Abstract
Background
Although trust is central to successful physician-family relationships in ICUs, little is known about how to promote surrogates’ trust of ICU physicians in this setting.
Research Question
Does the conduct of family conferences and physicians’ use of shared decision-making (SDM) within family conferences impact surrogates’ trust in the physician?
Study Design and Methods
A mixed-methods secondary analysis was done of a multicenter prospective cohort study of 369 surrogate decision-makers of 204 decisionally incapacitated patients at high risk of death or severe functional impairment within 13 ICUs at six US medical centers between 2008 and 2012. Surrogates completed the Abbreviated Wake Forest Physician Trust Scale (range, 5-25) before and after an audio-recorded family conference conducted within 5 days of ICU admission. We qualitatively coded transcribed conferences to determine physicians’ use of five SDM behaviors: discussing surrogate’s role, explaining medical condition and prognosis, providing emotional support, assessing understanding, and eliciting patient’s values and preferences. Using multivariable linear regression with adjustment for clustering, we assessed whether surrogates’ trust in the physician increased after the family meeting; we also examined whether the number of SDM behaviors used by physicians during the family meeting impacted trust scores.
Results
In adjusted models, conduct of a family meeting was associated with increased trust (average change, pre- to post family meeting: 0.91 point [95% CI, 0.4-1.4; P < .01]). Every additional element of SDM used during the family meeting, including discussing surrogate’s role, providing emotional support, assessing understanding, and eliciting patient’s values and preferences, was associated with a 0.37-point increase in trust (95% CI, 0.08-0.67; P = .01). If all four elements were used, trust increased by 1.48 points. Explaining medical condition or prognosis was observed in nearly every conference (98.5%) and was excluded from the final model.
Interpretation
The conduct of family meetings and physicians’ use of SDM behaviors during meetings were both associated with increases in surrogates’ trust in the treating physician.
Key Words: communication, goals of care, intensive care, qualitative methods, shared decision-making, trust
Graphical Abstract
Take-home Points.
Study Question: Does the conduct of family conferences and physicians’ use of shared decision-making within family conferences impact surrogates’ trust in the physician?
Results: In adjusted models, the conduct of family meetings was associated with an average increase in trust scores of 0.91 point (95% CI, 0.4-1.4; P < .01); every additional element of shared decision-making during the family meeting was associated with a 0.37-point increase in trust (95% CI, 0.08-0.67; P = .01).
Interpretation: The conduct of family meetings and physicians’ use of shared decision-making behaviors during meetings were both associated with increases in surrogates’ trust in the treating physician.
Trust, the expectation that another individual will act for one’s benefit, is essential to effective therapeutic relationships, especially those characterized by high levels of uncertainty or vulnerability.1,2 In light of the technical complexity of critical illness and its treatments, as well as attendant time pressures and prognostic uncertainty, trust may be especially important to surrogate decision-makers in ICUs who are asked to make life support decisions for an incapacitated love one.
However, little is known about how to engender trust in physicians among surrogates in the ICU context. In the outpatient setting, several studies have demonstrated higher trust of physicians rated to have better communication and emotion-handling skills.3, 4, 5, 6, 7, 8, 9 Another study found that patients’ trust in their physician increased with each time they met in an outpatient encounter.7 In the critical care setting, the family meeting may represent an opportunity for physicians to begin establishing trust by demonstrating personal attributes representing dimensions of the trust construct, such as fidelity, competence, and honesty.1 However, this has not been empirically studied and it is possible that time pressure, frequent physician turnover, and absence of preexisting relationship in the ICU context could weaken the associations observed in the outpatient setting. American and European critical care societies10, 11, 12, 13 recommend shared decision-making (SDM) as a central component of patient care in the ICU, and the model is supported by most critically ill patients14,15 and their family members.16 The conduct of family meetings and ICU physicians’ use of SDM may be important opportunities to enhance surrogates’ trust in ICU physicians.
We therefore sought to determine whether (1) family conferences and (2) physicians’ use of shared decision-making skills within those meetings were associated with increases in surrogates’ trust in their treating ICU physician.
Study Design and Methods
We performed a mixed-methods secondary analysis of a prospective, multicenter cohort study in which we audio-recorded a physician-family conference for incapacitated ICU patients that occurred during the first 5 days of mechanical ventilation.17 Participants were enrolled from 13 medical-surgical, trauma, cardiac, and neurologic ICUs at six academic and community medical centers across the United States between 2008 and 2012. Specific study sites included the University of Pittsburgh Medical Center; University of California, San Francisco Medical Center; University of California Fresno, Medical Center; Baystate Medical Center; Harborview Medical Center; and University of North Carolina-Chapel Hill Medical Center. The primary purpose of the parent study (R01 HL094553) was to characterize how physicians discuss prognosis with surrogate decision-makers of incapacitated, critically ill patients. The institutional review boards at all participating medical centers approved the study protocol (see e-Table 1 in the online article). A full description of study methods has been previously published.17,18
Eligible participants included the treating physician and surrogate decision-maker(s) of patients who met the following criteria: (1) lacked decision-making capacity, as judged by patient’s attending physician; (2) acute respiratory failure with ARDS19 requiring mechanical ventilation; (3) ≥ 50% risk for long-term, severe functional impairment indicated by an Acute Physiology and Chronic Health Evaluation (APACHE) II score ≥ 25 or the attending physician’s estimate for patients with neurologic diagnosis. Patients awaiting organ transplantation were excluded. We excluded surrogates < 18 years of age and those unable to read and converse in English well enough to not require an interpreter. Surrogate decision-makers were self-identified, and multiple individuals were enrolled if they rated their role in decision-making as significant. Physicians and surrogates provided written consent. Surrogates provided proxy consent for patient enrollment. The other attendees at the family conferences were given a written information sheet and gave verbal consent for audio-recording.
