Abstract
Background
Out-of-hospital cardiac arrest (OHCA) is a common cause of death. Early circulatory failure is the most common reason for death within the first 48 h. This study in intensive care unit (ICU) patients with OHCA was designed to identify and characterize clusters based on clinical features and to determine the frequency of death from refractory postresuscitation shock (RPRS) in each cluster.
Methods
We retrospectively identified adults admitted alive to ICUs after OHCA in 2011–2018 and recorded in a prospective registry for the Paris region (France). We identified patient clusters by performing an unsupervised hierarchical cluster analysis (without mode of death among the variables) based on Utstein clinical and laboratory variables. For each cluster, we estimated the hazard ratio (HRs) for RPRS.
Results
Of the 4445 included patients, 1468 (33%) were discharged alive from the ICU and 2977 (67%) died in the ICU. We identified four clusters: initial shockable rhythm with short low-flow time (cluster 1), initial non-shockable rhythm with usual absence of ST-segment elevation (cluster 2), initial non-shockable rhythm with long no-flow time (cluster 3), and long low-flow time with high epinephrine dose (cluster 4). RPRS was significantly associated with this last cluster (HR, 5.51; 95% confidence interval 4.51–6.74).
Conclusions
We identified patient clusters based on Utstein criteria, and one cluster was strongly associated with RPRS. This result may help to make decisions about using specific treatments after OHCA.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13613-023-01143-8.
Keywords: Sudden death, Mode of death, Shock, Post-resuscitation, Personalized medicine
Introduction
Out-of-hospital cardiac arrest (OHCA) is a common cause of death, with an annual incidence of 46 000 cases in France [1] and over 300 000 cases in the US. Despite decades of research, the prognosis remains poor, with less than 10% of patients surviving to hospital discharge [2, 3]. Most patients die before hospital admission, and among patients admitted alive, about 70% die in the intensive care unit (ICU) [2].
Death in the ICU may occur due to refractory postresuscitation shock (RPRS), or to hypoxic–ischemic brain injury [brain death or withdrawal of life-sustaining treatments (WLST)] [4–6]. Tailoring the treatment strategy to the most likely mechanism of death might improve outcomes. Interventions specifically designed to prevent death from RPRS include steroids [7–10], ciclosporine [11], extracorporeal support [12, 13], and goal-directed hemodynamic optimization [14–16]. Until now, trials testing these interventions have failed to show benefits. However, considering the heterogeneity of OHCA, specific interventions could have variable effects (both in magnitude and direction of treatment effect), also known as heterogeneity of treatment effect. To address this issue in other heterogenous syndromes, identification of homogenous clusters has been proposed to personalize treatment (in acute respiratory distress syndrome [17], or sepsis [18]), to offer the right therapy to the right patient. Accordingly, recent guidelines indicate that the treatment of OHCA should target goals determined on a case-by-case basis [19]. Contrary to this recommendation, the above-listed trials included unselected patients, most of whom died of events other than RPRS. Patient selection for specific treatment would require the identification of factors associated with death from RPRS. This goal could be achieved by using clustering techniques to reveal commonalities and identify uniform patient profiles within a heterogenous population.
The objective of this unsupervised clustering analysis of data from a prospectively established population-based registry was to identify patient subgroups with similar baseline features then to determine whether any of these subgroups was at particularly high risk for RPRS.
Methods
This study is reported according to strengthening the Reporting of Observational studies in Epidemiology guidelines [20]. We performed a population-based observational study, with a retrospective unsupervised clustering analysis of prospectively collected data from a multicentric cohort in France, between May 15, 2011, and December 31, 2018.
Population
In Paris and its inner suburbs, which have a population of about 6.8·million, patients with OHCA are managed on-scene by mobile emergency units and fire departments. Those who achieve the return of spontaneous circulation (ROSC) are taken to an ICU in a tertiary hospital. Since May 2011, these patients, if older than 18 years, are recorded in a prospective multicenter population-based registry managed by the Paris-Sudden Death Expertise Center [2, 21, 22]. The appropriate ethics committees approved the registry (CNIL approval #912309 and CCTIRS approval #12336).
We retrospectively studied the data recorded in the registry between May 15, 2011, and December 31, 2018. We included only patients with OHCA due to cardiac causes. We did not include patients with OHCA due to external factors (e.g., trauma, overdose, or drowning) [23], patients for whom no identifying data were available (unknown patients), or patients whose reason for death was unknown or unclassifiable according to Witten et al.[6] In order to be representative, we included all patients with OHCA due to cardiac causes recorded in this registry, consecutively and without selection. No sample size calculation was performed.
Data collection
Data were collected prospectively in the registry according to Utstein criteria [24], including sex, age, presence of a witness, cardiopulmonary resuscitation (CPR) performed by a bystander, location of the OHCA (home vs. public place), first-recorded cardiac rhythm, total epinephrine dose delivered by emergency medical staff during advanced life support, no-flow time (time from collapse to the initiation of CPR) and low-flow time (time from the initiation of CPR to the ROSC), targeted temperature management, arterial lactate and serum creatinine at ICU admission, use of vasoactive drugs (epinephrine, norepinephrine), ST-segment elevation, and percutaneous coronary intervention.
Two intensivists (YB and MR) independently reviewed the hospital records of each patient and categorized the reason for death as follows (adapted from Witten et al.[6]): RPRS, defined as refractory hemodynamic shock considered secondary to OHCA, including subsequent multiorgan failure, leading to death despite aggressive critical care (e.g., vasopressive or mechanical support); brain death; recurrent cardiac arrest; WLST warranted by severe hypoxic–ischemic brain injury, and WLST warranted by comorbidities.
Statistical analysis
We described categorical variables as proportions and continuous variables as median [interquartile range]. Comparisons were performed with Pearson’s Chi-square test for categorical variables and Student’s t-test or Wilcoxon’s rank sum test for continuous variables. Agreement between the two investigators who determined the reason for death was assessed by computing the kappa coefficient.
