Abstract
Unmet need for contraception is a widely used but frequently misunderstood indicator. Although calculated from measures of pregnancy intention and current contraceptive use, unmet need is commonly used as a proxy measure for 1) lack of access to contraception and 2) desire to use it. Using data from a survey in Burkina Faso, we examine the extent to which unmet need corresponds with/diverges from these two concepts, calculating sensitivity, specificity, and positive/negative predictive values. Among women assigned conventional unmet need, 67% report no desire to use contraception, and 61% report access to a broad range of affordable contraceptives. Results show unmet need has low sensitivity and specificity in differentiating those who lack access and/or who desire to use a method from those who do not. These findings suggest that unmet need is of limited utility to inform family planning programs and may be leading stakeholders to overestimate the proportion of women in need of expanded family planning services. We conclude that more direct measures are feasible at the population level, rendering the proxy measure of unmet need unnecessary. Where access to and/or desire for contraception are the true outcomes of interest, more direct measures should be used.
Keywords: Unmet need, family planning, contraception, access, measurement, sexual and reproductive health and rights, Burkina Faso, sub-Saharan Africa
Introduction
Unfettered access to a wanted contraceptive method is a core component of contraceptive autonomy and of sexual and reproductive health and rights more broadly (L. Senderowicz 2020; Starrs et al. 2018). Within the contested world of global family planning, the importance of access is a rare spot of broad consensus (Cohen and Richards 1994). While various constituencies within the family planning community disagree on why it is so critical, these diverse groups have traditionally found common ground in the importance of easy, affordable access to a range of contraceptive methods (Reichenbach and Roseman 2011). The idea that there are individuals or couples out there who desire a contraceptive method but do not use one for reasons of geography, affordability, or other barriers to access, is a driving motivation for family planning programs to expand and improve their offerings (Prata 2007; Choi, Fabic, and Adetunji 2016). Despite the centrality of the concept of access to family planning programs and initiatives, however, reproductive health researchers have tended to measure access to contraception at the population level only indirectly. Rather than developing population-based family planning indicators to measure the availability of contraceptive methods or respondents’ desire to use them, the family planning community has instead relied on an indicator of “unmet need for contraception.”
“Unmet need for contraception” is an important indicator with a misleading name. The term “unmet need” suggests an unfilled desire to use contraception or a lack of access to a wanted method, and has been interpreted this intuitive sense by both researchers and laypeople alike (Bradley and Casterline 2014; Casterline and Sinding 2000; Westoff 1994). In practice, however, the definition of unmet need has little to do with method access or desire for methods. Instead, unmet need is a composite of two other demographic measures: current contraceptive use and 2-year pregnancy intentions among women exposed to the risk of pregnancy. According to the Demographic and Health Surveys (DHS), the technical definition of unmet need for contraception is “the percentage of women who do not want to become pregnant but are not using contraception.” The DHS cautions readers that, “Though the concept seems straightforward, the calculation is extraordinarily complex,” with leading unmet need researchers going out of their ways to clarify that “the standard [unmet need] algorithm does not include any direct measures of the desire to practice contraception or any direct measures of access to contraception” (Bradley and Casterline 2014; The DHS Program 2022). A Guttmacher Institute report from 2016 uses data from 52 countries to highlight that lack of access is not among the leading reasons for contraceptive non-use among those ascribed an unmet need by the DHS algorithm (Sedgh, Ashford, and Hussain 2016).
Despite these admonitions by technical experts, however, the unmet need for contraception indicator has long been (and continues to be) widely used in the global sexual and reproductive health field as a proxy for access to contraception and for desire to use it. Examples of ways that prominent researchers and major reproductive health organizations deploy unmet need as a proxy for lack of access abound, both within the peer-reviewed literature as well as throughout the broader global health landscape. The UNFPA website, for example, cites unmet need in the warning that “More than 200 million women still lack access to contraception” (UNFPA 2010). This call is echoed by global reproductive health organization Marie Stopes International, which claims: “Right now, there are 214 million women around the world who want to use contraception but can’t” (“Marie Stopes International Australia” 2021). The 200+ million women figure that both of these organizations mention refer to estimates of unmet need for contraception in the Global South (Sully et al. 2020).
Perhaps even more consequentially, the unmet need indicator has been a primary indicator used to measure access to reproductive health by major global development initiatives. Unmet need was, for example, one of three reproductive health indicators used by the Millennium Development Goals, where it was employed as a measure of progress toward Goal 5b: “Universal access to reproductive health” (United Nations, n.d.). More recently, the Sustainable Development Goals have used the proportion of women with need satisfied by modern methods (an offshoot of the unmet need indicator based on the same fundamental logic) as one of only two indicators to measure progress toward Goal 3.7 “universal access to sexual and reproductive health-care services” (United Nations Population Division 2022). These development goals are demonstrative of the broader ways that the global health community has relied on the unmet need indicator as a proxy for access to reproductive health services for decades.
The ubiquity of the unmet need metric in family planning belies how contested the indicator has been over the years. Indeed, the weaknesses of the unmet need indicator are well known to generations of demographers and reproductive health researchers, highlighted by both the metric’s creator as well as outside critics (Westoff 1994; Casterline and Sinding 2000; Pritchett 1996). The decades-long controversy over unmet need has recently discussed at length in Senderowicz and Maloney, 2022. This controversy includes substantial critiques to 1) how unmet need is conceptualized; 2) how unmet need is measured; and 3) how unmet need is deployed. Critiques around conceptualization include that unmet need is a status ascribed to women who may not ascribe such a need to themselves, that the “need” in unmet need does not describe a true “need” in any accepted understanding of the term, and that there are several leaps in the logic that are severely called into question by a growing body of reproductive health research (Pritchett 1996; Cleland, Harbison, and Shah 2014; Yeatman and Smith-Greenaway 2021; Huber et al. 2017). Challenges to the measurement validity of unmet need include: who should comprise the metric’s denominator; the binary measurement of pregnancy intentions (which, in reality, fall along a complex continuum); the indicator’s use of marital status as a proxy for sexual activity (assuming all married are sexually active and often excluding unmarried women); the proper way to measure/classify users of fertility awareness-based methods; and the exclusion of contraceptive users ill-served by their current methods (Bell and Bishai 2017; Rominski and Stephenson 2019; Rossier, Senderowicz, and Soura 2013; Moreau et al. 2019; Rocca et al. 2019; Rossier et al. 2013; Sawadogo 2016). Finally, challenges to the use of unmet need include a fundamental misunderstanding of what unmet need actually measures, incorrect claims that unmet need is a “rights-based” indicator, and the unsubstantiated use of unmet need as a proxy for access to contraception and/or a thwarted desire to use it (Bernstein and Edouard 2007; Potts 2000; UNFPA 2019; United Nations Population Division 2022; L. Senderowicz and Maloney 2022).
These weaknesses have led some critics to denounce the unmet need indicator as “a failure as an analytic concept” and argue for its retirement from use altogether (Pritchett 1996). Other scholars have sought to propose a series of redefinitions and modifications over the years in an effort to make the unmet need indicator more intelligible, and more in line with the intuitive understanding of the term (Bradley et al. 2012; Moreau et al. 2019; Rominski and Stephenson 2019; Bradley and Casterline 2014). The most significant of these was an official revision to the DHS definition unmet need in 2012 (Bradley et al. 2012). Though this revision helped to streamline unmet need’s measurement algorithm and survey inputs, the fundamental logic of (and measurement approach to) the unmet need indicator remained largely the same. More recently, scholars from USAID and the FP2030 initiative have issued their own calls for increased clarity and precision around the terminology and measurement of “contraceptive need” (Speizer, Bremner, and Farid 2022; Fabic 2022).
