Abstract
Introduction
Children with bone and joint infections are traditionally treated with intravenous antibiotics for 3–10 days, followed by oral antibiotics. Oral-only treatment has not been tested in randomised trials.
Methods and analysis
Children (3 months to 18 years) will be randomised 1:1 with the experimental group receiving high-dose oral antibiotics and the control group receiving intravenous antibiotics with a shift in both groups to standard oral antibiotics after clinical and paraclinical improvement. Children in need of acute surgery or systemic features requiring intravenous therapy, including septic shock, are excluded. The primary outcome is defined as a normal blinded standardised clinical assessment 6 months after end of treatment. Secondary outcomes are non-acute treatment failure and recurrent infection. Outcomes will be compared by a non-inferiority assumption with an inferiority margin of 5%.
Ethics and dissemination
The trial has the potential to reduce unnecessary hospitalisation and use of intravenous antibiotics in children with bone or joint infections. Due to the close follow-up, exclusion of severely ill children and predefined criteria for discontinuation of the allocated therapy, we expect the risk of treatment failure to be minimal.
Trial registration number
Keywords: paediatric infectious disease & immunisation, clinical trial, oral medicine, patient-centered care
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The prospective randomised design with blinded evaluation of the primary outcome will reduce potential bias.
The primary outcome, sequelae at 6 months, is of clear clinical relevance.
The pragmatic design with full integration into daily clinical practice ensures a high transferability of the generated data.
The 12-month follow-up reduces the risk of missing long-term sequelae.
The pragmatic criteria of inclusion involve a risk of including children with non-bacterial bone or joint disease.
Introduction
In recent years, the necessity of intravenous antibiotic treatment of children and adults with severe bacterial infections has been questioned as the evidence hereof is lacking.1 Oral-only treatment has been demonstrated to be safe and non-inferior to intravenous treatment for children with, for example, severe pneumonia2 and febrile urinary tract infections3 including urinary tract infections with bacteraemia.4 In large prospective randomised trials, early shift from intravenous to oral antibiotic treatment and even oral-only antibiotic treatment has been demonstrated to be safe and non-inferior to longer courses of intravenous treatment for adults with infectious diseases such as endocarditis5 6 and bone and joint infection (BJI).1 7 Several oral antibiotics have demonstrated good bone and joint penetration profiles compared with their respective plasma concentrations.8
Prospective studies on children with BJI have demonstrated that individualised antibiotic therapy with significantly reduced treatment duration is non-inferior to the previous long-term treatment9–12 and that only 2–4 days of intravenous therapy followed by 1–3 weeks of oral therapy is sufficient in most cases. The recommendations of individualised and shorter treatment have been adopted in Denmark with good results.13 These significant changes in treatment strategies raise the question of whether most children with BJI could be treated with oral antibiotics only. One small case series14 and one retrospective case–control study15 found oral-only therapy as a valid alternative to the current standard treatment, but the issue has not been investigated in randomised controlled trials (RCTs).
Methods and analysis
Study hypothesis and design
We hypothesise that oral-only antibiotic therapy is non-inferior (non-inferior margin 5%) to initial intravenous therapy, followed by oral therapy in children and adolescents with BJI and test that hypothesis in a nationwide, multicentre, randomised, controlled, open-label, non-inferiority trial.
Included children will be randomised 1:1 with the experimental group receiving high-dose oral antibiotic therapy and the control group receiving intravenous antibiotic therapy with a shift in both groups to standard oral therapy after clinical and paraclinical improvement.
Trial participants
Children and adolescents are considered for inclusion when they present with suspicion of BJI. Recruitment will be nationwide from all 18 paediatric departments in Denmark. Request a complete list of study sites and primary investigators at allan.bybeck.nielsen@regionh.dk.
Criteria of inclusion are listed in box 1.
Box 1. Criteria of inclusion and exclusion.
Inclusion criteria
The participant must meet both of the following criteria:
Age: 3 months to 18 years at study entry.
Antibiotic treatment of uncomplicated bone or joint infection.
Exclusion criteria
Any of the following criteria exclude the participant from the study:
Severe disease at admission, for example, septic shock, or any concomitant invasive infection, for example, necrotising fasciitis, requiring intravenous antibiotics in the opinion of the treating clinician.
Complicated bone or joint infection, for example, prosthetic material, infection secondary to or complicated by trauma, severe pyomyositis or other substantial soft tissue infections.
Expected need of major surgery within the first 24 hours of treatment, for example, drilling, debridement, fenestration, surgical drainage, synovectomy. Minor surgery as diagnostic surgical bone biopsy or diagnostic joint fluid aspiration including lavage is not a criterion for exclusion.
