Abstract
Background
Lipoleiomyomas are uncommon uterine lesions containing adipose and smooth muscle tissue. They have a variable presentation and are usually found incidentally on imaging or post-hysterectomy tissue analysis. Given their low prevalence, there is a dearth of literature describing imaging characteristics for uterine lipoleiomyomas. In this image-rich case series, we summarize an example of an initial presentation as well as present ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) findings for 36 patients.
Case presentation
We present the detailed clinical course of a representative patient evaluated for uterine lipoleiomyoma and describe imaging findings seen in another 35 patients. This includes ultrasound findings from 16 patients, CT findings from 25 patients, and MRI findings from 5 patients. Among the 36 total patients, symptoms at the time of diagnosis were variable but often included abdominal or pelvic pain; however, most patients were asymptomatic, and the lipoleiomyomas were incidentally discovered on imaging.
Conclusions
Uterine lipoleiomyomas are rare and benign tumors with variable presentations. Ultrasound, CT, and MRI findings can assist in diagnosis. Findings on ultrasound typically include well-circumscribed hyperechoic and septated lesions with minimal to no internal blood flow. CT shows fat-containing either homogeneous or heterogeneous circumscribed lesions depending on their ratio of fat and smooth muscle tissue. Lastly, on MRI, uterine lipoleiomyomas commonly appear heterogenous with loss of signal on fat-suppressed sequences. These imaging findings are highly specific for lipoleiomyomas, and familiarity with these findings may reduce unnecessary and potentially invasive procedures.
Keywords: Uterine lipoleiomyoma, Pelvic neoplasms, Diagnostic imaging, Ultrasound, Computed tomography, Magnetic resonance imaging, Case series
Abbreviations
- Computed tomography
CT
- Magnetic resonance imaging
MRI
- Ultrasound
US
1. Background
Lipoleiomyomas are rare, benign uterine masses. Although they are often asymptomatic, patients can present with symptoms including abdominal or pelvic discomfort, palpable masses, and menstrual irregularities [[1], [2], [3]]. Uterine lipoleiomyomas are thought to arise from metaplastic degeneration of uterine smooth muscle into adipose tissue, and as a result, can be seen on imaging as a heterogeneous fatty mass on computed tomography (CT) or a lesion with heterogeneous T1 and T2 signal on magnetic resonance imaging (MRI) [4]. Specific treatment is not necessarily recommended, but if hysterectomy is performed, subsequent histopathology will typically show a mixture of adipose and smooth muscle tissue [[1], [2], [3]].
In this image-rich case series, we present 36 patients who were evaluated for uterine lipoleiomyomas and describe associated imaging findings. To our knowledge, there are no other published works that extensively detail the radiologic findings of uterine lipoleiomyoma in this number of patients.
2. Methods
After receiving approval from the University of California, Irvine Institutional Review Board, our single institution radiology database was retrospectively reviewed for reports suggestive of lipoleiomyoma. Reports dictated from January 1, 2010 through January 1, 2023 were included. Radiologic images were then reviewed by either an attending or resident radiologist to confirm the presence of lipoleiomyoma. To qualify for inclusion in this case series, patients were required to be at least 18 years of age and have had imaging in at least one modality (ultrasound, CT, or MRI).
3. Case presentation
A 67-year-old post-menopausal Hispanic woman with history of fibroids presented with lower abdominal discomfort and associated constipation. She reported no vaginal bleeding or acute pain. Her past medical history included five pregnancies, three uncomplicated spontaneous vaginal deliveries, and two spontaneous abortions. Laboratory tests were unremarkable. A transvaginal ultrasound (US) revealed a hyperechoic intramural mass. Pelvic CT revealed a well-defined homogenous fat-density mass within the uterine wall compatible with a uterine lipoleiomyoma. The patient's symptoms were thought not to be related to the presence of the lipoleiomyoma. The patient was offered hysterectomy but declined.
4. Results
Twenty-one patients met criteria for inclusion in this case series. Many (47.2%) were asymptomatic at the time of presentation. When symptoms were present, they most often included pelvic/abdominal pain (44.4%) or flank pain (13.9%). Patients usually had no significant past medical history (52.8%). In those with past medical history, fibroids were the most common prior diagnosis (11.1%). Demographic characteristics are summarized in Table 1.
Table 1.
