Abstract
BACKGROUND:
Although allergy to tree nuts is often considered a single entity, there is heterogeneity in patient reactivity and immune response to different tree nuts.
OBJECTIVE:
We sought to characterize tree nut oral food challenges (OFCs) in a pediatric population performed at a single center over a 12-year period and determine differences in OFC outcome to different tree nuts.
METHODS:
A retrospective chart review was conducted in patients (0–20 years) who completed an unblinded OFC to any tree nut from 2007 to 2019 at Lurie Chlildren’s Hospital of Chicago. Differences among almond, cashew, hazelnut, and walnut challenges were compared, and probability curves were used to estimate positive predictive values (PPVs) of specific IgE at OFC.
RESULTS:
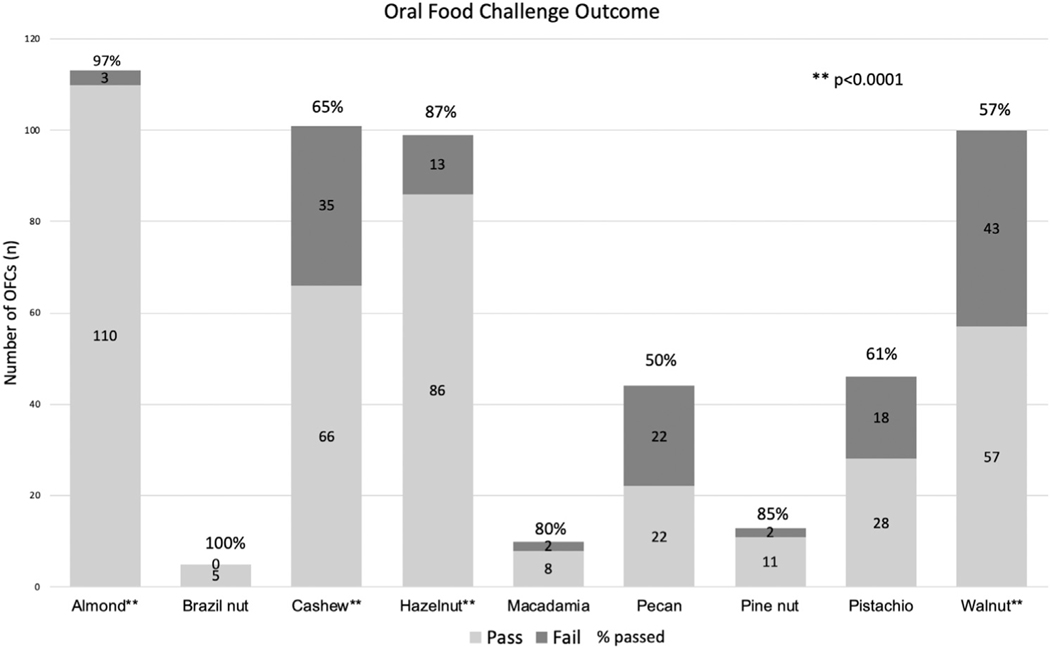
A total of 531 tree nut OFCs were included. The mean age at OFC was 7.77 years (standard deviation, 4.33). Overall, 74.0% of children passed clinically indicated OFCs. Of the 4 most commonly challenged tree nuts, almost all patients passed OFC to almond (97.3%) and hazelnut (87.9%). Pass rates were lower for cashew (65.3%) and walnut (57.0%), P < .0001. The odds of failure were 0.83 times lower for patients who were avoiding without a previous reaction compared with those who had previously reacted (P = .0025).
CONCLUSIONS:
The majority of patients pass low-risk almond and hazelnut OFCs. PPVs at the 50th percentile for walnut (2.84 kU/L) and cashew (3.35 kU/L) were lower than those previous studies have suggested.
