STRUCTURED ABSTRACT
BACKGROUND:
Although 50 years represents middle-age among uninfected individuals, studies have shown that PWH begin to demonstrate elevated risk for serious falls and fragility fractures in the sixth decade; the proportions of these outcomes attributable to modifiable factors are unknown.
METHODS:
We analyzed 21,041 older PWH on ART from the Veterans Aging Cohort Study from 01/01/2010 through 09/30/2015. Serious falls were identified by Ecodes and a machine-learning algorithm applied to radiology reports. Fragility fractures (hip, vertebral, and upper arm) were identified using ICD9 codes. Predictors for both models included a serious fall within the past 12 months, body mass index, physiologic frailty (VACS Index 2.0), illicit substance and alcohol use disorders, and measures of multimorbidity and polypharmacy. We separately fit multivariable logistic models to each outcome using generalized estimating equations. From these models, the longitudinal extensions of average attributable fraction (LE-AAF) for modifiable risk factors were estimated.
RESULTS:
Key risk factors for both outcomes included physiologic frailty (VACS Index 2.0) [serious falls (15%; 95% CI 14%–15%); fractures (13%; 95% CI 12%–14%)], a serious fall in the past year [serious falls (7%; 95% CI 7%–7%); fractures (5%; 95% CI 4%–5%)], polypharmacy [serious falls (5%; 95% CI 4%–5%); fractures (5%; 95% CI 4%–5%)], an opioid prescription in the past month [serious falls (7%; 95% CI 6%–7%); fractures (9%; 95% CI 8%–9%)], and diagnosis of alcohol use disorder [serious falls (4%; 95% CI 4%–5%); fractures (8%; 95% CI 7%–8%)].
CONCLUSIONS:
This study confirms the contributions of risk factors important in the general population to both serious falls and fragility fractures among older PWH. Successful prevention programs for these outcomes should build on existing prevention efforts while including risk factors specific to PWH.
Keywords: falls, fragility fractures, HIV, LE-AAF
INTRODUCTION
Although geriatrics has historically emphasized healthcare for persons 65 years and older, clinical research posits that the geriatric life-phase of persons living with HIV (PWH) begins earlier.1–6 Among older PWH (50+ years), falls and fragility fractures are key comorbidities.7–10 Research suggests that older PWH experience a higher prevalence of falls and fragility fractures than the general population.9,11–13 Many of these occur among older PWH who are chronologically middle-aged and in their most economically productive years.14,15 These events consequently result in financial burdens from health care costs and lost income and can lead to social isolation.16 If we are to preserve quality of life as PWH age, effective interventions to reduce falls and fragility fractures in this population are critically needed.
The damage wrought by these outcomes is not restricted to older PWH. In the general population, one in three women and one in five men over the age of 50 will break a bone due to osteoporosis.17,18 In addition to the short-term pain, functional impairment, and mortality risks associated with a fracture, longer-term consequences include chronic pain, permanent disability and long-term institutionalization.19–21 These fragility fractures are more costly than heart attack, stroke and breast cancer combined,22 and the majority result from a fall.23
While there are many interventions targeting the prevention of falls and fragility fractures among older adults in the general population, there are few published reports of interventions tailored to the needs of older PWH. Moreover, prevention programs designed for older adults in the general population may not address key risk factors among PWH. For example, the CDC’s STEADI program to reduce fall risk targets exercise, polypharmacy, home hazards, orthostatic hypotension, visual acuity, vitamin D intake, and footwear.24 While all of these factors are likely important concerns among older PWH, other key risk factors such as alcohol and substance use are not addressed.7
There are many modifiable risk factors that might serve as the basis for interventions. However, we have yet to objectively assess which of these modifiable risk factors account for the greatest proportion of serious falls and fragility fractures among older PWH. To address this gap, we used the Longitudinal Extension of the Average Attributable Fraction (LE-AAF) technique to identify the longitudinal proportional contributions to serious falls (those occurring in the community that were serious enough to require a visit with a healthcare provider) and fragility fractures attributable to individual conditions. Most research using LE-AAF has focused on mortality as an outcome, but a growing number of studies have used outcomes such as pneumonia25 and patient-reported outcomes among older patients.26 To our knowledge, this is the first analysis to use serious falls and fragility fractures as outcomes in a LE-AAF based analysis. Using LE-AAF, our goal was to separately quantify the respective proportions of these outcomes attributable to modifiable risk factors. As serious falls are a key risk factor for fragility factors,7 developing interventions that simultaneously reduce risk of serious falls and fragility fractures will likely have a greater impact on patient health than targeting them separately.
METHODS
Cohort
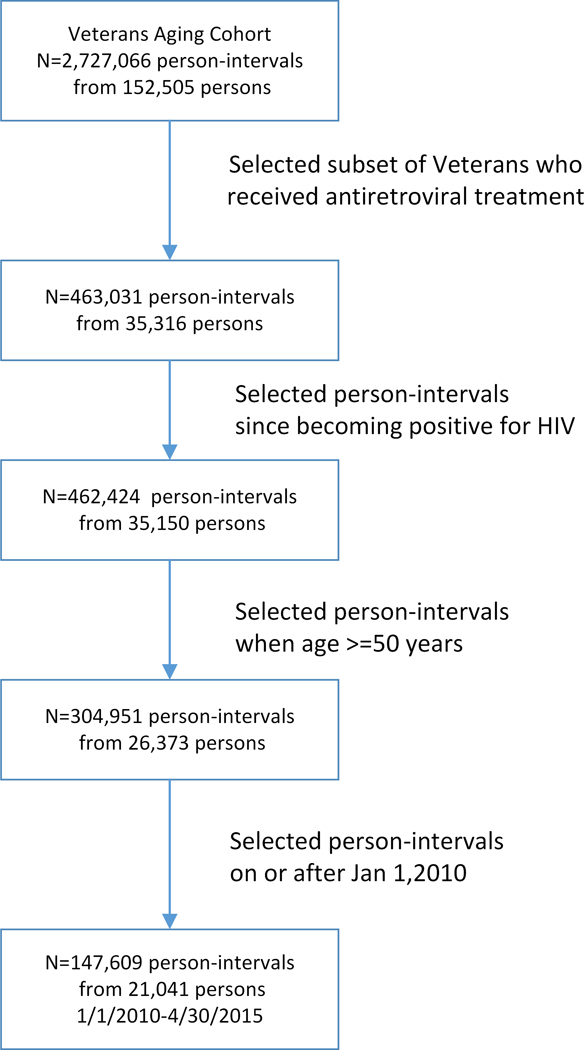
We used data from the Veterans Aging Cohort Study (VACS), an electronic health record (EHR)-based cohort that includes all individuals diagnosed with HIV who receive care within the Veterans Health Administration (VA).27 We included PWH on ART 50+ years of age who presented for care and were followed from 01/01/2010 through 09/30/2015 (Figure 1).
