Abstract
Although significant progress has been made in achieving goals for COVID-19 vaccine access, the quest for equity and justice remains an unfinished agenda. Vaccine nationalism has prompted calls for new approaches to achieve equitable access and justice not only for vaccines but also for vaccination. This includes ensuring country and community participation in global discussions and that local needs to strengthen health systems, address issues related to social determinants of health, build trust and leverage acceptance to vaccines, are addressed. Regional vaccine technology and manufacturing hubs are promising approaches to address access challenges and must be integrated with efforts to ensure demand. The current situation underlines the need for access, demand and system strengthening to be addressed along with local priorities for justice to be achieved. Innovations to improve accountability and leverage existing platforms are also needed. Sustained political will and investment is required to ensure ongoing production of non-pandemic vaccines and sustained demand, particularly when perceived threat of disease appears to be waning. Several recommendations are made to govern towards justice including codesigning the path forward with low-income and middle-income countries; establishing stronger accountability measures; establishing dedicated groups to engage with countries and manufacturing hubs to ensure that the affordable supply and predictable demand are in balance; addressing country needs for health system strengthening through leveraging existing health and development platforms and delivering on product presentations informed by country needs. Even if difficult, we must converge on a definition of justice well in advance of the next pandemic.
Keywords: Vaccines, COVID-19, Immunisation, Public Health, Prevention strategies
Summary box.
Equitable COVID-19 vaccine access remains elusive; reviewing the COVID-19 vaccination effort through an access, equity and justice lens helps elucidate challenges and promising approaches for achieving ongoing and future pandemic goals.
Pandemic efforts should leverage and build on existing structures and improve outcomes for a more just and equitable approach to not only vaccine access but also vaccination.
In light of competing views on the approach for access, equity and justice, the global health community should come together with state actors, manufacturers and donors to cocreate strategies that ensure these principles for all; even if difficult, a definition of justice, in particular, needs to be agreed on prior to the next pandemic.
Achievement of justice will require self-reliance and regional manufacturing supplemented with efforts to ensure predictable demand, financing and political will to sustainably support operations provides a promising approach.
Global and local governance needs to be strengthened to ensure accountability for equitable access and vaccination at national and subnational levels for all countries.
Introduction
Vaccination can help prevent the illness and death, economic repercussions and social impact of COVID-19 and future variants. Yet, calls for global solidarity in ensuring equitable vaccine access were not initially heeded1 and as the WHO called for prioritising vaccine doses for the vulnerable and healthcare workers, the calls for solidarity continued to be ignored.2 COVID-19 Vaccines Global Access (COVAX), the partnership formed to achieve quick and equitable vaccine access, was successful in speeding up COVID-19 vaccine availability3 but fell woefully short in achieving even the mid-2022, 70% vaccination target set by WHO.1 In July 2022, WHO updated targets to ensure coverage of health workers, older adults and other high-risk populations.4 WHO has acknowledged that achievement of goals require strategies beyond supply-side approaches, noting enablers include new delivery strategies across the life course and sustained political will and investment.4 At the end of 2022, 69% of people globally had received a COVID-19 vaccine.5 In low and middle-income countries (LMICs), however, vaccination coverage only reached just under 25% of the population.5 Healthcare worker coverage varies significantly across countries, particularly in low-income settings.6 At the end of 2022, among the 34 countries for concerted support reported by the COVID-19 Vaccine Delivery Partnership, 40% of countries reported COVID-19 vaccination coverage among healthcare workers below 50%, and 80% of countries reported older adult coverage below this same threshold, including those where data were not reported.6
Although deaths and hospitalisations are down dramatically since the beginning of the pandemic, variants are still emerging and the quest for equitable vaccination coverage continues. A new XBB.1.5 omicron subvariant has now emerged and its ability to both evade the immune system and exhibit enhanced binding to the human ACE-2 receptor translates into a variant that according to WHO may represent the most transmissible to date. This means that the goalposts for vaccine equity may shift to require global booster doses using bivalent (original plus BA.4/BA.5) or even trivalent (targeting XBB.1.5) vaccines.7 Vaccination has still achieved meaningful success; models estimate the vaccine prevented nearly 20 million deaths between December 2020 and 2021.8 If low-income countries (LICs) had met WHO targets of vaccinating 20% and 40% of the by the end of December 2021, substantially more lives could have been saved.8 The impact of COVID-19 in LICs is more than cases and deaths of COVID-19. There have been significant disruptions to households and their overall health and economic well-being, health systems, education and economies.9 As resources in countries continue to be diverted to fight the pandemic and its after effects, particularly in unvaccinated or under vaccinated populations, the concern is that the detrimental health, economic and social impact may continue to rise and affect every part of the globe if we do not adjust our approach.