Once clusters were identified, we compared differences using Pearson’s Chi-square test for categorical variables and ANOVA or Kruskal–Wallis test for continuous variables. Under the missing-at-random assumption, we imputed missing data for covariates using multiple imputations by chained equations, with logistic models for binary variables and predictive mean-matching for continuous variables. We created 20 datasets with missing values replaced by imputed values.
Hierarchical cluster analysis
We performed an unsupervised hierarchical cluster analysis (without reason for death among the clustering variables) based on Utstein variables including sex, age, presence of a witness, bystander CPR, location of the OHCA, first-recorded cardiac rhythm, total epinephrine dose delivered during advanced life support, no-flow and low-flow times, arterial lactate and serum creatinine at ICU admission. We sought to maximize within-cluster uniformity and to maximize differences across clusters. Hierarchical cluster analysis was used to identify the optimal number of clusters according to the minimal relative inertia loss [25]. The steps of this hierarchical cluster analysis were as follows. First, the clinical and laboratory variables were processed by dimensionality reduction using factor analysis of mixed data to correct for multicollinearity and to reduce data noise [26, 27]. We relied on the explained total inertia to determine the number of variables to include in the model. Ten dimensions (i.e., linear combinations of variables) explained 83% of the total inertia and were kept in the model. Second, to identify the optimal number of clusters, we included these ten dimensions in a hierarchical cluster analysis using Euclidean distance measures, with Ward’s linkage criterion [28] to minimize total within-cluster inertia. Third, we optimized within-cluster uniformity by using the k-means method to consolidate the optimal number of clusters. To determine the ideal number of clusters, we employed the elbow method [29, 30], identifying the point at which the decrease in within-cluster variability becomes flat. We assessed the reproductivity of the clustering using bootstrap dataset. Finally, we described the characteristics of the identified clusters by computing the V-test score to reflect the rank importance of each variable in each cluster. For a given cluster, a positive V-test score (≥ 1.96) for a variable indicates that this variable is overrepresented in the cluster compared to other clusters. By contrast, a negative V-test score (≤ − 1.96) indicates that the variable is underrepresented in the cluster.
Survival analyses
We performed survival analyses to assess the cumulative risk of RPRS in each cluster. The analysis period started at ICU admission and the time-to-event analysis was censored at the date of death or of ICU discharge alive. The proportionality assumption was assessed via log–log (survival) vs. log (time) plots. We described the incidence of RPRS in each cluster, using the Nelson–Aalen non-parametric estimator to account for competing risks. The global Gray test was applied to compare survivor function equality. In our analysis, death for reasons other than RPRS were competing risks. Fine and Gray proportional hazards regression models, accounting for competing risks [31], were built to estimate the hazard ratios (HRs) of RPRS associated with each cluster. We also performed a sensitivity analysis by applying the Kaplan–Meier method and log-rank tests to assess the significance of differences across clusters and by building Cox models to estimate the HRs.
All analyses were two-sided with a significance level of 0.05. We used RStudio version 1.4.1103 (RStudio PBC, Boston, MA) for the statistical analyses.
Results
Figure 1 is the patient flowchart. Between May 15, 2011, and December 31, 2018, 4635 patients were admitted alive to ICUs after OHCA without external causes, and 4445 were enrolled in the study, including 1468 (33%) who survived to ICU discharge and 2977 who died in the ICU (67%).
Fig. 1.
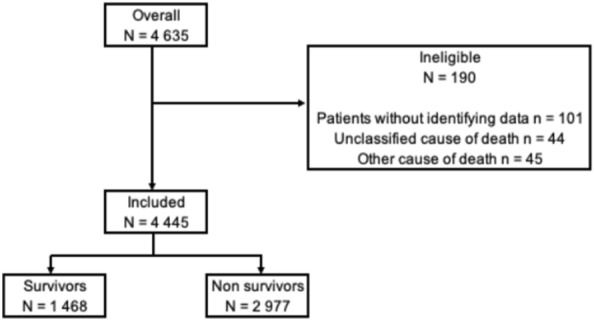
Patient flowchart
Baseline characteristics
Table 1 reports the main baseline characteristics of the 4445 study patients and compares the survivors and nonsurvivors. Overall, 528 patients treated with ECMO were included (12% of the whole population). The main reason for death in the ICU was WLST warranted by hypoxic–ischemic brain injury (1034/2977, 35%), followed by RPRS (832/2977, 28%). Brain death occurred in 481 (481/2977, 16%) patients. Agreement between investigators regarding classification of the reason for death was good, with a kappa coefficient of 0.87.
Table 1.