Figure 1.
Derivation of Sample
Observation time
Observations consisted of six-month person-intervals beginning January 1, 2010, for participants enrolled prior to 2010 and from the date of enrollment for all others.
Outcomes
The first outcome of interest was occurrence of a serious fall identified either by external cause of injury codes (Ecodes) (E880.X, E881.X, E884.X, E885.9, E886.9, E888.X)28 or by a machine learning algorithm applied to radiology reports.29 We used a support vector machine (SVM) classifier to identify serious falls using radiology reports. We also compared mutual information (MI) ranking and embedded feature selection approaches. The final SVM classifier with MI feature selection achieved an area under the curve score of 97% on the test set. We then validated the algorithm on a subset of VACS radiology reports, which demonstrated excellent metrics: positive predictive value: 93%; sensitivity: 95%; F measure: 94%; and accuracy: 99%.29
The second outcome of interest was fragility fractures. We explored hip fractures (ICD9 820.0X, 820.1X, 820.2X, 820.3X, 820.8, 820.9), vertebral fractures (805.2, 805.3, 805.4, 805.5, 805.6, 805.7), and upper arm fractures (812.0X, 812.1X, 812.2X, 812.3X, 812.4X, 812.5X). We excluded wrist fractures from this analysis. They occur far more often among women than men,30 and their incidence by age differs by gender: in women, the curve is “J” shaped, indicating a likely association with osteoporosis,31 while it is bi-modal in men, one peak between 20 and 45 and another beginning at the age of 65 years.32 The earlier peak is thought to be more related to severe trauma than to osteoporosis.33 As more than 70% of our sample was younger than 60 years of age and 98% were men, the predominant cause of wrist fractures in this group is likely trauma. Serious falls and fragility fractures were identified in the 6-month person-intervals.
Risk Factors and Covariates
We calculated the LE-AAF for dichotomous forms of risk factors associated with fragility fractures and serious falls identified among older PWH. Risk factors were those exposures that were potentially modifiable. Key risk factors for serious falls included body mass index (BMI) (≥ 25),34 indicators of visual impairment (blindness and cataracts), and illicit substance and alcohol use disorders based on ICD9 codes, and an indicator of a serious fall in the past year. Because increased use of alcohol, separate from a specific use disorder, carries higher risk for fracture, we added an indicator of current hazardous alcohol use. This was operationalized as an AUDIT-C score of three or greater for women and four or greater for men.35 The AUDIT-C includes three questions and is scored on a scale of 0–12. Each question has five possible answer choices valued from 0 to 4 points. The questions include: “How often did you have a drink containing alcohol in the past year?”; “How many drinks did you have on a typical day when you were drinking in the past year?”; and “How often did you have 6 or more drinks on 1 occasion in the past year?” We also used an indicator based on the VACS Index 2.0 to assess physiologic frailty.36–38 The VACS Index 2.0 serves as a measure of physiologic frailty among PWH.39 It uses the following demographic information and routinely assessed laboratory measures associated with all-cause mortality: age, hemoglobin, FIB-4 ((age[years] × aspartate aminotransferase[U/L]/platelet count [expressed as platelets × 109/L] × (alanine aminotransferase1/2[U/L])), estimated glomerular filtration rate ((186.3 × serum creatinine-1.154) × (age-0.203) × (1.21 if Black)), HCV status, BMI, albumin, and white blood cell count. We dichotomized the VACS Index 2.0 score at the median. Our model also included an indicator of prescriptions for five or more of the following chronic medications: antihypertensives,40 hypoglycemics,41 antithrombotic agents, proton pump inhibitors (PPIs),42 antiarrhythmics, nitrates43 statins,44 glucocorticoids,45 anticonvulsants, opioids, muscle relaxants, benzodiazepines, serotonin and norepinephrine reuptake inhibitors, selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants, atypical antidepressants (e.g. bupropion, maprotiline, mirtazapine, nefazodone, trazodone), antipsychotics, atypical sleep medications (e.g., amitriptyline, doxepin), and antihistamines. We also created separate flags for prescriptions of mental health medications, opioids, anticonvulsants, and benzodiazepines. Finally, we included an indicator of moderate to high pain (a Numeric Rating Scale [NRS] ≥ 4 with a range 0–10).
For fragility fractures, risk factors differed from those of serious falls in that we removed benzodiazepines and pain score and replaced them with indicators of use of PPIs and glucocorticoids.
Covariates (for adjustment only) for both outcomes included dichotomous indicators of female sex and non-White race or Hispanic ethnicity. They also included an indicator for those with two or more of the following chronic physical conditions (identified by ICD9 codes): cognitive impairment, dementia,45,46 stroke,47 seizure disorder,48 diabetes,41 anemia,49 HCV, cirrhosis,50 renal disease,51 hypertension,52 abnormal gait and osteoarthritis.53 We further included a flag for participants who had at least one mental health diagnosis54 (anxiety, major depressive disorder, bipolar disorder, schizophrenia, and psychosis). Because serious falls exhibited a significant association with calendar time, an indicator of person-intervals > 20 was added as a covariate for serious falls only.
Except for demographic variables (assessed at baseline), and pain score and medication use (assessed in the prior 6-month interval), all covariates were assessed at the start of each 6-month interval.
Ethics
VACS was approved by the Institutional Review Boards of VHA Connecticut Healthcare System (1583210) and Yale University School of Medicine (0309025943). It has been granted a waiver of informed consent and is HIPAA compliant.27
Statistical Analysis
The analytic unit was a six-month person-interval where the outcomes potentially occurred during the interval as a function of risk factors and covariates measured at the beginning of each interval. Of all variables, only BMI, pain score, and the VACS Index 2.0 score had missing values (8.3%, 7.9%, and 6.9%, respectively), which were assumed to be missing at random. As implemented in the SAS PROC MI,55 we used fully conditional specification for multiple imputation of variables with missing values56 that drew from a total of 38 informative variables.57 We first tabulated the prevalence of the risk factors and covariates among the 21,041 unique participants at baseline and calculated the incidence of each outcome occurrence (indicator of one or more times per participant) over the five and a half-year observation period (2010 – 2015). We separately fit multivariable logistic models to each of the dichotomous outcomes (serious falls and fragility fracture) by regressing on the risk factors using generalized estimating equations with an autoregressive correlation structure to address the serial correlation of person-intervals nested within participants. These models were separately fit to each of the five imputations, and coefficients were subsequently combined using Rubin’s Rules as implemented in SAS PROC MIANALYZE. The coefficients produced in this manner account for the uncertainty of the imputation process and were subsequently used for the calculation of the LE-AAF values.
