Abstract
Background
People with opioid use disorder (OUD) are overrepresented in US correctional facilities and experience disproportionately high risk for overdose after release. Medications for OUD (MOUD) are highly efficacious but not available to most incarcerated individuals. In 2018, Vermont began providing MOUD for all incarcerated individuals with OUD statewide. In 2020, the COVID-19 state of emergency began. We assessed the impact of both events on MOUD utilization and treatment outcomes.
Methodology
Analyses linked Vermont Department of Corrections administrative data and Medicaid claims data between 07/01/2017 and 03/31/2021. The study used logistic regression to analyze treatment engagement among all incarcerated individuals in Vermont. Multilevel modeling assessed change in clinical outcomes among release episodes that occurred among individuals with an OUD diagnosis Medicaid claim.
Results
Prescriptions for MOUD while incarcerated increased from 0.8% to 33.9% of the incarcerated population after MOUD implementation (OR = 67.4) and subsequently decreased with the onset of COVID-19 to 26.6% (OR = 0.7). After MOUD implementation, most prescriptions (63.1%) were to individuals who had not been receiving MOUD prior to incarceration, but this figure decreased to 53.9% with the onset of COVID-19 (OR = 0.7). Prescriptions for MOUD within 30 days after release increased from 33.9% of those with OUD before to 41.0% after MOUD implementation (OR = 1.4) but decreased to 35.6% with the onset of COVID-19 (OR = 0.8). Simultaneously, opioid-related nonfatal overdoses within 30 days after release decreased from 1.2% before to 0.8% after statewide MOUD implementation (OR = 0.3) but increased to 1.9% during COVID-19 (OR = 3.4). Fatal overdoses within 1 year after release decreased from 27 deaths before to ≤10 after statewide MOUD implementation and remained ≤10 during COVID-19.
Conclusions
This longitudinal evaluation demonstrated increased treatment engagement and a decrease in opioid-related overdose following implementation of MOUD in a statewide correctional system. In contrast, these improvements were somewhat attenuated with the onset of COVID-19, which was associated with decreased treatment engagement and an increase in nonfatal overdoses. Considered together, these findings demonstrate the benefits of statewide MOUD for incarcerated individuals as well as the need to identify and address barriers to continuation of care following release from incarceration in the context of COVID-19.
Keywords: Medication for opioid use disorder, Medication for addiction treatment, Prisons, Correctional facilities, Overdose, COVID-19
1. Introduction
Opioid use has reached epidemic proportions in the United States (Dowell et al., 2017; Wilson et al., 2020) and individuals with opioid use disorder (OUD) are disproportionately overrepresented in the criminal justice system (Winkelman et al., 2018). Overdose is the leading cause of death after release from incarceration (Binswanger et al., 2013), with overdose deaths >100 times more likely within the first two weeks of reentry from prison to the community compared to the general population (Binswanger et al., 2007). Medications for opioid use disorder (MOUD) are the only empirically based treatments for OUD (Schuckit, 2016; Volkow et al., 2014) and substantially decrease the risk of overdose and death (Schwartz et al., 2013). A large body of evidence demonstrates the positive effects of MOUD use in correctional facilities including reductions in illicit opioid use (Kinlock et al., 2009; Mattick et al., 2009), overdose (Degenhardt et al., 2011; Green et al., 2018; Kerr et al., 2007), and other negative outcomes (Evans, Wilson, & Friedmann, 2022; MacArthur et al., 2012). As such, the National Academies of Science have deemed withholding these medications as unethical (Mancher & Leshner, 2019). Nonetheless, MOUD is not available to most incarcerated individuals in the United States (Grella et al., 2020; Simon et al., 2021; Weizman et al., 2021).
In July 2018 Vermont began offering all three Food and Drug Administration (FDA) approved MOUDs (buprenorphine, methadone, and naltrexone) to all incarcerated individuals who meet criteria for OUD (Act 176, 2018). The Vermont Department of Corrections (VT DOC) is a unified (prison and jail) state-run correctional system and thus the implementation of MOUDs affected all pretrial and convicted residents of the six correctional facilities within the state. In 2016, Rhode Island became the first state to implement MOUD in a statewide correctional system (Clarke et al., 2018) and reported a 60.5% reduction in overdose deaths following MOUD implementation among people released from incarceration within the prior 12 months (Green et al., 2018). However, each US carceral setting is unique, with variation in the incarcerated population characteristics as well as the policies and practices that guide MOUD implementation, which could lead to variation in outcomes. As the second state to implement MOUD in a statewide correctional system, Vermont provides an important opportunity to build the knowledge base on the implementation and outcomes of MOUD in justice settings.
The context for providing MOUD in correctional facilities and continuing care in the community has changed due to the COVID-19 pandemic (Akiyama et al., 2020; Hawks, Woolhandler, & McCormick, 2020; Mukherjee & El-Bassel, 2020; Wallace et al., 2020). In correctional facilities across the United States, adaptations to COVID-19 include restricting residents' activity, changing prison protocols, mandatory masking, decreased in-person contact, and increased rapid release for individuals with nonviolent offenses to decrease risks of infection (Akiyama et al., 2020; Hawks, Woolhandler, & McCormick, 2020; Mukherjee & El-Bassel, 2020; Vermont Department of Corrections, 2020). In the community, treatment centers across the United States adjusted to decreased in-person care (Alexander et al., 2020), including increasing telehealth and buprenorphine take-home doses per the new SAMHSA guidelines (SAMHSA, 2020). However, we know little regarding how COVID-19 has impacted MOUD utilization in correctional facilities or clinical outcomes after release from incarceration (however see Harrington et al., 2023; Mukherjee & El-Bassel, 2020). The current study aimed to longitudinally assess the statewide implementation of MOUD in Vermont's correctional system and the subsequent impact of COVID-19 on MOUD engagement among individuals incarcerated in Vermont as well as continuation of MOUD and the prevalence of overdose following release from incarceration.
