Abstract
Background
With the growth of digital nursing, several studies have focused on recording patients' views on remote care, or specialised nurse staffing aspects. This is the first international survey on telenursing focused exclusively on clinical nurses that analyses the dimensions of usefulness, acceptability, and appropriateness of telenursing from the staff point of view.
Methods
A previously validated structured questionnaire including demographic variables, 18 responses with a Likert-5 scale, three dichotomous questions, and one overall percentual estimation of holistic nursing care susceptible to being undertaken by telenursing, was administered (from 1 September to 30 November 2022) to 225 clinical and community nurses from three selected EU countries. Data analysis: descriptive data, classical and Rasch testing.
Results
The results show adequacy of the model for measurement of the domains of usefulness, acceptability, and appropriateness of telenursing (overall Cronbach's alpha 0.945, Kaiser-Meyer-Olkin 0.952 and Bartlett's p < 0.001). Answers in favour of telenursing ranked 4 out of 5 in Likert scale, both globally and by the three domains. Rasch: reliability coefficient 0.94, Warm's main weighted likelihood estimate reliability 0.95. In the ANOVA analysis, the results for Portugal were significantly higher than those for Spain and Poland, both overall and for each of the dimensions. Respondents with bachelor's, master's and doctoral degrees score significantly higher than those with certificates or diplomas. Multiple regression did not yield additional data of interest.
Conclusions
The tested model proved to be valid, but although the majority of nurses are in favour of telenursing, given the nature of the care, which is mainly face-to-face, according to the respondents, the chances of carrying out their activities by telenursing is only 35.3%. The survey provides useful information on what can be expected from the implementation of telenursing and the questionnaire proves to be a useful tool to be applied in other countries.
Keywords: Telenursing, Nursing care, Enursing, Questionnaire, Rasch tests
1. Introduction
There are four key drivers for the rapid expansion of information and communication technologies (ICT) in virtual care. Technological advances, particularly in health informatics [1,2] contributing to a better systematisation, quality control, and self-assessment of care [[3], [4], [5]]; a societal demand for equity of access [6] and for greater attention to be paid to the ageing population or to those living in remote areas [7]; labour shortage of nursing and midwifery personnel, which is predicted to worsen in the coming years [8], and cost-effectiveness constraints [9,10].
Although etymologically telenursing implies any kind of holistic remote care (e.g., ordinary mailing), it usually refers to care administered through some form of ICT system, from email, telephone, chat, or messaging [[11], [12], [13]] to incorporating computer-based videoconferencing, remote monitoring or diagnosis, or the use of remote widgets requiring complex technologies [14,15].
The various telenursing experiences published in different articles, and in few existing monographs to date [14,16], analyse aspects from the patient's perspective [17] or from that of a specific nursing speciality [[18], [19], [20], [21], [22], [23]], staff management, or promotion [4,24,25].
There is a lack of a comprehensive practical nursing assessment of the intention to use telenursing that covers practicing nurses both with and without experience in virtual care. Hopefully, our work will not only be useful for nursing care staff, but also for guiding the process of change towards digital care and reinforcing nurse participation in managerial decisions.
This cross-sectional survey aims to fill this gap by analysing the positioning of nurses from three selected EU countries in relation to remote care. The study of telenursing from the nurse's point of view, presented in this paper, has not been addressed (to our knowledge) in a comprehensive and global approach before [26,27].
2. Material and method
We present a cross-sectional survey (1 September to 30 November 2022) in which 225 practicing nurses from three selected EU countries (Spain, Portugal, and Poland) participated, to test their opinion regarding telenursing.
A previously validated structured questionnaire created using computer simulation [28] was self-administered, either on paper or online, which included demographic data, 18 responses (Q11−Q36) (three paired questions for each dimension) on a Likert-5 scale, three dichotomous questions (D1−D3) (one per dimension), plus an open-ended response with an overall percentage estimate of the holistic nursing care that telenursing could provide. Respondents included nurses and auxiliary nurses practicing in community centres, hospitals, or nursing homes, excluding staff involved in teaching, research, or management.
In addition to general demographic statistics, both overall and by country, the results of the polytomous questions (Q11-Q36) are presented in graphical format. The answers were reordered and re-sorted where necessary, as questions were disordered and in some cases inverted, to avoid leading questions [28]. Additionally, to detect inconsistent answers, the theoretical value of each of the three dichotomous variables (D1-D3) was calculated for each domain as the sum of the six (three pairs) values. Score was set as 1 for sums over 15. Inconsistency was considered to be found when there was a discrepancy of more than one value between reported categorical values and the theoretical values computed as above. Discrepancies were confirmed with p-values in Rasch person data.
Calculations were performed with the IBM-SPSS statistics package V26 for Classical Test Theory (CTT) [29]. For Item Response Theory (IRT), a Rasch analysis was performed with R (basic packages: MASS, eRm, Itm, TAM), obtaining the reliability ratio, and Warm's mean weighted likelihood estimates (WLE) reliability.
A one-way ANOVA analysis was performed using the sum of the polytomous variables as the dependent variable and country, academic degree, and workplace as independent variables. Finally, multiple linear regression modelled the total score with these variables.