Significant comorbidities that might influence the choice of treatment or the course of the infection, for example, immunodeficiency or sickle cell anaemia.
Previous bone or joint infection.
Antibiotic therapy for more than 24 hours before inclusion.
Documented pathogen with limited treatment options that do not permit randomisation, for example, the pathogen is only sensitive to intravenous antibiotics.
Prior enrolment in the trial.
Delayed inclusion
Most patients will be included in the study before the start of treatment. If inclusion is not performed before administration of antibiotic therapy (eg, the treating physician is not aware of the project), up to 24 hours of antibiotic treatment will be accepted before inclusion in the study to achieve adequate participant enrolment.
Early termination of falsely included patients
To reflect the daily clinical setting and facilitate timely entry to the study, the patients are eligible for entry based on the available clinical information, often before the final diagnosis is made. In most cases, the clinical suspicion of infection is sustained (eg, by positive microbiology or imaging), and the study treatment is completed with or without further evidence of infection. If the suspicion of infection is abandoned during the study period, it will lead to early termination from the study according to the following criteria:
The suspicion of infection is abandoned, and antibiotic therapy is stopped prematurely.
-
The course of the disease is explained by another diagnosis (not BJI) that is made during treatment or follow-up. Examples:
Imaging reveals another diagnosis, for example, bone tumour, Legg-Calve-Perthes disease, or soft tissue infection with no involvement of bone or joint structures.
Recurrent symptoms with no confirmation of infection leads to another final diagnosis, such as juvenile idiopathic arthritis, chronic recurrent multifocal osteomyelitis or other non-infectious diseases.
Lyme arthritis is suspected, and the antibiotic treatment is changed targeting Borrelia burgdorferi.
Early terminated patients without BJI will not continue follow-up in the trial. They will be included in the analysis of the safety outcomes, but not in the analysis of any other outcomes. For transparency, details on all early terminated patients will be reported.
Minimising bias
Staff and participants are not blinded to the treatment allocation, since we consider intravenous placebo treatment to be unethical in this group of children and adolescents. To minimise bias, the evaluation of the primary outcome is blinded.
Diagnostic procedures and procedures during antibiotic treatment
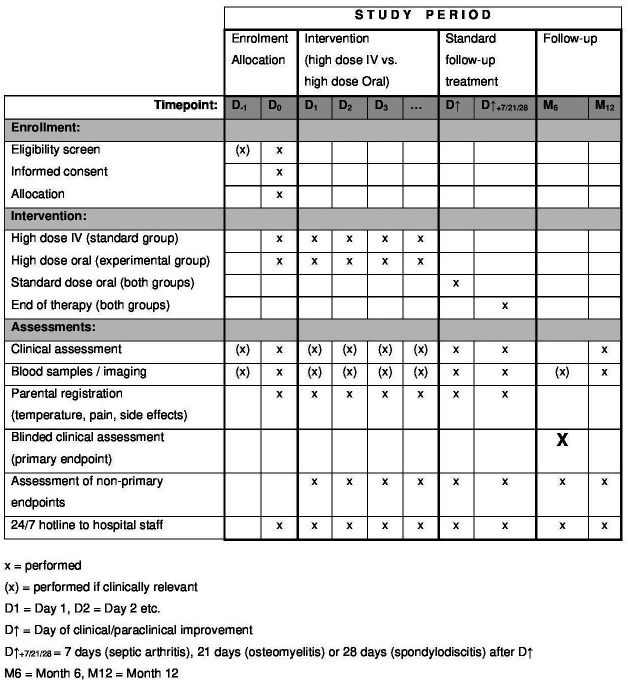
According to randomisation the child will receive (1) oral-only antibiotic therapy or (2) intravenous antibiotic therapy with shift to oral therapy after clinical and paraclinical improvement. All other aspects of diagnosing and treating the infection will follow current guidelines on paediatric BJI. This includes recommendations for mobilisation, physiotherapy, analgesic drugs, etc, which are all permitted during the trial. A throat swab for Kingella kingae will be added to the routine diagnostic procedures. All children will be evaluated with routine blood samples and clinical examination including grading of symptoms and pain score. See online supplemental appendix 1 for collection of extra material. The parents and/or the child will complete a daily registration of temperature and pain score, which will be reported weekly in an electronic questionnaire directly linked to the electronic case report form (eCRF). In these questionnaires, the parents and/or the child will also report adherence (number of missed doses) and drug side effects. The participant timeline is illustrated in figure 1.
Figure 1.
Participant timeline.
bmjopen-2023-072622supp001.pdf (60.9KB, pdf)
Choice of antibiotic treatment and predefined treatment strategies
The antibiotic treatment is administered as ‘initial treatment’ (intravenous vs high-dose oral) with a shift to ‘follow-up treatment’ (oral) after clinical and paraclinical improvement.
