Abstract
Simple Summary
Lymph node involvement is a prognostic determinant in the diagnostic work-up and management of muscle-invasive bladder cancer. Thus, it is crucial to provide an accurate staging of the bladder tumor to better identify the best therapeutic strategies to improve the chances of survival and the quality of life of patients affected by bladder cancer. Positron Emission Tomography/Computed Tomography (PET/CT) has been increasingly used in bladder cancer staging to improve the accuracy of lymph node detection and to overcome the lack of sensitivity and the understaging showed by conventional imaging. The aim of this narrative literature review is to provide an overview of the current evidence on the use of 18F-FDG PET/CT in the diagnosis, staging, and restaging of bladder cancer, with a particular focus on its sensitivity and specificity for the detection of LN metastasis. We aim to provide clinicians with a better understanding of 18F-FDG PET/CT’s potential benefits and limitations in clinical practice. Despite the heterogeneity of the studies in the literature and the lack of a consensus, 18F-FDG PET/CT provides important incremental staging and restaging information that can potentially influence the clinical management of patients affected by muscle-invasive bladder cancer.
Abstract
Introduction: Lymph node (LN) involvement is a crucial determinant of prognosis for patients with bladder cancer, and an accurate staging is of utmost importance to better identify timely and appropriate therapeutic strategies. To improve the accuracy of LN detection, as an alternative to traditional methods such as CT or MRI, 18F-FDG PET/CT has been increasingly used. 18F-FDG PET/CT is also used in post-treatment restaging after neoadjuvant chemotherapy. The aim of this narrative literature review is to provide an overview of the current evidence on the use of 18F-FDG PET/CT in the diagnosis, staging, and restaging of bladder cancer, with a particular focus on its sensitivity and specificity for the detection of LN metastasis. We aim to provide clinicians with a better understanding of 18F-FDG PET/CT’s potential benefits and limitations in clinical practice. Materials and Methods: We designed a narrative review starting from a wide search in the PubMed/MEDLINE and Embase databases, selecting full-text English articles that have examined the sensibility and specificity of PET/CT for nodal staging or restaging after neoadjuvant therapy in patients with bladder cancer. The extracted data were analyzed and synthesized using a narrative synthesis approach. The results are presented in a tabular format, with a summary of the main findings of each study. Results: Twenty-three studies met the inclusion criteria: fourteen studies evaluated 18F-FDG PET/CT for nodal staging, six studies examined its accuracy for restaging after neoadjuvant therapy, and three studies evaluated both applications. To date, the use of F-18 FDG PET/TC for detection of LN metastasis in bladder cancer is controversial and uncertain: some studies showed low accuracy rates, but over the years other studies have reported evidence of high sensitivity and specificity. Conclusions: 18F-FDG PET/CT provides important incremental staging and restaging information that can potentially influence clinical management in MIBC patients. Standardization and development of a scoring system are necessary for its wider adoption. Well-designed randomized controlled trials in larger populations are necessary to provide consistent recommendations and consolidate the role of 18F-FDG PET/CT in the management of bladder cancer patients.
Keywords: bladder cancer, lymph node, FDG PET/CT, staging, restaging
1. Introduction
Bladder Cancer (BCa) is a widespread disease that is ranked as the 10th most commonly diagnosed form of cancer globally. It has a notable effect on the wellbeing and longevity of individuals affected, in particular in situations where the cancer has progressed into a muscle invasive disease [1].
In fact, even if 70% of bladder cancer is represented by non-muscle-invasive tumors, the remaining 30% of patients have muscle-invasive bladder cancer (MIBC) associated with a high risk of lymph node (LN) involvement and distant metastases [2,3].
The presence of LN involvement in patients with BC, which indicates that cancer has progressed beyond the organ, is a crucial determinant of prognosis, with significant implications for treatment response and overall survival. The prognosis in cases of node-positive disease depends on multiple factors, including the stage and extent of the disease, as well as the presence of other risk factors such as advanced age, performance status, and comorbidities [4]. As such, a comprehensive evaluation of these factors is necessary to determine the optimal course of treatment and improve outcomes in affected individuals [5]. The management of node positive bladder cancer may involve a combination of surgery, chemotherapy, and/or radiation therapy.
It is important for these patients to receive an accurate staging of the bladder tumor to better identify timely and appropriate therapeutic strategies to improve their chances of survival and their quality of life [6]. Before a radical cystectomy, preoperative locoregional staging is important to define the indication to neoadjuvant chemotherapy (NAC) to eradicate any micro-metastatic disease or eventually to guide the clinician towards an extended pelvic LN dissection to improve the chances of performing a curative surgery. It is crucial to identify patients with advanced metastatic disease and carefully evaluate the indication for a salvage radical cystectomy [7]. If the surgery is not curative but only palliative, doctors and patients must consider the impact of a urinary diversion on the patient’s quality of life. Therefore, it is essential to weigh the potential benefits and drawbacks of the surgery and engage in a shared decision-making process to ensure that the patient’s goals and preferences are taken into account [8,9].
In routine clinical practice, preoperative staging of muscle-invasive bladder cancer (MIBC) typically involves performing a computed tomography (CT) scan of the chest, abdomen, and pelvis. Pelvic Magnetic Resonance Imaging (MRI) can also be used, although not routinely in clinical practice. However, despite their accuracy in detecting primary bladder disease, both CT and MRI have not proven to have high sensitivity for nodal staging. With a sensitivity of 50–85% for the detection of pelvic LN involvement, both CT and MRI understage about 1/3 of patients. CT and MRI remain valuable tools in the preoperative staging of muscle-invasive bladder cancer and can provide useful information for guiding treatment decisions. To improve the accuracy of LN detection, other imaging modalities such as positron emission tomography (PET) or sentinel LN biopsy may be considered in selected cases [10].
To overcome this lack of sensitivity in identifying lymph node involvement, Positron Emission Tomography/Computed Tomography (PET/CT) has been increasingly used in bladder cancer staging.
PET/CT is a non-invasive imaging modality which has gained increasing popularity in the evaluation of patients with cancer and provides whole-body imaging, even if imaging of chest, abdomen, and pelvis might be enough for many cancers [5].
PET/CT combines the functional information supplied by PET with the anatomic detail of CT, providing comprehensive information about the metabolic and structural changes in the body.
In particular, 18 F-fluoro-2-deoxy-D-glucose (18F-FDG) PET/CT confers information based on glucose uptake and identifies cells with a high uptake such as neoplastic cells with their increased utilization of glucose.
Since metabolic alterations occur before the morphological ones, 18F-FDG PET/CT enables an early detection of locoregional disease, distant metastases, and cancer recurrence, before they become evident by conventional imaging like TC or MRI.
Another important topic about MIBC is the post-treatment restaging after neoadjuvant chemotherapy.