Rasch analysis has also been performed including inlier-sensitive or information-weighted fit (infit-t), i.e., standardized as a z-score, standardized outlier-sensitive fit (outfit-t), betas, level of difficulty, level of discrimination, The item characteristic curves (ICC) and item information curves (IIC). Expected A Priori (EAP) and Warm's likelihood estimate (WLE) reliability ratios.
3. Results
3.1. Demographic statistics
The demographics (Table 1) show some differences in the average age of nurses, with Polish nurses about one decade younger than those of the other countries, giving an overall average of 39.18 ± 11.6 years. The majority (89.3%) of respondents were female. Years in this work provided a similar difference, matching the described differences in age (18.5–9.2), with an overall average of 14.6 ± 10.7 years. Hospital workers represented 84.0%. The post-Bologna generation, with at least a 4-year bachelor's degree, is beginning to predominate (54.7%). Almost 60% have a speciality, and 86.7% have no experience with telenursing. Respondents ranked telenursing as 4 out of 5 in the Likert scale, both globally and by the three domains of usefulness, acceptance, and appropriateness.
Table 1.
Demographic data.
| Spain | Portugal | Poland | ALL | |
|---|---|---|---|---|
| (n) | 90 | 60 | 75 | 225 |
| Age (Average, years) | 43.6 | 41.4 | 32.2 | 39.18 |
| (SD) | 10.9 | 9.0 | 11.2 | 11.6 |
| Females (%) | 86.7 | 85.0 | 96.0 | 89.3 |
| Years at work | 16.5 | 18.4 | 9.2 | 14.6 |
| (SD) | 10.3 | 8.8 | 10.7 | 10.6 |
| Place of Work (%) | ||||
| Hospital | 84.4 | 65.0 | 98.7 | 84.0 |
| Primary Care | 12.2 | 35.0 | 1.3 | 14.7 |
| Nursing homes | 3.3 | 0.0 | 0.0 | 1.3 |
| Highest professional degree (%) | ||||
| Nursing assistant certificate | 28.9 | N.A. | 0.0 | 11.6 |
| Nursing school diploma (3 years) | 32.2 | N.A. | 62.7 | 33.8 |
| Bachelor's degree in nursing (4 years) | 13.3 | 58.3 | 24.0 | 28.9 |
| Master's degree in nursing or health sciences | 21.1 | 40.0 | 8.0 | 21.8 |
| Doctorate in nursing or health sciences | 4.4 | 1.7 | 5.3 | 4.0 |
| N.A. Not applicable | ||||
| Specialty(Yes, %) | 19.0 | 78.3 | 65 | 58.8 |
| Telenursing experience (%) | ||||
| None | 84.4 | 86.7 | 89.3 | 86.7 |
| Two years or less | 12.2 | 11.7 | 4.0 | 9.3 |
| Over two years | 3.3 | 1.7 | 6.7 | 4.0 |
| Polytomous answers (Likert) | ||||
| Global Median | 4.0 | 4.0 | 4.0 | 4.0 |
| Usefulness | 4.0 | 4.0 | 3.5 | 4.0 |
| Acceptance | 4.0 | 4.0 | 4.0 | 4.0 |
| Appropriateness | 4.0 | 4.0 | 4.0 | 4.0 |
| Categorical answers (Y/N … % YES) | ||||
| Usefulness (D1) | 84.4 | 100.0 | 90.7 | 90.7 |
| Acceptance (D2) | 84.4 | 100.0 | 86.7 | 89.3 |
| Appropriateness (D3) | 70.6 | 85.0 | 58.7 | 70.5 |
| Estimation for telenursing use (%) | 33.5 | 36.3 | 34.5 | 34.3 |
Inconsistent careless answers were found in 16 cases (7.1%) when considering those cases where there were two or more discrepancies between the theoretical values of the categorical variables and the recorded data. It was confirmed by nonsignificant p values in Rasch person data. This data is in line with values reported previously [[30], [31], [32]].