Initial treatment (randomised)
Empiric intravenous treatment (standard group):
Ceftriaxone 100 mg/kg/day (maximum 4000 mg/day).
Empiric oral treatment (experimental group):
-
Age <5 years:
Amoxicillin+clavulanate 1:8, 100 mg/kg/day divided every 8 hours (maximum 3000 mg amoxicillin/day).
-
Age >5 years:
Dicloxacillin 200 mg/kg/day divided every 6 hours (maximum 8000 mg dicloxacillin/day).
Follow-up treatment (not randomised)
Empiric oral treatment (both groups):
-
Age <5 years:
Amoxicillin+clavulanate 1:4, 50 mg/kg/day divided every 8 hours (maximum 1500 mg amoxicillin/day).
-
Age >5 years:
Dicloxacillin, 100 mg/kg/day divided every 6 hours (maximum 4000 mg dicloxacillin/day).
If infection with Staphylococcus aureus is suspected or confirmed, oral rifampicin 20 mg/kg/day divided every 8 hours (maximum 900 mg/day) can be added to the empiric therapy in both groups for optimal penetration and staphylococcal coverage.
According to daily clinical practice, the empiric antibiotic can be adjusted within the same route of administration (oral to oral or intravenous to intravenous) due to susceptibility testing, allergic reactions, adverse events or patient preferences to increase adherence (eg, taste) in both groups.
Treatment duration
In both groups, the treatment duration is individualised according to the rate of improvement. The minimum duration of the ‘initial treatment’ is 3 days with a shift to ‘follow-up treatment’ after clinical improvement (pain and mobility) and paraclinical improvement (decreasing C reactive protein (CRP)). The follow-up treatment is given for 4 weeks (spondylodiscitis), 3 weeks (other bone infections) or 1 week (joint infection only). The follow-up treatment will only be terminated if the child has no symptoms and a normal clinical examination, otherwise, the antibiotic therapy can be prolonged until these criteria are fulfilled.
Follow-up
All children will receive a clinical follow-up after 6 and 12 months. Any complaints or positive findings during follow-up will be evaluated and treated according to local guidelines. All patients and parents will be instructed to contact the department in the case of any symptoms indicating BJI during follow-up.
Registration of information from patient records
During the treatment and follow-up, the local primary investigator will maintain contact with the clinical team to identify potential outcomes. The primary investigator will register information in the patient’s eCRF in a predesigned database (software version: REDCap 9.1.0). Registered data will include age, sex, medical history, symptoms, clinical findings, blood samples, microbiological findings, imaging, treatment details and absence/presence of predefined outcomes. Missing data will be retrieved by a telephone interview if possible.
Primary outcome
Proportion of children with sequelae 6 months after initiation of treatment defined as abnormal mobility or function of the affected joint/bone. Evaluated by blinded clinical examination by a qualified paediatrician and/or paediatric orthopaedic surgeon (6 months).
Blinding
The assessor (qualified paediatrician or paediatric surgeon) of the primary outcome will be blinded for the intervention as well as any other details on the course of disease. The assessor will be informed about the age of the child as well as the approximate location of the infection and will perform a predefined systematic clinical examination of the relevant area (categories: (1) lower extremities, (2) upper extremities including claviculae and scapulae and (3) columna, costae and sternum). The exact anatomical location including side (left or right) will not be revealed. The child and parents will be followed by a study nurse who will secure that the blinding is respected. The primary outcome is met if there are any positive findings related to the previously infected bone or joint.
If indicated, any clinical findings will be further evaluated according to standard clinical practice and if this evaluation fails in confirming the sequelae (eg, suspicion of clinical scoliosis followed by normal scoliosis imaging), the primary outcome is not met.
Secondary outcomes
-
Non-acute treatment failure. Proportion of children with change of antibiotic therapy due to non-acute treatment failure (28 days).
This will be evaluated by two paediatric specialists and is suggested by the following parameters:
Temperature above 38.5°C after more than 72 hours of antibiotic therapy.
Increasing CRP after more than 96 hours of antibiotic therapy.
No improvement in mobility or pain after 120 hours of antibiotic therapy.
Recurrent infection. Proportion of children with recurrence of symptoms and signs (same anatomical location) after completion of antibiotic treatment requiring further antibiotic administration (6 months).
Other predefined outcome measures
Safety outcomes and other predefined outcome measures are listed in table 1.
Table 1.