Even as the critiques of unmet need have continued to mount, the influence of this indicator in the family planning world has only grown in recent years. An array of novel indicators based on the logic of unmet need (such as SDG’s “proportion of demand satisfied by a modern method”) tweak the wording and exact calculation but leave fundamentally flawed assumptions about the nature of “demand” and “need” for contraception in place. This range of indicators based on unmet need and unsatisfied demand continue to give the impression that they measure access to contraception and/or desire to use it, while measuring only outcomes related to pregnancy intentions and current contraceptive use, not contraceptive intentions, desires, or access.
Although there has been a great deal of research from the sexual and reproductive health field calling into question the validity of unmet need, there has been very little research directly evaluating the relationship between lack of access to contraception, and the unmet need measure that is so frequently used as a proxy for it (Aiken et al. 2016; Johnson-Hanks 2002; Sedgh and Hussain 2014; Huber et al. 2017; Higgins 2017). As far back as 1995, leading family planning scholars were discovering that “the principal reasons for [contraceptive] nonuse are lack of knowledge, fear of side effects, and social and familial disapproval” as opposed to “geographic access” (Bongaarts and Bruce 1995). As family planning programs have grown and knowledge has improved in the interim 25 years, more recent studies have found that lack of knowledge and fear of social disapproval have been replaced by infrequent sex and concerns about health risks as the leading causes of contraceptive nonuse in the Global South (Sedgh and Hussain 2014).
Two important studies exploring access and unmet need were conducted by Machiyama and Cleland between 2013 and 2014, focusing on the cases of Ghana and Kenya (Machiyama and Cleland 2014, 2013). In both of these studies, the authors found that the vast majority (77% in Ghana and 84% in Kenya) of women ascribed a conventional unmet need had access to contraception. These works found that negative attitudes toward contraception and a lack of desire to use a method were substantially larger drivers of contraceptive nonuse than lack of access, with the role of attitudinal resistance growing over time, and the role of lack of access shrinking. More recently, Senderowicz and Maloney have used DHS data from seven sub-Saharan African countries to disaggregate the proportion of contraceptive nonuse due to lack of access or lack of demand among those ascribed an unmet need. That analysis found that that supply-side unmet need (lack of access to contraception) accounted for only between 9% and 22% of overall unmet need, with demand-side unmet need (lack of demand for contraception) accounting for at least 75% of unmet need in all countries (L. Senderowicz and Maloney 2022).
These previous works share DHS surveys as their common data source to measure access to contraception. Since the DHS data have no single, authoritative, direct measure of access, a few researchers have sought to develop alternative ways to quantify access using these data. Machiyama and Cleland, for example, define access to contraception in Ghana as knowledge of the two dominant methods (pills and injectables) and knowledge of a supply source of these methods. They note, however, that this measure is not ideal given that knowledge of methods may contain misinformation, restriction to only the dominant methods is not sufficient to measure overall access to family planning, and affordability and acceptability were not considered (Machiyama and Cleland 2014). Other studies have linked the same DHS question on reasons for nonuse of contraception used by Senderowicz to measures and conceptions of access (Choi, Fabic, and Adetunji 2016; Sedgh and Hussain 2014). This contraceptive nonuse question, however, gets at access to contraception only indirectly. And few (if any) population-based survey items ask respondents directly about their current contraceptive desires, despite the centrality of this question to person-centered family planning and contraceptive autonomy.
Efforts to measure access more directly have been complicated by the broad array of perspectives on what access actually means and how broadly it should be construed. Some prominent frameworks for access that have been applied to family planning programs over the years include Penchansky and Thomas’ “Five As” (availability, accessibility, accommodation, affordability, and accountability) from 1981, Bertrand et al.’s framework from 1995 (geographic, economic, administrative, cognitive, and psychosocial), as well as the 2000 AAAQ framework from the United Nations (availability, accessibility, acceptability, and quality) (Penchansky and Thomas 1981; Bertrand et al. 1995; United Nations Committee on Economic Social and Cultural Rights 2000). Each of these dimensions of access, in turn, contains an array of sub-dimensions, resulting in a complex web of factors ranging from geographic barriers to social approbation (Campbell, Sahin-Hodoglugil, and Potts 2006; Bertrand et al. 1995). Some scholars have defined lack of access to contraception broadly enough to include personal opposition to contraception as a lack of psychosocial access (Choi, Fabic, and Adetunji 2016). Others have argued that conceptualizing demand-side factors as a lack of access both paternalistically denies the agency of those who choose not to use contraception, and makes it difficult to isolate the barriers to access that can be ameliorated through health systems interventions (L. Senderowicz and Maloney 2022; Pritchett 1996).
This murkiness around the definition of access has perhaps contributed to the continued use of unmet need to indirectly assess the concept, despite the measure’s known shortcomings. Here, in an effort to recognize people’s autonomy to choose to not use contraception, we draw from the World Health Organization’s definition of access to health services as “the perceptions and experiences of people as to their ease in reaching health services or health facilities in terms of location, time, and ease of approach” (World Health Organization 2021). Our ability to measure access to a wanted contraceptive method at the population level has also been hampered by a lack of information regarding current contraceptive desires, which is equally essential for understanding unfulfilled demand for family planning services. As a result of limited this data, we know little about what proportion of those with a lack of access or desire to use contraception have an unmet need, and whether unmet need may indeed serve as a reasonable proxy measure for these concepts, in line with its intuitive understanding.
In this analysis, we measure the extent to which unmet need corresponds with or diverges from the two concepts with which it is most frequently conflated: 1) lack of access to contraception; and 2) desire to use contraception. We explore whether women of reproductive age assigned conventional unmet need would report either that they a wish to use a method or that they cannot access a broad, affordable contraceptive method mix. Using data from a survey tool piloted at two sites in Burkina Faso, we examine the extent to which conventional unmet need overlaps with desire to use contraception, access to contraception, and a joint measure of desire and access, to assess whether it may serve as a reasonable proxy for them.
Methods
Study setting and sampling
The data for the present analysis come from the cross-sectional, population-based survey of the Contraceptive Autonomy Study. Data collection took place between April and July of 2018. We carried out this survey within two Health and Demographic Surveillance Systems (HDSS) in Burkina Faso: The Ouagadougou HDSS (an urban research platform in the capital city), and the Nouna HDSS (a rural research platform in the semi-urban town of Nouna and 58 of its surrounding villages). The Ouagadougou Health and Demographic Surveillance System (Ouaga HDSS) is situated within the Institut Supérieur des Sciences de la Population, a demographic research institute within the Joseph KI-ZERBO University (formerly known as the University of Ouagadougou). The Ouaga HDSS is a research platform that was established in 2008 to study health and demographic phenomena in five neighborhoods on the northern periphery of the Burkinabè capital. Data on vital events are collected for the ~80,000 individuals within the catchment area with a periodicity of six to ten months, and special health questionnaires are also administered, though not at pre-defined intervals. Three of the neighborhoods in the HDSS are informal (zones non-loties, in Burkinabè French), without access to government services such as electricity or sanitation, while the other two neighborhoods are formally part of the city of Ouagadougou. The population of the HDSS includes a large proportion of rural-to-urban migrants, particularly in the zones non-loties, and features both in-migration and out-migration but is fairly stable.