2. Materials and methods
2.1. Administrative data sources and cohort construction
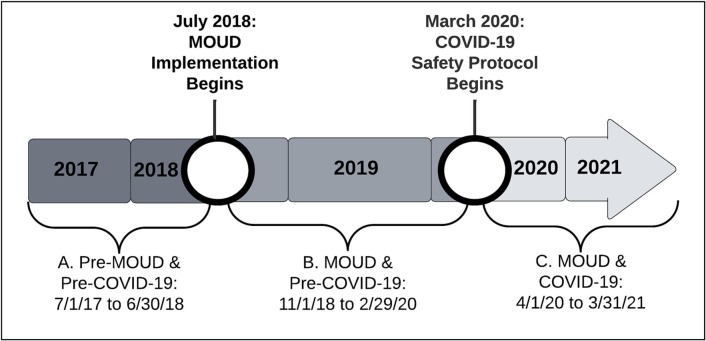
Data were provided by a statewide evaluation (Klemperer et al., 2022) that linked administrative records from three sources. First, the study team identified the cohort of interest using VT DOC data on all individuals who were incarcerated for one or more nights between 07/01/2017 and 03/31/2021. Next, we constructed three cohort groups, as the key independent variable, to examine outcomes during the year prior to MOUD implementation (Period A: 07/01/2017 to 06/30/2018, n = 5177) compared to the period after MOUD implementation and before the COVID-19 state of emergency (Period B: 11/01/2018 to 02/29/2020, n = 5665), and also compared to the year following the COVID-19 state of emergency (Period C: 04/01/2020 to 03/31/2021, n = 2926; Fig. 1 ). The study included individuals who were incarcerated during two (23%) or three (12%) time-periods in each time-period. Individuals who were incarcerated multiple times within the same time-period (Period A = 12%; Period B = 13%; Period C = 7%) were categorized according to whether they experienced the outcome during any of their incarcerations within the time-period in question.
Fig. 1.
Timeline for the implementation of medication for opioid use disorder (MOUD) in Vermont correctional facilities and the onset of COVID-19.
Implementation of MOUD occurred within the VT DOC between 07/01/2018 and 10/31/2018 and implementation of COVID-19 safety procedures occurred between 03/01/2020 to 03/31/2021. We omitted data from these time periods to reduce the potentially confounding influence of transitory factors and focus the analysis on outcomes when MOUD was fully implemented, and COVID-19 safety procedures were fully established (Vermont Department of Corrections, 2020). The DOC administrative data were linked with Medicaid claims and Vermont Department of Health data (described below) using incarcerated individuals' Social Security Numbers and birthdates in R (R Core Team, 2022). Following data linkage, the study team de-identified all datasets for analysis. The University of Vermont Institutional Review Board exempted the study.
2.2. Medications for opioid use disorder (MOUD) treatment while incarcerated
Vermont DOC administrative records provided demographic information and data on MOUD (e.g., buprenorphine, methadone, naltrexone) received while incarcerated. Screening for OUD was not consistently conducted in Period A, prior to MOUD implementation. Thus, we were unable to assess change in the proportion of incarcerated individuals with OUD who received MOUD while incarcerated. We report the proportion of people incarcerated during each time-period who were prescribed MOUD by VT DOC–contracted health care providers. Individuals could have been prescribed more than one MOUD while incarcerated and thus medication categories are not mutually exclusive. After Vermont implemented MOUD in its correctional system, individuals who met OUD criteria at intake could either continue MOUD from the community (i.e., those who had been prescribed MOUD prior to incarceration) or initiate MOUD induction (i.e., MOUD induction at intake). Some individuals who received an MOUD prescription (either continued from the community or newly inducted) were discontinued from all MOUD prior to their release. Health care providers within each correctional facility documented reasons for MOUD discontinuation.
2.3. Continuation of MOUD and other outcomes after release from incarceration
We analyzed Medicaid insurance claims data to identify treatment utilization and related outcomes after release from incarceration. These analyses were limited to the subset of Medicaid recipients with a current or recent OUD diagnosis (i.e., within 3 years prior to their release from incarceration) as has been used by prior research (Hser et al., 2015) and included 79.0% of incarcerated individuals in Period A, 76.1% in Period B, and 79.2% in Period C. In addition, we conducted sensitivity analyses to examine outcomes 1) among the entire Medicaid population and 2) among individuals who were receiving MOUD within the 30 days prior to their release from incarceration in Periods B and C (reported in the supplemental document). Both sensitivity analyses resulted in findings that were largely consistent with our primary analysis. We compared demographic characteristics between the analyzed Medicaid sample and those excluded because they did not have Medicaid to assess for potential bias resulting from our analytic sample.
The study measured outcomes based on Medicaid claims data 30 days after release from incarceration and included 1) MOUD continuation as indicated by prescriptions for buprenorphine, methadone, or naltrexone; 2) substance use disorder (SUD) counseling as indicated by one or more Medicaid claims for reimbursement; 3) mental health counseling as indicated by one or more Medicaid claims for reimbursement; 4) all-cause emergency room visits; and 5) nonfatal opioid overdoses. We chose a 30-day window given that the first month after release from incarceration is the period of highest risk for illicit opioid use and overdose among individuals with OUD (Binswanger et al., 2007; Merrall et al., 2010).
The Vermont Department of Health provided overdose fatality data. Similar to data on nonfatal overdoses, all fatal overdoses involved opioid use but could have also included other drug use. The absolute number of overdose fatalities in Vermont was small and thus we report overdose fatalities within 1 year after release from incarceration. We censored sample sizes with 10 or fewer individuals to maintain confidentiality.
2.4. Analysis
Descriptive statistics were calculated to describe population characteristics for each of the three time periods. We then used logistic regression to compare the use of MOUD between time-periods to evaluate change in treatment utilization before versus after MOUD implementation (Periods A vs B) and before versus after the onset of COVID-19 (Periods B vs C). Similarly, we used logistic regression to compare the type of MOUD used between time-periods, whether MOUD was continued from the community or initiated upon incarceration, and whether MOUD was discontinued prior to release from incarceration. For the subsample of individuals who discontinued MOUD while incarcerated, we calculated descriptive statistics to illustrate the reasons provided by health care personnel for MOUD discontinuation separately by time-period. We used Stata to conduct analysis of outcomes during incarceration (StataCorp, 2021).