Safety outcomes and other predefined outcome measures
| No | Category | Specification | Time frame |
| 1 | Safety | Proportion of children with severe complications during antibiotic treatment, for example, need for intensive care, septic shock, organ failure, pyomyositis, endocarditis, deep venous thrombosis. | 28 days |
| 2 | Safety | Proportion of children with need for surgical intervention during antibiotic treatment. Diagnostic surgical intervention (diagnostic joint aspiration or diagnostic bone biopsy) excluded | 28 days |
| 3 | Safety | Proportion of children with treatment-related adverse events for example, complications of intravenous access (infection, need for replacement, extravasation) and drug side effects reported by medical staff or by parents (electronic questionnaire) | 3 months |
| 4 | Exploratory | Time to apyrexia from initiation of antibiotic treatment | 28 days |
| 5 | Exploratory | Level of mobility and pain assessed by daily grading of symptoms by medical staff and daily standardised pain scores from participants and/or parents. Score systems: Visual Analogue Scale or Face Legs Activity Cry Consolability scale, both with scores from 0 (no pain) to 10 (worst pain). | 14 days |
| 6 | Exploratory | Total duration of antibiotic therapy | 3 months |
| 7 | Exploratory | Proportion of children with sequelae, for example, abnormal mobility and growth abnormalities, assessed by clinical examination by a qualified paediatrician 12 months after the initiation of treatment, accepted range 11–14 months | 14 months |
| 8 | Exploratory | Proportion of children with radiological abnormalities assessed by a qualified radiologist 12 months after initiation of treatment, accepted range 11–14 months | 14 months |
| 9 | Exploratory | Secondary infection with antimicrobial-resistant organisms or Clostridioides difficile | 3 months |
Discontinuation/withdrawal of participants from study treatment
If the allocated treatment is no longer compatible with good clinical care, the randomised strategy will be discontinued. The participant will continue follow-up in the trial and will be included in the primary analyses (intention to treat, ITT) but not in secondary analyses (per-protocol). Routine clinical care consistent with the new information will be recommended. Reasons for discontinuation/withdrawal of the randomised strategy include:
Development of severe disease or complications (safety outcome no. 1).
Non-acute treatment failure (secondary outcome no. 1). Non-acute treatment failure will be evaluated by two paediatric specialists, the local paediatrician responsible for the treatment, and one of the chief investigators. The decision to change therapy will be based on a complete evaluation of the clinical condition and the treating paediatrician will make the final decision.
Unable to receive oral treatment, for example, vomiting with no improvement on antinausea medications. If the patient is only temporarily unable to receive oral treatment, for example, intercurrent gastroenteritis or vomiting primarily due to pain or fever, intravenous treatment for maximum 24 hours will be accepted without discontinuation of the allocated oral strategy.
Unable to maintain intravenous access. If the participant is temporarily without intravenous access, for example, waiting for anaesthetic assistance, oral treatment for maximum 24 hours will be accepted without discontinuation of the allocated intravenous strategy.
No suitable medication exists within the allocated strategy (intravenous vs oral) due to susceptibility testing, contraindications or adverse reactions.
Non-adherence to the allocated therapy.
Withdrawal of consent from participant/parents.
Statistical methods and analyses
The plan for statistical analyses is based on the estimand framework.16 17
Sample size and power calculation
Outcomes will be compared by a non-inferiority assumption with an inferiority margin of 5% and an expected treatment success of 99% in both groups. With a one-sided significance level (alpha) of 2.5% and accounting for a 10% rate of drop-out, a sample size of 180 children in the principal stratum, 90 children in each group, will provide a power of 90% to detect non-inferiority.
Randomisation
Web-based computer randomisation (TrialPartner by DEFACTUM) will be used to allocate patients to the treatment groups at a 1:1 ratio stratified by CRP (<35 vs ≥35). The randomisation will be in randomly permuted blocks with varying block sizes of 4 and 6.
Target population/the principal stratum
The principal stratum will include all randomised children but exclude children with the intercurrent event of early termination, that is, children with no BJI. All randomised children will be included in the analysis of the three safety outcomes. For the remaining outcomes, including the primary and secondary outcomes, only data from children in the principal stratum will be analysed.
Statistical analyses for the primary outcome
Based on the principal stratum, the population-level summary measure will be the risk difference, calculated as the proportion with sequelae after 6 months in the experimental group (oral only) minus the proportion with sequelae after 6 months in the control group (intravenous+oral), with one-sided 97.5% confidence limits. If the absolute upper one-sided 97.5% CI is less than 5%, then the criteria of non-inferiority will be met.
Based on ITT principle, the primary analysis of the primary outcome will include all participants in the principal stratum.
A secondary per-protocol analysis (PPP) will also be performed excluding all participants experiencing one or more of the predefined intercurrent events leading to a discontinuation of the allocated treatment strategy.