Keywords: Food allergy, Tree nuts, Oral food challenges, Predictive value, Serum-specific IgE, Diagnosis
A tree nut is botanically defined as a dried fruit, sometimes referred to as the seed, with an inedible hard shell. The 9 most common tree nuts include almond, brazil nut, cashew, hazelnut, macadamia, pecan, pine nut, pistachio, and walnut.1 Although tree nuts are noted for being nutrient dense and provide various health benefits, they are common food allergens.1,2 In a cross-sectional survey administered from 2009 to 2010, approximately 1% of children in the United States were reported to have a tree nut allergy.2 Furthermore, children with an IgE-mediated tree nut or peanut allergy had a higher likelihood of having a severe reaction than children with other food allergies.2
Current methods of tree nut allergy diagnosis use a combination of clinical history, serum-specific IgE (sIgE), skin prick testing (SPT), and oral food challenges (OFCs).3 Although OFCs remain the gold standard for diagnosis, they are time-consuming and present inherent and potentially dangerous risk of anaphylaxis.4 When evaluating patients for tree nut allergy, sIgE and SPT assist in determining the need for an OFC to confirm the diagnosis.5 A 2006 study determined that for cashew, hazelnut, and walnut, an SPT ≥8 mm had a >95% accuracy for predicting a positive food challenge.6 Positive predictive values (PPVs) of SPT for almond, pistachio, pecan, and brazil nut have not been defined. Negative predictive values (NPVs) of SPT <3 mm are shown to be reliable indicators of excluding the allergy for all tree nuts.5 Along with SPT, sIgE can also guide clinical decisions around challenging a patient. Although diagnostic decision points with high PPVs and NPVs have been suggested for some common food allergens such as milk, egg, and peanut, widely accepted cutoffs have not been determined for tree nuts.7 A peanut and tree nut study from the United Kingdom reported that walnut sIgE ≥15 kU/L had a PPV of 99% and hazelnut sIgE <0.35 kU/L had an NPV of 95%, providing a preliminary threshold for further testing.8 Furthermore, sIgE predictive values may indicate the likelihood of a reaction, but cannot predict the severity of the reaction.5
Historically, tree nut allergy has been treated as 1 entity. Although concordance between specific nuts (eg, walnut and pecan, 0.96; cashew and pistachio, 0.95; and almond and hazelnut, 0.84)5 has been shown, little is known regarding differences between tree nut allergenicity and decision point thresholds for challenging individual tree nuts. Determining predictive sIgE levels for passing or failing a challenge for individual tree nuts would provide further nuance to guide clinicians regarding OFCs for specific nuts. This will help minimize the risk associated with food challenges, limit excessive dietary restrictions, lifestyle changes, and possible financial demands for families and the health care system. Also, providing evidence that specific tree nuts have different potential cutoffs from peanut and from other tree nuts suggest the need for further characterization of storage proteins or other nut components that make one nut more allergenic than another. Thus, we sought to characterize the differences in tree nut sIgE for almond, cashew, walnut, and hazelnut between those who passed and those who failed their OFCs.
METHODS
Study design
An institutional review board—approved retrospective chart review was conducted in children (0–20 years) who completed an unblinded standard of care OFC to any tree nut (almond, brazil nut, cashew, hazelnut, macadamia, pecan, pine nut, pistachio, and walnut) from 2007 to 2019 at Ann & Robert H. Lurie Children’s Hospital of Chicago. Patients were offered food challenges at the discretion of the treating provider to definitively diagnose food allergy or natural tolerance, as part of routine clinical care. In general, food challenges are offered in several scenarios such as suspected ingestion and subsequent reaction; negative testing with a history of reaction; or positive testing with a questionable reaction or history of tolerating the food. Challenges were typically offered when there was at least a 50% likelihood of passing the food challenge, often using an sIgE of 6 kU/L. Of note, these were clinically indicated food challenges performed for routine care (and not for the sake of research). The challenges were exclusively performed in an outpatient setting. Outpatient clinics are located throughout both city and suburban locations. All providers are trained and comfortable treating anaphylaxis.
Open OFCs were performed in a graded fashion, and a total goal dose of 6 to 8 g of tree nut protein was divided and administered in increasing doses with a 2-hour observation after the last dose. Dose preparation was standardized across food challenges. Clinicians provided recipes or food options for families to bring to the food challenge. Nurse protocols are standardized with 4 to 5 step dose escalations given in a graded fashion (typically 10%, 20%, 30%, and 40% of the total serving) as tolerated in 15-minute intervals. The goal dose is an age appropriate serving size. Resolution was determined when patients were able to tolerate 6 to 8 g of the nut protein. Challenge outcomes were determined as pass, fail, or inconclusive by the provider performing the challenge at the time of challenge.
To declare a failed OFC, objective symptoms observed by the provider were required. Food challenges were considered inconclusive if families chose not to proceed when the patient presented with only subjective symptoms. Based off of clinician notes, we determined a score based on the number of organ systems involved and objectivity of symptoms. Objective symptoms included urticarial lesions/hives, rash, sneezing, nasal congestion, rhinorrhea, emesis/diarrhea, and cough/wheeze. Subjective symptoms included abdominal pain, nausea, change in behavior, and distress. Challenges with subjective symptoms only were considered inconclusive and were excluded from the analysis.
Demographic data, personal and family history of atopy, details of previous reactions, sIgE levels to tree nuts, and SPT were also collected.
Skin prick testing.