In fact, an early evaluation of NAC response and of presence of residual disease is important to guide the perioperative management of patients. For example, patients with advanced disease and persistent LN involvement even after NAC have poor prognosis, and a multidisciplinary team has to evaluate whether to proceed with a radical cystectomy, intended for palliative rather than curative purpose. Patients who are unresponsive to neoadjuvant chemotherapy (NAC), particularly those with localized disease (cT2-T4aN0M0), might see more benefits from an immediate radical cystectomy rather than continuing NAC, especially considering chemotherapy-related side-effects.
Methods traditionally used for post-treatment restaging, such as cystoscopy, urine cytology, routine blood tests, CT, and MRI scans, do not have high diagnostic accuracy, and there is no consensus recommendation regarding restaging imaging during NAC.
18F-FDG PET/CT is already used to monitor response to NAC in other types of cancers, while its use in bladder cancer restaging is relatively new and controversial.
The aim of this narrative literature review is to provide an overview of the current evidence on the use of 18F-FDG PET/CT in the diagnosis, staging, and restaging of bladder cancer, with a particular focus on its sensitivity and specificity for the detection of LN metastasis. By synthesizing the available evidence on the use of 18-FDG PET/CT in MIBC, we aim to provide clinicians with a better understanding of its potential benefits and limitations in clinical practice.
2. Materials and Methods
2.1. Literature Search Strategy
A comprehensive literature search was performed in the PubMed/MEDLINE and Embase databases to identify relevant studies regarding the use of 18F-FDG PET/CT in the diagnosis, staging, and restaging of Muscle-Invasive Bladder Cancer (MIBC). Two independent authors (VS and MB) conducted the search using various combinations of the following terms: “PET/CT”, “18F-FDG PET/CT”, “bladder”, “locally advanced”, “cancer”, “tumour”, “carcinoma”, “pelvic lymph node”, and “staging”. The search strategy aimed to minimize bias and ensure a thorough review of the existing literature.
To further enhance the literature search, the reference lists of included studies and relevant reviews were manually screened to identify any additional pertinent publications. Additionally, a search for unpublished studies and conference abstracts was carried out to minimize the risk of publication bias.
2.2. Study Selection and Inclusion Criteria
Two authors (VS and MB) independently screened the titles and abstracts of the identified articles for relevance, and any disagreements were resolved by a third author (AM). Full-text articles were retrieved for those that met the following inclusion criteria:
Studies that examined the sensitivity and specificity of PET/CT for nodal staging or restaging after neoadjuvant therapy in patients with bladder cancer.
Studies published in English with no temporal restrictions.
Studies conducted in humans.
Only English-language articles were considered eligible. Both prospective and retrospective clinical studies were included, such as cohort studies and case–control studies. Case reports, case series, and review articles were excluded from the review.
2.3. Quality Assessment of Included Studies
The methodological quality of the included studies was assessed independently by two reviewers (VS and MB) using appropriate quality assessment tools. For randomized controlled trials, the Cochrane Risk of Bias tool was employed, while the Newcastle–Ottawa Scale was used for cohort and case–control studies. Any discrepancies in quality assessment were resolved through discussion and consensus or, if necessary, by involving a third reviewer (AM).
2.4. Data Extraction and Analysis
The two reviewers independently extracted data from the included studies using a standardized form. The extracted data encompassed the following categories:
Study design.
Patient characteristics (age, gender, stage of disease, and histology).
PET/CT parameters (radiotracer used, diuretic use, and acquisition protocol).
Main findings of each study (sensitivity and specificity of PET/CT for nodal staging, Positive Predictive Value (PPV), Negative Predictive Value (NPV), and accuracy).
Any discrepancies in the extracted data were resolved through consensus. A narrative synthesis approach was employed for analyzing and synthesizing the extracted data. The results were presented in a tabular format, with a summary of the main findings of each study.
2.5. Synthesis of Results
The extracted data were synthesized using a narrative synthesis approach, taking into consideration the various factors that could influence the performance of 18F-FDG PET/CT in bladder cancer diagnosis, staging, and restaging. The results were presented in a tabular format, with a summary of the main findings of each study. Based on the findings of this narrative review and the identified gaps in the current literature, recommendations for future research were formulated.
3. Results
A total of twenty-three studies, published between 2005 and 2019, met the inclusion criteria for this literature review. Table 1 presents the characteristics of the included studies. Fourteen studies evaluated the sensitivity and specificity of 18F-FDG PET/CT for nodal staging, while six studies examined its accuracy for restaging after neoadjuvant therapy. Three studies evaluated both applications. All included studies reported the number of patients, with the range varying from a minimum of 15 to a maximum of 287 patients (Table 1). Gender distribution was reported in all studies except for one, with a male prevalence above 70% observed across the studies (Table 1).
Table 1.
Characteristics of the included studies (publication year, patient selection, number of patients, gender distribution, histology, timing of image uptake, use of furosemide, and timing of image acquisition following diuretic administration).
| Study | Year | Patient Selection (Detecting, Staging, Restaging) |
N. Patients | Gender Male (%) |
Histology | Image Time | Furosemide | Time after Furosemide Administration |
|---|---|---|---|---|---|---|---|---|
| Drieskens et al. [11] | 2005 | Staging | 55 | 47 (85.5%) |
TCC | 60 min | 20 mg | 10 min |
| Anjos et al. [12] | 2007 | Detecting, staging Restaging |
17 | 15 (88.2%) |
TCC | 60, 120 min | 20 mg | 60 min |
| Jadvar et al. [13] | 2008 | Restaging | 35 | 25 (71.4%) |
TCC | 60 min | - | - |
| Swinnen et al. [14] | 2009 | Staging | 51 | 43 (84.3%) |
TCC | 30 min | - | - |
| Kibel et al. [15] | 2009 | Staging, restaging | 43 | 32 (74.4%) |
TCC Adenocarcinoma Squamoso |
60 min | 20 mg | 20 min |
| Lodde et al. [16] | 2010 | Staging | 70 | 57 (81.4%) |
TCC Epidermoide Neuroendocrino |
75, 110 min | 10 mg | 30 min |
| Harkirat et al. [17] | 2010 | Staging, restaging | 29 | - | TCC | 60, 150, 190 min | dosage not specified | 60, 90 min |
| Apolo et al. [18] | 2010 | Detecting, restaging | 57 | 38 (66.7%) |
TCC, Adenocarcinoma Neuroendocrino Squamoso | 60, 90 min | - | - |
| Jenses et al. [19] | 2011 | Staging | 18 | 14 (77.8%) |
TCC | 60 min | - | - |
| Mertens et al. [20] | 2013 | Restaging | 19 | 18 (94.7%) |
- | 60 min | - | - |
| Hitier-Berthault et al. [21] | 2013 | Staging | 52 | 44 (84.6%) |
TCC Adenocarcinoma Squamoso |
60, 90 min | - | - |
| Goodfellow et al. [22] | 2013 | Staging | 233 | 175 (75.1%) |
TCC Adenocarcinoma Neuroendocrino Paraganglioma Squamoso |
90 min | - | - |
| Nayak et al. [23] | 2013 | Staging | 25 | 21 (84%) |
- | 45, 60 min | 40 mg | 120 min |
| Jeong et al. [24] | 2015 | Staging | 61 | 46 75.4% |
- | 60 min | - | - |
| Aljabery et al. [25] | 2015 | Staging | 54 | 47 (87%) |
TCC | 60, 90 min | - | - |
| Pichler et al. [26] | 2016 | Staging | 70 | 53 (75.7%) |
- | 60 min | - | - |
| Uttam et al. [27] | 2016 | Staging | 15 | 14 (93.3%) |
- | 60 min | 20 mg | 10–15 min |
| Soubra et al. [28] | 2016 | Staging | 78 | 64 (81.1%) |
- | 60 min | 40 mg | 60 min |
| Alongi et al. [28] | 2016 | Restaging | 41 | 36 (87.8%) |
TCC Papillare Squamoso |
60, 90 min | - | - |
| Kollberg et al. [29] | 2017 | Restaging | 50 | 35 (78%) |
- | - | 20 mg | - |
| Zattoni et al. [30] | 2017 | Restaging | 287 | 223 (77.7%) |
TCC | 60 min | - | - |
| Higashiyama et al. [31] | 2018 | Staging | 25 | 19 (76%) |
TCC Small cell carcinoma |
60, 120 min | - | - |
| Girard et al. [10] | 2019 | Staging | 61 | 56 (91.8%) |
- | 60 min | - | - |
Histology was reported in fifteen studies reported, of which eight studies presented only patients with Transitional Cell Carcinoma. Instead, seven studies included also patients with histological variants such as adenocarcinoma, squamous cell carcinoma, epidermoid, papillary, neuroendocrine, and paraganglioma (Table 1).