Baseline characteristics of the 4445 study patients
| Characteristics | Overall population N = 4445 |
Nonsurvivorsa N = 2977 |
Survivorsa N = 1468 |
P valueb |
|---|---|---|---|---|
| Males, n (%) | 3112 (70) | 1999 (67) | 1113 (76) | < 0.001 |
| Age (years), median [IQR] | 62 [51–73] | 64 [53–75] | 57 [48–68] | < 0.001 |
| Witnessed, n (%) | 4001 (90) | 2591 (87) | 1410 (96) | < 0.001 |
| Bystander CPR, n (%) | 2985 (75) | 1798 (69) | 1187 (85) | < 0.001 |
| OHCA in a public area, n (%) | 1871 (42) | 1023 (34) | 848 (58) | < 0.001 |
| Shockable rhythm, n (%) | 2217 (53) | 1053 (37) | 1164 (85) | < 0.001 |
| No-flow timec (min), median [IQR] | 3.0 [0.0–8.0] | 5.0 [0.0–10.0] | 1.0 [0.0–5.0] | < 0.001 |
| Low-flow timed (min), median [IQR] | 22 [14–35] | 26 [17–40] | 15 [10–23] | < 0.001 |
| ST-segment elevation, n (%) | 1602 (45) | 866 (38) | 736 (56) | < 0.001 |
| Epinephrine dose (mg), median [IQR] | 2.0 [0.0–4.0] | 3.0 [1.0–5.0] | 0.0 [0.0–1.0] | < 0.001 |
| TTM, n (%) | 2300 (53) | 1425 (49) | 875 (62) | < 0.001 |
| Vasoactive drugs, n (%) | 2735 (66) | 2060 (75) | 675 (49) | < 0.001 |
| Successful angioplasty, n (%) | 1201 (27) | 614 (21) | 587 (40) | < 0.001 |
| Lactate (mmol/L), median [IQR] | 5.8 [2.9–10.6] | 7.9 [4.4–12.5] | 2.9 [1.7– 4.8] | < 0.001 |
| Creatinine (µmol/L), median [IQR] | 112 [86–145] | 126 [98–162] | 92 [75–116] | < 0.001 |
| Patients treated with ECMO, n (%) | 528 (12) | 442 (15) | 86 (6) | <0.001 |
CPR cardiopulmonary resuscitation, ROSC return of spontaneous circulation, TTM targeted temperature management
aSurvival was determined at discharge from the intensive care unit
bχ2 test for categorical variables, Student’s t-test or Wilcoxon’s rank sum test for continuous variables
cNo-flow time was the time from collapse to the initiation of cardiopulmonary resuscitation
dLow-flow time was the time from the initiation of cardiopulmonary resuscitation to the return of spontaneous circulation
Additional file 1: Fig. S1: shows the times for each reason for death. Of the 832 cases of RPRS, 772 (93%) occurred within 3 days after ICU admission. In contrast, of the 1034 patients with WLST for hypoxic–ischemic brain injury, 777 (75%) died on day 4 or later
Hierarchical cluster analysis
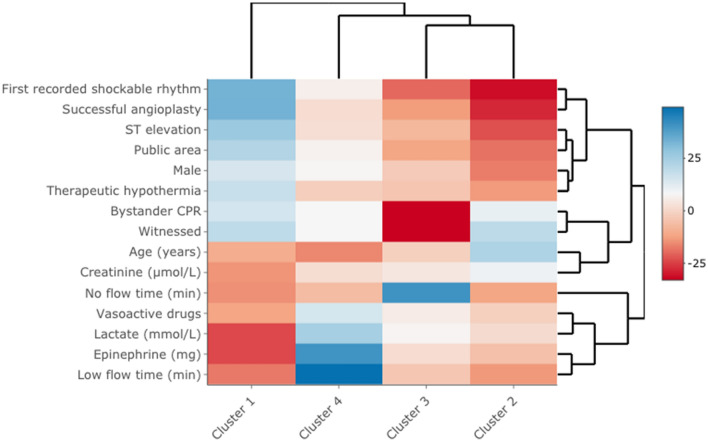
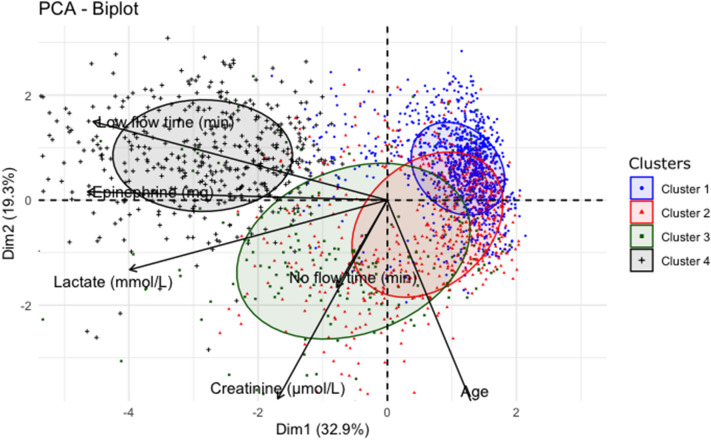
Ten dimensions explained 83% of the total inertia and were used to build the model. Unsupervised hierarchical clustering identified four clusters, with 1619, 1528, 727, and 571 patients, respectively (Table 2, Fig. 2, and Additional file 2: Fig. S2). Compared to the other clusters, cluster 1 had characteristics of “male with ischemic OHCA”: larger proportions of shockable rhythms, ST-segment elevation, and a higher proportion of angioplasty. Cluster 2 included mostly “women with non-ischemic OHCA”: smaller proportions of shockable rhythms, fewer ST-segment elevation, and fewer males. Cluster 3 was characterized by “non-witnessed, delayed treated OHCA”: fewer patients had a witness and received bystander CPR, resulting in a longer no-flow time. Finally, patients in cluster 4 had “difficult to treat OHCA, with aggressive and prolonged resuscitation”: higher epinephrine doses during resuscitation, longer low-flow times, and higher serum lactate levels at ICU admission. The two-dimensional biplot representation highlights the main differences across clusters (Fig. 3). Sensitivity analysis using bootstrap showed a strong reproductivity of the clusters.
Table 2.
Utstein clinical and laboratory features in each of the four clusters (imputed model)
| Characteristics | Cluster 1 N = 1619 |
Cluster 2 N = 1528 |
Cluster 3 N = 727 |
Cluster 4 N = 571 |
P valuea |
|---|---|---|---|---|---|
| Prehospital characteristics | |||||
| Males, n (%) | 1344 (83) | 822 (54) | 472 (65) | 474 (83) | < 0.001 |
| Age (years), median [IQR] | 58 [49–68] | 69 [60–80] | 61 [50–72] | 53 [44–61] | < 0.001 |
| Witnessed, n (%) | 1615 (100) | 1528 (100) | 299 (41) | 561 (98) | < 0.001 |
| Bystander CPR, n (%) | 1324 (82) | 1208 (78) | 6 (0.9) | 466 (82) | < 0.001 |
| OHCA in public area, n (%) | 1032 (64) | 358 (23) | 167 (23) | 315 (55) | < 0.001 |
| Shockable rhythm, n (%) | 1511 (93) | 324 (21) | 142 (19) | 370 (65) | < 0.001 |
| No-flowb (min), median [IQR] | 2 [0–5] | 2 [0–5] | 15 [10–20] | 2 [0–5] | < 0.001 |
| Low-flowc (min), median [IQR] | 18 [10–26] | 20 [13–30] | 25 [15–34] | 80 [52–100] | < 0.001 |
| ST-segment elevation, n (%) | 1149 (71) | 334 (22) | 227 (31) | 278 (49) | < 0.001 |
|
Epinephrine dose (mg) Median [IQR] |
0 [0–2] | 2 [1–4] | 3 [1–4] | 8 [5–11] | < 0.001 |
| Hospital management | |||||
| TTM, n (%) | 1142 (71) | 601 (39) | 335 (46) | 280 (49) | < 0.001 |
| Vasoactive drugs, n (%) | 902 (56) | 986 (65) | 552 (76) | 525 (92) | < 0.001 |
| Angioplasty success, n (%) | 933 (58) | 69 (4.5) | 68 (9.4) | 176 (31) | < 0.001 |
| Lactate (mmol/L), median [IQR] |
3.4 [1.9–5.7] |
6.5 [3.4– 11.0] |
8.1 [4.2– 13.0] |
12.4 [8.5– 17.0] |
< 0.001 |
| Creatinine (µmol/L), median [IQR] |
97 [78–121] |
124 [93–170] |
124 [93–164] |
132 [105–160] |
< 0.001 |
| Patients treated with ECMO, n (%) | 107 (7) | 39 (3) | 23 (3) | 359 (63) | < 0.001 |
| Follow-up (days), median [IQR] | 6 [3–10] | 2 [1–7] | 2 [1–6] | 1 [0–4] | < 0.001 |
CPR cardiopulmonary resuscitation, TTM targeted temperature management
aχ2 test for categorical variables, ANOVA or Kruskal–Wallis test for continuous variables
bNo-flow was the time from collapse to the initiation of cardiopulmonary resuscitation
cLow-flow was the time from the initiation of cardiopulmonary resuscitation to the return of spontaneous circulation
Fig. 2.
