Abstract
Specifications of what and how much health behavior change (BC) content within research interventions are needed to advance BC science, its implementation, and dissemination. We analyzed the types and dosages of the smallest potentially active BC ingredients and associated behavioral prescriptions intended to be delivered in an ongoing physical activity optimization trial for older adults (Ready Steady 3.0 [RS3]). We defined BC types as behavior change techniques (BCT) and behavioral prescriptions. Our protocol integrated the BCT Taxonomy coding procedures with BCT roles (primary or secondary) and, when relevant, linkages to behavioral prescriptions. Primary BCTs targeted theoretical mechanisms of action, whereas secondary BCTs supported primary BCT delivery. Behavioral prescriptions represented what participants were encouraged to do with each primary BCT in RS3 (ascertain, practice, implement). We assessed dosage parameters of duration, frequency, and amount in each BCT and prescription.
Results provided a catalog of in-depth, multidimensional content specifications with 12 primary BCTs, each supported by 2-7 secondary BCTs, with dosages ranging from 2 to 8 weeks, 1 to 8 contacts, and 5 to 451 minutes. Minutes spent on behavioral prescriptions varied: ascertain (1 to 41), practice (5 to 315), and implement (0 to 38). Results can be organized and summarized in varied ways (e.g., by content component) to strengthen future assessments of RS3 fidelity and intervention refinement.
Results highlight potential benefits of this early, integrated approach to analyzing BC content and frames questions about how such information might be incorporated and disseminated with reporting research outcomes.
Keywords: Health behavior change, Intervention content, Behavior change techniques, Dosages, Behavioral prescriptions
A new approach to reporting early, in-depth descriptions of the types and dosages of the smallest, potentially active behavior change ingredients within interventions designed to promote health-related behaviors.
Implications.
Practice: Specifying the types, dosages, and behavior prescriptions of the smallest potentially active behavior change ingredients early, during research, can advance effective implementation and dissemination of health behavior change interventions in practice.
Policy: Policymakers’ decisions about the potential impact of different physical activity programs for older adults should have detailed information about their physical activity and behavior change ingredients.
Research: Interdisciplinary investigators of behavior change interventions should establish how and where to share and maintain detailed, up-to-date reports of the types, dosages, and associated behavioral prescriptions of their smallest behavior change ingredients.
INTRODUCTION
Interventions designed to promote healthy behaviors, such as physical activity, are complex, in that the behavior change content within them typically comprises many strategies with varied dosages [1–3]. A detailed understanding of this content is an essential building block needed to advance health behavior change science and its implementation and dissemination [4]. This understanding partly depends on in-depth specifications of what and how much health behavior change content is included within an intervention. To this end, the Template for Intervention Description and Replication (TIDeir) defines 12 dimensions to describe in published reports, including what content was used, when, and how frequent [5]. Taxonomies developed to facilitate these descriptions, such as The Behavior Change Technique (BCT) Taxonomy (BCTTv1), include defined, standard labels for the smallest potentially active behavior change ingredients within interventions [3]. To specify when and how much behavior change content is intended to be delivered, experts recommend accounting for the dosage (e.g., duration, frequency, and amount) of intervention packages and their constituent components [2, 6, 7],. McVay and colleagues [8] also recommend differentiating the dosage parameter of amount into three behavioral prescriptions regarding what an intervention is asking a person to do. Despite these templates, taxonomies, and recommendations, many published reports (e.g., study protocols and results) lack sufficient details about which BCTs were used, how, and their intended dosages [9–11]. This lack of detail limits the precision of estimates made from accumulated data regarding the association between BCTs (at varied dosages) and their targets [12, 13]. Thus, it might be beneficial to rethink how and when to report behavior change content in interventions. In this paper, we describe a case study that integrates BCTT v1 [3] coding with the assessment of dosage parameters and behavioral prescriptions [8] to analyze the behavior change content included in the interventions used in an ongoing physical activity optimization trial for older adults (Ready Steady 3.0 [14].
The commonly used BCTT v1 includes 93 distinct BCTs [3]. Researchers often use BCTTv1 to investigate associations between BCTs and outcomes [15], and sometimes putative mechanisms of action [11] relying on data about intervention content found in published reports (e.g., study protocols and results). A strength of this approach is the identification of promising BCTs. A weakness is that applying the BCTTv1, or any taxonomy, to published research reports is inherently limited by the level of detail about behavior change content found in such reports [16], compounded by space restrictions, making it challenging to identify which BCTs were used. Another weakness is the limited level of detail about dosages. Although most reports include dosage information about the intervention package, in total, few include information about the dosage for the smallest potentially active behavior change ingredients (e.g., BCTs or BCT clusters) [2, 17]. This state of affairs makes it difficult to gain a detailed understanding of intervention content within individual studies and, in turn, to make valid inferences about BCT and dosage effects.
Experts in many fields suggest that imprecise details about intervention content can be improved by reporting the types of behavior change content included (e.g., BCTs and BCT clusters) along with specific dosage parameters of duration, frequency, and amount [6, 7]. Amount, according to McVay and colleagues [8] can be differentiated into three behavioral prescriptions: “intervention action, participant action, and behavioral target action.” The different definitions of intervention action, participant action, and behavioral target action relate to what participants are asked to do by the intervention deliverer, be it a person or a digital app. For example, “Intervention Action Prescriptions” refer to intervention content or materials participants are asked to read, listen to, and/ or view, such as information about goal setting. “Participant Action Prescriptions” refer to what the participants are asked to produce in response to receiving intervention content or materials, such as sharing one’s health behavior goals with another person or a digital bot. “Behavioral Target Actions” refer to requests by the intervention to engage in the health behavior it targets, such as physical activity or adjacent behaviors such as joining a walking club. Moreover, there are recommendations to provide such details early (e.g., before main study results) as they are essential for the efficient accumulation of knowledge about health behavior change [18]. Despite these recommendations, no procedures or protocols are available to guide the early, simultaneous analysis of what and how much behavior change content is in an intervention study.
Thus, we present the first case study to combine established and novel approaches to analyzing the smallest potentially active behavior change ingredients within an intervention. The objective was to develop a protocol that integrated the established BCTT v1 coding procedures [3] with recently described behavioral prescriptions [8] and recommended dosage assessment parameters [7]. Instead of applying this protocol to descriptions of intervention content found in published reports, we applied it to readily available, detailed information within the intervention materials in an ongoing optimization trial, known as Ready Steady 3.0 [14]. We focused our coding and data collection on weekly meeting materials used in the Ready Steady 3.0 interventions. Our research questions included:
Is it feasible to analyze the smallest potentially active behavior change ingredients in Ready Steady 3.0 using an integrated approach that combines BCTT v1 coding with assessments of behavioral prescriptions and dosages?
How many and which types of BCTs were identified?
What were the intended dosages of BCTs and behavioral prescriptions?