The Nouna HDSS was established in 1992 and has been conducting research on the semi-urban town of Nouna and surrounding rural areas since. There are over 78,000 individuals followed by the platform, of which 30% come from the small administrative town of Nouna itself, with the rest coming from 58 surrounding villages. Unlike Ouagadougou, which has historically been the land of the Mossi ethnic group but has been subject to considerable in-migration of diverse ethnic groups from all parts of the country, the Nouna HDSS is home to members of the Dafing, Bwaba, Fulani and Dioula ethnic groups, with Dioula serving as the regional lingua franca. The periodicity of routine interviews in the Nouna HDSS is higher than that of the Ouaga HDSS, at 4 months. While not nationally representative, the catchment areas for these two HDSSs capture a diversity of socioeconomic and demographic characteristics, with settings ranging from formal urban neighborhoods to informal peri-urban slums to fully rural areas. A wide swath of Burkina Faso’s ethno-linguistic and religious diversity is also captured between these two research platforms. Full profiles of these two HDSSs, their periodicity, demographic makeup, and methods can be found in Sié et al. 2010 and Rossier et al. 2012.
To be eligible for inclusion, women had to be residents of the catchment areas of the Nouna or Ouaga HDSS, be of reproductive age (15–49 years-old) and be able and willing to provide informed consent in French, Dioula or Mooré. Using the most recent HDSS census (from 2017) as a sampling frame, we drew a random sample of 2700 women and 800 potential replacements in Nouna. Given lower rates of contraceptive use in Nouna, we oversampled there as we sought to generate a sample of contraceptive users that was comparable between the two sites. Of the initial sample of 2,700 women in Nouna, 17 refused to participate and 72 were not found. All 94 women were replaced from the contingency list, for a total response rate of 96.7% in Nouna.
In Ouagadougou, an initial sample of 1300 women and 700 potential replacements was drawn. An error in the sampling process initially included 811 women on our list who were “visitors” rather than “residents” in the HDSS catchment area (and thus ineligible for inclusion). Of the remaining 1189 residents on our sampling list, our interviewers were able to locate 879 of them (73.9%). Since this number fell short of our intended sample size of 1300, we drew a second random sample of 500 women from the same initial list, of whom 421 were residents of the HDSS and eligible to participate. Of these 421, we were able to locate 415 (98.6%). Of all of those we located (during both the first and second drawings), none declined to participate. Our overall response rate among eligible participants for these two drawings was 80.4%. To account for the changes in the sampling approach, we have created individual level-sampling weights based on inverse probability weighting. All analyses presented here use weighted data.
Survey and data collection
We developed and piloted a survey instrument as part of a sequential mixed methods study on contraceptive autonomy(Senderowicz 2019). We used literature reviews, expert consultations, formative qualitative research, and cognitive interviews to develop and refine the survey items and the final survey instrument. The final survey included a mix of conventional family planning questions (such as those the Demographic and Health Surveys use to measure current contraceptive use, conventional unmet need, etc.) as well as novel questions that focus on various dimensions of contraceptive autonomy. These include questions on desire to use contraception as well as self-reported access to a wide range of contraceptive methods. Data were collected via household survey from April-July of 2018, during which time interviewers visited women at their homes and administered the survey using Android-based tablets.
Analytic Approach
The analysis focuses on access and desire for contraception among nonusers, so we excluded women who reported current family planning use at the time of survey from the analytic sample. Since conventional unmet need can be ascribed to pregnant people, we included this population in our analysis as well.
The four outcome variables used in this analysis are summarized in Figure 1. The first is conventional unmet need for contraception, which we defined using the standard algorithm refined by Bradley et al. in 2012 focusing on pregnancy intentions and current contraceptive use among women at risk of pregnancy. In brief, women who reported current contraceptive use were classified as not having unmet need. Women who were pregnant or postpartum amenorrheic were categorized based on the wantedness of their current or last pregnancy; those who wanted their current/last pregnancy at that time were categorized as not having unmet need, while those who did not want their current/last pregnancy at all or wanted it later were categorized as having unmet need. Those who were infecund, determined either through self-report or through based on DHS definitions of infecundity, were categorized as not having unmet need. Finally, women who were not using contraception, not pregnant nor postpartum amenorrheic, and fecund were categorized based on their two-year pregnancy intentions; those who wanted another child within two years were categorized as not having unmet need, while those who wanted no more children or wanted children in more than two years were categorized as having unmet need. Unmet need was calculated for all participants, regardless of marital status. Unmarried people who reported the last time they had sex was more than 30 days ago were classified as not having unmet need. Frequency of sex was not used to determine unmet need for married women.
FIGURE 1.

Analytic outcomes and how they are measured
The second outcome is current desire to use contraception. We measure this as a binary variable based on the respondent’s answer to the question, “Do you wish you were using a method of contraception currently?”
The third outcome is lack of access to a broad, affordable contraceptive method mix. We measure access by asking participants to self-report if they thought either of the 14 different family planning methods mentioned in the most recent Burkina Faso DHS (oral contraceptive pill, injectable, implant, IUD, condom, calendar method, emergency contraception, lactational amenorrhea method, Standard Days method, spermicide, withdrawal, diaphragm, and sterilization) would be A) available, and B) affordable for them if they wanted that method. If the person self-reported that the method would be both available and affordable to them if they wanted it, they were considered to have access to that method. If they reported that the method would be either unavailable and/or unaffordable to them, they were considered to lack access to that method. Participants who had never heard of a given method were assumed to have that method neither available nor affordable to them.
Drawing on Festin et al.’s 2016 schema of how to categorize contraceptive methods according to various method attributes, we went on define access to a broad contraceptive method mix as self-reported access to at least one method with each of the following method attributes: duration of action, presence of hormones, coital dependence, providence dependence, male or female controlled, return to fertility, and WHO tier of effectiveness. More information on the rationale and methodology for this approach to measuring self-reported availability and affordability of contraception is elaborated in Senderowicz 2020, and a more detailed explanation of the variable derivation for this outcome can be found here in Supplemental Table 1
The fourth outcome is a combination of outcomes 2 and 3, including all respondents who both lack access to a broad, affordable contraceptive method mix and desire to use to contraception, in line with the intuitive understanding of unmet need.
We created 2×2 contingency tables and calculated sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) to assess conventional unmet need as a diagnostic tool or valid proxy for desire for family planning and access to family planning. In this context, sensitivity is the probability that a diagnostic test (the unmet need measure) can correctly identify true positives (those who truly desire contraception, lack access to contraception, and both desire and lack access to contraception). Specificity is the probability that unmet need can correctly identify true negatives (those who truly do not desire contraception, have access to contraception, or don’t desire or have access to contraception). PPV is the probability that one truly has an outcome (a true desire to use contraception, lack of access, or desire and lack of access) given that they are ascribed an unmet need. NPV is the probability one truly does not have an outcome (desire, lack of access, or desire and lack of access) given that they are not ascribed an unmet need. We use these contingency tables to explore how well these concepts map onto one another and accurately predict each other. We also summarize reasons for nonuse of family planning, overall and disaggregated by unmet need to explore whether reasons for nonuse differ between those with and those without a conventional unmet need. Finally, we summarize reasons for nonuse of family planning by desire and access to contraception.
