Abstract
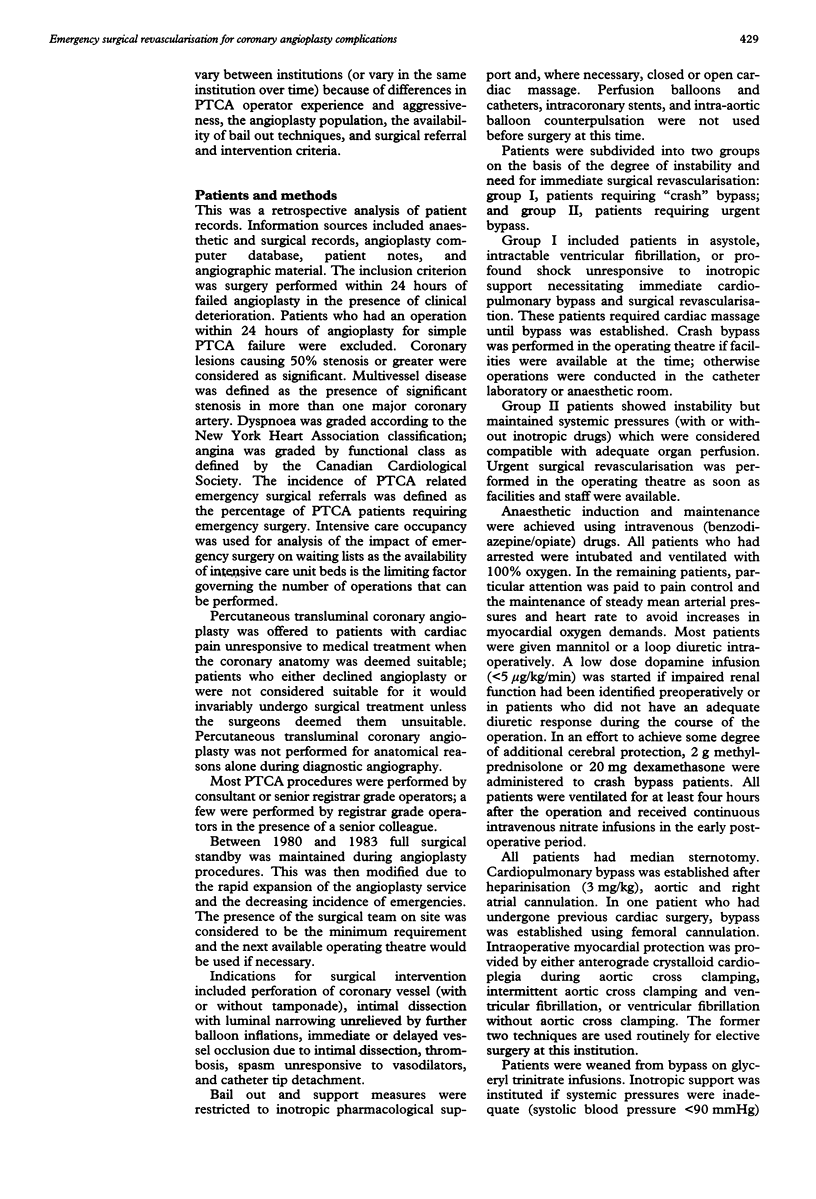
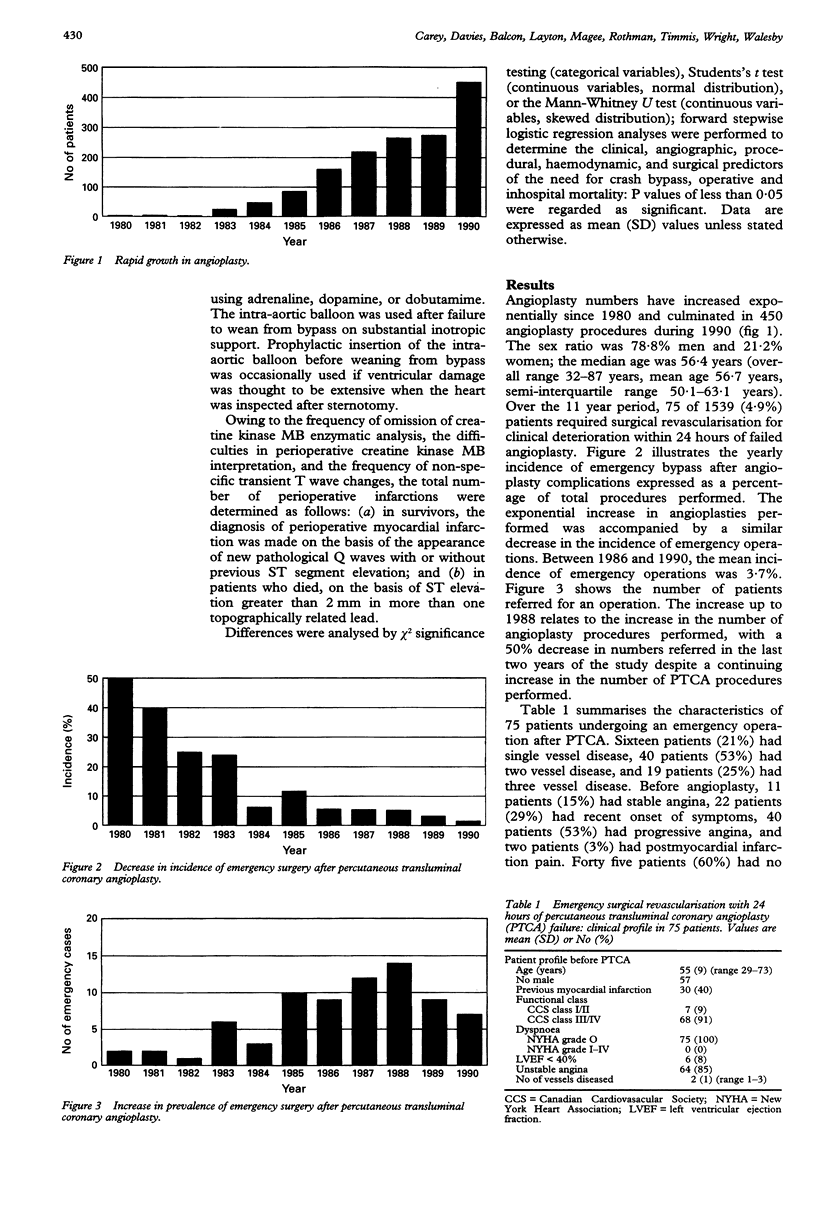
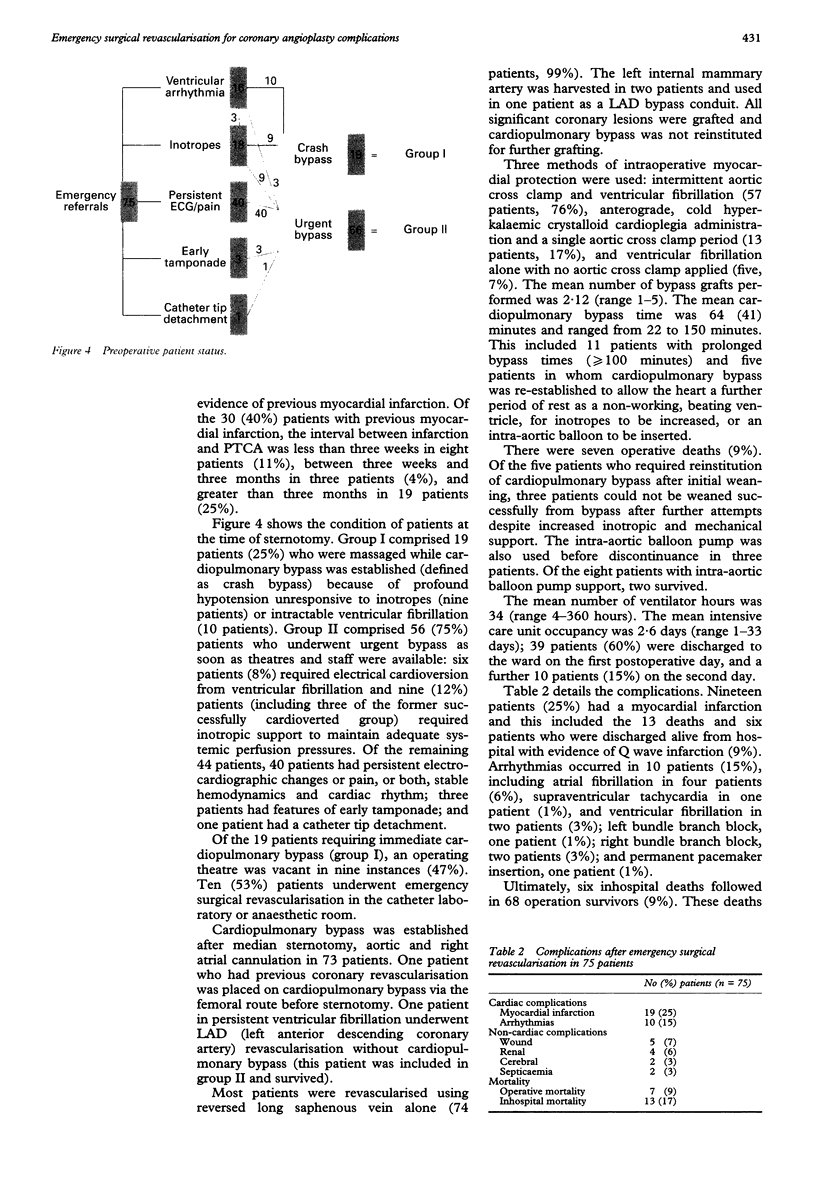
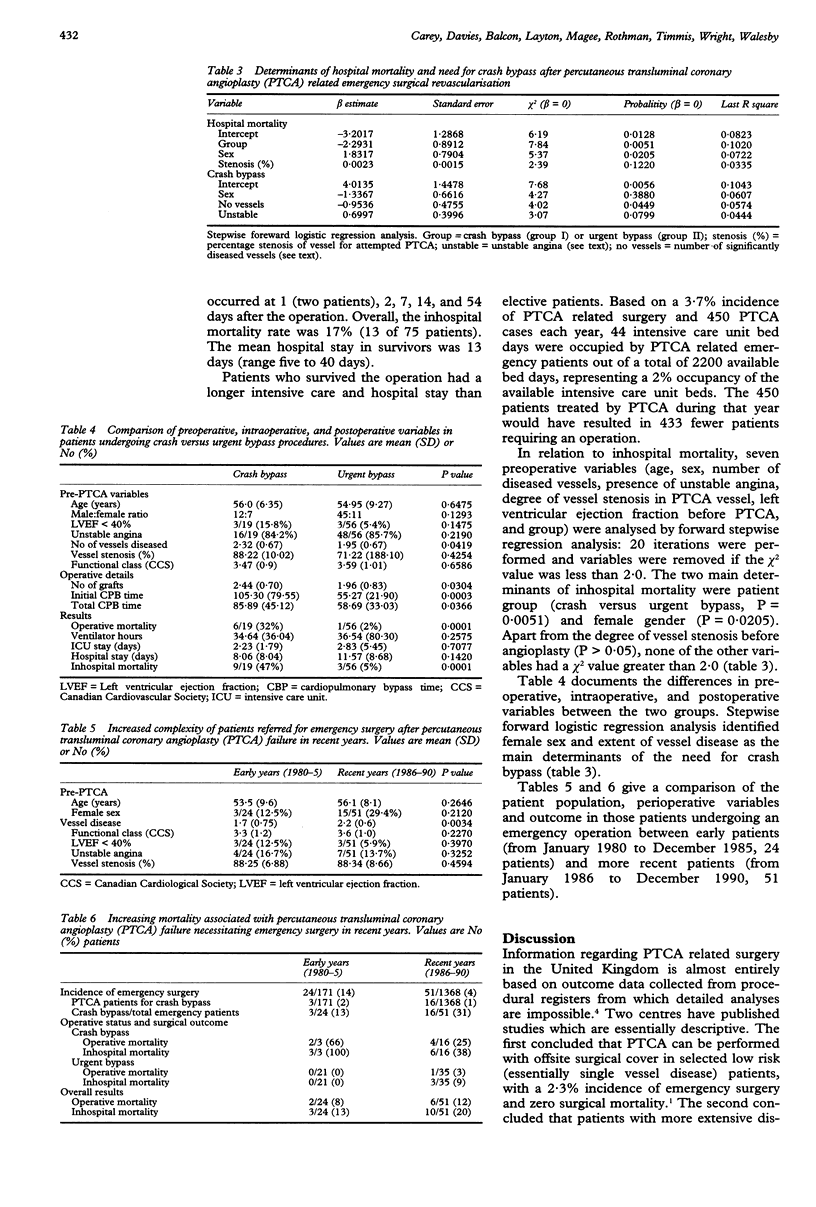
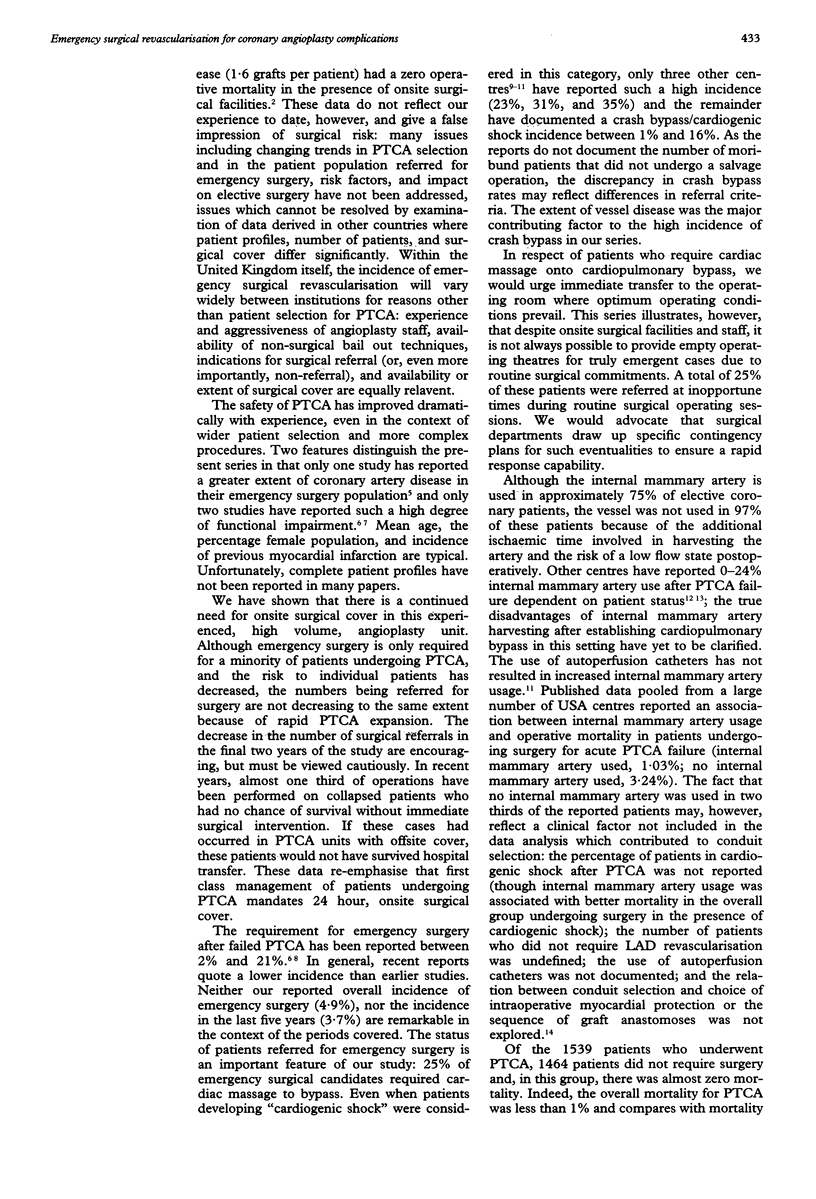
OBJECTIVES--To evaluate trends in referrals for emergency operations after percutaneous transluminal coronary angioplasty (PTCA) complications; to analyse morbidity and mortality and assess the influence of PTCA backup on elective surgery. DESIGN--A retrospective analysis of patients requiring emergency surgical revascularisation within 24 hours of percutaneous transluminal coronary angioplasty. PATIENTS--Between January 1980 and December 1990, 75 patients requiring emergency surgery within 24 hours of percutaneous transluminal coronary angioplasty. SETTING--A tertiary referral centre and postgraduate teaching hospital. RESULTS--57 patients (76%) were men, the mean age was 55 (range 29-73) years, and 30 (40%) had had a previous myocardial infarction. Before PTCA, 68 (91%) had severe angina, 59 (79%) had multivessel disease, and six (8%) had a left ventricular ejection fraction of less than 40%. A mean of 2.1 grafts (range one to five) were performed; the internal mammary artery was used in only one patient. The operative mortality was 9% and inhospital