3.2. Results for polytomous variables (Likert answers)
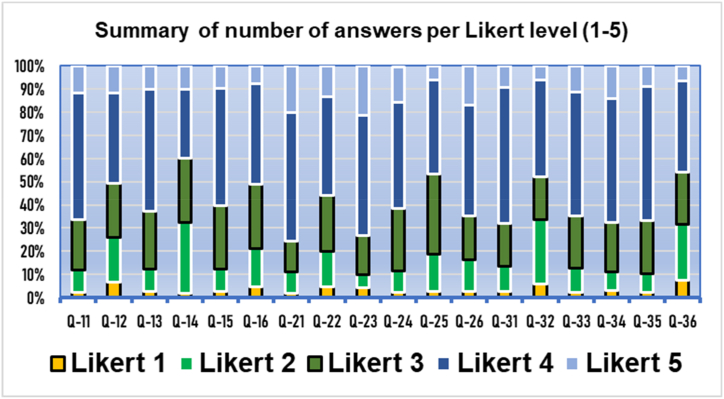
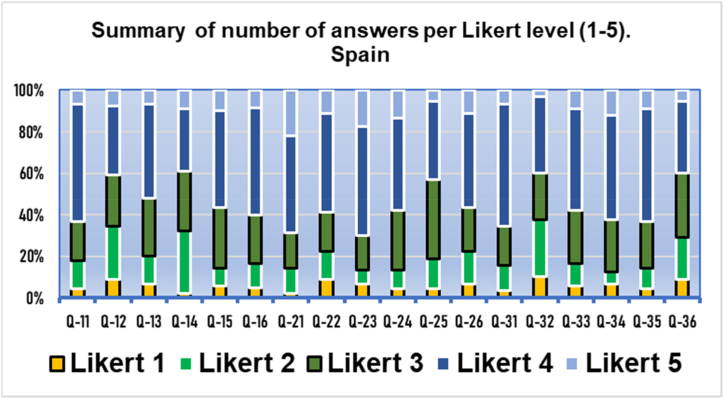
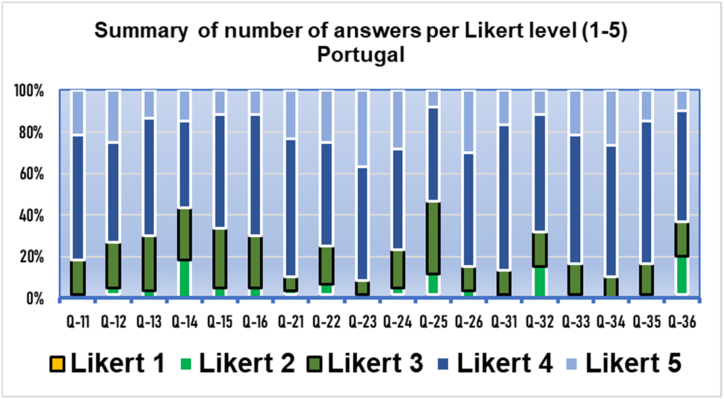
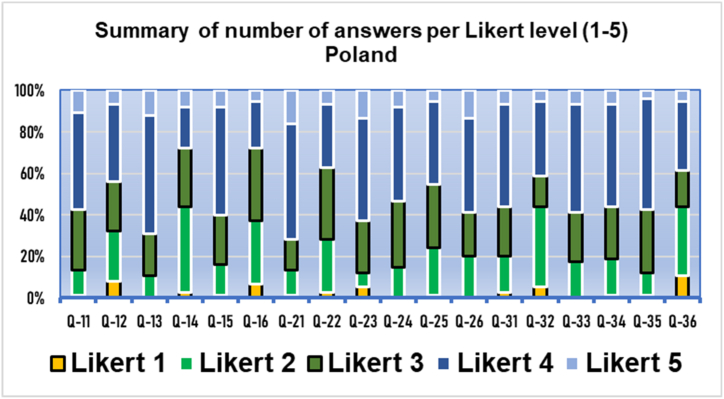
These are presented in summarised graphical formats. Questions Q11−Q16 correspond to usefulness, Q21−Q26 to acceptance, and Q31−Q36 to appropriateness (Fig. 1, Fig. 2, Fig. 3, Fig. 4). Values 4–5 are predominant, indicating a positive answer.
Fig. 1.
Results of the three domains by polytomous (Likert) answers. Q11−Q16 usefulness, Q21−Q26 acceptance. Q31−Q36) appropriateness. Overall results (n = 225).
Fig. 2.
Results of the three domains by polytomous (Likert) answers. Q11−Q16 usefulness, Q21−Q26 acceptance. Q31−Q36 appropriateness. Results from Spain (n = 90).
Fig. 3.
Results of the three domains by polytomous (Likert) answers. Q11−Q16 usefulness, Q21−Q26 acceptance. Q31−Q36 appropriateness. Results from Portugal (n = 60).
Fig. 4.
Results of the three domains by polytomous (Likert) answers. Q11−Q16 usefulness, Q21−Q26 acceptance. Q31−Q36 appropriateness. Results from Poland (n = 75).
3.2.1. Overall data (n = 225)
.
3.2.2. Data from Spain (n = 90)
.
3.2.3. Data from Portugal (n = 60)
.
3.2.4. Data from Poland (n = 75)
.
3.3. ANOVA results
An ANOVA analysis was performed to determine how the different parameters condition the total sum of the polytomous variables. The respondent characteristics that were significant in the ANOVA were: country, degree, and place of work. The scores obtained by respondents from Portugal are significantly higher than those from Spain and Poland, both for the total sum and for each of the dimensions. It should be noted, however, that there is no nursing assistant category in Portugal. Regarding the degree variable, groups 3, 4 and 5 (Bachelor, Master, and Doctorate) score significantly higher than groups 1 and 2 (certificate and diploma) (Table 2).
Table 2.