e-Figure 1 summarizes the outcome measures, instruments used, sources of data, and timing of collection. On enrollment, surrogates completed questionnaires assessing their demographics, prior experience as a surrogate decision-maker, health literacy (Short Test of Functional Health Literacy in Adults; range, 0-36),20,21 and numeracy (Lipkus Numeracy Scale; range, 0-11).22 Immediately before and after the family conference surrogates completed the Abbreviated Wake Forest Physician Trust Scale (A-WFPTS.)23 Following the family conference, the physician leading the meeting completed a brief questionnaire providing their demographic data and indicating whether previous communication with the surrogate had occurred. Researchers audio-recorded the physician-family conference, and the recordings were transcribed verbatim. Trained study personnel abstracted patient’s demographics and clinical data from the medical records.
The primary outcome measure was change in surrogates’ trust in the treating ICU physician as measured by the difference in A-WFPTS score from pre- to post-family conference. The measure was collected from surrogates immediately before and after the family conference to minimize the chance that events other than the family meeting might affect the trust score and to ensure clarity about which physician was being evaluated. The scale has demonstrated internal consistency, reliability (Cronbach’s α = 0.77), and validity23 in the outpatient setting and has been previously used in the ICU setting to assess surrogates’ trust in the treating physician.24, 25, 26 The A-WFPTS does not have a validated minimal clinical important difference (MCID), and the clinically meaningful difference is not known. Therefore, Cohen’s d was used to determine the standardized difference between two means with a value of 0.2 indicating small, 0.5 moderate, and 0.8 large effect size.27 The measurement ranges from 5 (no trust in the physician) to 25 (complete trust in the physician). The five questions within the A-WFPTS, focused on physician trust, and scoring methodology are provided in e-Table 2.
We coded transcripts of family conferences for key elements of shared decision-making in the ICU context drawn from recommendations by the American College of Critical Care Medicine and American Thoracic Society,28 including the following: explaining medical condition or prognosis, assessing surrogates’ understanding, explaining the surrogate decision-making role, eliciting patient’s values and preferences, and providing emotional support. Descriptions of the elements of shared decision-making and example quotes are shown in Table 1. The codes for medical condition or prognosis, assessing surrogates’ understanding, and providing emotional support were developed during the first pass of coding transcripts, whereas the codes for explaining the surrogate decision-making role and eliciting patient’s values and preference were developed during the second pass of coding transcripts. For both passes, we first developed a coding framework according to Crabtree and Miller’s template method and published frameworks for conducting goals of care discussions.29, 30, 31 Coders received training on the coding frameworks and then co-coded a subset of transcripts, line by line, with any differences resolved by discussion. Before final coding, we established interrater reliability using a bank of passages of family meetings32 (summary κ = 0.90 for first pass and κ = 0.92 for second pass coding). The interrater reliability was then retested to ensure quality control (κ = 0.85 for first pass and κ = 0.89 for second pass). For each pass, all transcripts were double coded by two, independent, trained coders (K. S. and E. N. for the first pass and L. S. and E. N. for the second pass), and any differences in coding were discussed until a consensus was reached. Details of the second pass coding and subsequent analyses have previously been published.33 We used ATLAS.ti, version 6.2 (ATLAS.ti Scientific Software Development), for all transcript data management.
Table 1.
