Abstract
Objective
Pulmonary hypertension (PHT) commonly coexists with significant mitral regurgitation (MR), but its prevalence and prognostic importance have not been well characterised. In a large cohort of adults with moderate or greater MR, we aimed to describe the prevalence and severity of PHT and assess its influence on outcomes.
Methods
In this retrospective study, we analysed the National Echocardiography Database of Australia (data from 2000 to 2019). Adults with an estimated right ventricular systolic pressure (eRVSP), left ventricular ejection fraction >50% and with moderate or greater MR were included (n=9683). These subjects were then categorised according to their eRVSP. The relationship between PHT severity and mortality outcomes was evaluated (median follow-up of 3.2 years, IQR 1.3–6.2 years).
Results
Subjects were aged 76±12 years, and 62.6% (6038) were women. Overall, 959 (9.9%) had no PHT, and 2952 (30.5%), 3167 (32.7%), 1588 (16.4%) and 1017 (10.5%) patients had borderline, mild, moderate and severe PHT, respectively. A ‘typical left heart disease’ phenotype was identified with worsening PHT, showing rising E:e′, right and left atrial sizes increasing progressively, from no PHT to severe PHT (p<0.0001, for all). With increasing PHT severity, 1- and 5-year actuarial mortality increased from 8.5% and 33.0% to 39.7% and 79.8%, respectively (p<0.0001). Similarly, adjusted survival analysis showed the risk of long-term mortality progressively increased with higher eRVSP levels (adjusted HR 1.20–2.86, borderline to severe PHT, p<0.0001 for all). A mortality inflection was apparent at an eRVSP level >34.00 mm Hg (HR 1.27, CI 1.00–1.36).
Conclusions
In this large study, we report on the importance of PHT in patients with MR. Mortality increases as PHT becomes more severe from an eRVSP of 34 mm Hg onwards.
Keywords: mitral valve insufficiency; hypertension, pulmonary; heart valve diseases
WHAT IS ALREADY KNOWN ON THIS TOPIC
Pulmonary hypertension (PHT) commonly coexists with significant mitral regurgitation (MR), but its prevalence, phenotype and prognostic importance have not been well characterised.
WHAT THIS STUDY ADDS
Within a large cohort of adults (n=9638) with moderate or greater MR and preserved left ventricular ejection fraction, a phenotype of ‘typical left heart disease’ has been described. Mortality increases progressively as PHT becomes more severe from an eRSVP 34 mm Hg onwards.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
This study highlights specific echocardiographic parameters associated with worsening PHT allowing for more accurate monitoring and prognostication in a cohort where even mild elevations of pulmonary pressures are associated with an increased risk of mortality.
Introduction
Mitral regurgitation (MR) is an increasingly prevalent valvular problem in developed countries1 and is the second-most common valve lesion requiring operative management in Europe2 and the USA,3 after aortic stenosis (AS). Symptoms and outcomes generally correlate with both the severity of the regurgitation and the myocardial response to volume overload.4 The identification of prognostic factors is important to risk stratify patients and to potentially guide treatment decisions. While it is recognised that pulmonary hypertension (PHT) is a potential complication of MR, this is actually not well documented. There are varying reports, in relatively small cohorts on the prevalence5 6 and echocardiographic phenotype7 8 of these patients and, thus, an incomplete understanding of the prognostic impact of PHT in significant MR.1
Group 2 PHT, or PHT due to left heart disease (LHD), is the most common type of PHT.9 10 PHT is thought to be a predictive feature of deterioration in these patients and likely arises from elevated left atrial (LA) pressure causing back pressure into the pulmonary vasculature.9 11 In MR specifically, PHT is thought to be due to the direct effect of systolic backflow into the LA and may develop before patients experience symptoms or left ventricular (LV) systolic dysfunction.5 9 12
Echocardiography remains the the most common screening tool for PHT and is widely used in clinical practice. Using the power of ‘big’ data from the National Echo Database of Australia (NEDA), a registry with contemporary community and hospital-based echo data on over 600 000 unique adult subjects from over 25 centres across Australia, we aimed to describe the prevalence of PHT in adults with moderate or greater MR and to assess the influence of PHT severity on outcomes.
Methods
NEDA database and study design
The NEDA is a multicentre registry, and the purpose and methodology of which have been previously described.13–15 NEDA contains basic demographic and detailed echocardiographic data of adults from >25 centres across Australia. The database is linked with the National Death Index (NDI), provided by the Australian Institute for Health and Welfare; the NDI provides mortality data on each individual. The study period included >1 million echo reports from >6 00 000 individuals, studied between January 2000 and June 2019. Vital status was determined as of 21 May 2019 (median follow-up of 6.2 years, IQR 3.8–9.8 years); patients alive at this date were censored alive. NEDA is registered with the Australian New Zealand Clinical Trials Registry (ACTRN12617001387314), and human ethics approval was obtained from the Sydney Local Health District Human Research Ethics Committee, protocol X15-0387 and 2019/ETH069899. A retrospective waiver of consent was authorised as part of this ethics protocol.