Kruskal-Wallis tests.
| Sample size (n) | Average rank | Confidence intervals (95.0%) |
|||
|---|---|---|---|---|---|
| Contrast | Difference | +/− Limits | |||
| Country | |||||
| Poland (PL) | 75 | 93.24 | PL - PT | −57.435a | 26.992 |
| Portugal (PT) | 60 | 150.68 | PL - SP | −11.110 | 24.365 |
| Spain (SP) | 90 | 104.35 | PT - SP | 46.325* | 25.973 |
| H = 28.6313 p < 0.000001 | PL - PT | −57.435 | * | 26.992 | |
| Place of work | |||||
| Hospital (H) | 189 | 105.86 | H–N | −15.1429 | 90.685 |
| Nursing home (N) | 3 | 121.00 | H–P | −47.3247a | 29.401 |
| Primary care (P) | 33 | 153.18 | N–P | −32.1818 | 93.974 |
| H = 14.9121 p < 0.001 | |||||
| Degree | |||||
| 1 Certificate | 26 | 74.269 | 1–2 | −20.4939 | 41.5155 |
| 2 Diploma | 76 | 94.763 | 1–3 | −58.4077a | 42.4014 |
| 3 Bachelor | 65 | 132.677 | 1–4 | −56.6287a | 44.3353 |
| 4 Master | 49 | 130.898 | 1–5 | −65.0641 | 70.6691 |
| 5 PhD | 9 | 139.333 | 2–3 | −37.9138a | 30.8709 |
| H = 26.3158 p < 0.0001 | 2–4 | −36.1348a | 33.4775 | ||
| 2–5 | −44.5702 | 64.4147 | |||
| 3–4 | 34.5701 | 34.5701 | |||
| 3–5 | 64.9892 | 64.9892 | |||
| 4–5 | 66.2671 | 66.2671 | |||
Indicates a significant difference.
3.4. Multiple linear regression statistical results
Multiple linear regression of the total score explains 14.7% of the variability. Age was not significant. The variables compare the Portugal group versus the rest (Spain and Poland), degree 3, 4 and 5 versus 1 and 2 and hospital as place of work versus primary care. All have been entered as two-level dummy variables and the 3 respondents from nursing homes were excluded. The mean score: increases 5.054 points on average if the respondent works in hospital versus primary care; increases 4.979 points on average if the respondent has a bachelor, master or doctoral degree versus certificate or diploma and increases 5.074 points on average if the respondent is from Portugal versus the respondents from Spain and Poland (Table 3).
Table 3.
Multiple regression analysis summary.
| Coefficientsa | ||||||||
|---|---|---|---|---|---|---|---|---|
| Model | Unstandardised coefficients |
Standardized Coefficients |
t | Sig. | 95.0% Confidence interval for B |
|||
| B | Std. Error | Beta | Lower Bound | Upper Bound | ||||
| 1 | (Constant) | 58.128 | 1.183 | 49.148 | .000 | 55.853 | 60.460 | |
| place | 5.054 | 2.342 | .143 | 2.158 | .032 | 0.824 | 9.578 | |
| degree | 4.979 | 1.878 | .197 | 2.651 | .009 | 1.275 | 8.602 | |
| Portugal | 5.074 | 2.195 | .179 | 2.311 | .022 | 0.744 | 9.325 | |
Dependent variable: Total score.
3.5. Classical theory results
Following our previous methodology, Table 4 summarises the non-standardised Cronbach's alpha of the polytomous variables for each database (based on covariance analyses) for each dimension. The 95% confidence intervals (CI) for Cronbach's alpha have been computed using the interclass correlation coefficients (two-way random consistency) model. Principal component analysis was performed to assess the strength of the partial correlation between the items, with Kaiser-Meyer-Olkin (KMO) and Bartlett's tests. All Cronbach's alpha excluding one question are over 0.94. Best exclusion is for question Q14 (α = 0.951).
Table 4.
Principal component tests for polytomous variables by domain and overall.
| Domain | Cronbach's alpha | Interclass correlation | Interval (95%CI) | KMO | Bartlett |
|---|---|---|---|---|---|
| Usefulness (D1) | 0.785 | 0.785 | 0.739–0.826 | 0.819 | <0.001 |
| Acceptance (D2) | 0.878 | 0.878 | 0.851–0.901 | 0.884 | <0.001 |
| Appropriateness (D3) | 0.883 | 0.883 | 0.857–0.905 | 0.871 | <0.001 |
| Overall | 0.945 | 0.945 | 0.934–0.955 | 0.952 | <0.001 |
3.6. IRT. Rasch analyses
The results are summarised in the following table (Table 5).
Table 5.
Summary of Item Response Theory data (Rasch test).
| Variables | Index | Value | |
|---|---|---|---|
| Dichotomic | EAP reliability. | 0.52 |
|
| WLE reliability. | −0.49 | ||
| Andersen LR test | 22.32 |
|
|
| p | 0.81 | ||
| D1-Infit-t | −1.07 |
|
|
| D2-Infit-t | −2.84 | ||
| D3-Infit-t | −2.03 | ||
| D1-Outfit-t | −1.12 | ||
| D2-Outfit-t | −2.75 | ||
| D3-Outfit-t | −3.09 |
|
|
| Beta-D1 (0.95CI) | −1.39 | ||
| Beta-D2 (0.95CI) | −0.91 | ||
| Beta-D3 (0.95CI) | 2.29 | ||
| D1-Dffclt | −1.40 |
|
|
| D1-Dscrmn | 4.56 | ||
| D1-P(x = 1|z = 0) | 1.00 | ||
| D2-Dffclt | −1.31 | ||
| D2-Dscrmn | 4.56 |
|
|
| D2-P(x = 1|z = 0) | 1.00 | ||
| D3-Dffclt | −0.53 | ||
| D3-Dscrmn | 4.56 | ||
| D3-P(x = 1|z = 0) | 0.92 | ||
| Polytomous | EAP reliability. | 0.95 | |
| WLE reliability. | 0.94 |
In addition to the EAP, WLE reliability scores, a complete Rasch test was performed for the categorical variables, although its value considering only three categorical questions cannot be taken into account alone.