Missing data
Data on current desire for family planning were missing for 301 contraceptive nonusers. To account for impact of these missing data on results, we ran sensitivity analyses assessing unmet need as a proxy for desire for contraception three times: 1) only including those with non-missing data on contraceptive desire, 2) including all contraceptive nonusers and classifying those with missing contraceptive desire as desiring contraception, and 3) including all contraceptive nonusers and classifying those with missing contraceptive desire as not desiring contraception. The two latter analyses allowed us to create bounds on sensitivity, specificity, and positive/negative predictive value for unmet need as a proxy for desire to use contraception without making assumptions about the distribution of underlying missing data. We present results for unmet need as a proxy for contraceptive access and affordability both including and excluding the 301 contraceptive nonusers with missing data on contraceptive desire.
Ethics Approval
This research was reviewed and approved by 1) The Institutional Review Board of the Office of Human Research Administration at the Harvard T. H. Chan School of Public Health in Boston, USA (#IRB17-0511); 2) Le Comité d’Ethique pour la recherche en santé du Ministère de la santé du Burkina Faso in Ouagadougou, Burkina Faso (#2017-5-067); and 3) Le Comité d’Ethique local du Centre de Recherche en Santé de Nouna, in Nouna Burkina Faso (#2017-01). Written informed consent was obtained for all adult participants. For minors, parental informed consent was obtained in addition to assent from the minor.
Results
A total of 3,928 women were enrolled in the Contraceptive Autonomy Study. In the total sample, 26% reported modern contraceptive use and 22% had DHS-defined unmet need for family planning, both of which are comparable to findings from the Performance for Monitoring Action survey in Burkina Faso, which showed an mCPR of 28% and an unmet of 16.8% nationally in 2017 (PMA2020 2018). 1,210 contraceptive users (31%) and 301 women (8%) with missing data on desire for contraception were excluded. Our final analytic sample of contraceptive nonusers included 851 women from the Ouaga HDSS, 1566 women from the Nouna HDSS, and 2417 women overall. We show the sociodemographic characteristics of these contraceptive nonusers in Table 1. Most were married (60%) and nearly half (49%) had no formal education, with women in Ouagadougou more likely to have some formal education compared to women in Nouna. We also present the woman’s mode of transportation in Table 1, as this is often used as a proxy for household wealth in the Burkinabè context, with a more expensive mode of transport associated with higher levels of economic prosperity (Moran et al., 2006). Most participants from Nouna traveled by foot (25%) or bicycle (69%) as their primary mode of transportation, whereas 68% of participants from Ouagadougou traveled by motorbike, indicating a higher average material standard of living for those from the urban site. Just over one third (35%) of our sample of family planning nonusers had a conventional unmet need for family planning as defined by the DHS, with unmet need slightly higher (37%) in the rural area compared to the urban area (33%). Under half (43%) of the sample lacked access to a broad range of contraceptives and 17% reported a desire to use contraception, with more women in Nouna reporting desire (21%) compared to Ouagadougou (11%). Seven percent of women reported both a lack of access to contraceptive and a desire to use it.
TABLE 1.
Select demographic characteristics of 2,417 contraceptive nonusers in Ouagadougou and Nouna, Burkina Faso, 2018
| Ouagadougou n=851 |
Nouna n=1,566 |
Overall n=2,417 |
||||
|---|---|---|---|---|---|---|
| median | [IQR] | median | [IQR] | median | [IQR] | |
| Age | 28 | [20, 37] | 25 | [18, 35] | 26 | [19, 36] |
| n | % | n | % | n | % | |
| Married | 515 | 61 | 938 | 60 | 1,452 | 60 |
| Education | ||||||
| None | 324 | 38 | 872 | 56 | 1,196 | 49 |
| At least some primary school | 198 | 23 | 354 | 23 | 552 | 23 |
| At least some secondary school | 300 | 35 | 339 | 22 | 639 | 26 |
| Missing | 29 | 3 | 1 | 0 | 30 | 1 |
| Primary mode of transport | ||||||
| Foot or other | 70 | 8 | 392 | 25 | 462 | 19 |
| Bicycle | 121 | 14 | 1,081 | 69 | 1,202 | 50 |
| Motorcycle | 582 | 68 | 93 | 6 | 675 | 28 |
| Car | 78 | 9 | 0 | 0 | 78 | 3 |
| Unmet need (conventional) | 278 | 33 | 572 | 37 | 850 | 35 |
| Lack access to contraception | 422 | 50 | 743 | 40 | 1,165 | 43 |
| Desire to use contraception | 90 | 11 | 332 | 21 | 422 | 17 |
| Desire to use contraception and lack access | 37 | 4 | 137 | 9 | 174 | 7 |
In Figure 2, we present results on the desire to use contraception, and self-reported access to a range of family planning methods among those with conventional unmet need. In the pooled analysis, 33% of participants who are classified as having unmet need according to the DHS definition indicated that they wished they were using a method of contraception at the time of interview. The remaining 68% of those with an unmet need reported not wanting to use a contraceptive method. More than a quarter (27%) of respondents with an unmet need reported a lack of access to wide range of contraceptive methods, and 38% reported that they would not be able to afford a wide range of methods. These proportions were considerably higher for all three outcomes among women from the (rural) Nouna HDSS, compared to the (urban) Ouagadougou HDSS.
FIGURE 2.
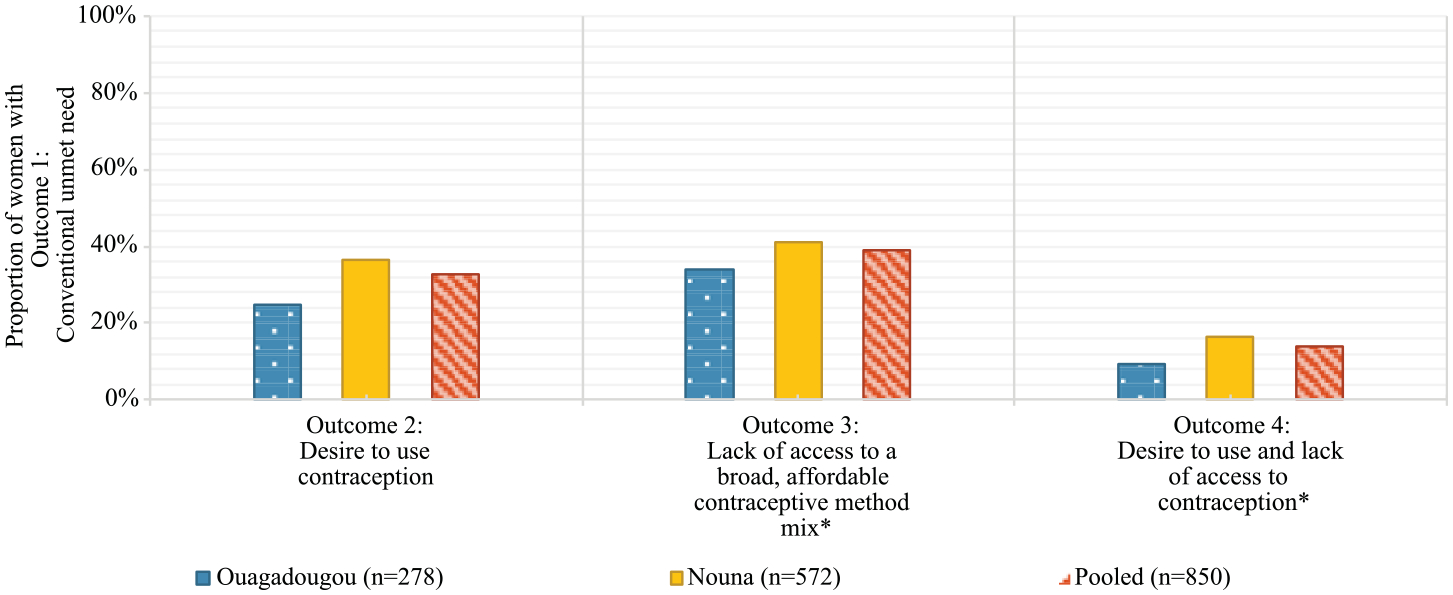
Proportion of women with a desire to use and/or a lack of access to contraception among those with conventional unmet need in a sample of 2,417 contraceptive users in Burkina Faso, 2018
* Method attribute groups included: long-acting, short-acting, hormonal, non-hormonal, coitally dependent, coitally independent, provider dependent, provider independent, male controlled, female controlled, immediate return to fertility, and tier 1 (as per Family Planning, Global Handbook for providers, 2011).