Study cohort
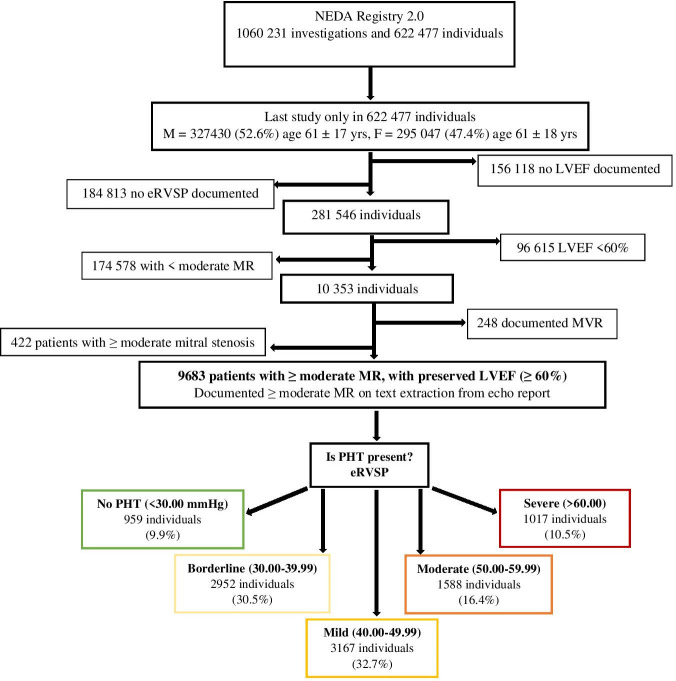
Figure 1 shows our study flow diagram, and this is consistent with our previous work on PHT in left-sided valvular pathology.16 17 NEDA data at the time of study census were used to identify a cohort of patients with significant MR to characterise their relationship with PHT: (1) adults ≥18 years of age, (2) with at least one echocardiogram recorded on the system (where patients had multiple studies only the last study was included in the analysis), (3) with a recorded left ventricular ejection fraction (LVEF), estimated right ventricular systolic pressure (eRVSP) and (4) with moderate or greater MR. Text extraction was used to identify patients with moderate and severe MR as well as right ventricular (RV) size and function.14 While quantitative measures of MR were interrogated, sufficient data were not available in the majority of patients, a reflection of real-world practice within Australia. All participating laboratories use an integrative and semiquantitative approach for grading MR severity as recommended by the American Society of Echocardiography.18 Patients with mitral valve (MV) replacements were excluded from primary analysis as were patients with evidence of significant mitral stenosis (conservatively defined as mitral valve gradient >5 mm Hg), LVEF <60% and patients with less than moderate MR. eRVSP was conservatively derived using the Bernoulli equation (4×[(tricuspid regurgitation velocity) TRV]2+assumed RA pressure of 5 mm Hg).19
Figure 1.
Study flow chart. This figure shows the analysis flow chart, performed in this study. eRVSP, estimated right ventricular systolic pressure; LVEF, left ventricular ejection fraction; MR, mitral regurgitation; MVR, mitral valve replacement; NEDA, National Echo Database Australia; PHT, pulmonary hypertension.
Study methods
Similar to our previous work,16 17 once the cohort of patients with moderate or greater MR was established, subjects were categorised according to their eRVSP, according to clinical guidelines10 20 to document the distribution of eRVSP and thence PHT severities. A ‘borderline PHT’ group which has previously been determined as potentially significant in both NEDA papers and other recent prospective publications14 21 22 was included. Defined categories were: (1) normal (eRVSP <30 mm Hg), (2) borderline (30.00–39.99 mm Hg), (3) mildly elevated (40.00–49.99 mm Hg), (4) moderately elevated (50.00–59.99 mm Hg) and (5) severely elevated (eRVSP ≥60 mm Hg).14 20
We then analysed the eRVSP data according to decile distribution14: first decile—5.00–30.00 mm Hg, second decile—30.01–34.00 mm Hg, third decile—34.01–37.04 mm Hg, fourth decile—37.05–39.16 mm Hg, fifth decile—39.17–43.00 mm Hg, sixth decile—43.01–46.00 mm Hg, seventh decile—46.01–48.44 mm Hg, eighth decile—48.45–53.00 mm Hg, ninth decile—53.01–61.00 mm Hg and 10th decile—>61.00 mm Hg.
All-cause mortality was determined during a median follow-up of 3.2 years (IQR 1.3–6.2 years). We explored the relationship between eRVSP level and survival, looking at both clinically defined groups (as above) and the eRVSP deciles.
Statistical analysis
All continuous variables are expressed as mean±SD, unless otherwise stated, and categorical data are expressed as frequency and percentages. For continuous variables, linear regression analysis using analysis of variance was used to test whether the trend of the mean across the categorical groups of eRVSP levels was linear. For binary variables, the χ2 test was used to determine if there was a trend in the change in proportions across the groups.
Actuarial 1-year and 5-year survival rates for all-cause mortality were calculated from 9439 (97.9%) and 6780 (70.3%) subjects with complete follow-up for those time points. Multiple logistic regression models (entry at univariate p-value <0.05) were used to derive adjusted ORs for mortality models at fixed time points. Cox regression hazard models were used to derive adjusted HRs for mortality outcomes during follow-up (entry model at a univariate p-value <0.05). Adjusted analyses included age and sex. A sensitivity analysis was performed excluding patients with significant concurrent severe AS and moderate or greater aortic regurgitation (AR). Patients with moderate and severe MR were also assessed separately to determine if there were differences between these two groups. Severe MR was defined as ‘severe mitral regurgitation’ on text extraction. All analyses were performed with SPSS software version 25.0 (IBM, Armonk, New York, USA), and statistical significance was accepted at a two-tailed p-value of <0.05.
Results
Prevalence of PHT and distribution of eRVSP
A total of 9638 patients with moderate or greater MR, normal left ventricular systolic function and eRVSP data were identified; the majority (62.6%) were women. Figure 2 shows the frequency distribution of eRSVP levels (median 43.00 mm Hg, IQR 35.46–50.96 mm Hg). The number of patients in each subgroup was as follows: no PHT (eRVSP <30 mm Hg)—959 individuals (9.9%), borderline PHT (eRVSP 30.00–39.99 mm Hg)—2952 individuals (30.5%), mild PHT (eRVSP 40.00–49.99 mm Hg)—3167 individuals (32.7%), moderate PHT (eRVSP 50.00–59.99 mm Hg)—1588 individuals (16.4%) and severe individuals (eRVSP >60 mm Hg)—1017 individuals (10.5%).
Figure 2.