All included studies, except one, reported the timing of image uptake after the administration of 18F-FDG, with eighteen studies acquiring the first PET/CT images 60 min after administration. This standardized timing of image acquisition was assessed for ensuring consistency and accuracy in the interpretation of PET/CT results across studies. Two authors performed the first acquisition earlier, respectively, at 30 and 45 min; two authors posticipated the first acquisition, respectively, at 75 and 90 min.
Of the included studies, nine studies highlighted the use of furosemide as a diuretic, and eight studies specified the timing of PET/CT image acquisition following diuretic administration. In all the studies to evaluate the sensitivity and specificity of the technique, 18F-FDG PET/CT findings were compared to pathological reports; for distance metastases, moreover, it is necessary to also perform a comparison to follow-up imaging.
The distribution of studies reporting both staging classification by 18F-FDG PET/CT and pathological staging is presented in Table 2.
Table 2.
Clinical and pathological staging. AP (Anatomical Pathology), FU (Follow-up).
| Study | Year | Patient Selection (Detecting or Staging or Restaging) |
Reference Test | Clinical t Stage | Clinical n Stage | Pathological t Stage | Pathological n Stage |
|---|---|---|---|---|---|---|---|
| Drieskens et al. [11] | 2005 | Staging | AP or FU | - | - | pT0: 0% pT1: 16% pT2: 47% pT3: 31% pT4: 6%. |
- |
| Anjos et al. [12] | 2007 | Detecting Staging Restaging |
APor FU | cT+: 35% | cN+: 47% cM+: 35% |
pT+: 35% | pN0: 47% pM+: 35% |
| Jadvar et al. [13] | 2008 | Restaging | AP or FU | - | cN0: 34% cN+: 54% |
- | pN0: 54% pN-: 34% |
| Swinnen et al. [14] | 2009 | Staging | AP | - | cN0: 86% cN+: 14% |
pT0: 0% pT1: 24%; pT2: 43% pT3: 24%; pT4: 8%. |
pN0: 75% pN+: 25% |
| Kibel et al. [15] | 2009 | Staging Restaging |
AP | - | cN0: 79% cN+: 21% |
- | pN0: 75% pN+: 25% |
| Lodde et al. [16] | 2010 | Staging | AP or FU | - | cN0: 82% cN1: 4% cN2: 14% |
- | pN0: 3% pN1: 13% pN2: 12% pN3: 7% |
| Harkirat et al. [17] | 2010 | Staging Restaging |
AP or FU | cT0: 45% cT+: 55% |
cN+: 21% cM+: 7% |
; - |
pN+: 28% pM+: 14% |
| Apolo et al. [18] | 2010 | Detecting Restaging |
AP or FU | cT0-T1: 23% pT2-3-4: 77% |
- | pT0-T1: 12% pT2-T3: 44% pT4: 44% |
- |
| Jenses et al. [19] | 2011 | Staging | AP | - | cN0: 99% cN+: 11% |
- | pN0: 83% pN+: 17% |
| Mertens et al. [20] | 2013 | Restaging | AP | - | cN0: 63% | - | pN0: 74% |
| Hitier-Berthault et al. [21] | 2013 | Staging | AP | - | cN0: 77% cN+: 23% |
pT0: 10% pTis: 4% pT1: 6% pT2: 13% pT3: 36% pT4: 31% |
pN0: 58% pN+: 42% |
| Goodfellow et al. [22] | 2013 | Staging | AP or FU | - | cM0: 76% cM+: 24% |
pTa: 7% pTis: 3% pT1: 26% pT2: 35% pT3: 21%; pT4: 8% |
pN0: 88% pN+: 12% |
| Nayak et al. [23] | 2013 | Staging | AP | cT0: 4% cT+: 96% |
cN0: 72%; cN+: 28% |
pT0: 0% pT+:100%. |
pN0: 64% pN+: 36% |
| Jeong et al. [24] | 2015 | Staging | AP | - | cN0: 69%; cN+: 31% |
- | pN0: 72% pN+: 28% |
| Aljabery et al. [25] | 2015 | Staging | AP | cT0: 8% cT1:17% cT2: 19% cT3: 30% cT4: 26% |
cN0: 88%; cN+: 22% |
pT0: 0% pT1: 26% pT2: 18% pT3: 30% pT4: 26% |
pN0: 69% pN+: 31% |
| Pichler et al. [32] | 2016 | Staging | AP | - | cN0: 83% cN+: 17% |
pT0: 0% pTis: 3% pT1: 24% pT2: 35% pT3: 27% pT4: 11% |
pN0: 84% pN1: 7% pN2: 7% pN3: 2% |
| Uttam et al. [26] | 2016 | Staging | AP | - | cN0: 47%; cN+: 53% |
- | pN0: 80% pN+: 20% |
| Soubra et al. [27] | 2016 | Staging | AP (lynfh nodes and biopsy) |
- | cM0: 90% cM+: 10% |
pT0: 9% pTis: 14% pTa: 8% pT1: 8% pT2: 27% pT3: 19% pT4: 15% |
pM0: 90% pM+: 10% |
| Alongi et al. [28] | 2016 | Restaging | AP or FU | cT1: 15% cT2: 10% cT3: 10% cT4: 10% |
cN0: 49% cN+: 51% |
pT0: 0% pT1: 29% pT2: 23% pT3: 25% pT4: 23% |
pN0: 44% pN+: 56% |
| Kollberg et al. [29] | 2017 | Restaging | AP | cN0: 98% cN1: 2% |
pN0: 86% pN1:14% |
||
| Zattoni et al. [30] | 2017 | Restaging | FU | - | - | pT0: 5% pTis: 6% pTa: 2% pT1: 9% pT2: 14% pT3: 34% pT4: 14% NA: 16% |
pN0: 51% pN1: 12% pN2: 16% pN3: 4% pNx: 17 % |
| Higashiyama et al. [31] | 2018 | Staging | AP | cT0: 8% cT+: 92% |
- | pT0: 0% pT+: 100% |
- |
| Girard et al. [10] | 2019 | Staging | AP | - | cN0: 84%; cN+: 16% |
pT0: 0% pT1: 25%; pT2: 16% pT3-4: 59% |
pN0: 72% pN+: 28% |
Anatomical pathology was the reference test used in all but one of the studies included. Clinical T stage was reported in seven (30%) of the twenty-three studies while clinical node and metastasis were reported in nineteen (82%) of the studies reviewed.