Access, equity and justice
At the height of the pandemic, a significant amount of attention was placed on equitable access. COVAX was designed to ensure that vaccines were developed rapidly and distributed equitably.10 How this aim is achieved is the subject of much discussion. There was grave concern that vaccine nationalism had taken hold, undermining the tenets of COVAX.11–13 This led to further calls for sharing of intellectual property, dismantling of global structures and development and manufacturing of vaccines at a country and regional level to address what has been coined as ‘vaccine apartheid’.2 14 15 Ethicists describe a moral duty for reparative justice and a move away from short-term fixes that do little to address the problem, such as donations that countries were unable to absorb.14 15 Local or regional manufacturing is consistent with principles of self-determination and participation that move away from the global structures and colonialism that plague LICs.16 The establishment of regional technology hubs may be a step in the right direction to reduce concerns about a lack of supply and reliance on donations that further vaccine hesitancy and do little for achieving the longer term goals of justice.14 17 To achieve a regional solution that promotes vaccine confidence, sustained political will on the part of the countries in the region, empowerment of LMIC producers independent of considerations of their economic or political situation, a strong commitment to quality and funding to support this effort will be needed to ensure vaccines are developed to consistently meet needs of the countries and regions (further discussed in other papers in this issue).18 19 Additionally, vaccine design and research should be conducted with the participation of the countries in the region.
Others, including those directly involved in COVAX, concur with the need for continuing improvements to ensure equity but focus on improving existing governance. Although the immediate concern of vaccine supply has passed, and COVAX has helped address equity disparities;20 longer term solutions are still needed, particularly if new, more deadly variants emerge and new vaccines are required.
Vaccines and vaccination
Donations, while welcomed, have been problematic for some countries, and as mentioned previously, may help in achieving shorter term equity goals. They do not advance longer term goals of justice, however. Donations do not always reach recipient countries when needed and the capacity to use these vaccines is diminished by short expiration dates21 22 and health systems that are still stretched.23 Demand for COVID-19 vaccines is waning and hesitancy still exists.24 25 With countries challenged by finances and wide variations in prices,25 some political leaders have moved on from the pandemic.26 Access to vaccines remains an important priority; but to ensure equity and justice, the focus needs to be on vaccination27 and engagement