Abstract
Background
COVID-19 pandemic introduced significant challenges that may have exacerbated healthcare worker (HCW) burnout. To date, assessments of burnout during COVID-19 pandemic have been cross-sectional, limiting our understanding of changes in burnout. This longitudinal study assessed change across time in pediatric HCW burnout during the COVID-19 pandemic and whether demographic and psychological factors were associated with changes in burnout.
Methods
This longitudinal study included 162 physicians, physician assistants, nurses, and medical technicians within the emergency department (ED), intensive care, perioperative, and inter-hospital transport services in a children’s hospital. HCW demographics, anxiety and personality traits were reported via validated measures. HCWs completed the Maslach Burnout Inventory in April 2020 and March 2021. Data were analyzed using generalized estimating equations.
Results
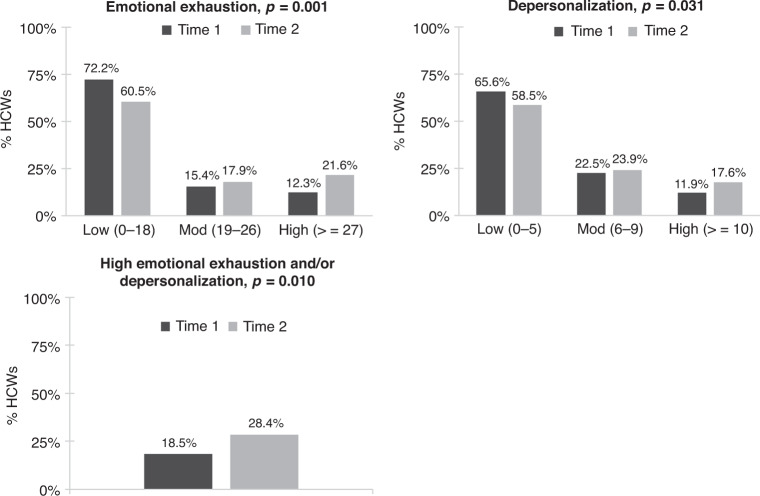
The percentage of HCWs reporting high emotional exhaustion and/or depersonalization burnout increased significantly across time (18.5% to 28.4%, P = 0.010). Factors associated with increased emotional exhaustion included working in the ED (P = 0.011) or perioperative department (P < 0.001), being a nurse or medical technician (P’s < 0.001), not having children (P < 0.001), and low conscientiousness (P < 0.001).
Conclusions
Pediatric HCW burnout significantly increased over 11-months of the COVID-19 pandemic. Results suggest that certain demographic and psychological factors may represent potential area to target for intervention for future pandemics.
Impact
This longitudinal study revealed that the COVID-19 pandemic has had a significant impact on pediatric healthcare worker burnout.
The percentage of healthcare workers reporting high levels of emotional exhaustion and depersonalization burnout increased significantly over 11-months of the COVID-19 pandemic.
Results suggest that certain demographic and psychological factors may represent potential targets for future interventions.
Introduction
Burnout in healthcare is a growing concern with current data estimating that 30–70% of healthcare providers experience burnout.1–4 Prevalence of burnout is similar in pediatric care settings, with data indicating that 20–67% of pediatric healthcare workers (HCWs), including physicians, nurses, and support staff report experiencing burnout.1,4–8 According to the multidimensional theory of burnout, burnout is an individual experience of work- or care-related stress that occurs within a social context and has three components: emotional exhaustion, an impersonal attitude, and a decreased sense of personal competence.9 HCW burnout can result in a host of negative professional and personal consequences including poor clinical care, patient satisfaction, and HCW mental and physical health.2,10–15 Previous work has collectively identified certain demographic (younger age, female, unmarried), occupational (less experience, high-acuity setting, workload), professional role (nurses, technicians), and psychological (anxiety, depression) factors associated with higher levels of burnout.3,4,8,15–17
The COVID-19 pandemic has introduced significant clinical care and personal safety challenges that may exacerbate levels of burnout in HCWs.18 A recent review on physician psychological symptoms during infectious disease outbreaks, including COVID-19, reported burnout prevalence rates up to 75%.19 Results from cross-sectional studies assessing burnout during COVID-19 specifically indicate that United States HCWs may be experiencing higher levels of burnout compared to those in other countrie,20–22 and data suggest that social isolation, work experience, and contact with COVID-19 patients may be associated with higher levels of burnout.22–26
To date, limited longitudinal data exist on burnout HCW during the COVID-19 pandemic and most of the existing data were collected early in the first year of the pandemic. Longitudinal assessments of burnout may help us better understand the impact of the pandemic on HCWs and, importantly, identify risk and protective factors associated with burnout trajectory.
The objective of the current study was to conduct a longitudinal assessment of burnout among pediatric HCWs from April 2020 to March 2021. We aimed to assess whether there was a change in pediatric HCW burnout over an eleven-month period during the COVID-19 pandemic and identify demographic and psychological factors associated with change in burnout. Informed by the multidimensional theory of burnout and by previous results from cross-sectional studies of HCW burnout, we hypothesized that years of experience,5,15 parental status,3 anxiety,19,22 and conscientious27 and neuroticism personality characteristics27,28 would be associated with changes in burnout.
Methods
Design/Participants
The current study employed a longitudinal, observational study design to assess change in burnout during the COVID-19 pandemic. The study included a convenience sample of HCWs enrolled in a larger longitudinal study29,30 assessing COVID-19 antibody seroprevalence in HCWs at a quaternary care pediatric hospital in Orange, California USA. Participants of the study included attending physicians, physician assistants (PAs), nurse practitioners (NPs), registered nurses (RNs), and medical technicians with direct patient contact in the emergency department (ED), pediatric intensive care unit, perioperative services, and the inter-hospital transport services teams. Results of this the larger seroprevalence study were previously reported elsewhere.29,30 This present analysis focuses only on a sub-sample of HCWs who were given and completed burnout measures on April 2020 (Time 1) and March 2021 (Time 2). Results included in this report were not published previously.
