Abstract
Background
Osteoporosis is common among elderly patients and can result in vertebral fractures requiring surgical treatment. This study assessed clinical outcomes associated with spinal surgery in patients with osteoporosis/osteopenia with an additional focus on Asian patients.
Methods
A PRISMA-compliant systematic review and meta-analysis were conducted using the PubMed and ProQuest databases to identify articles published up to May 27, 2021, that included outcomes for patients with osteoporosis or osteopenia undergoing spinal surgery. Statistical analysis was conducted comparing rates of proximal junctional kyphosis (PJK)/proximal junctional failure (PJF), implant loosening, and revision surgery. A qualitative summary of Asian studies was also conducted.
Results
A total of 16 studies comprising 133,086 patients were included; among the 15 studies reporting rates of osteoporosis/osteopenia, 12.1% (16,127/132,302) of patients overall and 38.0% (106/279) of Asian patients (n=4 studies) had osteoporosis/osteopenia. The risks of PJK/PJF (relative risk [RR]=1.89; 95% confidence interval [CI]=1.22-2.92, p=0.004), screw loosening (RR=2.59; 95% CI=1.67-4.01, p<0.0001), and revision surgery (RR=1.65; 95% CI=1.13-2.42, p=0.010) were higher in patients with poor bone quality compared with those with healthy bone. In the qualitative review of Asian studies, all studies found that osteoporosis increased the risk of complications and/or revision for spinal surgery patients.
Conclusions
This systematic literature review and meta-analysis indicate that spinal surgery patients with compromised bone quality have more complications and higher healthcare utilization than those with normal bone quality. To our knowledge, this is the first study to focus on the pathophysiology and disease burden among Asian patients. Given the high rate of poor bone quality in this aging population, additional high-quality Asian studies, with uniform definitions and data reporting, are needed.
Keywords: Spinal Fusion, Osteoporosis, Spine Surgery, Degenerative Spine Disease, Asia-Pacific
Introduction
Osteoporosis predominantly affects older people and is a major risk factor for bone fractures1). Estimates of osteoporosis prevalence vary greatly, but a recent meta-analysis reported a global prevalence of 23.1% (95% confidence interval [CI] 19.8-26.9) in women and 11.7% (95% CI 9.6-14.1) in men, with the highest rates among Asian and African women (24.3% and 42.4%, respectively)2). The overall osteoporosis rate in Asia was estimated at 16.7%2), though a country-specific meta-analysis undertaken in China found an overall osteoporosis rate of 20%3), and a study of several industrialized countries found that the prevalence of osteoporosis in the spine or hip was highest in Japan (26.3%)4). Among osteoporotic fractures, vertebral fractures are extremely common5), with a lifetime risk of at least 15.6% in white women and 5.0% in white men6), and a true incidence that is likely higher given that many vertebral fractures are asymptomatic and never diagnosed7).
As populations age, the prevalence of osteoporosis and associated vertebral fractures is expected to increase8,9). In particular, between 2019 and 2050, the proportion of older people in Asia is projected to at least double10); as a result, vertebral fractures are likely to rise substantially in this region11). Currently, the rates of osteoporotic vertebral fractures in Asia are not well documented. A study in India using two population-based databases reported 42.7% and 27.7% of subjects had osteoporosis of the spine, respectively12), and a study conducted in Japan reported a prevalence of osteoporotic vertebral fractures of 17.8%13). Given the wide variation in reported rates and scarcity of data, additional studies of Asian osteoporotic patients are needed.
Although most symptomatic osteoporotic vertebral fractures require conservative management, a subset with spinal canal compromise and neurological deficit require surgery14). Osteoporosis increases the risk of complications during surgery15-17) and is associated with vertebral fractures after instrumentation, pseudoarthrosis, implant failure15), and a significant risk for revision surgery15,18-20).
Given the aging of the world population, particularly in the Asia-Pacific region, the accumulated evidence on the prevalence and clinical outcomes of surgical management of vertebral fractures in patients with osteoporosis can inform current challenges and future best practices. This systematic review and meta-analysis assessed clinical outcomes associated with surgical management of vertebral fractures in patients with concurrent osteoporosis or osteopenia compared with those with normal bone quality. Studies conducted in Asian countries were also qualitatively assessed to evaluate what is known about spinal surgery patients with osteoporosis compared with those without osteoporosis in this population.
Methods
The study protocol was conducted in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) statement21).
Literature search
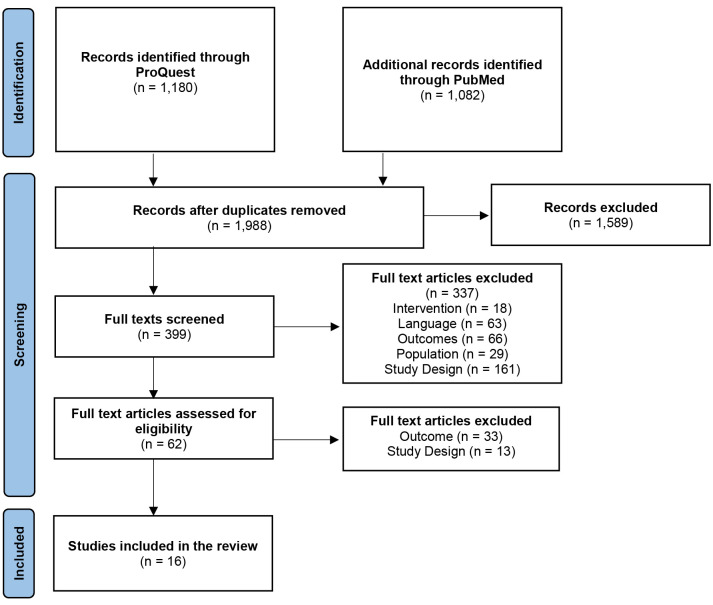
The literature search was performed with the PubMed (on May 27, 2021) and ProQuest (on March 29, 2021) databases. Detailed search terms are shown in Table S1. Duplicate articles were excluded. Two independent reviewers screened titles and abstracts, and, when necessary, full texts; disagreements were adjudicated by a third independent reviewer. Study selection followed the PRISMA flow diagram presented in Fig. 1.