mortality was 17%. There was a need for cardiac massage until bypass was established in 19 patients (25%): this was the most important outcome determinant (P = 0.0051) and was more common in those patients with multivessel disease (P = 0.0449) and in women (P = 0.0388). In 10 of the 19 cases a vacant operating theatre was unavailable, the operation being performed in the catheter laboratory or anaesthetic room. These 19 patients had an operative mortality of 32% and inhospital mortality of 47%, compared with 2% and 7% respectively for the 56 patients who awaited the next available operating theatre. Complications included myocardial infarction, 19 patients (25%); arrhythmias, 10 patients (3%); and gross neurological event, two patients (3%). The mean intensive care unit stay was 2.6 days (range 1 to 33 days) and the mean duration of hospital admission was 13 days (range 5-40 days). CONCLUSIONS--Patients undergoing emergency surgery after PTCA complications have a substantially increased inhospital mortality and morbidity. PTCA in this unit continues to require surgical cover. Delays in operating on stable patients in centres which operate a "next available theatre" backup policy may not differ from some units performing PTCA with offsite cover for PTCA complications. Particularly in the presence of multivessel disease, however, PTCA complications may be associated with the need for "crash" bypass and such patients are unlikely to survive hospital transfer. The proportion of patients requiring "crash" bypass has increased during the period reviewed because of the extent of disease in the emergency surgical group increased. These results indicate that surgery should not be denied to these patients.
Full text
PDF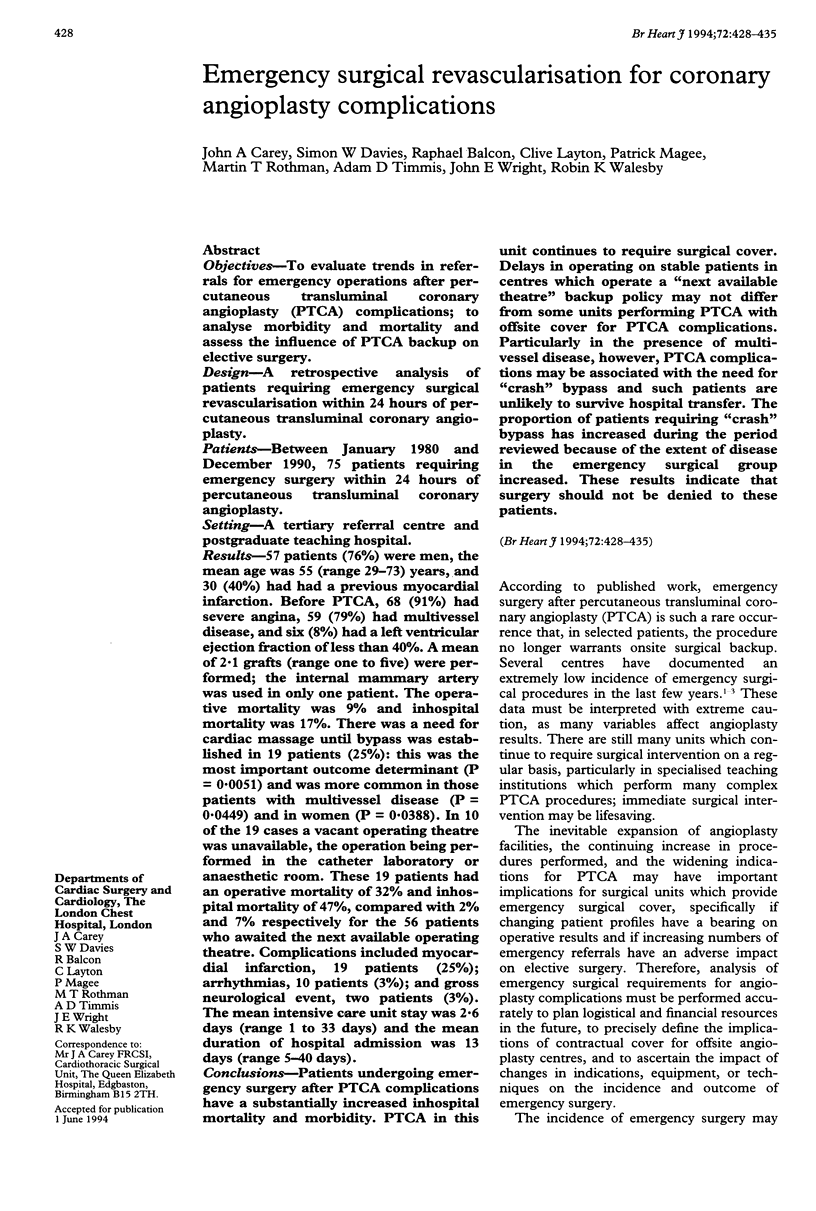
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beyersdorf F., Mitrev Z., Sarai K., Eckel L., Klepzig H., Maul F. D., Ihnken K., Satter P. Changing patterns of patients undergoing emergency surgical revascularization for acute coronary occlusion. Importance of myocardial protection techniques. J Thorac Cardiovasc Surg. 1993 Jul;106(1):137–148. [PubMed] [Google Scholar]
- Borkon A. M., Failing T. L., Piehler J. M., Killen D. A., Hoskins M. L., Reed W. A. Risk analysis of operative intervention for failed coronary angioplasty. Ann Thorac Surg. 1992 Nov;54(5):884–891. doi: 10.1016/0003-4975(92)90641-g. [DOI] [PubMed] [Google Scholar]