We examined change in treatment utilization and overdose following release from incarceration. The study used release episodes as the unit of analysis for outcomes following release from incarceration to account for individuals with more than one release from incarceration. We performed multi-level logistic regressions to examine change between time-periods in MOUD prescriptions, SUD counseling, mental health counseling, emergency room visits, and nonfatal overdoses within 30 days following release from incarceration. We conducted analysis of outcomes after release from incarceration using R (R Core Team, 2022). The study set significance at p < .05 for all analyses.
3. Results
A total of 5177 individuals were incarcerated in Vermont correctional facilities for a minimum of 1 night during Period A (pre-MOUD implementation and pre-COVID-19), 5665 during Period B (post-MOUD implementation and pre-COVID-19) and 2926 during Period C (post-MOUD implementation and during COVID-19). Most people who were incarcerated during these time-periods were white, non-Hispanic, male, in their mid- to late-thirties, and unmarried (see Table 1 ).
Table 1.
Incarcerated population characteristics.
| A) Pre-MOUD implementation & pre-COVID-19 (n = 5177) | B) Post-MOUD implementation & pre-COVID-19 (n = 5665) | C) Post-MOUD implementation & during COVID-19 (n = 2926) | |
|---|---|---|---|
| Demographics | |||
| Mean (SD) age | 36.3 (11.5) | 36.8 (11.5) | 38.0 (11.4) |
| Gender, n (%) | |||
| Female | 852 (16.5) | 975 (17.2) | 368 (12.6) |
| Male | 4299 (83.0) | 4651 (82.1) | 2516 (86.0) |
| Transgender | 22 (0.4) | 24 (0.4) | 24 (0.8) |
| Missing or not reported | 4 (0.1) | 15 (0.3) | 18 (0.6) |
| Race, n (%) | |||
| Black or AA | 497 (9.6) | 544 (9.6) | 270 (9.2) |
| White | 4267 (82.4) | 4623 (81.6) | 2490 (85.1) |
| Other | 74 (1.4) | 93 (1.6) | 92 (3.1) |
| Missing or not reported | 339 (6.6) | 405 (7.2) | 74 (2.5) |
| Ethnicity, n (%) | |||
| Hispanic | 441 (8.5) | 553 (9.8) | 270 (9.2) |
| Non-Hispanic | 4735 (91.5) | 5111 (90.2) | 2655 (90.7) |
| Missing or not reported | 1 (0.02) | 1 (0.02) | 1 (0.03) |
| Marital status, n (%) | |||
| Married/civil union | 574 (11.1) | 643 (11.4) | 313 (10.7) |
| Divorced/separated | 682 (13.2) | 753 (13.3) | 378 (12.9) |
| Single | 2885 (55.7) | 3041 (53.7) | 1656 (56.6) |
| Widowed | 44 (0.9) | 57 (1.0) | 30 (1.0) |
| Missing or not reported | 992 (19.2) | 1171 (20.7) | 549 (18.8) |
AA = African American; MOUD = Medication for opioid user disorder; SD=Standard deviation.
3.1. Use of MOUD while incarcerated
During Period A (pre-MOUD implementation and pre-COVID-19), <1 % of individuals were prescribed MOUD while incarcerated (Table 2 ). Prescriptions for MOUD during this time-period were associated with a program to pilot time-limited MOUD treatment in two of the state's six correctional facilities. After state-wide MOUD implementation (Period B), prescriptions increased such that one third (33.9%) of incarcerated individuals were receiving MOUD. With the onset of COVID-19 (Period C), MOUD prescriptions decreased such that 26.6% (OR = 0.7, 95% CI = 0.6, 0.8) of the incarcerated population were maintained on MOUD. Analysis exploring this decrease identified a simultaneous increase in the mean percent of individuals released from incarceration who were receiving MOUD at the time of their release from 27.0% (SD = 2.0%) before to 34.9% (SD = 4.8%) after the onset of COVID-19 (Periods B vs C; p = .037). This change corresponded with the rapid release of people with nonviolent convictions across the state in response to COVID-19, which may have driven a reduction in OUD in the remaining incarcerated population in Period C and also indicates an increased need for OUD treatment in the community.
Table 2.
Medication for opioid use disorder (MOUD) prescriptions among people incarcerated in Vermont.
| A) Pre-MOUD implementation & pre-COVID-19 (n = 5177) | B) Post-MOUD implementation & pre-COVID-19 (n = 5665) | C) Post-MOUD implementation & during COVID-19 (n = 2926) | |
|---|---|---|---|
| Any MOUD, n (%) | 39 (0.8) | 1918 (33.9) | 779 (26.6) |
|
Any vs no MOUD OR (95% CI) |
Referent | 67.4 (49.0, 92.9) | 47.8 (34.5, 66.2) |
| – | Referent | 0.7 (0.6, 0.8) |
Bolded text = statistically significant (p < .05); CI=Confidence interval; MOUD = Medication for opioid use disorder; OR = Odds ratio.
Among individuals who received MOUD while incarcerated, the majority (66.7% to 84.0%) were prescribed buprenorphine regardless of time-period (Table 3 , Panel A). Interpretation of the proportion of individuals who received a prescription for buprenorphine, methadone, or naltrexone in Period A is limited due to the small number of individuals (n = 39) who received MOUD prior to statewide implementation. After MOUD implementation, the proportion of individuals who received buprenorphine versus methadone or naltrexone did not significantly differ before versus during COVID-19 (Periods B vs C; OR = 1.1, 95% CI = 0.9, 1.4). Most individuals who were prescribed MOUD while incarcerated initiated their MOUD upon incarceration (Table 3, Panel B). However, the proportion who initiated MOUD upon incarceration decreased from 63.1% to 53.9% with the onset of COVID-19 (Periods B vs C; OR = 0.7, 95% CI = 0.6, 0.8).