Heatmap (v-test score scale) of clinical and laboratory variables in each of the four clusters. A V-test score ≥ 1.96 or ≤ − 1.96 was taken as the cutoff indicating variable over- or underrepresentation in clusters. For example, in cluster 1, a first-recorded shockable rhythm was significantly overrepresented (V-test score, 33; blue color), whereas no-flow time was shorter than in the other clusters (V-test score, − 14.9; red color)
Fig. 3.
Biplot representation of clinical and laboratory variables in each of the four clusters. PCA principal component analysis, Dim dimension
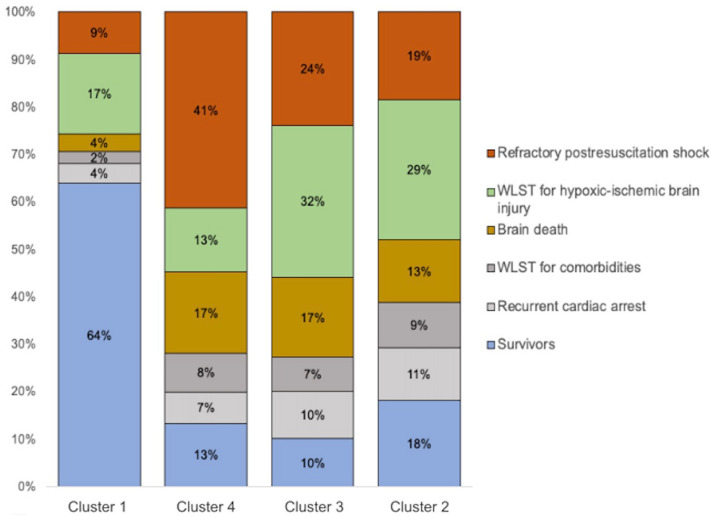
Vital status and reason for death differed significantly across clusters (Fig. 4). Survival was significantly higher in cluster 1 (1036/1619, 64%) than in each of the other three clusters (P < 0.01 for all comparisons). RPRS was significantly more common in cluster 4 (237/571, 41%) than in each of the other clusters (P < 0.01 for all comparisons).
Fig. 4.
Vital status and reasons for death in each of the four clusters. WLST withdrawal of life-sustaining treatments
Survival analysis
Median follow-up was 6 days [4–12 days] in survivors and 2 days [1–6 days] in nonsurvivors. The unadjusted cumulative hazard functions for RPRS differed significantly across clusters (P < 0.001, global Gray test) (Fig. 5). The incidence of RPRS was significantly higher in cluster 4 compared to each of the other clusters (P < 0.001 for all comparisons) and significantly lower in cluster 1 compared to each of the other clusters (Table 3). The sensitivity analysis done using Kaplan–Meier and Cox models showed similar results with a significant difference across clusters (P < 0.001, global log-rank test) and a significant association between cluster 4 and RPRS (HR, 3.12; 95% CI 2.35–4.14).
Fig. 5.
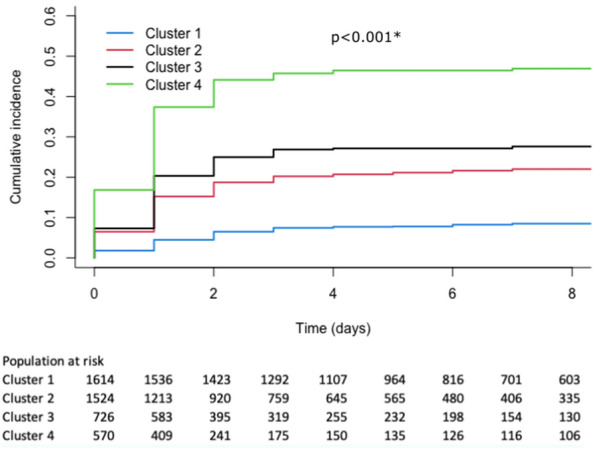
Cumulative incidence of refractory postresuscitation shock (RPRS) in each of the four clusters
Table 3.
Hazard ratios (Fine and Gray) for refractory postresuscitation shock associated with each cluster
| Eventsa | HR | 95%CI | P value | |
|---|---|---|---|---|
| Cluster 1 | 140 | Reference | – | |
| Cluster 2 | 284 | 2.20 | 1.80–2.68 | < 0.001 |
| Cluster 3 | 171 | 2.82 | 2.26–3.50 | < 0.001 |
| Cluster 4 | 237 | 5.51 | 4.51–6.74 | < 0.001 |
HR hazard ratio, 95%CI 95% confidence interval
aDeaths due to refractory postresuscitation shock
Discussion
Our population-based, real-life study utilized an innovative, unsupervised clustering analysis that yielded several important findings. Firstly, two-thirds of patients admitted to the ICU after OHCA died before ICU discharge, with RPRS accounting for 28% of these deaths. Secondly, we identified four distinct clusters based on their baseline characteristics. Notably, one of these clusters was characterized by longer low-flow times, higher epinephrine doses and higher lactate levels. Finally, patients in this cluster were found to be at a significantly higher risk of RPRS, indicating the potential importance of targeted interventions aimed at this mode of death.
