Video
EUS-guided Roux-en-Y gastric bypass reversal procedure to treat a refractory marginal ulcer following Roux-en-Y gastric bypass.
Introduction
Marginal ulcers are a common adverse event of Roux-en-Y gastric bypass (RYGB), with an incidence of up to 16%.1, 2, 3, 4 Although the exact pathophysiology underlying the development of marginal ulcers is unclear, possible risk factors include smoking, diabetes, nonsteroidal anti-inflammatory drugs, aspirin use, alcohol, and gastro-gastric fistulas, among others.5, 6, 7, 8, 9 Management of marginal ulcers is typically conservative, with smoking cessation and pharmacologic therapy (proton-pump inhibitors [PPIs] and sucralfate), and carries a high healing rate.10 An endoscopy may be performed to remove staples/suture material, and interventions aimed to cover the ulcer bed using sutures and metallic stents to avoid gastric acid exposure have been reported.11 In this video (Video 1, available online at www.videogie.org), we present the case of a persistent marginal ulcer post-RYGB managed with EUS-guided RYGB reversal.
Case Presentation
A 58-year-old woman who was a heavy smoker presented with a refractory marginal ulcer following RYGB. In 2014, the patient underwent RYGB for obesity, with a nadir weight of 51 kg and a nadir body mass index (BMI) of 17 kg/m2. In 2018, she had a marginal ulcer-related perforation, requiring emergent revision. Later, she underwent hiatal hernia repair as well as endoscopic drainage of an inflammatory postoperative abdominal fluid collection. The marginal ulcer was refractory, despite full-dose PPI and sucralfate, as well as smoking cessation. The patient had decreased appetite and intermittent abdominal pain, which made it difficult for her to maintain a healthy weight. Her weight prior to the procedure was 62 kg, with a BMI of 20 kg/m2. Helicobacter pylori was negative on biopsy. Treatment options were discussed with the multidisciplinary team and the patient. Because she had several previous abdominal interventions, we opted to proceed with the EUS-guided RYGB reversal (2022).
During the procedure, the gastrojejunal anastomosis (GJA) was severely stenotic (Fig. 1) because of a large, deep marginal ulcer on the jejunal limb (Fig. 2). After identifying an appropriate window and excluding intervening vessels, the remnant stomach was accessed with a 19-gauge needle and filled with a mixture of saline and contrast (Fig. 3). Fluoroscopy confirmed the filling of the gastric remnant with contrast (Fig. 4). The remnant stomach was then accessed after placement of a 20-mm lumen-apposing metal stent (LAMS) (AXIOS; Boston Scientific, Mass, USA) to create a gastro-gastric anastomosis (Fig. 5). The LAMS was then sutured in place using 2 interrupted sutures administered by the Apollo Overstitch device (Apollo Endosurgery, Austin, Tex, USA).