SPT was performed using a bifurcated needle with Greer (Cambridge, Mass) food allergen extracts. An SPT was considered positive if the wheal diameter was 3 mm greater than the negative control. In the case of multiple SPTs, the first recorded patient SPT results on file were used for statistical analysis.
sIgE testing.
sIgE testing was performed using the Immunocap fluorescence enzyme immunoassay (Phadia Immunocap, Uppsala, Sweden). Any IgE levels reported as more than 100 kU/L were analyzed as 100.1 kU/L, less than 0.35 kU/L as 0.34 kU/L, and less than 0.1 kU/L as 0.09 kU/L. The first recorded sIgE on file was used as the sIgE at diagnosis. The most recent sIgE to the time of the challenge was used as sIgE at challenge. sIgE testing (and not SPT) was performed routinely at the time of OFC.
Statistical methods
For statistical analyses, only almond, cashew, hazelnut, and walnut were used as our power calculations suggested that we did not have sufficient numbers of brazil nut, macadamia, pine nut, pecan, and pistachio challenges to make meaningful conclusions. Using standard deviation (SD) estimates derived from Fleischer et al9 and using a type 1 error rate of 0.05, our power calculations suggested that we needed approximately 100 challenges per nut to detect a significant difference. To compare demographic variables, the reported P values are type III P values from generalized estimating equation models with repeated measures where challenge status (pass/fail) was used as the outcome.
Within the subset of food challenges that were either almond, cashew, hazelnut, or walnut, descriptive statistics were calculated for type of food challenge by challenge outcome (pass/fail). A generalized estimating equation model with repeated measures was fit to assess the association between the predictor of food type and the outcome of challenge status.
Within each subset of tree nut, the box plot distributions used median (interquartile range [IQR]) and are reported for IgE at OFC, IgE at diagnosis, and SPT. There were 4 patients who had multiple walnut challenges. For these 4 individuals, their most recent walnut challenge was used. Wilcoxon rank sum tests were then used to assess the association between each measure (IgE at OFC, IgE at diagnosis, SPT) and challenge outcome (if passed/failed). Within the subset of observations where food challenges were either from almond, cashew, hazelnut, or walnut, receiver operating characteristic (ROC) curves were created for 3 models: IgE at OFC predicting a failed challenge, IgE at Dx predicting a failed challenge, and SPT predicting a failed challenge. Each ROC curve was created using the predicted probability values generated from Generalize Estimating Equation (GEE) models with repeated measures. In addition, within the subset of observations from each individual nut (almond, cashew, hazelnut, or walnut), ROC curves were created from a logistic regression model with the challenge result as the outcome and IgE at OFC as the predictor. Again, for the 4 patients who had multiple challenges, only their most recent walnut challenge was used.
Within the subset of failed food challenges that were either almond, cashew, hazelnut, or walnut, descriptive statistics were calculated for type of food challenge by epinephrine requirement status. To assess this association, generalized estimating equations models with repeated measures were used. Type III P value is reported.
Within the subset of failed challenges, descriptive statistics of allergic comorbidities were reported by epinephrine requirement status. To assess these associations, generalized estimating equation models with repeated measures were used. Type III P values are reported.
RESULTS
Overall, 531 tree nut (almond, brazil nut, cashew, hazelnut, macadamia, pecan, pine nut, pistachio, and walnut) challenges were reviewed and analyzed. The population was pediatric with 98.5% of patients younger than 18 years (100% younger than 21 years) and a mean age of 7.78 (SD, 4.33) years. The study population was slightly more male than female patients (57.5% and 42.5%, respectively). Allergic comorbidities were common with nearly half of patients having eczema, 40.2% having wheezing or asthma, and over half (59.5%) with allergic rhinitis.
Of the total 531 tree nut OFCs reviewed, 74.0% passed and 26.0% failed. No significant difference in demographic characteristics was found when comparing challenges that were passed or failed. The demographic characteristics of each group are presented in Table I.
TABLE I.
Demographics and allergic diagnoses of the study population
| Level | Overall (n = 531) | Pass (n = 393) | Fail (n = 138) | P value |
|---|---|---|---|---|
|
| ||||
| Age at visit, mean (SD) | 7.78 (4.33) | 7.73 (4.33) | 7.92 (4.35) | .6714 |
| Sex, n (%) | ||||
| Female | 225 (42.5) | 164 (41.8) | 61 (44.5) | .6045 |
| Male | 304 (57.5) | 228 (58.2) | 76 (55.5) | |
| Race, n (%) | ||||
| Non-white | 177 (33.8) | 140 (36.1) | 37 (27.4) | .0630 |
| White | 346 (66.2) | 248 (63.9) | 98 (72.6) | |
| Eczema, n (%) | ||||
| No | 272 (51.8) | 195 (50.3) | 77 (56.2) | .2502 |
| Yes | 253 (48.2) | 193 (49.7) | 60 (43.8) | |
| Asthma, n (%) | ||||
| No asthma or wheezing | 313 (59.7) | 224 (57.9) | 89 (65.0) | .2560 |
| Asthma | 182 (34.7) | 139 (35.9) | 43 (31.4) | |
| Wheezing | 29 (5.5) | 24 (6.2) | 5 (3.6) | |
| Allergic rhinitis, n (%) | ||||
| No | 210 (40.1) | 152 (39.3) | 58 (42.3) | .5518 |
| Yes | 314 (59.9) | 235 (60.7) | 79 (57.7) | |
SD, Standard deviation.