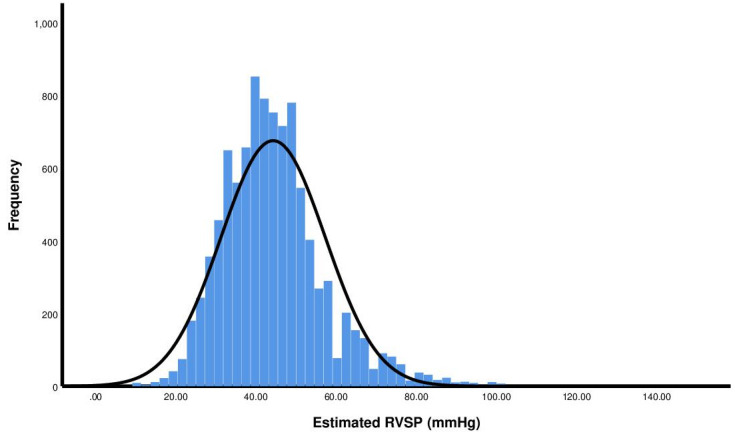
Frequency distribution of estimated right ventricular systolic pressure within the cohort. These data show the statistical distribution of estimated right ventricular systolic pressure (RVSP) levels.
Cohort profile
Table 1 summarises the demographic and echocardiographic characteristics of the study cohort divided into subgroups based on measured eRVSP levels. Age was greater in those with higher eRVSP levels, from a mean of 69±17 years in patients with no PHT to 81±10 years in patients with moderate PHT, before a plateau was noted in those with severe PHT (80±11 years) (p<0.0001 for all). The proportion of patients with atrial fibrillation or an atrial arrhythmia was greater in those with higher eRVSP levels (24.0% vs 54.8%, no PHT vs severe PHT, respectively).
Table 1.
Baseline characteristics of study cohort (N=9683)
| eRSVP 0.00–29.99 n=959 |
eRVSP 30.00–39.99 n=2952 |
eRVSP 40–49.99 n=3167 |
eRVSP 50–59.99 n=1588 |
eRVSP >60.00 n=1017 |
P value | |
| Demographics | ||||||
| Age, years | 69±17 | 74±13 | 78±11 | 81±10 | 80±11 | < 0.0001 |
| Female (%) | 611 (63.7) | 1773 (60.1) | 1992 (62.9) | 1011 (63.7) | 651 (64.0) | <0.0001 |
| Anthropometrics | ||||||
| BMI | 25.92±5.15 | 26.02±5.40 | 26.52±5.76 | 26.56±6.03 | 26.05±5.73 | 0.48 |
| BSA | 1.80±0.24 | 1.80±0.24 | 1.80±0.25 | 1.80±0.24 | 1.76±0.24 | <0.0001 |
| Rhythm | ||||||
| Atrial fibrillation/arrhythmia | 230 (24.0) | 947 (32.1) | 1268 (40.0) | 770 (48.5) | 557 (54.8) | <0.0001 |
| LV dimensions and function | ||||||
| LVEF % | 66.14±5.41 | 68.13±6.89 | 70.53±7.90 | 70.40±7.89 | 70.02±7.90 | <0.0001 |
| Stroke volume index (mL/m2) | 44.06±11.97 | 44.98±14.37 | 44.96±14.79 | 43.49±14.09 | 42.15±14.99 | 0.06 |
| E:e′ ratio | 12.90±5.63 | 13.07±5.68 | 14.14±5.27 | 15.35±5.51 | 17.16±7.01 | <0.0001 |
| LVEDD | 4.50±0.67 | 4.71±0.69 | 4.87±0.73 | 4.92±0.77 | 4.85±0.82 | <0.0001 |
| LVESD | 2.87±0.53 | 2.87±0.57 | 2.84±0.64 | 2.87±0.65 | 2.83±0.69 | 0.009 |
| Atrial dimensions | ||||||
| LA volume index, mL/m2 | 43.84±24.23 | 67.90±41.04 | 95.53±47.82 | 108.92±54.28 | 108.95±55.95 | <0.0001 |
| RA area, cm2 | 18.18±7.25 | 24.21±8.76 | 29.03±8.50 | 32.12±9.01 | 33.71±9.35 | <0.0001 |
| Right heart dimensions and function | ||||||
| eRSVP, mm Hg | 25.66±3.63 | 35.43±2.94 | 44.69±2.76 | 53.97±2.93 | 71.10±10.84 | <0.0001 |
| TR peak velocity, m/s | 2.19±0.23 | 2.56±0.17 | 2.94±0.14 | 3.30±0.14 | 3.86±0.33 | <0.0001 |
| RV basal diameter | 3.53±0.75 | 3.30±0.47 | 3.36±0.37 | 3.44±0.40 | 3.56±0.47 | <0.0001 |
| Dilated RV | 95 (9.9) | 509 (17.2) | 1051 (33.2) | 673 (42.4) | 521 (51.2) | <0.0001 |
| Impaired RV function | 14 (1.5) | 28 (0.9) | 59 (1.9) | 54 (3.4) | 82 (8.1) | <0.0001 |
| Mitral valve dimensions and function | ||||||
| MV mean gradient, mm Hg | 2.32±1.18 | 2.63±1.20 | 3.01±1.16 | 3.31±1.18 | 3.09±1.22 | <0.0001 |
| Concomitant valvular pathology | ||||||
| Moderate or greater aortic regurgitation | 85 (8.9) | 246 (8.3) | 369 (11.7) | 229 (14.4) | 156 (15.3) | <0.0001 |
| Severe AS <1 cm2 | 26 (2.7) | 89 (3.0) | 121 (3.8) | 82 (5.2) | 77 (7.8) | <0.0001 |
Values are n (%) unless otherwise indicated.
AS, aortic stenosis; AV, aortic valve; BMI, body mass index; BSA, body surface area; eRVSP, estimated right ventricular systolic pressure (mm Hg); LA, left atrial; LV, left ventricle; LVEDD, left ventricular end diastolic diameter; LVEF, left ventricular ejection fraction; LVESD, left ventricular end systolic pressure; MV, mitral valve; RA, right atrial; RV, right ventricle; TR, tricuspid regurgitant; VTI, velocity time integral.