The pathological N stage was evaluated in twenty (86%) of the twenty-three studies included with an expected good and promising concordance between the clinical and the pathological data.
It should be noted that not all included studies reported both types of staging classification, highlighting the variability in reporting practices across studies. Sensitivity of 18F-FDG PET/CT was reported in all the studies, but not all authors provided interquartile range. All the studies provided specificity of 18F-FDG PET/CT, except one.
Sensitivity, specificity, PPV, NPV, and accuracy of the studies included are summarized in Table 3. Sensitivity ranged between 33% (Jensen et al.) and 100% in six studies (26%). Specificity ranged between 17% (Kollberg et al.) and 100% in five (21%) of the studies included.
Table 3.
Sensitivity, PPV (Positive Predictive Value), NPV (Negative Predictive Value), Accuracy, and Specificity.
| Study | Year | Patient Selection (Detecting or Staging/Restaging) | Sensitivity (IQR) |
PPV | NPV | Accuracy | Specificity (IQR) |
|---|---|---|---|---|---|---|---|
| Drieskens et al. [11] | 2005 | Staging | 53% (27–79%) |
75% | 79% | 78% | 72% (0.51–0.88) |
| Anjos et al. [12] | 2007 | Detecting Staging Restaging |
100% (54–100%) |
100% (0.48–1.00) |
|||
| Jadvar et al. [13] | 2008 | Restaging | 100% (83–100%) |
100% (0.78–1.00) |
|||
| Swinnen et al. [14] | 2009 | Staging | 46% | 85% | 84% | 84% | 97% |
| Kibel et al. [15] | 2009 | Staging Restaging |
70% (35–93%) |
78% | 91% | 94% (0.79–0.99) |
|
| Lodde et al. [16] | 2010 | Staging | 57% (37–74%) |
100% | 80% | 77% | 100% |
| Harkirat et al. [17] | 2010 | Staging Restaging |
87% (60–98%) |
100% | 78% | 100% (0.59–1.00) |
|
| Apolo et al. [18] | 2010 | Detecting Restaging |
81% (63–93%) |
94% (0.70–1.00) |
|||
| Jenses et al. [19] | 2011 | Staging | 33% | 50% | 87% | 93% | 97% |
| Mertens et al. [20] | 2013 | Restaging | 100% | 94% | 100% | 67% | |
| Hitier-Berthault et al. [21] | 2013 | Staging | 36% | 67% | 65% | 65% | 87% |
| Goodfellow et al. [22] | 2013 | Staging | 69% | 87% | 81% | 86% | 95% |
| Nayak et al. [23] | 2013 | Staging | 100% | 100% | |||
| Jeong et al. [24] | 2015 | Staging | 47% | 73% | 82% | 93% | |
| Aljabery et al. [25] | 2015 | Staging | 41% | 58% | 76% | 86% | |
| Pichler et al. [26] | 2016 | Staging | 69% | 50% | 93% | 84% | 88% |
| Uttam et al. [27] | 2016 | Staging | 100% | 37% | 100% | 58% | |
| Soubra et al. [28] | 2016 | Staging | 56% | 90% | 98% | ||
| Alongi et al. [29] | 2016 | Restaging | 87% | 95% | 85% | 90% | 94% |
| Kollberg et al. [30] | 2017 | Restaging | 100% | 88% | 100% | 17% | |
| Zattoni et al. [31] | 2017 | Restaging | 95% | 95% | 78% | 91% | 78% |
| Higashiyama et al. [32] | 2018 | Staging | 92% | ||||
| Girard et al. [10] | 2019 | Staging | 47% | 80% | 82% | 82% | 95% |
The Positive Predictive Value (PPV) and Negative Predictive Value (NPV) were reported in seventeen (74%) of the twenty-three included studies, providing important information on the diagnostic accuracy of 18F-FDG PET/CT for bladder cancer. Additionally, thirteen (56%) of the twenty-three studies evaluated the accuracy of PET/CT through various parameters, such as different radiotracers, acquisition protocols, and patient characteristics. Sensitivity, specificity, PPV, NPV, and accuracy of the studies are summarized in Table 3.
4. Discussion
18F-FDG PET/CT has demonstrated promising results in detecting and staging various human cancers, as evidenced by previous studies [33]. However, the evidence regarding its use in bladder cancer is still a matter of debate. The use of 18F-FDG in primary bladder cancer detection is limited due to its high urinary excretion in the bladder and ureters which could be a confounding factor for detection of bladder wall lesions and metastatic regional LNS [34]. Identifying peri-vesical LN can be particularly challenging as they may be too small to be detected on CT or may be masked by adjacent 18F-FDG excretion in the urinary tract on PET/CT. The urinary excretion of 18F-FDG can lead to increased background activity in the pelvis, which can make it difficult to distinguish small LNs from surrounding urinary activity. As a result, accurate detection of peri-vesical LNs may require the use of more advanced imaging techniques, such as diffusion-weighted imaging (DWI) or dynamic contrast-enhanced MRI (DCE-MRI). Nonetheless, 18F-FDG PET/CT remains a valuable tool in identifying LN involvement and guiding treatment decisions in patients with bladder cancer.
Several measures may be employed to improve the accuracy of 18F-FDG PET/CT in bladder cancer imaging. These include oral pre-hydration to dilute the urinary tracer and the use of diuretics to enhance local regional accuracy in scans following furosemide administration. Bladder catheterization may also be effective in limiting 18F-FDG accumulation in the bladder and ureters, thereby improving the detection of bladder wall lesions and regional LNs. While these measures may improve the accuracy of 18F-FDG PET/CT in bladder cancer imaging, their routine use may not be practical or feasible in all patients, and their benefits should be weighed against potential risks and inconveniences [34,35]. To date, the use of F-18 FDG PET/TC for detection of LN metastasis in bladder cancer is controversial and uncertain: some studies showed low accuracy rates, but over the years other studies have reported evidence of high sensitivity and specificity [5,36].