of communities to address the issues that are most relevant to them.16 Countries themselves have a responsibility for their own health systems, but there is also a role for the global community to facilitate action, particularly where health systems are weak28 and barriers such as food and housing insecurity, poor air quality, discrimination, lack of jobs and education and persistent healthcare access challenges affect health and willingness to be vaccinated.29 In LMICs, COVID-19 vaccine acceptance is generally high; however, this as well is under threat due to the globalisation of anti-vaccine activism from the USA and Europe.30 Therefore, prioritising access goes a long way along with messaging that deliberately reflects the specific needs and context of countries would help in building acceptance. Strong health systems and vaccination programmes grounded in the concerns of social determinants of health are at the core of achieving justice and equity.3 31
Supply and demand interrelationship
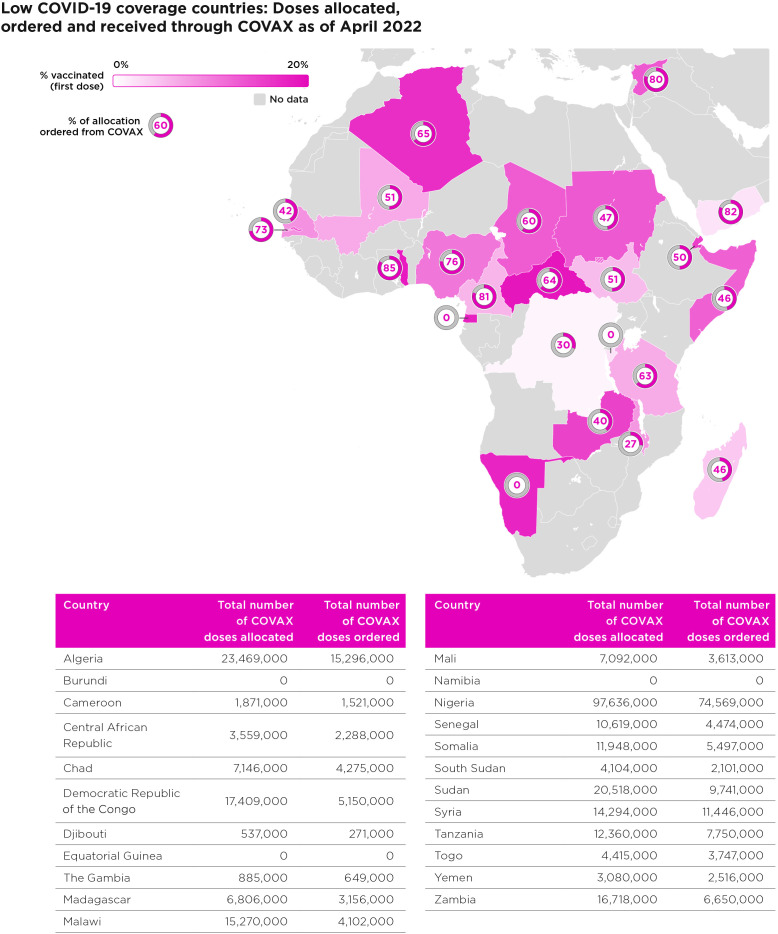
The inequitable distribution and access of vaccines has been attributed to a number of factors. Much of the debate to-date has centred on limited supply and inequitable distribution due to vaccine nationalism; limited vaccine manufacturing in LMICs; a lack of affordability and transparency around pricing.25 32 While all of these discussions have been happening, there have been efforts to ensure readiness; but stark realities of the need to engage countries have become more and more evident. WHO, UNICEF and other partners provide support, but it is clearly not enough. We have been here before with previous pandemics and risk history repeating itself where demand begins to wane just as supply becomes available.33 With calls for local manufacturing, there also should be plans to sustain newly installed vaccine manufacturing. Already, one manufacturing facility in Africa may close due to a lack of demand34 and Serum Institute of India and Bharat Biotech stopped their production.35 Countries with the lowest vaccination rates had not ordered their allocation of vaccine (figure 1). Getting the timing right for supply and demand is paramount. Unpredictable or waning demand will most certainly have an impact on the ability to keep manufacturing plants producing and a lack of demand has been problematic, not boding well for the future of regional manufacturing. Some countries may feel they are past the worst phase of the pandemic, which they are not seeing big surges of disease and can take other measures to control the pandemic or simply opt to wait for a better vaccine, we cannot risk countries or the global community moving on to other priorities, particularly as the risk of new variants has not passed.26 We need open and honest dialogue about the expectations for the way forward to ensure that when manufacturers finally have the vaccines, supply does not become short-dated or discarded.
Figure 1.