Missing data
The primary outcome will be evaluated in all participants who attend the follow-up after 6 months. We only expect missing data if the participant is lost to follow-up or withdraw their consent. Due to the close follow-up at each local department, we expect missing data to be less than 5% and equal in both groups. If the missing data are more than 5%, we will impute data based on available knowledge for the patient and the observations of the other patients in the same randomised group. Sensitivity analyses will include tipping point analyses for the imputation.
Statistical analyses for the secondary outcomes
Based on the principal stratum, the primary analysis (ITT) described in 6.4.2 will be repeated for the secondary outcomes: ‘non-acute treatment failure’ and ‘recurrent infection’. The secondary analysis (PPP) described above will be repeated for ‘recurrent infection’ but not for ‘non-acute treatment failure’ while this outcome is one of the intercurrent events excluding the participant from the secondary analysis (PPP).
Missing data
If a participant experiences one of the secondary outcomes, it will be registered in the medical record. Due to the close follow-up and the national design including complete surveillance of all paediatric departments in Denmark with access to all electronic medical records, only cases where participants withdraw from all follow-up or relocate to another country are at risk for missing data on secondary outcomes. We expect this to be less than 5% and no imputation is planned for the secondary outcomes.
Statistical analyses for the safety outcomes
For safety outcomes 1 and 2, we will report the total number of participants in each treatment group meeting these outcomes.
For safety outcome 3, the outcome will be the fraction of days the child is affected by one or more of these non-serious adverse events (SAEs). The two randomised groups will be compared using the Wilcoxon-Mann-Whitney test. The population-level summary measure will be the difference between the means of the fractions with two-sided 95% CLs based on the normal approximation for the estimated mean difference. The mean of the individual fractions in each randomised group will also be presented with two-sided 95% CLs based on the normal approximation for the estimated mean.
In addition, we will also for each randomised group present the total number of non-SAEs, the number of children who had one or more non-SAEs, the number of non-SAEs per person-year at risk and the total number of days with one or more non-SAE.
Risks and safety monitoring
All antibiotics used in the trial are licensed agents with well described safety profiles approved for treating BJIs in children. The trial is not a clinical trial of an investigational medical product. The following, therefore, describes our own procedures for safety reporting.
Since our hypothesis is founded on the existing literature14 15 as well as the general development in antibiotic treatment for children in recent years2–4 and since we are excluding children with severe disease, we consider the risk of insufficient treatment to be minimal. Due to the close follow-up, we expect to promptly recognise insufficient treatment and evaluate whether a change in treatment is needed. In our recent retrospective study on Danish paediatric BJI infections,13 approximately 5% of children receiving the current standard treatment needed a change in antibiotic therapy due to insufficient effect (data not published). In the current study, we expect a similar need for change in therapy in both groups. The infection and the antibiotic treatment may result in discomfort (pain, fever), side effects (loose stool, abdominal pain, rash) or rarely other complications, but the risk of these events is not increased due to participation in the study. Unexpected adverse effects may occur, but the close follow-up including a 24/7 hotline to the hospital staff, enables us to react promptly to any unexpected incidents. Children and adolescents in the experimental group can avoid the establishment of intravenous access which in most children is a painful procedure. On the other hand, children in the experimental group need to take oral antibiotics for a longer period.
SAEs are not expected in this study due to the exclusion of patients with septic appearance and the fact that paediatric BJI is a condition not associated with mortality or severe morbidity. Only 1 of 82 children in our recent retrospective study of paediatric BJI developed sepsis or any other SAE.13
Safety and data monitoring committee
For monitoring the study, an independent safety and data monitoring committee will be established. The committee will consist of two independent paediatricians and a biostatistician with experience in paediatric infectious diseases and in the monitoring of RCTs will be consulted if needed. The committee will function independently of all other individuals conducting the study and all potential and SAEs will be reported to the committee. The committee will review all safety data by treatment arm every 6–12 months. The committee will be empowered to advise suspending the trial.
Roles, funding and patient compensation
The project is initiated by chief investigators Allan Bybeck Nielsen and Ulrikka Nygaard (sponsor). Each site has a primary investigator. The protocol is finalised by the listed authors which includes the chief investigators, main collaborators (Professor Lone Graff Stensballe and Professor Kjeld Schmiegelow) as well as primary investigators from sites with an expected inclusion of more than 10 participants. Funding is received from The Research Foundation of Copenhagen University Hospital, Copenhagen Health Science Partners and Innovation Fund Denmark. None of the investigators or main collaborators are financially attached to private enterprises, foundations, etc that have interests in the research project. Neither the patients enrolled in the project, nor their families, will receive any kind of payment for participating in the project.
