Abstract
Introduction
Psoriasis is a common skin disorder associated with physical and psychological burdens. Visible disfiguration can trigger a negative reaction which can cause much of the readily measurable psychological burden of the disease. Although many biological treatments provide some success in the initial clearance of lesions, there is a dispute about the long-term maintenance of the disease, as no current biological treatment has been shown to be curative. Topical therapies are still the most widely used agents as first-line and maintenance treatment for psoriasis. The present study aimed to investigate the safety, tolerability, and, to some extent, efficacy of GN-037 cream in patients with psoriasis and healthy volunteers.
Methods
A randomized, double-blind, single-center, placebo-controlled phase 1 clinical study was conducted to evaluate the safety, tolerability, and clinical efficacy of GN-037 cream topically applied twice daily for 2 weeks in healthy subjects (n = 12) and patients (n = 6) diagnosed with plaque-type psoriasis. Six healthy subjects received placebo. Patients with plaque psoriasis were evaluated by a dermatologist, and Physician Global Assessment (PGA) score was required to be ≥ 3 (moderate psoriasis) at screening.
Results
A total of 31 adverse events (AEs) occurred in 13 participants during the study: 9 AEs in healthy subjects receiving GN-037 cream, 3 AEs in healthy subjects receiving placebo, and 1 AE in one psoriatic patient. The most frequently reported AEs were reactions at the application site, including erythema, exfoliation, pruritus, and burning sensation. During the baseline evaluation, one patient had a PGA score of 3 (moderate) and five patients had a PGA score of 4 (severe). On day 14, in treatment, four patients experienced second grade and two patients third grade improvements compared with baseline, indicating a shift of patients from moderate and severe disease to mild disease and to almost clear (score 2 or 1). There were slight increases in plasma tumor necrosis factor (TNF)-α, interleukin-17 (IL-17) and interleukin-23 (IL-23) levels in both healthy volunteers and patients throughout the study, as compared with baseline.
Conclusion
The results of this phase 1 trial conducted in 18 healthy volunteers and 6 patients with plaque psoriasis demonstrated a favorable safety and tolerability profile for GN-037; therefore, further clinical development of GN-037 in a phase 2 clinical trial has been initiated in patients with mild to moderate plaque psoriasis (NCT05706870).
Trial Registration Number
Keywords: GN-037, Phase 1, Plaque psoriasis, Topical treatment
Key Summary Points
| Psoriasis is a common skin disorder associated with physical and psychological burdens. |
| Long‐term management of plaque psoriasis with topical agents is reported to be suboptimal; therefore, frequent relapses are inevitable. |
| Novel topical combination treatment options may provide better outcomes in reducing the occurrence of relapses in patients with plaque psoriasis and eventually improving the quality of life in these patients. |
| GN-037 was developed as a new combination product with four active ingredients aiming at different activities such as suppression of inflammation, desquamation of lesions, moistening, and inhibition of decolorization of skin. |
| GN-037 cream with a novel formulation was safe in healthy volunteers and patients with plaque psoriasis. |
| A clinically meaningful efficacy was observed in six patients. Therefore, it may represent a well-tolerated topical treatment option for patients with plaque psoriasis. |
Introduction
Psoriasis is a common skin disorder associated with physical and psychological burdens, and as with similar dermatoses, visible disfiguration can trigger a negative reaction in close encounters, which can cause much of the readily measurable psychological burden of the disease. In Europe and North America, psoriasis prevalence is 2–4%, respectively, and prevalence increases in a linear curve during life, with an almost tenfold increase at 18 years of age as compared with newborns [1, 2]. A great majority of patients (70–80%) generally present with mild psoriasis, which may benefit from topical therapy [3]. Climate exposure to the sun and ethnicity are thought to affect psoriasis prevalence; however, a relatively recent study showed a weak correlation between latitude and the prevalence of psoriasis, suggesting that other factors or combinations of factors may play a role [4–7].
Topical treatments are generally selected during the patient’s treatment, and a succession of increasingly potent topical steroids, followed by the introduction of topical hydrocortisone by Sulzberger and Witten in 1952 [8]. However, the relatively recent introduction of monoclonal antibodies for treating various disease algorithms caused major treatment advancements in dermatology, especially for treating psoriasis [9, 10]. Although many biological treatments provide some success in the initial clearance of lesions, there is a dispute on the long-term maintenance of the disease, since no current biological treatment has been shown to be curative [11, 12]. Therefore, topical therapies, including topical corticosteroids, are still the most widely used agents for first-line and maintenance treatment of psoriasis and can be used as monotherapy or in combination with other agents [13, 14].
GN-037 was developed as a new combination product with four active ingredients aiming at different activities such as suppression of inflammation, desquamation of lesions, moistening, and inhibition of decolorization of skin. After completion of preclinical proof-of-concept animal studies, this new formulation with lower concentrations of active ingredients compared with marketed products was subject to clinical testing.
The aim of this phase 1 study was to investigate the safety, tolerability, and, to a certain extent, efficacy of GN-037 topical cream in psoriasis patients and healthy volunteers in two stages.