In our large population-based registry, among patients admitted alive after OHCA, ICU mortality was 67%. This result is consistent with previous studies (61% [4], 66% [5], and 57% [32]) and with a 2020 meta-analysis [33]. To strengthen our analysis, we used a previously published classification to characterize the reasons for death [6] and adjudication of the reason for death was performed by two independent investigators. Regarding mode of death, our population is in line with previous data, the most common reasons (51%) being neurological death (brain death or WLST for hypoxic–ischemic brain injury) [5, 6, 34]. We also evaluated the time to death in the ICU for each reason. There again, our data confirmed previously published populations, with over 90% of deaths from RPRS occurring during the first 3 days [5]. Overall, our findings in a large population provide external validation of previous data, and mortality, mode and timing of deaths of our patients are highly similar with other studies, reinforcing the external validity of our results. The adjudication of the reason for death by two independent investigators is among the strengths of our study.
RPRS is a complication of postresuscitation disease, which is due to both the underlying cause of OHCA and ischemia–reperfusion syndrome [19, 35–37]. Postresuscitation disease can combine myocardial dysfunction [38–40], vasoplegia [41–43], and relative adrenal insufficiency [42, 44]. Interventions being evaluated for preventing RPRS include steroids [7–10], ciclosporine [11], and goal-directed hemodynamic optimization [14–16]. These interventions have not been proven beneficial in unselected populations but have not been evaluated in patient subgroups defined by their risk of specific adverse outcomes. Two previous studies looked for factors associated with a higher risk of circulatory death. In a multicenter cohort of 956 patients, a model based on five factors had an area under the receiver-operating-characteristics curve of 0.73 for predicting RPRS [32]; and in a single-center study of 303 patients, arterial pH below 7.11 and need for vasoactive drugs at ICU admission were associated with RPRS [45]. In contrast to previous studies, which utilized a smaller set of variables and a priori selection of variables, our analysis included 10 dimensions (linear combination of variables) and a larger set of variables in an unselected population. Our data-driven approach enabled an agnostic exploration of the data, and we performed a centralized, double-adjudicated mode of death, which is a significant strength compared to the two studies cited. This rigorous and comprehensive approach provides greater confidence in the accuracy and reliability of our findings. The cluster 4 had specific features that might prove helpful in selecting patients and designing post hoc analyses of treatments targeting RPRS (for example, arginine-vasopressin and/or hydrocortisone, NCT04591990). Ideally, clustering of patients should allow for the identification of RCT candidates as early as possible after ROSC. However, our methodology requires information on interventions such as angioplasty or hypothermia that are only available after ICU admission.
Cluster 1 had large proportions of patients with first-recorded shockable rhythms, angioplasty, with shorter no-flow and low-flow times at ICU admission. Consistent with these favorable characteristics, survival was highest and the frequency of RPRS lowest in this cluster. Patients in cluster 2 rarely had a first-recorded shockable rhythm or ST-segment elevation and had short no-flow times, contrasting with the long no-flow times in cluster 3. Most patients in these two clusters (2 and 3) died after WLST warranted by hypoxic–ischemic brain injury. They might constitute the population most likely to benefit from neuroprotective treatments such as targeted temperature management.
Our study has several strengths. To the best of our knowledge, it is the largest in its field. The reason for death was adjudicated centrally by two investigators working independently from each other. Moreover, interobserver agreement was good (Kappa 0.87, compared to 0.61 in a previous study [6]). Competing risks are a major issue in studies of OHCA and we accounted for them by using a Fine and Gray model. Our population was composed of consecutive unselected patients managed at multiple centers in the real-life setting. Finally, we conducted an unsupervised clustering analysis to distinguish patient subgroups, thereby acquiring additional information over that provided by studies of overall mortality.
The limitations of our study include missing data for some of the variables. Nonetheless, we performed multiple imputation to circumvent this issue. We were unable to include echocardiographic parameters among the variables used to characterize patients and clusters. However, confining the study to variables immediately available at ICU admission, even to clinicians without echocardiography skills, can also be seen as an advantage. Furthermore, the multicentric nature of our registry presents a potential risk of bias. There is a possibility of different definitions of RPRS (which could lead to outcome detection bias) and variations in the timing of lactate measurement or ICU treatment strategies due to local policies. However, most of the variables included in our analysis are independent of local practices, and we believe that the advantages provided by the multicentric design outweigh the potential disadvantages. We cannot exclude residual confounding by unmeasured factors. Firstly, we were unable to collect data on comorbidities or past medical history of patients, which could have been useful for clustering analysis, but were not available in our database, potentially leading to information bias. Secondly, due to limited availability, echocardiographic parameters could not be included in our characterization of patients and clusters. Finally, although lactate and creatinine were included as biological markers, some data such as pH were not available. Nevertheless, the dimensions used to build our model explained 83% of the total inertia. Further prospective work is needed to assess our cluster analysis results.
Conclusion
In this population-based unsupervised clustering analysis of over 4400 patients, we identified a specific subpopulation at high risk for death from RPRS. These patients might be most likely to benefit from interventions targeting shock.
Supplementary Information
Additional file 1: Fig. S1. Times of deaths due to the five reasons, in days since admission to the intensive care unit.
Additional file 2: Fig. S2. Hierarchical clustering.
Acknowledgements
We thank Antoinette Wolfe, M.D. (Issy-les-Moulineaux, France), for helping to prepare the manuscript.