COVID-19 vaccine allocation and orders in low-income countries. Excler et al.46 Sources: Our World in Data;47 UNICEF supply division COVID-19 vaccine market dashboard.48
Lack of demand is just as important to address as lack of supply. In Africa, from 2022 onwards, the biggest concern was not supply, but demand-related factors.36 African leaders have the solutions and have outlined a variety actions to improve accountability, sharing of information, engagement and addressing access obstacles in a more human centred way, leveraging existing platforms such as the US President’s Plan for AIDS Relief (PEPFAR) and Malaria Initiative36 or the Global Fund. Perceptions about both the disease and vaccines in the context of the local situation to be addressed while continuing the commitment to obtain supply.36
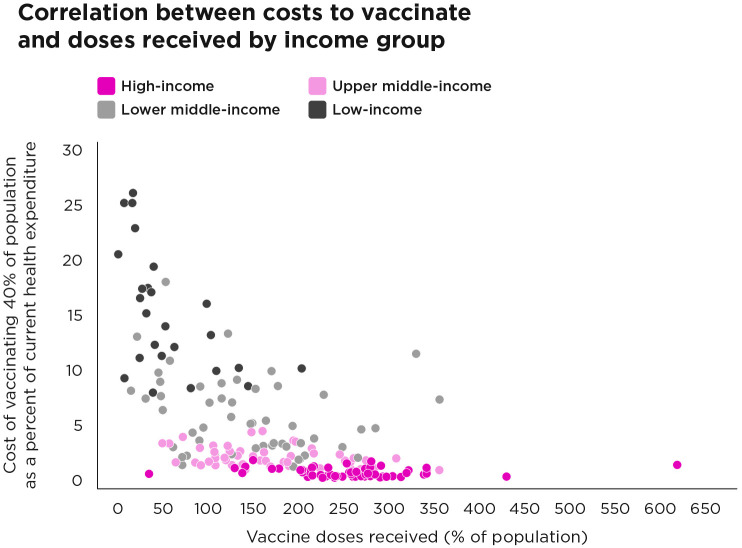
Some low-vaccination countries, including Democratic Republic of Congo (DRC), Madagascar and South Sudan would require nearly 25% of their total health expenditure to vaccinate 40% of their citizens (figure 2) and a UNDP/WHO/UNICEF survey of countries reports over 56% increase in expenditures needed to meet the 70% vaccination goal.37 Many of the same countries have relatively low reported case counts and deaths, contributing to a perception of little disease.37 It is not simply a lack of planning. In DRC, for example, there have been efforts to engage the community, combat misinformation and keep vaccination centres open. Challenges of other diseases such as Ebola and malaria, a health system that is underresourced, healthworkers who are overworked and underpaid, and systemic issues of violence and mistrust in government, however, have limited the amount of progress that can be made in a short period of time.38 Increased assistance is needed to address urgent country priorities in addition to access to vaccines in countries struggling to protect their populations and is all parts of achieving justice.
Figure 2.
Costs to vaccinate and vaccine access by income group. Excler et al.46 Adapted from UNDP Equity Dashboard.37
Health system capacity and acceptance of vaccine are also important factors influencing uptake of vaccine and more attention is needed to ensure that the subnational variations are addressed.25 32 Additionally, specific populations, including older adults, migrant workers and refugees, irrespective of their legal status and others, necessitate different delivery strategies. Few countries, for example, have vaccination programmes for older adults, who may be less willing to attend vaccination centres or have other specific concerns that lead to vaccine hesitancy. Addressing the needs of this population requires advance planning and engagement with a coalition of partners who have interest in healthy ageing and understand the unique concerns of this community39 A more organised global effort, including a wide variety of country stakeholders who can identify relevant platforms and help build political will, is needed as well as partners on the ground that can complement the activities of WHO and UNICEF whose focus is largely on younger age groups.39
Global and local trust
Research has shown that a globally coordinated approach is required to achieve speed of response and to bring the pandemic to an end.40 But as supply issues ease, the progress in equity both among and within countries is revealed. In order to see equitable allocations, there must be three things that happen: the product that fits the needs of the countries, financing to ensure they can access it and the demand from countries.33 The first two have only been partially addressed. Vaccines were quickly developed and produced, including both mRNA vaccines and vector-based vaccines, which, if had gone to plan, would have provided 2 billion doses to vaccinate 20% of the world by December 2021.41 Although COVAX warned countries, there would be limited supply and hoarding in the acute phase of the pandemic,41 there was little they could do to prevent that. As a result, some countries felt the need to resort to bilateral deals at an elevated price.42 The third element is perhaps the trickiest as it impacts and is impacted by trust between all parties. In times of scarce supply, there needs to be both demand from the countries and some mechanism to monitor and enforce commitments when demand materialises. It is not entirely clear whether LMICs ordered vaccines. When Pfizer was asked about demand, they claimed they reached out.43 Whether they did or not, the perceptions have a way of sowing distrust. It did not help that anti-vaccine activists piled on to further weaponise appropriate health communications around vaccine safety and equity.30
Governing towards justice