Methods
Study Design
A randomized, double-blind, single-center, placebo-controlled phase 1 clinical study was conducted to evaluate the safety, tolerability, and clinical efficacy of topically applied GN-037 cream in healthy subjects and in patients diagnosed with plaque-type psoriasis. The clinical phase of the trial was initiated in February 2022 and completed in April 2022 in Erciyes University Hakan Çetinsaya Good Clinical Practice and Research Centre (IKUM). The trial was carried out according to the ethical standards of the Declaration of Helsinki and the International Conference on Harmonisation of Good Clinical Practice Guidelines and its revisions. The study protocol was approved by the Ethics Committee for Clinical Trials of Erciyes University, Kayseri, Turkey, and the Republic of Turkey.
The trial was planned with three periods: up to 1 month of screening, 14 days of treatment, and 14 days of post-treatment follow-up. Study visits were made at screening, baseline (day 1), days 6 and 14 during the treatment period, and days 19 (follow-up visit to the clinic) and 28 (telephone visit) and were carried out as two stages with healthy volunteers and patients with psoriasis.
During the first stage of the study, 18 healthy subjects were randomly assigned to receive either GN-037 cream or vehicle (placebo) cream, applied twice daily to selected areas of the body for 14 days. The study treatments were applied topically over 5 cm2 selected target area (low-dose group), or 15 cm2 selected target area (medium-dose group) or 30 cm2 selected target area (high-dose group). Six subjects were randomized in 2:1 ratio to study groups at each planned dose level. During the day 14 visit, the study investigator performed a safety assessment. After confirmation of an acceptable safety assessment in the low-dose group, the dose was subsequently increased for medium- and high-dose applications. After completion of the first stage with healthy volunteers, the second stage was started and six patients with plaque psoriasis were enrolled. One target lesion was determined by the dermatologist, and all psoriasis patients were treated with GN-037 cream twice daily for 14 days.
Eligibility Criteria
Healthy volunteers and patients with plaque psoriasis of both sexes, aged 18–65 years, were enrolled. Patients with plaque psoriasis were evaluated by a dermatologist, and Physician Global Assessment (PGA) score was required to be ≥ 3 (moderate psoriasis) at screening. The diseased area should cover less than 5% of the total body surface area (BSA). The main exclusion criteria for patients with psoriasis were the non-plaque form of psoriasis and skin conditions that would interfere with the evaluation of psoriasis. A history of acute or chronic infection that requires treatment with systemic antibiotics, antivirals, antiparasitic, antiprotozoal, or antifungal therapies within 4 weeks prior to baseline, the need for the use of other medications such as topical or systemic antibiotics or antihistamines that can affect the course of the disease, a history of psoriasis that does not respond to topical treatment, ongoing use of moisturizer or skin softening ointment/lotion/cream involving study treatment areas within 3 days before enrollment, hypersensitivity to any component of the investigational product, hepatitis B/C or human immunodeficiency virus (HIV) infection, and alcohol and/or drug abuse were defined as other exclusion criteria for healthy volunteers and patients with psoriasis.
Treatment
GN-037 cream contained clobetasol 17-propionate (0.0356%), salicylic acid (4.74%), urea (9.48%), and retinoic acid (0.0012%) as active pharmaceutical ingredients. Placebo cream was produced with the same appearance, color, and odor as GN-037 cream, except for active pharmaceutical ingredients. Study treatments were dispensed to subjects during clinic visits and administered at home between clinic visits after the initial instructive application at the clinical site. Subjects were instructed to apply topically a sufficient quantity of study medication to cover the target lesion as a thin layer twice daily for 14 days. For dosage titration in healthy volunteers (low, medium, and high dose), the application target area was defined by a plastic wrap provided to volunteers with the exact cm2 area that volunteers were asked to cover the skin area during the application to prevent excessive use. Study medication tubes were collected and weighed after the study to define the amount of cream applied by volunteers.
Assessments
Safety assessments in healthy subjects and patients with psoriasis included the continuous assessment of the incidence and severity of AEs, local tolerability in the treatment area, clinical laboratory assessments (including hematology, fasting chemistry, fasting lipid panels, and urinalysis), electrocardiogram (ECG) changes, vital signs, and physical examinations. Blood samples were taken for the evaluation of plasma TNF-α, IL-17 and IL-23 at the screening, at the time points of day 6 and day 19. TNF-α analysis was performed using the DiaSource enzyme-linked immunosorbent assay (ELISA) kit (ImmunoAssays S.A., Louvain-la-Neuve, Belgium), and interleukin analysis was performed using LSBio kits (Seattle, WA, USA). Pharmacokinetic (PK) endpoints were evaluated through detection of clobetasol 17-propionate concentrations in postdose samples at steady state through blood samples collected 1 and 5 h after the last administration of study treatment on day 14. Quantitative determination of clobetasol 17-propionate in human plasma was performed using the liquid chromatography tandem mass spectroscopy (LC–MS/MS) method developed and validated with calibration curves ranging from 0.1 to 10 ng/mL at Novagenix Bioanalytical Drug R&D Center, Ankara, Turkey.