Table 2 shows a contingency table comparing unmet need by conventional measure for family planning with desire to use a method. The PPV of unmet need to capture those who desire to use contraception is 33%, indicating that less than one-third those with unmet need by conventional measure expressed a desired to use contraception. PPV ranged from 27% (when classifying those with missing contraceptive desire as not desiring contraception) to 45% (when classifying them as desiring contraception) (Supplemental Tables 2 and 3). The sensitivity of conventional unmet need to capture those who wish to be using a contraceptive method is 65.5% (bounds when reclassifying missing desire: 65–66%), while 35% those who wish to use contraception were classified as not having an unmet need. The specificity of unmet need to capture desire to use contraception is 71% (bounds: 67–71%), while 29% of those who had no desire for family planning were classified as having unmet need by conventional measure.
TABLE 2.
Testing the validity of conventional unmet need against self-reported desire to use contraception (Outcome 2), in a sample of 2,417 contraceptive nonusers in Burkina Faso, 2018
| Wish to use method | ||||
|---|---|---|---|---|
| Yes n (row %) |
No n (row %) |
Total n |
||
| Unmet need | Yes | 277 (32.6%) | 573 (67.4%) | 850 |
| No | 146 (9.3%) | 1,421 (90.7%) | 1,567 | |
| Total | 423 (17.5%) | 1,994 (82.5%) | 2,417 | |
Table 3 compares DHS-defined unmet need for family planning with access to a broad range of contraceptive methods. The PPV for unmet need to capture those who lack access is 39% (40% including those with missing contraceptive desire; Supplemental Table 4), indicating that less than half of those with conventional unmet need report a lack of access to a broad range of affordable contraceptive methods. The sensitivity of conventional unmet need to capture those who lack access to a contraceptive method is 32% (36% including those with missing contraceptive desire), while 68% of those who lack access to affordable contraception were classified as not having an unmet need by conventional measure. The specificity of unmet need to capture access to affordable contraception is 63% (60% including those with missing contraceptive desire), while 38% of nonusers who reported access to affordable contraception were classified as having unmet need by conventional measure.
TABLE 3.
Testing the validity of conventional unmet need against self-reported lack of access to a broad contraceptive method mix (Outcome 3), in a sample of 2,417 contraceptive nonusers in Burkina Faso, 2018
| Lack access to a broad, affordable contraceptive method mix* | ||||
|---|---|---|---|---|
| Yes n (row %) |
No n (row %) |
Total n |
||
| Unmet need | Yes | 332 (39.1%) | 518 (60.9%) | 850 |
| No | 703 (44.9%) | 864 (55.1%) | 1,567 | |
| Total | 1,035 (42.8%) | 1,382 (57.2%) | 2,417 | |
Could not access or afford a method from each of the following groups: long-acting, short-acting, hormonal, non-hormonal, coitally dependent, coitally independent, provider dependent, provider independent, male controlled, female controlled, immediate return to fertility, and tier 1 (as per Family Planning, Global Handbook for providers, 2011).
Table 4 compares DHS-defined unmet need for family planning with an indicator for desire to use family planning and lack of access to a range of methods. The PPV for unmet need to capture those who desire contraception but lack access to it is 14%, demonstrating that few women with conventional unmet need have both the desire to use contraception and lack access. The sensitivity of unmet need to capture those who wish to be using a contraceptive method but do not have access is 68%, while 32% of those who wish to use contraception and lack access were classified as not having an unmet need. The specificity of unmet need to capture desire to use contraception is 67%, while 33% of nonusers who had no desire for family planning were classified as having unmet need.
TABLE 4.
Testing the validity of conventional unmet need against combined 1) self-reported desire to use contraception and 2) lack of access to contraception (Outcome 4), in a sample of 2,417 contraceptive nonusers in Burkina Faso, 2018
| Have desire to use family planning but no access to a broad, affordable contraceptive method mix* | ||||
|---|---|---|---|---|
| Yes n (row %) |
No n (row %) |
Total n |
||
| Unmet need | Yes | 119 (14.0%) | 731 (86.0%) | 850 |
| No | 55 (3.5%) | 1,512 (96.5%) | 1,567 | |
| Total | 174 (7.2%) | 2,243 (92.8%) | 2,417 | |
Has desire to use family planning but could not access or afford a method from each of the following groups: long-acting, short-acting, hormonal, non-hormonal, coitally dependent, coitally independent, provider dependent, provider independent, male controlled, female controlled, immediate return to fertility, and tier 1 (as per Family Planning, Global Handbook for providers, 2011).
Reported primary reasons for contraceptive nonuse stratified by conventional unmet need are shown in Table 5. A similar proportion of women with and without conventional unmet need report lack of desire as their primary reason for contraceptive non-use (56% vs. 55%, p=0.8). About 27% of participants without conventional unmet need reported their primary reason for nonuse was lack of sexual activity, compared to 3% of participants with unmet need (p<0.01). A similar proportion of participants with and without unmet need reported nonuse because they did not think they were fertile (7% vs. 6%, p=0.3). A higher proportion of participants with unmet need reported a partner or family member not allowing them to use contraception as their primary reasons for nonuse compared to people without unmet need (8% vs. 2%, p<0.01). Additionally, a higher proportion of participants with unmet need reported fear of side effects compared to participants without unmet need (3% vs. 2%, p<0.01). In terms of access, only 0.1% of nonusers said they did not know where to get family planning and 3% reported they could not afford a method. One percent of nonusers reported that they did not have enough information to decide about family planning. We summarize reasons for nonuse by desire and access to family planning in Supplementary Table 5.
Table 5.