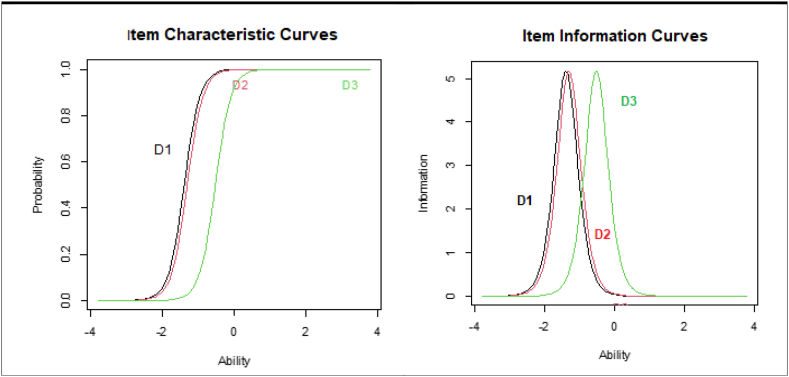
The following graphics, included in Fig. 5, depict the Item Characteristic Curves (ICC) and the Item Information Curves (IIC) for categorical (D1−D3) variables.
Fig. 5.
Item Characteristic Curves (ICC) and the Item Information Curves (IIC) for categorical variables.
The IIC and ICC curves are used to assess the internal consistency of the Rasch data. The ICC curve measures the reliability of the measurement and assesses whether the measurement instrument is reliable in measuring the desired construct. The slope of the ICC represents how much the probability of giving a positive answer increase for supporters of telenursing.
There is a left displacement of the ICC, particularly for usefulness and acceptance. This is probably due to a high degree of ‘ceiling’ effect, meaning that the items are too easy for the majority of the test takers, together with an unequal distribution of scores, resulting in a large number of test takers scoring at the same (positive) level. An average respondent has a probability over 90% in all the cases.
The IIC peak at the difficult value (highest discrimination of the item). It provides information on how much ‘information’ about the latent trait ability is given by an item. The curves are again left biased. The most likely reason for the left shift of the IIC Curves is that the items are too easy for the group of test subjects.
The real value of the Rasch analyses rely on the reliability coefficients for polytomous questions (0.94–0.95).
4. Discussion
Technological factors, increase in community needs, severe staff shortages and cost effectiveness will drive the growth of telenursing, which needs to include the vision of nurses and their active participation in the design and implementation of the programme as essential elements for success [33,34]. Often, organisational changes in health care start from the upper levels of management, with a top-down approach, where not infrequently the professional community is ignored. This leads to delays, if not the abandonment of the new procedure [33,34].
As reported, our questionnaire [28] has been inspired by previous experiences of healthcare staff already teleworking [[35], [36], [37], [38]]; by general questionnaires on the incorporation of technologies [39,40]; and by a previous design focusing on patients' behaviour towards telenursing (TISQ) [17].
Taking these previous experiences into account, and focusing on eliciting the essential elements [41], careful attention has been paid to avoid the frequent error of leading questions [42]. Therefore, each question is paired with an opposing question and the pairs were randomly unordered so that the questions cannot be answered routinely. This allows testing for consistency.
Following the philosophy of the TSQ questionnaire, designed specifically for telemedicine systems, it is assumed that the equipment will be used by patients and professionals once it has been installed and tested, so technical questions relating to the interface have not been included. However, some related aspects have been included, inspired by the TAM, a questionnaire not specific to health sciences but widely used in the commercial world and which includes questions related to usability factors of usefulness and ease of use [39,40].
Details on Classical Test Theory methodology (for polytomous variables) can be found in our previous work [28]. Cronbach's alpha, KMO and Bartlett's tests confirm the adequacy of the results. Overall, Cronbach's alpha is very high (0.945), with interclass correlation of 0.940. KMO 0.952 and Bartlett p < 0.001 (Table 4).
The Kaiser-Meyer-Olkin Sphericity Test (KMO) assesses the correlation between variables and determines whether the data set is adequately related to apply dimensionality reduction. This means that it measures the degree to which a set of variables is related to each other. A KMO score above 0.6 indicates that the set of variables is sufficiently related to perform a factor analysis.
Bartlett's test of sphericity (Bartlett's method of covariance and varimax rotation) tests whether the correlation matrix is an identity matrix. It is used to determine whether variables in a data set were correlated. It tests the null hypothesis that all of the variables are uncorrelated against an alternative hypothesis of at least one pair of variables being correlated. If p is not significant, principal component analysis is not appropriate.