Measures
Demographics and occupation
A demographics questionnaire assessed HCWs self-reported age, sex, race, marital status, number of children, job position, and years of experience (post-training).
Personality
The Big Five Inventory31 assessed the ‘Big Five’ dimensions of personality: openness (sample α = 0.66), conscientiousness (sample α = 0.69), extraversion (sample α = 0.762), agreeableness (sample α = 0.77), and neuroticism (sample α = 0.78). This 44-item measure is widely used to assess personality, has demonstrated reliability and validity across large international adult samples, and has been used in health care worker samples.27,32,33 The personality dimension subscale average scores were used for analyses.
Anxiety
HCW trait anxiety was assessed via the State-Trait Anxiety Inventory (STAI), which is a 20- item self-report measure used to assess adult general (trait) anxiety. The STAI is considered a gold standard measurement for anxiety, demonstrating good reliability and validity in diverse adult samples and health care workers.34–38 A cut-off score of 4039 has been utilized to detect clinically significant symptoms of anxiety. The total and cut-off scores were used in analyses (α = 0.87).
Primary outcome
Burnout
Maslach Burnout Inventory – Human Services Survey (MBI-HSS)11 is the most widely accepted measure for the assessment of burnout in health care workers and has demonstrated validity across international samples of health care workers.40–43 This measure assesses three dimensions of burnout in healthcare service workers: emotional exhaustion (i.e., feelings of being emotionally overextended by one’s work), depersonalization (i.e., an impersonal response to one’s service or responsibilities), and personal accomplishment (i.e., feelings of competence and successful achievement in one’s work with people) dimensions of burnout. Each of the 22 items are rated on a seven-point Likert-type scale ranging from never to everyday. Higher emotional exhaustion and depersonalization scores reflect higher burnout within those dimensions whereas lower personal accomplishment scores reflect higher burnout within the personal accomplishment burnout dimension. The MBI-HSS authors recommend utilizing continuous total scores for each burnout dimension when examining predictors or outcomes of burnout, but low, moderate and high population norms can be used to characterize levels of burnout across samples.11,44,45 This study utilized both the continuous total emotional exhaustion, depersonalization, and personal accomplishment scores and characterized burnout dimension scores into low, moderate, and high levels based on published norms.11 Sample Cronbach’s alphas for Emotional Exhaustion, Depersonalization and Personal Accomplishment were 0.89, 0.71, and 0.80, respectively.
Procedures
Study data were collected during the spring of 2020 (April–May; Time 1) and in March 2021 (Time 2) as part of a larger study examining seroprevalence of SARS-CoV-2 in HCWs.29,30 HCWs were recruited via department-wide emails and interested HCWs completed informed consent. At Time 1, selected participants completed demographics and the first burnout assessment. At Time 2, those participants completed the second burnout assessment and personality and anxiety questionnaires. Participant questionnaires were administered via REDCap. Ethical approval for all study procedures was obtained from the Children’s Hospital of Orange County Institutional Review Board (# 200452).
Data analyses
Study participants were described by percentage with defined trait for categorical and by mean (SD) for continuous factors. Burnout outcomes were described by mean (SD) and categorically (percent low, moderate, and high) at Time 1 and Time 2. Based on normative data,11 the interpretation of the total subscale scores are as follows: emotional exhaustion low 0–16, moderate 17–26, high 27–54; depersonalization low 0–6, moderate 7–12, high 13–35; personal accomplishment (lower scores reflect higher burnout) low 0–31, moderate 32–38, high 39–48. To aide in the comparison of current sample burnout levels to other health care provider samples,3,46,47 categorical burnout data for those that endorsed high emotional exhaustion and/or depersonalization burnout are also reported. When <10% of items were missing on any measure subscale, the value was imputed based on mean of remaining items. Imputation was required in less than 5% (n = 6) of participants. Generalized estimating equations (GEE) analyses with specification of repeat measures and exchangeable correlation structure assessed significance of change across time in burnout scale scores. In the GEE analyses, distribution specification was determined by parameterization of outcome (binomial, ordinal, or linear). For burnout subscales that demonstrated a significant change from Time 1 to Time 2, bivariate analyses examined whether change in average burnout scale scores were associated with HCW demographics and occupational and psychological characteristics. Multivariate analyses were used to model the composite of risk and protective factors that contributed to change in burnout using a stepwise procedure. Each factor and interaction with time was stepped into the multivariate model in order of significance in the bivariate examination. Factors were retained in the final model when their interaction with time was significant at the 0.05 level. The study sample size of 162 participants provided 99.0% power to detect the average difference of 3.3 points (SD = 9.7) in our primary outcome of pediatric HCW’s burnout from emotional exhaustion at the 0.05 level of significance. Analyses were conducted using SPSS Statistics for Windows, Version 27.0. Armonk, NY:IBM Corp.
Results
A total of 863-institution wide HCWs were emailed about the study and enrollment was discontinued at 382 due to availability of testing resources for the larger seroprevalence study.29,30 Out of the 382 participants that completed study measures at Time 1 (T1), 162 (42.4%) completed measures at Time 2 (T2). Sample demographics and descriptive statistics for participants that completed measures at T1 and T2 are presented in Table 1. It is important to note that T1 emotional exhaustion (t = –0.77, P > 0.05) and depersonalization burnout (t = –1.34, P > 0.05) did not significantly differ between the HCWs who completed only T1 and the HCWs who completed T1 and T2.
Table 1.