Primary reasons for nonuse of family planning among contraceptive nonusers, by unmet need status
| No unmet need n=1,567 |
Unmet need n=850 |
Overall n=2,417 |
p-value | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Does not want to use family planning | 873 | 55.7 | 469 | 55.2 | 1,342 | 55.5 | 0.8 |
| Is currently pregnant | 21 | 1.3 | 76 | 8.9 | 97 | 4.0 | <0.01 |
| Provider refused | 1 | 0.0 | 6 | 0.7 | 7 | 0.3 | <0.01 |
| Partner or family member will not allow | 37 | 2.4 | 66 | 7.8 | 103 | 4.3 | <0.01 |
| Does not know where to get family planning | 2 | 0.1 | 0 | 0.0 | 2 | 0.1 | 0.5 |
| Cannot afford family planning | 8 | 0.5 | 28 | 3.3 | 36 | 1.5 | <0.01 |
| Does not think they are fertile | 89 | 5.7 | 57 | 6.7 | 146 | 6.0 | 0.3 |
| Cannot get to the clinic | 1 | 0.0 | 3 | 0.4 | 4 | 0.2 | 0.1 |
| Not sexually active | 422 | 26.9 | 23 | 2.7 | 445 | 18.4 | <0.01 |
| Health reason for nonuse | 20 | 1.3 | 12 | 1.4 | 32 | 1.3 | 0.8 |
| Not married | 19 | 1.2 | 7 | 0.8 | 26 | 1.1 | 0.4 |
| Afraid of side effects | 24 | 1.5 | 39 | 4.6 | 63 | 2.6 | <0.01 |
| Does not have enough information | 8 | 0.5 | 11 | 1.3 | 19 | 0.8 | 0.04 |
| Other | 42 | 2.7 | 53 | 6.2 | 95 | 3.9 | <0.01 |
Discussion
Two thirds of women assigned a conventional unmet need reported no desire to use contraception, while 61% of those assigned an unmet need report access to a broad range of affordable contraceptive methods. These findings, accompanied by the low sensitivity and specificity of unmet need in differentiating those who lack access and those who desire to use a method from those who do not, suggest that the unmet need metric may be misleading donors, researchers, and family planning program implementers into overestimating the unfulfilled demand for a method among contraceptive nonusers. Positive predictive value is the metric that most aligns with the misinterpretation of the unmet need indicator and was the lowest performing for measuring access and desire to use contraception, further highlighting that unmet need is not an appropriate proxy for these concepts. Put simply, many of the women to who researchers ascribe an unmet need do not wish to be using a contraceptive method.
When reporting on their primary reason for contraceptive nonuse, among those women ascribed traditional unmet need, very few reported insufficient information or inability to afford contraception, while large numbers reported their primary reason for nonuse was that they simply did not wish to use a method, further confirming the results of our contingency tables. While information and access (both geographic and financial) were not frequently reported as the primary reason for nonuse, collecting data on additional or secondary reasons may be informative for family planning programs designed to address all barriers. It is both vital to respect people’s autonomy to choose contraceptive nonuse, as well as to probe into the underlying barriers that may be conditioning this preference.
We find that, though access to a broad range of affordable contraceptive methods is common among the women in this sample, there are differences between women from the urban and rural research sites that deserve attention. Over 40% of respondents from the Nouna HDSS reported that affordability could present a barrier to accessing a broad contraceptive method mix for them, compared to approximately 33% in the capital city. Levels of unmet need for contraception, as conventionally measured, also varied slightly between the sites (37% in Nouna vs. 33% in Ouagadougou). Seventeen percent of all contraceptive nonusers reported a current desire to use contraception, which may indicate a real need for improved services among those who wish to contracept but are not doing do. A better understanding of what the barriers to use are among that group is an important next step for this research.
This study is subject to some important limitations. Notably, the construct of “access” in family planning (and in health services more broadly) is contested, without a single, universally agreed upon definition. The approach we use to measuring access to a broad contraceptive method mix here is a new one, and one that has not been subject to formal psychometric validation techniques. While relying on respondent perceptions of availability and affordability allows our measure to be more patient-centered, it also complicates the measure of access, allowing it to be conditioned on respondents’ knowledge of method availability and affordability, rather than some objective third party assessment of those factors. The implications of this distinction for family planning initiatives are important, especially given the literature demonstrating that fertility and contraceptive desires are not static over the reproductive life course, but instead are dynamic in response both to changing life conditions as well as the quality of contraceptive services available (Zimmerman et al. 2021; Agadjanian 2005; Kodzi, Casterline, and Aglobitse 2010; Downey et al. 2017). Additionally, many of the known limitations of the unmet need indicator also apply to the measurement of unmet need for the purposes of this analysis. For example, prior evidence from Ghana and from Burkina Faso shows that many women ascribed an unmet need by the DHS algorithm, are actually miscategorized users of traditional methods of contraception (Rossier, Senderowicz, and Soura 2013; Staveteig 2017).
We demonstrate here that it is feasible and practical to measure lack of access and desire to use contraception directly at the population level, obviating the need for a proxy measure to begin with. We use a novel indicator of access to family planning, measuring directly whether women can access and afford 14 contraceptive methods in various attribute groups, rather than inferring access based on a series of indirect questions. We also ask women about their desire to use contraception and trust their answers, rather than assuming desire based on a combination of pregnancy intentions and contraceptive uptake. Adding the desire to use measure to existing surveys would add just one additional question to questionnaires, while measuring access to a broad contraceptive method mix would add to survey burden a bit more, requiring two questions (“Do you think [method x] would be available to you if you wanted it?” and “Do you think [method x] would be affordable to you if you wanted it?”) be added for each contraceptive method.
Additional research in a range of contexts with diverse family planning landscapes would help to further understand dynamics of access, desire to use, and unmet need, and to further refine the measurement approach going forward. Such refinement might include asking method-specific questions about contraceptive desire and examining who has access to the specific method(s) they desire, rather than measuring desire for contraception overall. Future work exploring desire for and access to contraception and specific contraceptive methods among current users of family planning would help provide a fuller picture of desire and access among all people at risk of getting pregnant.
Making changes to legacy indicators, such as unmet need, is always fraught, due to data inertia and the desirability of measurement consistency to help track trends over time (Merry 2016). Yet given how common and significant the misinterpretation of the unmet need indicator is, and how important the concept of access is for motivating family planning programs, it is clear that direct population-based measures of access and desire to use contraception would help guide person-centered contraceptive policy and programming.
Conclusion
As the orientation of the family planning community has pivoted from concerns about fertility control to concerns about reproductive rights and health, the field’s measures have not always kept pace with this change (Senderowicz 2020). It is essential for family planning researchers to continually reevaluate the usefulness of inherited tools, given the changing priorities of our measurement agenda. This study shows that, by failing to distinguish between those who lack access to a wanted contraceptive method and those content with their decision not to use contraception, unmet need is of limited utility for reproductive health scholars and decision-makers interested in understanding rights-based or person-centered family planning outcomes.
A reliance on the unmet need metric as a proxy for access is likely leading the global health community to substantially overestimate the proportion of women who cannot access a wanted contraceptive method. Further, this reliance on unmet need contravenes the principles of contraceptive autonomy and reproductive justice, which affirm the primacy of each individual’s expertise about their reproductive lives and decisions. Rather than assigning an unmet need to a person based on a researcher-perceived conflict between their pregnancy intentions and contraceptive use patterns, we might simply ask people about their contraceptive desires and barriers to access, and then base our programs on meeting people’s self-professed needs and goals. By asking women directly and trusting their answers, we can begin to develop a wave of contraceptive programs founded and evaluated on the basis of contraceptive autonomy and reproductive justice.
Supplementary Material
Funding:
This work was supported by The David and Lucile Packard Foundation under grant #2016-64774 and the Society of Family Planning Research Fund under grant #11-13.