PGA, Psoriasis Area and Severity Index (PASI), Target Plaque Severity Score (TPSS), and percentage of BSA involvement were evaluated at screening, day 6, and day 14 during the application of study drugs to patients. Clinical evaluations of psoriasis were performed by an experienced and qualified dermatologist. The efficacy outcomes were defined as the change from baseline in the PGA, and TPSS scores on days 6 and 14. PASI and BSA% on days 6 and 14 were also assessed for monitorization, since only one target lesion in each patient was treated with GN-037 as mentioned above. PGA was scored on a five-point scale from clear (score = 0) to severe (score = 5), reflecting an overall assessment of erythema, induration, and scaling across all lesions over the whole body. BSA involvement was assessed separately for four body regions: head and neck, upper limbs, trunk, and lower limbs. The total BSA affected by psoriasis is estimated based on the area of the patient’s handprint (the entire palmar surface, including the fingers), which is approximately 1% of the total BSA.
For TPSS evaluation, a single target plaque was selected at baseline. It was assessed separately for induration, scaling, and erythema using a five-point severity scale (0, none; 1, slight; 2, moderate; 3, marked; 4, very marked), and the scores were summed to obtain the TPSS sum score [13-point scale = 0 (no severity), 12 (high severity)]. PASI was defined as a composite score of the degree of erythema, induration, and scaling (each scored separately) for each of the four body regions, with adjustment for the percentage of BSA involved for each region and for the proportion of the region to the whole body.
Data Analysis
The main objective of this study was to explore the safety and tolerability of the investigational product GN-037. The secondary objectives were efficacy and evaluation of PK and plasma cytokine levels. The safety population included all subjects who received at least one dose of the study drug. Efficacy was evaluated for the per-protocol population, including a psoriatic patient population (n = 6) with no critical protocol violations. The PK population included all subjects with at least one blood sample collected at a time appropriate for steady-state concentrations, and analysis was performed for plasma clobetasol 17-propionate concentrations.
Only descriptive statistical evaluations were performed for the treatment groups. Categorical variables were summarized with counts (n) and percentages (%). For plasma TNF-α, IL-17, and IL-23 cytokine levels, the geometric means were calculated in all treatment groups, and cytokine levels are shown as pg/mL. The descriptive statistics were calculated by using SPSS version 24.0.
The incidence of AE was based on the number of subjects in the respective analysis population and treatment group. AEs were coded according to the Medical Dictionary for Regulatory Activities (MedDRA) for reporting at the “Preferred Terms” level.
Results
Patients
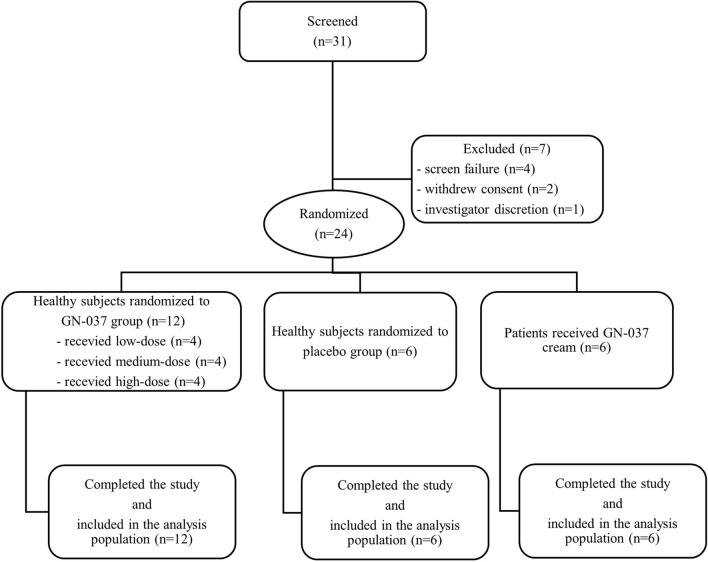
A total of 31 participants were screened between 17 February 2022 and 28 April 2022. Seven out of 31 were assessed as ineligible during the screening process (four screen failed, two withdrew consent, and one investigator discretion). Twenty-four participants who met the inclusion/exclusion criteria consisted of 18 healthy subjects and 6 patients with plaque psoriasis received study treatment. Out of 18 healthy volunteers, 12 were randomized to GN-037 and 6 to placebo group. Six patients with plaque psoriasis were treated with GN-037 cream (Fig. 1). Across the study groups, all subjects completed the study and were included in the safety and efficacy analysis.
Fig. 1.
Participant flow and disposition
The mean age was 38.0 and 33.3 years and 77.8% and 66.7% were men in the healthy subjects and patient groups, respectively. All subjects had no concomitant diseases or treatments, and mean body mass index was 26.1 and 23.6 kg m−2, in the healthy subjects and patient groups, respectively (Table 1).
Table 1.