The LE-AAF is a refinement of the average attributable fraction (AAF), a descendant of the attributable fraction (AF) introduced by Levin in 1953.58 The AF is the degree to which the occurrence of a disease can be reduced, assuming the entire population remains free from exposure. The AF for a specific risk factor is calculated based on the probability of the outcome (conditional on the presence of that risk factor) as well as on the prevalence of that same risk factor. Because the AF accounts for the maximum possible contribution, it does not adjust for the overlapping contributions of multiple risk factors. This limitation is addressed by the AAF,59 which features the property of additivity. This means that for any group of risk factors, the sum of the individual AAFs will not exceed 100%, providing greater face validity. Confidence intervals for point estimates of the risk factors were generated by applying the outcome models to 200 bootstrapped samples and taking the 2.5 and 97.5 percentiles as the limits. Statistical significance was defined as a 95% confidence interval exclusive of the null. Models were fit using SAS version 9.4 with SAS/STAT 15.2.60 LE-AAF point estimates and confidence intervals were generated using MATLAB R2021b.61
RESULTS
Our cohort was 98% male and 60% non-White (Table 1). The median age was 57 years (interquartile range [IQR] 52, 62). Median BMI was 26 kg/m2(IQR 23, 29). Twenty-six percent of the cohort had a diagnosis of alcohol use disorder, and 13% reported hazardous levels of alcohol use. Twenty-eight percent had a diagnosis of illicit substance use. The median CD4 count was 471 cells/mL (IQR 309, 663) and the median HIV-1 RNA was 48 copies/mL (IQR 40, 119), reflecting the good viral control. The median number of physical comorbidities was two (IQR 1, 3), and the median number of mental health comorbidities was one (IQR 0, 2). Fifteen percent experienced at least one serious fall during the five years of follow-up, and 6% experienced at least one fragility fracture. There were 4,337 serious falls and 1,785 fragility fractures. Twenty-two percent of the sample were taking five or more medications at baseline, 29% were prescribed an opioid, 16% an anticonvulsant, 37% a mental health medication, 11% a benzodiazepine, 19% a PPI, and 14% a glucocorticoid.
Table 1.
Description of sample (N=21,041)
| Variables | % or Median (IQR) |
|---|---|
| Outcome variables | |
| Serious falls (N=4337) | 21% |
| Fragility fractures (N=1785) | 8% |
| Predictor variables | |
| Age (years) | 57 (52, 62) |
| Female sex | 2% |
| Non-White race (including Hispanic ethnicity) | 60% |
| Body Mass Index (kg/m2) | 26 (23, 29) |
| Alcohol use disorder | 26% |
| Hazardous alcohol use (AUDIT-C score ≥ 3 for women and ≥ 4 for men) | 13% |
| Illicit substance use disorder | 28% |
| VACS Index 2.0 | 52 (42, 64) |
| Laboratory | |
| HIV-1 RNA (copies/mL) | 48 (40, 119) |
| CD4 Count (cells/mL) | 471 (309, 663) |
| Comorbidities | |
| Count of physical comorbidities | 2 (1, 3) |
| Count of mental health comorbidities | 1 (0, 2) |
| Vision impairment | 10% |
| Prior serious falls (within 1 year of baseline) | 5% |
| Serious falls during follow-up | 15% |
| Hip, vertebral or upper arm fractures during follow-up | 6% |
| Medications | |
| Count of chronic medications (excluding ART) | 2 (1, 4) |
| Participants taking 5 or more medications | 22% |
| Participants taking 1 or more mental health medications | 37% |
| Participants with at least one prescription for an opioid | 29% |
| Participants with at least one prescription for a benzodiazepine | 11% |
| Participants with at least one prescription for proton pump inhibitors | 19% |
| Participants with at least one prescription for glucocorticoids | 14% |
| Participants with at least one prescription for anticonvulsants | 16% |
AUDIT-C: The Alcohol Use Disorders Identification Test-Concise
VACS: Veterans Aging Cohort Study
ART: Antiretroviral Therapy
SSRI: Selective Serotonin Reuptake Inhibitor
LE-AAF analyses
Models for serious falls and fragility fractures included many of the same variables with similar proportions of attribution. Both included a diagnosis of alcohol use disorder; hazardous alcohol consumption; a diagnosis of substance use disorder; polypharmacy; prescriptions for anticonvulsants, mental health medications, and opioids; a serious fall in the past 12 months; visual impairment, and an indicator of physiologic frailty identified as a VACS Index 2.0 score greater than or equal to the median value. BMI ≥ 25 was protective against both serious falls and fractures.