Table 3.
Medication for opioid use disorder (MOUD) characteristics among individuals who were prescribed an MOUD while incarcerated in Vermont.
| A) Pre-MOUD implementation & pre-COVID-19 (n = 39) | B) Post-MOUD implementation & pre-COVID-19 (n = 1918) | C) Post-MOUD implementation & during COVID-19 (n = 779) | |
|---|---|---|---|
| A. MOUD type | |||
| Buprenorphine, n (%) | 26 (66.7) | 1585 (82.6) | 654 (84.0) |
| Methadone, n (%) | 13 (33.3) | 268 (14.0) | 112 (14.4) |
| Naltrexone, n (%) | 0 (0) | 65 (3.4) | 13 (1.7) |
| Buprenorphine vs other MOUD OR (95% CI) | Referent | 2.3 (1.2, 4.6) | 2.6 (1.3, 3.9) |
| – | Referent | 1.1 (0.9, 1.4) | |
| B. MOUD initiation, continuation, or discontinuation | |||
| Initiated any MOUD, n (%) | 16 (41.0) | 1210 (63.1) | 420 (53.9) |
| Continued any MOUD, n (%) | 23 (59.0) | 708 (36.9) | 359 (46.1) |
|
Initiation vs continuation OR (95% CI) |
Referent | 2.5 (1.3, 4.7) | 1.7 (0.9, 3.2) |
| – | Referent | 0.7 (0.6, 0.8) | |
| Discontinued any MOUD, n (%) | 0 (0) | 307 (16.0) | 62 (8.0) |
| Discontinued vs did not discontinue OR (95% CI) | – | Referent | 0.5 (0.3, 0.6) |
Bolded text = statistically significant (p < .05); CI=Confidence interval; MOUD = Medication for opioid use disorder; OR = Odds ratio.
Prior to COVID-19 (Period B), 16.0% of people who received MOUD while incarcerated later discontinued all MOUD while incarcerated and discontinuation significantly decreased to 8.0% with the onset of COVID-19 in Period C (OR = 0.5, 95% CI = 0.3, 0.6). The study found a total of 372 MOUD discontinuations among 307 individuals in Period B, prior to COVID-19. During COVID-19 (Period C) a total of 85 MOUD discontinuations occurred among 62 individuals. The majority of discontinuations in both time-periods were attributed to diversion (Period B = 59.4% and Period C = 71.8%; Supplemental Table 1). The next most common reason for discontinuation was per the patient's request (Period B = 12.9% and Period C = 20.0%). Importantly, interpretation of changes in reasons for discontinuation prior to versus during COVID-19 (Periods B vs C) are limited due to the fact that over a quarter (25.5%) of reasons for MOUD discontinuation before COVID-19 were not reported in the electronic health record system, highlighting the importance of complete data collection in correctional facilities.
3.2. Continuation of MOUD and other treatment after release from incarceration
In total,1552 individuals released from incarceration in Period A (pre-MOUD implementation and pre-COVID-19), 1851 in Period B (post-MOUD implementation and pre-COVID-19), and 735 in Period C (post-MOUD implementation and during COVID-19) had a Medicaid claim indicating an OUD diagnosis and thus were included in the primary analysis of outcomes following release from incarceration. During Period A, individuals with an OUD diagnosis contributed to 2456 releases from incarceration (mean = 1.6 [SD = 1.2] per individual). During Period B, there were 3253 releases (mean = 1.8 [SD = 1.3] per individual) occurred and 956 releases from incarceration (mean = 1.3 [SD = 0.7] per individual) occurred during Period C. Compared to individuals with Medicaid who were included in analysis, those who were excluded because they did not have Medicaid were less likely to identify as female in Periods A (13.5% vs 22.4%), B (10.8% vs 23.0%) and C (10.8% vs 18.7%; all p < .05) and less likely to identify as white in Periods A (74.7% vs 82.7%) and B (71.2% vs 81.7%; all p < .05), but otherwise did not differ in demographic characteristics reported in Table 1.
In Period A (pre-MOUD implementation and pre-COVID-19), approximately one-third (33.9%) of releases among individuals with OUD resulted in an MOUD prescription in the community within 30 days following release from incarceration (Table 4 , Panel A). This increased to 41.0% after statewide MOUD implementation in Period B (OR = 1.4, 95% CI = 1.3, 1.7) and then decreased with the onset of COVID-19 in Period C (35.6%; OR = 0.8, 95% CI = 0.6, 0.9) to a level that did not significantly differ from before MOUD implementation. Sensitivity analysis including the entire Vermont Medicaid incarcerated population demonstrated a similar increase in community MOUD prescriptions after the implementation of MOUD in correctional facilities (OR = 2.2, 95% CI = 1.8, 2.7). However, in contrast to primary findings among those with an OUD diagnosis, MOUD prescriptions after release from incarceration did not significantly change with the onset of COVID-19 in the entire Medicaid incarcerated population (Supplemental Table 2, Panel A). In a second sensitivity analysis including only individuals who were prescribed MOUD while incarcerated in Periods B and C, MOUD prescriptions after release from incarceration did not significantly change with the onset of COVID-19 (Supplemental Table 3, Panel A).
Table 4.