Previous studies have suggested that the advantage of combined PET/CT over CT alone in detecting bladder cancer is minimal, likely due to the significant overlap between standardized uptake values (SUVs) of malignant lesions and active inflammatory processes. This overlap in SUVs can limit the specificity of 18F-FDG PET/CT in detecting bladder tumors and regional LNs, particularly in cases where there is significant inflammation or infection in the bladder or adjacent tissues.
While the combination of PET and CT imaging may still provide some additional information beyond what can be obtained with either modality alone, the limited advantage in diagnostic accuracy suggests that the routine use of combined PET/CT for bladder cancer imaging may not be justified in all cases.
A review of 2012 showed a sensitivity for combined PET-CT scan of 82% (95% CI: 0.72–0.89) [34].
Girard et al. in 2018 concluded that 18F-FDG PET/CT correctly detect LNs involvement in an additional 8% of patients compared to CT alone and that 18F-FDG PET/CT accuracy is 82% compared to 74% of CT alone [10]. Several studies have also shown that combined 18F-FDG PET/CT is superior for detection of distant metastases in bladder cancer [5,10]. The ability of PET to detect small metastases or LNs with high metabolic activity can increase the specificity of 18F-FDG PET/CT in detecting bladder cancer and regional metastasis [37].
According to Goodfellow et al., PET scans are considered useful if they result in a change in management for more than 10% of patients. In such cases, routine use of PET scans would be recommended. When PET scans lead to a change in management in 5–10% of patients, they should be used selectively for certain patients. However, if PET scans result in a change in management for less than 5% of patients, their routine use may not be justified. These recommendations highlight the need for careful consideration of the potential benefits and limitations of PET imaging, and the importance of individualized decision-making in the management of bladder cancer [22].
A recent review of 2022 on preoperative detection of pelvic LN involvement confirmed a higher sensitivity and specificity combining PET and CT scan when compared to the traditional imaging modalities [5]. A recent consensus statement by the European Association of Urology (EAU) and the European Society for Medical Oncology (ESMO) stated that 18F-FDG PET/CT should be included in oligometastatic disease staging to minimize the risk of overtreatment, when radical treatment options are being considered [37].
18F-FDG PET/CT has multiple applications beyond preclinical staging, including post-treatment restaging after neoadjuvant chemotherapy (NAC). Traditional modalities, such as cytology, cystoscopy, CT scans, MRIs, and routine blood tests, are often inaccurate in detecting residual disease or assessing treatment response. Early assessment of NAC response and/or residual disease is crucial for guiding perioperative management, limiting chemotherapy-related side effects and improving quality of life. 18F-FDG PET/CT is a reliable tool for monitoring response to chemotherapy in various cancer types and has been shown to be more accurate than conventional imaging. Recent studies have identified 18F-FDG PET/CT as an effective method for detecting both residual and recurrent disease, with superior accuracy in detecting post-treatment recurrence outside the urinary tract, primarily bone lesions, compared to conventional restaging techniques. Despite its potential benefits, there is currently no consensus on the use of 18F-FDG PET/CT for identifying chemo-sensitive bladder tumors during NAC. Nonetheless, the use of 18F-FDG PET/CT in post-treatment restaging may help to guide treatment decisions, such as whether to proceed with radical cystectomy or continue with NAC, based on the presence or absence of residual disease [5].
In addition to its potential role in bladder cancer staging, 18F-FDG PET/CT has applications in sentinel lymph node (SLN) mapping to aid in the resection of selected, invaded LNs during pelvic LND [38]. This approach can simplify histopathological examination and reduce the extent of LN dissection (LND) compared to blind template resection. Lymphoscintigraphy, CT, MRI, and fluoroscopy are commonly used methods for SLN mapping. SLN biopsy (SLNB) has been successfully used in breast and skin cancer treatment, contributing to a reduction in LND extent. Recent evidence suggests that 18F-FDG PET/CT combined with CT or MRI can be useful in evaluating LNs suspected to be involved based on CT/MRI findings, with a sensitivity of 92% and specificity of 91%. However, its sensitivity is considerably lower (7–23%) in patients with no suspicion of LN involvement on CT. Studies have shown that SLN mapping has a high detection rate and sensitivity in MIBC, particularly in patients with low pT stage bladder cancers and clinically negative LNs.
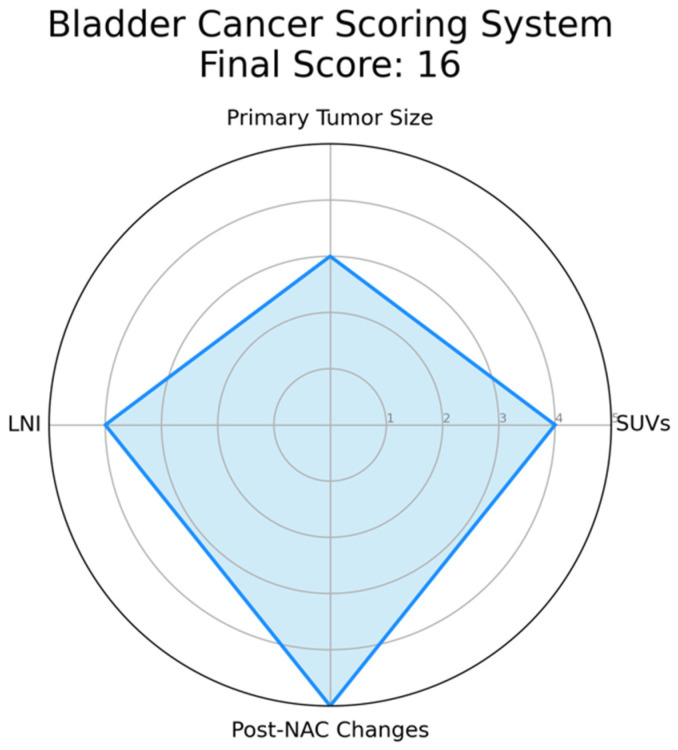
The complexity of bladder cancer staging using PET/CT prompts the need for a scoring system to improve its precision. This system should integrate key parameters like standardized uptake values (SUVs), indicative of tumor metabolic activity, and primary tumor size, which could correlate with disease progression. Lymph node involvement, particularly peri-vesical nodes, and the presence of distant metastases identified by PET/CT should also be incorporated due to their prognostic implications. Furthermore, changes in PET/CT findings post-neoadjuvant chemotherapy (NAC) could provide insights into tumor chemosensitivity and could thus influence the score. This score has been explained in detail in Figure 1.
Figure 1.