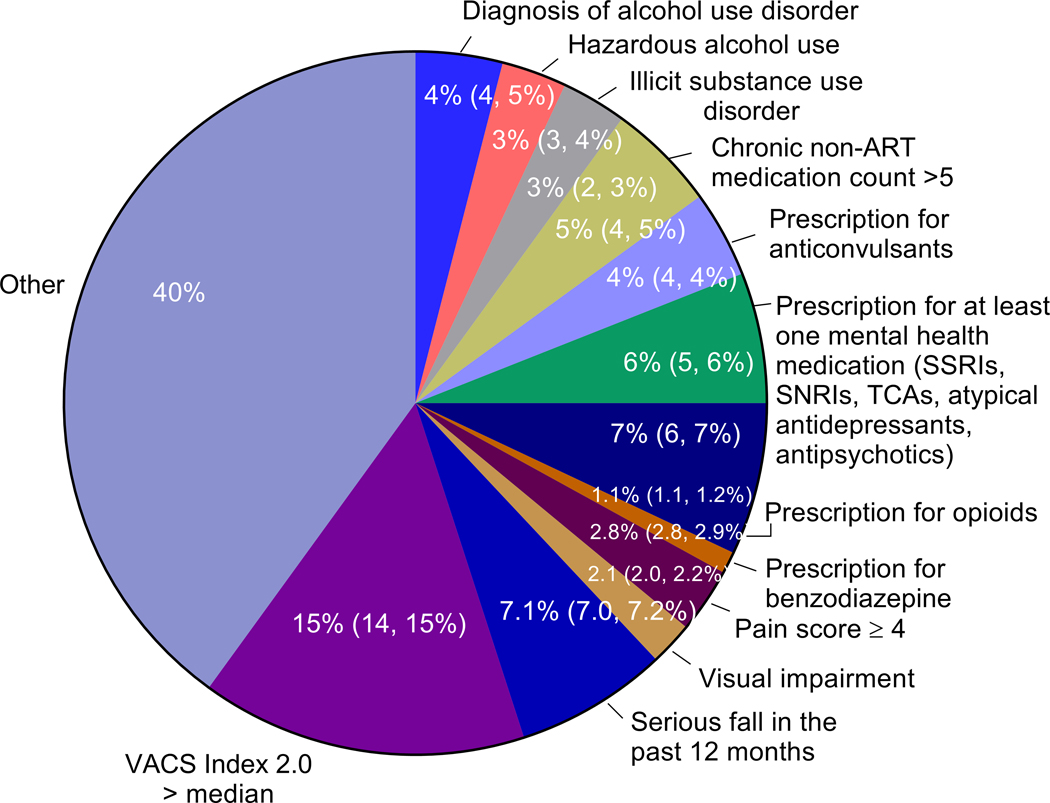
Serious Falls.
For serious falls (Figure 2), risk factors that contributed most to the outcome were a VACS Index score > median (15%; 95% confidence intervals [CI] 14%–15%), a serious fall in the past 12 months (7.1%; 95% CI 7.1%–7.2%), a prescription for an opioid (7%; 95% CI 6%–7%), prescription for at least one mental health medication (6%; 95% CI 5%–6%), chronic non-ART medication count > 5 (5%; 95% CI 4%–5%), prescription for anticonvulsants (4%; 95% CI 4%- 4%), alcohol use disorder (4%; 95% CI 4%–5%), hazardous alcohol use (3%; 95% CI 3%–4%), substance use disorder (3%; 95% CI 2%–3%), pain score > 4 (2.8%; 95% CI 2.8%–2.9%), visual impairment (2.1%; 95% CI 2.0%–2.2%), and having a prescription for a benzodiazepine (1.1%; 95% CI 1.1%–1.2%). Combined, prescription medications (polypharmacy, anticonvulsants, mental health medications, opioids, and benzodiazepines) accounted for 23% of the risk for serious falls. Substance use (alcohol use disorder, elevated AUDIT-C score, and substance use disorder) accounted for 10% of the risk of serious falls. BMI ≥ 25 reduced the risk of a serious fall by 1.9% (95% CI −1.9%–1.8%). Overall, our model accounted for 60% of the risk for serious falls in this cohort.
Figure 2.
LE-AAF for serious falls
Legend: This figure demonstrates the results of the LE-AAF analysis for serious falls. Specifically, the percent is the degree to which the occurrence of serious falls could be reduced, assuming that the entire population remains free from the specific exposure of interest. For example, the occurrence of serious falls could be reduced by 4% if no one in the population had a diagnosis of alcohol use disorder.
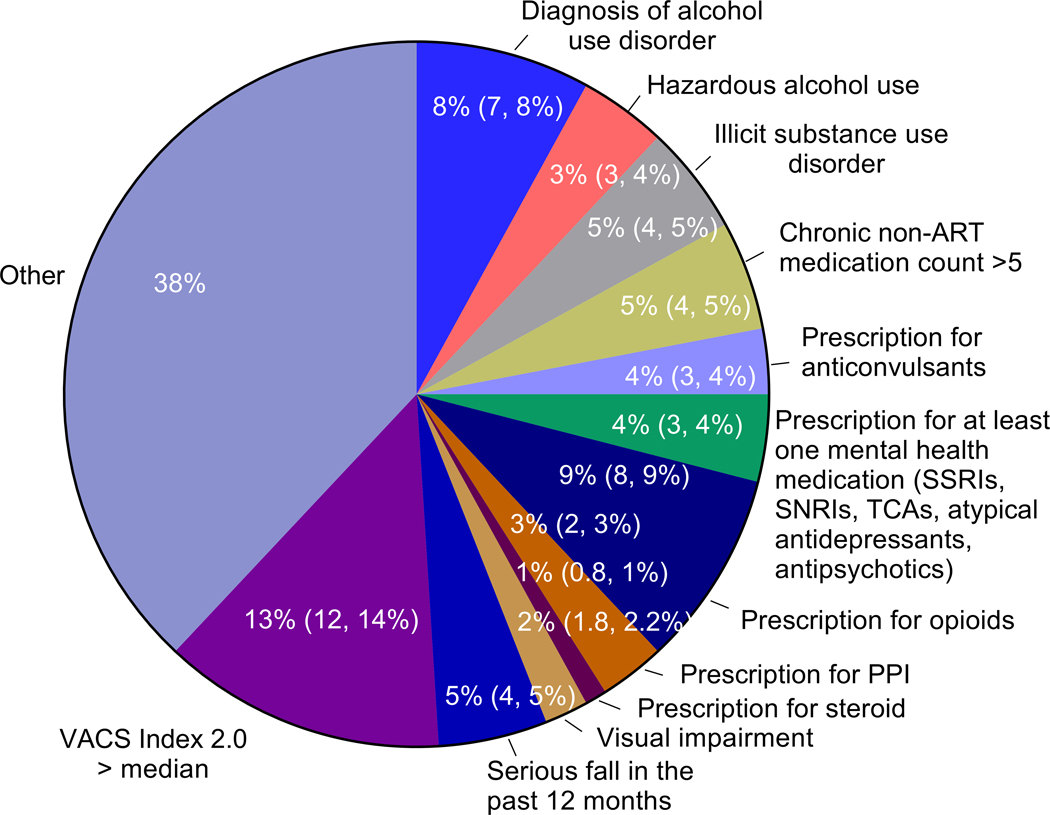
Fragility Fractures.