Treatment utilization, emergency room visits, and overdose after release from incarceration.
| A) Pre-MOUD implementation & pre-COVID-19 (n releases = 2456) | B) Post-MOUD implementation & pre-COVID-19 (n releases = 3253) | C) Post-MOUD implementation & during COVID-19 (n releases = 956) | |
|---|---|---|---|
| A. Treatment utilization | |||
| % prescribed MOUD within 30 days of release | 33.9 | 41.0 | 35.6 |
| OR (95% CI) | Referent | 1.4 (1.3, 1.7) | 1.1 (0.9, 1.4) |
| – | Referent | 0.8 (0.6, 0.9) | |
| % attended SUD counseling within 30 days of release | 15.6 | 10.0 | 5.6 |
| OR (95% CI) | Referent | 0.5 (0.3, 0.6) | 0.2 (0.1, 0.3) |
| – | Referent | 0.3 (0.2, 0.5) | |
| % attended MH counseling within 30 days of release | 16.9 | 15.1 | 10.7 |
| OR (95% CI) | Referent | 0.9 (0.7, 1.1) | 0.5 (0.3, 0.7) |
| – | Referent | 0.6 (0.4, 0.9) | |
| B. Emergency room visits and overdose | |||
| % emergency room visit within 30 days of release | 13.5 | 14.5 | 12.2 |
| OR (95% CI) | Referent | 1.1 (0.9, 1.4) | 0.7 (0.5, 1.0) |
| – | Referent | 0.4 (0.3, 0.7) | |
| % non-fatal overdose within 30 days of release | 1.2 | 0.8 | 1.9 |
| OR (95% CI) | Referent | 0.3 (0.1, 0.8) | 1.5 (0.5, 4.2) |
| – | Referent | 2.5 (1.3, 4.5) | |
| % fatal overdose within one year of release | 1.1 | Censored because ≤10 events occurreda | Censored because ≤10 events occurreda |
All release episodes are from individuals with a Medicaid claim indicating a diagnosis of opioid use disorder (OUD).
Bolded text = statistically significant (p < .05); CI=Confidence interval; MH = Mental health; MOUD = Medication for opioid use disorder; SUD=Substance use disorder.
Data were censored to protect confidentiality because ≤10 events occurred.
Among individuals with OUD, 15.6% of releases resulted in engagement in SUD counseling in the community during Period A (pre-MOUD implementation and pre-COVID-19). Substance use disorder counseling subsequently decreased to 10.0% after MOUD implementation (Periods A vs B: OR = 0.5, 95% CI = 0.3, 0.6) and to 5.6% with the onset of COVID-19 (Periods B vs C: OR = 0.3, 95% CI = 0.2, 0.5). Use of mental health counseling did not significantly change prior to versus following MOUD implementation (Period A = 16.9%; Period B = 15.1%) but decreased to 10.7% following the onset of COVID-19 (Periods B vs C: OR = 0.6, 95% CI = 0.4, 0.9; Table 4, Panel A). Findings were similar in sensitivity analyses including the entire Vermont Medicaid incarcerated population (Supplemental Table 2, Panel A) and when limited to those who received MOUD while incarcerated (Supplemental Table 3, Panel A).
3.3. Emergency room visits and overdose after release from incarceration
Less than 15% of releases resulted in one or more trips to the emergency room within 30 days following release from incarceration. This did not significantly differ prior to versus following MOUD implementation (Periods A vs B), but emergency room trips significantly decreased following the onset of COVID-19 (Periods B vs C: OR = 0.4, 95% CI = 0.3, 0.7; Table 4, Panel B). Although absolute numbers were small, the proportion of releases that resulted in a nonfatal overdose decreased by one-third when MOUD was implemented from 1.2% in Period A to 0.8% in Period B (OR = 0.3, 95% CI = 0.1, 0.8). However, nonfatal overdoses subsequently increased from 0.8% in Period B to 1.9% with the onset of COVID-19 in Period C (OR = 2.5, 95% CI = 1.3, 4.5). Twenty-seven (1.1%) individuals who were incarcerated prior to MOUD implementation (Period A) died from an opioid-related overdose within the year following release from incarceration. Opioid-related fatal overdoses following release from incarceration decreased to ≤10 deaths (i.e., ≤0.3%) after MOUD implementation (Period B) and remained at ≤10 deaths (i.e., ≤1.0%) following the onset of COVID-19 (Period C). The exact number of opioid-related overdose deaths in Periods B and C were censored to protect confidentiality, and thus analysis was not possible. Findings were similar in sensitivity analyses including the entire Vermont Medicaid incarcerated population (Supplemental Table 2, Panel B) and when limited to those who received MOUD while incarcerated (Supplemental Table 3, Panel A).
4. Discussion
This evaluation linked data from the Vermont Department of Corrections, the Vermont Department of Health, and Medicaid claims to longitudinally assess the impacts of MOUD implementation and COVID-19 in a statewide correctional system. Implementation of MOUD resulted in more than one-third of the Vermont incarcerated population receiving MOUD, most of whom received buprenorphine. After the onset of COVID-19, the percentage of incarcerated individuals who were prescribed MOUD decreased to 26.6%. Rapid release of individuals convicted of nonviolent crimes following the onset of COVID-19 was associated with an increase in releases among people prescribed MOUD, suggesting that the simultaneous reduction in MOUD prescriptions could be attributable to a decline in the prevalence of OUD in the remaining incarcerated population. Though estimates of the prevalence of OUD in US correctional facilities vary (Maruschak et al., 2021; Simon et al., 2021), our findings are consistent with prior findings that people with OUD are disproportionately overrepresented in US correctional facilities (Simon et al., 2021; Winkelman et al., 2018) and indicate that at least one quarter to one-third of individuals incarcerated for ≥1 night in Vermont met criteria for OUD since MOUD was implemented in 2018.
Most individuals who received MOUD while incarcerated had not been receiving MOUD in the community prior to incarceration (63% before COVID-19 and 54% after COVID-19). These individuals represent a group who met OUD criteria but were not receiving MOUD at the time of incarceration. This finding underscores that the justice system can substantially increase treatment engagement in a highly vulnerable population by offering MOUD in correctional facilities. Importantly, increasing access to MOUD in the community in the absence of incarceration must remain a high priority in addition to providing treatment within correctional facilities. The observed decline in MOUD initiations between Periods B and C could be associated with COVID-19 precautions (e.g., limited face-to-face interactions) or simply a change in the overall incarcerated population (e.g., fewer individuals who were not receiving MOUD at the time of incarceration). While buprenorphine is provided within each VT DOC correctional facility, methadone is provided by an outside vendor, requiring patients to leave the correctional facility to initiate the medication at a clinic in the community, which may have contributed to the overall decline in MOUD initiations during COVID-19.