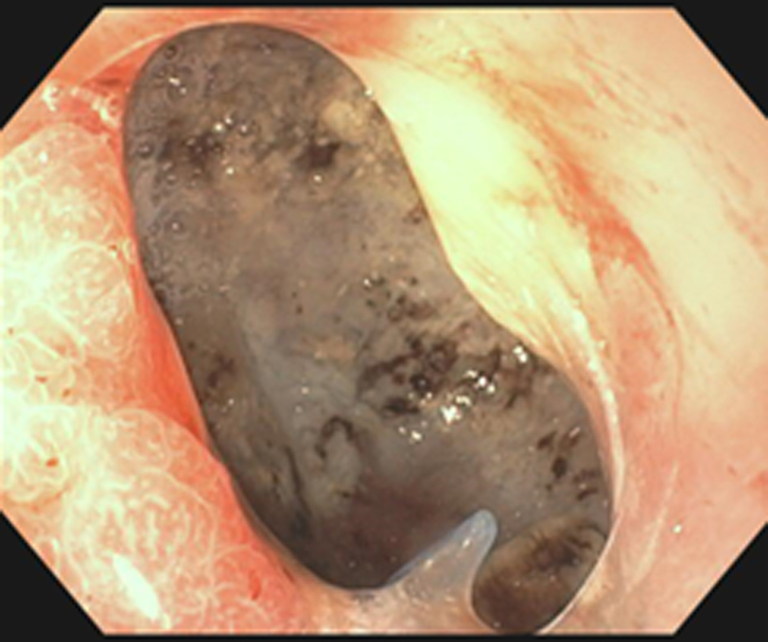
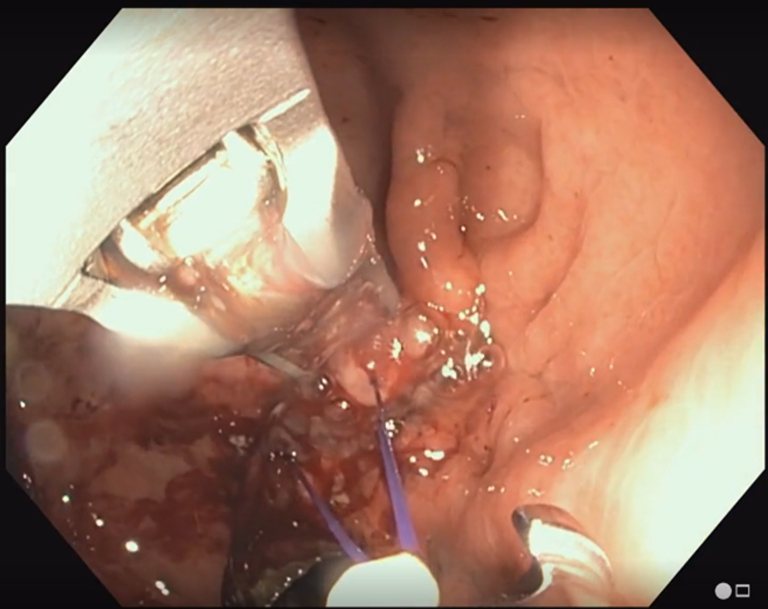
Figure 1.
EGD view from the gastric pouch showing a narrowing of the gastrojejunal anastomosis caused by extensive fibrosis and a deep marginal ulcer on the jejunal limb.
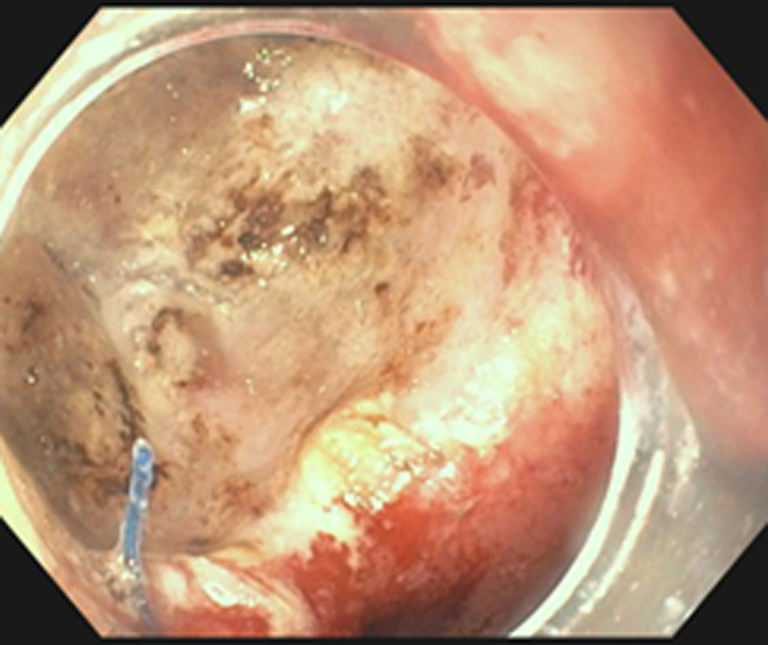