What information was generated from this early, integrated analysis?
METHOD
This case study is a descriptive analysis of the types and dosages of behavior change content intended to be delivered within Ready Steady 3. The protocol and rationale for Ready Steady 3.0 were published [14] and registered at Clinicaltrials.gov (NCT03326141). Ready Steady 3.0 was designed to test the effects of two experimental intervention content components with distinct behavior change strategies: interpersonal (e.g., encourage social support) and intrapersonal (e.g., facilitate goal setting), using a 2x2 factorial design in community-residing adults aged 70 years and over [14]. The trial design also included two core components: an evidence-based physical activity protocol and a personal physical activity monitor. The four content components were combined differently in four study conditions (intervention packages): i) core components and attention control content about health and wellness; ii) core components and the interpersonal component; iii) core components and the intrapersonal component; iv) core components, the interpersonal and the intrapersonal components. Ethical approval of Ready Steady 3.0 was obtained from the University of Minnesota Institutional Review Board (1607S90922). Because there are no human subjects in this case study, it was exempt from IRB approval.
Ready Steady 3.0 recruitment strategies and entrance criteria
Community-dwelling older adults were recruited for Ready Steady 3.0 using advertisements in local newspapers, on Facebook, in two University of Minnesota websites, and in church bulletins near community centers that hosted the study meetings [14]. To be eligible for Ready Steady 3.0, participants had to speak English, be ≥ 70 years,walk with or without an aid, have levels of physical activity below those recommended in national and international guidelines [19] for older adults, have no lower extremity injuries or surgeries in the last six weeks, and no formal or informal diagnosis of dementia.
Ready Steady 3.0 interventions
The following several paragraphs provide a brief description of the interventions in Ready Steady 3.0, guided by the TIDieR [5], the Intervention Setting Ontology [20], and Mode of Delivery Ontology [21]. Each study condition (intervention package) was delivered by trained personnel with bachelor’s degrees in nursing or a related field and competent to deliver the Otago Exercise Program [22] and all intervention content. The setting of the intervention was in five urban neighborhoods near community centers accessible to older adults. The informational mode of delivery was primarily face-to-face via small group meetings augmented with printed materials in a workbook and electronic materials in the form of a wearable activity monitor (e.g., step count, physical activity minutes, distance). All four study conditions had a total duration of 8 weeks, with weekly contacts, each lasting 90 minutes.
Content in each of the four Ready Steady intervention component was designed and developed based on empirical and theoretical evidence, and refined after initial preparation research studies [23, 24]. Although behavior change content, identified as behavior change strategies in Ready Steady, aligns with the BCTTv1, explicit links between behavior change content and BCTs were done after intervention development, as part of this case study.
Interpersonal behavior change strategies
This component included five behavior change strategies that require communication between group members about physical activity-related ideas, strategies, experiences, and knowledge to elicit change. The strategies in this component were managing environmental barriers, friendly social comparisons, using environmental prompts and cues, increasing social support, and recognizing self as a role model. These strategies were selected based on the constructs of social and environmental resources in the wellness motivation theory [25, 26], and evidence generated by research supporting their positive effects [9, 27, 28]. They target the constructs of the environmental resources, social support, enjoyment, and self-efficacy as theoretical mechanisms of action.
Intrapersonal behavior change strategies
This component included five behavior change strategies, emphasizing one’s reflection about personal preferences, values, goals, and schedules to elicit change. The strategies in this component were managing personal barriers; planning processes that include goals, actions, and self-assessment; and building habits. These strategies were selected based on the constructs of self-knowledge, readiness, self-regulation in the wellness motivation theory [25, 26], and evidence that shows each is associated with older adults’ physical activity [29–31]. They target the constructs of self-efficacy, enjoyment, and self-regulation as theoretical mechanisms of action.
Physical activity protocol
The Otago Exercise Program (OEP) adapted for small groups [24, 32], was selected as a core component to be delivered across all conditions. Substantial evidence supports the positive effects of OEP on falls and fall risk [33]. It guides the safe performance of 21 specific exercises categorized into four types of physical activity: balance-challenging (n = 11), leg-strengthening (n = 5), and flexibility (n = 5) [22]. This component was designed to help participants gradually increase the frequency, duration, and difficulty of OEP movements, according to protocol and tailored to participant abilities. Additionally, it was designed to help participants independently perform the OEP movements in free-living contexts between meetings and after completing the intervention, consistent with national and international physical activity guideline recommendations for older adults [19].
Physical activity monitor
The commercially available physical activity monitor, Fitbit Charge 2, was selected as a core component to augment the intervention delivery across all study conditions and the collection of physical activity data. It was selected because its features complimented some of Ready Steady’s behavior change content and it was affordable, convenient to wear, only needed weekly (not daily) charging, was relatively simple to use, and provided accurate physical activity data [34, 35]. Participants received beginning and advanced orientations (verbal and written) to their monitors and were encouraged to adjust their settings according to personal preferences and progress. During three intervention meetings, participants received graphs displaying one-week trends of their step counts.
Attention control intervention content
Because the first study condition did not include the interpersonal or intrapersonal components, we added attention control content to this condition comprised of health and wellness topics. Main topics included fall prevention, pain, nutritional supplements, sleep, memory, hearing, and vaccinations. An additional attention control strategy across all four conditions was variable amounts of time allotted for technical questions about the exercises and physical activity monitors, at each meeting for 0-10 minutes to ensure each was approximately 90 minutes. All participants were also encouraged to contact the intervention staff at any time with these technical questions.
Coding procedures
Two graduate research assistants (RA) were oriented to Ready Steady 3.0 and trained to conduct this case study. Both RAs (KM and EAC) understood the purpose, aims, outcomes, and intervention content of Ready Steady 3.0 through reading and meeting with the investigators [36]. Each RA completed the online BCTTv1 training (www.bct-taxonomy.com) that included progressive instruction, practice arenas, tutoring, and two formal assessments, organized around six key principles and learning modules. Research assistants in this study did not progress to a new module until they scored at least 70% on the previous module, per their preference to master the material. In addition, per course structure, RAs scored at least 70% on each of the two formal course assessments to pass the course and become certified as a trained BCT coder. Each RA also developed the skills and abilities to code, assess, collect, and manage data according to our integrated protocol.
Data was collected from Ready Steady 3.0 intervention materials such as manuals (interventionist and participant), hand-outs, and flipcharts. Each of the four interventionist manuals, one for each condition, had eight sections: one for each weekly meeting, with objectives, scripted tactics, activities, and timing. Participant manuals had five main sections with information about i) contacting study staff, ii) exercising safely, iii) using the physical activity monitors, iv) weekly meetings, and v) recommended physical activities and diagrams of each OEP exercise.