LS’s contribution was supported by a Ruth L Kirschstein National Research Service Award (T32 HD049302) and Population Research Infrastructure grant (P2C HD047873). BB’s contribution was supported by a National Research Service Award (T32HD52468) and a Population Infrastructure grant (P2CHD050924). The Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health (NIH) awarded these grants. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the NIH/NICHD. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Footnotes
Conflict of Interest:
The authors have no conflicts of interest to report
Data availability:
The data that support the findings of this study are not openly available due to the terms of our ethics approval. Data may be made available by the corresponding author on a case-by-case basis upon reasonable request and ethical clearance.
References
- Agadjanian Victor. 2005. “Fraught with Ambivalence: Reproductive Intentions and Contraceptive Choices in a Sub-Saharan Fertility Transition.” Population Research and Policy Review 24 (6): 617–45. [Google Scholar]
- Aiken Abigail R.A., Borrero Sonya, Callegari Lisa S., and Dehlendorf Christine. 2016. “Rethinking the Pregnancy Planning Paradigm: Unintended Conceptions or Unrepresentative Concepts?” Perspectives on Sexual and Reproductive Health 48 (3): 147–51. 10.1363/48e10316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell Suzanne O., and Bishai David. 2017. “Unmet Need and Sex: Investigating the Role of Coital Frequency in Fertility Control.” Studies in Family Planning 48 (1): 39–53. 10.1111/sifp.12012. [DOI] [PubMed] [Google Scholar]
- Bernstein Stan, and Edouard Lindsay. 2007. Targeting Access to Reproductive Health: Giving Contraception More Prominence and Using Indicators to Monitor Progress. Reproductive Health Matters. Vol. 15. Elsevier BV. 10.1016/S0968-8080(07)29284-5. [DOI] [PubMed] [Google Scholar]
- Bertrand Jane T, Hardee Karen, Magnani Robert J, and Angle Marcia A. 1995. “Access, Quality Of Care and Medical Barriers In Family Planning Programs.” International Family Planning Perspectives 21 (2). 10.2307/2133525. [DOI] [Google Scholar]
- Bongaarts John, and Bruce Judith. 1995. “The Causes of Unmet Need for Contraception and the Social Content of Services.” Studies in Family Planning, 57–75. [PubMed] [Google Scholar]
- Bradley Sarah, and Casterline John. 2014. “Understanding Unmet Need: History, Theory, and Measurement.” Studies in Family Planning 45 (2): 123–50. 10.1111/j.1728-4465.2014.00381.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley Sarah, Croft Trevor, Fishel Joy, and Westoff Charles. 2012. “Revising Unmet Need For Family Planning.” http://dhsprogram.com/pubs/pdf/AS25/AS25[12June2012].pdf.
- Campbell Martha, Sahin-Hodoglugil Nuriye Nalan, and Potts Malcolm. 2006. “Barriers to Fertility Regulation: A Review of the Literature.” Studies in Family Planning 37 (2): 87–98. http://www.ncbi.nlm.nih.gov/pubmed/16832983. [DOI] [PubMed] [Google Scholar]
- Casterline John, and Sinding Steven. 2000. “Unmet Need for Family Planning in Developing Countries and Implications for Population Policy.” Population and Development Review 26 (4): 691–723. [Google Scholar]
- Choi Yoonjoung, Fabic Madeleine Short, and Adetunji Jacob. 2016. “Measuring Access to Family Planning: Conceptual Frameworks and DHS Data.” Studies in Family Planning 47 (2). 10.1111/j.1728-4465.2016.00059.x. [DOI] [PubMed] [Google Scholar]
- Cleland John, Harbison Sarah, and Shah Iqbal H. 2014. “Unmet Need for Contraception: Issues and Challenges.” Studies in Family Planning 45 (2): 105–22. 10.1111/j.1728-4465.2014.00380.x. [DOI] [PubMed] [Google Scholar]
- Cohen Susan A, and Richards Cory L. 1994. “The Cairo Consensus: Population, Development and Women.” Family Planning Perspectives 26 (6): 272–77. [PubMed] [Google Scholar]
- Downey Margaret Mary, Arteaga Stephanie, Villaseñor Elodia, and Gomez Anu Manchikanti. 2017. “More Than a Destination: Contraceptive Decision Making as a Journey.” Women’s Health Issues 27 (5): 539–45. 10.1016/j.whi.2017.03.004. [DOI] [PubMed] [Google Scholar]
- Fabic Madeleine Short. 2022. “What Do We Demand? Responding to the Call for Precision and Definitional Agreement in Family Planning’s ‘Demand’ and ‘Need’ Jargon.” Global Health: Science and Practice 10 (1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins Jenny A. 2017. “Pregnancy Ambivalence and Long-Acting Reversible Contraceptive (LARC) Use Among Young Adult Women: A Qualitative Study.” Perspectives on Sexual and Reproductive Health 49 (3): 149–56. 10.1363/psrh.12025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber Sarah, Esber Allahna, Garver Sarah, Banda Venson, and Norris Alison. 2017. “The Relationship Between Ambivalent and Indifferent Pregnancy Desires and Contraceptive Use Among Malawian Women.” International Perspectives on Sexual and Reproductive Health 43 (1): 13–19. 10.1363/43e3417. [DOI] [PubMed] [Google Scholar]
- Johnson-Hanks Jennifer. 2002. “On the Modernity of Traditional Contraception: Time and the Social Context of Fertility.” Population and Development Review 28 (2): 229–49. 10.1111/j.1728-4457.2002.00229.x. [DOI] [Google Scholar]
- Kodzi Ivy, Casterline John, and Aglobitse Peter. 2010. “The Time Dynamics of Individual Fertility Preferences among Rural Ghanaian Women.” Studies in Family Planning 41 (1): 45–54. http://www.ncbi.nlm.nih.gov/pubmed/21465721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machiyama Kazuyo, and Cleland John. 2013. “Insights into Unmet Need in Kenya.” London. https://knowledgecommons.popcouncil.org/departments_sbsr-rh/280/. [Google Scholar]
- ———. 2014. “Unmet Need for Family Planning in Ghana: The Shifting Contributions of Lack of Access and Attitudinal Resistance.” Studies in Family Planning 45 (2): 203–26. 10.1111/j.1728-4465.2014.00385.x. [DOI] [PubMed] [Google Scholar]
- “Marie Stopes International Australia.” 2021. 2021. https://www.mariestopesinternational.org.au/.
- Merry Sally Engle. 2016. The Seductions of Quantification : Measuring Human Rights, Gender Violence, and Sex Trafficking. Chicago: University of Chicago Press. [Google Scholar]
- Moran Allisyn C, Sangli Gabriel, Dineen Rebecca, Rawlins Barbara, Yaméogo Mathias, and Baya Banza. 2006. “Birth-Preparedness for Maternal Health: Findings from Koupéla District, Burkina Faso.” Journal of Health, Population, and Nutrition 24 (4): 489. [PMC free article] [PubMed] [Google Scholar]
- Moreau Caroline, Shankar Mridula, Helleringer Stephane, and Becker Stanley. 2019. “Measuring Unmet Need for Contraception as a Point Prevalence.” BMJ Global Health 4 (4): 1–12. 10.1136/bmjgh-2019-001581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penchansky Roy, and Thomas J William. 1981. “The Concept of Access: Definition and Relationship to Consumer Satisfaction.” Medical Care 19 (2): 127–40. 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- PMA2020. 2018. “BURKINA FASO ROUND 6 INDICATORS.” https://www.pmadata.org/sites/default/files/data_product_results/PMA2020-Burkina-R6-FP-Brief-EN.pdf.