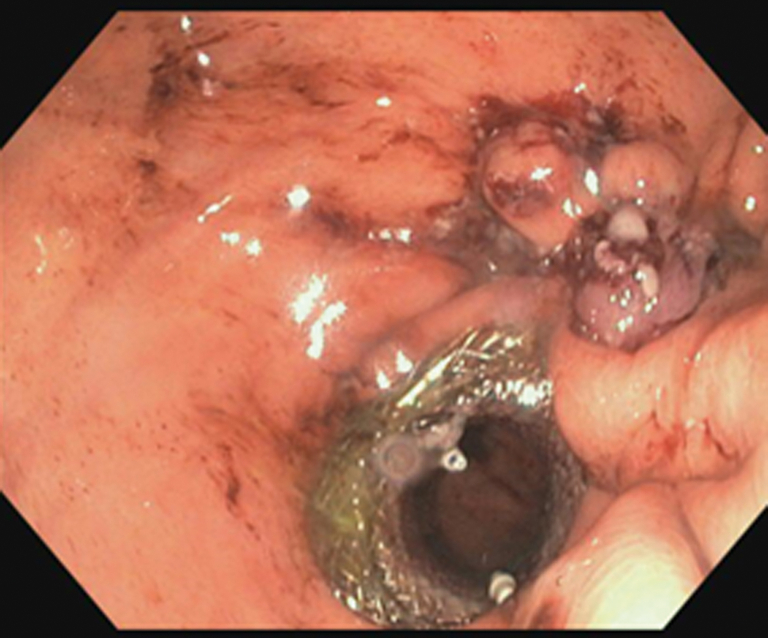
Figure 2.
EGD view from the gastric pouch showing a large marginal ulcer extending to the jejunal limb.
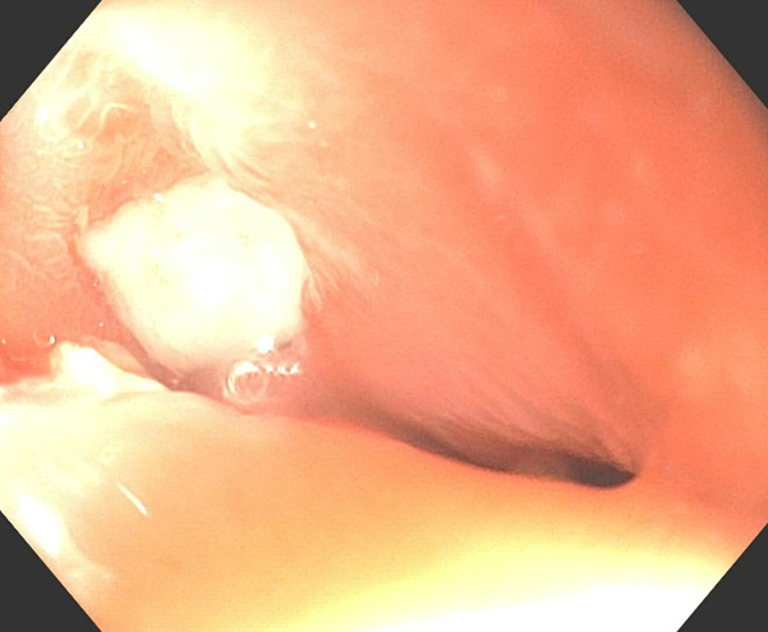
Figure 3.
EUS showing the injection of the gastric remnant with a mixture of contrast and saline.