For fragility fractures (Figure 3), risk factors that contributed most to the outcome were VACS Index score > median (13%; 95% CI 12%, 14%), prescription for an opioid (9%; 95% CI 8%, 9%), diagnosis of alcohol use disorder (8%; 95% CI 7%, 8%), serious fall in the past 12 months (5%; 95% CI 4%, 5%), substance use disorder (5%; 95% CI 4%–5%), chronic non-ART medication count > 5 (5%; 95% CI 4%–5%), prescription for anticonvulsants (4%; 95% CI 3%–4%); prescription for at least one mental health medication (4%; 95% CI 3%–4%), hazardous alcohol use (3%; 95% CI 3%–4%), prescription for PPI ( 3%; 95% CI 2%–3%), visual impairment (2%; 95% CI 1.8%–2.2%), and prescription for glucocorticoids (1%; 95% CI 0.8%–1.0%). Combined prescription medications (polypharmacy, anticonvulsants, mental health medications, opioids, PPIs and glucocorticoids) accounted for 26% of the risk for fragility fractures. Substance use (alcohol use disorder, elevated AUDIT C score, and substance use disorder) accounted for 16% of the risk for fragility fractures. BMI ≥ 25 reduced the risk of a fragility fracture by 9% (95% CI −10%–9%). Overall, our model accounted for 61% of the risk for fragility fractures in this population.
Figure 3.
LE-AAF for fragility fractures
Legend: This figure demonstrates the results of the LE-AAF analysis for fragility fractures. Specifically, the percent is the degree to which the occurrence of fragility fractures could be reduced, assuming that the entire population remained free from the specific exposure of interest. For example, the occurrence of fragility fractures could be reduced by 8% if no one in the population had a diagnosis of alcohol use disorder.
DISCUSSION
Our research suggests that similar variables drive risk for serious falls and fragility fractures among older PWH. Physiologic frailty as assessed by the VACS Index 2.0 accounted for the highest proportion of both outcomes. Being prescribed 5 or more medications, and individual medications and substance use (alcohol and illicit substances), accounted for clinically meaningful proportions of these outcomes. As in all clinical research, whether the factors identified are the direct causes of falls or fractures, or whether they are markers for other causative agents that were not included in the study, is not known.
Among older adults, polypharmacy and individual, high-risk medications (e.g. anticonvulsants, benzodiazepines, PPIs) have long been recognized as important drivers of serious falls and/or fractures.62,63 Alcohol consumption is a well-recognized risk for fragility fractures,64 but illicit substance use has received less attention. Fall prevention programs rarely address alcohol and/or illicit substance use, and yet these are important drivers among older PWH. The message, then, is that serious fall and fracture prevention programs in this population need to address alcohol and substance use as well as polypharmacy and specific high-risk medications. The prevention of serious falls and fragility fractures among older PWH may be best accomplished by modifying existing programs to jointly target both outcomes as well as substance and alcohol use disorders. While we acknowledge the inconclusive evidence that cessation of licit and illicit substance use is associated with reduced risk of these outcomes, the strong associations estimated from reliable records of such usage available in this study suggest its potential.
It is important to put our results in the context of falls and fragility fractures among older adults in the general population. Our sample is chronologically younger than those in the general population. However, discussions about premature aging among PWH have been ongoing for years. It is well-established that older PWH experience more comorbidities that uninfected individuals.65 In particular, older PWH are more likely to experience geriatric syndromes at younger ages than uninfected controls.1–4 Finally, older PWH are more likely to have biomarkers associated with aging than their uninfected counterparts.5,6 Comparing rates of falls and fragility fractures between the two populations, in 2018, 27.5% of adults aged 65+ years reported at least one fall in the past year and 10.2% reported a fall-related injury.66 In our sample, the annual rate of occurrence of serious falls was approximately 5%, and the annual rate of incident fragility fractures was approximately 2%. There are a number of possible explanations for these differences. First, we must note that our approach was restricted to the identification of serious falls (Ecodes and a machine learning algorithm that identifies falls using radiology reports), likely more serious that those that are self-reported. We therefore expect the rate of occurrence to be lower. Furthermore, our population includes primarily men, while falls and fragility fractures disproportionally impact women in the general population. It is likely that the younger chronologic age of our population results in lower rates of falls and fractures, but further research is necessary to better understand the difference in falls and fragility fractures between these two populations. The risk factors that drive falls and fragility fractures are also slightly different among PWH than in the general population. Gait and balance difficulties are a common cause of falls among older adults in the general population. We were not able to assess these factors directly as our cohort is EHR-based. In contrast, alcohol and illicit substance use contribute more to these outcomes among PWH. There are also many similarities: physiologic frailty and polypharmacy are important in both populations as are specific high-risk medications and vision impairment.
The extent to which specific medications may increase the risk of falls is nuanced. Sedating medications are an important risk,67–70 however pain medications, such as opioids, have been inconsistently linked to falls. Opioids have been associated with falls through their impact on orthostatic hypotension, 71 drowsiness,72 dizziness,71 sedation,73 confusion and blurred vision.72 However, tolerance to many of these side effects may develop over time, placing long-term users at lower risk for falls than those who have just started to use these medications.74
Alcohol consumption has also demonstrated an inconsistent association with falls among older adults.69,75 The unambiguous results in the current study may result from the increased impact that alcohol has on PAH relative to those not living with HIV. Research from our colleagues suggests that mortality and physiologic injury are far more common among PAH than among uninfected individuals at similar levels of alcohol consumption.76
This study has important strengths and limitations. A primary strength is that VACS includes all Veterans diagnosed with HIV who receive care within the VA system, the largest provider of HIV care within the US.77 This cohort provided access to a greater range of variables than is available in many cohorts, including pharmacy fill-refill and free text data (clinical notes) that facilitated expanded and improved variable capture. We were able to follow many PWH over five years, which enabled us to reliably assess the historically low incidence of fragility fracture. Although PWH in VACS are older and include very few women, in most other respects the demographics of VACS closely resemble those of the U.S. HIV epidemic.78 The LE-AAF enjoys the strengths of additivity and symmetry, which yield a convenient measure that accounts for all combinations of the risk factors and covariates present in the data. Because of these properties, the relative magnitudes of the LE-AAF allow for a simple ranking of the risk factors that explain the largest proportions of the outcomes. This is a valuable tool for identifying which modifiable factors to prioritize during policy discussions and during development of interventions.