Ethics and dissemination
The treating paediatrician will obtain informed consent according to the ethical approval, see information for parents in online supplemental appendix 2. As described in ‘risks and safety monitoring’, we consider the risk of harm to the participants to be minimal. The hypothesis has never been tested before and the radical change in treatment cannot be made in a scientific ethical sense without being based on a study at the current level of evidence. The hypothesis has not been tested in adults and it is not possible to perform the study on adults and transmit the data directly to children, as there are large differences in the course of BJIs between children and adults. If the experimental therapy is non-inferior to the standard therapy, the study is expected to lead to a radical change in the treatment of BJI in children and adolescents. The results of the project (whether positive, negative or inconclusive) will be submitted for publication in scientific peer-reviewed international journals. All investigators and main collaborators will be given the opportunity of authorship of the main publication(s) according to the International Committee of Medical Journal Editors (ICJME) criteria.
bmjopen-2023-072622supp002.pdf (128.9KB, pdf)
The study will be performed under the approval of The Ethics Committee of the Capital Region of Denmark (Ref.: H-20009117) and conducted according to the guidelines and recommendations of Good Clinical Practice and the Declaration of Helsinki.
Patient and public involvement
Parents of children in different age groups were involved in designing the participant information. No patient, parent or the public was involved in designing, writing or editing the protocol.
Trial registration, trial status and protocol amendments
The study is registered at www.clinicaltrials.gov (NCT04563325), trial registration dataset in online supplemental appendix 3. Recruitment was started on 15 September 2020. All sites are active, and 148 patients have been recruited in the principal stratum by 1 February 2023.
bmjopen-2023-072622supp003.pdf (48.8KB, pdf)
In version 1.0 of the protocol and at the initial registration on www.clinicaltrials.gov, all outcomes, except the primary outcome, were categorised as secondary outcomes. After finishing the statistical analysis plan, the categories of the outcomes were changed so that only two secondary outcomes are now registered. The remaining nine are now registered as ‘Other Outcome Measures’ including three safety outcomes corresponding to the current protocol version 2.0. In this revision of the outcome categories after the initiation of the study, four exploratory outcomes were dismissed:
Level of CRP. Comment: Will be reported but not considered as an outcome.
Disability days. Comment: This registration was missed in the electronic questionnaire and data are not registered.
Duration of intravenous antibiotics. Comment: Will be reported but not considered as an outcome.
Adherence (parental report of missed doses). Comment: Will be reported but not considered as an outcome.
Discussion
With the current protocol, we aim to investigate if oral-only antibiotic treatment is non-inferior to the current standard therapy of initially intravenous antibiotic treatment followed by oral treatment in children and adolescents with BJI.
The strengths of our study are the randomised controlled design with a blinded primary outcome evaluation and the national inclusion of all 18 paediatric departments in Denmark. The trial is fully embedded into daily clinical practice and reflects standard practice in all aspects other than randomisation and collection of data. The main limitation is the pragmatic criteria of inclusion without strict diagnostic criteria introducing a potential risk of including children with non-bacterial arthritis or osteomyelitis. We aim to reduce this risk by early termination of children if a non-infectious condition is established during treatment or follow-up. The pragmatic design ensures timely inclusion of patients and reflects daily clinical practice where antibiotic therapy is often initiated before strict diagnostic confirmation of bacterial infection.
The choice of a non-inferiority design was based on the combination of (1) the high treatment success of the current intravenous treatment and the overall favourable outcomes of these types of infection, (2) the practical aspects of realistic recruitment and (3) the potential large benefits of the experimental oral treatment. This choice is in accordance with current recommendations on non-inferiority clinical trials.18 We initially decided to use a 10% non-inferiority margin, which was based on consensus among a wide range of infectious disease specialists, paediatric infectious disease specialists and paediatric orthopaedic surgeons balancing the potential risks and benefits of oral treatment. This margin was further supported by published guidelines suggesting similar non-inferiority margins when evaluating treatment of other bacterial infections.19 After 6-month follow-up of the first 100 children, no sequelae were registered in the trial, equalling a treatment success of 100% in both groups. Due to this very high overall treatment success, we reduced the non-inferiority margin to 5% and adjusted the sample size estimation to 184 (initially 180) with expected treatment success of 99%.
Based on extrapolated Danish data from 2012 to 2017,13 more than 100 children are diagnosed with BJI in Denmark each year. If the experimental therapy is successful, these children will benefit significantly from the new treatment in terms of shorter admissions, avoidance of intravenous access, earlier return to everyday activities and better quality of life during the treatment. The results are expected to influence the treatment strategies of children with BJIs worldwide. Especially in countries with similar resistance spectrum where the results can be directly applied, but also in countries with a more challenging resistance spectrum, where the general demand (often non-evidence based) of intravenous antibiotics for severe infections will be challenged.