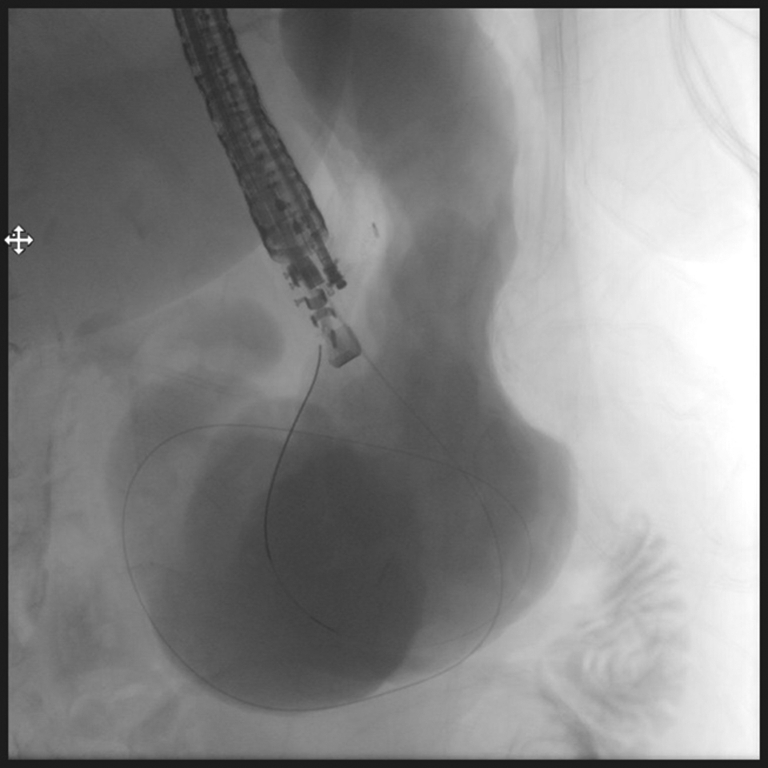
Figure 4.
Fluoroscopic image showing the gastric pouch and remnant stomach filled with contrast after a guidewire was inserted in the gastric remnant. Contrast can also be seen in the duodenum.
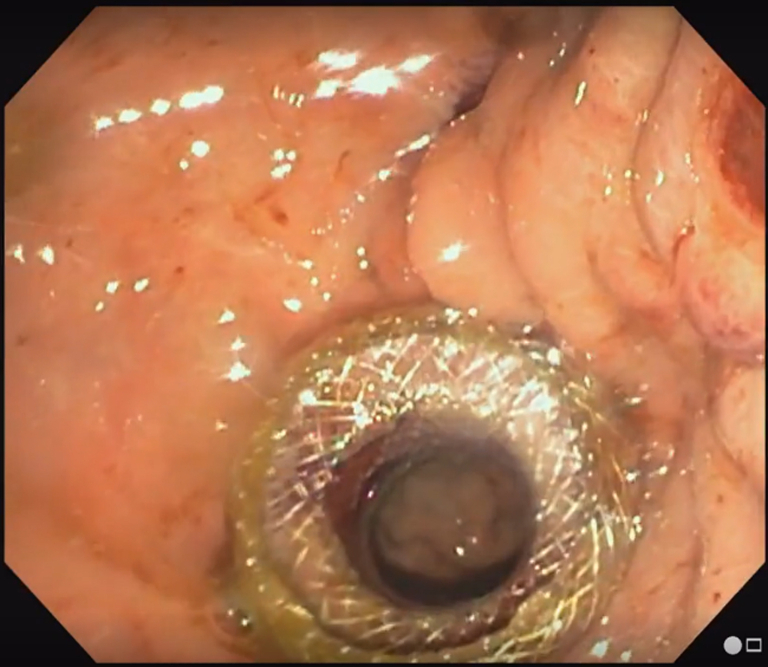
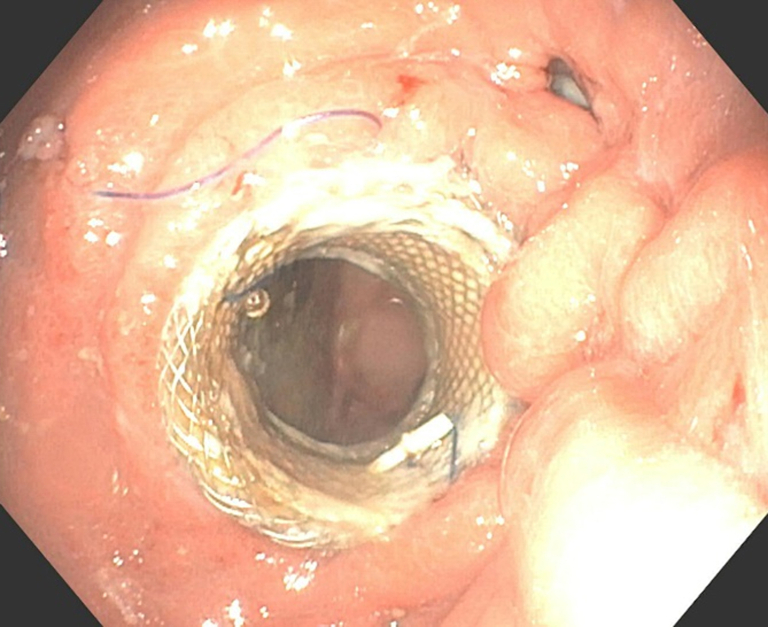
Figure 5.
EGD view from the gastric pouch showing the lumen-apposing metal stent in place forming the gastro-gastric anastomosis.
With the aid of the tissue helix, we closed the GJA using the endoscopic suturing device to completely divert food from the ulcerated site (Figs. 6 and 7). In the end, we could easily access the excluded stomach through the LAMS and the scope was easily advanced to a normal duodenum.
Figure 6.
EGD view from the gastric pouch showing the gastrojejunal anastomosis suturing using the Apollo Overstitch.
Figure 7.
EGD view from the gastric pouch showing complete closure of gastrojejunal anastomosis and the gastro-gastric stent in place.
Following the procedure, the patient continued the same medical therapy. A follow-up EGD 4 months later revealed significant healing of the marginal ulcer (Fig. 8). The GJA was still almost entirely closed, and the LAMS was kept in place (Fig. 9). The patient was asymptomatic; she was able to gain 9 kg and her BMI had increased to 23 kg/m2.
Figure 8.
EGD view inside the jejunal limb showing significant healing of the marginal ulcer 4 months after the EUS-guided Roux-en-Y gastric bypass reversal procedure.
Figure 9.