The LE-AAF also has limitations that warrant mention. Notably, the LE-AAF can only explain the proportions of the outcomes attributable to risk factors that are measured. For this reason, and as illustrated in this study, the overall sum of the LE-AAF values often ranges between 60% and 70%. This means that between 30–40% of the outcomes are not attributable to modifiable factors, an important limitation to what LE-AAF can provide. A second important study limitation is that our serious fall outcome was restricted to those falls that caused a patient to present for health care, reflecting the definition used by Tinetti and colleagues.79 Although this approach did not identify all falls, it likely identified those that were most concerning to both patient and provider. Nonetheless, this definition biases our study towards an underestimation of the falls. We were also unable to consider all potentially significant risk factors. For example, peripheral neuropathy is underassessed in clinical care, which suggests that neither administrative codes nor machine-learning algorithms can reliably identify this condition. Nor were some rare conditions included (e.g., Parkinson’s disease). In addition, we were unable to capture some of the key fall risk factors identified in older adults, including balance and gait impairments, lower extremity strength, cognition, and environmental hazards.67,68 While we did include a validated measure of physiologic frailty,39 we did not include any of the measures of frailty often used in studies of older adults such as the Fried criteria, which are not available as structured data in our EHR. Finally, because many studies suggest that women with HIV are at greater risk for falls than men, and because women are often underrepresented in HIV research, the very low proportion of women in this study (2%) is an important limitation.
In summary, this study confirms the contributions of risk factors important in the general population to both serious falls and fragility fractures among older PWH. It also identifies other risk factors that are more prominent among older PWH. The latter include hazardous alcohol consumption, illicit substance use disorder, and having a prescription for an opioid, factors that are usually ignored in mainstream prevention efforts. Successful prevention programs for serious falls and fragility fractures should build on existing prevention efforts while including risk factors specific to PWH.
Key Points.
Among older PWH, serious falls and fragility fractures share many risk factors.
Key risk factors that should be prioritized for prevention of both serious falls and fragility fractures include physiologic frailty, alcohol use disorder, polypharmacy, opioid prescriptions, and prior falls.
Why does this paper matter?
Although geriatrics has historically focused on the health care of persons 65+ years of age, a considerable body of clinical research posits that the geriatrics life-phase of PWH may begin in the sixth decade of life because of chronic immune activation and inflammation, leading to earlier multimorbidity and polypharmacy. For example, research has demonstrated a higher prevalence, incidence, and earlier onset of serious falls and fragility fractures among older PWH (50+ years) than among uninfected comparators. For older PWH, many of whom are chronologically middle-aged, this period of life is often their most economically productive. For this reason, fractures that result in hospitalization, disability, or death, often impose crippling financial burdens and lead to social isolation. A number of risk factors driving serious falls and fragility fractures have been identified, but there is as yet no objective basis to choose which risk factors should be targeted for prevention. This manuscript quantifies the proportions of these traumatic outcomes contributed by modifiable risk factors. This provides information on how to target interventions that will most effectively prevent serious falls and fragility fractures among older PWH.
ACKNOWLEDGEMENTS
This work uses data provided by patients and collected by the VA as part of their care and support.
The views and opinions expressed in this manuscript are those of the authors and do not necessarily represent those of the Department of Veterans Affairs or the United States government.
Funding sources:
This work was supported by the National Institute of Nursing Research [grant number K01 NR013437]; the National Center for Research Resources and National Center for Advancing Translational Sciences [grant number UL1 RR024139]; the National Institute of Arthritis and Musculoskeletal and Skin Diseases [grant number R01 AR078715]; the National Institute on Aging [grant number P30 AG21342]; and the National Institute on Alcohol Abuse and Alcoholism [grant numbers U10 AA013566, U24 AA022001, U01 AA020790, U01 AA026224].
Footnotes
Conflict of Interest: None of the authors identify any conflicts of interest.
REFERENCES
- 1.Wing EJ. HIV and aging. Int J Infect Dis. 2016;53:61–68. [DOI] [PubMed] [Google Scholar]
- 2.Nordell AD, McKenna M, Borges AH, et al. Severity of cardiovascular disease outcomes among patients with HIV is related to markers of inflammation and coagulation. J Am Heart Assoc. 2014;3(3):e000844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Justice A, Falutz J. Aging and HIV: an evolving understanding. Curr Opin HIV AIDS. 2014;9(4):291–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pathai S, Bajillan H, Landay AL, High KP. Is HIV a model of accelerated or accentuated aging? J Gerontol A Biol Sci Med Sci. 2014;69(7):833–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Horvath S, Levine AJ. HIV-1 Infection Accelerates Age According to the Epigenetic Clock. J Infect Dis. 2015;212(10):1563–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.So-Armah KA, Tate JP, Chang CH, et al. Do Biomarkers of Inflammation, Monocyte Activation, and Altered Coagulation Explain Excess Mortality Between HIV Infected and Uninfected People? J Acquir Immune Defic Syndr. 2016;72(2):206–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Womack JA, Murphy TE, Ramsey C, Bathulapalli H, Leo-Summers L, Smith AC, Bates J, Jarad S, Gill TM, Hsieh E, Rodriguez-Barradas MC, Tien PC, Yin MT, Brandt C, Justice Are serious falls associated with subsequent fragility fractures among Veterans living with HIV?. JAIDS. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim TW, Walley AY, Ventura AS, et al. Polypharmacy and risk of falls and fractures for patients with HIV infection and substance dependence. AIDS Care. 2017:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Erlandson KM, Zhang L, Ng DK, et al. Risk Factors for Falls, Falls With Injury, and Falls With Fracture Among Older Men With or at Risk of HIV Infection. J Acquir Immune Defic Syndr. 