Of note, MOUD discontinuations while incarcerated decreased by 50% with the onset of COVID-19, with diversion cited as the most common reason for discontinuation both prior to and during COVID-19. The observed decrease in MOUD discontinuations could be due to changes in factors that affect diversion, such as decreased contact between incarcerated individuals or modified medication distribution procedures. Although no official VT DOC policy changes occurred regarding MOUD discontinuation, the observed reduction in discontinuations may reflect a change in provider practices regarding MOUD diversion or discontinuation. Future research should identify mechanisms by which COVID-19 influenced MOUD prescriptions, diversion, and discontinuation in correctional facilities to optimize OUD treatment for incarcerated individuals.
Consistent with prior research (Moore et al., 2019; Sharma et al., 2016; Simon et al., 2021), we found that MOUD prescriptions following release from incarceration increased after MOUD was implemented in correctional facilities statewide. This finding held true in our primary sample of individuals with an OUD diagnosis and in a sensitivity analysis of the entire incarcerated Medicaid population. Given the elevated risk for illicit opioid use and overdose immediately following release from incarceration (Binswanger et al., 2007; Merrall et al., 2010), this increase in treatment engagement suggests a substantial public health benefit from the statewide implementation of MOUD in correctional facilities.
Among individuals with OUD who were released from incarceration, nonfatal overdoses decreased by one-third and fatal overdoses decreased from 27 to ≤10 deaths following statewide MOUD implementation, representing a >60% reduction in fatalities. This figure is consistent with prior research, which identified a 60.5% reduction in fatal overdoses following MOUD implementation among individuals released from incarceration in Rhode Island (Green et al., 2018). Considered together, our findings provide further support for the substantial reduction in overdose and death associated with MOUD among incarcerated individuals and demonstrate the importance of implementing MOUD in US correctional systems.
In contrast, the onset of COVID-19 was associated with a decrease in MOUD prescriptions, counseling, and emergency room visits as well as an increase in opioid-related nonfatal overdoses following release from incarceration. Although reductions in emergency room visits could reflect changes in medical need or access, the observed reduction in treatment engagement and increase in nonfatal overdoses demonstrate adverse public health consequences associated with COVID-19 among recently incarcerated individuals, a population highly vulnerable to harm from opioids. These findings are consistent with the devastating consequences of COVID-19 throughout the United States, including decreases in all-cause emergency room visits (Soares III et al., 2021) as well as increases in overdose (Linas et al., 2021; Mason et al., 2021; Slavova et al., 2020) and barriers to MOUD (Joudrey et al., 2021; Leppla & Gross, 2020; Wakeman et al., 2020). The absolute number of opioid-related fatal overdoses following MOUD implementation remained low after the onset of COVID-19 (≤10 deaths) but interpretation of the relative change in mortality is limited due to censorship of the specific number of deaths to protect confidentiality. Nonetheless, findings from this evaluation demonstrate a need to improve substance use treatment for incarcerated individuals reentering the community (Moore et al., 2020), with reentry services tailored to surmount the unique barriers associated with COVID-19.
4.1. Strengths and limitations
Strengths of this evaluation include the use of a data set that included all incarcerated individuals in Vermont and the examination of longitudinal outcomes during incarceration as well as following release into the community in a subset of individuals with Medicaid insurance. This evaluation is among the first to report outcomes from MOUD implementation in a statewide correctional system (Clarke et al., 2018) and the first to address the statewide impact of COVID-19 on MOUD treatment for people who are incarcerated. Our findings demonstrate an overall public health benefit associated with the statewide implementation of MOUD for incarcerated individuals and serve as an example to support MOUD implementation in other states' correctional systems (Weizman et al., 2021).
Despite these strengths, several limitations are worth bearing in mind. First, causal interpretation of these findings is limited by the fact that the data are observational in nature and thus subject to confounding biases. Second, as previously noted, screening for OUD was not consistently conducted prior to MOUD implementation and thus we were unable to assess change in the proportion of incarcerated individuals with OUD who received MOUD while incarcerated, highlighting the importance of universal screening for OUD in correctional systems. Third, we report MOUD prescriptions within 30-days following release from incarceration; however, the proportion of individuals who took the medication as prescribed is unclear. Fourth, outcomes following release from incarceration were limited to the 76.1% to 79.2% of individuals who had Medicaid, a population that was more likely to be female and white than those who did not have Medicaid. Finally, this evaluation examined changes in the incarcerated population in Vermont, which is a small rural state with a unified (jail and prison) state-run correctional system. Accordingly, our findings may have limited generalizability to other more urban states with different correctional systems.
5. Conclusion
This longitudinal evaluation found increased treatment engagement and a decrease in opioid-related overdoses following implementation of MOUD in a statewide correctional system. These findings are consistent with prior research and provide compelling evidence in support of implementing MOUD in statewide correctional systems to increase access to these lifesaving medications. Improvements related to MOUD were somewhat attenuated with the onset of COVID-19, which was associated with decreased treatment engagement and an increase in nonfatal overdoses. Considered together, these findings demonstrate the benefits to statewide MOUD for incarcerated individuals as well as the need to identify and address barriers to continuation of care following release from incarceration in the context of COVID-19.
Funding
This study was funded by a JCOIN-Rapid Innovation Grant awarded to EMK from the JCOIN cooperative agreement (MPI Taxman and Rudes) funded through the National Institute on Drug Abuse (NIDA) by the National Institutes of Health (NIH). We gratefully acknowledge the collaborative contributions of NIDA and support from the U2CDA050097 award. Additionally, EE is funded by NIDA 1UG1DA050067-01 and EMK and KRP are funded by the National Institute of General Medical Sciences of the National Institutes of Health (P20GM103644). The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of NIDA or NIH.
Declaration of competing interest
The authors have nothing to disclose.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.josat.2023.209103.