Global models of governance are inherently complicated and COVAX is no exception. Many actors want a seat at the table and a say in how the pandemic will end. There are many disparate interests that can be challenging to manage, but the responsibility of the coordinator is to bring multiple actors together to define collective action (eg, solidarity) that benefits everyone.44 In the case of COVAX, the equity goal was clearly defined, but high and middle-income countries undermined the COVAX model through bilateral deals at the early stages of the pandemic; ironically, India, an LMIC itself, contributed to the problem by halting planned exports to take care of domestic concerns after a second wave of COVID.44
Some perceive that a select number of global actors, particularly the leaders of COVAX, donors and governments, moved forward in their own vision and vested interests rather than codesigning solutions that may have facilitated not only a better path forward but also a way to enforce.44 These measurements of justice include a realisation of regional manufacturing, participation in research and design and adjustments in the power dynamics between countries through efforts towards increased self-reliance. A more holistic measurement of justice also includes improvements in addressing demand side factors affecting vaccination, that are interconnected with supply. This requires data to track equity goals and the authority of civil society and the public to hold governments accountable. Both global and regional actors play a role in supporting countries with limited strength in their health systems, lack political will and/or resources to absorb vaccines and have competing priorities. Countries need cold storage space at every level (including ultra-cold storage if they use any of the current mRNA vaccines), the ability to ship vaccines and manage the distribution to those that are eligible. Considering that systems to distribute routine immunisations may already be suboptimal in some countries and the vaccines for COVID need to reach populations that are not typically vaccinated, additional support is needed to ensure that shots make it to arms, and that the ability to do so is monitored as a measure of justice. Furthermore, both vaccine hesitancy and the ability to access vaccines, even when supply is available, have the potential to erode trust not only in vaccines but also in the health system more broadly.
To achieve this shared vision of access, equity and justice for COVID-19 vaccines and other priority diseases, countries could work with independent non-governmental organizations or consortium of partners at regional level to provide support consistent with the vision of the country (eg, similar to Gavi’s Accelerated Development and Introduction Plans or product development partnerships). Africa is establishing mRNA technology transfer hubs and a new global biomanufacturing training hub in South Korea will assist in training skilled workers and strengthening regulatory capacity in the regions.45 Hubs such as those in Africa and Asia may also offer opportunities to engage more closely with countries in the regions not only to build capacity, but also to integrate the demand-side intelligence needed to ensure that products reflect the needs of local populations, forecasts are accurate and there is public and political support for the vaccines. While WHO and UNICEF engagement helps, having a dedicated group outside of the UN system may provide additional perspective. Understanding demand, potential barriers and how they are addressed around the region can help establish a more predictable supply of product and innovations to evaluate how barriers to development, licensure, production, distribution, monitoring acceptance and trust, particularly in populations with historically low vaccine uptake should be leveraged.
While at the global-level coordination focuses largely on supply and distribution, country voices still need to be strengthened to ensure product presentations better reflect the needs and challenges of their specific contexts whether products are produced globally or at a regional level. Although vaccines were developed quickly to distribute to the entire world, that does not diminish the need for vaccines that work with the existing platforms and priorities of particular countries. In future, vaccines that do not require refrigerated storage and can be administered as a pill, patch or nasal spray could obviate the need for highly trained healthcare workers to administer vaccines as well as improving vaccine uptake. However, this will require extensive investment in developing novel formulations followed by further clinical trials to assess safety, immunogenicity and efficacy. Delivery of a vaccine that is effective after intramuscular immunisation by a different route may result in considerably reduced efficacy, and if the vaccine is effective, novel correlates of protection must be determined. We can deliver services in the midst of existing inequity in poor countries—we have done it for AIDS with global solidarity (through the GFATM and PEPFAR) and with political will at country level.13 Strengthened engagement and coordination with existing priority programmes can help strengthen political will and lead to greater equity and justice through ownership of shared goals. A further outline of issues is provided in figure 3.