Elements of Shared Decision-Making
| Element of Shared Decision-Making | Description of Physician Behavior | Example of Coded Behavior |
|---|---|---|
| Elicit or assess understanding | Asks the surrogate to state his/her general or prognosis-specific understanding of the situation | “Why don’t you tell me about your understanding of your mother’s condition and I will fill in the gaps.” |
| Explain the patient’s medical condition or prognosis | Any statement that tells about, comments on, or predicts any domain regarding the patient’s future | “I think we will simply be causing him more pain without doing any good.” |
| Provide emotional support | Expresses empathy to the family regarding the surrogate’s situation. Reflects the internal state of the family, as opposed to empathy regarding the patient’s situation or medical situation | “I know this was unexpected. It makes it more difficult when you aren’t prepared to make these decisions.” |
| Explain surrogate decision-making role | Discusses how surrogate decision-making happens or ought to happen. Explains principles of surrogate decision-making or discusses permission to follow the patient’s wishes | “It is important to focus on what your father would hope for, given what is going on medically.” |
| Elicit patient’s values, goals, and preferences | Patient-focused questions inquiring about the patient’s past statements about what treatments may be acceptable to them (preferences) or patient’s attitudes, opinions, beliefs, or feelings about what is important, including hopes and concerns for the future (values) | “I guess I wanted to get a sense from you, what kind of a man he is and what his feelings about being kept alive on life support would be. Can you tell me a little bit about him?” |
To focus our investigation of physician SDM behaviors, we turned to the key behaviors recommended to accomplish the major elements of this collaborative decision-making model.28 We created the SDM (shared decision-making) score to assess the additive impact of five shared decision-making behaviors on surrogates’ physician trust. The SDM score is an aggregate score in which all categories are equally weighted. The SDM score is not a validated measure, and the clinically meaningful difference is not known. We found that nearly every physician explained the medical condition or prognosis and, therefore, this element was excluded from the multivariable analysis; hence the SDM score ranges from 0 to 4. To determine the association between change in surrogates’ trust and physicians’ use of key elements of shared decision-making we used multilevel, mixed-effects linear regression modeling. This approach allowed accounting for clustering of patients and physicians within surrogates. Random effects for patients and physicians were inserted into the regression model and assessed using likelihood ratio tests and intraclass correlations. We opted to adjust only for patient-level clustering within surrogates, based on the results of sensitivity analyses, and proceeded using a mixed-effects linear regression model with only patient random effect (e-Appendix 1).
We identified potential confounding variables through a univariate analysis of the effect of surrogate-, patient-, and physician-level demographic variables on the change in surrogates’ trust score. We included in the multivariable model demographic variables found to be associated with trust modulation at P < .10. We also completed an analysis using linear mixed-effects models adjusting for clustering of family members on the impact of physician race, physician sex, and surrogate race, on preconference, postconference, and change in trust score.
We had > 80% power to detect an alternative slope as small as 0.36 from the available nested data of 204 patients and 369 surrogates (trust score change SD, 3.6; SDM score SD, 1.2; within-family intraclass correlation, 0.18).
We also performed a sensitivity analysis treating the SDM score as a categorical variable. We used a t-test to compare surrogates’ change in trust following physician-family conferences in which the physician used none or only one shared decision-making behavior (low SDM score group) to conferences in which the physician used four or five behaviors (high SDM score group).
All analyses were performed with STATA 13 (StataCorp), and two-sided statistical significance was defined as P ≤ .05.
Results
Demographics
Table 220,21,22 shows the demographic characteristics of the participating patients, surrogates, and physicians. Of the 366 surrogates who completed the demographic questionnaire, 243 (66.4%) had at least some college education, median numeracy was low (Lipkus, 8.0), and health literacy was adequate (STOFHLA, 35). Nearly one-half of surrogates considered religion to be very important (n = 176; 48.1%). Surrogate’s relationship to their critically ill loved one was variable; 82 (22.4%) were a spouse or partner, 137 (37.4%) a child, 42 (11.5%) a parent, and 104 (28.4%) another relation to the patient, such as a sibling or friend. About one-half of family members (n = 180; 49.2%) had prior experience with surrogate decision-making. On the day of the family meeting, patients had a mean APACHE II score of 26.3 (± 6.8) and had been in the ICU for 6.4 (± 3.7) days.34 Just over one-half of the 204 patients were admitted from home (n = 106; 52%). Physicians were mostly attending physicians (n = 63; 50.4%) with an average mean ± SD of 8.67 (± 9.4) years in practice. Most physicians were trained in internal medicine (n = 58; 58.6%), followed by surgery (n = 15; 15.2%) and anesthesia (n = 5; 5.1%).
Table 2.
Surrogate, Patient, and Physician Demographics