Overall demographics of children (0–20 years) who completed an unblinded oral food challenge of any tree nut from 2007 to 2019 at Lurie Children’s Hospital, overall and by challenges that passed and failed. The P value compared children who passed to those that failed an oral food challenge. Frequency and percent are reported for all categorical variables, whereas mean (SD) are reported for numeric variables.
Almond, cashew, hazelnut, and walnut were used in the analyses as the number of challenges for the other nuts (brazil nut, macadamia, pine nut, pecan, and pistachio) was small. Approximately 100 challenges for each of the 4 tree nuts were reviewed to include in the analyses (Figure 1). A significant difference was found between pass and fail rates of the 4 different tree nuts (P < .0001, Table II). Most patients passed OFC to almond (97.3%), and walnut was the least likely OFC passed, although the majority still passed (57.0%).
FIGURE 1.
Oral food challenge (OFC) outcome for all tree nuts. Stacked bars represent the number of OFCs. The light stack represents passed challenges and the dark represents failed challenges. Percentages above the stack represent the pass rate for that tree nut. The P value indicates that there are significant differences in pass rates among the tree nuts.
TABLE II.
Tree nut challenge by outcome
| Tree nut | Pass (n = 319) | Fail (n = 94) | P value | |
|---|---|---|---|---|
|
| ||||
| Food (%) | Almond | 110 (97.3) | 3 (2.7) | <.0001 |
| Cashew | 66 (65.3) | 35 (34.7) | ||
| Hazelnut | 86 (87.9) | 13 (12.1) | ||
| Walnut | 57 (57.0) | 43 (43.0) | ||
| Overall | 319 (77.2) | 94 (22.8) | ||
Number (percent) of challenges passed and failed are shown for each nut. The percent represents the percent of challenges that passed out of the total number of challenges for a given tree nut. The global P value indicates that there is significance between pass and fail rates depending on which tree nut is challenged.
Using pairwise comparisons, we analyzed the odds ratio of passing 1 tree nut over another. Most patients did not have more than 1 challenge. Because a few patients had multiple challenges, our statistical analyses required generalized estimating equation models to appropriately take the repeated measures into account. We found that participants were most likely pass an almond challenge compared with any other tree nut, and less likely to pass a cashew or walnut challenge (Table III). Although there was significance between most pairs of tree nuts, there was no difference in pass rates between cashew and walnut (P = .25).
TABLE III.
Odds ratio of passing individual nut oral food challenges (OFCs)
| Comparison | Odds ratio | 95% confidence interval | P value |
|---|---|---|---|
|
| |||
| Almond vs cashew | 0.73 | 0.66, 0.80 | <.0001 |
| Almond vs hazelnut | 0.90 | 0.84, 0.96 | .0027 |
| Almond vs walnut | 0.67 | 0.60, 0.75 | <.0001 |
| Cashew vs hazelnut | 1.24 | 1.10, 1.39 | .0003 |
| Cashew vs walnut | 0.92 | 0.80, 1.06 | .2483 |
| Hazelnut vs walnut | 0.74 | 0.66, 0.84 | <.0001 |
Pairwise comparisons were performed between each possible pair of tree nuts. The odds ratio compares the chance of failing the OFC to the first nut with that to the second nut listed.
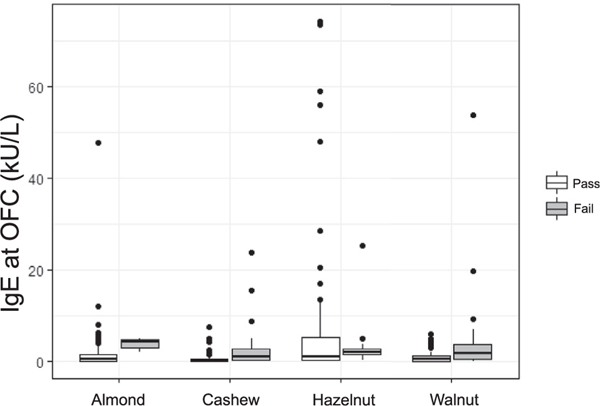
We next compared participants who passed or failed their tree nut OFC and found an association between sIgE at OFC for almond (P = .029), cashew (P = .011), and walnut (P = .0007). There was also an association between OFC outcome and sIgE at diagnosis for cashew (P = .0053) and walnut (P < .0001). In addition, an association between SPT at diagnosis and OFC outcomes was found for almond (P = .012), cashew (P = .0076), and walnut (P = .012). There was no association between diagnostic test results and outcome for the hazelnut challenges (Table IV).