Figure 3.
Potential solutions for improving COVID-19 vaccine and vaccination equity and justice. Excler et al.46
Conclusion
Although sufficient supply of COVID-19 vaccines is no longer an issue, the necessity of adjusting our approach to access, equity and justice remains. In particular, as a global community, we need to converge on what justice means. This will be difficult with competing interests of so many actors, but at the very least, it must include elements of vaccine security, potentially in the form of regional manufacturing that produces an affordable, predictable supply of quality vaccines that reflect the needs of countries in the region while balancing the challenges of ensuring demand for vaccination. Engaging countries of all income levels, including both state and non-state actors to cocreate a new shared vision of access, equity and justice is an urgent action that must include measurements of success of the items listed above. Engagement in a common vision will help all of us and cocreation of that vision must be defined, agreed on and implemented well in advance of the next pandemic.
Acknowledgments
We are grateful to the World Innovation Summit for Health (WISH), Secretariat and Maha El-Akoum for their support, helpful comments and assistance in graphic creation for this work. Funding to provide open access for this work was made possible by WISH.
Footnotes
Handling editor: Seye Abimbola
Twitter: @lprivord, @PeterHotez
Contributors: LP-D, J-LE and JHK conceptualised. LP-D wrote the first draft of the manuscript and designed and conducted the analysis. All coauthors contributed to writing and editing of the manuscript. DT contributed to some of the figures.
Funding: This study was funded by World Innovation Summit for Health (WH-21-002).
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: LPD served on an advisory board for GSK; JLE is an employee of the International Vaccine Institute. He is Chair of the Military HIV Research Program/Emerging Infectious Diseases Branch/Henry M. Jackson Foundation Safety Monitoring Committee and member of the Benefit-Risk Assessment of Vaccines by Technology Working Group (BRAVATO) part of the Brighton Collaboration; SG is an inventor of intellectual property licensed by Oxford University Innovation to AstraZeneca; SAK serves as a Special Advisor (on pandemics) to the Director-General of the WHO. He is a Commissioner of the African Union Commission on COVID-19. He had served on the SANOFI medical advisory board for COVID-19 vaccines and as a Commissioner of the Lancet Commission on COVID-19; PJH is a co-inventor of a COVID-19 recombinant protein vaccine technology owned by Baylor College of Medicine (BCM) that was recently licensed by BCM non-exclusively and with no patent restrictions to several companies committed to advance vaccines for low- and middle-income countries. He has no involvement in license negotiations conducted by BCM; JHK was a consultant for SK Bioscience and serves on the Scientific Advisory Board for Everest.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available in a public open access repository.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.World Health Organization . Achieving 70% COVID-19 immunization coverage by Mid-2022. Statement of the Independent Allocation Vaccines Group (IAVG) of COVAX. Geneva, 2021. [Google Scholar]
- 2.Hunter DJ, Abdool Karim SS, Baden LR, et al. Addressing vaccine inequity - COVID-19 vaccines as a global public good. N Engl J Med 2022;386:1176–9. 10.1056/NEJMe2202547 [DOI] [PubMed] [Google Scholar]
- 3.Hotez PJ, Batista C, Amor YB, et al. Global public health security and justice for vaccines and therapeutics in the COVID-19 pandemic. EClinicalMedicine 2021;39:101053. 10.1016/j.eclinm.2021.101053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . Global COVID-19 vaccination strategy in a changing world July 2022 update. Geneva, 2022. [Google Scholar]
- 5.Mathieu E, Ritchie H, Rodés-Guirao L, et al. Coronavirus pandemic (COVID-19). Our World in Data, 2022. [Google Scholar]