| Characteristic of Study Participants | Surrogates (n = 366)a | Patients (n = 204) | Physicians (n = 125)b |
|---|---|---|---|
| Age, mean ± SD, y | 48.8 ± 13.7 | 58.2 ± 15.9 | 38.4 ± 9.6 |
| Male, No. (%) | 124 (33.9) | 108 (52.9) | 86 (68.8) |
| Race/ethnicity, No. (%) | |||
| Non-Hispanic White | 280 (76.5) | 154 (75.5) | 87 (69.6) |
| Non-Hispanic Black | 38 (10.4) | 24 (11.8) | 3 (2.4) |
| Hispanic | 31 (8.5) | 16 (7.8) | 7 (5.6) |
| Asian/Pacific Islander | 14 (3.8) | 7 (3.4) | 22 (17.6) |
| Other | 3 (0.8) | 0 | 5 (4.0) |
| Not documented | 0 | 3 (1.5) | 1 (0.8) |
| Relationship to patient, No. (%) | |||
| Spouse/partner | 82 (22.4) | … | … |
| Child | 137 (37.4) | … | … |
| Parent | 42 (11.5) | … | … |
| Other relationship | 104 (28.4) | … | … |
| No response | 1 (0.3) | … | … |
| Level of education, No. (%) | |||
| Less than high school diploma | 31 (8.5) | … | … |
| High school diploma | 91 (24.9) | … | … |
| Some college | 174 (47.5) | … | … |
| Graduate school | 69 (18.9) | … | … |
| No response | 1 (0.3) | … | … |
| Level of English comprehension, No. (%) | |||
| Poorly | 1 (0.3) | … | … |
| Fairly well | 8 (2.2) | … | … |
| Well | 24 (6.6) | … | … |
| Very well | 332 (90.7) | … | … |
| No response | 1 (0.3) | … | … |
| Lipkus Numeracy Scalec (range, 0-11), median (IQR) | 8 (5-9) | … | … |
| Level of health literacy measured using STOFHLAd (range, 0-36), median (IQR) | 35 (34-36) | … | … |
| Religiosity, No. (%) | |||
| Not at all important | 29 (7.9) | … | … |
| Not too important | 54 (14.8) | … | … |
| Fairly important | 106 (29.0) | … | … |
| Very important | 176 (48.1) | … | … |
| No response | 1 (0.3) | … | … |
| Past experience as surrogate decision-maker, No. (%) | 180 (49.2) | … | … |
| APACHE IIe (measured on conference day) | … | 26.3 (6.8) | … |
| Admission source, No. (%) | |||
| Home/group home | … | 106 (52.0) | … |
| Acute care facility/outside hospital | … | 81 (39.7) | … |
| Skilled nursing facility | … | 10 (4.9) | … |
| Rehabilitation facility | … | 2 (1.0) | … |
| Other | … | 5 (2.5) | … |
| ICU days before meeting, No. (%) | … | 6.4 (3.7) | … |
| Physician position, No. (%) | |||
| Attending | … | … | 63 (50.4) |
| Fellow | … | … | 36 (28.8) |
| Resident | … | … | 24 (19.2) |
| Nurse practitioner | … | … | 2 (1.6) |
| Medical specialty, No. (%) | |||
| Internal medicine | … | … | 58 (58.6) |
| Surgery | … | … | 15 (15.2) |
| Anesthesia | … | … | 5 (5.1) |
| Other | … | … | 10 (10.1) |
| Internal medicine and other | … | … | 7 (7.1) |
| Surgery and other | … | … | 2 (2.0) |
| Internal medicine, anesthesia, and other | … | … | 2 (2.0) |
| Provider years in practice, mean ± SD | … | … | 8.67 ± 9.4 |
APACHE = Acute Physiology and Chronic Health Evaluation; IQR = interquartile range; STOFHLA = Short Test of Functional Health Literacy in Adults.
Three hundred sixty-nine surrogates completed the pre- and postconference questionnaires. However, three did not complete their baseline questionnaire.
One hundred twenty-six physicians cared for the 204 patients. However, one physician did not complete the MD questionnaire.
The Lipkus Health Numeracy Scale is an 11-item scale (range, 0-11), with higher values indicating better numeracy.22
The Short Test of Functional Health Literacy in Adults is a validated health literacy tool (range, 0-36) with three classifications based on score range: inadequate (1-13), marginal (14-19), and adequate (24-36).20,21
The Acute Physiology and Chronic Health Evaluation II is a validated disease severity tool (range, 0-71), with increasing scores correlating with increasing mortality rates.34
Most of the physicians were male (68.8%) and non-Hispanic White (69.6%). On average, there were 1.8 physicians and 2.6 family members present at each meeting.
Demographic Variables Associated With Change in Trust
Among the 391 eligible surrogates, 382 completed the preconference questionnaire, 384 completed the postconference questionnaire, and 369 completed both. Surrogates’ age (regression coefficient, –0.024; 95% CI, –0.05 to 0.00; P = .073) and health literacy score (regression coefficient, 0.115; 95% CI, 0.06-0.17; P < .001); surrogate having a relationship to patient of spouse, child, or parent (regression coefficient, –1.248; 95% CI, –2.03 to –0.46; P = .001); and physicians of male gender (regression coefficient, 1.449; 95% CI, 0.54-2.36; P = .002) were found to be associated with change in trust at P < .10 and, therefore, were included in the adjusted models. The complete list of surrogate and physician demographic variables included in searching for univariate associations and the results of the analyses are available (e-Table 3).
We performed an exploratory analysis using linear mixed-effects models of preconference and postconference trust score to explore the finding regarding physician gender. On average, male physicians had significantly lower baseline trust scores (–1.17 points; P = .026) than female physicians. Whereas male physicians had, comparatively, a larger increase in trust compared with female physicians, postconference trust scores were not significantly different (e-Table 4).
Notably, physician and surrogate race were not found to be associated with the change in trust score (e-Online Data, e-Online Data). We performed an exploratory analysis using linear mixed-effects models of preconference and postconference trust score by physician and surrogate race. Whereas physician race did not significantly impact pre- and postconference trust scores (e-Table 5), surrogates of Hispanic ethnicity had lower baseline trust (–1.63 points; P = .041) and postconference trust (–1.51 points; P = .044) scores compared with non-Hispanic White surrogates (e-Table 6).