TABLE IV.
Diagnostic test results: sIgE levels at OFC and diagnosis, SPTresults at diagnosis
| Almond | Cashew | Hazelnut | Walnut | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||||
| Pass (n = 110) | Fail (n = 3) | P value | Pass (n = 66) | Fail (n = 35) | P value | Pass (n = 86) | Fail (n = 13) | P value | Pass (n = 56) | Fail (n = 38) | P value | |
|
| ||||||||||||
| IgE at OFC (kU/L) | 0.70 [0.20, 1.70] | 4.46 [3.23, 4.73] | .0290 | 0.34 [0.11, 0.64] | 1.06 [0.26, 2.96] | .0108 | 1.00 [0.35, 5.46] | 2.10 [1.68, 2.97] | .2160 | 0.71 [0.15, 1.35] | 1.86 [0.64, 3.94] | .0007 |
| IgE at dx (kU/L) | 0.67 [0.20, 2.19] | 4.00 [3.00, 4.23] | .0562 | 0.37 [0.15, 0.97] | 1.14 [0.33, 3.25] | .0053 | 0.87 [0.33, 5.46] | 2.58 [1.68, 3.48] | .0582 | 0.35 [0.14, 1.29] | 2.41 [0.67, 3.64] | <.0001 |
| SPT at dx (mm) | 4.00 [2.75, 5.00] | 8.00 [7.00, 9.00] | .0122 | 3.00 [0.00, 5.00] | 6.00 [3.00, 8.00] | .0076 | 4.00 [1.50, 5.00] | 6.00 [3.00, 7.00] | .1403 | 3.00 [0.00, 4.00] | 4.00 [3.00, 6.00] | .0115 |
OFC, Oral food challenge; SPT, skin prick test; dx, diagnosis.
Allergy test results comparing participants who passed and failed challenges to almond, cashew, hazelnut, and walnut. Median (interquartile range) are represented in results.
The IQRs of sIgE at OFC for almond, cashew, hazelnut, and walnut were plotted with outliers (Figure 2). Patients who passed hazelnut challenges had IgE at OFC values with the largest range. Cashew and walnut appeared to have more narrow ranges for challenges that passed.
FIGURE 2.
Specific IgE at time of oral food challenge (OFC). White boxes represent passed OFCs; gray boxes represent failed OFCs. The line represents the median and boxes represent the 25th and 75th percentiles. Outliers are shown.
We compared epinephrine requirement for failed challenges among the 4 tree nuts and also separated by allergic comorbidities. We did not find a significant difference among conditions in either analysis (Tables E1 and E2, available in this article’s Online Repository at www.jaci-inpractice.org).
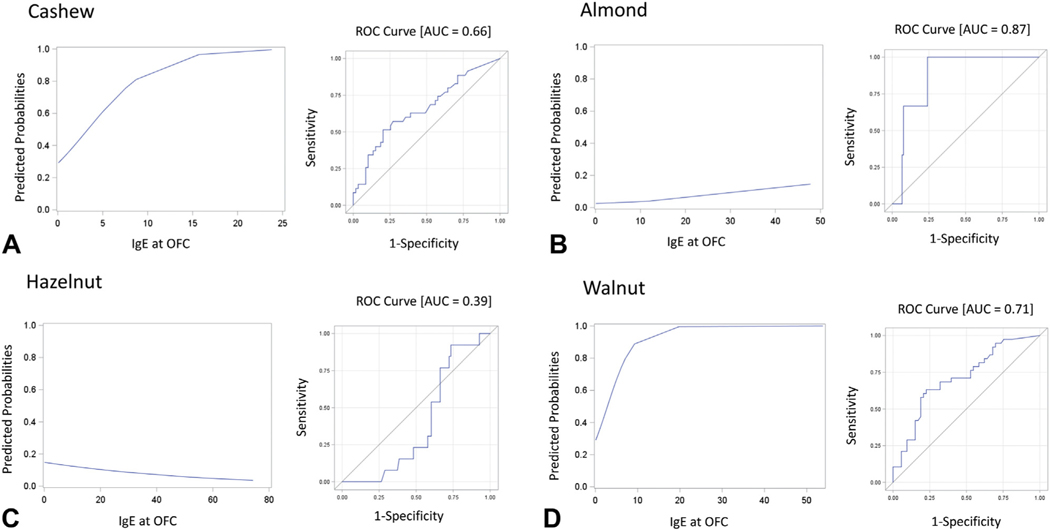
ROC analysis revealed that cashew (area under the curve [AUC], 0.66) and hazelnut (AUC, 0.39) IgE at OFC were poor predictors of failed challenge outcome (Figure 3, A and B). Although there is an association between IgE at OFC and failing an almond challenge (AUC, 0.87), the IgE at the estimated 95% predicted probability of challenge failure would be 167 kU/L (Table E3, available in this article’s Online Repository at www.jaci-inpractice.org), which is much higher than any of the observed almond IgE results in our population (Figure 3, C). This could be due to the small number of failed almond challenges used for the analysis (n = 3). We also found an association between IgE at OFC and failing a walnut challenge (AUC, 0.7; Figure 3, D). The IgE at the estimated 95% predicted probability of walnut challenge failure was slightly lower than 12 kU/L (Table E3, available in this article’s Online Repository at www.jaci-inpractice.org ). PPVs at the 50th percentile for the nuts are shown in Table V. As shown, for cashew and walnut, we further specified our analyses to determine PPVs separated by the reason for avoidance. “Prior ingestion” accounted for challenges performed after a known ingestion of the allergen. “Preventatively avoiding” accounted for challenges performed without a suspected ingestion, but had positive SPT or sIgE, indicating sensitivity to the specific tree nut allergen (Table V).