Patient summary.
| Total number of patients | 36 |
|---|---|
| Average age at presentation | 61.9 ± 13.1 years |
| Percent asymptomatic | 47.2% |
| Percent postmenopausal | 72.2% |
4.1. Imaging findings
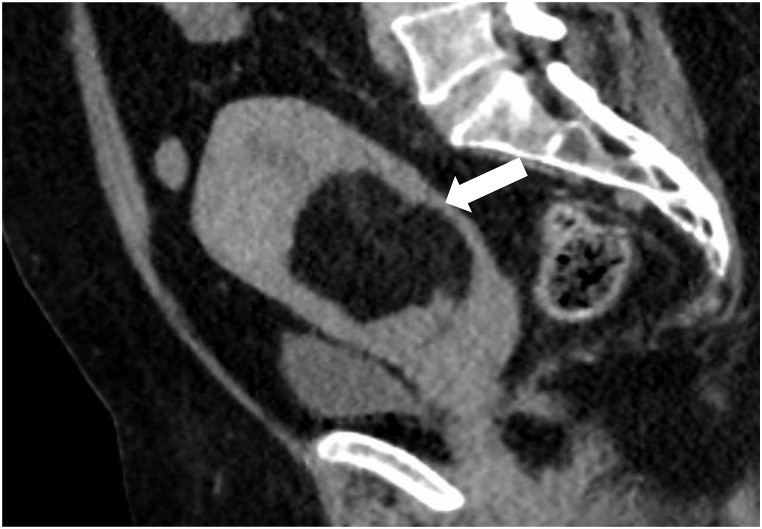
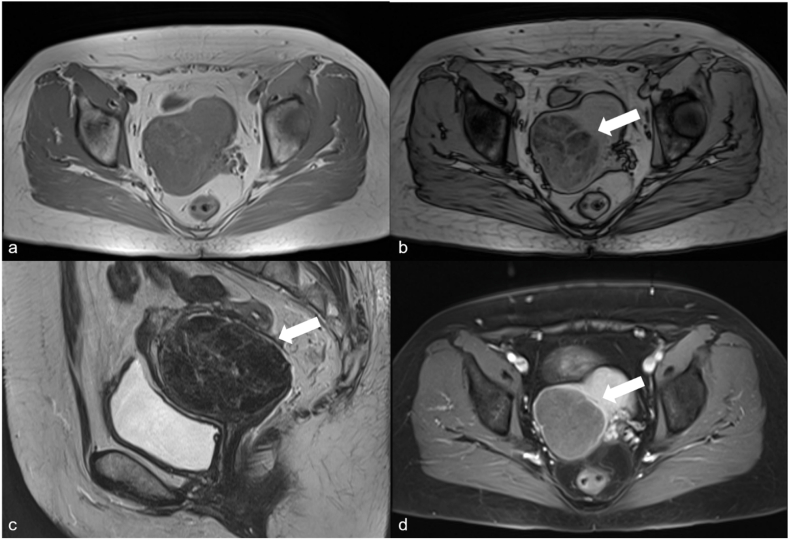
Imaging data was available for all 36 patients. This included 16 patients who underwent ultrasound, 25 patients who underwent CT scan, and 5 patients who received an MRI. The most common findings on ultrasound (Fig. 1 a-c) were hyperechogenicity (100%) and circumscribed (93.8%) and septated (75%) lesions. 43.8% lesions demonstrated internal flow. CT imaging (Fig. 1, Fig. 2) most frequently demonstrated fat density (100%), with circumscribed (88%) lesions with septations (64%). On MRI (Fig. 3 a-d), uterine lipoleiomyomas demonstrated hypointensities on fat-suppressed sequences (100%) and generally appeared heterogeneous (80%). Summary of imaging findings is characterized in Table 2.
Fig. 1.
Patient 1 (a,b) Sagittal grayscale image (a) of the uterus (orange arrow) shows a well circumscribed echogenic lesion (white arrow) in the posterior uterine body, without internal color blood flow (b). Patient 2 (c,d) sagittal grayscale image of the midline pelvis (c) shows a large echogenic lesion in the expected location of the uterus (white arrowheads). Sagittal CT of the pelvis (d) for the same patient demonstrates a large fat containing lesion replacing the majority of the uterus (white arrowheads). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Fig. 2.
Sagittal abdominopelvic CT with contrast showing a well-defined, homogenous, fat-density lesion (arrow) within the uterus.
Fig. 3.