Relationship Between Family Meeting and Surrogates’ Trust
Overall, surrogates reported high trust in their physicians with a mean ± SD preconference trust score measured with the A-WFPTS of 20.5 ± 3.9. From pre- to postconference, the trust score decreased for 68 (18.4%), remained stable in 112 (30.4%), and increased in 189 (51.2%) surrogates. In unadjusted analyses, the conduct of a family meeting was associated with an increase in mean ± SD trust scores from 20.5 ± 3.9 preconference to 21.5 ± 3.8 postconference (P < .0001). In adjusted models, family meetings were associated with an average increase in trust scores of 0.91 point (95% CI, 0.4-1.4; P < .01) with a small effect based on Cohen d standardized effect size of 0.25.
Shared Decision-Making During Family Conferences
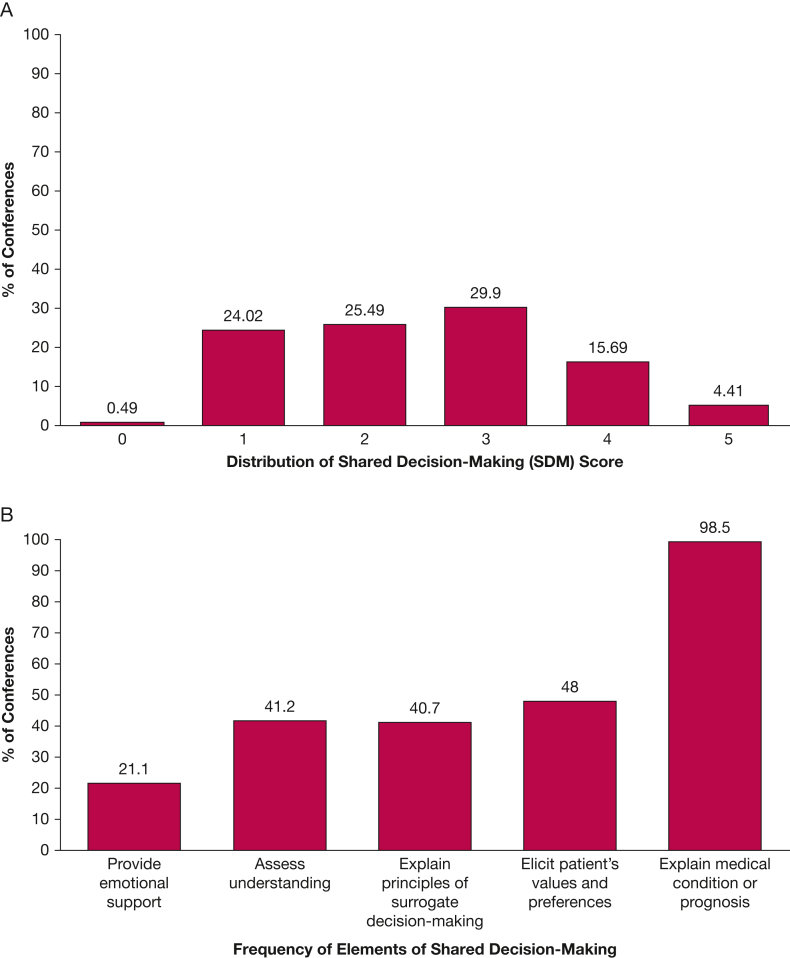
During the audio-recorded family meetings, the mean ± SD SDM score was 2.5 ± 1.2. Figure 1A shows the distribution of physicians’ SDM scores. Figure 1B shows the frequency of each element of shared decision-making within conferences. Nearly every physician explained medical condition or prognosis (98.5% of 204 conferences.) When we included this variable in the SDM score, making it a categorical variable with count 0 to 5, the regression coefficient was positively skewed and counts were disproportionate. For example, we found that trust increased by 11.2 points if the physician used one SDM element compared with none. By excluding explaining medical condition or prognosis from the SDM score, each count was proportionate. Therefore, this element was excluded from the SDM score and the final mixed-effects linear regression model used SDM score, count 0 to 4, as the primary predictor of interest.
Figure 1.
A, Distribution of shared decision-making scores on a scale of 0 (least) to 5 (most). The highest point on each bar indicates the percentage of conferences with that score. B, Proportion of conferences in which the individual decision elements occurred (eg, decision element 1, providing emotional support, occurred in 21% of conferences).
Relationship Between Shared Decision-Making and Trust
A univariate mixed-effects linear regression model assessing each SDM element as the only predictor of change in trust showed statistically significant associations between explaining the surrogate decision-making role (regression coefficient, 1.10; 95% CI, 0.31-1.90; P = .007) and eliciting patients’ values and preferences (regression coefficient, 1.09; 95% CI, 0.31-1.88; P = .006) with increases in trust. e-Table 7 shows the impact of each SDM element on change in trust. Univariate analysis revealed that the SDM score (range, 0-4) was associated with increases in surrogates’ trust (regression coefficient, 0.59; 95% CI, 0.25-0.93; P = .001). After adjusting for physician gender and surrogate age, health literacy score, relationship to patient, and preconference trust score, we found a strong positive association between physicians’ use of key elements of shared decision-making and trust modulation. For every element of shared decision-making used during a family meeting, beyond explaining medical condition or prognosis, surrogates’ trust in their ICU physician increased by 0.37 point (95% CI, 0.08-0.67; P = .013). On the basis of these findings, if all four elements were used by a physician trust increased by approximately 1.5 points. Table 3 shows the multivariable model analyzing the relationship between the predictor variables and physician trust.