Before starting the case study, RAs used a sample of intervention materials to practice coding and collecting data. During this practice time, RAs and the Principal Investigator (SKM) also refined the data collection protocol according to observations that one BCT definition, BCT groupings, and behavioral prescriptions in Ready Steady 3.0 were slightly different from the BCTTv1 [3] and original descriptions by McVay and colleagues [8]. Specific refinements and adaptations are described in the following paragraphs. The final, refined data collection protocol was made into a REDCap case report form and, once the case study began, applied to one week of intervention materials at a time. The RAs and Principal Investigator met weekly to discuss progress, compare coding, discuss, and reach a consensus on discrepant codes. Each RA completed 32 forms, given the 32 weeks of materials.
Variables
Variables in the protocol were structural or representative of BCTs, behavioral prescriptions, and dosages. Structural variables included the author of the form, meeting analyzed (1 to 8), study condition (1,2,3,4), discussion needed for coding discrepancies (yes or no), and consensus reached (yes or no).
BCTs
The BCT variables addressed the number of BCTs, BCT codes, and BCT roles. The first variable indicated the number of BCTs identified in the weeks’ worth of materials (0 to 10). Two additional variables represented an evidence statement and the BCTTv1 code for each BCT identified. Evidence statements were verbatim quotes of text from the interventionist manuals that represented the BCT identified. Code options reflected the 93 codes and definitions in the BCTTv1, with one adaptation. Instead of “performance,” the focus of 6.2 Social Comparison [3] in Ready Steady 3.0 was comparisons of knowledge of and experiences implementing BCTs and physical activities/exercise outside the intervention meetings.
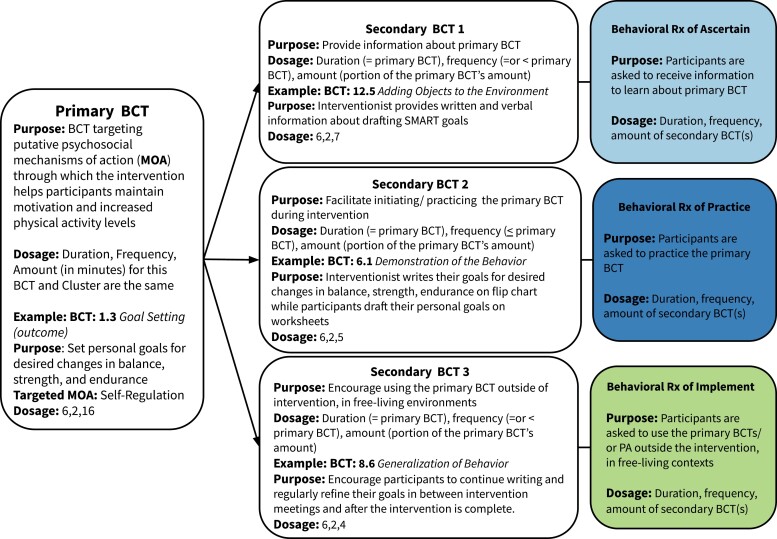
The variable of BCT role (primary or secondary) was created because of our observations during initial coding practice that BCTs in Ready Steady 3.0 were delivered in groupings, which we labeled as hierarchical intervention bundles. Primary BCTs in these bundles were those targeting putative mechanisms of action (e.g., social support, self-regulation, self-efficacy for exercise), while secondary BCTs were those supporting the delivery and use of the primary BCT. An example of a hierarchical intervention bundle used during two meetings in Ready Steady 3.0’s interpersonal component included the primary BCT of Social Comparison (6.2) and four secondary BCTs, as well as a non-BCT, to support its delivery. Social Support (unspecified) (3.3) was identified as a secondary BCT because the delivery of Social Comparison was embedded in friendly, supportive interactions with others that involved sharing knowledge, experiences, and lessons learned about practicing recommended physical activity/exercises (successes, challenges). Behavioral Practice (8.1) was identified as another secondary BCT in this bundle because time was dedicated to actively practicing Social Comparison with peers during the intervention meetings. Generalization of Target Behavior (8.6) was also identified as a secondary BCT because interventionists encouraged participants to engage in similar conversations with others outside the intervention about their knowledge, experiences, and lessons learned about exercises/ physical activity. Finally, the non-BCT in this bundle involved providing participants with background information about social comparisons used in this intervention as one way to validate and broaden one’s knowledge and possibly experiences about performing recommended exercises/physical activity in their everyday lives. Figure 1 illustrates a prototype of the hierarchical bundles based on their temporal and functional relationships in the delivery of Ready Steady 3.0. Of note, we intentionally used the label of hierarchical intervention bundles and the variable of BCT roles to differentiate them from previously published groupings of BCTs in the BCTTv1 identified as hierarchical clusters based on the similarity of their active ingredient(s) [3] or thematic domains within the Theoretical Domain Framework [37].
Fig 1.
BCT Bundle Prototype in Ready Steady 3.0. Notes: BCT = Behavior Change Technique, Dosage = Duration (Portion of intervention that addresses this BCT bundle/BCT, in weeks), Frequency (Number of Contacts during which this BCT bundle/ BCT was addressed), Amount (Minutes spent delivering this BCT bundle/ BCT); Rx = Prescription.
Behavioral prescriptions
Three behavioral prescription variables indicated whether a BCT was linked to the behavioral prescriptions of “Intervention Action” (yes or no), “Participant Action” (yes or no), or “Behavioral Target Action” (yes or no). When a behavioral prescription was identified, an evidence statement (i.e., a supporting quote from the interventionist manual) was also captured. During the data collection process, we adapted the original labels [8] (see Table 1) to more specifically represent what participants were asked to do as part of Ready Steady 3.0. “Intervention Action,” defined as asking participants to receive intervention content, was modified as “Ascertain” with a slightly more specific definition of participants learning information about the primary BCT of interest. For example, when delivering the BCT bundle of goal-setting, ascertain is identified when participants were asked to review (e.g., read, listen, view graphics) information about personal physical activity goals and drafting those. Similar changes were made to render the other behavioral prescriptions more specific. The behavioral prescription of “Participant Action” was modified to read “Practice,” defined as participants being asked to initiate and practice the primary BCT of interest during an intervention meeting. Finally, the behavioral prescription “Behavioral Target Action” was modified to read “Implement.” and was defined as encouraging participants to use the primary BCT of interest to help them regularly perform fall-reducing physical activities in their free-living contexts.
Table 1.