- 6.World Health Organization . COVID-19 vaccine delivery partnership. Vaccine implementation indicators across countries for concerted support. WHO and Unicef, 2022. [Google Scholar]
- 7.Hotez PJ. SARS-Cov-2 variants offer a second chance to fix vaccine inequities. Nat Rev Microbiol 2022;21:127–8. 10.1038/s41579-022-00824-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Watson OJ, Barnsley G, Toor J, et al. Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect Dis 2022;22:1293–302. 10.1016/S1473-3099(22)00320-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mobarak AM, Miguel E, Abaluck J, et al. End COVID-19 in low- and middle-income countries. Science 2022;375:1105–10. 10.1126/science.abo4089 [DOI] [PubMed] [Google Scholar]
- 10.Gavi . Covax 2022. Geneva, Switzerland, Available: https://www.gavi.org/covax-facility [Accessed 15 Apr 2022]. [Google Scholar]
- 11.Wagner CE, Saad-Roy CM, Morris SE, et al. Vaccine nationalism and the dynamics and control of SARS-CoV-2. Science 2021;373:eabj7364. 10.1126/science.abj7364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eaton L. Covid-19: WHO warns against "vaccine nationalism" or face further virus mutations. BMJ 2021;372:292. 10.1136/bmj.n292 [DOI] [PubMed] [Google Scholar]
- 13.Katz IT, Weintraub R, Bekker L-G, et al. From vaccine nationalism to vaccine equity - finding a path forward. N Engl J Med 2021;384:1281–3. 10.1056/NEJMp2103614 [DOI] [PubMed] [Google Scholar]
- 14.Jecker NS. Global sharing of COVID-19 vaccines: a duty of justice, not charity. Dev World Bioeth 2023;23:5–14. 10.1111/dewb.12342 [DOI] [PubMed] [Google Scholar]
- 15.Harman S, Erfani P, Goronga T, et al. Global vaccine equity demands reparative justice - not charity. BMJ Glob Health 2021;6:e006504. 10.1136/bmjgh-2021-006504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mutombo PN, Fallah MP, Munodawafa D, et al. COVID-19 vaccine hesitancy in Africa: a call to action. Lancet Glob Health 2022;10:e320–1. 10.1016/S2214-109X(21)00563-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization . Establishment of a COVID-19 mRNA vaccine technology transfer hub to scale up global manufacturing. Geneva: WHO, 2021. [Google Scholar]
- 18.Excler J-L, Saville M, Privor-Dumm L, et al. Factors, Enablers, and challenges for COVID-19 vaccine development. BMJ Glob Health 2023;8:e011879. 10.1136/bmjgh-2023-011879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hotez PJ, Saville M, Privor-Dumm L, et al. COVID-19 vaccines and the pandemic: lessons learned for other neglected diseases and future threats. BMJ Glob Health. 2023;0:e011883. doi:10.1136/bmjgh-2023-011883 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yoo KJ, Mehta A, Mak J, et al. COVAX and equitable access to COVID-19 vaccines. Bull World Health Organ 2022;100:315–28. 10.2471/BLT.21.287516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bollyky TJ, Murray CJL, Reiner RC. Epidemiology, not geopolitics, should guide COVID-19 vaccine donations. Lancet 2021;398:97–9. 10.1016/S0140-6736(21)01323-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jerving S. The long road ahead for COVID-19 vaccination in Africa. Lancet 2021;398:827–8. 10.1016/S0140-6736(21)01967-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bong C-L, Brasher C, Chikumba E, et al. The COVID-19 pandemic: effects on low- and middle-income countries. Anesth Analg 2020;131:86–92. 10.1213/ANE.0000000000004846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dzinamarira T, Nachipo B, Phiri B, et al. COVID-19 vaccine roll-out in South Africa and Zimbabwe: urgent need to address community preparedness, fears and hesitancy. Vaccines 2021;9:250. 10.3390/vaccines9030250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yamey G, Garcia P, Hassan F, et al. It is not too late to achieve global COVID-19 vaccine equity. BMJ 2022:e070650. 10.1136/bmj-2022-070650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berkley S. Ending the COVID-19 pandemic means helping countries to catch-up with vaccination, not giving up. BMJ 2022;376:786. 10.1136/bmj.o786 [DOI] [PubMed] [Google Scholar]