Table 3.
Mixed-Effects Multivariable Linear Regression Model Analyzing the Relationship Between Shared Decision-Making Score and Physician Trust
| Variable | Regression Coefficienta | 95% CI | P Value |
|---|---|---|---|
| Shared decision-making (SDM) score | 0.37 | 0.08 to 0.67 | .013 |
| Surrogate age | –0.01 | –0.03 to 0.16 | .581 |
| Surrogate health literacy score | 0.08 | 0.03 to 0.13 | .003 |
| Closeness of relationship to patient: spouse/child/parent (Ref: other relationship) | –0.78 | –1.47 to –0.08 | .029 |
| Physician male (Ref: female) | 0.80 | 0.02 to 1.59 | .046 |
| Preconference trust score | –0.41 | –0.50 to –0.33 | < .001 |
Ref = reference.
Regression coefficient interpretation: For every additional element of SDM used by the physician, surrogate trust in the treating physician increased by 0.37 point.
e-Table 8 shows the results of a sensitivity analysis of the SDM score as a categorical variable, which confirmed the findings.
Discussion
Among a cohort of surrogates for critically ill patients at high risk of death, the conduct of a family meeting was associated with an increase in surrogates’ trust of the ICU physician, measured immediately before and after the meeting. More use of shared decision-making behaviors by physicians within the meetings was associated with larger increases in trust.
Shared decision-making in ICUs is widely endorsed by American and European critical care societies,10, 11, 12, 13 as well as by critically ill patients14,15 and their family members.16 Shared decision-making has a strong ethical rationale; however, there is a paucity of empirical evidence supporting the model’s value in ICUs. Prior studies have shown potential for decreased risk of psychological distress and increased satisfaction for family members using the collaborative approach.35, 36, 37 We previously reported in a prior study of 51 physician-family conferences in ICUs that more shared decision-making by physicians was associated with greater family satisfaction.36 Gries and colleagues35 found that most families (85%) preferred to be involved in decision-making and those that experienced discordance between their preferred and actual role in decision-making reported higher levels of symptoms of both posttraumatic stress disorder (PTSD) and depression. Our finding that physicians’ use of shared decision-making behaviors is associated with higher trust scores adds to the evidence base with, to the best of our knowledge, the largest study of the topic to date.
We found that at least one of the five core elements of shared decision-making was missing from 196 of 204 audio-recorded family meetings (95%). This finding adds to prior literature demonstrating that shared decision-making in the ICU is often incomplete.33,36 Many critical care physicians feel unprepared to engage in goals of care conversations with families.38 In addition, a systematic review has shown that evidence-based training in end-of-life communication skills remains rare in critical care fellowship programs.39 Several educational programs have been developed to improve critical care physicians’ communication skills and to guide preference-sensitive decisions.40, 41, 42 The Critical Care Communication (C3) program was found to improve fellow physicians’ self-assessed competence in communication skills,40 but there are limited data on how these and other physician educational interventions impact patient-centered outcomes such as physician trust, surrogates’ psychological distress, or provision of goal-concordant care.
We found statistically significant associations between increased trust and increased surrogate age, literacy score, and distance of relationship to patient, and male physician sex. Baseline trust scores were higher for female than male physicians, but male physicians had significantly higher increases in trust scores due to the family conference. Our data do not explain the reason for these findings. It is possible that female physicians had little room for improvement in trust scores from pre- to postconference. One possible explanation for both findings is that before the family meetings female physicians undertook actions that were more trust-engendering than did male physicians and, in light of the high overall trust scores in the cohort, there was little room for improvement in female physicians’ trust scores. Another possibility is that the data demonstrate a bias against how female physicians interact with families during family meetings. Given the well-documented presence of sex bias in medicine and society, further research is needed to understand the causes and implications of these findings.
This study has several limitations. First, although we conducted the study in diverse ICUs, all had academic affiliations, and the results may not be generalizable to hospitals without academic affiliations. Second, the study represents a secondary analysis. As such, not every element of shared decision-making was coded and the variables included in the multivariable model were not selected a priori.28 Third, we did not list the name of the doctor the surrogates should evaluate on the questionnaire and therefore it is possible that they may have been considering a different physician than the one who directed the family meeting. However, we minimized this risk by collecting the questionnaires immediately before and after family conferences. Fourth, because of the sample size, we had limited ability to assess the importance of racial/ethnic concordance for non-White surrogates, which has been identified as an important variable when assessing physician trust by other studies. Fifth, there are limitations to using the A-WPFTS within this study and within the ICU. There is no established MCID for the trust scale and therefore the clinical significance of the observed improvements in trust is uncertain. The trust scale was designed to measure trust in an individual physician in the outpatient setting and therefore may not fully capture all relevant dimensions of trust across all members of the interprofessional ICU team. Nonetheless, research from families in ICUs indicates that trust in the treating physician is ranked most highly by family members as among important elements of care.43 Sixth, we only studied SDM behaviors during a single-family conference. It is likely that there are other elements of communication outside family conferences that could enhance trust.