As expected with IRT analysis when considering a construct with only three categorical variables, the EAP reliability is 0.52, indicating an insufficient fit of the Rasch model when only dichotomous variables are included; this is confirmed by WLE of −0.49. Therefore, polytomous analysis is imperative, or else a new design of the test with no less than six categorical questions per domain should be included. In other words, the short version of using only dichotomous questions is not appropriate. The dichotomous variables provide usefulness, basically when tested against the theoretical expected values D1T−D3T obtained from Likert responses for testing careless (inconsistent) answers.
The real utility results of the IRT analysis to be evaluated for polytomous variables is the EAP reliability of 0.95, indicating that the rating scale fits the underlying Rasch model very well. It has been described that there are no major differences between different likelihood estimates (LE) approaches [43]. We have used the Warm's likelihood estimate (WLE), again providing a very good result (0.94).
Although telenursing is a promising technique and will undoubtedly be implemented progressively, the results obtained show that, according to the average of the responses obtained, the degree of application to nursing care will be limited due to the fundamentally face-to-face component of the professional activity.
This study has some limitations. The survey has been carried out in three EU countries. It remains to be analyzed in the future whether the results obtained can be replicated in other contexts and health systems, particularly in developing countries and in non-public health systems.
5. Conclusions
The results are not unexpected. Most nursing care needs face to face activities, but even so, there is a substantial part of the activity that practicing nurses consider may be covered by e-nursing.
It is not necessary for a telenursing programme to start with a complex computer system that allows for comprehensive patient care, management, quality control and includes a decision tree. Dedicating a few hours of professional activity to telephone (and/or video telephonic) care through an appropriately designed programme in collaboration with nursing, could be a perfectly reasonable start.
This questionnaire meets the expected objective as a starting tool to guide the process of change towards digital care and reinforcing nurse and patient participation in managerial decisions in three selected countries and could be extended to analyse the issue in the rest of EU countries.
As for the future, unless complex Rasch developments for polytomous variables are to be used, consideration could be given to transforming these questions into a series of categorical variables to facilitate Rasch analysis.
This pilot study proves that this questionnaire is robust and allows separate analysis of the three domains (usefulness, acceptability, and appropriateness). Categorial data should not be used alone, but in conjunction with polytomous data. Results show a favourable opinion from nurses about telenursing, although they consider that appropriateness for providing holistic nursing care is limited (34.3%).
6. Summary table
What was already known on the topic?
-
●
The various telehealth experiences analyse aspects from the patient's or from the doctor's perspective. In telenursing, only aspects of a specific nursing speciality or aspects of management and teaching have been analyzed.
-
●
The implementation of a telenursing programme requires knowledge of the acceptance, usefulness, and appropriateness of the programme by the personnel who will use it. This information was missing.
What did this study add to our knowledge?
-
●
The development and validation of a questionnaire to analyse telenursing.
-
●
Acceptance of telenursing is generally high among nursing staff, although it is not the same in all countries and is mostly related to the nurse's academic level, regardless of age. Even considering all aspects (holistic approach), telenursing, according to the respondents, is only applicable in about one third of the nursing procedures.
Author contribution statement
Julio Emilio Marco-Franco: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Ramón Camaño-Puig: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Margarida Reis-Santos: Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Isabel Barrachina-Martinez: Performed the experiments; Analyzed and interpreted the data.
Alina Jurewicz: Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Data availability statement
Data will be made available on request.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgement
We are grateful to the various institutions from Spain, Portugal, Poland, and Brazil that have participated. The results submitted from Brazil were not included due to the small sample size. We would like to thank John Wright for help with English editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e16760.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Dreyer K.J., Hirschorn D.S., Thrall J.H., Mentha A. In: A Guide to the Digital Revolution. Dreyer K.J., Hirschorn D.S., Thrall J.H., Mentha A., editors. Springer Science + Business Media, LLC; New York: 2006. p. 570. [Google Scholar]