Example of a Radar Chart for the Proposed Bladder Cancer Scoring System. This chart represents an illustrative application of the proposed scoring system. Each axis corresponds to a parameter of the scoring system: standardized uptake values (SUVs), primary tumor size, lymph node involvement, and post-neoadjuvant chemotherapy (NAC) changes. The value along each axis represents the score for that parameter. SUVs is assigned as follows: 1 if SUV ≤ 2.5, indicating low metabolic activity and potentially less aggressive disease; 2 if 2.5 < SUV ≤ 5.0, suggesting moderate metabolic activity; 3 if 5.0 < SUV ≤ 7.5, suggesting relatively higher metabolic activity; 4 if 7.5 < SUV ≤ 10.0, indicative of high metabolic activity; 5 if SUV > 10.0, indicative of extremely high metabolic activity and potentially more aggressive disease. Primary tumor size is defined as follows: 1 if tumor size ≤ 2 cm, considered a small tumor; 2 if 2 cm < tumor size ≤ 4 cm, considered a moderately sized tumor; 3 if 4 cm < tumor size ≤ 6 cm, considered a relatively larger tumor, 4 if 6 cm < tumor size ≤ 8 cm, considered a large tumor, 5 if tumor size > 8 cm, considered a very large tumor, often associated with a worse prognosis. Lymph Node Involvement is defined as follows: 1 in case of no lymph nodes involved; 2 in case of single lymph node involvement; 3 in case of 2–3 lymph nodes involved, 4 in case of 4–6 lymph nodes involved, 5 in case of more than 6 lymph nodes involved, indicating extensive disease spread. Post-Neoadjuvant Chemotherapy (NAC) Changes are summarized as follows: 1 in case of no reduction in tumor size post-NAC, indicating no response; 2 in case of 1–25% reduction in tumor size post-NAC, suggesting a minimal response; 3 in case of 25–50% reduction in tumor size post-NAC, indicative of a partial response; 4 in case of 50–75% reduction in tumor size post-NAC, indicating a good response; 5 in case of more than 75% reduction or complete disappearance of the tumor post-NAC, indicating an excellent response. In this instance, hypothetical values are used for demonstration purposes: SUVs (4), Tumor Size (3), Lymph Node Involvement (4), and Post-NAC Changes (5). The filled area in the chart represents the composite score profile for a patient, providing a visual summary of the tumor’s characteristics according to the scoring system. Please note that in an actual case, values would be derived from clinical and imaging data, not randomly assigned.
The development of this scoring system calls for rigorous validation through future studies, correlating the score with patient outcomes in various settings and patient groups. Such a scoring system could reconcile PET/CT discrepancies and enhance its utility in bladder cancer assessment. However, ongoing research is essential to confirm the value of this proposed scoring system, as it presents a promising avenue to optimize PET/CT’s role in bladder cancer management.
Despite its potential benefits, 18F-FDG PET/CT has several limitations, including high cost, higher radiation exposure, lack of anatomic reference frame when performed alone, and prolonged lag time between PET and staging CT scans. A full-dose diagnostic staging CT with intravenous contrast medium may provide a better assessment of LNs and metastases than the CT component of the PET scan. False positive results can also lead to delay of treatment, unnecessary procedures, and additional costs. Therefore, PET scan results should be interpreted with caution in conjunction with CT scan and clinical judgment, particularly in cases of benign tumors or inflammatory lesions. Nonetheless, accurate staging information provided by 18F-FDG PET/CT can significantly influence therapeutic management and serve as an important prognostic indicator for progression-free survival (PFS) and overall survival (OS).
5. Conclusions and Future Directions
Although 18F-FDG PET/CT has shown promise as a feasible and reliable tool for bladder cancer staging, evidence for its use in diagnosis and staging is not yet strong. Like all radiological exams, 18F-FDG PET/CT is limited by the inability to retrieve a histological sample. Its non-invasive nature also makes it a potential tool for follow-up, but further studies are needed to evaluate its effectiveness in this setting. A standardized reporting system for characterizing bladder cancer using 18F-FDG PET/CT is still lacking, and efforts should be aimed at developing and validating a scoring system to improve its accuracy in staging. Despite these limitations, 18F-FDG PET/CT remains a valuable tool in the management of bladder cancer and can provide important information for treatment planning and prognostication.
In conclusion, 18F-FDG PET/CT provides important incremental staging information that can potentially influence clinical management in MIBC patients, although it can also lead to false positive results. However, supporting clinical evidence for its use is limited and requires further confirmation. Standardization of this approach and development of a scoring system are necessary for its wider adoption. In addition, 18F-FDG PET/CT has potential applications in sentinel LN mapping, which can guide the resection of selected and suspicious LNs during pelvic lymph node dissection. Sentinel LN biopsy is commonly used in breast and skin cancer treatment and can simplify histopathological examination and reduce the extent of LND.
Author Contributions
M.B.: Methodology, Resources, Formal analysis, Investigation, Data curation, and Writing original draft; V.S.: Resources Formal analysis, Investigation, Data curation, Formal analysis, and Writing original draft; E.M.: Resources and Data curation; R.M.: Resources and Data curation; A.S.: Resources and Data curation; A.C.: Resources and Data curation; F.D.M.: Methodology, Data curation, and Formal analysis; B.P.: Methodology and Data curation; L.S.M.: Methodology and Data curation; M.L.: Methodology and Data curation; W.K.: Methodology and Data curation; F.D.G.: Methodology and Data curation; D.D.: Methodology and Data curation; E.L.: Methodology and Data curation; S.F.S.: Conceptualization; A.M. (Andrea Minervini): Conceptualization and Project administration; M.M.: Conceptualization, Methodology, Supervision, and Project administration; A.M. (Andrea Mari): Conceptualization, Methodology, Formal analysis, Writing—review and editing, Supervision, and Project administration. On behalf of European Association of Urology-Young Academic Urologists (EAU-YAU): Urothelial Carcinoma Working Group. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Chang S.S., Bochner B.H., Chou R., Dreicer R., Kamat A.M., Lerner S.P., Lotan Y., Meeks J.J., Michalski J.M., Morgan T.M., et al. Treatment of Non-Metastatic Muscle-Invasive Bladder Cancer: AUA/ASCO/ASTRO/SUO Guideline. J. Urol. 2017;198:552–559. doi: 10.1016/j.juro.2017.04.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Josephson D., Pasin E., Stein J.P. Superficial bladder cancer: Part 2. Management. Expert Rev. Anticancer Ther. 2007;7:567–581. doi: 10.1586/14737140.7.4.567. [DOI] [PubMed] [Google Scholar]