A typical pattern of worsening ‘LHD’ phenotypic response with worsening PHT was evident. E:e′ increased progressively with increased severity of PHT (12.90±5.63 vs 17.16±7.01, no PHT vs severe PHT, respectively, p<0.0001 for all). An increase in right atrial area and indexed left atrial volume was also noted (18.18±7.25 cm2 vs 33.71±9.35 cm2 and 43.84±24.21 vs 108.95±55.95 mL/m2, no PHT vs severe PHT, respectively, p<0.0001 for all) though indexed left atrial volume plateaued in those with severe PHT. Qualitative observations showed an increased proportion of patients with increased RV dilation and functional impairments as eRVSP levels increased.
The differences between male and female patients are shown in online supplemental table 1. Female patients were older than their male counterparts (77±13 years vs 75±12 years) but did not show clinically meaningful differences in eRVSP level. Females had higher E:e’ but lower right atrial area and indexed LA volume compared with males.
openhrt-2023-002268supp001.pdf (72.2KB, pdf)
Survival data
The survival profile of the cohort based on the severity of PHT as determined on echocardiography is summarised in table 2. All-cause mortality at 1 and 5 years (actuarial mortality) and long-term survival (all adjusted for age and gender) were reported between those with eRVSPs <30.00 mm Hg and the four categories of progressively elevated eRSVP. As predicted, the risk for mortality markedly increased with higher eRVSP levels. This was shown by the range in 1-year and 5-year actuarial mortality from a low of 8.5% and 33.0% to a high of 39.7% and 79.8%, in those with normal to severely elevated eRVSPs. This trend was mirrored in adjusted long-term mortality results which showed a 1.20-fold increase in risk in those with borderline PHT compared to a 2.86-fold increase in those with severe PHT (p<0.0001 for all) (figure 3A). Cardiovascular mortality trends showed an increased risk in those with moderate and severe PHT (table 2). Trends were less clear in those with smaller numbers and possible inaccurate coding for causes of death documented on death certificates, as possible contributing factors.
Table 2.
Survival profile and adjusted risk for mortality according to estimated right ventricular systolic pressure levels
| 1-year actuarial mortality (N=9439) |
5-year actuarial mortality (N=6780) |
All fatal events (N=9638) |
Cardiovascular mortality (N=9638) |
|
| OR (95% CI) | OR (95% CI) | HR (95% CI) | HR (95% CI) | |
| All individuals, N=9638 | 1573 (16.7) | 3603 (53.1) | 4614 (47.9) | 1777 (18.4) |
| Normal eRVSP (<30 mm Hg), n=959 | 79/950 (8.5) Reference |
192/581 (33.0) Reference |
247 (25.8) Reference |
83 (8.7) Reference |
| Borderline PHT (eRVSP 30.00–39.99 mm Hg), n=2952 |
304/2869 (12.0) OR 1.14 (1.02–1.47) |
791/1970 (40.2) OR 1.18 (1.01–1.45) |
1098 (37.2) HR 1.20 (1.04–1.38) |
383 (13.0) HR 0.77 (0.61–0.97) |
| Mild PHT (eRVSP 40.00–49.99 mm Hg), n=3167 |
468/3088 (17.0) OR 1.52 (1.18–1.96) p=0.001 |
1179/2280 (51.7) OR 1.58 (1.34–1.86) |
1612 (50.9) HR 1.54 (1.34–1.76) |
607 (19.2) HR 0.81 (0.64–1.01) |
| Moderate PHT (eRSVP 50.00–59.99 mm Hg), n=1588 | 342/1533 (25.8) OR 2.22 (1.71–2.90) |
787/1129 (69.7) OR 2.93 (2.32–3.70) |
922 (58.1) HR 2.00 (1.73–2.30) |
383 (24.1) HR 1.19 (0.94–1.51) |
| Severe PHT (eRVSP >60 mm Hg), n=1017 |
380/999 (39.7) OR 4.64 (3.55–6.08) |
654/820 (79.8) OR 5.18 (3.98–6.73) |
1068 (72.3) HR 2.86 (2.48–3.31) |
321 (31.6) HR 1.62 (1.27–2.06) |
Analyses adjusted for age and sex. Values are n (%) or n/mean (%), unless otherwise indicated.