Interpretation
This study provides evidence of a positive association between the conduct of family meetings and surrogates’ trust in the treating ICU physician. Increases in trust were larger with increasing use of shared decision-making elements by physicians during family meetings. These results provide further justification for use of the shared decision-making model during family meetings discussing goals of care. The finding that shared decision-making was frequently incomplete suggests the need for the development and testing of scalable interventions to help physicians acquire expertise in engaging surrogate decision-makers in ICUs in shared decision-making.
Funding/Support
D. B. W. is the principal investigator and received funding from National Institutes of Health (NIH) [Grants R01 HL094553 and K24 HL148314].
Financial/Nonfinancial Disclosures
None declared.
Acknowledgments
Author contributions: D. B. W. is the guarantor of the content of the manuscript, including the data and analysis. Concept and design: T. E. L. and D. B. W.; acquisition, analysis, or interpretation of the data: T. E. L., P. B., L. P. S., N. C. E., R. M. A., S. S. C., C. L. H., J. R. C., W. A., J. S., M. W. P., B. L., M. A. M., and D. B. W.; statistical analysis: P. B. and C.-C. H. C.; drafting of the manuscript: T. E. L. and D. B. W.; revising the manuscript critically for important intellectual content: all authors; approval of the version to be published: all authors; agreement to be accountable for all aspects of the work: all authors.
Role of sponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Other contributions: The parent study was performed at the University of Pittsburgh Medical Center; University of California San Francisco, Medical Center; University of California Fresno, Medical Center; Baystate Medical Center; Harborview Medical Center; and University of North Carolina-Chapel Hill Medical Center.
Additional information: The e-Appendix, e-Figure, and e-Tables are available online under “Supplementary Data.”
Supplementary Data
References
- 1.Hall M.A., Dugan E., Zheng B., Mishra A.K. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q. 2001;79(4):613–639, v. doi: 10.1111/1468-0009.00223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mechanic D. The functions and limitations of trust in the provision of medical care. J Health Polit Policy Law. 1998;23(4):661–686. doi: 10.1215/03616878-23-4-661. [DOI] [PubMed] [Google Scholar]
- 3.Kao A.C., Green D.C., Davis N.A., Koplan J.P., Cleary P.D. Patients’ trust in their physicians: effects of choice, continuity, and payment method. J Gen Intern Med. 1998;13(10):681–686. doi: 10.1046/j.1525-1497.1998.00204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thom D.H., Campbell B. Patient-physician trust: an exploratory study. J Fam Pract. 1997;44(2):169–176. [PubMed] [Google Scholar]
- 5.Hall M.A., Zheng B., Dugan E., et al. Measuring patients’ trust in their primary care providers. Med Care Res Rev. 2002;59(3):293–318. doi: 10.1177/1077558702059003004. [DOI] [PubMed] [Google Scholar]
- 6.Tulsky J.A., Arnold R.M., Alexander S.C., et al. Enhancing communication between oncologists and patients with a computer-based training program: a randomized trial. Ann Intern Med. 2011;155(9):593–601. doi: 10.1059/0003-4819-155-9-201111010-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gordon H.S., Pugach O., Berbaum M.L., Ford M.E. Examining patients’ trust in physicians and the VA healthcare system in a prospective cohort followed for six-months after an exacerbation of heart failure. Patient Educ Couns. 2014;97(2):173–179. doi: 10.1016/j.pec.2014.07.022. [DOI] [PubMed] [Google Scholar]
- 8.Martin K.D., Roter D.L., Beach M.C., Carson K.A., Cooper L.A. Physician communication behaviors and trust among black and white patients with hypertension. Med Care. 2013;51(2):151–157. doi: 10.1097/MLR.0b013e31827632a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coats H., Downey L., Sharma R.K., Curtis J.R., Engelberg R.A. Quality of communication and trust in patients with serious illness: an exploratory study of the relationships of race/ethnicity, socioeconomic status, and religiosity. J Pain Symptom Manage. 2018;56(4):530–540.e6. doi: 10.1016/j.jpainsymman.2018.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carlet J., Thijs L.G., Antonelli M., et al. Challenges in end-of-life care in the ICU. Statement of the 5th International Consensus Conference in Critical Care: Brussels, Belgium, April 2003. Intensive Care Med. 2004;30(5):770–784. doi: 10.1007/s00134-004-2241-5. [DOI] [PubMed] [Google Scholar]
- 11.Thompson B.T., Cox P.N., Antonelli M., et al. Challenges in end-of-life care in the ICU: statement of the 5th International Consensus Conference in Critical Care: Brussels, Belgium, April 2003: executive summary. Crit Care Med. 2004;32(8):1781–1784. doi: 10.1097/01.ccm.0000126895.66850.14. [DOI] [PubMed] [Google Scholar]
- 12.Davidson J.E., Powers K., Hedayat K.M., et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004-2005. Crit Care Med. 2007;35(2):605–622. doi: 10.1097/01.CCM.0000254067.14607.EB. [DOI] [PubMed] [Google Scholar]