Study sites
Department of Pediatrics and Adolescent Medicine, Lillebaelt Hospital, Kolding
Department of Pediatrics and Adolescent Medicine, Regional Hospital, Viborg
Department of Pediatrics and Adolescent Medicine, Sydvestjysk Hospital, Esbjerg
Department of Pediatrics and Adolescent Medicine, Aalborg University Hospital
Department of Pediatrics and Adolescent Medicine, Nordsjælland Hospital, Hillerød
Department of Pediatrics and Adolescent Medicine, Slagelse Hospital
Department of Pediatrics and Adolescent Medicine Pediatrics, Herlev Hospital
Department of Pediatrics and Adolescent Medicine, Zealand University Hospital, Roskilde
Department of Pediatrics and Adolescent Medicine, Regional Hospital Vestjylland, Herning
Department of Pediatrics and Adolescent Medicine, Holbæk Hospital
Department of Pediatrics and Adolescent Medicine, Aarhus University Hospital
Department of Pediatrics and Adolescent Medicine, Regional Hospital Randers
Department of Pediatrics and Adolescent Medicine, Hjørring Hospital
Department of Pediatrics and Adolescent Medicine, Sønderjylland Hospital, Aabenraa
Department of Pediatrics and Adolescent Medicine, Nykøbing Falster Hospital
Department of Pediatrics and Adolescent Medicine, Hvidovre Hospital
Department of Pediatrics and Adolescent Medicine, Odense University Hospital
Department of Pediatrics and Adolescent Medicine, Rigshospitalet, Copenhagen University Hospital
Supplementary Material
Footnotes
Collaborators: The authors thank all the local investigators (Grethe Lemvik Mikkelsen, Regional Hospital Viborg; Jens Jakob Herrche Petersen, Sydvestjysk Hospital, Esbjerg; Jesper Thaarup, Aalborg University Hospital; Kim Kristensen; Lise Heilmann Jensen, Zealand University Hospital, Roskilde; Marie Cecilie Lawaetz, Holbæk Hospital; Morten Søndergaard Lindhard, Regional Hospital Randers; Pawel Andrej Marcinski, Hjørring Hospital; Lotte Høeg Hansen, Sønderjylland Hospital, Aabenraa, Tanja Hübertz Horsager, Regional Hospital Viborg; Maren Rytter, Slagelse Hospital; Tatjana Zaharov, Nykøbing Falster Hospital) for their big effort in preparing and informing the individual sites about the trial before initiation. We also thank Jakob Hjort, data manager, Department of Clinical Medicine, Aarhus University, for establishing the web-based randomisation module as well as Ulrik Justesen, Odense University Hospital for microbiological advice.
Contributors: ABN and UN initiated and planned the study, and they contributed equally to the initial conception and design of the study protocol. ABN and UN drafted the first and subsequent versions of the study protocol. LB, MD, JPG, UH, TUH, MH, AHR, LSS, KS and LGS made substantial contributions to the design of the study, and they critically revised the study protocol. All authors read and approved the final manuscript and agree to be accountable for all aspects of the work.
Funding: Funding is received from The Research Foundation of Copenhagen University Hospital, Copenhagen Health Science Partners and Innovation Fund Denmark. The funding covers salaries for study doctors, statisticians, and additional expenses (eg, software and hardware). The funding is administered through research accounts at the Copenhagen University Hospital Rigshospitalet.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
Local Investigators:
Grethe Lemvik Mikkelsen, Jens Jakob Herrche Petersen, Jesper Thaarup, Kim Kristensen, Lise Heilmann Jensen, Marie Cecilie Lawaetz, Morten Søndergaard Lindhard, Pawel Andrej Marcinski, Lotte Høeg Hansen, Tanja Hübertz Horsager, Tatjana Zaharov, Jakob Hjort, Ulrik Justesen, and Maren Rytter
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Spellberg B, Aggrey G, Brennan MB, et al. Use of novel strategies to develop guidelines for management of Pyogenic Osteomyelitis in adults: A Wikiguidelines group consensus statement. JAMA Netw Open 2022;5:e2211321. 10.1001/jamanetworkopen.2022.11321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lodha R, Kabra SK, Pandey RM, et al. Antibiotics for community-acquired pneumonia in children. Cochrane Database of Systematic Reviews 2013. 10.1002/14651858.CD004874.pub4 [DOI] [PubMed] [Google Scholar]