Figure 1.
PRISMA study flow diagram.
Study selection criteria
Studies of adult (>18 years) patients with compromised bone quality (osteoporosis or osteopenia) undergoing spine surgery published between January 1, 2015, and May 27, 2021, in English, Chinese, Japanese, or Korean that reported one of the primary outcomes of interest by osteoporosis status were eligible for inclusion. Patients could be from any geographical region. Surgical management procedures included open reduction and internal fixation, conducted either at the thoracic, lumbar, thoracolumbar, lumbosacral, or sacral spine. Surgical management using instruments, implants or screws, vertebral body augmentation, kyphoplasty, stenting, and vertebroplasty were eligible for inclusion. All comparative studies were eligible for inclusion.
Studies were excluded for the following reasons: 1) patients did not have concurrent osteoporosis or osteopenia; 2) the study described conventional nonsurgical management or pharmacological or experimental treatments; 3) the study was not an appropriate article type (technical article, including animal, biomechanical or cadaver studies; case report; narrative review; editorial; opinion piece or letter; ongoing clinical trial; or conference abstract that did not report results on outcomes of interest); or 4) the study did not include comparative data between patients with and without osteoporosis.
Outcomes
The primary outcomes were the rate of proximal junctional kyphosis (PJK)/proximal junctional failure (PJF), implant-related complications/implant loosening, and revision surgery.
Data collection
Pre-determined items were extracted by one reviewer and independently checked for accuracy by a second reviewer. Reviewers were not blinded to the authors' names, institutions, journal of publication, or study results. Conflict resolution was done through discussion or by a third reviewer. The extracted data included: study reference, objective, study design, patient counts, demographics and comorbidities, indication for surgery, follow-up time, study groups and treatments, and complications (PJK, PJF, implant-related complications/implant loosening, revision surgeries).
Quality assessment
All included studies were rated by two independent researchers as low, good, or high-quality using the Evidence Level and Quality Guide from Johns Hopkins Nursing Evidence-Based Practice (Table S2)22). Quality was primarily determined by the principles of hierarchy of evidence and evidence-based practice guidelines. The quality of the study results within each level of evidence was also assessed. Publication bias was assessed for all outcomes with at least 10 data points using funnel plots.
Statistical analysis
A meta-analysis was performed to compare patients with and without osteoporosis on primary outcomes of interest. For binary outcomes, aggregate risks with 95% CIs were calculated and pooled risk ratios between cohorts with and without osteoporosis were estimated. The DerSimonian and Laird random-effects model was used when there was high heterogeneity (I2>50%); otherwise, fixed-effect models were applied. Statistical heterogeneity was assessed using I2 statistics. A p-value of <0.05 was considered statistically significant. Review Manager (RevMan) [Computer program]. Version 5.5, The Cochrane Collaboration, 2020 was used for statistical analysis.
Results
The literature searches yielded 2,262 citations (1,180 through ProQuest; 1,082 through PubMed). A total of 274 duplicate citations were removed, and 1,589 studies did not meet the inclusion and exclusion criteria. Full texts of the remaining studies were screened and 381 were excluded (Fig. 1). A total of 16 articles were deemed eligible and included in the analysis, including 11 cohort studies, two case series, one case-control study, one registry, and one economic study. One study reported lumbar levels rather than number of patients and reported that 72 of 881 lumbar levels had osteoporosis and 809 had either osteopenia or no osteoarthritis/osteopenia. Excluding this study, the 15 remaining studies comprised 132,302 patients, among whom 16,127 had a compromised bone quality condition (14,244 had osteoporosis and/or osteopenia, and 1,883 had osteopenia).
The study characteristics are presented in detail in Table 1. Most (n=9) studies were conducted in the US, followed by Korea (n=3), Japan (n=2), and Germany (n=2). The size of the patient population in the included studies ranged from 1823) to 116,74924). Fifteen studies reported data on sex (78,368 females and 54,718 males). The mean age at the time of surgery ranged from 3323) to 71.5 years25). Fifteen studies were graded as level III evidence while the remaining study had level IV23).
Table 1.
Characteristics of the Included Studies.