2019;81(4):e117–e126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma A, Hoover DR, Shi Q, et al. Longitudinal study of falls among HIV-infected and uninfected women: the role of cognition. Antivir Ther. 2018;23(2):179–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Womack JA, Goulet JL, Gibert C, et al. Increased Risk of Fragility Fractures among HIV Infected Compared to Uninfected Male Veterans. PLoS One. 2011;6(2):e17217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sharma A, Shi Q, Hoover DR, et al. Increased Fracture Incidence in Middle-Aged HIV-Infected and HIV-Uninfected Women: Updated Results From the Women’s Interagency HIV Study. J Acquir Immune Defic Syndr. 2015;70(1):54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shiau S, Broun EC, Arpadi SM, Yin MT. Incident fractures in HIV-infected individuals: a systematic review and meta-analysis. AIDS. 2013;27(12):1949–1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Slade SC, Carey DL, Hill AM, Morris ME. Effects of falls prevention interventions on falls outcomes for hospitalised adults: protocol for a systematic review with meta-analysis. BMJ Open. 2017;7(11):e017864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kool B, Ameratunga S, Robinson E, Jackson R. Hospitalisations and deaths due to unintentional falls at home among working-aged New Zealanders. Injury. 2007;38(5):570–575. [DOI] [PubMed] [Google Scholar]
- 16.Womack JA, Novick G, Fried T. The beginning of the end: A qualitative study of falls among HIV+ individuals. PLoS One. 2019;14(4):e0216192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kanis JA, Johnell O, Oden A, et al. Long-term risk of osteoporotic fracture in Malmo. Osteoporos Int. 2000;11(8):669–674. [DOI] [PubMed] [Google Scholar]
- 18.Melton LJ Atkinson EJ, O’Connor, O’Fallon WM, Riggs BL Bone density and fracture risk in men. J Bone Miner Res. 1998;13(12):1915–1923. [DOI] [PubMed] [Google Scholar]
- 19.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17(12):1726–1733. [DOI] [PubMed] [Google Scholar]
- 20.Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301(5):513–521. [DOI] [PubMed] [Google Scholar]
- 21.Bertram M, Norman R, Kemp L, Vos T. Review of the long-term disability associated with hip fractures. Inj Prev. 2011;17(6):365–370. [DOI] [PubMed] [Google Scholar]
- 22.Lippuner K, Golder M, Greiner R. Epidemiology and direct medical costs of osteoporotic fractures in men and women in Switzerland. Osteoporos Int. 2005;16 Suppl 2:S8–S17. [DOI] [PubMed] [Google Scholar]
- 23.Nyberg L, Gustafson Y, Berggren D, Brannstrom B, Bucht G. Falls leading to femoral neck fractures in lucid older people. J Am Geriatr Soc. 1996;44(2):156–160. [DOI] [PubMed] [Google Scholar]
- 24.Eckstrom E, Parker EM, Shakya I, and Lee R. Coordinated Care Plan to Prevent Older Adult Falls. 1.1 ed. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2021. [Google Scholar]
- 25.Juthani-Mehta M, De Rekeneire N, Allore H, et al. Modifiable risk factors for pneumonia requiring hospitalization of community-dwelling older adults: the Health, Aging, and Body Composition Study. J Am Geriatr Soc. 2013;61(7):1111–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murphy TE, McAvay GJ, Allore HG, Stamm JA, Simonelli PF. Contributions of COPD, asthma, and ten comorbid conditions to health care utilization and patient-centered outcomes among US adults with obstructive airway disease. Int J Chron Obstruct Pulmon Dis. 2017;12:2515–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fultz SL, Skanderson M, Mole LA, et al. Development and verification of a “virtual” cohort using the National VA Health Information System. Med Care. 2006;44(8 Suppl 2):S25–30. [DOI] [PubMed] [Google Scholar]
- 28.Tinetti ME, Baker DI, McAvay G, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med. 1994;331(13):821–827. [DOI] [PubMed] [Google Scholar]
- 29.Bates J, Fodeh SJ, Brandt CA, Womack JA. Classification of radiology reports for falls in an HIV study cohort. J Am Med Inform Assoc. 2016;23(e1):e113–e117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hajcsar EE, Hawker G, Bogoch ER. Investigation and treatment of osteoporosis in patients with fragility fractures. Cmaj. 2000;163(7):819–822. [PMC free article] [PubMed] [Google Scholar]
- 31.Buhr AJ, Cooke AM. Fracture patterns. Lancet. 1959;1(7072):531–536. [DOI] [PubMed] [Google Scholar]
- 32.McQueen MaC-B CM. Increasing age and fractures of the distal radius. Current Orthopaedics. 2003;17:360–368. [Google Scholar]
- 33.Lindau TR, Aspenberg P, Arner M, Redlundh-Johnell I, Hagberg L. Fractures of the distal forearm in young adults. An epidemiologic description of 341 patients. Acta Orthop Scand. 1999;70(2):124–128. [DOI] [PubMed] [Google Scholar]
- 34.Ren J, Waclawczyk A, Hartfield D, et al. Analysis of fall injuries by body mass index. South Med J. 2014;107(5):294–300. [DOI] [PubMed] [Google Scholar]
- 35.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789–1795. [DOI] [PubMed] [Google Scholar]
- 36.Tate JP, Justice AC, Hughes MD, et al. An internationally generalizable risk index for mortality after one year of antiretroviral therapy. AIDS. 2013;27(4):563–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Justice AC, Modur SP, Tate JP, et al. Predictive accuracy of the Veterans Aging Cohort Study index for mortality with HIV infection: a North American cross cohort analysis. J Acquir Immune Defic Syndr. 2013;62(2):149–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Akgun KM, Gordon K, Pisani M, et al. Risk factors for hospitalization and medical intensive care unit (MICU) admission among HIV-infected Veterans. J Acquir Immune Defic Syndr. 2013;62(1):52–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Justice AC, Tate JP. Strengths and Limitations of the Veterans Aging Cohort Study Index as a Measure of Physiologic Frailty. AIDS Res Hum Retroviruses. 2019;35(11–12):1023–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tinetti ME, Han L, Lee DS, et al. Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med. 2014;174(4):588–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yau RK, Strotmeyer ES, Resnick HE, et al. Diabetes and risk of hospitalized fall injury among older adults. Diabetes Care. 2013;36(12):3985–3991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kuschel BM, Laflamme L, Moller J. The risk of fall injury in relation to commonly prescribed medications among older people--a Swedish case-control study. Eur J Public Health. 2015;25(3):527–532. [DOI] [PubMed] [Google Scholar]