- 27.Nachega JB, Sam-Agudu NA, Masekela R, et al. Addressing challenges to rolling out COVID-19 vaccines in African countries. Lancet Glob Health 2021;9:e746–8. 10.1016/S2214-109X(21)00097-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Assefa Y, Gilks CF, van de Pas R, et al. Reimagining global health systems for the 21st century: lessons from the COVID-19 pandemic. BMJ Glob Health 2021;6:e004882. 10.1136/bmjgh-2020-004882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bono SA, Faria de Moura Villela E, Siau CS, et al. Factors affecting COVID-19 vaccine acceptance: an international survey among Low- and middle-income countries. Vaccines 2021;9:515. 10.3390/vaccines9050515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hotez PJ. Will anti-vaccine activism in the USA reverse global goals. Nat Rev Immunol 2022;22:525–6. 10.1038/s41577-022-00770-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Braverman P, Orleans T, Proctor D, et al. What is health equity? And what difference does a definition make? Princeton, NJ: Foundation RWJ, 2017. [Google Scholar]
- 32.PLOS Medicine Editors . Vaccine equity: a fundamental imperative in the fight against COVID-19. PLoS Med 2022;19:e1003948. 10.1371/journal.pmed.1003948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.So AD, Woo J. Achieving path-dependent equity for global COVID-19 vaccine allocation. Med 2021;2:373–7. 10.1016/j.medj.2021.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cocks T. South Africa’s aspen COVID-19 vaccine plant risks closure after no orders, executive says. Reuters; 2022. [Google Scholar]
- 35.Das S. SII. Bharat BIOTECH halt production of Covid vaccines as demand slips. Business Standard; 2022. [Google Scholar]
- 36.Africa Centres for Disease Control and Prevention . Report of the high-level ministerial meeting: partnerships to accelerate COVID-19 vaccination in Africa. Addis Ababa, 2022. [Google Scholar]
- 37.UNDP . Global dashboard for vaccine equity. 2022. Available: https://data.undp.org/vaccine-equity/ [Accessed 01 May 2022].
- 38.Kakule B, Muhindo E, Janoch E, et al. At the last mile: COVID-19 vaccines in DRC: care; 2022.
- 39.Privor-Dumm LA, Poland GA, Barratt J, et al. A global agenda for older adult immunization in the COVID-19 era: a roadmap for action. Vaccine 2021;39:5240–50. 10.1016/j.vaccine.2020.06.082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peacocke EF, Heupink LF, Frønsdal K, et al. Global access to COVID-19 vaccines: a scoping review of factors that may influence equitable access for low and middle-income countries. BMJ Open 2021;11:e049505. 10.1136/bmjopen-2021-049505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.World Health Organization . Fair allocation mechanism for COVID-19 vaccines through the COVAX facility; 2020.
- 42.Hall S, Sun YS, Holt TZ. None are safe until all are safe’: COVID-19 vaccine Rollout in Low- and middle-income countries; 2021.
- 43.Griffin R. Pfizer CEO says lower-income countries didn’t order vaccines. Bloomberg, 2021. [Google Scholar]
- 44.Jecker NS, Atuire CA, Bull SJ. Towards a new model of global health justice: the case of COVID-19 vaccines. J Med Ethics 2023;49:367–74. 10.1136/medethics-2022-108165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.World Health Organization . Moving forward on goal to boost local pharmaceutical production, WHO establishes global biomanufacturing training hub in Republic of Korea. Geneva, 2022. [Google Scholar]
- 46.Excler J-L, Privor-Dumm L, Hotez P, et al. A new era for vaccine innovation: harnessing the lessons learned from COVID-19. Doha, Qatar: World Innovation summit for health, 2022. [Google Scholar]
- 47.Ritchie H, Mathieu E, Rodés-Guirao L, et al. Share of people who have received at least 1 dose of COVID-19 vaccine -Coronavirus pandemic (COVID-19) [online]. Our World in Data 2022. Available: https://ourworldindata.org/coronavirus#coronavirus-country-profiles [Google Scholar]
- 48.UNICEF Supply Division. COVID-19 deliveries [online]. n.d.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available in a public open access repository.