| Study | Study Design | Country | Level of Evidence | Patients (n) | Treatment | Female (n) | Mean Age at Surgery (Years) | Follow-up (Months, Unless Indicated) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | With Osteoporosis | With Osteopenia | Without Osteoporosis/
Osteopenia* |
||||||||
| Loffler et al. (2021) 28) | Case-Control | Germany# | III C | 46 | 13 | 20 | 13 | Primary surgery w/ semi-rigid instrumentation of the lumbar spine | 28 | 69.9 | Mean, 12.2 |
| Roberts et al. (2021) 16) | Cohort | USA# | III C | 4,743μ | 3,162μ | NR | 1,581μ | Posterior lumbar fusion w/ or w/out bisphosphonate | NR | NR | ≥12 |
| Sumiya et al. (2021) 29) | Cohort | Japan# | III C | 76 | 33 | NR | 43 | Long posterior spinal instrumented fixation at ≥3 levels | 29 | 69.2 | 2 days |
| Khalid et al. (2020) 36) | Cohort | USA# | III B | 5,169 | 1,723 | 1,723 | 1,723 | Single-level lumbar fusion | 4,413 | NR | 24 |
| Park et al. (2020) 26) | Cohort | Korea# | III B | 63 | 18 | NR | 45 | Long instrumented fusion stopping at thoracolumbar junction in adult spinal deformity | 57 | 67.2 | Mean, 51.7 |
| Rentenberger et al. (2020) 33) | Cohort | USA# | III C | 133 | 33 | 58 | 42 | Lateral lumbar interbody fusion | 82 | 67.5 | ≥12 |
| Rodriguez-Fontan et al. (2020) 17) | Cohort | Germany# | III C | 80 | 28 | NR | 52 | Posterior instrumented fusion with or without Mersilene tape | 51 | 62.3 | 24 |
| Sharma et al. (2020) 24) | Economic | USA# | III B | 116,749 | 7,145 | NR | 109,604 | Lumbar fusion | 69,421 | 57 | ≥24 |
| Shimizu et al. (2020) 23) | Case Series | USA | IV C | 18 | 1 | NR | 17 | Pre-operative halo-gravity traction; definitive fusion by 1 or 2-staged posterior-alone approach w/ osteotomies depending on severity | 7 | 33 | 3 |
| St Jeor et al. (2020) 31) | Cohort | USA# | III B | 140 | 14 | 82 | 44 | Primary posterior thoracolumbar or lumbar fusion | 88 | 68.8 | Mean, 2.1 years (minimum 1 year) |
| Varshneya et al. (2020) 25) | Cohort | USA# | III B | 2,564 | 971 | NR | 1,593 | Thoracolumbar adult spinal deformity surgery | 1,755 | 71.5 | 24 |
| Park et al. (2019) 30) | Cohort | Korea | III B | 881 lumbar levels (784 patients) | 72 lumbar levels (T-score≤ −2.5) ǂ | Combined with No Osteoporosis patientsǂ | 809 lumbar levels (T-score>−2.5) Φ | Transforaminal lumbar interbody fusion with a bilateral pedicle screw | 483 | 63.3 | 18 |
| Cho et al. (2018) 15) | Cohort | Korea | III B | 86 | 31 (T-score≤ −2.5) | NR | 55 (T-score≥ −1.0) | Posterior lumbar interbody fusion w/ pedicle screw fixation followed by interbody polyetheretherketone cage | 60 | 66 | >24 |
| Uei et al. (2018) 34) | Cohort | Japan# | III C | 54 | 24 (Osteoporosis or Osteopenia) | Combined with Osteoporosis patients | 30 | Spinal deformity patients ≥65 years treated with correction and fusion surgery of ≥4 levels | 50 | NR | Mean, 38 |
| Formby et al. (2016) 27) | Case Series | USA | III B | 88 | 18 | NR | 70 | Instrumented transforaminal lumbar interbody fusion w/ pedicle screw instrumentation with polyetheretherketone cage | 34 | NR | Mean, 35.8 |
| Puvanesarajah et al. (2016) 32) | Registry | USA | III C | 2,293 | 1,030 | NR | 1,263 | Posterolateral fusion of ≥8 levels | 1,810 | <75, n=1,676; ≥75, n=617 | 5 years |
*In studies that do not include osteopenia patients (all except for Park et al., 2019), this group consists of patients without osteoporosis only.
#Country inferred through author’s affiliation.
ǂT-score, a measure of bone density measured in standard deviations from the average bone density of healthy same-sex 30-year-olds.
ΦT-score between 1 and 2.5 standard deviations below the young adult mean (−1 to −2.5) is considered low bone density, or osteopenia.
μNumbers following matching of three groups: osteoporosis patients w/ and without bisphosphonate use, and non-osteoporosis patients without bisphosphonate use.
NR, not reported; USA, United States of America
Primary outcomes
PJK and PJF
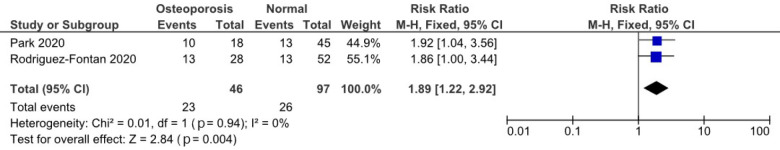
Four studies reported rates of PJK and PJF (Table 2). Of these studies, two had sufficient data to compare the risk for PJK/PJF between those with and without compromised bone quality17,26). A forest plot of the random-effects model is shown in Fig. 2. The studies exhibited low heterogeneity (I2=0%). Those with compromised bone quality were at higher risk for PJK and PFK (relative risk [RR]=1.89; 95% CI=1.22-2.92, p=0.004) compared with those with normal bone quality.
Table 2.