FIGURE 3.
Predicted probabilities and receiver operating characteristic (ROC) curves of IgE at oral food challenge (OFC) for cashew (A), hazelnut (B), almond (C), and walnut (D). AOC, Area under the curve.
TABLE V.
Predicted probabilities for failing a cashew or walnut challenge separated by reason for avoidance
| Prior ingestion | Preventatively avoiding | ||
|---|---|---|---|
|
|
|
||
| Tree nut | Predicted probability | Corresponding value of IgE at OFC | Corresponding value of IgE at OFC |
|
| |||
| Cashew | .25 | −1.67185 | 0.5040 |
| .50 | 0.82500 | 4.3765 | |
| .95 | 7.51691 | 14.7552 | |
| Walnut | .25 | −0.08492 | 0.3056 |
| .50 | 0.62607 | 3.4553 | |
| .95 | 2.53161 | 11.8969 | |
OFC, Oral food challenge.
DISCUSSION
As common food allergens, tree nut allergy affects 1% of all children in the United States.3 In addition, children with IgE-mediated nut allergy have been shown to have more severe reactions than those with other food allergies.3 Although OFCs remain the gold standard for food allergy diagnosis, there are various obstacles such as time, resources, and risk of a severe reaction. Thus, it is important to develop a clearer idea of the diagnostic utility and accuracy of SPTs and sIgE tests to help guide clinical decisions.
We performed an examination of over 500 OFCs characterizing the diagnostic testing for tree nut allergy and found that there were differences among tree nuts. Overall, 74.0% of children passed their OFC, and regarding the 4 most commonly challenged tree nuts (almond, cashew, hazelnut, and walnut), most patients passed OFC to almond (97.3%) and hazelnut (87.9%). Pass rates for cashew and walnut were significantly lower (P < .0003), that is, 65.3% and 57.0%, respectively. Comparing participants who passed or failed their tree nut OFC, we found an association between sIgE at OFC for almond (P = .029), cashew (P = .011), and walnut (P = .0007). Furthermore, the odds of failure were 0.83 times lower for patients who were preventatively avoiding compared with those who were not (P = .0025).
This study reviewed tree nut OFCs performed for standard clinical care. Therefore, oral challenges were performed to confirm or refute a diagnosis of food allergy, or to determine the development of natural tolerance. Fleischer et al9 suggested that in children >5 years of age, an sIgE value of <5 kU/L conferred a 58% chance of passing the challenge. In our study, 459 of 531 challenges (86.4%) had an sIgE <5 kU/L at OFC. Looking at only those OFCs with a tree nut sIgE <5 kU/L, 335 of 459 challenges (73.0%) passed. In a tree nut study conducted by Couch et al,10 76% of 67 tree nut OFCs passed, even as most challenges took place with the recent SPT wheal size <3 mm and/or sIgE <2 kU/L and the median sIgE of the passed challenges was 0.35 kU/L (mean sIgE, 0.99 kU/L). Thus, our study had a higher median sIgE of 0.61 kU/L (mean, 2.56 kU/L) than the Couch study, with a similar pass rate; and a higher pass rate than the Fleischer study.