Healthcare worker demographic characteristics (N = 162).
| N (%) | Mean (SD) | |
|---|---|---|
| Age (years) | ||
| ≤30 | 44 (27.2%) | |
| 31–40 | 53 (32.7%) | |
| 41–50 | 40 (24.7%) | |
| >50 | 25 (15.4%) | |
| Sex (Female) | 115 (71.0%) | |
| Race | ||
| Asian | 24 (14.8%) | |
| Hispanic | 20 (12.3%) | |
| White | 112 (61.1%) | |
| Multi-Racial/ Other | 6 (3.7%) | |
| Marital Status (Married) | 107 (66.0%) | |
| Children (Yes) | 78 (65.0%) | |
| Department | ||
| Emergency Department | 87 (53.7%) | |
| Intensive Care Unit | 31 (19.1%) | |
| Perioperative | 36 (22.2%) | |
| Transport | 8 (4.9%) | |
| Position | ||
| Nurse (RN) | 85 (52.5%) | |
| Nurse Practitioner/ Physician Assistant | 11 (6.8%) | |
| Physician (MD) | 36 (22.2%) | |
| Medical Techniciana | 30 (18.5%) | |
| Years of experience (median (IQR)) | 12.2 (6.0, 20.0) | |
| Big Five Personality Domains (Score ≥ 4)b | ||
| Extraversion | 88 (54.3%) | 3.5 (0.8) |
| Agreeableness | 135 (83.3%) | 4.2 (0.6) |
| Conscientiousness | 132 (81.5%) | 4.0 (0.6) |
| Neuroticism/Negative Emotionality | 10 (6.2%) | 2.2 (0.8) |
| Openness | 113 (69.8%) | 3.7 (0.6) |
| Trait Anxiety (Total Score > 40)b | 70 (43.2%) | 39.7 (7.9) |
aMedical Technician’ included specialty technicians, medical assistants, transport staff, and administrative support.
bPersonality domain item agreement score ranges from 1 to 5 with higher scores suggesting attitude more aligned with domain; agree or strongly agree, score ≥4; bScores >40 indicate high anxiety.
From T1 to T2, we observed a significant increase in the percentage of HCWs endorsing high levels of emotional exhaustion and/or high levels of depersonalization burnout from T1 to T2 (18.5% vs. 28.4%, P = 0.01; Fig. 1). There was also a significant increase in both emotional exhaustion and depersonalization total burnout scores (Table 2 and Table 3, respectively). Personal accomplishment burnout did not significantly change from T1 (40.0, 95% CI 39.0–41.1) to T2 (39.2, 95% CI 38.2–40.3; P = 0.08).
Fig. 1. Change in burnout from emotional exhaustion and depersonalization evaluated categorically (Time 1 to Time 2), unadjusted.
GEE analyses with repeat measures specified determined significance of change, respectively. HCWs=Healthcare Workers.
Table 2.
Bivariate emotional exhaustion burnout results.
| Estimated mean sum score | Emotional exhaustion burnout | Factor level p value | |
|---|---|---|---|
| Time 1 (95% CI) | Time 2 (95% CI) | ||
| Burnout | 14.4 (12.8, 16.0) | 17.7 (16.2, 19.3)** | |
| Age, years | <0.001 | ||
| <=30 | 15.2 (12.3, 18.1) | 23.9 (21.0, 26.9)** | |
| 31–40 | 15.0 (12.4, 17.7) | 17.4 (14.7, 20.0) | |
| 41–50 | 13.4 (10.3, 16.4) | 14.1 (11.0, 17.1) | |
| >=50 | 13.4 (9.6, 17.3) | 13.4 (9.6, 17.3) | |
| Sex | 0.380 | ||
| Female | 14.5 (12.6, 16.4) | 18.2 (16.4, 20.1)** | |
| Male | 14.2 (11.3, 17.1) | 16.5 (13.6, 19.4) | |
| Race | 0.150 | ||
| Asian | 17.1 (13.0, 21.1) | 19.8 (15.7, 23.8) | |
| Hispanic | 10.1 (5.6, 14.5) | 17.7 (13.2, 22.1)** | |
| White | 14.7 (12.8, 16.6) | 17.6 (15.7, 19.5)** | |
| Multi-Racial/Other | 12.5 (4.4, 20.6) | 12.5 (4.4, 20.6) | |
| Marital Status | <0.001 | ||
| Married | 14.7 (12.8, 16.6) | 16.0 (14.1, 17.9) | |
| Not married | 13.9 (11.2, 16.5) | 21.1 (18.4, 23.8)** | |
| Children | <0.001 | ||
| Yes | 13.6 (11.5, 15.8) | 14.3 (12.1, 16.4) | |
| No | 15.4 (12.5, 18.4) | 23.3 (20.3, 26.3)** | |
| Department | 0.258 | ||
| Emergency Department | 14.6 (12.4, 16.7) | 18.2 (16.1, 20.4)** | |
| Intensive Care Unit | 13.8 (10.2, 17.4) | 15.8 (12.2, 19.4) | |
| Perioperative | 15.0 (11.6, 18.3) | 19.8 (16.5, 23.1)** | |
| Transport | 12.6 (5.6, 19.7) | 10.7 (3.6, 17.7) | |
| Position | 0.008 | ||
| Nurse (RN) | 14.9 (12.8, 17.1) | 17.9 (15.7, 20.0)** | |
| NP/PA | 10.9 (5.0, 16.9) | 12.8 (6.9, 18.8) | |
| Physician | 14.1 (10.8, 17.4) | 14.7 (11.4, 18.0) | |
| Medical Technician | 14.7 (11.1, 18.3) | 22.8 (19.2, 26.4)** | |
| Years of experience | (r = –0.303**) | <0.001 | |
| Personality | |||
| Extraversion | 0.399 | ||
| ≥4 | 12.7 (10.6, 14.9) | 15.2 (13.1, 17.4)* | |
| <4 | 16.4 (14.1, 18.8) | 20.2 (17.8, 22.6)** | |
| Agreeableness | 0.293 | ||
| ≥4 | 16.8 (15.1, 18.5) | 13.9 (12.2, 15.6)** | |
| <4 | 16.5 (12.6, 20.3) | 21.5 (17.7, 25.3)** | |
| Conscientiousness | 0.041 | ||
| ≥4 | 13.7 (12.0, 15.4) | 16.4 (14.6, 18.1)** | |
| <4 | 17.8 (14.1, 21.4) | 24.4 (20.8, 28.1)** | |
| Neuroticism | 0.172 | ||
| ≥4 | 21.7 (15.5, 27.8) | 29.0 (22.8, 35.2)* | |
| <4 | 14.0 (12.4, 15.6) | 17.0 (15.5, 18.6)** | |
| Openness | 0.942 | ||
| ≥4 | 13.9 (11.9, 15.8) | 17.1 (15.2, 19.0)** | |
| <4 | 15.6 (12.8, 18.4) | 19.0 (16.2, 21.8)* | |
| Trait Anxiety | 0.016 | ||
| >40 | 18.6 (16.5, 20.8) | 24.0 (21.9, 26.1)** | |
| ≤40 | 11.2 (9.3, 13.1) | 13.0 (11.1, 14.8) | |
Notes. Score norm interpretation: 0–18 low, 19-26, moderate, ≥27 high burnout. Bold italics indicate within level scores that cross burnout norm levels (only noted for variables that were significant at the factor level). NP nurse practitioner; PA physician associate *within level P < .05; **within level P < 0.01.