Studies Reporting Proximal Junctional Kyphosis and Failure.
| Study | Study Groups | Proximal Junctional Kyphosis
n/N (%) |
Additional Analysis | Proximal Junctional Failure
n/N (%) |
Additional Analysis |
|---|---|---|---|---|---|
| Park et al. (2020) 26) | Osteoporosis
No Osteoporosis |
NR
13/45 (28.9) |
NR | 10/18 (55.6)
NR |
NR |
| Rodriguez-Fontan et al. (2020) 17) | Osteoporosis | 13/28 (46.4)
(Both PJK and PJF) |
Osteoporosis vs. No
Osteoporosis, OR 2.6 (95% CI 0.9–6.8, p=0.08) |
Values combined with PJK | Values combined with PJK |
| No Osteoporosis | 13/52 (25.0)
(Both PJK and PJF) |
||||
| Shimizu et al. (2020) 23) | Osteoporosis
No Osteoporosis |
0/1 (0.0)
3/17 (17.6) |
NR | NR | NR |
| St Jeor et al. (2020) 31) | Osteoporosis | 5/14 (35.7)
(Pooled rate of ORCs*) |
Osteoporosis vs. No
Osteoporosis/Osteopenia, p=0.138 Osteoporosis vs. No Osteoporosis/Osteopenia, p=0.005 |
NR | NR |
| Osteopenia | 33/82 (40.2)
(Pooled rate of ORCs*) |
||||
| No Osteoporosis/
Osteopenia |
7/44 (15.9)
(Pooled rate of ORCs*) |
*Osteoporosis-related complications (ORCs) are defined as one of the following: revision surgery, compression fracture, proximal junctional kyphosis, pseudarthrosis, accelerated adjacent segment disease, or instrumentation failure (including screw loosening).
NR, not reported; OR, odds ratio; ORC, osteoporosis-related complication; PJF, proximal junctional failure; PJK, proximal junctional kyphosis
Figure 2.
Risk ratio for proximal junction kyphosis and failure in patients with versus without osteoporosis/osteopenia.
Implant-related complications/screw loosening
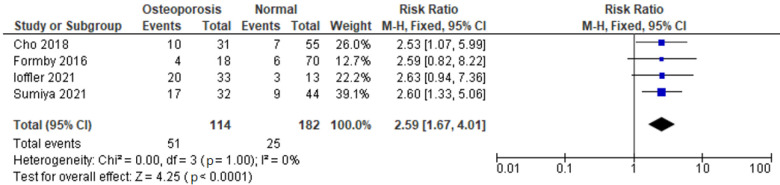
Seven studies reported rates of implant-related complications (Table 3)15,16,27-31). Four of these studies had sufficient data to compare rates of screw loosening by bone quality15,27-29). A forest plot of the random-effects model for the screw loosening analysis is presented in Fig. 3. The studies have low heterogeneity (I2=0%). Those with compromised bone quality were over two times more likely (RR=2.59; 95% CI=1.67-4.01, p<0.0001) to have screw loosening compared with those with normal bone quality.
Table 3.
Studies Reporting Implant-related Complications, Including Screw Loosening by Osteoporosis/osteopenia Status.
| Study | Study Groups | Implant-related Complications
n/N (%) |
Additional Analysis |
|---|---|---|---|
| Loffler et al. (2021) 28) | Osteoporosis | 11/13 (84.6) (screw loosening) | NR |
| Osteopenia | 9/20 (45.0) (screw loosening) | ||
| No Osteoporosis/Osteopenia | 3/13 (23.1) (screw loosening) | ||
| Roberts et al. (2021) 16) | Osteoporosis
No Osteoporosis |
192/3,162 (6.1) (instrumentation failure)
76/1,581 (4.8) (instrumentation failure) |
Osteoporosis w/ bisphosphonate vs.
No Osteoporosis, OR 1.20 (95% CI 0.88–1.65); Osteoporosis w/out bisphosphonate vs. No Osteoporosis, OR 1.35 (1.00–1.84) |
| Sumiya et al. (2021) 29) | Osteoporosis
No Osteoporosis |
17/33 (51.5) (screw pull-out)
9/43 (20.9) (screw pull-out) |
NR |
| St Jeor et al. (2020) 31) | Osteoporosis | 5/14 (35.7) (pooled rate of ORCs*) | Osteoporosis vs. No Osteoporosis/
Osteopenia, p=0.138 Osteopenia vs. No Osteoporosis/ Osteopenia, p=0.005 |
| Osteopenia | 33/82 (40.2) (pooled rate of ORCs*) | ||
| No Osteoporosis/Osteopenia | 7/44 (15.9) (pooled rate of ORCs*) | ||
| Park et al. (2019) 30) | Osteoporosis
(T-score≤−2.5) # |
7/72 lumbar levels (9.7%) (CM w/o subsidence)
13/72 lumbar levels (18.1%) (CM w/ subsidence), 9/72 lumbar levels (12.5%) (CR) |
Osteoporosis was a risk factor for:
CM w/out subsidence, OR 8.73, p<0.001; CM w/ subsidence, OR 5.77, p<0.001; CR, OR 7.86, p<0.001 |
| No Osteoporosis/Osteopenia
(T-score≤−2.5) ǂ |
13/809 lumbar levels (1.6%) (CM w/o subsidence),
23/809 (0.1%) (CM w/ subsidence), 8/809 lumbar levels (1.0%) (CR) |
||
| Cho et al. (2018) 15) | Osteoporosis
(T-score≤−2.5) # No Osteoporosis (T-score≥−1.0) # |
10/31 (32.3) (screw loosening)
17/24 (70.8) (cage subsidence) 7/55 (12.7) (screw loosening) 9/39 (23.1) (cage subsidence) |
Osteoporosis vs. No Osteoporosis,
screw loosening, p=0.029; cage subsidence, p<0.001 |
| Formby et al. (2016) 27) | Osteoporosis
No Osteoporosis |
4/18 (22.2) (pedicle screw loosening)
6/70 (8.6) (pedicle screw loosening) |
Osteoporosis vs. No Osteoporosis
p=0.14 |
*Osteoporosis-related complications (ORCs) were defined as one of the following categories: revision surgery, compression fracture, proximal junctional kyphosis, pseudarthrosis, accelerated adjacent segment disease, or instrumentation failure (including screw loosening).