Baseline demography and disease characteristics
| Characteristic | Patients with plaque psoriasis | Healthy subjects |
|---|---|---|
| N = 6 | N = 18 | |
| Sex (male), n (%) | 4 (66.7) | 14 (77.8) |
| Age (years) mean (SD) | 33.3 (9.2) | 38.0 (4.4) |
| Range | 19–43 | 26–43 |
| Weight (kg), mean (SD) | 71.0 (12.3) | 79.9 (13.5) |
| Range | 51.9–84.0 | 48.0–102.0 |
| Body mass index (kg m−2), mean (SD) | 23.6 (2.9) | 26.1 (2.7) |
| Range | 20.0–27.1 | 20.0–29.8 |
| PGA score, mean (SD)a | 3.83 (0.41) | – |
| 3: Moderate, n (%) | 1 (16.7) | – |
| 4: Severe, n (%) | 5 (83.3) | – |
| TPSS score, mean (SD)b | 2.33 (0.52) | – |
| 2: Moderate, n (%) | 4 (66.7) | – |
| 3: Severe, n (%) | 2 (33.3) | – |
| BSA %, rangec | 1–4 | – |
| PASI score, ranged | 0.5–1.6 | – |
a The Physician’s Global Assessment (PGA) is a five-point scale for assessing plaque thickening, scaling, and erythema; scores range from 0 (clear) and 1 (almost clear) to 4 (severe), with higher scores indicating more severe psoriasis. Patients in this trial were required to have a score of 3 (moderate) or higher
b The target plaque severity score (TPSS) is a measurement that scores the selected target lesion at baseline individually for signs of induration, scaling, and erythema using a five-point severity scale: 0 = none; 1 = mild; 2 = moderate; 3 = severe; 4 = very severe
c Percentage of the body surface area affected by psoriasis
d Psoriasis Area and Severity Index (PASI) is a measurement that combines the affected severity of the lesions and the area into one score; scores range from 0 (no disease) to 72 (maximal disease)
At baseline, psoriatic patients had PGA scores of 3 (n = 1, 16.7%) or 4 (n = 5, 83.3%) and TPSS scores of 2 (n = 4, 66.7%) or 3 (n = 2, 33.3%). The percentage of baseline BSA involvement of psoriatic plaques ranged from 1.0% to 4.0%, and the baseline PASI scores ranged from 0.9 to 1.6. The mean PGA and TPSS scores at baseline for the patient population were 3.83 and 2.33, respectively.
Safety
A total of 31 AEs occurred in 13 participants throughout the study: 9 healthy subjects who received GN-037 cream, 3 who received placebo, and 1 psoriasis patient who received GN-037 cream. Most AEs (97%) were mild in severity, and only one case of headache reported at the medium dose level of the GN-037 group was rated moderate. There were no relevant differences in laboratory values, vital signs, electrocardiograms, or physical (nondermatological) examinations across groups. There were no serious AEs, deaths, or discontinuations due to AEs.
Ten frequently reported AEs were application site reactions, including erythema, exfoliation, pruritus, and burning sensation. Three healthy subjects receiving medium dose, two receiving low-dose, and one receiving a high-dose GN-037 cream experienced erythema and exfoliation. Pruritus and burning sensation were reported in two healthy subjects in the medium- and high-dose groups. Pruritus (n = 2), erythema (n = 1), and increase in temperature at the application site (n = 1) occurred in the placebo group. Only one patient with plaque psoriasis experienced a burning sensation at the application site during the first 4 days of treatment, which resolved within a few minutes after the administration of the GN-037 cream (Table 2). All reactions at the application site were considered treatment related in each treatment group.
Table 2.
Overall summary of adverse events
| Healthy volunteers | Patients with plaque psoriasis | ||||
|---|---|---|---|---|---|
| Low dose GN-037 |
Medium dose GN-037 |
High dose GN-037 |
Placebo | GN-037 | |
| MedDRA SOC/PT, n (%) | N = 4 | N = 4 | N = 4 | N = 6 | N = 6 |
| General disorders and administration site conditions | 2 (50) | 3 (75) | 2 (50) | 2 (33.3) | 1 (16.7) |
| Application site burning sensation | – | 1 (25) | 1 (25) | – | 1 (16.7) |
| Application site erythema | 2 (50) | 2 (50) | 1 (25) | 1 (16.7) | – |
| Application site exfoliation | 2 (50) | 2 (50) | 1 (25) | – | – |
| Application site pain | 1 (25) | – | – | – | – |
| Application site pruritus | – | 1 (25) | 1 (25) | 2 (33.3) | – |
| Application site rash | – | 1 (25) | – | – | – |
| Application site swelling | – | – | 1 (25) | – | – |
| Application site temperature increase | – | – | – | 1 (16.7) | – |
| Investigations | – | 1 (25) | – | – | – |
| Alanine aminotransferase increased | – | 1 (25) | – | – | – |
| Aspartate aminotransferase increased | – | 1 (25) | – | – | – |
| Cardiac disorders | – | – | – | 1 (16.7) | – |
| Tachycardia | – | – | – | 1 (16.7) | – |
| Skin and subcutaneous tissue disorders | 1 (25) | – | – | – | – |
| Paresthesia | 1 (25) | – | – | – | – |
| Nervous system disorders | – | 1 (25) | – | – | – |
| Headache | – | 1 (25) | – | – | – |
| Infections and infestations | – | – | – | 1 (16.7) | – |
| COVID-19 infection | – | – | – | 1 (16.7) | – |
| Gastrointestinal disorders | – | – | – | 1 (16.7) | – |
| Aphthous ulcer | – | – | – | 1 (16.7) | – |
N number of patients, SOC system organ classes, PT preferred term
Nondermatological AEs including elevation of alanine aminotransferase (ALT) and aspartate aminotransferase (AST), headache, tachycardia, coronavirus disease 2019 (COVID-19) infection, paresthesia, and aphthous ulcer were reported in five healthy subjects, none of which was related to treatment as judged by the investigator. The elevation of ALT and AST occurred in one healthy subject in the medium-dose group who had recovered after 1 week without requiring any action. A subject who received placebo tested positive on day 14 for COVID-19 infection; the polymerase chain reaction (PCR) test was performed 10 days after the disease and was found to be negative without the need for any treatment.