Table 3.
Bivariate depersonalization burnout results.
| Depersonalization burnout | Factor level P value | ||
|---|---|---|---|
| Estimated mean sum score | Time 1 (95% CI) | Time 2 (95% CI) | |
| Burnout | 4.7 (4.0, 5.4) | 5.4 (4.7, 6.1)* | |
| Age, years | 0.012 | ||
| <=30 | 5.8 (4.5, 7.0) | 8.2 (6.9, 9.5)** | |
| 31–40 | 5.3 (4.1, 6.5) | 5.3 (4.2, 6.5) | |
| 41–50 | 3.7 (2.3, 5.1) | 4.1 (2.7, 5.4) | |
| >=50 | 3.3 (1.6, 5.0) | 3.1 (1.4, 4.8) | |
| Sex | 0.989 | ||
| Female | 4.5 (3.7, 5.3) | 5.2 (4.4, 6.0) | |
| Male | 5.3 (4.0, 6.6) | 6.0 (4.7, 7.3) | |
| Race | 0.247 | ||
| Asian | 6.6 (4.8, 8.4) | 6.5 (4.7, 8.3) | |
| Hispanic | 2.5 (0.5, 4.5) | 4.6 (0.5, 4.5)* | |
| White | 4.7 (3.9, 5.5) | 5.3 (4.4, 6.1) | |
| Multi-Racial/Other | 4.8 (1.0, 8.6) | 7.3 (3.8, 10.9) | |
| Marital Status | 0.011 | ||
| Married | 4.5 (3.6, 5.3) | 4.6 (3.7, 5.4) | |
| Not married | 5.2 (4.0, 6.4) | 7.1 (5.9, 8.3)** | |
| Children | 0.001 | ||
| Yes | 3.8 (3.0, 4.7) | 3.9 (3.0, 4.8) | |
| No | 4.3 (3.1, 5.5) | 6.6 (5.4, 7.8)** | |
| Department | 0.159 | ||
| Emergency Department | 6.0 (5.0, 6.9) | 6.3 (5.4, 7.3) | |
| Intensive Care Unit | 3.7 (2.1, 5.2) | 5.5 (3.9, 7.0)* | |
| Perioperative | 3.1 (1.6, 4.5) | 4.1 (2.6, 5.5) | |
| Transport | 3.0 (-0.0, 6.0) | 1.5 (–1.5, 4.5) | |
| Position | 0.051 | ||
| Nurse (RN) | 4.6 (3.7, 5.6) | 5.5 (4.5, 6.4) | |
| NP/PA | 5.5 (4.1, 6.8) | 5.0 (3.7, 6.3) | |
| Physician | 6.5 (3.8, 9.1) | 4.2 (1.4, 6.9) | |
| Medical Technician | 4.1 (2.5, 5.7) | 5.9 (4.3, 7.5)* | |
| Years of experience | (r = –0.225*) | 0.015 | |
| Personality | |||
| Extraversion | 0.153 | ||
| ≥4 | 4.2 (3.3, 5.2) | 4.5 (3.5, 5.4) | |
| <4 | 5.3 (4.3, 6.3) | 6.5 (5.5, 7.6)* | |
| Agreeableness | 0.028 | ||
| ≥4 | 4.3 (3.6, 5.0) | 4.7 (4.0, 5.4) | |
| <4 | 6.9 (5.3, 8.6) | 9.3 (7.6, 11.0)** | |
| Conscientio usness | 0.039 | ||
| ≥4 | 4.2 (3.4, 4.9) | 4.6 (3.8, 5.3) | |
| <4 | 7.2 (5.7, 8.8) | 9.4 (7.8, 11.0)** | |
| Neuroticism | 0.025 | ||
| ≥4 | 5.2 (2.4, 8.0) | 8.8 (6.0, 11.6)** | |
| <4 | 4.7 (4.0, 5.4) | 5.2 (4.5, 5.9) | |
| Openness | 0.826 | ||
| ≥4 | 4.7 (3.8, 5.5) | 5.4 (4.6, 6.2) | |
| <4 | 4.9 (3.6, 6.1) | 5.5 (4.2, 6.7) | |
| Trait anxiety | 0.265 | ||
| >40 | 6.2 (5.2, 7.2) | 7.3 (6.3, 8.3)* | |
| ≤40 | 3.6 (2.7, 4.5) | 4.0 (3.1, 4.9) | |
Notes. Score norm interpretation: 0–5 low, 6–9 moderate, >=10 high burnout. Bold italics indicate within level scores that cross burnout norm levels (only noted for variables that were significant at the factor level).
NP nurse practitioner, PA physician associate.
*within level P < 0.05; **within level P < 0.01.
HCW characteristics and change in emotional exhaustion burnout
As shown in Table 2, results from bivariate analyses revealed that demographic variables such as age (P < 0.001), job position (P = 0.008), and years of experience (P < 0.001), and psychological variables such as conscientiousness personality (P = 0.041) and anxiety (P = 0.016) factors were significantly associated with increases in emotional exhaustion burnout.