eRVSP, estimated right ventricular systolic pressure; PHT, pulmonary hypertension.
Figure 3.
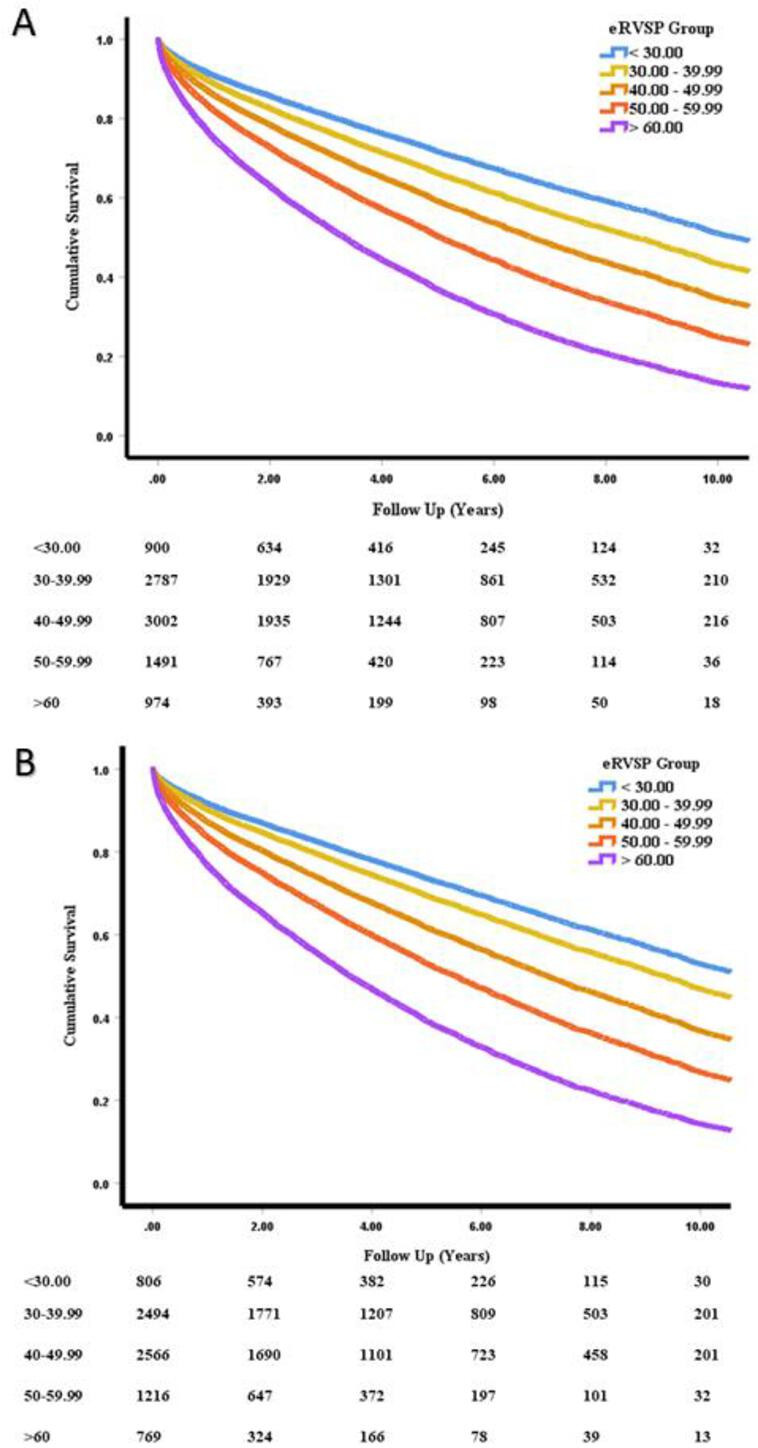
Adjusted risk for all-cause mortality using Cox proportional hazards showing as estimated right ventricular systolic pressure (eRVSP) level increases based on clinical severity, risk of mortality increases in (A) the total cohort and (B) the cohort excluding patients with severe aortic stenosis and/or moderate or greater aortic regurgitation.
A sensitivity analysis was performed excluding patients with moderate or greater AR or severe AS. The trends were maintained in 1-year and 5-year actuarial analysis, though only achieved statistical significance from mild PHT onwards. Adjusted long-term mortality continued to progressively increase as eRVSP level increased (table 3, figure 3B). Indexed LA volume was also included as a variable in the survival models, with mortality trends mirroring the above results (online supplemental table 2). In all models, increasing age and male sex were also associated with increasing mortality (p<0.0001, for all).
Table 3.
Sensitivity analysis—survival profile and adjusted risk for mortality according to estimated right ventricular systolic pressure levels (excluding patients with moderate or greater aortic regurgitation and severe aortic stenosis, N=8293)
| 1-year actuarial mortality (n=8094) |
5-year actuarial mortality (n=5793) |
All fatal events (N=8293) |
Cardiovascular mortality (N=8293) |
|
| OR (95% CI) | OR (95% CI) | HR (95% CI) | HR (95% CI) | |
| All individuals, N=8293 | 1235 (15.3) | 2917 (50.4) | 3812 (46.0) | 1419 (17.1) |
| Normal eRVSP (<30 mm Hg), n=857 | 68/852 (8.0) Reference |
164/523 (31.4) Reference |
209 (24.4) Reference |
70 (8.2) Reference |
| Borderline PHT (eRSVP 30.00–39.99 mm Hg), n=2634 |
234/2566 (9.1) OR 1.09 (0.75–1.32) |
648/1749 (37.0) OR 1.10 (0.88–1.38) |
933 (35.4) HR 1.15 (1.03–1.34) |
315 (12.0) HR 0.70 (0.54–0.91) |
| Mild PHT (eRVSP 40.00–49.99 mm Hg), n=2704 |
376/2640 (14.2) OR 1.45 (1.10–1.92) |
974/1949 (50.0) OR 1.58 (1.26–1.97) |
1355 (50.1) HR 1.54 (1.33–1.78) |
506 (18.7) HR 0.76 (0.59–0.98) |
| Moderate PHT (eRSVP 50.00–59.99 mm Hg), n=1294 | 268/1245 (21.5) OR 2.19 (1.64–2.93) |
623/925 (67.4) OR 2.77 (2.16–3.56) |
741 (57.3) HR 1.99 (1.71–2.32) |
297 (23.0) HR 1.12 (0.86–1.45) |
| Severe PHT (eRVSP >60 mm Hg), n=804 |
289/791 (36.5) OR 4.51 (3.36–6.06) |
508/647 (78.5) OR 5.18 (3.90–6.88) |
574 (71.4) HR 2.96 (2.52–3.47) |
231 (28.7) HR 1.50 (1.14–1.96) |
Analyses adjusted for age and sex. Values are n (%) or n/mean (%), unless otherwise indicated.
eRVSP, estimated right ventricular systolic pressure; PHT, pulmonary hypertension.
Mortality was assessed when the cohort was divided into two cohorts based on severity (moderate MR—8214 patients, severe MR—1469 patients). In the moderate MR cohort, which had larger numbers, mortality outcomes mirrored that of the total cohort (online supplemental table 3). Mortality outcomes had a similar trend in those with severe MR, although statistical significance was not reached at milder elevations of eRVSP level, most likely a consequence of the smaller subject numbers (online supplemental table 4). Mortality outcomes among women (n=6038) matched with those in the total cohort (HR 1.32, 95% CI 1.10–1.58 for borderline PHT vs HR 2.92, 95% CI 2.42–3.53 for severe PHT) (online supplemental table 5). The male cohort (n=3645) had similar trends, though significance was only reached when pulmonary pressures were mildly elevated (online supplemental table 6).