- Brahos G. J., Baker N. H., Ewy H. G., Moore P. J., Thomas J. W., Sanfelippo P. M., McVicker R. F., Fankhauser D. J. Aortocoronary bypass following unsuccessful PTCA: experience in 100 consecutive patients. Ann Thorac Surg. 1985 Jul;40(1):7–10. doi: 10.1016/s0003-4975(10)61159-9. [DOI] [PubMed] [Google Scholar]
- Edwards F. H., Clark R. E., Schwartz M. Impact of internal mammary artery conduits on operative mortality in coronary revascularization. Ann Thorac Surg. 1994 Jan;57(1):27–32. doi: 10.1016/0003-4975(94)90360-3. [DOI] [PubMed] [Google Scholar]
- Ellis S. G., Roubin G. S., King S. B., 3rd, Douglas J. S., Jr, Shaw R. E., Stertzer S. H., Myler R. K. In-hospital cardiac mortality after acute closure after coronary angioplasty: analysis of risk factors from 8,207 procedures. J Am Coll Cardiol. 1988 Feb;11(2):211–216. doi: 10.1016/0735-1097(88)90082-4. [DOI] [PubMed] [Google Scholar]
- Ellis S. G., Vandormael M. G., Cowley M. J., DiSciascio G., Deligonul U., Topol E. J., Bulle T. M. Coronary morphologic and clinical determinants of procedural outcome with angioplasty for multivessel coronary disease. Implications for patient selection. Multivessel Angioplasty Prognosis Study Group. Circulation. 1990 Oct;82(4):1193–1202. doi: 10.1161/01.cir.82.4.1193. [DOI] [PubMed] [Google Scholar]