EGD view from the gastric pouch showing the gastro-gastric stent in place and the gastrojejunal anastomosis almost entirely closed 4 months after the EUS-guided Roux-en-Y gastric bypass reversal procedure.
Discussion
In the case discussed, we used the EUS-guided RYGB reversal procedure in treating a severe case of refractory marginal ulcer along with overstitch and complete closure of the GJA overlying the ulcer. On follow-up EGD, there was almost complete recovery of the marginal ulcer. The exact mechanism by which the EUS-guided RYGB reversal procedure promoted ulcer healing is unclear. Our rationale was focused on diverting ingested material away from the ulcer and restoring physiological anatomy by closing the GJA and creating a gastro-gastric bypass. This highlights the importance of preventing ulcer exposure to gastric acid as well as prophylactic acid suppression in preventing ulcer formation.11 However, more research is needed to determine the precise underlying mechanisms.
The promising outcome seen in this case opens the door for further research on extended indications of the EUS-guided RYGB reversal in the management of RYGB adverse events. It also provides a foundation for a better understanding of the pathophysiology of marginal ulcers.
Disclosure
Dr Abu Dayyeh is a consultant for Metamodix, BFKW, DyaMx, Boston Scientific, USGI Medical, and Endo-TAGSS, and he does research support for Boston Scientific, USGI Medical, Apollo Endosurgery, Spatz Medical, GI Dynamics, Cairn Diagnostics, Aspire Bariatrics, and Medtronic. He is also a speaker for Johnson and Johnson, Endogastric Solutions, and Olympus. All other authors disclosed no financial relationships.