- 3.Rieken M., Shariat S.F., Kluth L., Crivelli J.J., Abufaraj M., Foerster B., Mari A., Ilijazi D., Karakiewicz P.I., Babjuk M., et al. Comparison of the EORTC tables and the EAU categories for risk stratification of patients with nonmuscle-invasive bladder cancer. Urol. Oncol. Semin. Orig. Investig. 2018;36:8. doi: 10.1016/j.urolonc.2017.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mari A., Kimura S., Foerster B., Abufaraj M., D’Andrea D., Gust K.M., Shariat S.F. A systematic review and meta-analysis of lymphovascular invasion in patients treated with radical cystectomy for bladder cancer. Urol. Oncol. Semin. Orig. Investig. 2018;36:293–305. doi: 10.1016/j.urolonc.2018.03.018. [DOI] [PubMed] [Google Scholar]
- 5.Omorphos N.P., Ghose A., Hayes J.D., Kandala A., Dasgupta P., Sharma A., Vasdev N. The increasing indications of FDG-PET/CT in the staging and management of Invasive Bladder Cancer. Urol. Oncol. Semin. Orig. Investig. 2022;40:434–441. doi: 10.1016/j.urolonc.2022.05.017. [DOI] [PubMed] [Google Scholar]
- 6.Mari A., D’andrea D., Abufaraj M., Foerster B., Kimura S., Shariat S.F. Genetic determinants for chemo- and radiotherapy resistance in bladder cancer. Transl. Androl. Urol. 2017;6:1081–1089. doi: 10.21037/tau.2017.08.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.González-Del-Alba A., Conde-Moreno A.J., Vicente A.M.G., González-Peramato P., Linares-Espinós E., Climent M.Á. Management of Patients with Metastatic Bladder Cancer in the Real-World Setting from the Multidisciplinary Team: Current Opinion of the SOGUG Multidisciplinary Working Group. Cancers. 2022;14:1130. doi: 10.3390/cancers14051130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cacciamani G.E., Ghodoussipour S., Mari A., Gill K.S., Desai M., Artibani W., Shariat S.F., Djaladat H. Association between Smoking Exposure, Neoadjuvant Chemotherapy Response and Survival Outcomes following Radical Cystectomy: Systematic Review and Meta-Analysis. J. Urol. 2020;204:649–660. doi: 10.1097/JU.0000000000000813. [DOI] [PubMed] [Google Scholar]
- 9.Siles M.G., López-Beltran A., Pelechano P., Vicente A.M.G., Sarrió R.G., Peña E.G.-H., Antolín A.R., Zapatero A., Arranz J., Climent M. Advances in Transversal Topics Applicable to the Care of Bladder Cancer Patients in the Real-World Setting. Cancers. 2022;14:3968. doi: 10.3390/cancers14163968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Girard A., Rouanne M., Taconet S., Radulescu C., Neuzillet Y., Girma A., Beaufrere A., Lebret T., Le Stanc E., Grellier J.-F. Integrated analysis of 18F-FDG PET/CT improves preoperative lymph node staging for patients with invasive bladder cancer. Eur. Radiol. 2019;29:4286–4293. doi: 10.1007/s00330-018-5959-0. [DOI] [PubMed] [Google Scholar]
- 11.Drieskens O., Oyen R., Van Poppel H., Vankan Y., Flamen P., Mortelmans L. FDG-PET for preoperative staging of bladder cancer. Eur. J. Nucl. Med. Mol. Imaging. 2005;32:1412–1417. doi: 10.1007/s00259-005-1886-9. [DOI] [PubMed] [Google Scholar]
- 12.Dos Anjos D.A., Etchebehere E., Ramos C.D., Santos A., Albertotti C., Camargo E.E. 18F-FDG PET/CT Delayed Images After Diuretic for Restaging Invasive Bladder Cancer. J. Nucl. Med. 2007;48:764–770. doi: 10.2967/jnumed.106.036350. [DOI] [PubMed] [Google Scholar]
- 13.Jadvar H., Quan V., Henderson R.W., Conti P.S. [F-18]-Fluorodeoxyglucose PET and PET-CT in diagnostic imaging evaluation of locally recurrent and metastatic bladder transitional cell carcinoma. Int. J. Clin. Oncol. 2008;13:42–47. doi: 10.1007/s10147-007-0720-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Swinnen G., Maes A., Pottel H., Vanneste A., Billiet I., Lesage K., Werbrouck P. FDG-PET/CT for the Preoperative Lymph Node Staging of Invasive Bladder Cancer. Eur. Urol. 2010;57:641–647. doi: 10.1016/j.eururo.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 15.Kibel A.S., Dehdashti F., Katz M.D., Klim A.P., Grubb R.L., Humphrey P.A., Siegel C., Cao D., Gao F., Siegel B.A. Prospective Study of [18F]Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography for Staging of Muscle-Invasive Bladder Carcinoma. J. Clin. Oncol. 2009;27:4314–4320. doi: 10.1200/JCO.2008.20.6722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lodde M., Lacombe L., Friede J., Morin F., Saourine A., Fradet Y. Evaluation of fluorodeoxyglucose positron-emission tomography with computed tomography for staging of urothelial carcinoma. BJU Int. 2010;106:658–663. doi: 10.1111/j.1464-410X.2010.09212.x. [DOI] [PubMed] [Google Scholar]
- 17.Harkirat S., Anand S., Jacob M. Forced diuresis and dual-phase 18F-fluorodeoxyglucose-PET/CT scan for restaging of urinary bladder cancers. Indian J. Radiol. Imaging. 2010;20:13–19. doi: 10.4103/0971-3026.59746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Apolo A.B., Riches J., Schöder H., Akin O., Trout A., Milowsky M.I., Bajorin D.F. Clinical Value of Fluorine-18 2-Fluoro-2-Deoxy-D-Glucose Positron Emission Tomography/Computed Tomography in Bladder Cancer. J. Clin. Oncol. 2010;28:3973–3978. doi: 10.1200/JCO.2010.28.7052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jensen T.K., Holt P., Gerke O., Riehmann M., Svolgaard B., Marcussen N., Bouchelouche K. Preoperative lymph-node staging of invasive urothelial bladder cancer with 18F-fluorodeoxyglucose positron emission tomography/computed axial tomography and magnetic resonance imaging: Correlation with histopathology. Scand. J. Urol. Nephrol. 2011;45:122–128. doi: 10.3109/00365599.2010.544672. [DOI] [PubMed] [Google Scholar]