Complete list of Sudden-Death-Expertise-Center investigators: Adnet F, Agostinucci JM, Aissaoui-Balanant N, Algalarrondo V, Alla F, Alonso C, Amara W, Annane D, Antoine C, Aubry P, Azoulay E, Beganton F, Billon C, Bougouin W, Boutet J, Bruel C, Bruneval P, Cariou A, Carli P, Casalino E, Cerf C, Chaib A, Cholley B, Cohen Y, Combes A, Coulaud JM, Crahes M, Da Silva D, Das V, Demoule A, Denjoy I, Deye N, Diehl JL, Dinanian S, Domanski L, Dreyfuss D, Duboc D, Dubois-Rande JL, Dumas F, Duranteau J, Empana JP, Extramiana F, Fagon JY, Fartoukh M, Fieux F, Gabbas M, Gandjbakhch E, Geri G, Guidet B, Halimi F, Henry P, Hidden Lucet F, Jabre P, Joseph L, Jost D, Jouven X, Karam N, Kassim H, Lacotte J, Lahlou-Laforet K, Lamhaut L, Lanceleur A, Langeron O, Lavergne T, Lecarpentier E, Leenhardt A, Lellouche N, Lemiale V, Lemoine F, Linval F, Loeb T, Ludes B, Luyt CE, Maltret A, Mansencal N, Mansouri N, Marijon E, Marty J, Maury E, Maxime V, Megarbane B, Mekontso-Dessap A, Mentec H, Mira JP, Monnet X, Narayanan K, Ngoyi N, Perier MC, Piot O, Pirracchio R, Plaisance P, Plaud B, Plu I, Raphalen JH, Raux M, Revaux F, Ricard JD, Richard C, Riou B, Roussin F, Santoli F, Schortgen F, Sharifzadehgan A, Sharshar T, Sideris G, Similowski T, Spaulding C, Teboul JL, Timsit JF, Tourtier JP, Tuppin P, Ursat C, Varenne O, Vieillard-Baron A, Voicu S, Wahbi K, Waldmann V.
Abbreviations
- CPR
Cardiopulmonary resuscitation
- ICU
Intensive care unit
- IQR
Interquartile range
- HR
Hazard ratio
- OHCA
Out-of-hospital cardiac arrest
- RPRS
Refractory postresuscitation shock
- ROSC
Return of spontaneous circulation
- WLST
Withdrawal of Life-Sustaining Treatments
Author contributions
YB, MR and WB analyzed and interpreted data and wrote the manuscript; YY contributed to formal analysis and methodology of the project; FD, DJ, LL, EM, XJ contributed to project administration; FB collected data and performed data curation; AC supervised the project and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Appropriate Institutional Review Boards approved the investigation (CNIL approval #912309 and CCTIRS approval #12336) and with waiver of informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Wulfran Bougouin, Email: wulfran.bougouin@gmail.com.
the Sudden-Death-Expertise-Center investigators:
F. Adnet, J. M. Agostinucci, N. Aissaoui-Balanant, V. Algalarrondo, F. Alla, C. Alonso, W. Amara, D. Annane, C. Antoine, P. Aubry, E. Azoulay, F. Beganton, C. Billon, W. Bougouin, J. Boutet, C. Bruel, P. Bruneval, A. Cariou, P. Carli, E. Casalino, C. Cerf, A. Chaib, B. Cholley, Y. Cohen, A. Combes, J. M. Coulaud, M Crahes, D. Da Silva, V. Das, A. Demoule, I. Denjoy, N. Deye, J. L. Diehl, S. Dinanian, L. Domanski, D. Dreyfuss, D. Duboc, J. L. Dubois-Rande, F. Dumas, J. Duranteau, J. P. Empana, F. Extramiana, J. Y. Fagon, M. Fartoukh, F. Fieux, M. Gabbas, E. Gandjbakhch, G. Geri, B. Guidet, F. Halimi, P. Henry, F. Hidden Lucet, P. Jabre, L. Joseph, D. Jost, X. Jouven, N. Karam, H. Kassim, J. Lacotte, K. Lahlou-Laforet, L. Lamhaut, A. Lanceleur, O. Langeron, T. Lavergne, E. Lecarpentier, A. Leenhardt, N. Lellouche, V. Lemiale, F. Lemoine, F. Linval, T. Loeb, B. Ludes, C. E. Luyt, A. Maltret, N. Mansencal, N. Mansouri, E. Marijon, J. Marty, E. Maury, V. Maxime, B. Megarbane, A. Mekontso-Dessap, H. Mentec, J. P. Mira, X. Monnet, K. Narayanan, N. Ngoyi, M. C. Perier, O. Piot, R. Pirracchio, P. Plaisance, B. Plaud, I. Plu, J. H. Raphalen, M. Raux, F. Revaux, J. D. Ricard, C. Richard, B. Riou, F. Roussin, F. Santoli, F. Schortgen, A. Sharifzadehgan, T. Sharshar, G. Sideris, T. Similowski, C. Spaulding, J. L. Teboul, J. F. Timsit, J. P. Tourtier, P. Tuppin, C. Ursat, O. Varenne, A. Vieillard-Baron, S. Voicu, K. Wahbi, and V. Waldmann
References
- 1.Luc G, Baert V, Escutnaire J, Genin M, Vilhelm C, Di Pompéo C, et al. Epidemiology of out-of-hospital cardiac arrest: a French national incidence and mid-term survival rate study. Anaesth Crit Care Pain Med. 2019;38:131–135. doi: 10.1016/j.accpm.2018.04.006. [DOI] [PubMed] [Google Scholar]
- 2.Bougouin W, Lamhaut L, Marijon E, Jost D, Dumas F, Deye N, et al. Characteristics and prognosis of sudden cardiac death in Greater Paris: population-based approach from the Paris Sudden Death Expertise Center (Paris-SDEC) Intensive Care Med. 2014;40:846–854. doi: 10.1007/s00134-014-3252-5. [DOI] [PubMed] [Google Scholar]
- 3.Nakahara S, Tomio J, Ichikawa M, Nakamura F, Nishida M, Takahashi H, et al. Association of bystander interventions with neurologically intact survival among patients with bystander-witnessed out-of-hospital cardiac arrest in Japan. JAMA. 2015;314:247–254. doi: 10.1001/jama.2015.8068. [DOI] [PubMed] [Google Scholar]
- 4.Laver S, Farrow C, Turner D, Nolan J. Mode of death after admission to an intensive care unit following cardiac arrest. Intensive Care Med. 2004;30:2126–2128. doi: 10.1007/s00134-004-2425-z. [DOI] [PubMed] [Google Scholar]
- 5.Lemiale V, Dumas F, Mongardon N, Giovanetti O, Charpentier J, Chiche J-D, et al. Intensive care unit mortality after cardiac arrest: the relative contribution of shock and brain injury in a large cohort. Intensive Care Med. 2013;39:1972–1980. doi: 10.1007/s00134-013-3043-4. [DOI] [PubMed] [Google Scholar]