The median total amount of cream applied in 14 days by healthy subjects in different groups was as follows: low-dose group: 13 g, medium-dose group: 23.5 g; high-dose group: 33.5 g.
Efficacy
The efficacy results were measured in six patients with psoriasis: four men and two women. At baseline, one patient had a PGA score of 3 (moderate) and five patients had a PGA score of 4 (severe), and the PGA score remained stable until day 6. Four patients had a two-grade improvement in PGA score and two patients experienced a three-grade improvement on day 14 compared with baseline, indicating a shift of patients from moderate and severe disease to mild and almost clear (score 2 or 1).
Four patients had a TPSS score of 2 (moderate) and two patients had a TPSS score of 3 (severe) to target plaque severity at baseline. GN-037 cream showed sustained efficacy during the 2-week treatment period. Three patients had a TPSS score of 1 (mild) by experiencing at least ≥ 1-grade improvement on day 6, and all patients achieved mild (score 1) TPSS scores with day 14 (Table 3). Since only one target lesion in each patient was treated with GN-037, BSA and PASI scores remained stable throughout the assessments.
Table 3.
Score evaluations in patients with plaque psoriasis
| Day 0 | Day 6 | Day 14 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Target lesion | BSA | PGA | TPSS | BSA | PGA | TPSS | BSA | PGA | TPSS | |
| Patient 1 | Back of the neck | 2% | 4 | 2 | 2% | 4 | 2 | 2% | 1 | 1 |
| Patient 2 | Sacral region | 1% | 3 | 2 | 1% | 3 | 1 | 1% | 1 | 1 |
| Patient 3 | Outer plaque on the right leg | 3% | 4 | 2 | 3% | 4 | 1 | 3% | 2 | 1 |
| Patient 4 | Right tibia anterior surface | 3% | 4 | 2 | 3% | 4 | 2 | 3% | 2 | 1 |
| Patient 5 | Right tibia anterior surface | 4% | 4 | 3 | 4% | 4 | 1 | 4% | 2 | 1 |
| Patient 6 | Back of the right lower leg | 2% | 4 | 3 | 2% | 4 | 3 | 2% | 1 | 1 |
BSA body surface area, PGA Physician Global Assessment, TPSS Target Plaque Severity Score
Pharmacokinetic Data
Blood samples were taken for PK evaluation from all subjects; however, plasma concentrations of clobetasol-17 propionate were not detected in most of the samples (70 out of 72, 97.2%), where the lower limit of quantification (LLOQ) was 100 pg/mL. Detected clobetasol-17 propionate concentrations were below the LLOQ.
Plasma Cytokine Levels
Subjects in the placebo group had slightly lower levels of the geometric mean of plasma IL-23 cytokines compared with other groups; the highest level was observed on day 19, which was 6.71 pg/mL. Although there was a slight increase between baseline and day 6 in healthy volunteers who received low-dose GN-037 cream, IL-23 levels did not change on day 19. Moreover, a gradual increase in the level of IL-23 cytokines from baseline to day 19 was observed in healthy volunteers who were treated with medium-dose treatment. IL-23 levels decreased from 6.12 to 4.91 pg/mL on day 6 in healthy volunteers who were treated with high doses and showed an increase on day 19. There was a gradual increase in the level of IL-23 cytokines in the placebo group on day 19, similarly to other dose groups treated with GN-037 (Table 4).
Table 4.
Plasma cytokine levels in healthy subjects and psoriasis patients
| Healthy volunteers | Patients with plaque psoriasis | ||||
|---|---|---|---|---|---|
| Low dose GN-037 |
Medium dose GN-037 |
High dose GN-037 |
Placebo | GN-037 | |
| N = 4 | N = 4 | N = 4 | N = 6 | N = 6 | |
| IL-23 | |||||
| Day 0 | 6.43 | 5.61 | 6.12 | 5.36 | 6.00 |
| Day 6 | 7.27 | 6.43 | 4.91 | 5.09 | 5.72 |
| Day 19 | 7.31 | 8.12 | 7.40 | 6.71 | 7.57 |
| IL-17 | |||||
| Day 0 | 2.99 | 2.76 | 2.96 | 2.66 | 2.84 |
| Day 6 | 2.99 | 4.89 | 4.96 | 3.85 | 4.39 |
| Day 19 | 4.75 | 4.78 | 5.18 | 3.96 | 5.17 |
| TNF-α | |||||
| Day 0 | 4.99 | 4.38 | 5.34 | 4.74 | 4.57 |
| Day 6 | 5.01 | 5.10 | 6.35 | 6.02 | 5.79 |
| Day 19 | 6.85 | 4.29 | 3.11 | 6.07 | 7.24 |
IL interleukin, TNF-α tumor necrosis factor alpha
While IL-17 levels were not changed until day 6, a slight increase was observed in healthy volunteers who received low-dose GN-037 cream on day 19. Moreover, IL-17 level increased to ~ 4.9 pg/mL in healthy volunteers treated with medium- and high-dose GN-037 cream, and the level remained stable until day 19. Furthermore, a gradual increase in IL-17 levels was detected in patients throughout the study (Table 4).