Behavioral Prescriptions: Labels and Definitions originally published by McVay and colleagues (2019) and adaptations for Ready Steady 3.0
| Source | Behavioral Rx 1 | Behavioral Rx 2 | Behavioral Rx 3 |
|---|---|---|---|
| McVay et al (2019) | Intervention Action: Participants asked to receive intervention content |
Participant Action:
Participants asked to produce/provide content to the intervention |
Behavioral Target Action: Participants asked to engage in health behavior targets (e.g., physical activity, eat more fruit) |
| Modifications in Ready-Steady 3.0 | Ascertain: Participants asked to receive information about primary BCT | Practice: Participants are asked to initiate/ practice the Primary BCTs | Implement: Participants encouraged to use BCTs to help them sustain motivation for, and regularly perform/engage-in, fall-reducing physical activities in free-living contexts |
Dosages
The intended dosages of BCTs and behavioral prescriptions in Ready Steady 3.0 were represented by duration, frequency, and amount [7, 8], with respective definitions of the number of weeks over which the BCT was delivered, contacts during which the BCT was addressed, and minutes the BCT was addressed. Amount was further differentiated by the secondary BCT(s) and behavioral prescriptions linked to primary BCTs. Duration and frequency were calculated during analysis, while amount was collected during the coding and data collection processes.
Analysis
Variables were analyzed using descriptive statistics, such as counts, frequencies, and percentages. We identified and counted all BCTs and calculated their dosage parameters of duration, frequency, and amount. When relevant, we divided the amount (minutes) for each primary BCT according to the secondary BCTs (or non-BCT strategies) and behavioral prescriptions to which they were linked. This granular data is reported according to the smallest potentially active types and dosages of behavior change content within Ready Steady 3.0.
RESULTS
Feasibility of analyzing the smallest potentially active behavior change ingredients
In total, materials for 32 weekly meetings in the Ready Steady 3.0 trial were reviewed and analyzed by both RAs, who reached consensus on all coding, demonstrating the successful application of our integrated protocol to study materials. As mentioned, behavior change content was delivered in hierarchical bundles. Each bundle had a primary BCT and one to six secondary BCTs that augmented the delivery of the primary BCT. Each secondary BCT was linked to a behavioral prescription: ascertain, practice, or implement. Figure 1 illustrates a prototypical BCT bundle found in Ready Steady 3.0 with linkages between primary BCTs, secondary BCTs, and behavioral prescriptions.
Number and types of BCTs identified
Table 2 details all BCTs used in Ready Steady 3.0 and their codes, behavioral prescriptions to which they were linked, and dosages. Coders identified 12 primary BCTs across all intervention materials. These included: 1.2 Problem Solving (environment); 1.2 Problem Solving (personal); 6.2 Social Comparison (of experiences); 7.1 Prompts and Cues; 3.1 Social Support (unspecified); 13.1 Identification of Self as a Role Model; 1.3 Goal Setting (outcome); 8.3 Habit Formation; 1.4 Action Planning; 1.7 Review Outcome Goals; 8.1 Behavior Practice/Rehearsal; and 2.3 Self-monitoring of Behavior.
Table 2.
Behavior Change Content in Ready Steady 3.0: Intended types, roles, and dosages, by behavior change content bundle and intervention content component
| Intervention Content Components | Type | Dosage | |||
|---|---|---|---|---|---|
| Behavior Change Content Bundles BCTs as coded using BCTT v1 | BCT Role | Duration (Weeks) | Frequency (Contacts) | Amount (Minutes) | |
| Interpersonal Behavior Change | 1.2 Problem Solving (environment) | Primary | 7 | 2 | 32 |
| NA. Information | Secondary | 7 | 2 | 4 | |
| 6.2 Social comparison | Secondary | 7 | 2 | 22 | |
| 12.1 Restructuring the Physical Environment | Secondary | 7 | 2 | ||
| 12.2 Restructuring the Social Environment | Secondary | 7 | 2 | ||
| 8.1 Behavior Practice/Rehearsal | Secondary | 7 | 2 | ||
| 4.4 Behavioral Experiments | Secondary | 7 | 1 | 6 | |
| 8.6 Generalization of Behavior | Secondary | 7 | 2 | ||
| 6.2 Social Comparison | Primary | 6 | 2 | 30 | |
| NA. Information | Secondary | 6 | 2 | 4 | |
| 3.1 Social Support (unspecified) | Secondary | 6 | 2 | 19 | |
| 8.1 Behavioral Practice/ Rehearsal | Secondary | 6 | 2 | ||
| 8.6 Generalization of Behavior | Secondary | 6 | 1 | 7 | |
| 7.1 Prompts and Cues (for exercise) | Primary | 5 | 2 | 30 | |
| NA. Information | Secondary | 5 | 2 | 6 | |
| 6.2 Social Comparison | Secondary | 5 | 2 | 16 | |
| 1.2 Problem-solving | Secondary | 5 | 2 | ||
| 8.1 Behavioral Practice/ Rehearsal | Secondary | 5 | 2 | ||
| 4.4 Behavioral Experiments | Secondary | 5 | 1 | 8 | |
| 8.6 Generalization of Behavior | Secondary | 5 | 2 | ||
| 3.1 Social Support (unspecified) | Primary | 4 | 1 | 17 | |
| NA. Information | Secondary | 4 | 1 | 2 | |
| 6.2 Social Comparison | Secondary | 4 | 1 | 12 | |
| 8.1 Behavioral Practice/ Rehearsal | Secondary | 4 | 1 | ||
| 8.6 Generalization of Behavior | Secondary | 4 | 1 | 3 | |
| 13.1 Identification of Self as a Role Model | Primary | 3 | 1 | 6 | |
| NA. Information | Secondary | 3 | 1 | 1 | |
| 6.2 Social Comparison | Secondary | 3 | 1 | 5 | |
| Intrapersonal Behavior Change | 1.2 Problem Solving (personal) | Primary | 7 | 2 | 32 |
| NA. Information | Secondary | 7 | 2 | 4 | |
| 6.2 Social Comparison | Secondary | 7 | 2 | 22 | |
| 8.1 Behavioral Practice/Rehearsal | Secondary | 7 | 2 | ||
| 4.4 Behavioral Experiments | Secondary | 7 | 2 | 6 | |
| 8.6 Generalization of Behavior | Secondary | 7 | 1 | ||
| 1.3 Goal Setting (outcome) | Primary | 6 | 2 | 16 | |
| NA. Information | Secondary | 6 | 2 | 5 | |
| 12.5 Adding Objects to the Environment | Secondary | 6 | 2 | ||
| 6.1 Demonstration of Behavior | Secondary | 6 | 1 | 8 | |
| NA. Reflection: writing personal goals | Secondary | 6 | 2 | ||
| 8.1 Behavioral Practice/Rehearsal | Secondary | 6 | 2 | ||
| 8.6 Generalization of Behavior | Secondary | 3 | |||
| 8.3 Habit Formation | Primary | 5 | 2 | 31 | |
| NA. Information | Secondary | 5 | 2 | 8 | |
| 12.5 Adding Objects to the Environment | Secondary | 5 | 2 | ||
| 6.1 Demonstration of the Behavior | Secondary | 5 | 1 | 15 | |