Appendix A. Supplementary data
Supplementary tables
References
- Act 176 Vermont General Assembly, 2018 Reg. Sess. (VT 2018) 2018. https://legislature.vermont.gov/bill/status/2018/S.166
- Akiyama M.J., Spaulding A.C., Rich J.D. Flattening the curve for incarcerated populations - COVID-19 in jails and prisons. The New England Journal of Medicine. 2020;382(22):2075–2077. doi: 10.1056/NEJMp2005687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander G.C., Stoller K.B., Haffajee R.L., Saloner B. An epidemic in the midst of a pandemic: Opioid use disorder and COVID-19. Annals of Internal Medicine. 2020;173(1):57–58. doi: 10.7326/M20-1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binswanger I.A., Blatchford P.J., Mueller S.R., Stern M.F. Mortality after prison release: Opioid overdose and other causes of death, risk factors, and time trends from 1999 to 2009. Annals of Internal Medicine. 2013;159(9):592–600. doi: 10.7326/0003-4819-159-9-201311050-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binswanger I.A., Stern M.F., Deyo R.A., Heagerty P.J., Cheadle A., Elmore J.G., Koepsell T.D. Release from prison—A high risk of death for former inmates. New England Journal of Medicine. 2007;356(2):157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke J.G., Martin R.A., Gresko S.A., Rich J.D. The first comprehensive program for opioid use disorder in a US statewide correctional system. American Journal of Public Health. 2018;108(10):1323–1325. doi: 10.2105/AJPH.2018.304666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L., Bucello C., Mathers B., Briegleb C., Ali H., Hickman M., McLaren J. Mortality among regular or dependent users of heroin and other opioids: A systematic review and meta-analysis of cohort studies. Addiction. 2011;106(1):32–51. doi: 10.1111/j.1360-0443.2010.03140.x. [DOI] [PubMed] [Google Scholar]
- Dowell D., Arias E., Kochanek K., Anderson R.N., Guy G.P., Losby J.L., Baldwin G. Contribution of opioid-involved poisoning to the change in life expectancy in the United States, 2000-2015. JAMA: The Journal of the American Medical Association. 2017;318(11):1065–1067. doi: 10.1001/jama.2017.9308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans E.A., Wilson D., Friedmann P.D. Recidivism and mortality after in-jail buprenorphine treatment for opioid use disorder. Drug and Alcohol Dependence. 2022;231:109254. doi: 10.1016/j.drugalcdep.2021.109254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green T.C., Clarke J., Brinkley-Rubinstein L., Marshall B.D., Alexander-Scott N., Boss R., Rich J.D. Postincarceration fatal overdoses after implementing medications for addiction treatment in a statewide correctional system. JAMA Psychiatry. 2018;75(4):405–407. doi: 10.1001/jamapsychiatry.2017.4614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella C.E., Ostile E., Scott C.K., Dennis M., Carnavale J. A scoping review of barriers and facilitators to implementation of medications for treatment of opioid use disorder within the criminal justice system. International Journal of Drug Policy. 2020;81 doi: 10.1016/j.drugpo.2020.102768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington C., Bailey A., Delorme E., Hano S., Evans E.A. “And Then COVID Hits”: A qualitative study of how jails adapted services to treat opioid use disorder during COVID-19. Substance Use & Misuse. 2023;58(2):266–274. doi: 10.1080/10826084.2022.2155480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawks L., Woolhandler S., McCormick D. COVID-19 in prisons and jails in the United States. JAMA Internal Medicine. 2020;180(8):1041–1042. doi: 10.1001/jamainternmed.2020.1856. [DOI] [PubMed] [Google Scholar]
- Hser Y.-I., Evans E., Grella C., Ling W., Anglin D. Long-term course of opioid addiction. Harvard Review of Psychiatry. 2015;23(2):76–89. doi: 10.1097/HRP.0000000000000052. [DOI] [PubMed] [Google Scholar]
- Joudrey P.J., Adams Z.M., Bach P., Van Buren S., Chaiton J.A., Ehrenfeld L., Guerra M.E., Gleeson B., Kimmel S.D., Medley A. Methadone access for opioid use disorder during the COVID-19 pandemic within the United States and Canada. JAMA Network Open. 2021;4(7) doi: 10.1001/jamanetworkopen.2021.18223. e2118223-e2118223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr T., Fairbairn N., Tyndall M., Marsh D., Li K., Montaner J., Wood E. Predictors of non-fatal overdose among a cohort of polysubstance-using injection drug users. Drug and Alcohol Dependence. 2007;87(1):39–45. doi: 10.1016/j.drugalcdep.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Kinlock T.W., Gordon M.S., Schwartz R.P., Fitzgerald T.T., O’Grady K.E. A randomized clinical trial of methadone maintenance for prisoners: Results at 12 months postrelease. Journal of Substance Abuse Treatment. 2009;37(3):277–285. doi: 10.1016/j.jsat.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klemperer E.M., Wreschnig L., Crocker A., King-Mohr J., Ramniceanu A., Evans E.A., Rawson R.A. A statewide evaluation of the implementation and effectiveness of medications for opioid use disorder in Vermont correctional facilities and the impact of COVID-19. Vermont General Assembly Senate Committee on Institutions. 2022. https://legislature.vermont.gov/committee/detail/2022/28/Reports (Accessed November 3 2022)
- Leppla I.E., Gross M.S. Optimizing medication treatment of opioid use disorder during COVID-19 (SARS-CoV-2) Journal of Addiction Medicine. 2020;14(4):e1–e3. doi: 10.1097/ADM.0000000000000678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linas B.P., Savinkina A., Barbosa C., Mueller P.P., Cerdá M., Keyes K., Chhatwal J. A clash of epidemics: Impact of the COVID-19 pandemic response on opioid overdose. Journal of Substance Abuse Treatment. 2021;120:108158. doi: 10.1016/j.jsat.2020.108158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacArthur G.J., Minozzi S., Martin N., Vickerman P., Deren S., Bruneau J., Degenhardt L., Hickman M. Opiate substitution treatment and HIV transmission in people who inject drugs: systematic review and meta-analysis. BMJ (Clinical research ed.) 2012:345. doi: 10.1136/bmj.e5945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancher M., Leshner A.I. National Acadamies Press; 2019. Medications for opioid use disorder save lives. [PubMed] [Google Scholar]