- 20.Mertens L.S., Fioole-Bruining A., Van Rhijn B.W., Kerst J.M., Bergman A.M., Vogel W.V., Vegt E., Horenblas S. FDG-Positron Emission Tomography/Computerized Tomography for Monitoring the Response of Pelvic Lymph Node Metastasis to Neoadjuvant Chemotherapy for Bladder Cancer. J. Urol. 2013;189:1687–1691. doi: 10.1016/j.juro.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 21.Hitier-Berthault M., Ansquer C., Branchereau J., Renaudin K., Bodere F., Bouchot O., Rigaud J. 18F-fluorodeoxyglucose positron emission tomography-computed tomography for preoperative lymph node staging in patients undergoing radical cystectomy for bladder cancer: A prospective study. Int. J. Urol. 2013;20:788–796. doi: 10.1111/iju.12045. [DOI] [PubMed] [Google Scholar]
- 22.Goodfellow H., Viney Z., Hughes P., Rankin S., Rottenberg G., Hughes S., Evison F., Dasgupta P., O’Brien T., Khan M.S. Role of fluorodeoxyglucose positron emission tomography (FDG PET)-computed tomography (CT) in the staging of bladder cancer. BJU Int. 2014;114:389–395. doi: 10.1111/bju.12608. [DOI] [PubMed] [Google Scholar]
- 23.Nayak B., Dogra P.N., Naswa N., Kumar R. Diuretic 18F-FDG PET/CT imaging for detection and locoregional staging of urinary bladder cancer: Prospective evaluation of a novel technique. Eur. J. Nucl. Med. Mol. Imaging. 2013;40:386–393. doi: 10.1007/s00259-012-2294-6. [DOI] [PubMed] [Google Scholar]
- 24.Jeong I.G., Hong S., You D., Hong J.H., Ahn H., Kim C.-S. FDG PET–CT for Lymph Node Staging of Bladder Cancer: A Prospective Study of Patients with Extended Pelvic Lymphadenectomy. Ann. Surg. Oncol. 2015;22:3150–3156. doi: 10.1245/s10434-015-4369-7. [DOI] [PubMed] [Google Scholar]
- 25.Aljabery F., Lindblom G., Skoog S., Shabo I., Olsson H., Rosell J., Jahnson S. PET/CT versus conventional CT for detection of lymph node metastases in patients with locally advanced bladder cancer. BMC Urol. 2015;15:87. doi: 10.1186/s12894-015-0080-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pichler R., De Zordo T., Fritz J., Kroiss A., Aigner F., Heidegger I., Virgolini I., Horninger W., Uprimny C. Pelvic Lymph Node Staging by Combined 18 F-FDG-PET/CT Imaging in Bladder Cancer Prior to Radical Cystectomy. Clin. Genitourin. Cancer. 2017;15:e387–e395. doi: 10.1016/j.clgc.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 27.Mete U.K., Nayak P., Bhattacharya A., Kakkar N., Mandal A. Is [F-18]-fluorodeoxyglucose FDG-PET/CT better than ct alone for the preoperative lymph node staging of muscle invasive bladder cancer? Int. braz j urol. 2016;42:234–241. doi: 10.1590/s1677-5538.ibju.2014.0579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Soubra A., Hayward D., Dahm P., Goldfarb R., Froehlich J., Jha G., Konety B.R. The diagnostic accuracy of 18F-fluorodeoxyglucose positron emission tomography and computed tomography in staging bladder cancer: A single-institution study and a systematic review with meta-analysis. World J. Urol. 2016;34:1229–1237. doi: 10.1007/s00345-016-1772-z. [DOI] [PubMed] [Google Scholar]
- 29.Alongi P., Caobelli F., Gentile R., Stefano A., Russo G., Albano D., Baldari S., Gilardi M.C., Midiri M. Recurrent bladder carcinoma: Clinical and prognostic role of 18 F-FDG PET/CT. Eur. J. Nucl. Med. Mol. Imaging. 2017;44:224–233. doi: 10.1007/s00259-016-3500-8. [DOI] [PubMed] [Google Scholar]
- 30.Kollberg P., Almquist H., Bläckberg M., Cwikiel M., Gudjonsson S., Lyttkens K., Patschan O., Liedberg F. [18F]Fluorodeoxyglucose-positron emission tomography/computed tomography response evaluation can predict histological response at surgery after induction chemotherapy for oligometastatic bladder cancer. Scand. J. Urol. 2017;51:308–313. doi: 10.1080/21681805.2017.1321579. [DOI] [PubMed] [Google Scholar]
- 31.Zattoni F., Incerti E., Colicchia M., Castellucci P., Panareo S., Picchio M., Fallanca F., Briganti A., Moschini M., Gallina A., et al. Comparison between the diagnostic accuracies of 18F-fluorodeoxyglucose positron emission tomography/computed tomography and conventional imaging in recurrent urothelial carcinomas: A retrospective, multicenter study. Abdom. Radiol. 2018;43:2391–2399. doi: 10.1007/s00261-017-1443-6. [DOI] [PubMed] [Google Scholar]
- 32.Higashiyama A., Komori T., Juri H., Inada Y., Azuma H., Narumi Y. Detectability of residual invasive bladder cancer in delayed 18F-FDG PET imaging with oral hydration using 500 mL of water and voiding-refilling. Ann. Nucl. Med. 2018;32:561–567. doi: 10.1007/s12149-018-1280-x. [DOI] [PubMed] [Google Scholar]
- 33.Antoch G., Saoudi N., Kuehl H., Dahmen G., Mueller S.P., Beyer T., Bockisch A., Debatin J.F., Freudenberg L.S. Accuracy of Whole-Body Dual-Modality Fluorine-18–2-Fluoro-2-Deoxy-d-Glucose Positron Emission Tomography and Computed Tomography (FDG-PET/CT) for Tumor Staging in Solid Tumors: Comparison With CT and PET. J. Clin. Oncol. 2004;22:4357–4368. doi: 10.1200/JCO.2004.08.120. [DOI] [PubMed] [Google Scholar]
- 34.Lu Y.-Y., Chen J.-H., Liang J.-A., Wang H.-Y., Lin C.-C., Lin W.-Y., Kao C.-H. Clinical value of FDG PET or PET/CT in urinary bladder cancer: A systemic review and meta-analysis. Eur. J. Radiol. 2012;81:2411–2416. doi: 10.1016/j.ejrad.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 35.Civelek A.C., Niglio S.A., Malayeri A.A., Lin J., Gurram S., Chalfin H.J., Turkbey B., Valera V., Steinberg S.M., Apolo A.B. Clinical value of 18FDG PET/MRI in muscle-invasive, locally advanced, and metastatic bladder cancer. Urol. Oncol. Semin. Orig. Investig. 2021;39:787. doi: 10.1016/j.urolonc.2021.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zattoni F., Incerti E., Moro F.D., Moschini M., Castellucci P., Panareo S., Picchio M., Fallanca F., Briganti A., Gallina A., et al. 18F-FDG PET/CT and Urothelial Carcinoma: Impact on Management and Prognosis—A Multicenter Retrospective Study. Cancers. 2019;11:700. doi: 10.3390/cancers11050700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Voskuilen C.S., van Gennep E.J., Einerhand S.M., Vegt E., Donswijk M.L., Bruining A., van der Poel H.G., Horenblas S., Hendricksen K., van Rhijn B.W., et al. Staging 18F-fluorodeoxyglucose Positron Emission Tomography/Computed Tomography Changes Treatment Recommendation in Invasive Bladder Cancer. Eur. Urol. Oncol. 2022;5:366–369. doi: 10.1016/j.euo.2021.01.005. [DOI] [PubMed] [Google Scholar]
- 38.Sinha A., West A., Hayes J., Teoh J., Decaestecker K., Vasdev N. Methods of Sentinel Lymph Node Detection and Management in Urinary Bladder Cancer—A Narrative Review. Curr. Oncol. 2022;29:1335–1348. doi: 10.3390/curroncol29030114. [DOI] [PMC free article] [PubMed] [Google Scholar]