| 15.2 Mental Rehearsal | Secondary | 5 | 1 | ||
| 1.2 Problem Solving | Secondary | 5 | 1 | ||
| 8.1 Behavioral Practice/Rehearsal | Secondary | 5 | 2 | ||
| 8.6 Generalization of Behavior | Secondary | 5 | 2 | 8 | |
| 1.4 Action Planning | Primary | 4 | 1 | 16 | |
| NA. Information | Secondary | 4 | 1 | 5 | |
| 12.5 Adding Objects to the Environment | Secondary | 4 | 1 | ||
| 1.7 Review Outcome Goals | Secondary | 4 | 1 | 7 | |
| NA. Reflection: write action plans, adjust goals prn | Secondary | 4 | 1 | ||
| 6.1 Demonstration of Behavior | Secondary | 4 | 1 | ||
| 8.1 Behavioral Practice/Rehearsal | Secondary | 4 | 1 | ||
| 8.6 Generalization of Behavior | Secondary | 4 | 1 | 4 | |
| 1.7 Review Outcome Goals | Primary | 2 | 1 | 16 | |
| NA. Information | Secondary | 2 | 1 | 5 | |
| 12.5 Adding Objects to the Environment | Secondary | 2 | 1 | ||
| 1.6 Discrepancy Between Current Behavior and Goal | Secondary | 2 | 1 | 7 | |
| NA. Reflection: Adjust goals & plans | Secondary | 2 | 1 | ||
| 6.1 Demonstration of Behavior | Secondary | 2 | 1 | ||
| 8.1 Behavioral Practice/Rehearsal | Secondary | 2 | 1 | ||
| 8.6 Generalization of Behavior | Secondary | 2 | 1 | 4 | |
| Physical Activity Protocol | 8.1 Behavior Practice/Rehearsal | Primary | 8 | 8 | 451 |
| 4.1 Instruction on how to perform behavior | Secondary | 8 | 8 | 41 | |
| 3.2 Social Support (practical) | Secondary | 8 | 8 | 16 | |
| 6.1 Demonstrating of the behavior | Secondary | 8 | 8 | 41 | |
| 8.1 Behavior Practice/Rehearsal | Secondary | 8 | 8 | 315 | |
| 8.6 Generalization of Behavior | Secondary | 8 | 8 | 38 | |
| Physical Activity Monitor | 2.3 Self-monitoring of behavior | Primary | 8 | 8 | 25 |
| NA. Information | Secondary | 8 | 8 | 10 | |
| 12.5 Adding objects to the environment | Secondary | 8 | 8 | 15 |
Notes. BCTT v1 = Behavior Change Technique Taxonomy (ref); BCT = Behavior Change Technique, Primary = BCT whose primary purpose is to target the theoretical psychosocial mechanism of action in the study to help participants perform Ready Steady 3.0 physical activities in their free-living contexts; Supplementary = BCTs that are used as tactics for delivering the primary BCTs; Light Shade = amount differentiated as the behavioral prescription of ascertain (to receive and understand information about the primary BCT); Medium Shade = amount differentiated as the behavioral prescription of practice (to practice the primary BCT during an intervention contact/ meeting); Darker Shade = amount differentiated as the behavioral prescription of implement (to use the primary BCT outside the intervention meetings, in participants’ free-living contexts).
Thirteen secondary BCTs were also identified: 6.2 Social Comparison; 12.1 Restructuring the Physical Environment; 12.2 Restructuring the Social Environment; 4.4 Behavioral Experiments; 8.1 Behavioral Practice/ Rehearsal; 3.1 Social Support (unspecified); 1.2 Problem Solving; 12.5 Adding Objects to the Environment; 6.1 Demonstration of the Behavior; 15.2 Mental Rehearsal; 1.7 Review Outcome Goals; 1.6 Discrepancy Between Behaviors and Goals; 8.6 Generalization of Behavior.
Two additional secondary intervention strategies were identified that could not be captured by the BCTTv1 codes. The first non-BCT strategy focused on Providing Information about the primary BCTs (e.g., explaining different types of commonly experienced social support). The second non-BCT strategy focused on Facilitating Reflection time for some primary BCTs in the intrapersonal intervention content component.
Intended dosages of BCTs and behavioral prescriptions
Overall, the dosages of primary BCTs varied, with durations ranging from 2 to 8 weeks, frequencies ranging from 1 to 8 contacts, and amounts ranging from 5 to 451 minutes. BCT 8.1, behavior practice/rehearsal, had the largest dosage, with a duration of 8 weeks, frequency of 8 contacts, and amount of 451 minutes. It was the only primary BCT in the component comprised of the physical activity protocol. Behavior Change Technique 13.1, Identification of Self as a Role Model, had the smallest dosage with a duration of 3 weeks, frequency of 1 contact, and amount of 5 minutes. It was one of five primary BCTs in the intervention component comprised of interpersonal behavior change strategies.
Secondary BCTs and behavioral prescriptions had dosages that mirrored the primary BCTs to which they were linked (Fig. 1), with differentiation of amount (minutes) described below.
Types and amount of secondary BCTs linked to the behavioral prescription of ascertain
The secondary BCTs 12.5 Adding Objects to the Environment, 4.1 Instruction on How to Perform the Behavior, 6.1 Demonstration of the Behavior, and the non-BCT of Providing Information were used to help participants ascertain information about primary BCTs. The amount of time spent delivering these secondary BCTs and the behavioral prescription of ascertain to which they were linked ranged from 2 to 41 minutes across meetings, accounting for, on average, 22% of the delivery time for each primary BCT.
Types and amounts of secondary BCTs linked to the behavioral prescription of practice
Nine secondary BCTs facilitated participants’ initial practice of the primary BCTs within the context of Ready Steady 3.0 interventions, such as 8.1 Behavioral Practice/ Rehearsal, 6.2 Social Comparison, 12.1 Restructuring the Physical Environment, and 15.2 Mental Rehearsal (see Table 2). Also, the non-BCT strategy, Facilitating Reflection, was linked to the prescription of practice. The amount of time spent delivering these secondary BCTs and the behavioral prescription of practice to which they were linked ranged from 5 to 386 minutes across all primary BCTs, accounting for, on average, 62% of the delivery time for each primary BCT.
Types and amounts of secondary BCTs linked to the behavioral prescription of implement
Finally, the secondary BCTs of 8.6 Generalization of Behavior and 4.4 Behavioral Experiments were used to encourage participants to implement primary BCTs in their free-living contexts. The amount of time spent delivering these secondary BCTs and the behavioral prescription of implement, to which they were linked, ranged from 0 to 38 minutes across all primary BCTs, accounting for, on average, 18% of the intervention time taken to deliver each primary BCT.