Finally, subjects who received placebo demonstrated an increase in the geometric mean of plasma TNF-α on day 6, and this level did not increase further on day 19. In subjects receiving low-dose GN-037 cream, similar levels of TNF-α were detected at baseline and on day 6, but it was increased to 6.85 pg/mL at the follow-up visit on day 19. TNF-α levels fluctuated throughout the study in subjects treated with medium and high doses. TNF-α levels slightly increased on day 6 in both medium- and high-dose groups and then returned to the baseline level in medium-dose group, whereas it was below the baseline level in high-dose group. Similar to IL-17 levels, TNF-α levels also steadily increased in psoriasis patients throughout the study (Table 4).
Discussion
The results of this phase 1 trial in 18 healthy volunteers and 6 patients with plaque psoriasis demonstrated a favorable safety and tolerability profile of GN-037 cream. Furthermore, the GN-037 cream showed an excellent efficacy signal in six patients with mild to moderate plaque psoriasis as evidenced by lower PGA and TPSS scores on day 14.
The GN-037 cream formulation contains clobetasol 17-propionate, salicylic acid, retinoic acid, and urea as active pharmaceutical ingredients. Clobetasol-17 propionate, a potent corticosteroid, is commonly used in topical formulations to treat local lesions. Several studies have evaluated the efficacy of clobetasol 17-propionate as a cream or ointment in treating psoriasis [15]. However, since most psoriasis patients have mild psoriasis at presentation and such mild lesions can be controlled using topical therapies, only, optimized topical combination preparations of corticosteroids with other active pharmaceutical compounds may also be preferred [3].
Long‐term management of plaque psoriasis with topical agents is reported to be suboptimal [16]; therefore, frequent relapses are inevitable. Thus, novel topical combination treatment options may provide better outcomes in reducing the occurrence of these relapses and eventually improving the quality of life in these patients.
The most common AEs in the present study were reactions at the application site, including erythema, exfoliation, pruritus, and burning sensation in healthy subjects, and almost all AEs (97%) were mild in severity. These AEs were well tolerated, and none resulted in discontinuation of treatment, clearly indicating that GN-037 cream is tolerable. Furthermore, most of the AEs were similar to the AEs reported for other topical corticosteroid preparations [17–19]. We did not observe folliculitis, telangiectasia, or atrophy in our study, whereas these were previously reported for other topical preparations [20].
Although only six patients with plaque psoriasis received GN-037 treatment for a relatively short duration (i.e., 2 weeks), a remarkable clinical improvement was seen in this group. This positive observation will be explored for a possible significant improvement in a randomized double-blind phase 2 setting in which the safety and efficacy of GN-037 cream will be investigated in a larger patient population with optimal treatment duration.
In psoriasis, increased levels of TNF-α and interferon promote the activation of IL-23-producing dermal dendritic cells, causing the expansion of Th17 cell clones producing IL-17 [21]. Activated Th17 cells secrete large amounts of IL-17, IL-26, IL-29, and TNF-α, resulting in a “feedforward” inflammatory cytokine cascade in epidermal keratinocytes and the development of early psoriatic lesions [22]. Since TNF-α, IL-17, and IL-23 were shown to be upregulated in patients with psoriasis, these three cytokine levels were measured in all volunteers at baseline and on days 6 and 19. In this study, we did not intend to monitor cytokine expression alterations in patients with psoriasis but rather to explore the effects of an investigational GN-037 cream formulation on systemic cytokine levels. Furthermore, a 2-week treatment period was designed to obtain more information on the safety of GN-037 in patients with psoriasis. Therefore, a major alteration in plasma cytokine levels was not expected. Additionally, except for two sporadic observations of clobetasol 17-propionate in the plasma of healthy volunteers, there was no systemic absorption of clobetasol 17-propionate, which may explain the similar levels of plasma cytokines in both GN-037 and placebo-treated healthy subjects.
Long-term safety of GN-037 is an essential point for consideration during product development. In similar products that contain relatively potent corticosteroids, local side effects such as cutaneous atrophy, striae, and systemic side effects of adrenal suppression and pustular flares were reported [23]. Although we did not observe these reactions in our trial with a relatively shorter duration of treatment, such reactions might be possible with more prolonged use. Theoretically, as the lesions improve and subsequently reduced amounts of drug application are required, this may result in a lower amount of topical cream use and a potentially limited amount of drug absorbed systemically. In this study, we did not aim to measure hypothalamic–pituitary–adrenal (HPA) axis suppression, which is a commonly reported AE in topical corticosteroid use [24, 25]. However, undetectable steady-state plasma levels of clobetasol 17-propionate in our cohort exclude systemic exposure. Therefore, suppression of the HPA axis with GN-037 treatment would be unlikely.