Threshold for mortality
A Cox regression model was constructed using the decile distribution of eRVSP and adjusted for age and sex. This confirmed that the adverse effects of PHT were noted from the third decile (eRVSP 34.01–37.04 mm Hg) relative to the lowest decile <30.00 mm Hg (HR 1.16, 95% CI 1.00–1.36, p=0.05). Risk increased progressively from those with borderline PHT in the third decile to the 10th decile (eRVSP 60.01–143.63; HR 2.89, 95% CI 2.51–3.32, p<0.0001) (online supplemental table 7). Hence, the adjusted risk for mortality is markedly higher in those with borderline PHT and above regardless of age, gender or cause of death.
Discussion
This large, ‘real-world’ cohort study, including over 9500 patients examines the relationship between MR and PHT, in patients with preserved ejection fraction (EF). The use of ‘big data’ through the NEDA, which includes over 1 million echoes in over 600 000 individuals, allowed for a more detailed, contemporary description of the prevalence and phenotype of these patients. We confirmed the negative short-term and long-term prognostic impact PHT has in MR and have documented that the threshold for excess mortality lies within the range of ‘borderline PHT’.
PHT is likely to occur in patients with significant MR via the following mechanism; in the initial phase, the direct effect of systolic backflow into the LA and subsequent volume overload leads to compensatory LA and LV dilation.12 Over time, there is decompensation leading to both LV systolic and diastolic dysfunction and reduced LA compliance. This causes elevated LA pressure and increases pulmonary capillary wedge pressure1 causing postcapillary PHT. This may develop before patients experience symptoms or LV dysfunction.5 9
Prevalence and phenotype of PHT with MR
The prevalence of PHT complicating significant MR remains unclear with the rate thought to be tied to the grade of MR.12 Prevalence increases with the presence of symptoms and LV systolic dysfunction, with rates as high as 64%23 reported in those with New York Heart Association function classes III and IV and symptoms compared with <20% in asymptomatic patients with severe MR and preserved EF.6 Significant PHT (eRVSP >50 mm Hg) was reported in 23% in a contemporary cohort of patients with severe degenerative MR.7 In our large, contemporary cohort of hospital-based and community-based patients, who underwent an echocardiogram, we confirm the high prevalence of PHT in patients with significant MR and preserved LVEF; 59.6% of patients had some degree of PHT as defined by clinical guidelines (mild—32.7%, moderate—16.4%, severe—10.5%). Patients with ‘borderline PHT’ (eRVSP 30–39 mm Hg) represented 30.5% of the cohort.
Prior studies have shown that increased age,7 female sex,24 increased E:e′,8 and larger LA size7 8 24 are all independent predictors of raised pulmonary pressures in patients with significant MR. We confirmed this echocardiographic phenotype in our cohort and reported progressively higher proportions of RV dilation and dysfunction as PHT worsens. While there is a close relationship between PHT and both mitral stenosis25 and LV systolic dysfunction,12 the prospective exclusion of these patients from our cohort allows a greater understanding of the impact of PHT per se in patients with MR with preserved EF. A comprehensive understanding of this echocardiographic phenotype is important as it provides clinicians with an easily accessible, non-invasive method to monitor specific parameters associated with worsening PHT and thus prognosticate these patients more accurately.
Outcomes of PHT in patients with MR
The presence of PHT negatively impacts outcomes with previous studies reporting increased postoperative heart failure,23 worse LV systolic dysfunction26 27 and poorer survival7 28 in patients with preoperative PHT compared with those without. Our much larger study confirms the serious impact of PHT on patients with significant MR, even in the absence of LV systolic dysfunction, with 59.6% of patients with eRVSP >40.00 mm Hg having a 1.20- to 2.86-fold adjusted increased risk of long-term all-cause mortality (dependent on PHT severity) compared with those with no PHT. Similar to our previous studies,14 29 we find that even ‘borderline’ PHT (eRVSP30.00–39.99 mm Hg) confers an increased risk of all-cause mortality compared with those with normal eRVSP. This was evident in the short term, with 1-year actuarial mortality increasing 1.14-fold, and, in the long-term, with all-cause mortality risk increasing 1.20-fold. Furthermore, the large numbers provided by the NEDA allowed us to identify an inflection point for excess mortality risk, at eRVSP >34.00 mm Hg. These results were independent of age and gender and did not appear to be confounded by the presence of concomitant valvular pathology including moderate or greater AR or severe AS.
Clinical implications
Current clinical guidelines include the presence of significant PHT (eRSVP >50 mm Hg, confirmed on right heart catheterisation) as an indication for the operative management in asymptomatic patients with severe MR.30 Prior studies have shown that ‘early’ MV repair in asymptomatic patients with severe MR and normal LVEF leads to improvements in long-term mortality and HF hospitalisation.31 Furthermore, while there is a decrease in pulmonary pressures post-intervention, a significant degree of PHT remains despite amelioration of the valvular pathology.23 28 While we do not report on treatment effect, we demonstrate that even minor elevations in pulmonary pressures are associated with negative prognostic implications. With no specific medical therapy approved for PHT in the setting of MR, further studies will be needed to determine whether early mitral valve intervention might improve outcomes in those patients with MR with early stages of PHT or perhaps even before it develops.1
Limitations
NEDA provides detailed echocardiographic data and linkage to mortality, and NEDA does not (yet) provide granular clinical data such as symptoms, comorbidities or pharmacological treatments. Most patients included in the database have undergone an echocardiogram for investigation of confirmed or suspected cardiac disease and should not be taken to reflect the population prevalence.
As noted in our previous studies,14 the data concerning PHT in NEDA are based on echocardiography-based measures, rather than haemodynamic assessment at right heart catheterisation. Prior studies have correlated eRVSP with invasive pulmonary artery systolic pressure,19 32 33 supporting the broad validity of our approach. Furthermore, echocardiography remains the the most common screening tool to detect PHT and is the guideline-recommended diagnostic method of choice, to allow for monitoring and follow-up. We acknowledge that the definitive diagnosis of PHT and its underlying aetiology (precapillary vs postcapillary vs combined) should generally be confirmed on right heart catheterisation, after initial screening is suggestive of PHT. We also note that the absence of a tricuspid regurgitation jet does not preclude the presence of PHT and there may be a number of patients with MR and PHT who were not included in the study due to the lack of correct tricuspid regurgitant (TR) sampling or no quantifiable TR. Hence, both the prevalence and prognostic impacts reported in this cohort should be interpreted as the minimum indicative values, from an epidemiological standpoint.