Information generated from this early, integrated analysis
Information about multiple dimensions of the smallest potentially active ingredients in Ready Steady 3.0 can be organized in different ways to generate precise summaries and qualitative comparisons. It is beyond the scope of this case study to conceptualize or delve into all inferences from this data. However, to describe a few lessons learned, we summarized and compared: i) data about BCT types and dosages in Ready Steady’s experimental components of interpersonal and intrapersonal behavior change strategies, and ii) the number of minutes dedicated to each behavioral prescription by intervention component. Supplementary Table 1 illustrates another way to organize and summarize the behavior change content: by each Ready Steady 3.0 condition (intervention package).
The interpersonal and intrapersonal intervention components had distinct sets of primary BCTs that were conceptually consistent with BCTs and categories in BCTTv1 that reflect social interaction (e.g., social support and comparison) or personal reflection/thinking (e.g., goals and planning). As expected, their overall BCT dosages were also similar (see Table 2). Also, as expected, the types of secondary BCTs used to support the delivery of each primary BCT were different. Social Comparison was identified often in the interpersonal component, whereas Facilitating Reflection and Demonstration of Behavior were identified often in the intrapersonal component.
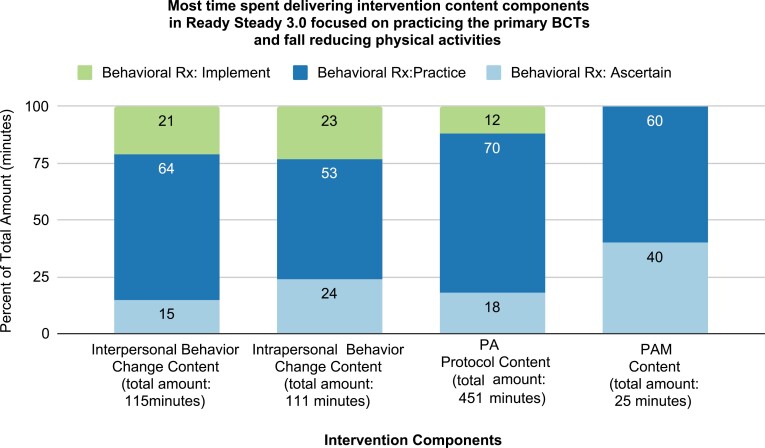
Time dedicated to encouraging each behavioral prescription (ascertain, practice, and implement) across intervention content components have similarities and differences (see Fig. 2). For instance, time was mostly spent practicing the primary BCT in all four intervention content components, with a few visually apparent variations. Practice accounted for 64% of the amount of time delivering the interpersonal component (comparing experiences via peer discussions) and 53% of the time delivering the intrapersonal component (thinking about/drafting goals and plans).
Fig 2.
Behavioral Prescriptions in Ready Steady 3.0, by intervention component. Notes: Rx = Prescription (recommendation, encouragement).
DISCUSSION
After rethinking how and when the behavior change content in interventions might be analyzed and reported, we conducted a case study integrating established and new approaches. We combined BCTTv1 [3] coding, identifying behavioral prescriptions [8], and assessing dosage parameters [6, 7], into a data collection protocol, and applied it to intervention materials in a physical activity optimization trial (Ready Steady 3.0) for older adults [14]. This integrated approach resulted in three main findings. First, it was feasible to analyze multiple dimensions of the BCTs, and behavioral prescriptions using intervention materials and generate in-depth specifications of the types and dosages of behavior change content in Ready Steady 3.0. Second, the results can be organized and summarized in various ways to provide helpful information. Third, we found that while most behavior change content in Ready Steady 3.0’s interventions was consistent with the BCTTv1, there were differences. Two strategies in the intervention were not defined with BCTs; one BCT was defined differently, and bundled groupings identified in the case study were distinct from clusters previously described.
While more granular than typical descriptions found in published research reports, early, in-depth specifications of behavior change content in interventions have several potential uses and benefits. Most published reports describing the intervention research results identify BCTs or behavior change strategies used in their intervention package. Still, few such publications provide in-depth details about BCT dosages or the behavioral prescriptions to which they are linked. Thus, our results provide a catalog of behavior change content within Ready Steady 3.0 that goes beyond identifying BCTs that are present by including the dimensions of intended dosages and how BCTs are intended to be used (primary and secondary behavioral prescriptions). Such a catalog might be helpful to researchers and theorists when developing, refining, replicating, and testing specific intervention content and dosages. Additionally, having this information before evaluating intervention fidelity will provide in-depth details to compare what was intended with what was delivered, received, and enacted [38]. Finally, it may be beneficial if other investigators similarly analyze the multiple dimensions of the smallest potentially active behavior change ingredients in their interventions. The accumulation of such precise specifications could motivate more investigations to focus on the relative effects of distinct behavior change content and dosages on targeted mechanisms of action. Such investigations would address a significant challenge to the acceleration of behavior change science: identifying the best ways to change targeted, theory-based, hypothetical mechanisms of action, and ultimately outcomes [4].
Information provided in our results can be organized, summarized, and compared in multiple ways to inform further development, testing, and refinement. For example, the summaries and comparisons we presented of the interpersonal and intrapersonal components in Ready Steady 3.0 validate that its experimental content components have distinct BCTs, consistent with their orientations, yet have similar overall dosages. Summaries and comparisons of behavioral prescriptions (Table 2) show similarities and differences. Because these prescriptions are modifiable, this summary also raises questions that might warrant future investigation of this new dimension of behavior change content. A few examples include: What are the minimal dosages needed in physical activity interventions to help older adults ascertain, practice, and implement the primary BCTs? What are the durations of action of each behavioral prescription? What are the best BCTs (or non-BCT strategies) for recommending or delivering these behavioral prescriptions? Do minimal effective dosages vary according to delivery mode (e.g., digital versus face to face)?
Finally, we found that not all the behavior change content in Ready Steady 3.0 fits the definitions and categorizations of BCTs and BCT clusters in the BCTTv1 or the original descriptions of behavioral prescriptions. The two secondary behavior change strategies that were not consistent with BCTTv1codes and our adapted definition of BCT of 6.2 Social Comparison are partially consistent with prior research. Agbadjé and colleagues [39] identified the new BCTs of “Providing Background Information” and “Experience Sharing and Learning,” that are similar to our secondary strategy of Providing Information about primary BCTs and our adapted definition of 6.2 Social Comparison--but tailored to clinician-patient interactions, not peer-to-peer interactions. The BCT groupings we described and accounted for differed from the BCTTv1 [3]; they were a function of delivering the behavior change content, not a function of conceptual or thematic consistency. It is plausible that our unique groupings reflect the analysis of detailed intervention materials (e.g., objectives, scripting, and rationale for contacts), data not typically available in published reports. These inconsistencies combined with our adaptations of the labels and definitions of behavioral prescriptions (Table 1) support the expectation that, by design, the BCTTv1 and reporting methods will continue to develop and expand to envelop diverse content [3] and dimensions.