#T-score, a measure of bone density measured in standard deviations from the average bone density of healthy same-sex young adults.
ǂT-score between 1 and 2.5 standard deviations below the young adult mean is considered low bone density, or osteopenia.
CI, confidence interval; CM, cage migration; CR, cage retropulsion; OR, odds ratio; ORC, osteoporosis-related complications; NR, not reported
Figure 3.
Forest plot for screw loosening in patients with versus without osteoporosis/osteopenia.
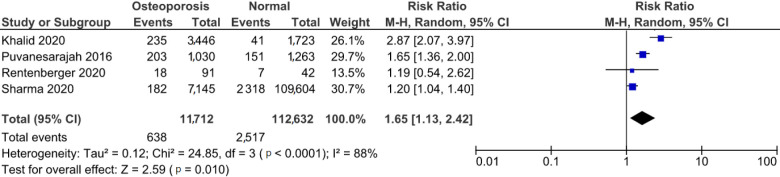
Revision surgery
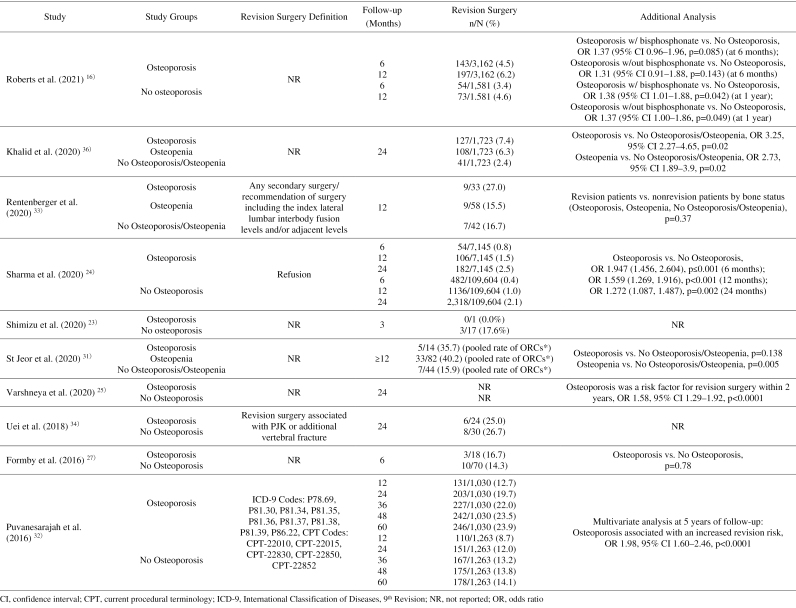
Ten studies reported rates of revision surgeries by osteoporosis status (Table 4)16,23-25,27,32-36). Four studies compared the risk for revision surgery by bone quality24,32,33,36). A forest plot of the random-effects model for the revision analysis is presented in Fig. 4. The studies exhibited high heterogeneity (I2=88%). The risk for revision surgery was higher among those with compromised bone quality than for those with normal bone quality (RR=1.65; 95% CI=1.13-2.42, p=0.010).
Table 4.
Studies Reporting Revision Surgery.
Figure 4.
Forest plot for revision surgery in patients with and without osteoporosis/osteopenia.
Outcomes among asian patients
Five of the included studies were conducted in Asian countries. As noted above, one study conducted in Korea reported an osteoporosis rate of 8.2% (72/881) among lumbar levels30). Among the four studies that reported rates among patients, 38.0% of Asian spinal surgery patients had osteoporosis (none of the studies reported rates of osteopenia). All five studies found that osteoporosis increased the risk of complications and/or revision for spinal surgery patients15,26,29,34). Three of the studies focused on screw loosening or implant failure (Table 3). The study by Sumiya et al. on Japanese patients retrospectively analyzed the risk of pedicle screw pull-out in 76 patients (746 screws) who underwent at least triple-level posterior fixation for thoracic or lumbar spinal injury, spinal metastasis, or pyogenic spondylitis. By comparing intraoperative cone-beam computed tomography scans with two-day postoperative computed tomography scans, the authors found that patients with screw pull-out were more likely to have osteoporosis than those without (17 vs. 15 patients, p=0.0038)29). Similarly, Park et al. found that among 784 Korean patients undergoing transforaminal lumbar interbody fusion, osteoporosis was a significant risk factor for cage migration with subsidence (OR 5.77, p<0.001), cage migration without subsidence (OR 8.73, p<0.001), and cage retropulsion (OR 7.86, p<0.001)30). Cho et al. also evaluated the impact of osteoporosis on the clinical and radiological outcomes among Korean patients. Results from 86 Korean patients at least 2 years after undergoing one-level posterior lumbar interbody fusion indicated that even though osteoporosis patients had higher cage subsidence (65.4% vs. 17.6%, p<0.001) and pedicle screw loosening rates (32.3% vs. 12.7%, p<0.029), these did not significantly affect the fusion rate (p=0.727)15).
Two studies in Asia focused on patients with adult spinal deformity (ASD)26,34). Uei et al. examined 54 elderly Japanese with ASD treated with correction and fusion at four or more levels and found that elderly patients who required revision surgery within 2 years had significantly lower mean bone densities of vertebral bodies at T8 (158 vs. 213 Hounsfield units, p=0.03) and T9 (158 vs. 203 Hounsfield units, p=0.02) (Table 4)34). Park et al. investigated the risk factors for PJF following long instrumented fusion stopping at the thoracolumbar junction (TLJ) in Korean ASD patients to determine which cases are suitable for TLJ stop without increasing the risk for PJF (Table 2). Osteoporosis was identified as a significant risk factor for PJF in patients with TLJ as the uppermost instrumented vertebra (OR 4.459, p=0.033), making this level unsuitable for osteoporotic patients26).