These studies were primarily derived from specialist centres or clinics across Australia, so some caution should be applied when applying these findings to other populations. However, Australia is a diverse and multiethnic population with universal health coverage aspects captured within the NEDA database. Finally, our data are lacking in quantitative measures of MR or RV dysfunction, a reflection of real-world echocardiographic practices in Australia. We were also unable to ascertain the underlying aetiology of the MR, so could not definitively differentiate between the primary versus secondary MR. However, patients with reduced LVEF were prospectively excluded, thus, our cohort likely represents a combination of patients with primary MR and atrial functional MR.
Conclusion
This is the largest series of adults to characterise the close, but incompletely understood, relationship between significant MR and complicating PHT. In patients with moderate or greater MR and preserved LV systolic function, mortality increases progressively as PHT becomes more severe from an eRSVP 34 mm Hg onwards.
Acknowledgments
We would like to thank all the NEDA centres and their patients for contributing to these data.
Footnotes
Twitter: @PlayfordDavid
Contributors: GS and DP conceived and designed the NEDA Study. SR and DSC conceived this analysis and conducted study analyses, and all authors contributed to the interpretation of study data. SR and DSC wrote the manuscript, and all authors contributed to its revision. GS and DP are the guarantors of the overall veracity and accuracy of NEDA data presented in this manuscript.
Funding: This research did not receive any specific grants from funding agencies in the public, commercial, or not for profit sectors. However, NEDA has received investigator initiated funding support from Janssen, Novartis Pharmaceuticals and Edwards Lifesciences in the past 3 years. SR is supported by the Heart Research Institute Australia, Emerging Cardiovascular Researcher Education Scholarship. Both NEDA (grant 1055214) and SS (grant 11358940) are supported by the National Health and Medical Research Council of Australia.
Competing interests: SS, DP and GS have previously received consultancy/speaking fees from Edwards Lifesciences. DP and GS have received consultancy fees from Medtronic, Edwards Lifesciences, Abbott Laboratories and ECHO IQ Pty Ltd.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics approval
This study involves human participants and was approved by Sydney Local Health District Human Research Ethics Committee, protocol X15-0387 and 2019/ETH069899. A retrospective waiver of consent was obtained.
References
- 1.Patel H, Desai M, Tuzcu EM, et al. Pulmonary hypertension in mitral regurgitation. J Am Heart Assoc 2014;3:e000748. 10.1161/JAHA.113.000748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iung B, Baron G, Butchart EG, et al. A prospective survey of patients with valvular heart disease in Europe: the Euro heart survey on valvular heart disease. Eur Heart J 2003;24:1231–43. 10.1016/s0195-668x(03)00201-x [DOI] [PubMed] [Google Scholar]
- 3.Gammie JS, Chikwe J, Badhwar V, et al. Isolated mitral valve surgery: the society of thoracic surgeons adult cardiac surgery database analysis. Ann Thorac Surg 2018;106:716–27. 10.1016/j.athoracsur.2018.03.086 [DOI] [PubMed] [Google Scholar]
- 4.Galusko V, Sekar B, Ricci F, et al. Mitral regurgitation management: a systematic review of clinical practice guidelines and recommendations. Eur Heart J Qual Care Clin Outcomes 2022;8:481–95. 10.1093/ehjqcco/qcab082 [DOI] [PubMed] [Google Scholar]
- 5.Alexopoulos D, Lazzam C, Borrico S, et al. Isolated chronic mitral regurgitation with preserved systolic left ventricular function and severe pulmonary hypertension. J Am Coll Cardiol 1989;14:319–22. 10.1016/0735-1097(89)90180-0 [DOI] [PubMed] [Google Scholar]
- 6.Kusunose K, Popović ZB, Motoki H, et al. Prognostic significance of exercise induced right ventricular dysfunction in asymptomatic degenerative mitral regurgitation. Circ: Cardiovascular Imaging 2013;6:167–76. 10.1161/CIRCIMAGING.112.000162 [DOI] [PubMed] [Google Scholar]
- 7.Barbieri A, Bursi F, Grigioni F, et al. Prognostic and therapeutic implications of pulmonary hypertension complicating degenerative mitral regurgitation due to flail leaflet: a multicenter long-term international study. Eur Heart J 2011;32:751–9. 10.1093/eurheartj/ehq294 [DOI] [PubMed] [Google Scholar]
- 8.Le Tourneau T, Richardson M, Juthier F, et al. Echocardiography predictors and Prognostic value of pulmonary artery systolic pressure in chronic organic mitral regurgitation. Heart 2010;96:1311–7. 10.1136/hrt.2009.186486 [DOI] [PubMed] [Google Scholar]
- 9.Vachiéry J-L, Tedford RJ, Rosenkranz S, et al. Pulmonary hypertension due to left heart disease. Eur Respir J 2019;53:1801897. 10.1183/13993003.01897-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strange G, Playford D, Stewart S, et al. Pulmonary hypertension: prevalence and mortality in the Armadale echocardiography cohort. Heart 2012;98:1805–11. 10.1136/heartjnl-2012-301992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosenkranz S, Gibbs JSR, Wachter R, et al. Left ventricular heart failure and pulmonary hypertension. Eur Heart J 2016;37:942–54. 10.1093/eurheartj/ehv512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maeder MT, Weber L, Buser M, et al. Pulmonary hypertension in aortic and mitral valve disease. Front Cardiovasc Med 2018;5:40. 10.3389/fcvm.2018.00040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Strange G, Celermajer DS, Marwick T, et al. The National echocardiography database Australia (NEDA): rationale and methodology. Am Heart J 2018;204:186–9. 10.1016/j.ahj.2018.07.001 [DOI] [PubMed] [Google Scholar]