In the final multivariate model (see Table 4), certain job professions (i.e., nurse or technician; P’s < 0.001), departments (i.e., ED [P = 0.011] or perioperative [P < .001]), and conscientiousness personality (P = 0.030) were found to be independent contributing factors to change in emotional exhaustion burnout. In HCWs that endorsed low conscientiousness, average emotional exhaustion increased from low to moderate burnout levels (+7.2, 95% CI 3.3–11.0, P < 0.001).
Table 4.
Multivariate model burnout results.
| Emotional exhaustion | Factor P value | Depersonalization | Factor P value | |||
|---|---|---|---|---|---|---|
| Time 1 (95%CI) | Time 2 (95%CI) | Time 1 (95%CI) | Time 2 (95%CI) | |||
| Adjusted Burnout | 14.3 (12.6–16.0) | 17.4 (15.7–19.1)** | 4.7 (4.1–5.3) | 5.4 (4.8–6.1)* | ||
| Age-years | 0.008 | |||||
| <=30 | 5.2 (3.9–6.4) | 7.8 (6.5–9.0)** | ||||
| Children | <0.001 | |||||
| Yes | 13.6 (11.4–15.7) | 14.4 (12.3–16.5) | ||||
| No | 15.6 (12.7–18.5) | 23.0 (20.0–25.9)** | ||||
| Department | 0.038 | 0.051 | ||||
| Emergency | 14.2 (11.4–17.0) | 17.3 (14.5–20.1)* | 5.9 (5.0–6.7) | 6.0 (5.0–6.9) | ||
| Intensive Care | 13.4 (10.0–16.7) | 15.3 (12.0–18.7) | 3.8 (2.3–5.2) | 5.5 (4.1–7.0)** | ||
| Perioperative | 15.2 (12.1–18.4) | 20.9 (17.7–24.0)** | 3.1 (1.7–4.4) | 4.7 (3.3–6.0)* | ||
| Transport | 13.7 (7.0–20.4) | 10.6 (4.0–17.3) | 3.2 (0.3–6.0) | 2.3 (–0.6 to 5.1) | ||
| Position | 0.008 | |||||
| Nurse (RN) | 14.5 (12.2–16.8) | 18.3 (16.0–20.6)** | ||||
| NP/PA | 11.5 (3.8–19.2) | 12.6 (4.9–20.3) | ||||
| Physician | 14.6 (11.2–18.1) | 14.0 (10.5–17.5) | ||||
| Medical Technician | 13.8 (9.4–18.2) | 21.2 (16.7–25.6)** | ||||
| Personality | ||||||
| Agreeableness | 0.040 | |||||
| ≥4 | 4.3 (3.6–5.0) | 4.8 (4.1–5.5) | ||||
| <4 | 6.8 (5.2–8.3) | 8.9 (7.3–10.5)** | ||||
| Conscientiousness | 0.030 | |||||
| ≥4 | 13.5 (11.7–15.3) | 16.0 (14.2–17.8)** | ||||
| <4 | 18.7 (14.2–23.3) | 25.9 (21.4–30.4)** | ||||
| Neuroticism | 0.037 | |||||
| ≥4 | 4.4 (1.9–7.0) | 7.5 (5.0–10.1)** | ||||
| <4 | 4.7 (4.1–5.4) | 5.3 (4.6–5.9) | ||||
Notes. Score norm interpretation for emotional exhaustion: 0–18 low, 19-26, moderate, ≥27 high burnout. Score norm interpretation for depersonalization: 0–5 low, 6–9 mod, ≥10 high burnout. Bold italics indicate within level scores that cross burnout norm levels (only noted for variables that were significant at the factor level).
NP nurse practitioner, PA physician associate.
*within level P < 0.05; **within level P < 0.01.
HCW characteristics and change in depersonalization burnout
Bivariate analyses for depersonalization burnout also indicated that both demographic (HCW age, marital status, parental status, job position, and years of experience) and psychological (conscientiousness, agreeableness, and neuroticism personality) factors were associated with a significant increase in depersonalization burnout from T1 to T2 (see Table 3).
In the multivariate model (Table 4), younger age (P < 0.001) and working within the intensive care (P = 0.008) or perioperative departments (P = 0.012) were the only demographic characteristics that were independently associated with change in depersonalization burnout. Lower agreeableness (P = 0.004) and higher neuroticism personality traits were also significant independent contributing factors to change in depersonalization burnout, with higher neuroticism contributing to an increase in depersonalization burnout from low to moderate levels (+3.1, 95% CI 0.80–5.40, P = 0.008).
Discussion
Under the conditions of this study, we found that the percentage of HCWs reporting high emotional exhaustion and/or depersonalization burnout increased significantly from 18.5% to 28.4% during an 11-month period of the COVID-19 pandemic. The theoretical contribution of this manuscript is that we have identified a number of factors that are associated with increased emotional exhaustion or depersonalization burnout such as unit in the hospital, function in the hospital, family status, low conscientiousness, low agreeableness and high neuroticism. While many of these predictive variables have only theoretical implications, some have contribution for the practitioners and hospital administration. For example, while one is not likely to change their role or unit in the hospital, it is the case that if hospital administration is aware of this increased risk, they can provide more resources to these personnel. Similarly, more psychological support and intervention may be especially beneficial for those who score high on neuroticism and for those who scored low conscientiousness there is a need for more support to address challenges surrounding prioritizing tasks and assertiveness.
Factors independently associated with emotional exhaustion burnout included being in a nursing or medical technician role, not having children, and low conscientiousness. The emotional exhaustion dimension of burnout reflects feeling emotionally overextended and fatigued by one’s work. Having a family may have offered additional emotional support outside of work3,16,24,48 and working in a more senior role, non-support position may have afforded more autonomy and control1,49 to protect against the emotional toll of working in a healthcare setting during the pandemic. Further, high conscientiousness, a trait that reflects a tendency to be responsible, organized, and industrious, may have been protective against feeling emotionally depleted in the context of COVID-19-related clinical care challenges. Cross-sectional studies have also shown a beneficial effect of conscientiousness on burnout,27 and current results suggest that characteristics reflective of this personality trait may have a prolonged protective effect.