- 3. Strohmeier Y, Hodson EM, Willis NS, et al. Antibiotics for acute Pyelonephritis in children. Cochrane Database Syst Rev 2014:CD003772. 10.1002/14651858.CD003772.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hoberman A, Wald ER, Hickey RW, et al. Oral versus initial intravenous therapy for urinary tract infections in young febrile children. Pediatrics 1999;104:79–86. 10.1542/peds.104.1.79 [DOI] [PubMed] [Google Scholar]
- 5. Iversen K, Ihlemann N, Gill SU, et al. Partial oral versus intravenous antibiotic treatment of Endocarditis. N Engl J Med 2019;380:415–24. 10.1056/NEJMoa1808312 [DOI] [PubMed] [Google Scholar]
- 6. Heldman AW, Hartert TV, Ray SC, et al. Oral antibiotic treatment of right-sided Staphylococcal Endocarditis in injection drug users: prospective randomized comparison with parenteral therapy. Am J Med 1996;101:68–76. 10.1016/s0002-9343(96)00070-8 [DOI] [PubMed] [Google Scholar]
- 7. Wald-Dickler N, Holtom PD, Phillips MC, et al. Oral is the new IV. challenging decades of blood and bone infection dogma: A systematic review. Am J Med 2022;135:369–79. 10.1016/j.amjmed.2021.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Thabit AK, Fatani DF, Bamakhrama MS, et al. Antibiotic penetration into bone and joints: an updated review. Int J Infect Dis 2019;81:128–36. 10.1016/j.ijid.2019.02.005 [DOI] [PubMed] [Google Scholar]
- 9. Valenzuela MC, Viviani ST. Short duration of initial intravenous treatment in 70 pediatric patients with Osteoarticular infections. Rev Chil Infectologia Organo Of Soc Chil Infectologia 2008;25:30–6. [PubMed] [Google Scholar]
- 10. Jagodzinski NA, Kanwar R, Graham K, et al. Prospective evaluation of a shortened regimen of treatment for acute Osteomyelitis and septic arthritis in children. J Pediatr Orthop 2009;29:518–25. 10.1097/BPO.0b013e3181ab472d [DOI] [PubMed] [Google Scholar]
- 11. Peltola H, Pääkkönen M, Kallio P, et al. Versus long-term antimicrobial treatment for acute Hematogenous Osteomyelitis of childhood: prospective, randomized trial on 131 culture-positive cases. Pediatr Infect Dis J 2010;29:1123–8. 10.1097/INF.0b013e3181f55a89 [DOI] [PubMed] [Google Scholar]
- 12. Peltola H, Pääkkönen M, Kallio P, et al. Prospective, randomized trial of 10 days versus 30 days of antimicrobial treatment, including a short-term course of parenteral therapy, for childhood septic arthritis. CLIN INFECT DIS 2009;48:1201–10. 10.1086/597582 Available: http://www.journals.uchicago.edu/toc/cid/48/9 [DOI] [PubMed] [Google Scholar]
- 13. Nielsen AB, Nygaard U, Hoffmann T, et al. Short Individualised treatment of bone and joint infections in Danish children. Arch Dis Child 2019;104:205–6. 10.1136/archdischild-2018-315734 [DOI] [PubMed] [Google Scholar]
- 14. Alcobendas R, Remesal A, Murias S, et al. Outpatients with acute Osteoarticular infections had favourable outcomes when they received just oral antibiotics without intravenous antibiotics. Acta Paediatr 2018;107:1792–7. 10.1111/apa.14373 [DOI] [PubMed] [Google Scholar]
- 15. Roul-Levy A, Looten V, Bachy M, et al. Oral ambulatory treatment of acute Osteomyelitis in children: A case-control study. Pediatr Emerg Care 2016;32:154–6. 10.1097/PEC.0000000000000725 [DOI] [PubMed] [Google Scholar]
- 16. International Council for Harmonisation . Addendum on Estimands and sensitivity analysis in clinical trials to the guideline OM statistical principles for clinical trials E9(R). n.d. Available: https://database.ich.org/sites/default/files/E9-R1_Step4_Guideline_2019_1203.pdf
- 17. Clark TP, Kahan BC, Phillips A, et al. Estimands: bringing clarity and focus to research questions in clinical trialsBMJ open 2022;12:E052953. BMJ Open 2022;12:e052953. 10.1136/bmjopen-2021-052953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. FDA guidance on non-inferiority clinical trials. n.d. Available: https://www.fda.gov/media/78504/download
- 19. EMA guideline on the evaluation of medicinal products indicated for treatment of bacterial infections. EMA/844951/2018Rev. n.d. Available: https://www.ema.europa.eu/en/documents/scientific-guideline/draft-guideline-evaluation-medicinal-products-indicated-treatment-bacterial-infections-revision-3_en.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-072622supp001.pdf (60.9KB, pdf)
bmjopen-2023-072622supp002.pdf (128.9KB, pdf)
bmjopen-2023-072622supp003.pdf (48.8KB, pdf)