Together, our results engender ideas for expanding our beginning catalog of behavior change content. For example, can a comprehensive, dynamic catalog of information be built that focuses on behavior change content, analogous to information about drugs found in monographs or packages of synthesized monographs and related literature such as Micromedex or Lexicomp [40] These up-to-date standardized drug information sources provide in-depth specifications about individual drugs (e.g., description, mechanism of action, uses, administration options, dosages, precautions, and monitoring parameters) that guide clinicians’ decision-making, practice, and patient education in all contexts. So too, should behavior change science researchers and practitioners build monographs providing in-depth specifications about individual BCTs, the smallest potentially active behavior change ingredients that have the potential for use in many different interventions. Such products could include up-to-date information about individual BCTs, particularly their definitions, uses, possible groupings, mechanisms of action, theoretical underpinnings, delivery, dosages, behavioral prescriptions, interactions, and monitoring parameters. Behavior Change Technique monographs, or similar products, would help researchers and practitioners maintain a detailed understanding of health behavior change content within interventions. Such detailed catalogs would also compliment and link with ontologies being developed by the Human Behavior Change Project [41].
This case study has important limitations. The data collection focused on intended types and dosages; thus, the analysis does not represent intervention behavior change content or dosages delivered, received, or enacted. However, the results can be used to compare what was planned and what happened and motivate dose-response investigations.
Another limitation is that it took considerable time and effort to apply our integrated protocol to Ready Steady 3.0 intervention materials. The amount of time taken to conduct this study, including time spent on the BCT training course, developing the study protocol, coding, analyzing, and interpreting data was approximately 151 hours, over 8 months. Approximately 16 hours were spent on training for BCT coding (8 hours per RA), 20 hours for developing the protocol and case report form (5 hours for 2 RAs and for 2 supervisors), 60 hours for coding (30 hours per RA), 15 hours for supervising the coding and data management processes, and 40 hours for analyzing and interpreting data (10 per RA and supervisor). We hope that sharing our processes, approach, and case report form can help to decrease the amount of time needed to describe behavior change content within interventions, particularly time needed for developing the study protocol, supervision, and interpreting the data. Additionally, the potential benefits of this early, time-intensive analysis will need to be evaluated. Hekler and colleagues [18] suggest that analyzing and sharing such information before evaluating main intervention effects enables more rapid and parallel use of, or repurposing of, the smallest, meaningful behavior change content. Another possible benefit is that early analysis of intervention materials in an ongoing trial by intervention researchers may offset the time and effort required of others to analyze behavior change content retrospectively in published research reports. Additionally, the data collected are likely more precise and detailed than data collected from a published report.
Finally, another significant limitation of this case study is that our results occupy more space than in publications addressing study protocols and results. One possible solution is to publish such information in publicly accessible data-sharing repositories [42]. For example, data and information about this case study will be publicly accessible in the Data Repository for University of Minnesota.
CONCLUSION
This case study integrated new and established approaches to collecting and reporting behavior change content within interventions, motivated by the limitations of identifying such content using data found in published reports. We collected data representing the types and dosages of the smallest potentially active behavior change ingredients from intervention materials of an ongoing optimization trial of a physical activity intervention for older adults (Ready Steady 3.0). The results include a catalog of in-depth, multidimensional specifications of inter-related BCTs, behavioral prescriptions, and their dosages, which can be organized and summarized in varied ways to strengthen future evaluations of Ready Steady 3.0‘s fidelity and intervention development. Results also accentuate the potential benefits of early, in-depth reports of intervention content while raising questions about how and where to share such information and how to maintain a detailed, up to date, understanding of individual BCTs, behavioral prescriptions, and their dosages based on synthesized evidence.
Supplementary Material
Contributor Information
Siobhan K McMahon, School of Nursing, University of Minnesota, Minneapolis, MN, USA.
Kait Macheledt, University of Minnesota School of Public Health, Minneapolis, MN, USA.
Elizabeth A Choma, DPT Doctor of Physical Therapy Program, Whitworth University, Spokane, WA, USA.
Beth A Lewis, School of Kinesiology, Minneapolis, MN, USA.
Weihua Guan, University of Minnesota School of Public Health, Minneapolis, MN, USA.
Jean F Wyman, School of Nursing, University of Minnesota, Minneapolis, MN, USA.
Alexander J Rothman, University of Minnesota, Psychology, Twin Cities, MN.
Funding
This case study was funded, in part, by the National Institutes of Nursing Research of the National Institutes of Health under Award Number 5R01NR016705-05
Compliance with Ethical Standards
Conflict of Interest: We have read and understood TBM’s policy on the declaration of interests and declare that all of the authors have no competing interests.
Human Rights: This article does not contain any studies with human participants performed by any of the authors.
Informed Consent: Ethical approval of the parent Ready Steady 3.0 study was obtained from the University of Minnesota Institutional Review Board (1607S90922). Because there are no human subjects in this case study, it was exempt from IRB approval
Welfare of Animals: This article does not contain any studies with animals
Transparency Statements: Study registration: This study was not formally registered. Analytic plan registration: The analysis plan was not pre-registered officially. Availability of data: Data from this study will be available in the Data Repository for U of M. De-identified data from this study will be made available (as allowable according to institutional IRB standards) by emailing the corresponding author. Availability of analytic code: There is no analytical code associated with this study.