Although using the overall threshold of 5 kU/L shows a high pass rate, our study sought to determine differences between individual tree nuts. Overall, we found that patients challenged to almond or hazelnut were likely to pass, with 97.3% of almond and 87.9% of hazelnut challenges passing. This was similar to results found in Couch’s study where 100% of almond challenges and 83% of hazelnut challenges passed—the highest pass rates out of the nuts they examined.10 Of all 9 tree nuts that we included in our study, cashew and walnut accounted for the majority of reactions, similar to results found by Fleischer et al.9 These data suggest that pass rates may be different among the tree nuts. Therefore, we sought to examine differences among the tree nuts more closely.
Patients challenged to cashew and walnut passed with significantly lower rates (65.3% and 57.0%, respectively) as compared with almond and hazelnut (P < .0001). These data suggest that almond and hazelnut challenges may be able to be offered at higher sIgE levels than cashew and walnut. In addition, ROC analysis was done to determine the predictive strength of sIgE at OFC for failed challenges. The ROC curves revealed that almond (AUC, 0.87) and walnut (AUC, 0.71) IgE at OFC were acceptable predictors for failed challenge outcome. However, the calculated almond and walnut IgEs at the estimated 95% predicted probability, 167 and 12 kU/L, respectively, were much higher than those observed in our study population. For almond, this could be due to the high passing rate for almond challenges (97.3%). ROC analysis for cashew (AUC, 0.66) and hazelnut (AUC, 0.39) IgE at OFC were insufficient predictors of failed challenge outcome. Overall, the PPV at the 50th percentile was 3.35 kU/L for cashew and 2.84 kU/L for walnut.
On review of hazelnut OFCs, we found that 63.6% of our study population did not have birch sensitization testing. Of the 36.4% total subjects who did have birch testing, 66.7% tested positive to birch. Of those who passed the hazelnut OFC and were tested to birch (28 subjects), 67.9% were sensitized to birch (n = 19). Of those who failed the challenge and were tested to birch (8 subjects), 62.5% were sensitized to birch (n = 5). Although the numbers are small, this suggests that birch sensitization was common among all children who were tested, but sensitization rates did not differ between children who passed or failed their hazelnut OFC. The high rates of birch sensitization in both groups support the use of component testing for hazelnut in children. Larger studies are needed to confirm these observations.
Reason for avoidance also affected pass rates of tree nut OFC. “Prior ingestion” indicates children who were avoiding the nut because of prior symptoms on ingestion along with positive testing. “Preventative avoidance” is defined as avoiding the nut because of positive testing only (without prior ingestion) or allergy to another nut. Only cashew and walnut are compared for reason of avoidance because so few patients failed almond and hazelnut challenges; therefore, we had insufficient sample size to compare failed challenges for almond and hazelnut. When challenged after avoiding due to prior reaction (to that specific nut), the predicted probability at the 50th percentile was 0.83 kU/L for cashew and 0.63 kU/L for walnut (Table V). When challenged after preventative avoidance, the predicted probability at the 50th percentile was noticeably higher, with a corresponding sIgE of 4.38 kU/L for cashew and 3.46 kU/L for walnut. Furthermore, we found that the overall odds of failing a challenge are 0.83 times lower for those who were avoiding tree nuts due to sensitivity indicated by sIgE results of 1 or more other nuts (including peanut) compared with those who had a prior ingestion and subsequent reaction to the challenged nut (P = .0025). This suggests that those children preventatively avoiding tree nuts due to another nut allergy (including peanut or other tree nut) pass tree nut challenges at higher sIgE levels. In addition, Couch et al found that 91% (n = 42) of tree nut sensitized patients who were challenged after preventatively avoiding tree nuts passed their OFC, further supporting the claim that more aggressive use of OFCs in these patients should be considered.
The PPVs at the 50th percentile for cashew and walnut, not taking into consideration reason for avoidance, were 3.35 and 2.84 kU/L, respectively. Because both values fall within the range of observed sIgE at OFC of our study population, it is reasonable to use these 2 probabilities to assess clinical outcomes for failed OFCs. The PPV at the 50th percentile for almond was calculated to be 92.8 kU/L, which reflected the low fail rate we observed. For hazelnut, PPVs were unable to be attained by the statistical model because the values in its corresponding plot fell below a predicted probability of 0.2. Because of the inconclusive values derived for almond and hazelnut, it would be valuable to study a large cohort of almond and/or hazelnut sensitized patients challenged at a higher sIgE at OFC to develop a better model to estimate PPVs.