Discussion
According to this systematic review and meta-analysis, poor bone quality is associated with worse outcomes after spinal surgery. Compared with patients without osteoporosis/osteopenia, those with osteoporosis/osteopenia undergoing spinal surgery are at higher risk of PJK/PJF, screw loosening, and revision surgery. Additionally, our review of Asian studies underscores the burden of poor bone quality in this population and highlights the need for further study and focus on these patients. Similar to previous studies37,38), we found that many patients undergoing spinal surgery have compromised bone quality. Bjerke et al. reported that among 140 patients undergoing primary posterior thoracolumbar or lumbar fusion, 22.7% had normal bone density, 32.9% had osteopenia, and 50.0% had osteoporosis37). Given the high proportion of patients with poor bone quality undergoing spinal surgery, it is critical to understand how outcomes differ among these patients. Our results indicate that in addition to a high risk for primary surgery, osteoporotic patients are also more likely to need revision surgery. Indeed, the increased rate of revision surgery is quite notable; Khalid et al. found that patients with compromised bone quality were almost three times more likely (odd ratio 2.73, 95% CI 1.89-3.94) to need revision surgery than those with normal bone quality36). Additionally, the increased risk for screw loosening and PJK//PJF among these patients further underscores the increased risk for additional surgery as both are associated with pain and neurological issues that can require reoperation39-45). Costs associated with both primary and revision surgery can result in a heavy and increasing economic burden46). According to a report published by the Health Insurance Review and Assessment Service in South Korea, osteoporosis-related medical costs increased by 35% from 2007 to 201147). These costs will likely grow substantially as the population ages.
To our knowledge, this is the first review to focus on the pathophysiology of poor bone quality among the Asian population overall. We found that the rate of osteoporosis was higher overall in studies conducted in Asian countries compared with that in all the included studies. This is consistent with other studies that have suggested that regional and country-specific osteoporosis prevalence varies greatly4,5,48). A comprehensive review of prevalence rates in several industrialized countries in people above 50 years old documented the wide variation in disease burden with rates of 26.3% in Japan, 21% in the US, 14.3% in Germany, 9.9% in France, 9.7% in Italy, 7.8% in the United Kingdom, 6.3% in Spain, 2.6% in Canada, and 2% in Australia4). The prevalence of osteoporosis in many parts of Asia is not well-documented, but according to a meta-analysis, that in China from 2003 to October 2015 was 15.3% in men and 25.4% in women3). Given the size and aging of the Asian population worldwide, studies have projected that by the year 2050, Asian patients will account for more than 50% of global osteoporotic hip fractures49,50). Moreover, the International Osteoporosis Foundation reported that osteoporosis has been greatly underdiagnosed in Asia, particularly in rural areas12). Additionally, almost all Asian countries fall far below the World Health Organization recommendations for appropriate calcium intake (between 1,000 and 1,300 mg/day); for example, the calcium intake for Malaysia, the Philippines, and India remains <500 mg/day12). The findings from the studies conducted in Asian countries included in our review underscore the fact that elderly patients in the Asia-Pacific region are a high-risk population for osteoporosis-related ailments. Sufficient studies were not available to perform a meta-analysis on the Asian population overall, highlighting the need for additional research on this population to guide policy development on prevention and treatment in this region.
Limitations
This study had multiple limitations, including incomplete or nonstandardized outcome reporting in the included publications, which limited the number of studies included in the meta-analyses. A second limitation was the relatively low quality of published studies reporting the outcomes of interest; the included studies were cohort studies, which may suffer from selection bias. Third, a lack of large-scale population-based studies and the lack of osteoporosis-oriented studies limited the scope of generalizations and comparisons. Fourth, additional potential complications (distal junctional kyphosis, distal junctional failure, adjacent level fracture, etc.) that may be associated with compromised bone quality were not included in this study, as the relationship between these outcomes and compromised bone quality may be difficult to determine due to limited data. Finally, in many large-scale retrospective studies, osteoporosis was part of multivariate analysis, but further subgroup analysis was not presented. The results of such studies should be interpreted with caution.
Conclusions
According to this systematic review and meta-analysis, patients with poor bone quality undergoing spinal surgery are at higher risk for complications and healthcare utilization than those with normal bone quality. A focus specifically on patients in Asian countries underscored that this patient population is at high risk for osteoporosis-related complications. High-quality studies with uniform definitions and data reporting are needed, particularly among Asian patients, to confirm the study findings and inform strategies for prevention of postoperative complications.
Conflicts of Interest: MO, AR, and HP are employed by Johnson & Johnson.
Sources of Funding: This work was supported by Johnson & Johnson.
Author Contributions: All authors made substantial contributions to the conception or design of the work, or the acquisition, analysis, or interpretation of data for the work. All authors drafted the work or revised it critically for important intellectual content, provided final approval of the version to be published, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethical Approval and Patient Consent: Institutional Review Board approval and patient consent are not required for this study type.
Data Availability: All data relevant to the study are included in the article or uploaded as supplementary information.
Supplementary Materials
Acknowledgement
The authors acknowledge ClinChoice, Inc. for assistance with data analysis and systematic literature review, and Superior Medical Experts for manuscript drafting and editorial assistance.