- Maruschak L.M., Bronson J., Alper M. In: Survey of prison inmates, 2016: Alcohol and drug use and treatment reported by prisoners. Bureau of Justice Statistics, editor. Bureau of Justice Statistics: Office of Justice Programs; 2021. [Google Scholar]
- Mason M., Welch S.B., Arunkumar P., Post L.A., Feinglass J.M. Notes from the field: Opioid overdose deaths before, during, and after an 11-week COVID-19 stay-at-home order—Cook County, Illinois, January 1, 2018–October 6, 2020. Morbidity and Mortality Weekly Report. 2021;70(10):362. doi: 10.15585/mmwr.mm7010a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattick R.P., Breen C., Kimber J., Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database of Systematic Reviews. 2009;(3) [Google Scholar]
- Merrall E.L., Kariminia A., Binswanger I.A., Hobbs M.S., Farrell M., Marsden J., Hutchinson S.J., Bird S.M. Meta-analysis of drug-related deaths soon after release from prison. Addiction (Abingdon, England) 2010;105(9):1545–1554. doi: 10.1111/j.1360-0443.2010.02990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore K.E., Hacker R.L., Oberleitner L., McKee S.A. Reentry interventions that address substance use: A systematic review. Psychological Services. 2020;17(1):93–101. doi: 10.1037/ser0000293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore K.E., Roberts W., Reid H.H., Smith K.M., Oberleitner L.M., McKee S.A. Effectiveness of medication assisted treatment for opioid use in prison and jail settings: A meta-analysis and systematic review. Journal of Substance Abuse Treatment. 2019;99:32–43. doi: 10.1016/j.jsat.2018.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherjee T.I., El-Bassel N. The perfect storm: COVID-19, mass incarceration and the opioid epidemic. The International Journal on Drug Policy. 2020;102819 doi: 10.1016/j.drugpo.2020.102819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2022. R: A language and environment for statistical computing.https://www.R-project.org/ (Accessed November 3 2022) [Google Scholar]
- Schuckit M.A. Treatment of opioid-use disorders. New England Journal of Medicine. 2016;375(4):357–368. doi: 10.1056/NEJMra1604339. [DOI] [PubMed] [Google Scholar]
- Schwartz R.P., Gryczynski J., O’Grady K.E., Sharfstein J.M., Warren G., Olsen Y.…Jaffe J.H. Opioid agonist treatments and heroin overdose deaths in Baltimore, Maryland, 1995–2009. American Journal of Public Health. 2013;103(5):917–922. doi: 10.2105/AJPH.2012.301049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma A., O’Grady K.E., Kelly S.M., Gryczynski J., Mitchell S.G., Schwartz R.P. Pharmacotherapy for opioid dependence in jails and prisons: Research review update and future directions. Substance Abuse and Rehabilitation. 2016;7:27. doi: 10.2147/SAR.S81602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon R., Rich J.D., Wakeman S.E. Springer; 2021. Treating opioid use disorder in correctional settings, treating opioid use disorder in general medical settings; pp. 77–90. [Google Scholar]
- Slavova S., Rock P., Bush H.M., Quesinberry D., Walsh S.L. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug and Alcohol Dependence. 2020;214 doi: 10.1016/j.drugalcdep.2020.108176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soares W.E., III, Melnick E.R., Nath B., D’Onofrio G., Paek H., Skains R.M.…Hoppe J.A. Emergency department visits for nonfatal opioid overdose during the COVID-19 pandemic across 6 US healthcare systems. Annals of Emergency Medicine. 2021;79(2):158–167. doi: 10.1016/j.annemergmed.2021.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp . StataCorp LLC; College Station, TX: 2021. Stata statistical software: Release 17.https://www.stata.com/ (Accessed November 3 2022) [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Opioid Treatment Program (OTP) guidance. 2020. https://www.samhsa.gov/sites/default/files/otp-guidance-20200316.pdf Accessed November 3 2022.
- Vermont Department of Corrections COVID-19 protocols and guidelines. 2020. https://doc.vermont.gov/content/covid-19-protocols-and-guidelines (Accessed July 10 2020)
- Volkow N.D., Frieden T.R., Hyde P.S., Cha S.S. Medication-assisted therapies—Tackling the opioid-overdose epidemic. New England Journal of Medicine. 2014;370(22):2063–2066. doi: 10.1056/NEJMp1402780. [DOI] [PubMed] [Google Scholar]
- Wakeman S.E., Green T.C., Rich J. An overdose surge will compound the COVID-19 pandemic if urgent action is not taken. Nature Medicine. 2020;26(6):819–820. doi: 10.1038/s41591-020-0898-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace M., Hagan L., Curran K.G., Williams S.P., Handanagic S., Bjork S.L., Davidson S.L., Lawrence R.T., McLaughlin J., Butterfield M. COVID-19 in correctional and detention facilities—United States, February–April 2020. MMWR. 2020:69. doi: 10.15585/mmwr.mm6919e1. [DOI] [PubMed] [Google Scholar]
- Weizman S., Perez P., Manoff I., Melissa B., El-Sabawi T. O'Neill Institute for National and Global Health Law at Gerogetown Law Center; 2021. National snapshot: Access to medications for opioid use disorder in U.S. jails and prisons. https://oneill.law.georgetown.edu/publications/national-snapshot-access-to-medications-for-opioid-use-disorder-in-u-s-jails-and-prisons/ (Accessed November 3 2022).
- Wilson N., Kariisa M., Seth P., Smith H., IV, Davis N.L. Drug and opioid-involved overdose deaths—United States, 2017–2018. MMWR. 2020;69(11):290. doi: 10.15585/mmwr.mm6911a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkelman T.N., Chang V.W., Binswanger I.A. Health, polysubstance use, and criminal justice involvement among adults with varying levels of opioid use. JAMA Network Open. 2018;1(3) doi: 10.1001/jamanetworkopen.2018.0558. e180558-e180558. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary tables