5. doi: 10.1097/PEC.0000000000000324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fever in infants less than 60 days. Clinical Pathway – Children’s Hospital Colorado. https://www.childrenscolorado.org/49e72a/globalassets/healthcare-professionals/clinical-pathways/fever-in-infants-less-than-60-days.pdf (accessed 23 Sep 2022).
- 20.Lo YHJ, Ramgopal S, Hashikawa AN, Cranford JA, Rogers AJ. Variability in emergency department management of hypothermic infants ≤90 days of age [published online ahead of print, 2022 Aug 3]. Am J Emerg Med. 2022;60:121–127. doi: 10.1016/j.ajem.2022.07.058 [DOI] [PubMed] [Google Scholar]
- 21.Herzog LW, Coyne LJ. What is fever? Normal temperature in infants less than 3 months old. Clin Pediatr (Phila). 1993;32(3):142–146. doi: 10.1177/000992289303200303 [DOI] [PubMed] [Google Scholar]
- 22.Wailoo MP, Petersen SA, Whittaker H, Goodenough P. Sleeping body temperatures in 3–4 month old infants. Arch Dis Child. 1989;64(4):596–599. doi: 10.1136/adc.64.4.596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anderson ES, Petersen SA, Wailoo MP. Factors influencing the body temperature of 3–4 month old infants at home during the day. Arch Dis Child. 1990;65(12):1308–1310. doi: 10.1136/adc.65.12.1308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morley CJ, Hewson PH, Thornton AJ, Cole TJ. Axillary and rectal temperature measurements in infants. Arch Dis Child. 1992;67(1):122–125. doi: 10.1136/adc.67.1.122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tappin DM, Ford RP, Nelson KP, et al. Breathing, sleep state, and rectal temperature oscillations. Arch Dis Child. 1996;74(5):427–431. doi: 10.1136/adc.74.5.427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilshaw R, Beckstrand R, Waid D, Schaalje GB. A comparison of the use of tympanic, axillary, and rectal thermometers in infants. J Pediatr Nurs. 1999;14(2):88–93. doi: 10.1016/S0882-5963(99)80042-6 [DOI] [PubMed] [Google Scholar]
- 27.Siberry GK, Diener-West M, Schappell E, Karron RA. Comparison of temple temperatures with rectal temperatures in children under two years of age. Clin Pediatr (Phila). 2002;41(6):405–414. doi: 10.1177/000992280204100605 [DOI] [PubMed] [Google Scholar]
- 28.Woll C, Neuman MI, Pruitt CM, et al. Epidemiology and Etiology of Invasive Bacterial Infection in Infants ≤60 Days Old Treated in Emergency Departments. J Pediatr. 2018;200:210–217.e1. doi: 10.1016/j.jpeds.2018.04.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bonadio W, Maida G. Urinary tract infection in outpatient febrile infants younger than 30 days of age: a 10-year evaluation. Pediatr Infect Dis J. 2014;33(4):342–344. doi: 10.1097/INF.0000000000000110 [DOI] [PubMed] [Google Scholar]
- 30.Tzimenatos L, Mahajan P, Dayan PS, et al. Accuracy of the Urinalysis for Urinary Tract Infections in Febrile Infants 60 Days and Younger. Pediatrics. 2018;141(2):e20173068. doi: 10.1542/peds.2017-3068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aronson PL, Williams DJ, Thurm C, et al. Accuracy of diagnosis codes to identify febrile young infants using administrative data. J Hosp Med. 2015;10:787–793. 10.1002/jhm.2441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tieder JS, Hall M, Auger KA, et al. Accuracy of administrative billing codes to detect urinary tract infection hospitalizations. Pediatrics. 2011;128:323–330. 10.1542/peds.2010-2064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Connell TG, Rele M, Cowley D, Buttery JP, Curtis N. How reliable is a negative blood culture result? Volume of blood submitted for culture in routine practice in a children’s hospital. Pediatrics. 2007;119(5):891–896. doi: 10.1542/peds.2006-0440 [DOI] [PubMed] [Google Scholar]