- Greene M. A., Gray L. A., Jr, Slater A. D., Ganzel B. L., Mavroudis C. Emergency aortocoronary bypass after failed angioplasty. Ann Thorac Surg. 1991 Feb;51(2):194–199. doi: 10.1016/0003-4975(91)90781-k. [DOI] [PubMed] [Google Scholar]
- Huber M. S., Mooney J. F., Madison J., Mooney M. R. Use of a morphologic classification to predict clinical outcome after dissection from coronary angioplasty. Am J Cardiol. 1991 Aug 15;68(5):467–471. doi: 10.1016/0002-9149(91)90780-o. [DOI] [PubMed] [Google Scholar]
- Hubner P. J. Cardiac interventional procedures in the United Kingdom in 1989. Br Heart J. 1991 Dec;66(6):469–471. doi: 10.1136/hrt.66.6.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iñiguez A., Macaya C., Hernandez R., Alfonso F., Goicolea J., Casado J., Zarco P. Comparison of results of percutaneous transluminal coronary angioplasty with and without selective requirement of surgical standby. Am J Cardiol. 1992 May 1;69(14):1161–1165. doi: 10.1016/0002-9149(92)90929-s. [DOI] [PubMed] [Google Scholar]
- Kannel W. B. Bishop lecture. Contribution of the Framingham Study to preventive cardiology. J Am Coll Cardiol. 1990 Jan;15(1):206–211. doi: 10.1016/0735-1097(90)90203-2. [DOI] [PubMed] [Google Scholar]
- Leon M. B., Wong S. C. Intracoronary stents. A breakthrough technology or just another small step? Circulation. 1994 Mar;89(3):1323–1327. doi: 10.1161/01.cir.89.3.1323. [DOI] [PubMed] [Google Scholar]