- 2.Matsushita H. In: Matsushita H., editor. Springer Nature Singapore; Singapore: 2020. pp. 1–173. (Health Informatics: Translating Information into Innovation). [Google Scholar]
- 3.Rysst-Gustafsson S., Eriksson I. Quality indicators in telephone nursing – an integrative review. Nurs Open. 2021;8(3):1301–1313. doi: 10.1002/nop2.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnson C., Wilhelmsson S., Börjeson S., Lindberg M. Improvement of communication and interpersonal competence in telenursing - development of a self-assessment tool. J. Clin. Nurs. 2015;24(11–12):1489–1501. doi: 10.1111/jocn.12705. [DOI] [PubMed] [Google Scholar]
- 5.Schuelke S., Aurit S., Connot N., Denney S. Virtual nursing : the new reality in quality care. Nurs. Adm. Q. 2019;43(4):322–328. doi: 10.1097/NAQ.0000000000000376. [DOI] [PubMed] [Google Scholar]
- 6.Richard L., Furler J., Densley K., Haggerty J., Russell G., Levesque J.F., et al. Equity of access to primary healthcare for vulnerable populations: the IMPACT international online survey of innovations. Int. J. Equity Health. 2016;15(1):1–20. doi: 10.1186/s12939-016-0351-7. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Llorent-Bedmar V., Cobano-Delgado Palma V.C., Navarro-Granados M. The rural exodus of young people from empty Spain. Socio-educational aspects. J. Rural Stud. 2021;82(January):303–314. [Google Scholar]
- 8.Buchan J., Catton H., Schaffer F.A. 2022. Sustain and Retain in 2022 and beyond: the Global Nursing Workforce and the Covid-19 Pandemic.https://www.icn.ch/node/1463 [Internet] Available from: [Google Scholar]
- 9.Grustam A.S., Severens J.L., De Massari D., Buyukkaramikli N., Koymans R., Vrijhoef H.J.M. Cost-effectiveness analysis in telehealth: a comparison between home telemonitoring, nurse telephone support, and usual care in chronic heart failure management. Value Heal [Internet] 2018;21(7):772–782. doi: 10.1016/j.jval.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 10.Hagan L., Morin D., Lépine R. Evaluation of telenursing outcomes: satisfaction, self-care practices, and cost savings. Publ. Health Nurs. 2000;17(4):305–313. doi: 10.1046/j.1525-1446.2000.00305.x. [DOI] [PubMed] [Google Scholar]
- 11.Raphael D., Waterworth S., Gott M. Telephone communication between practice nurses and older patients with long term conditions – a systematic review. J. Telemed. Telecare. 2016 Jan 18;23(1):142–148. doi: 10.1177/1357633X15625398. [Internet] [DOI] [PubMed] [Google Scholar]
- 12.Imlach F., McKinlay E., Middleton L., Kennedy J., Pledger M., Russell L., et al. Telehealth consultations in general practice during a pandemic lockdown: survey and interviews on patient experiences and preferences. BMC Fam. Pract. 2020;21(1):1–14. doi: 10.1186/s12875-020-01336-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Souza-Junior V.D., Mendes I.A.C., Mazzo A., Godoy S. Application of telenursing in nursing practice: an integrative literature review. Appl. Nurs. Res. 2016;29:254–260. doi: 10.1016/j.apnr.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 14.Kumar S., Snooks H., Telenursing, Kumar S., Snooks H. 2011. London: Springer-Verlag London; pp. 1–207. [Google Scholar]
- 15.Vijayalakshmi P., Kathyayani B., Nirmala M.H., Reddemma K., Narayana M., Naveen K.C., et al. National Institute of Mental Health and Neuro Science; 2020. NIMHANS Telenursing Practice Guidelines.https://nimhans.co.in/wp-content/uploads/2021/09/TeleNursing-Practice-Guideline-2020.pdf [Internet] Available from: [Google Scholar]
- 16.American Academy of Ambulatory Care Nursing . In: Scope and Standards of Practice for Professional Telehealth Nursing. sixth ed. Anglea T., editor. American Academy of Ambulatory Care Nursing; New Jersey: 2018. pp. 1–55. (Pitman). [Google Scholar]
- 17.Mattisson M., Johnson C., Börjeson S., Årestedt K., Lindberg M. Development and content validation of the telenursing interaction and satisfaction questionnaire (TISQ) Health Expect. 2019;22(6):1213–1222. doi: 10.1111/hex.12945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaminsky E., Aurin I.E., Hedin K., Andersson L., André M. Registered nurses' views on telephone nursing for patients with respiratory tract infections in primary healthcare - a qualitative interview study. BMC Nurs. 2020;19(1):1–10. doi: 10.1186/s12912-020-00459-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nejadshafiee M., Bahaadinbeigy K., Kazemi M., Nekoei-Moghadam M. Telenursing in incidents and disasters: a systematic review of the literature. J. Emerg. Nurs. 2020;46(5):611–622. doi: 10.1016/j.jen.2020.03.005. [DOI] [PubMed] [Google Scholar]
- 20.Shahrokhi A., Azimian J., Amouzegar A., Oveisi S. The effect of telenursing on referral rates of patients with head trauma and their family's satisfaction after discharge. J. Trauma Nurs. 2018;25(4):248–253. doi: 10.1097/JTN.0000000000000382. [DOI] [PubMed] [Google Scholar]
- 21.Pourbalouch O., Navidian A., Askari H. Assessing the impact of telenursing on self-care in hemodialysis patients: a clinical trial study. Medsurg Nurs. J. 2020;8(4) [Google Scholar]