Axial T1 in-phase (a) and out-of-phase (b) pelvic MRI shows a large right uterine body lipoleiomyoma with signal loss on out-of-phase imaging (arrow). Sagittal T2 imaging (c) demonstrates decreased T2 signal in the lipoleiomyoma. Axial post-contrast imaging (d) shows minimal contrast enhancement.
Table 2.
Summary of imaging features.
| Modality | Feature | Prevalence |
|---|---|---|
| US | Hyperechogenicity | 100% (16/16) |
| US | Circumscribed | 93.8% (15/16) |
| MRI | Signal loss on fat suppression sequence | 100% (5/5) |
| MRI | T1 and T2 Heterogeneity | 80% (4/5) |
| CT | Fat density | 100% (25/25) |
| CT | Circumscribed | 88% (22/25) |
*US = Ultrasound, CT = Computed Tomography, MRI = Magnetic Resonance Imaging.
4.2. Pathology findings
Pathology results were available for three patients. In each case, gross pathologic examination showed well circumscribed masses with firm, tan-white, and whorled cut surface in myometrium. Histological analysis showed a mixture of adipose and smooth muscle tissue (Fig. 4).
Fig. 4.
Hematoxylin and eosin stain at 100-times magnification shows a mixture of mature adipose tissue and proliferating smooth muscle and fibrosis. There is no cytologic atypia, increased mitotic activity, or necrosis.
5. Discussion
Uterine lipoleiomyoma is a rare and benign tumor composed of smooth muscle and adipose tissue. While it is often reported to have an incidence of 0.03%–0.2%, the true incidence in the general population has not been well studied [ [4,5]]. One analysis found that lipoleiomyomas made up 0.28% of leiomyomas and were present in 0.39% of patients undergoing hysterectomies [6]. Elsewhere, it was reported that 0.20% of leiomyomas were lipoleiomyomas [7]. Overwhelmingly, most common fat containing lesions of the uterus are lipoleiomyomas. Other diagnoses are extremely rare and include mixed lipomas such as angiomyolipomas or fibrolipomas [4]. Biopsies or resections are no longer performed on these lesions as the imaging features are pathognomonic.
The relative amount of adipose and smooth muscle tissue within each lipoleiomyoma lesion is variable, which may be due to their proposed origin as a fatty transformation of smooth muscle [ [7,8]]. As the lesion progresses, smooth muscle makes up a relatively smaller proportion of the lesion as it transforms to adipose tissue. Other proposed mechanisms for pathogenesis include origin from misplaced stem cells, lipoblasts infiltrating from nearby tissue, and displacement of adipose tissue during surgery [ [7,8]].
Like leiomyomas, from which they are proposed to originate, lipoleiomyomas have a wide range of clinical presentations. In fact, it is not possible to differentiate them based on symptoms alone. Within our cohort, most lipoleiomyomas were found incidentally during workup for pelvic or flank pain in patients who had diverse medical histories ranging from cancer to fibroids to renal stones. Lipoleiomyomas were most commonly discovered in relatively older, postmenopausal women and are likely not related to patient symptoms. Of note, there is no definitive evidence to support growth of lipoleiomyomas after menopause [12].
Diagnosis of lipoleiomyoma is aided by imaging in the form of ultrasound, CT, and MRI. Ultrasound findings in our cohort typically revealed a circumscribed, echogenic lesion that contained septations and showed minimal to no internal blood flow. Of the 16 patients with CT findings, lesions could be described as a circumscribed mass with fat or soft tissue-density and containing internal septations. They were typically located intramurally. Of the 5 patients with MRI findings, lesions appeared heterogeneous with hypointensities on fat-suppressed sequences. This characteristic can be attributed to the variable amounts of adipose and smooth muscle tissue that compose lipoleiomyomas. Signal loss was present on opposed phase T1-weighted imaging as well as T1-and T2-fat saturated imaging. This correlates with the adiposity of these lesions. The most prevalent imaging features included echogenic lesions on ultrasound, loss of T1 signal on T1 fat suppressed imaging, and intralesional fat density on CT imaging.
While biopsy could be used to differentiate a uterine lipoleiomyoma from malignant lesions of the uterus, they can usually be differentiated on imaging alone. Uterine lesions with a lipomatous component are nearly always benign [ [5,7,9,10]]. When imaging features are suggestive of lipoleiomyoma and there are no signs concerning for malignant disease, patients may be managed similarly to those with uterine leiomyoma. Surgery can be beneficial if lipoleiomyomas start to demonstrate mass effect but is typically not needed [ [11,12]].