Younger age, low agreeableness and high neuroticism were each independently associated with increased depersonalization burnout. Depersonalization is indicative of a more interpersonal component of burnout and reflects an impersonal response to one’s service or responsibilities and the development of a more negative or callous attitude. Study findings align with previous cross-sectional work indicating that high neuroticism and low agreeableness are associated with higher depersonalization burnout.5,27,28,48 Attributes associated with agreeableness including compassion, trust and respectfulness may have contributed to lower levels of interpersonal detachment while navigating fluctuating clinical and personal stressors during the pandemic. Neuroticism, on the other hand, is characterized by emotional instability and more intense negative affect. HCWs high on this trait may have had increased difficulty navigating exposure to uncertainty and stressors throughout the pandemic and subsequent negative emotional responses and volatility may have contributed to interpersonal challenges and detachment. Studies conducted prior to and during the COVID-19 pandemic have also reported that older age is associated with lower risk for HCW burnout more generally and have suggested that training and experience may play a role in this association.5,15 Years of experience did not remain a significant contributor to change in burnout in our study, however the association between age and depersonalization burnout may reflect related factors such as time within in the institution and/or current role, with older HCWs potentially having more seniority with regards to scheduling and more time within their departments to build interpersonal relationships.
This study identified demographic and psychological factors unique to the individual HCW (i.e., age, family, personality characteristics) as well as those pertaining to the work environment and occupational role (i.e., department, job position) that may independently contribute to changes in burnout in the context of a stressor such as a pandemic. These findings are relatively consistent with past cross-sectional studies conducted prior to and during the COVID-19 pandemic that have reported higher burnout in HCWs that do not have children and endorse less support from family, less experience, and lower conscientiousness and agreeableness.3–5,49,50 The longitudinal methodology of the current study, conducted over approximately one-year of the COVID-19 pandemic, builds on past work by providing important data on the changes in HCW burnout during the pandemic and multiple potential targets for intervention.
Interventions and workplace health promotion programs aimed at early identification as well as offering emotional support and enhancing appropriate coping skills (e.g., mindfulness) have shown promise in minimizing burnout and preventing negative long-term outcomes.51,52 Given the current results, access to these interventions may be especially important for HCWs in lower-level, support roles and those working in high acuity departments. HCW personality traits and associated characteristics can change over time and in response to training or intervention.53–55 Thus, the assessment of HCW personality, and subsequent identification of potentially protective and detrimental characteristics, may also further direct intervention efforts to mitigate burnout. For example, prioritizing access to psychological support and intervention may be especially beneficial for those who score high on neuroticism and might be prone to experience increased emotional distress when exposed to new stressors. On the other hand, low conscientiousness scores may indicate a need for more administrative and/or team support to address potential challenges surrounding prioritizing tasks and assertiveness.
The current study findings should be considered in the context of potential limitations. Data were collected from a convenience sample from four units within a single children’s hospital and the majority of the sample was White, female, nurses, and worked in the ED. Collectively, the under- or over-representation of certain groups within the sample may limit the generalizability of current study findings to other medical settings. Although time 1 burnout among study completers did not differ from those lost to follow-up, attrition from time 1 to time 2 may have implications for external validity and selection bias. Other factors not assessed, including employment status or resignation, which has accelerated during the COVID-19 pandemic52 may have also affected study attrition. We also did not collect pre-COVID-19 burnout levels nor assess safety concerns or family stressors, which may have affected burnout in our sample.
Conclusion
In a sample of pediatric HCWs, emotional exhaustion and depersonalization burnout significantly increased over 11-months of working during the COVID-19 pandemic, with the proportion of HCWs endorsing high emotional exhaustion or depersonalization burnout rising significantly. Study results demonstrated that certain demographic and psychological factors were associated with increased burnout, which may have implications for burnout mitigation strategies. Additional longitudinal research assessing HCW burnout during pandemic surges is needed to confirm the current results. Future research including more diverse HCW samples working in other units and within other institutions, as well as the assessment of additional social and institutional-level variables may help further characterize risk and protective factors associated with HCW burnout trajectory and inform the development and implementation of burnout interventions.
Author contributions
Each author has met the Pediatric Research authorship requirements. The authors that met each criterion are listed below. - Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: S.R.M., Z.N.K., T.H., M.A.F., L.S., T.S., and T.M.. -Drafting the article or revising it critically for important intellectual content: S.R.M., Z.N.K., T.H., M.A.F., L.S., T.S., and T.M. -Final approval of the version to be published: S.R.M., T.H., M.A.F., L.S., T.S., Z.N.K., and T.M.
Funding
S.R.M. is supported by the National Institutes of Health National Institute for Child Health and Human Development (K23HD105042, PI: Martin).
Data availability
The de-identified datasets analyzed during the current study are available from the corresponding author upon reasonable request.
Competing interests
Z.N.K. serves as a consultant for Edwards Lifesciences and Pacira and is the President of the American College of Perioperative Medicine. All other authors have no conflicts of interest to report.