References
- 1.Cosman F, de Beur SJ, LeBoff MS, et al. Clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salari N, Ghasemi H, Mohammadi L, et al. The global prevalence of osteoporosis in the world: a comprehensive systematic review and meta-analysis. J Orthop Surg Res. 2021;16(1):609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen P, Li Z, Hu Y. Prevalence of osteoporosis in China: a meta-analysis and systematic review. BMC Public Health. 2016;16(1):1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wade SW, Strader C, Fitzpatrick LA, et al. Estimating prevalence of osteoporosis: examples from industrialized countries. Arch Osteoporos. 2014;9:182. [DOI] [PubMed] [Google Scholar]
- 5.Melton JL, 3rd. Epidemiology of spinal osteoporosis. Spine. 1997;22(24 Suppl):2S-11S. [DOI] [PubMed] [Google Scholar]
- 6.Melton LJ, 3rd, Chrischilles EA, Cooper C, et al. Perspective. How many women have osteoporosis? J Bone Miner Res. 1992;7(9):1005-10. [DOI] [PubMed] [Google Scholar]
- 7.Cooper C, Atkinson EJ, Kotowicz M, et al. Secular trends in the incidence of postmenopausal vertebral fractures. Calcif Tissue Int. 1992;51(2):100-4. [DOI] [PubMed] [Google Scholar]
- 8.Reginster JY, Burlet N. Osteoporosis: a still increasing prevalence. Bone. 2006;38(2 Suppl 1):S4-9. [DOI] [PubMed] [Google Scholar]
- 9.Schousboe JT. Epidemiology of vertebral fractures. J Clin Densitom. 2016;19(1):8-22. [DOI] [PubMed] [Google Scholar]
- 10.United Nations Department of Economic and Social Affairs. World population ageing 2019: highlights (ST/ESA/SER.A/430). New York, NY, USA: United Nations Department of Economic and Social Affairs; 2019. [Google Scholar]
- 11.Sambrook P, Cooper C. Osteoporosis. Lancet. 2006;367(9527):2010-8. [DOI] [PubMed] [Google Scholar]
- 12.Mithal A, Bansal B, Kyer CS, et al. The Asia-Pacific regional audit-epidemiology, costs, and burden of osteoporosis in India 2013: a report of international osteoporosis foundation. Indian J Endocrinol Metab. 2014;18(4):449-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Horikawa K, Kasai Y, Yamakawa T, et al. Prevalence of osteoarthritis, osteoporotic vertebral fractures, and spondylolisthesis among the elderly in a Japanese village. J Orthop Surg (Hong Kong). 2006;14(1):9-12. [DOI] [PubMed] [Google Scholar]
- 14.Patil S, Rawall S, Singh D, et al. Surgical patterns in osteoporotic vertebral compression fractures. Eur Spine J. 2013;22(4):883-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cho JH, Hwang CJ, Kim H, et al. Effect of osteoporosis on the clinical and radiological outcomes following one-level posterior lumbar interbody fusion. J Orthop Sci. 2018;23(6):870-7. [DOI] [PubMed] [Google Scholar]
- 16.Roberts S, Formanek B, Buser Z, et al. The impact of bisphosphonates on postoperative complication rates in osteoporotic patients undergoing posterior lumbar fusion. Eur Spine J. 2021;30(5):1329-36. [DOI] [PubMed] [Google Scholar]
- 17.Rodriguez-Fontan F, Reeves BJ, Noshchenko A, et al. Strap stabilization for proximal junctional kyphosis prevention in instrumented posterior spinal fusion. Eur Spine J. 2020;29(6):1287-96. [DOI] [PubMed] [Google Scholar]
- 18.Halvorson TL, Kelley LA, Thomas KA, et al. Effects of bone mineral density on pedicle screw fixation. Spine (Phila Pa 1976). 1994;19(21):2415-20. [DOI] [PubMed] [Google Scholar]
- 19.Paxinos O, Tsitsopoulos PP, Zindrick MR, et al. Evaluation of pullout strength and failure mechanism of posterior instrumentation in normal and osteopenic thoracic vertebrae. J Neurosurg Spine. 2010;13(4):469-76. [DOI] [PubMed] [Google Scholar]
- 20.Zindrick MR, Wiltse LL, Widell EH, et al. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986;203(203):99-112. [PubMed] [Google Scholar]
- 21.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Newhouse R, Dearholt S, Poe S, et al. Evidence-based practice: a practical approach to implementation. J Nurs Adm. 2005;35(1):35-40. [DOI] [PubMed] [Google Scholar]
- 23.Shimizu T, Lenke LG, Cerpa M, et al. Preoperative halo-gravity traction for treatment of severe adult kyphosis and scoliosis. Spine Deform. 2020;8(1):85-95. [DOI] [PubMed] [Google Scholar]
- 24.Sharma M, John K, Dietz N, et al. Factors impacting outcomes and health care utilization in osteoporotic patients undergoing lumbar spine fusions: a MarketScan database analysis. World Neurosurg. 2020;141:e976-88. [DOI] [PubMed] [Google Scholar]
- 25.Varshneya K, Jokhai RT, Fatemi P, et al. Predictors of 2-year reoperation in Medicare patients undergoing primary thoracolumbar deformity surgery. J Neurosurg Spine. 2020;33(5):572-6. [DOI] [PubMed] [Google Scholar]
- 26.Park SJ, Lee CS, Park JS, et al. Should thoracolumbar junction be always avoided as upper instrumented vertebra in long instrumented fusion for adult spinal deformity?: risk factor analysis for proximal junctional failure. Spine. 2020;45(10):686-93. [DOI] [PubMed] [Google Scholar]