6. Conclusion
Uterine lipoleiomyomas are rare anomalous degenerations of uterine smooth muscle into fatty tissue. These lesions have a variable presentation related to their histologic evolution over time but are often incidentally identified by imaging studies. Ultrasound typically reveals well-circumscribed hyperechoic and septated lesions with minimal to no internal blood flow. CT shows fat-containing either homogeneous or heterogeneous circumscribed lesions depending on their ratio of fat and smooth muscle tissue. Uterine lipoleiomyomas appear heterogenous with demonstrated hypointensities on fat-suppressed sequences on MRI. These key imaging findings on ultrasound, CT, or MRI, when present, are highly specific for uterine lipoleiomyomas. Any of the three study types can be used to appropriately diagnose uterine lipoleiomyomas, preventing unwarranted additional work up such as potentially invasive procedures.
Patient Consent: Written informed consent was obtained for publication. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Author contribution statement
All authors listed have significantly contributed to the investigation, development and writing of this article.
Data availability statement
The data that has been used is confidential.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Tyagi N., Tyagi R., Griffin Y. Uterine lipoleiomyoma. Case Rep. 2014;2014 doi: 10.1136/bcr-2014-207763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Avritscher R., Iyer R.B., Ro J., Whitman G. Lipoleiomyoma of the uterus. Am. J. Roentgenol. 2001;177(4):856. doi: 10.2214/ajr.177.4.1770856. [DOI] [PubMed] [Google Scholar]
- 3.Tsushima Y., Kita T., Yamamoto K. Uterine lipoleiomyoma: MRI, CT and ultrasonographic findings. Br. J. Radiol. 1997;70(838):1068–1070. doi: 10.1259/bjr.70.838.9404215. [DOI] [PubMed] [Google Scholar]
- 4.Chu C.Y., Tang Y.K., Chan T.S., Wan Y.H., Fung K.H. Diagnostic challenge of lipomatous uterine tumors in three patients. World J. Radiol. 2012;4(2):58. doi: 10.4329/wjr.v4.i2.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kitajima K., Kaji Y., Imanaka K., Sugihara R., Sugimura K. MRI findings of uterine lipoleiomyoma correlated with pathologic findings. Am. J. Roentgenol. 2007;189(2):W100–W104. doi: 10.2214/AJR.07.2230. [DOI] [PubMed] [Google Scholar]
- 6.Lin K.C., Sheu B.C., Huang S.C. Lipoleiomyoma of the uterus. Int. J. Gynecol. Obstet. 1999;67(1):47–49. doi: 10.1016/s0020-7292(99)00094-6. [DOI] [PubMed] [Google Scholar]
- 7.Willén R., Gad A., Willén H. Lipomatous lesions of the uterus. Virchows Arch. 1978;377(4):351–361. doi: 10.1007/BF00507135. [DOI] [PubMed] [Google Scholar]
- 8.Havel G., Wedell B., Dahlenfors R., Mark J. Cytogenetic relationship between uterine lipoleiomyomas and typical leiomyomas. Virchows Arch. B. 1989;57(1):77. doi: 10.1007/BF02899067. [DOI] [PubMed] [Google Scholar]
- 9.Dodd G.D., 3rd, Budzik R.F., Jr. Lipomatous uterine tumors: diagnosis by ultrasound, CT, and MR. J. Comput. Assist. Tomogr. 1990;14(4):629–632. [PubMed] [Google Scholar]
- 10.Sośnik H., Sośnik K. Investigations on uterine fatty lesions. Pol. J. Pathol. 2013;64(2):136–143. doi: 10.5114/pjp.2013.36017. [DOI] [PubMed] [Google Scholar]
- 11.Loffroy R., Nezzal N., Mejean N., Sagot P., Krausé D. Lipoleiomyoma of the uterus: imaging features. Gynecol. Obstet. Invest. 2008;66(2):73–75. doi: 10.1159/000127409. [DOI] [PubMed] [Google Scholar]
- 12.Oh S.R., Cho Y.J., Han M., Bae J.W., Park J.W., Rha S.H. Uterine lipoleiomyoma in peri or postmenopausal women. J. Menopausal Med. 2015;21(3):165. doi: 10.6118/jmm.2015.21.3.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that has been used is confidential.