Along with analyzing sIgE of individual tree nuts, our study also reviewed epinephrine requirement for failed challenges among the different nuts. We found that epinephrine use for failed OFC was not significantly different based on the specific nut (P = .53). Because there is provider-based variability and subjectivity when epinephrine is used, epinephrine use was looked at independently from severity scoring.
Our study provides a real-world examination of people who get offered an OFC. Because of current clinical recommendations, challenges are only offered to patients who have a high likelihood of passing, meaning that sIgE at OFC and SPT are likely to be lower in our study population than if we had offered OFCs to all patients presenting with tree nut allergy. In addition, challenges are offered to and performed on food allergic or sensitized individuals and thus may not be generalizable to other populations. All challenges were open and not double blinded, which could make subjective failure a possibility and influence challenge results.
In conclusion, we have shown that differences exist among individual tree nuts. Most children pass almond and hazelnut OFCs even with sIgE at OFC over the current suggested decision point thresholds. Children who are avoiding tree nuts due to sensitization to 1 or more other nut are also more likely to pass their OFC compared with those who have had a prior ingestion and reaction. Although further work is needed on hazelnut and almond challenges to determine more clinically relevant PPVs, our data suggest that almond and hazelnut can be challenged more aggressively and cashew and walnut challenged more conservatively.
Supplementary Material
What is already known about this topic?
Tree nuts are common food allergens and have a higher likelihood of triggering a severe reaction compared with other food allergens. Little is known regarding differences between tree nut allergenicity and decision point thresholds for individual tree nuts.
What does this article add to our knowledge?
Patients are more likely to pass almond and hazelnut challenges than cashew or walnut.
How does this study impact current management guidelines?
Almond and hazelnut could be challenged more aggressively, and cashew and walnut challenged more conservatively.
Acknowledgments
This study was funded by NIAID K23 AI100995–03. Anonymous grant was provided to Northwestern Feinberg School of Medicine and University of Wisconsin-Madison.
Conflicts of interest:
A. M. Singh reports grants from NIH and grants from Northwestern University during the conduct of the study. M. Makhija reports research support from Aimmune Therapeutics, Regeneron Pharmaceuticals, and DBV Technologies.
Abbreviations used
- AUC
Area under the curve
- IQR
Interquartile range
- NPV
Negative predictive value
- OFC
Oral food challenge
- PPV
Positive predictive value
- ROC
Receiver operating characteristic
- sIgE
Serum allergen-specific IgE
- SPT
Skin prick test
Footnotes
The rest of the authors declare that they have no relevant conflicts of interest.
REFERENCES
- 1.Alsalvar C, Shahidi F. Tree nuts: composition, phytochemicals, and health effects. Boca Raton, FL: CRC Press; 2008. [Google Scholar]
- 2.Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics 2011;128:e9–17. [DOI] [PubMed] [Google Scholar]
- 3.Weinberger T, Sicherer S. Current perspectives on tree nut allergy: a review. J Asthma Allergy 2018;11:41–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perry TT, Matsui EC, Conover-Walker MK, Wood RA. Risk of oral food challenges. J Allergy Clin Immunol 2004;114:1164–8. [DOI] [PubMed] [Google Scholar]
- 5.Moloney JM, Rudengren M, Ahlstedy S, Bock SA, Sampson HA. The use of serum-specific IgE measurements for the diagnosis of peanut, tree nut, and seed allergy. J Allergy Clin Immunol 2008;122:145–51. [DOI] [PubMed] [Google Scholar]
- 6.Ho MH, Heine RG, Wong W, Hill DJ. Diagnostic accuracy of skin prick testing in children with tree nut allergy. J Allergy Clin Immunol 2006;117:1506–8. [DOI] [PubMed] [Google Scholar]
- 7.Branum AM, Lukacs SL. Food allergy among US children: trends in prevalence and hospitalizations. NCHS Data Brief 2008;10:1–8. [PubMed] [Google Scholar]
- 8.Steifel G, Anagnostous K, Boyle RJ, Brathwaite N, Ewan P, Fox AT, et al. BSACI guideline for the diagnosis and management of peanut and tree nut allergy. Clin Exp Allergy 2017;47:719–39. [DOI] [PubMed] [Google Scholar]
- 9.Fleischer DM, Conover-Walker MK, Matsui EC, Wood RA. The natural history of tree nut allergy. J Allergy Clin Immunol 2005;116:1087–93. [DOI] [PubMed] [Google Scholar]
- 10.Couch C, Franxman T, Greenhawt M. Characteristics of tree nut challenges in tree nut allergic and tree nut sensitized individuals. Ann Allergy Asthma Immunol 2017;118:591–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.