- 27.Formby PM, Kang DG, Helgeson MD, et al. Clinical and radiographic outcomes of transforaminal lumbar interbody fusion in patients with osteoporosis. Glob Spine J. 2016;6(7):660-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Löffler MT, Sollmann N, Burian E, et al. Opportunistic osteoporosis screening reveals low bone density in patients with screw loosening after lumbar semi-rigid instrumentation: a case-control study. Front Endocrinol (Lausanne). 2020;11:552719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sumiya S, Fukushima K, Kurosa Y, et al. Comparative analysis of clinical factors associated with pedicle screw pull-out during or immediately after surgery between intraoperative cone-beam computed tomography and postoperative computed tomography. BMC Musculoskelet Disord. 2021;22(1):55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Park MK, Kim KT, Bang WS, et al. Risk factors for cage migration and cage retropulsion following transforaminal lumbar interbody fusion. Spine J. 2019;19(3):437-47. [DOI] [PubMed] [Google Scholar]
- 31.St Jeor JD, Jackson TJ, Xiong AE, et al. Average lumbar Hounsfield units predicts osteoporosis-related complications following lumbar spine fusion. Glob Spine J. 2020;12(5):851-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Puvanesarajah V, Shen FH, Cancienne JM, et al. Risk factors for revision surgery following primary adult spinal deformity surgery in patients 65 years and older. J Neurosurg Spine. 2016;25(4):486-93. [DOI] [PubMed] [Google Scholar]
- 33.Rentenberger C, Okano I, Salzmann SN, et al. Perioperative risk factors for early revisions in stand-alone lateral lumbar interbody fusion. World Neurosurg. 2020;134:e657-63. [DOI] [PubMed] [Google Scholar]
- 34.Uei H, Tokuhashi Y, Maseda M, et al. Exploratory analysis of predictors of revision surgery for proximal junctional kyphosis or additional postoperative vertebral fracture following adult spinal deformity surgery in elderly patients: a retrospective cohort study. J Orthop Surg Res. 2018;13(1):252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.St Jeor JD, Jackson TJ, Xiong AE, et al. Osteoporosis in spine surgery patients: what is the best way to diagnose osteoporosis in this population? Neurosurg Focus. 2020;49(2):E4. [DOI] [PubMed] [Google Scholar]
- 36.Khalid SI, Nunna RS, Maasarani S, et al. Association of osteopenia and osteoporosis with higher rates of pseudarthrosis and revision surgery in adult patients undergoing single-level lumbar fusion. Neurosurg Focus. 2020;49(2):E6. [DOI] [PubMed] [Google Scholar]
- 37.Bjerke BT, Zarrabian M, Aleem IS, et al. Incidence of osteoporosis-related complications following posterior lumbar fusion. Glob Spine J. 2018;8(6):563-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Paz RD, Henriquez MS, Melian KA, et al. Prevalence of poor bone quality in patients undergoing spine surgery: a comprehensive approach. Glob Spine J. 2021;12(7):1412-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim HJ, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis results in inferior SRS pain subscores in adult deformity patients. Spine. 2013;38(11):896-901. [DOI] [PubMed] [Google Scholar]
- 40.Kim HJ, Bridwell KH, Lenke LG, et al. Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine (Phila Pa 1976). 2014;39(9):E576-80. [DOI] [PubMed] [Google Scholar]
- 41.Hart R, McCarthy I, O'brien M, et al. Identification of decision criteria for revision surgery among patients with proximal junctional failure after surgical treatment of spinal deformity. Spine (Phila Pa 1976). 2013;38(19):E1223-7. [DOI] [PubMed] [Google Scholar]
- 42.Nguyen NL, Kong CY, Hart RA. Proximal junctional kyphosis and failure-diagnosis, prevention, and treatment. Curr Rev Musculoskelet Med. 2016;9(3):299-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hart RA, McCarthy I, Ames CP, et al. Proximal junctional kyphosis and proximal junctional failure. Neurosurg Clin N Am. 2013;24(2):213-8. [DOI] [PubMed] [Google Scholar]
- 44.Galbusera F, Volkheimer D, Reitmaier S, et al. Pedicle screw loosening: a clinically relevant complication? Eur Spine J. 2015;24(5):1005-16. [DOI] [PubMed] [Google Scholar]
- 45.Röllinghoff M, Schlüter-Brust K, Groos D, et al. Midrange outcomes in 64 consecutive cases of multilevel fusion for degenerative diseases of the lumbar spine. Orthop Rev (Pavia). 2010;2(1):e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee CK, Choi SK, An SB, et al. Influence of osteoporosis following spine surgery on reoperation, readmission, and economic costs: an 8-year nationwide population-based study in Korea. World Neurosurg. 2021;149:e360-8. [DOI] [PubMed] [Google Scholar]
- 47.Yoo JE, Park HS. Prevalence and associated risk factors for osteoporosis in Korean men. Arch Osteoporos. 2018;13(1):88. [DOI] [PubMed] [Google Scholar]
- 48.O'Neill TW, Felsenberg D, Varlow J, et al. The prevalence of vertebral deformity in European men and women: the European Vertebral Osteoporosis Study. J Bone Miner Res. 1996;11(7):1010-8. [DOI] [PubMed] [Google Scholar]
- 49.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7(5):407-13. [DOI] [PubMed] [Google Scholar]
- 50.Cooper C, Campion G, Melton LJ, 3rd. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2(6):285-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.