- 43.Baranzini F, Diurni M, Ceccon F, et al. Fall-related injuries in a nursing home setting: is polypharmacy a risk factor? BMC Health Serv Res. 2009;9:228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ray WA, Daugherty JR, Griffin MR. Lipid-lowering agents and the risk of hip fracture in a Medicaid population. Inj Prev. 2002;8(4):276–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bergland A, Wyller TB. Risk factors for serious fall related injury in elderly women living at home. Inj Prev. 2004;10(5):308–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.van Doorn C, Gruber-Baldini AL, Zimmerman S, et al. Dementia as a risk factor for falls and fall injuries among nursing home residents. J Am Geriatr Soc. 2003;51(9):1213–1218. [DOI] [PubMed] [Google Scholar]
- 47.Grundstrom AC, Guse CE, Layde PM. Risk factors for falls and fall-related injuries in adults 85 years of age and older. Arch Gerontol Geriatr. 2012;54(3):421–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nguyen-Michel VH, Bornand A, Balathazar AM, et al. Fall related to epileptic seizures in the elderly. Epileptic Disord. 2015;17(3):287–291. [DOI] [PubMed] [Google Scholar]
- 49.Duh MS, Mody SH, Lefebvre P, Woodman RC, Buteau S, Piech CT. Anaemia and the risk of injurious falls in a community-dwelling elderly population. Drugs Aging. 2008;25(4):325–334. [DOI] [PubMed] [Google Scholar]
- 50.Yildirim M. Falls in Patients With Liver Cirrhosis. Gastroenterol Nurs. 2017;40(4):306–310. [DOI] [PubMed] [Google Scholar]
- 51.Kistler BM, Khubchandani J, Jakubowicz G, Wilund K, Sosnoff J. Falls and Fall-Related Injuries Among US Adults Aged 65 or Older With Chronic Kidney Disease. Prev Chronic Dis. 2018;15:E82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–1707. [DOI] [PubMed] [Google Scholar]
- 53.Saari P, Heikkinen E, Sakari-Rantala R, Rantanen T. Fall-related injuries among initially 75- and 80-year old people during a 10-year follow-up. Arch Gerontol Geriatr. 2007;45(2):207–215. [DOI] [PubMed] [Google Scholar]
- 54.Bunn F, Dickinson A, Simpson C, et al. Preventing falls among older people with mental health problems: a systematic review. BMC Nurs. 2014;13(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rubin D. Inference and missing data. Biometrika. 1976;63(3):581–592. [Google Scholar]
- 56.White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30(4):377–399. [DOI] [PubMed] [Google Scholar]
- 57.Womack JA, Murphy TE, Bathulapalli H, Smith A, Bates J, Jarad S, Redeker NS, Luther SL, Gill TM, Brandt CA, Justice AC Serious falls in middle-aged Veterans: Development and validation of a predictive risk model. Journal of the American Geriatrics Society. 2020;In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Levin ML. The occurrence of lung cancer in man. Acta Unio Int Contra Cancrum. 1953;9(3):531–541. [PubMed] [Google Scholar]
- 59.Eide GE, Gefeller O. Sequential and average attributable fractions as aids in the selection of preventive strategies. J Clin Epidemiol. 1995;48(5):645–655. [DOI] [PubMed] [Google Scholar]
- 60.SAS Institute Inc. SAS 9.4 Procedures Guide. SAS Institute; 2013. [Google Scholar]
- 61.MATLAB and Statistics Toolbox Release 2012b [computer program]. Natick, Massachussetts: The MathWorks, Inc; 2012. [Google Scholar]
- 62.CDC. STEADI -- Older Adult Fall Prevention. 2017. Accessed 25 October, 2017. [Google Scholar]
- 63.Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008;19(4):385–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kanis JA, Johansson H, Johnell O, et al. Alcohol intake as a risk factor for fracture. Osteoporos Int. 2005;16(7):737–742. [DOI] [PubMed] [Google Scholar]
- 65.Salter ML, Lau B, Go VF, Mehta SH, Kirk GD. HIV infection, immune suppression, and uncontrolled viremia are associated with increased multimorbidity among aging injection drug users. Clin Infect Dis. 2011;53(12):1256–1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Moreland B, Kakara R, Henry A. Trends in Nonfatal Falls and Fall-Related Injuries Among Adults Aged >/=65 Years - United States, 2012–2018. MMWR Morb Mortal Wkly Rep. 2020;69(27):875–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61. [DOI] [PubMed] [Google Scholar]
- 68.Ganz DA, Latham NK. Prevention of Falls in Community-Dwelling Older Adults. N Engl J Med. 2020;382(8):734–743. [DOI] [PubMed] [Google Scholar]
- 69.Sheahan SL, Coons SJ, Robbins CA, Martin SS, Hendricks J, Latimer M. Psychoactive medication, alcohol use, and falls among older adults. J Behav Med. 1995;18(2):127–140. [DOI] [PubMed] [Google Scholar]
- 70.Seppala LJ, Wermelink A, de Vries M, et al. Fall-Risk-Increasing Drugs: A Systematic Review and Meta-Analysis: II. Psychotropics. J Am Med Dir Assoc. 2018;19(4):371 e311–371 e317. [DOI] [PubMed] [Google Scholar]
- 71.Chen A, Ashburn MA. Cardiac Effects of Opioid Therapy. Pain Med. 2015;16 Suppl 1:S27–31. [DOI] [PubMed] [Google Scholar]
- 72.Duran CE, Azermai M, Vander Stichele RH. Systematic review of anticholinergic risk scales in older adults. Eur J Clin Pharmacol. 2013;69(7):1485–1496. [DOI] [PubMed] [Google Scholar]
- 73.Guerriero F. Guidance on opioids prescribing for the management of persistent non-cancer pain in older adults. World J Clin Cases. 2017;5(3):73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Seppala LJ, van de Glind EMM, Daams JG, et al. Fall-Risk-Increasing Drugs: A Systematic Review and Meta-analysis: III. Others. J Am Med Dir Assoc. 2018;19(4):372 e371–372 e378. [DOI] [PubMed] [Google Scholar]
- 75.Chen CM, Yoon YH. Usual Alcohol Consumption and Risks for Nonfatal Fall Injuries in the United States: Results From the 2004–2013 National Health Interview Survey. Subst Use Misuse. 2017;52(9):1120–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Justice AC, McGinnis KA, Tate JP, et al. Risk of mortality and physiologic injury evident with lower alcohol exposure among HIV infected compared with uninfected men. Drug Alcohol Depend. 2016;161:95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Relations VOoPAaM. VA is the largest single provider of HIV care in the United States. VA Fact Sheet. 2020. https://www.hiv.va.gov/pdf/HIV-program-factsheet.pdf. Accessed 09 August 2022. [Google Scholar]
- 78.Centers for Disease Control and Prevention. HIV Surveillance Report, 2018 (Preliminary). 2020;30. [Google Scholar]
- 79.Tinetti ME, Baker DI, King M, et al. Effect of dissemination of evidence in reducing injuries from falls. N Engl J Med. 2008;359(3):252–261. [DOI] [PMC free article] [PubMed] [Google Scholar]