Ethical Approval
Ethical approval has been waived by the Mayo Institution Board Review.
Footnotes
Anthony Kerbage and Karim Al Annan contributed equally to this work.
Supplementary data
EUS-guided Roux-en-Y gastric bypass reversal procedure to treat a refractory marginal ulcer following Roux-en-Y gastric bypass.
References
- 1.Boutari C., Mantzoros C.S.A. 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism. 2022;133 doi: 10.1016/j.metabol.2022.155217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Csendes A., Burgos A.N., Altuve J., et al. Incidence of marginal ulcer 1 month and 1 to 2 years after gastric bypass: a prospective consecutive endoscopic evaluation of 442 patients with morbid obesity. Obes Surg. 2009;19:135–138. doi: 10.1007/s11695-008-9588-6. [DOI] [PubMed] [Google Scholar]
- 3.Di Palma A., Liu B., Maeda A., et al. Marginal ulceration following Roux-en-Y gastric bypass: risk factors for ulcer development, recurrence and need for revisional surgery. Surg Endosc. 2021;35:2347–2353. doi: 10.1007/s00464-020-07650-0. [DOI] [PubMed] [Google Scholar]
- 4.Süsstrunk J., Wartmann L., Mattielo D., et al. Incidence and prognostic factors for the development of symptomatic and asymptomatic marginal ulcers after Roux-en-Y gastric bypass procedures. Obes Surg. 2021;31:3005–3014. doi: 10.1007/s11695-021-05363-4. [DOI] [PubMed] [Google Scholar]
- 5.Hedberg J., Hedenström H., Nilsson S., et al. Role of gastric acid in stomal ulcer after gastric bypass. Obes Surg. 2005;15:1375–1378. doi: 10.1381/096089205774859380. [DOI] [PubMed] [Google Scholar]
- 6.Rasmussen J.J., Fuller W., Ali M.R. Marginal ulceration after laparoscopic gastric bypass: an analysis of predisposing factors in 260 patients. Surg Endosc. 2007;21:1090–1094. doi: 10.1007/s00464-007-9285-x. [DOI] [PubMed] [Google Scholar]
- 7.Azagury D.E., Abu Dayyeh B.K., Greenwalt I.T., et al. Marginal ulceration after Roux-en-Y gastric bypass surgery: characteristics, risk factors, treatment, and outcomes. Endoscopy. 2011;43:950–954. doi: 10.1055/s-0030-1256951. [DOI] [PubMed] [Google Scholar]
- 8.Keith J.N. Endoscopic management of common bariatric surgical complications. Gastrointest Endosc Clin N Am. 2011;21:275–285. doi: 10.1016/j.giec.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 9.Portela R.C., Sharma I., Vahibe A., et al. Aspirin use as a risk factor for marginal ulceration in Roux-en-Y gastric bypass patients: a meta-analysis of 24,770 patients. Am Surg. Epub 2022 May 18 doi: 10.1177/00031348221103647. [DOI] [PubMed] [Google Scholar]
- 10.Schulman A.R., Chan W.W., Devery A., et al. Opened proton pump inhibitor capsules reduce time to healing compared with intact capsules for marginal ulceration following Roux-en-Y gastric bypass. Clin Gastroenterol Hepatol. 2017;15:494–500.e1. doi: 10.1016/j.cgh.2016.10.015. [DOI] [PubMed] [Google Scholar]
- 11.Barola S., Fayad L., Hill C., et al. Endoscopic management of recalcitrant marginal ulcers by covering the ulcer bed. Obes Surg. 2018;28:2252–2260. doi: 10.1007/s11695-018-3162-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
EUS-guided Roux-en-Y gastric bypass reversal procedure to treat a refractory marginal ulcer following Roux-en-Y gastric bypass.
EUS-guided Roux-en-Y gastric bypass reversal procedure to treat a refractory marginal ulcer following Roux-en-Y gastric bypass.