Consent statement
Healthcare worker participants completed informed consent prior to completing study procedures.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann. Fam. Med. 2014;12:573–576. doi: 10.1370/afm.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jun J, Ojemeni MM, Kalamani R, Tong J, Crecelius ML. Relationship between nurse burnout, patient and organizational outcomes: Systematic review. Int. J. Nurs. Stud. 2021;119:103933. doi: 10.1016/j.ijnurstu.2021.103933. [DOI] [PubMed] [Google Scholar]
- 3.Kemper KJ, et al. Burnout in pediatric residents: three years of national survey data. Pediatrics. 2020;145:e20191030. doi: 10.1542/peds.2019-1030. [DOI] [PubMed] [Google Scholar]
- 4.Shanafelt TD, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch. Intern. Med. 2012;172:1377–1385. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 5.Buckley L, Berta W, Cleverley K, Medeiros C, Widger K. What is known about paediatric nurse burnout: a scoping review. Hum. Resour. Health. 2020;18:9. doi: 10.1186/s12960-020-0451-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gribben JL, MacLean SA, Pour T, Waldman ED, Weintraub AS. A cross-sectional analysis of compassion fatigue, burnout, and compassion satisfaction in pediatric emergency medicine physicians in the United States. Acad. Emerg. Med. 2019;26:732–743. doi: 10.1111/acem.13670. [DOI] [PubMed] [Google Scholar]
- 7.Patterson J, Gardner A. Burnout rates in pediatric emergency medicine physicians. Pediatr. Emerg. Care. 2020;36:192–195. doi: 10.1097/PEC.0000000000001379. [DOI] [PubMed] [Google Scholar]
- 8.Starmer AJ, Frintner MP, Freed GL. Work-life balance, burnout, and satisfaction of early career pediatricians. Pediatrics. 2016;137:e20153183. doi: 10.1542/peds.2015-3183. [DOI] [PubMed] [Google Scholar]
- 9.Maslach, C. A multidimensional theory of burnout. in Theories of organizational stress (ed. Cooper, C.) vol. 68 68–85 (Oxford University Press, 1998).
- 10.Dyrbye LN, et al. A cross-sectional study exploring the relationship between burnout, absenteeism, and job performance among American nurses. BMC Nurs. 2019;18:1–8. doi: 10.1186/s12912-019-0382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maslach, C., Jackson, S. E. & Leiter, M. P. Maslach Burnout Inventory Manual 191–205 (Consulting Psychologists Press Inc, 1996).
- 12.Montgomery AP, Patrician PA, Azuero A. Nurse Burnout Syndrome and Work Environment Impact Patient Safety Grade. J. Nurs. Care Qual. 2022;37:87–93. doi: 10.1097/NCQ.0000000000000574. [DOI] [PubMed] [Google Scholar]
- 13.Shanafelt, T. D., Dyrbye, L. N. & West, C. P. Addressing physician burnout: the way forward. JAMA 317, 901–902 (2017). [DOI] [PubMed]
- 14.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374:1714–1721. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 15.West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J. Intern. Med. 2018;283:516–529. doi: 10.1111/joim.12752. [DOI] [PubMed] [Google Scholar]
- 16.Schooley B, Hikmet N, Tarcan M, Yorgancioglu G. Comparing burnout across emergency physicians, nurses, technicians, and health information technicians working for the same organization. Med. (Baltim.) 2016;95:e2856. doi: 10.1097/MD.0000000000002856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chirico F, et al. Prevalence, risk factors and prevention of burnout syndrome among healthcare workers: an umbrella review of systematic reviews and meta-analyses. J. Health Soc. Sci. 2021;6:465–491. [Google Scholar]
- 18.CHIRICO F, et al. Workplace violence against healthcare workers during the COVID-19 pandemic: A systematic review. J. Health Soc. Sci. 2022;7:14–35. [Google Scholar]
- 19.Fiest KM, et al. Experiences and management of physician psychological symptoms during infectious disease outbreaks: a rapid review. BMC Psychiatry. 2021;21:91. doi: 10.1186/s12888-021-03090-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morgantini LA, et al. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: A rapid turnaround global survey. PloS One. 2020;15:e0238217. doi: 10.1371/journal.pone.0238217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amanullah, S. & Ramesh Shankar, R. The Impact of COVID-19 on Physician Burnout Globally: A Review. in vol. 8 421 (Multidisciplinary Digital Publishing Institute, 2020). [DOI] [PMC free article] [PubMed]
- 22.Rodriguez RM, et al. Academic Emergency Medicine Physicians’ Anxiety Levels, Stressors, and Potential Stress Mitigation Measures During the Acceleration Phase of the COVID-19 Pandemic. Acad. Emerg. Med. 2020;27:700–707. doi: 10.1111/acem.14065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kelker H, et al. Prospective study of emergency medicine provider wellness across ten academic and community hospitals during the initial surge of the COVID-19 pandemic. BMC Emerg. Med. 2021;21:1–12. doi: 10.1186/s12873-021-00425-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nguyen J, et al. Impacts and challenges of the COVID-19 pandemic on emergency medicine physicians in the United States. Am. J. Emerg. Med. 2021;48:38–47. doi: 10.1016/j.ajem.2021.03.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Firew T, et al. Protecting the front line: a cross-sectional survey analysis of the occupational factors contributing to healthcare workers’ infection and psychological distress during the COVID-19 pandemic in the USA. BMJ Open. 2020;10:e042752. doi: 10.1136/bmjopen-2020-042752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maunder RG, et al. Psychological impact of the COVID-19 pandemic on hospital workers over time: Relationship to occupational role, living with children and elders, and modifiable factors. Gen. Hosp. Psychiatry. 2021;71:88–94. doi: 10.1016/j.genhosppsych.2021.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brown PA, Slater M, Lofters A. Personality and burnout among primary care physicians: an international study. Psychol. Res. Behav. Manag. 2019;12:169–177. doi: 10.2147/PRBM.S195633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kroencke, L., Geukes, K., Utesch, T., Kuper, N. & Back, M. Neuroticism and emotional risk during the Covid-19 Pandemic. (2020). [DOI] [PMC free article] [PubMed]
- 29.Heyming, T. W. et al. Predictors for COVID-19-related new-onset maladaptive behaviours in children presenting to a paediatric emergency department. J. Paediatr. Child Health10.1111/jpc.15579 (2021). [DOI] [PMC free article] [PubMed]
- 30.Heyming TW, et al. Rapid antibody testing for SARS-CoV-2 vaccine response in pediatric healthcare workers. Int. J. Infect. Dis. 2021;113:1–6. doi: 10.1016/j.ijid.2021.09.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.John, O. P., Naumann, L. P. & Soto, C. J. Paradigm shift to the integrative Big Five trait taxonomy: History, measurement, and conceptual issues. in Handbook of personality: Theory and research (eds. John, O. P., Robins, R. W. & Pervine, L. A.) 114–158 (Guilford Press, 2008).