- 6.Witten L, Gardner R, Holmberg MJ, Wiberg S, Moskowitz A, Mehta S, et al. Reasons for death in patients successfully resuscitated from out-of-hospital and in-hospital cardiac arrest. Resuscitation. 2019;136:93–99. doi: 10.1016/j.resuscitation.2019.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mentzelopoulos SD, Zakynthinos SG, Tzoufi M, Katsios N, Papastylianou A, Gkisioti S, et al. Vasopressin, epinephrine, and corticosteroids for in-hospital cardiac arrest. Arch Intern Med. 2009;169:15–24. doi: 10.1001/archinternmed.2008.509. [DOI] [PubMed] [Google Scholar]
- 8.Mentzelopoulos SD, Malachias S, Chamos C, Konstantopoulos D, Ntaidou T, Papastylianou A, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest: a randomized clinical trial. JAMA. 2013;310:270–279. doi: 10.1001/jama.2013.7832. [DOI] [PubMed] [Google Scholar]
- 9.Tsai M-S, Chuang P-Y, Huang C-H, Tang C-H, Yu P-H, Chang W-T, et al. Postarrest steroid use may improve outcomes of cardiac arrest survivors. Crit Care Med. 2019;47:167–175. doi: 10.1097/CCM.0000000000003468. [DOI] [PubMed] [Google Scholar]
- 10.Donnino MW, Andersen LW, Berg KM, Chase M, Sherwin R, Smithline H, et al. Corticosteroid therapy in refractory shock following cardiac arrest: a randomized, double-blind, placebo-controlled, trial. Crit Care. 2016;20:82. doi: 10.1186/s13054-016-1257-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Argaud L, Cour M, Dubien P-Y, Giraud F, Jossan C, Riche B, et al. Effect of cyclosporine in nonshockable out-of-hospital cardiac arrest: the CYRUS randomized clinical trial. JAMA Cardiol. 2016;1:557–565. doi: 10.1001/jamacardio.2016.1701. [DOI] [PubMed] [Google Scholar]
- 12.Bougouin W, Aissaoui N, Combes A, Deye N, Lamhaut L, Jost D, et al. Post-cardiac arrest shock treated with veno-arterial extracorporeal membrane oxygenation: an observational study and propensity-score analysis. Resuscitation. 2017;110:126–132. doi: 10.1016/j.resuscitation.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 13.de Pineton Chambrun M, Bréchot N, Lebreton G, Schmidt M, Hekimian G, Demondion P, et al. Venoarterial extracorporeal membrane oxygenation for refractory cardiogenic shock post-cardiac arrest. Intensive Care Med. 2016;42:1999–2007. doi: 10.1007/s00134-016-4541-y. [DOI] [PubMed] [Google Scholar]
- 14.Jakkula P, Pettilä V, Skrifvars MB, Hästbacka J, Loisa P, Tiainen M, et al. Targeting low-normal or high-normal mean arterial pressure after cardiac arrest and resuscitation: a randomised pilot trial. Intensive Care Med. 2018;44:2091–2101. doi: 10.1007/s00134-018-5446-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ameloot K, De Deyne C, Eertmans W, Ferdinande B, Dupont M, Palmers P-J, et al. Early goal-directed haemodynamic optimization of cerebral oxygenation in comatose survivors after cardiac arrest: the neuroprotect post-cardiac arrest trial. Eur Heart J. 2019;40:1804–1814. doi: 10.1093/eurheartj/ehz120. [DOI] [PubMed] [Google Scholar]
- 16.Ameloot K, Jakkula P, Hästbacka J, Reinikainen M, Pettilä V, Loisa P, et al. Optimum blood pressure in patients with shock after acute myocardial infarction and cardiac arrest. J Am Coll Cardiol. 2020;76:812–824. doi: 10.1016/j.jacc.2020.06.043. [DOI] [PubMed] [Google Scholar]
- 17.Sinha P, Spicer A, Delucchi KL, McAuley DF, Calfee CS, Churpek MM. Comparison of machine learning clustering algorithms for detecting heterogeneity of treatment effect in acute respiratory distress syndrome: a secondary analysis of three randomised controlled trials. EBioMedicine. 2021;74:103697. doi: 10.1016/j.ebiom.2021.103697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seymour CW, Kennedy JN, Wang S, Chang C-CH, Elliott CF, Xu Z, et al. Derivation, validation, and potential treatment implications of novel clinical phenotypes for sepsis. JAMA. 2019;321:2003–2017. doi: 10.1001/jama.2019.5791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nolan JP, Sandroni C, Böttiger BW, Cariou A, Cronberg T, Friberg H, et al. European resuscitation council and European society of intensive care medicine guidelines 2021: post-resuscitation care. Intensive Care Med. 2021;47:369–421. doi: 10.1007/s00134-021-06368-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–808. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bougouin W, Dumas F, Karam N, Maupain C, Marijon E, Lamhaut L, et al. Should we perform an immediate coronary angiogram in all patients after cardiac arrest? Insights from a large French registry. JACC Cardiovasc Interv. 2018;11:249–256. doi: 10.1016/j.jcin.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 22.Bougouin W, Dumas F, Lamhaut L, Marijon E, Carli P, Combes A, et al. Extracorporeal cardiopulmonary resuscitation in out-of-hospital cardiac arrest: a registry study. Eur Heart J. 2020;41:1961–1971. doi: 10.1093/eurheartj/ehz753. [DOI] [PubMed] [Google Scholar]
- 23.Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation. 2015;132:1286–1300. doi: 10.1161/CIR.0000000000000144. [DOI] [PubMed] [Google Scholar]
- 24.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 25.Dalton L, Ballarin V, Brun M. Clustering algorithms: on learning, validation, performance, and applications to genomics. Curr Genomics. 2009;10:430–445. doi: 10.2174/138920209789177601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Perez LV. Principal component analysis to address multicollinearity. Whitman College: Walla Walla, WA, USA; 2017.