- Levy R. D., Bennett D. H., Brooks N. H. Desirability of immediate surgical standby for coronary angioplasty. Br Heart J. 1991 Feb;65(2):68–71. doi: 10.1136/hrt.65.2.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincoff A. M., Popma J. J., Ellis S. G., Hacker J. A., Topol E. J. Abrupt vessel closure complicating coronary angioplasty: clinical, angiographic and therapeutic profile. J Am Coll Cardiol. 1992 Apr;19(5):926–935. doi: 10.1016/0735-1097(92)90272-o. [DOI] [PubMed] [Google Scholar]
- Naunheim K. S., Fiore A. C., Fagan D. C., McBride L. R., Barner H. B., Pennington D. G., Willman V. L., Kern M. J., Deligonul U., Vandormael M. C. Emergency coronary artery bypass grafting for failed angioplasty: risk factors and outcome. Ann Thorac Surg. 1989 Jun;47(6):816–823. doi: 10.1016/0003-4975(89)90010-6. [DOI] [PubMed] [Google Scholar]
- Parsonnet V., Fisch D., Gielchinsky I., Hochberg M., Hussain S. M., Karanam R., Rothfeld L., Klapp L. Emergency operation after failed angioplasty. J Thorac Cardiovasc Surg. 1988 Aug;96(2):198–203. [PubMed] [Google Scholar]
- Ralevic V., Burnstock G. Roles of P2-purinoceptors in the cardiovascular system. Circulation. 1991 Jul;84(1):1–14. doi: 10.1161/01.cir.84.1.1. [DOI] [PubMed] [Google Scholar]