The present study had certain limitations, such as a small sample size and a relatively short duration (2 weeks) of the treatment period. However, as this study was planned for exploring the initial safety of a topically applied preparation, the sample size was sufficient for providing data specifically for safety in this first-in-human trial. The safety and efficacy of GN-037 cream will be explored in a larger population and for a longer duration in the phase 2 trial. Moreover, changes in the plasma cytokine concentrations and the impact of these changes on the pharmacodynamics of GN-037 will also be investigated in that study.
Conclusions
Topical GN-037 cream treatment was safe in healthy volunteers and patients with plaque psoriasis. Furthermore, clinically meaningful efficacy was observed in six patients; therefore, further clinical development of GN-037 in a phase II clinical trial in patients with mild to moderate plaque psoriasis has been initiated (NCT05706870).
Acknowledgements
We thank the study investigators, the participating sites, the nurses, and study personnel who were involved in this clinical trial, and the healthy subjects, patients, and their families. The authors acknowledge Eyup Topcu and Ahmet Sencan for their contribution to formulation development and Irem Unsal for medical writing support.
Funding
This study was sponsored by Gen İlaç ve Sağlık Ürünleri A.Ş. and partially supported by a research grant from The Scientific and Technological Research Council of Turkey [TUBITAK 1505, grant number: 5180004]. The journal’s Rapid Service Fee is funded by Gen İlaç ve Sağlık Ürünleri A.Ş.
Medical Writing and Editorial Assistance
The authors acknowledge Irem Unsal from Monitor CRO (Istanbul, Turkey) for her contribution to medical writing/editorial assistance. This assistance service was funded by Gen İlaç ve Sağlık Ürünleri A.Ş.
Author Contributions
Zafer Sezer, Ahmet Inal, Mustafa M. Mazicioglu, Hatice Y. Karasulu, Sedat Altug and Nadir Ulu contributed to the study design. All authors contributed to data collection. Salih L. Cinar, Sedat Altug, Serhat Kozlu and Nadir Ulu contributed to data analysis. All authors contributed to drafting and critical appraisal of the manuscript and approved the final version for submission.
Disclosures
Nadir Ulu and Serhat Kozlu report employment on Gen İlaç ve Sağlık Ürünleri A.Ş. Mine Diril and Ayca Mehmetoglu report employment on Sedef İlaç ve Medikal Ürünleri Ind. Trade. Co. Ltd. Other authors declared that they have no potential conflicts of interest with respect to the investigation, authorship, and/or publication of this article.
Compliance with Ethics Guidelines
The trial was carried out according to the ethical standards of the Declaration of Helsinki and the International Conference on Harmonization of Good Clinical Practice Guidelines and its revisions. The study protocol was approved by the Ethics Committee for Clinical Trials of Erciyes University, Kayseri, Turkey, and the Republic of Turkey and was registered on www.clinicaltrials.gov (NCT05428202). Written informed consent/assent was provided by all patients before enrollment.
Data Availability
The analyzed data sets generated during the study are available from the corresponding author on reasonable request.
References
- 1.Augustin M, Glaeske G, Radtke MA, Christophers E, Reich K, Schäfer I. Epidemiology, and comorbidity of psoriasis in children. Br J Dermatol. 2010;162(3):633–636. doi: 10.1111/j.1365-2133.2009.09593.x. [DOI] [PubMed] [Google Scholar]
- 2.Danielsen K, Olsen AO, Wilsgaard T, Furberg AS. Is the prevalence of psoriasis increasing? A 30-year follow-up of a population-based cohort. Br J Dermatol. 2013;168(6):1303–1310. doi: 10.1111/bjd.12230. [DOI] [PubMed] [Google Scholar]
- 3.Schön MP, Boehncke WH. Psoriasis. N Engl J Med. 2005;352(18):1899–1912. doi: 10.1056/NEJMra041320. [DOI] [PubMed] [Google Scholar]
- 4.Jacobson CC, Kumar S, Kimball AB. Latitude and psoriasis prevalence. J Am Acad Dermatol. 2011;65(4):870–873. doi: 10.1016/j.jaad.2009.05.047. [DOI] [PubMed] [Google Scholar]
- 5.Hjuler KF, Gormsen LC, Vendelbo MH, Egeberg A, Nielsen J, Iversen L. Increased global arterial and subcutaneous adipose tissue inflammation in patients with moderate-to-severe psoriasis. Br J Dermatol. 2017;176(3):732–740. doi: 10.1111/bjd.15149. [DOI] [PubMed] [Google Scholar]
- 6.Armstrong AW, Read C. Pathophysiology, clinical presentation, and treatment of psoriasis: a review. JAMA. 2020;323(19):1945–1960. doi: 10.1001/jama.2020.4006. [DOI] [PubMed] [Google Scholar]
- 7.Kamata M, Tada Y. Efficacy and safety of biologics for psoriasis and psoriatic arthritis and their impact on comorbidities: a literature review. Int J Mol Sci. 2020;21(5):1690. doi: 10.3390/ijms21051690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sulzberger MB, Witten VH. The effect of topically applied compound F in selected dermatoses. J Invest Dermatol. 1952;19(2):101–102. doi: 10.1038/jid.1952.72. [DOI] [PubMed] [Google Scholar]