- 32.Soto CJ, John OP. Short and extra-short forms of the Big Five Inventory–2: The BFI-2-S and BFI-2-XS. J. Res. Personal. 2017;68:69–81. doi: 10.1016/j.jrp.2017.02.004. [DOI] [Google Scholar]
- 33.Schmitt DP, Allik J, McCrae RR, Benet-Martínez V. The geographic distribution of Big Five personality traits: Patterns and profiles of human self-description across 56 nations. J. Cross-Cult. Psychol. 2007;38:173–212. doi: 10.1177/0022022106297299. [DOI] [Google Scholar]
- 34.Spielberger, C. D. State-trait anxiety inventory for adults. (1983).
- 35.Kendall PC, Finch AJ, Jr, Auerbach SM, Hooke JF, Mikulka PJ. The State-Trait Anxiety Inventory: a systematic evaluation. J. Consult. Clin. Psychol. 1976;44:406. doi: 10.1037/0022-006X.44.3.406. [DOI] [PubMed] [Google Scholar]
- 36.LeBlanc VR, Bandiera GW. The effects of examination stress on the performance of emergency medicine residents. Med. Educ. 2007;41:556–564. doi: 10.1111/j.1365-2923.2007.02765.x. [DOI] [PubMed] [Google Scholar]
- 37.Wong ML, Anderson J, Knorr T, Joseph JW, Sanchez LD. Grit, anxiety, and stress in emergency physicians. Am. J. Emerg. Med. 2018;36:1036–1039. doi: 10.1016/j.ajem.2018.02.021. [DOI] [PubMed] [Google Scholar]
- 38.González-Cabrera J, Fernández-Prada M, Iribar-Ibabe C, Peinado JM. Acute and chronic stress increase salivary cortisol: a study in the real-life setting of a national examination undertaken by medical graduates. Stress. 2014;17:149–156. doi: 10.3109/10253890.2013.876405. [DOI] [PubMed] [Google Scholar]
- 39.Spielberger, C. D., Gorsuch, P. L. & Lushene, R. E. Manual for the State-Trait Anxiety Inventory. (Consulting Psychologist Press, 1970).
- 40.Maslach, C., Jackson, S. E., Leiter, M. P., Schaufeli, W., & Schwab, R. Maslach Burnout Inventory Manual. 13–29 (Mind Garden, 2016).
- 41.Poghosyan L, Aiken LH, Sloane DM. Factor structure of the Maslach burnout inventory: an analysis of data from large scale cross-sectional surveys of nurses from eight countries. Int. J. Nurs. Stud. 2009;46:894–902. doi: 10.1016/j.ijnurstu.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hwang C-E, Scherer RF, Ainina MF. Utilizing the Maslach Burnout Inventory in cross-cultural research. Int. J. Manag. 2003;20:3. [Google Scholar]
- 43.Greenglass ER, Burke RJ, Fiksenbaum L. Workload and burnout in nurses. J. Community Appl. Soc. Psychol. 2001;11:211–215. doi: 10.1002/casp.614. [DOI] [Google Scholar]
- 44.Maslach, C., Leiter, M. P. & Schaufeli, W. Measuring Burnout. in The Oxford Handbook of Organizational Well-being (eds. Cartwright, S. & Cooper, C. L.) (Oxford University Press, 2009).
- 45.Chirico F, Nucera G, Leiter M. Measuring burnout syndrome requires reliable and standardized measures. Hong. Kong J. Emerg. Med. 2022;29:325–326. doi: 10.1177/10249079221096920. [DOI] [Google Scholar]
- 46.Pantaleoni JL, Augustine EM, Sourkes BM, Bachrach LK. Burnout in pediatric residents over a 2-year period: a longitudinal study. Acad. Pediatr. 2014;14:167–172. doi: 10.1016/j.acap.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 47.Campbell J, Prochazka AV, Yamashita T, Gopal R. Predictors of Persistent Burnout in Internal Medicine Residents: A Prospective Cohort Study. Acad. Med. 2010;85:1630–1634. doi: 10.1097/ACM.0b013e3181f0c4e7. [DOI] [PubMed] [Google Scholar]
- 48.Geuens N, Van Bogaert P, Franck E. Vulnerability to burnout within the nursing workforce-The role of personality and interpersonal behaviour. J. Clin. Nurs. 2017;26:4622–4633. doi: 10.1111/jocn.13808. [DOI] [PubMed] [Google Scholar]
- 49.Giusti EM, et al. The psychological impact of the COVID-19 outbreak on health professionals: a cross-sectional study. Front. Psychol. 2020;11:1684. doi: 10.3389/fpsyg.2020.01684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Staples BB, et al. Burnout and Association With Resident Performance as Assessed by Pediatric Milestones: An Exploratory Study. Acad. Pediatr. 2021;21:358–365. doi: 10.1016/j.acap.2020.08.006. [DOI] [PubMed] [Google Scholar]
- 51.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388:2272–2281. doi: 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 52.Chirico, F. & Leiter, M. Tackling stress, burnout, suicide and preventing the “great resignation” phenomenon among healthcare workers (during and after the COVID-19 pandemic) for maintaining the sustainability of healthcare systems and reaching the 2030 sustainable development goals. J. Health Soc. Sci. 9–13 (2022).
- 53.Specht J, Egloff B, Schmukle SC. Stability and change of personality across the life course: the impact of age and major life events on mean-level and rank-order stability of the big five. J. Pers. Soc. Psychol. 2011;101:862–882. doi: 10.1037/a0024950. [DOI] [PubMed] [Google Scholar]
- 54.Borges, N. J. & Savickas, M. L. Personality and medical specialty choice: a literature review and integration. J of Career Assess.10, 362–380 (2002).
- 55.Spinhoven P, Huijbers MJ, Ormel J, Speckens AE. Improvement of mindfulness skills during mindfulness-based cognitive therapy predicts long-term reductions of neuroticism in persons with recurrent depression in remission. J. Affect. Disord. 2017;213:112–117. doi: 10.1016/j.jad.2017.02.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The de-identified datasets analyzed during the current study are available from the corresponding author upon reasonable request.