- Richardson S. G., Morton P., Murtagh J. G., O'Keeffe D. B., Murphy P., Scott M. E. Management of acute coronary occlusion during percutaneous transluminal coronary angioplasty: experience of complications in a hospital without on site facilities for cardiac surgery. BMJ. 1990 Feb 10;300(6721):355–358. doi: 10.1136/bmj.300.6721.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman M. T., Davies S. W. Intracoronary stents. Br Heart J. 1992 Jun;67(6):425–427. doi: 10.1136/hrt.67.6.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiu M. F. Angioplasty: here's the proof. Br J Hosp Med. 1990 Jun;43(6):410–411. [PubMed] [Google Scholar]
- Stark K. S., Satler L. F., Krucoff M. W., Rackley C. E., Kent K. M. Myocardial salvage after failed coronary angioplasty. J Am Coll Cardiol. 1990 Jan;15(1):78–82. doi: 10.1016/0735-1097(90)90179-s. [DOI] [PubMed] [Google Scholar]
- Zapolanski A., Rosenblum J., Myler R. K., Shaw R. E., Stertzer S. H., Millhouse F. G., Zatzkis M., Wulff C., Schechtmann N. S., Siegel S. Emergency coronary artery bypass surgery following failed balloon angioplasty: role of the internal mammary artery graft. J Card Surg. 1991 Dec;6(4):439–448. doi: 10.1111/j.1540-8191.1991.tb00343.x. [DOI] [PubMed] [Google Scholar]