References
- 1. Conn VS, Cooper PS, Ruppar TM, Russell CL.. Searching for the intervention in intervention research reports. J Nurs Scholarsh. 2008;40(1):52–59. [DOI] [PubMed] [Google Scholar]
- 2. Conn VS, Chan KC.. How much, how often, how long? Addressing dosage in intervention studies. West J Nurs Res. 2016;38(1):3–4. [DOI] [PubMed] [Google Scholar]
- 3. Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. [DOI] [PubMed] [Google Scholar]
- 4. Rothman AJ, Sheeran P.. What is slowing us down? Six challenges to accelerating advances in health behavior change. Ann Behav Med. 2020;54(12):948–959. [DOI] [PubMed] [Google Scholar]
- 5. Hoffmann, TC, Glasziou, PP, Boutron, I, Milne, R, Perera, R, Moher, D,...Michie, S.. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;34:8. [DOI] [PubMed] [Google Scholar]
- 6. Sidani S, Braden CJ.. Design, Evaluation, and Translation of Nursing Interventions. West Sussex: John Wiley & Sons, Inc.; 2011. [Google Scholar]
- 7. Voils CI, Chang Y, Crandell J, Leeman J, Sandelowski M, Maciejewski ML.. Informing the dosing of interventions in randomized trials. Contemp Clin Trials. 2012;33(6):1225–1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McVay MA, Bennett GG, Steinberg D, Voils CI.. Dose–response research in digital health interventions: concepts, considerations, and challenges. Health Psychol. 2019;38(12):1168–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Carraça E, Encantado J, Battista F, et al. Effective behavior change techniques to promote physical activity in adults with overweight or obesity: a systematic review and meta-analysis. Obes Rev. 2021;22(Suppl 4):e13258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Senkowski V, Gannon C, Branscum P.. Behavior change techniques used in theory of planned behavior physical activity interventions among older adults: a systematic review. J Aging Phys Act. 2019;27(5):746–754. [DOI] [PubMed] [Google Scholar]
- 11. French DP, Olander EK, Chisholm A, Mc Sharry J.. Which behaviour change techniques are most effective at increasing older adults’ self-efficacy and physical activity behaviour? A systematic review. Ann Behav Med. 2014;48(2):225–234. [DOI] [PubMed] [Google Scholar]
- 12. Teng B, Gomersall SR, Hatton A, Brauer SG.. Combined group and home exercise programmes in community-dwelling falls-risk older adults: systematic review and meta-analysis. Physiother Res Int. 2020;25(3):e1839. [DOI] [PubMed] [Google Scholar]
- 13. Heerman WJ, JaKa MM, Berge JM, et al. The dose of behavioral interventions to prevent and treat childhood obesity: a systematic review and meta-regression. Int J Behav Nutr Phys Act. 2017;14(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. McMahon SK, Lewis BA, Guan W, Wyman JF, Rothman AJ.. Community-based intervention effects on older adults’ physical activity and falls: protocol and rationale for a randomized optimization trial (Ready Steady3. 0). Contemp Clin Trials. 2021;101:106238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zubala A, MacGillivray S, Frost H, et al. Promotion of physical activity interventions for community dwelling older adults: a systematic review of reviews. PLoS One. 2017;12(7):e0180902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gardner B, Jovicic A, Belk C, et al. Specifying the content of home-based health behaviour change interventions for older people with frailty or at risk of frailty: an exploratory systematic review. BMJ Open. 2017;7(2):e014127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Conn VS, Groves PS.. Protecting the power of interventions through proper reporting. Nurs Outlook. 2011;59(6):318–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hekler EB, Klasnja P, Riley WT, et al. Agile science: creating useful products for behavior change in the real world. Transl Behav Med. 2016;6(2):317–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020–2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Norris E, Marques MM, Finnerty AN, et al. Development of an Intervention Setting Ontology for behaviour change: specifying where interventions take place. Wellcome Open Res. 2020;5:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Marques MM, Carey RN, Norris E, et al. Delivering behaviour change interventions: development of a mode of delivery ontology. Wellcome Open Res. 2020;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gardner MM, Buchner DM, Robertson MC, Campbell AJ.. Practical implementation of an exercise-based falls prevention programme. Age Ageing. 2001;30(1):77–83. [DOI] [PubMed] [Google Scholar]
- 23. McMahon SK, Wyman JF, Belyea MJ, Shearer N, Hekler EB, Fleury J.. Combining motivational and physical intervention components to promote fall-reducing physical activity among community-dwelling older adults: a feasibility study. Am J Heal Promot. 2015;30(8):638–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McMahon SK, Lewis B, Oakes JM, Wyman JF, Guan W, Rothman AJ.. Assessing the effects of interpersonal and intrapersonal behavior change strategies on physical activity in older adults: a factorial experiment. Ann Behav Med. 2017;51(3):376–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fluery JD. Empowering potential: a theory of wellness motivation. Nurs Res. 1991;40(5):286–291. [PubMed] [Google Scholar]
- 26. Perez A, Fleury J.. Wellness motivation theory in practice. Geriatr Nurs. 2009;30(2 Suppl):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Devereux-Fitzgerald A, Powell R, Dewhurst A, French DP.. The acceptability of physical activity interventions to older adults: a systematic review and meta-synthesis. Soc Sci Med. 2016. Dec: 158:14–23. [DOI] [PubMed] [Google Scholar]
- 28. Lindsay Smith G, Banting L, Eime R, O’Sullivan G, Van Uffelen JG.. The association between social support and physical activity in older adults: a systematic review. Int J Behav Nutr Phys Act. 2017;14(1):1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chase JAD. Interventions to increase physical activity among older adults: a meta-analysis. Gerontologist. 2015;55(4):706–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Arnautovska U, O’Callaghan F, Hamilton K.. Behaviour change techniques to facilitate physical activity in older adults: what and how. Ageing Soc. 2018;38(12):2590–2616. [Google Scholar]
- 31. Fleig L, McAllister MM, Chen P, et al. Health behaviour change theory meets falls prevention: feasibility of a habit-based balance and strength exercise intervention for older adults. Psychol Sport Exerc. 2016;22:114–122. [Google Scholar]
- 32. Kyrdalen IL, Moen K, Røysland AS, Helbostad JL.. The Otago exercise program performed as group training versus home training in fall-prone older people: a randomized controlled trial. Physiother Res Int. 2014;19(2):108–116. [DOI] [PubMed] [Google Scholar]
- 33. Thomas S, Mackintosh S, Halbert J.. Does the ‘Otago exercise programme’reduce mortality and falls in older adults? A systematic review and meta-analysis. Age Ageing. 2010;39(6):681–687. [DOI] [PubMed] [Google Scholar]
- 34. Straiton N, Alharbi M, Bauman A, et al. The validity and reliability of consumer-grade activity trackers in older, community-dwelling adults: a systematic review. Maturitas. 2018;112:85–93. [DOI] [PubMed] [Google Scholar]
- 35. W Brewer W, Swanson BT, Ortiz A.. Validity of Fitbit’s active minutes as compared with a research-grade accelerometer and self-reported measures. BMJ Open Sport Exerc Med. 2017;3(1):e000254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. JaKa MM, Wood C, Veblen-Mortenson S, et al. Applying the behavior change technique taxonomy to four multicomponent childhood obesity interventions. West J Nurs Res. 2021;43(5):468–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cane J, Richardson M, Johnston M, Ladha R, Michie S.. From lists of behaviour change techniques (BCT s) to structured hierarchies: comparison of two methods of developing a hierarchy of BCT s. Br J Health Psychol. 2015;20(1):130–150. [DOI] [PubMed] [Google Scholar]
- 38. Bellg AJ, Borrelli B, Resnick B, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol. 2004;23(5):443. [DOI] [PubMed] [Google Scholar]
- 39. Agbadjé TT, Elidor H, Perin MS, Adekpedjou R, Légaré F.. Towards a taxonomy of behavior change techniques for promoting shared decision making. Implement Sci. 2020;15(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. A Chatfield AJ. Lexicomp online and Micromedex 2.0. J Med Libr Assoc. 2015;103(2):112. [Google Scholar]
- 41. Michie S, Thomas J, Johnston M, et al. The Human Behaviour-Change Project: harnessing the power of artificial intelligence and machine learning for evidence synthesis and interpretation. Implement Sci. 2017;12(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Norris E, Sulevani I, Finnerty AN, Castro O.. Assessing Open Science practices in physical activity behaviour change intervention evaluations. medR. 202; doi: 10.1101/2021.12.01.21267126 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.