- 9.Reich K, Armstrong AW, Langley RG, Flavin S, Randazzo B, Li S, et al. Guselkumab versus secukinumab for the treatment of moderate-to-severe psoriasis (ECLIPSE): results from a phase 3, randomised controlled trial. Lancet. 2019;394(10201):831–839. doi: 10.1016/S0140-6736(19)31773-8. [DOI] [PubMed] [Google Scholar]
- 10.Sbidian E, Chaimani A, Afach S, Doney L, Dressler C, Hua C, et al. Systemic pharmacological treatments for chronic plaque psoriasis: a network meta-analysis. Cochrane Database Syst Rev. 2017;12(12):CD011535. doi: 10.1002/14651858.CD011535.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Korman NJ. Management of psoriasis as a systemic disease: what is the evidence? Br J Dermatol. 2020;182(4):840–848. doi: 10.1111/bjd.18245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mahil SK, Ezejimofor MC, Exton LS, Manounah L, Burden AD, Coates LC, et al. Comparing the efficacy and tolerability of biologic therapies in psoriasis: an updated network meta-analysis. Br J Dermatol. 2020;183(4):638–649. doi: 10.1111/bjd.19325. [DOI] [PubMed] [Google Scholar]
- 13.Issa N, Kircik L. Supplement individual article: a reappraisal of fixed-combination halobetasol propionate and tazarotene for the treatment of psoriasis: biological underpinnings, therapeutic mechanisms, and economic considerations. J Drugs Dermatol. 2023;22(1):3446174–34461710. [PubMed] [Google Scholar]
- 14.Megna M, Cinelli E, Camela E, Fabbrocini G. Calcipotriol/betamethasone dipropionate formulations for psoriasis: an overview of the options and efficacy data. Expert Rev Clin Immunol. 2020;16(6):599–620. doi: 10.1080/1744666X.2020.1776116. [DOI] [PubMed] [Google Scholar]
- 15.Samarasekera EJ, Sawyer L, Wonderling D, Tucker R, Smith CH. Topical therapies for the treatment of plaque psoriasis: systematic review and network meta-analyses. Br J Dermatol. 2013;168(5):954–967. doi: 10.1111/bjd.12276. [DOI] [PubMed] [Google Scholar]
- 16.Lebwohl M, Thaçi D, Warren RB. Addressing challenges associated with long-term topical treatment and benefits of proactive management in patients with psoriasis. J Eur Acad Dermatol Venereol. 2021;35(Suppl 1):35–41. doi: 10.1111/jdv.17053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gold LS, Lebwohl MG, Sugarman JL, et al. Safety and efficacy of a fixed combination of halobetasol and tazarotene in the treatment of moderate-to-severe plaque psoriasis: results of 2 phase 3 randomized controlled trials. J Am Acad Dermatol. 2018;79(2):287–293. doi: 10.1016/j.jaad.2018.03.040. [DOI] [PubMed] [Google Scholar]
- 18.Chung M, Yeroushalmi S, Hakimi M, Bartholomew E, Liao W, Bhutani T. A critical review of halobetasol propionate foam (0.05%) as a treatment option for adolescent plaque psoriasis. Expert Rev Clin Immunol. 2022;18(10):997–1003. doi: 10.1080/1744666X.2022.2110071. [DOI] [PubMed] [Google Scholar]
- 19.Bhatia N, Stein Gold L, Kircik LH, Schreiber R. Two multicenter, randomized, double-blind, parallel group comparison studies of a novel foam formulation of halobetasol propionate, 0.05% vs its vehicle in adult subjects with plaque psoriasis. J Drugs Dermatol. 2019;18(8):790–796. [PubMed] [Google Scholar]
- 20.Jhaj R, Asati DP, Chaudhary D, Sadasivam B. Topical steroid containing combinations: burden of adverse effects and why the recent regulatory action may not be enough. Indian J Pharmacol. 2021;53(5):371–376. doi: 10.4103/ijp.IJP_728_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hawkes JE, Chan TC, Krueger JG. Psoriasis pathogenesis and the development of novel targeted immune therapies. J Allergy Clin Immunol. 2017;140(3):645–653. doi: 10.1016/j.jaci.2017.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lowes MA, Suarez-Farinas M, Krueger JG. Immunology of psoriasis. Annu Rev Immunol. 2014;32:227–255. doi: 10.1146/annurev-immunol-032713-120225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nakamura M, Abrouk M, Zhu H, Farahnik B, Koo J, Bhutani T. Update on the systemic risks of superpotent topical steroids. J Drugs Dermatol. 2017;16(7):643–648. [PubMed] [Google Scholar]
- 24.Kerdel FA, Draelos ZD, Tyring SK, Lin T, Pillai R. A phase 2, multicenter, double-blind, randomized, vehicle-controlled clinical study to compare the safety and efficacy of a halobetasol propionate 0.01% lotion and halobetasol propionate 0.05% cream in the treatment of plaque psoriasis. J Dermatolog Treat. 2019;30(4):333–339. doi: 10.1080/09546634.2018.1523362. [DOI] [PubMed] [Google Scholar]
- 25.Walsh P, Aeling JL, Huff L, Weston WL. Hypothalamus-pituitary-adrenal axis suppression by superpotent topical steroids. J Am Acad Dermatol. 1993;29(3):501–503. doi: 10.1016/S0190-9622(08)82011-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The analyzed data sets generated during the study are available from the corresponding author on reasonable request.