- 22.Kord Z., Fereidouni Z., Mirzaee M.S., Alizadeh Z., Behnammoghadam M., Rezaei M., et al. Telenursing home care and COVID-19: a qualitative study. BMJ Support. Palliat. Care. 2021 Jun 28 doi: 10.1136/bmjspcare-2021-003001. http://spcare.bmj.com/content/early/2021/06/28/bmjspcare-2021-003001.abstract [Internet]. bmjspcare-2021-003001. Available from: [DOI] [PubMed] [Google Scholar]
- 23.Kamei T., Yamamoto Y., Kajii F., Nakayama Y., Kawakami C. Systematic review and meta-analysis of studies involving telehome monitoring-based telenursing for patients with chronic obstructive pulmonary disease. Jpn. J. Nurs. Sci. 2013;10(2):180–192. doi: 10.1111/j.1742-7924.2012.00228.x. [DOI] [PubMed] [Google Scholar]
- 24.Chang M.Y., Kuo F.L., Lin T.R., Li C.C., Lee T.Y. The intention and influence factors of nurses' participation in telenursing. Informatics. 2021;8(2):1–15. [Google Scholar]
- 25.Hanan M.M., El-Said A.E.-S.H. Tele-Nursing: opportunities for nurses to shape their profession's future. Int J Nov Res Healthc Nurs. 2020;7(3):660–676. http://www.noveltyjournals.com [Internet] Available from: [Google Scholar]
- 26.Snooks H.A., Williams A.M., Griffiths L.J., Peconi J., Rance J., Snelgrove S., et al. Real nursing? The development of telenursing. J. Adv. Nurs. 2008;61(6):631–640. doi: 10.1111/j.1365-2648.2007.04546.x. [DOI] [PubMed] [Google Scholar]
- 27.Koivunen M., Saranto K. Nursing professionals' experiences of the facilitators and barriers to the use of telehealth applications: a systematic review of qualitative studies. Scand. J. Caring Sci. 2018;32(1):24–44. doi: 10.1111/scs.12445. [DOI] [PubMed] [Google Scholar]
- 28.Marco-Franco J.E., Reis-Santos M., Barrachina-Martínez I., González-de-Julián S., Camaño-Puig R. Validation of a new telenursing questionnaire : testing the test. Mathematics. 2022;10(2463):1–13. [Google Scholar]
- 29.Strudwick G. Predicting nurses' use of healthcare technology using the technology acceptance model: an integrative review. Comput. Inf. Nurs. 2015;33(5):189. doi: 10.1097/CIN.0000000000000142. E1. [DOI] [PubMed] [Google Scholar]
- 30.Meade A.W., Craig S.B. Identifying careless responses in survey data. Psychol. Methods. 2012;17(3):437–455. doi: 10.1037/a0028085. [DOI] [PubMed] [Google Scholar]
- 31.Akbulut Y. Predictors of inconsistent responding in web surveys. Internet Res. 2015;25(1):131–147. [Google Scholar]
- 32.Reyes D.L. Combatting carelessness: can placement of quality check items help reduce careless responses? Curr. Psychol. 2022;41(10):6858–6866. [Google Scholar]
- 33.Erlingsdottir G., Ersson A., Borell J., Rydenfält C. Driving for successful change processes in healthcare by putting staff at the wheel. J. Health Organisat. Manag. 2018;32(1):69–84. doi: 10.1108/JHOM-02-2017-0027. [DOI] [PubMed] [Google Scholar]
- 34.Holmström I. Decision aid software programs in telenursing: not used as intended? Experiences of Swedish telenurses. Nurs. Health Sci. 2007;9(1):23–28. doi: 10.1111/j.1442-2018.2007.00299.x. [DOI] [PubMed] [Google Scholar]
- 35.Chen P., Xiao L., Gou Z., Xiang L., Zhang X., Feng P. Telehealth attitudes and use among medical professionals, medical students and patients in China: a cross-sectional survey. Int. J. Med. Inf. 2017;108(September):13–21. doi: 10.1016/j.ijmedinf.2017.09.009. [Internet] [DOI] [PubMed] [Google Scholar]
- 36.Kayyali R., Hesso I., Mahdi A., Hamzat O., Adu A., Nabhani Gebara S. Telehealth: misconceptions and experiences of healthcare professionals in England. Int. J. Pharm. Pract. 2017;25(3):203–209. doi: 10.1111/ijpp.12340. [DOI] [PubMed] [Google Scholar]
- 37.Vidal-Alaball J., Mateo G.F., Domingo J.L.G., Gomez X.M., Valmaña G.S., Ruiz-Comellas A., et al. Validation of a short questionnaire to assess healthcare professionals' perceptions of asynchronous telemedicine services: the Catalan version of the health optimum telemedicine acceptance questionnaire. Int. J. Environ. Res. Publ. Health. 2020;17(7):1–11. doi: 10.3390/ijerph17072202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gagnon M.P., Orruño Aguado E., Asua J., Abdeljelil A.B., Emparanza Knör J. Using a modified Technology Acceptance Model to evaluate healthcare professionals' adoption of a new telemonitoring system. Telemed Heal. 2012;18:54–59. doi: 10.1089/tmj.2011.0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Davis F.D. User acceptance of information technology: system characteristics, user perceptions and behavioral impacts. Int. J. Man Mach. Stud. 1993;38:475–487. [Google Scholar]
- 40.Venkatesh V., Bala H. Technology acceptance model 3 and a research agenda on interventions. Decis. Sci. J. 2008;39(2):273–315. [Google Scholar]
- 41.Rattray J., Jones M.C. Essential elements of questionnaire design and development. J. Clin. Nurs. 2007;16(2):234–243. doi: 10.1111/j.1365-2702.2006.01573.x. [DOI] [PubMed] [Google Scholar]
- 42.Loftus E.F. Leading questions and the eyewitness report. Cognit. Psychol. 1975;7(4):560–572. https://www.sciencedirect.com/science/article/pii/0010028575900237 [Internet] Available from: [Google Scholar]
- 43.Nicklin C., Vitta J.P. Assessing rasch measurement estimation methods across R Packages with yes/no vocabulary test data. Lang Test. 2022 doi: 10.1177/02655322211066822. [Internet]. Feb 3. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.