- Potts Malcolm. 2000. “The Unmet Need for Family Planning.” Scientific American 282 (1): 88–93. [Google Scholar]
- Prata Ndola. 2007. “The Need for Family Planning.” Population and Environment 28 (4): 212–22. [Google Scholar]
- Pritchett Lant. 1996. “No Need for Unmet Need.” https://sites.hks.harvard.edu/fs/lpritch/Population-docs/noneedforunmetneed_hopkins.pdf.
- Reichenbach Laura, and Roseman Mindy. 2011. Reproductive Health and Human Rights: The Way Forward. Philadelphia: University of Pennsylvania Press. [Google Scholar]
- Rocca Corinne H., Ralph Lauren J., Wilson Mark, Gould Heather, and Foster Diana G.. 2019. “Psychometric Evaluation of an Instrument to Measure Prospective Pregnancy Preferences: The Desire to Avoid Pregnancy Scale.” Medical Care 57 (2): 1. 10.1097/MLR.0000000000001048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rominski Sarah D, and Stephenson Rob. 2019. “Toward a New Definition of Unmet Need for Contraception.” Studies in Family Planning 50 (2): 195–98. [DOI] [PubMed] [Google Scholar]
- Rossier Clémentine, Sawadogo Nathalie, Soubeiga André, and Aproberts Lucy Tr. 2013. “Premarital Sexuality, Gender Relations and Unplanned Pregnancies in Ouagadougou.” Population, English Edition 68 (1): 89–113. [Google Scholar]
- Rossier Clémentine, Senderowicz Leigh, and Soura Abdramane. 2013. “Do Natural Methods Count? Underreporting of Natural Contraception in Urban Burkina Faso.” In Is Access Enough? Understanding and Addressing Unmet Need in Family Planning, 45:171–82. Nanyuki, Kenya. 10.1111/j.1728-4465.2014.00383.x. [DOI] [PubMed] [Google Scholar]
- Sawadogo Nathalie. 2016. “De l’initiation Sexuelle Au Mariage Chez Les Jeunes Urbains Burkinabè: Relations, Vécu et Risques.” Louvain-La-Neuve, Presses Universitaires de Louvain. [Google Scholar]
- Sedgh Gilda, Ashford Lori S, and Hussain Rubina. 2016. “Unmet Need for Contraception in Developing Countries: Examining Women’s Reasons for Not Using a Method.” https://www.guttmacher.org/report/unmet-need-for-contraception-in-developing-countries.
- Sedgh Gilda, and Hussain Rubina. 2014. “Reasons for Contraceptive Nonuse among Women Having Unmet Need for Contraception in Developing Countries.” Studies in Family Planning 45 (2): 151–69. 10.1111/j.1728-4465.2014.00382.x. [DOI] [PubMed] [Google Scholar]
- Senderowicz Leigh. 2020. “Contraceptive Autonomy: Conceptions and Measurement of a Novel Family Planning Indicator.” Studies in Family Planning 51 (2). 10.1111/sifp.12114. [DOI] [PubMed] [Google Scholar]
- Senderowicz Leigh Gabrielle. 2019. “Conceptions and Measurement of Contraceptive Autonomy.” Harvard T.H. Chan School of Public Health. http://nrs.harvard.edu/urn-3:HUL.InstRepos:40976626. [Google Scholar]
- Senderowicz Leigh, and Maloney Nicole. 2022. “Supply-Side Versus Demand-Side Unmet Need: Implications for Family Planning Programs.” Population and Development Review Forthcomin. 10.1111/padr.12478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speizer Ilene S, Bremner Jason, and Farid Shiza. 2022. “Language and Measurement of Contraceptive Need and Making These Indicators More Meaningful for Measuring Fertility Intentions of Women and Girls.” Global Health: Science and Practice 10 (1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starrs Ann M, Ezeh Alex C, Barker Gary, Basu Alaka, Bertrand Jane T, Blum Robert, Coll-Seck Awa M, et al. 2018. “Accelerate Progress-Sexual and Reproductive Health and Rights for All: Report of the Guttmacher-Lancet Commission.” Lancet 391 (10140): 2642–92. 10.1016/S0140-6736(18)30293-9. [DOI] [PubMed] [Google Scholar]
- Staveteig Sarah. 2017. “Fear, Opposition, Ambivalence, and Omission: Results from a Follow-up Study on Unmet Need for Family Planning in Ghana.” PloS One 12 (7): e0182076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sully Elizabeth, Biddlecom Ann, Darroch Jacqueline, Riley Taylor, Ashford Lori, Naomi Lince-Deroche, Firestein Lauren, and Murro Rachel. 2020. “Adding It Up: Investing in Sexual and Reproductive Health 2019.” New York. https://www.guttmacher.org/report/adding-it-up-investing-in-sexual-reproductive-health-2019. [Google Scholar]
- The DHS Program. 2022. “Unmet Need for Family Planning.” 2022. https://dhsprogram.com/topics/unmet-need.cfm.
- UNFPA. 2010. “Fifty Years after the Pill, More than 200 Million Women Still Lack Access to Contraception | UNFPA - United Nations Population Fund.” 2010. https://www.unfpa.org/news/fifty-years-after-pill-more-200-million-women-still-lack-access-contraception.
- ———. 2019. “One Vision Three Zeros.” UNFPA Annual Report. 2019. https://esaro.unfpa.org/en/publications/one-vision-three-zeros.
- United Nations. n.d. “Millenium Development Goals: Goal 5.” https://www.un.org/millenniumgoals/maternal.shtml.
- United Nations Committee on Economic Social and Cultural Rights. 2000. “The Right to the Highest Attainable Standard of Health (Article 12 of the International Covenant on Economic, Social and Cultural Rights).” Geneva. https://digitallibrary.un.org/record/425041?ln=en. [Google Scholar]
- United Nations Population Division. 2022. “SDG Indicator 3.7.1 on Contraceptive Use.” 2022. https://www.un.org/development/desa/pd/data/sdg-indicator-371-contraceptive-use.
- Westoff CF. 1994. “The Concept of Unmet Need.” Planned Parenthood Challenges, no. 1: 5–8. http://www.ncbi.nlm.nih.gov/pubmed/12345744. [PubMed] [Google Scholar]
- World Health Organization. 2021. WHO Guideline on Health Workforce Development, Attraction, Recruitment and Retention in Rural and Remote Areas. Geneva: World Health Organization. https://www.who.int/publications/i/item/9789240024229. [PubMed] [Google Scholar]
- Yeatman Sara, and Smith-Greenaway Emily. 2021. “Women’s Health Decline Following (Some) Unintended Births: A Prospective Study.” Demographic Research 45: 547–76. 10.4054/DemRes.2021.45.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman Linnea A, Sarnak Dana O, Karp Celia, Wood Shannon N, Moreau Caroline, Kibira Simon P S, and Makumbi Fredrick. 2021. “Family Planning Beliefs and Their Association with Contraceptive Use Dynamics: Results from a Longitudinal Study in Uganda.” Studies in Family Planning 52 (3): 241–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are not openly available due to the terms of our ethics approval. Data may be made available by the corresponding author on a case-by-case basis upon reasonable request and ethical clearance.