- 27.Jolliffe I. Principal component analysis. In: Everitt BS, Howell DC, editors. Encyclopedia of statistics in behavioral science. Chichester: John Wiley & Sons Ltd.; 2005. p. bsa501. [Google Scholar]
- 28.Husson F, Josse J, et Pages J. Principal component methods—hierarchical clustering—partitional clustering: why would we need to choose for visualizing data. Applied Mathematics Department; 2010. vol. 17.
- 29.Sammouda R, El-Zaart A. An optimized approach for prostate image segmentation using K-means clustering algorithm with elbow method. Comput Intell Neurosci. 2021;2021:4553832. doi: 10.1155/2021/4553832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barth E, de Resende JTV, Mariguele KH, de Resende MDV, da Silva ALBR, Ru S. Multivariate analysis methods improve the selection of strawberry genotypes with low cold requirement. Sci Rep. 2022;12:11458. doi: 10.1038/s41598-022-15688-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509. doi: 10.1080/01621459.1999.10474144. [DOI] [Google Scholar]
- 32.Bascom KE, Dziodzio J, Vasaiwala S, Mooney M, Patel N, McPherson J, et al. Derivation and validation of the CREST model for very early prediction of circulatory etiology death in patients without ST-segment-elevation myocardial infarction after cardiac arrest. Circulation. 2018;137:273–282. doi: 10.1161/CIRCULATIONAHA.116.024332. [DOI] [PubMed] [Google Scholar]
- 33.Yan S, Gan Y, Jiang N, Wang R, Chen Y, Luo Z, et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. 2020;24:61. doi: 10.1186/s13054-020-2773-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nolan JP, Sandroni C, Böttiger BW, Cariou A, Cronberg T, Friberg H, et al. European resuscitation council and European society of intensive care medicine guidelines 2021: post-resuscitation care. Resuscitation. 2021;161:220–269. doi: 10.1016/j.resuscitation.2021.02.012. [DOI] [PubMed] [Google Scholar]
- 35.Negovsky VA. The second step in resuscitation–the treatment of the “post-resuscitation disease”. Resuscitation. 1972;1:1–7. doi: 10.1016/0300-9572(72)90058-5. [DOI] [PubMed] [Google Scholar]
- 36.Negovsky VA. Postresuscitation disease. Crit Care Med. 1988;16:942–946. doi: 10.1097/00003246-198810000-00004. [DOI] [PubMed] [Google Scholar]
- 37.Jozwiak M, Bougouin W, Geri G, Grimaldi D, Cariou A. Post-resuscitation shock: recent advances in pathophysiology and treatment. Ann Intensive Care. 2020;10:170. doi: 10.1186/s13613-020-00788-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Laurent I, Monchi M, Chiche JD, Joly LM, Spaulding C, Cariou A, et al. Reversible myocardial dysfunction in survivors of out-of-hospital cardiac arrest. J Am Coll Cardiol. 2002;40:2110–2116. doi: 10.1016/S0735-1097(02)02594-9. [DOI] [PubMed] [Google Scholar]
- 39.Kern KB, Hilwig RW, Rhee KH, Berg RA. Myocardial dysfunction after resuscitation from cardiac arrest: an example of global myocardial stunning. J Am Coll Cardiol. 1996;28:232–240. doi: 10.1016/0735-1097(96)00130-1. [DOI] [PubMed] [Google Scholar]
- 40.Kern KB, Hilwig RW, Berg RA, Rhee KH, Sanders AB, Otto CW, et al. Postresuscitation left ventricular systolic and diastolic dysfunction: treatment with dobutamine. Circulation. 1997;95:2610–2613. doi: 10.1161/01.CIR.95.12.2610. [DOI] [PubMed] [Google Scholar]
- 41.Adrie C, Adib-Conquy M, Laurent I, Monchi M, Vinsonneau C, Fitting C, et al. Successful cardiopulmonary resuscitation after cardiac arrest as a “sepsis-like” syndrome. Circulation. 2002;106:562–568. doi: 10.1161/01.CIR.0000023891.80661.AD. [DOI] [PubMed] [Google Scholar]
- 42.Hékimian G, Baugnon T, Thuong M, Monchi M, Dabbane H, Jaby D, et al. Cortisol levels and adrenal reserve after successful cardiac arrest resuscitation. Shock. 2004;22:116–119. doi: 10.1097/01.shk.0000132489.79498.c7. [DOI] [PubMed] [Google Scholar]
- 43.Gando S, Nanzaki S, Morimoto Y, Kobayashi S, Kemmotsu O. Out-of-hospital cardiac arrest increases soluble vascular endothelial adhesion molecules and neutrophil elastase associated with endothelial injury. Intensive Care Med. 2000;26:38–44. doi: 10.1007/s001340050009. [DOI] [PubMed] [Google Scholar]
- 44.Pene F, Hyvernat H, Mallet V, Cariou A, Carli P, Spaulding C, et al. Prognostic value of relative adrenal insufficiency after out-of-hospital cardiac arrest. Intensive Care Med. 2005;31:627–633. doi: 10.1007/s00134-005-2603-7. [DOI] [PubMed] [Google Scholar]
- 45.Voicu S, Baud FJ, Malissin I, Deye N, Bihry N, Vivien B, et al. Can mortality due to circulatory failure in comatose out-of-hospital cardiac arrest patients be predicted on admission? A study in a retrospective derivation cohort validated in a prospective cohort. J Crit Care. 2016;32:56–62. doi: 10.1016/j.jcrc.2015.11.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Fig. S1. Times of deaths due to the five reasons, in days since admission to the intensive care unit.
Additional file 2: Fig. S2. Hierarchical clustering.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.