- 14.Strange G, Stewart S, Celermajer DS, et al. Threshold of pulmonary hypertension associated with increased mortality. J Am Coll Cardiol 2019;73:2660–72. 10.1016/j.jacc.2019.03.482 [DOI] [PubMed] [Google Scholar]
- 15.Strange G, Stewart S, Celermajer D, et al. Poor long-term survival in patients with moderate aortic stenosis. J Am Coll Cardiol 2019;74:1851–63. 10.1016/j.jacc.2019.08.004 [DOI] [PubMed] [Google Scholar]
- 16.Ratwatte S, Stewart S, Strange G, et al. Prevalence of pulmonary hypertension in aortic stenosis and its influence on outcomes. Heart 2023. 10.1136/heartjnl-2022-322184 [DOI] [PubMed] [Google Scholar]
- 17.Ratwatte S, Playford D, Stewart S, et al. Prevalence of pulmonary hypertension in aortic regurgitation and its influence on outcomes. Heart 2023. 10.1136/heartjnl-2022-322187 [DOI] [PubMed] [Google Scholar]
- 18.Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the American society of echocardiography developed in collaboration with the society for cardiovascular magnetic resonance. J Am Soc Echocardiogr 2017;30:303–71. 10.1016/j.echo.2017.01.007 [DOI] [PubMed] [Google Scholar]
- 19.Currie PJ, Seward JB, Chan KL, et al. Continuous wave doppler determination of right ventricular pressure: a simultaneous Dopplercatheterization study in 127 patients. J Am Coll Cardiol 1985;6:750–6. 10.1016/s0735-1097(85)80477-0 [DOI] [PubMed] [Google Scholar]
- 20.G N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the joint task force for the diagnosis and treatment of pulmonary hypertension of the European society of cardiology (ESC). Eur Heart J 2016;37:67–119. 10.1093/eurheartj/ehv317 [DOI] [PubMed] [Google Scholar]
- 21.Maron BA, Hess E, Maddox TM, et al. Association of borderline pulmonary hypertension with mortality and hospitalization in a large patient cohort: insights from the veterans affairs clinical assessment reporting, and tracking program. Circulation 2016;133:1240–8. 10.1161/CIRCULATIONAHA.115.020207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kolte D, Lakshmanan S, Jankowich MD, et al. Mild pulmonary hypertension is associated with increased mortality: a systematic review and meta-analysis. J Am Heart Assoc 2018;7:e009729. 10.1161/JAHA.118.009729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ghoreishi M, Evans CF, DeFilippi CR, et al. Pulmonary hypertension adversely affects Short- and long-term survival after mitral valve operation for mitral regurgitation: implications for timing of surgery. J Thorac Cardiovasc Surg 2011;142:1439–52. 10.1016/j.jtcvs.2011.08.030 [DOI] [PubMed] [Google Scholar]
- 24.Mentias A, Patel K, Patel H, et al. Effect of pulmonary vascular pressures on long-term outcome in patients with primary mitral regurgitation. J Am Coll Cardiol 2016;67:2952–61. 10.1016/j.jacc.2016.03.589 [DOI] [PubMed] [Google Scholar]
- 25.Humbert M, Kovacs M, Hoeper M, et al. 2022 ESC/ERS endorsed by the International society for heart and lung transplantation (ISHLT) and the European reference network on rare respiratory diseases. guidelines for the diagnosis and treatment of pulmonary hypertension: developed by the task force for the diagnosis and treatment of pulmonary hypertension of the European society of cardiology (ESC) and the European respiratory society (ERS). Eur Heart J 2022. 10.1183/13993003.00879-2022 [DOI] [PubMed] [Google Scholar]
- 26.Yang H, Davidson WR, Chambers CE, et al. Preoperative pulmonary hypertension is associated with postoperative left ventricular dysfunction in chronic organic mitral regurgitation: an Echocardiographic and hemodynamic study. J Am Soc Echocardiogr 2006;19:1051–5. 10.1016/j.echo.2006.03.016 [DOI] [PubMed] [Google Scholar]
- 27.Baskett RJF, Exner DV, Hirsch GM, et al. Mitral insufficiency and morbidity and mortality in left ventricular dysfunction. Can J Cardiol 2007;23:797–800. 10.1016/s0828-282x(07)70830-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Collins N, Sugito S, Davies A, et al. Prevalence and survival associated with pulmonary hypertension after mitral valve replacement: national echocardiography database of Australia study. Pulm Circ 2022;12:e12140. 10.1002/pul2.12140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stewart S, Chan Y-K, Playford D, et al. Mild pulmonary hypertension and premature mortality among 154, 956 men and women undergoing routine echocardiography. Eur Respir J 2022;59:2100832. 10.1183/13993003.00832-2021 [DOI] [PubMed] [Google Scholar]
- 30.Vahanian A, Beyersdorf F, Praz F, et al. ESC/EACTS Scientific Document Group, ESC National Cardiac Societies, 2021 ESC/EACTS Guidelines for the Management of Valvular Heart Disease: developed by the Task Force for the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic surgery (EACTS). Eur Heart J 2022;43:561–632. 10.1093/eurheartj/ehab395 [DOI] [PubMed] [Google Scholar]
- 31.Kang D-H, Kim JH, Rim JH, et al. Comparison of early surgery versus conventional treatment in asymptomatic severe mitral regurgitation. Circulation 2009;119:797–804. 10.1161/CIRCULATIONAHA.108.802314 [DOI] [PubMed] [Google Scholar]
- 32.Chemla D, Castelain V, Humbert M, et al. New formula for predicting mean pulmonary artery pressure using systolic pulmonary artery pressure. Chest 2004;126:1313–7. 10.1378/chest.126.4.1313 [DOI] [PubMed] [Google Scholar]
- 33.Lam CSP, Borlaug BA, Kane GC, et al. Age-associated increases in pulmonary artery systolic pressure in the general population. Circulation 2009;119:2663–70. 10.1161/CIRCULATIONAHA.108.838698 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
openhrt-2023-002268supp001.pdf (72.2KB, pdf)
Data Availability Statement
Data are available on reasonable request.