- 13.Lanken P.N., Terry P.B., Delisser H.M., et al. An official American Thoracic Society clinical policy statement: palliative care for patients with respiratory diseases and critical illnesses. Am J Respir Crit Care Med. 2008;177(8):912–927. doi: 10.1164/rccm.200605-587ST. [DOI] [PubMed] [Google Scholar]
- 14.Pochard F., Darmon M., Fassier T., et al. Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death: a prospective multicenter study. J Crit Care. 2005;20(1):90–96. doi: 10.1016/j.jcrc.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 15.Heyland D.K., Tranmer J., O’Callaghan C.J., Gafni A. The seriously ill hospitalized patient: preferred role in end-of-life decision making? J Crit Care. 2003;18(1):3–10. doi: 10.1053/jcrc.2003.YJCRC2. [DOI] [PubMed] [Google Scholar]
- 16.Heyland D.K., Cook D.J., Rocker G.M., et al. Decision-making in the ICU: perspectives of the substitute decision-maker. Intensive Care Med. 2003;29(1):75–82. doi: 10.1007/s00134-002-1569-y. [DOI] [PubMed] [Google Scholar]
- 17.Chiarchiaro J., Buddadhumaruk P., Arnold R.M., White D.B. Quality of communication in the ICU and surrogate's understanding of prognosis. Crit Care Med. 2015;43(3):542–548. doi: 10.1097/CCM.0000000000000719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ernecoff N.C., Curlin F.A., Buddadhumaruk P., White D.B. Health care professionals’ responses to religious or spiritual statements by surrogate decision makers during goals-of-care discussions. JAMA Intern Med. 2015;175(10):1662–1669. doi: 10.1001/jamainternmed.2015.4124. [DOI] [PubMed] [Google Scholar]
- 19.Bernard G.R., Artigas A., Brigham K.L., et al. The American-European Consensus Conference on ARDS: definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149(3 Pt 1):818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- 20.Baker D.W., Williams M.V., Parker R.M., Gazmararian J.A., Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38(1):33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 21.Collins S.A., Currie L.M., Bakken S., Vawdrey D.K., Stone P.W. Health literacy screening instruments for eHealth applications: a systematic review. J Biomed Inform. 2012;45(3):598–607. doi: 10.1016/j.jbi.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lipkus I.M., Samsa G., Rimer B.K. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21(1):37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- 23.Dugan E., Trachtenberg F., Hall M.A. Development of abbreviated measures to assess patient trust in a physician, a health insurer, and the medical profession. BMC Health Serv Res. 2005;5:64. doi: 10.1186/1472-6963-5-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Majesko A., Hong S.Y., Weissfeld L., White D.B. Identifying family members who may struggle in the role of surrogate decision maker. Crit Care Med. 2012;40(8):2281–2286. doi: 10.1097/CCM.0b013e3182533317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson S.K., Bautista C.A., Hong S.Y., Weissfeld L., White D.B. An empirical study of surrogates’ preferred level of control over value-laden life support decisions in intensive care units. Am J Respir Crit Care Med. 2011;183(7):915–921. doi: 10.1164/rccm.201008-1214OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee Char S.J., Evans L.R., Malvar G.L., White D.B. A randomized trial of two methods to disclose prognosis to surrogate decision makers in intensive care units. Am J Respir Crit Care Med. 2010;182(7):905–909. doi: 10.1164/rccm.201002-0262OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Astiti N., Marhaeni A., Suputra P. The effect of thematic patterning technique on students’ writing competency of tenth grade students at SMAN 4 Singaraja. Jurnal Pendidikan Bahasa Inggris undiksha. 2020;8(1):35–41. [Google Scholar]
- 28.Kon A.A., Davidson J.E., Morrison W., Danis M., White D.B. American College of Critical Care Medicine; American Thoracic Society. Shared decision making in ICUs: an American College of Critical Care Medicine and American Thoracic Society policy statement. Crit Care Med. 2016;44(1):188–201. doi: 10.1097/CCM.0000000000001396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Crabtree B.F., Miller W.L. 2nd ed. Sage Publications; Thousand Oaks, CA: 1999. Doing Qualitative Research. [Google Scholar]
- 30.Scheunemann L.P., Arnold R.M., White D.B. The facilitated values history: helping surrogates make authentic decisions for incapacitated patients with advanced illness. Am J Respir Crit Care Med. 2012;186(6):480–486. doi: 10.1164/rccm.201204-0710CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.White D.B., Engelberg R.A., Wenrich M.D., Lo B., Curtis J.R. Prognostication during physician-family discussions about limiting life support in intensive care units. Crit Care Med. 2007;35(2):442–448. doi: 10.1097/01.CCM.0000254723.28270.14. [DOI] [PubMed] [Google Scholar]
- 32.Scheunemann L.P., Cunningham T.V., Arnold R.M., Buddadhumaruk P., White D.B. How clinicians discuss critically ill patients’ preferences and values with surrogates: an empirical analysis. Crit Care Med. 2015;43(4):757–764. doi: 10.1097/CCM.0000000000000772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Scheunemann L.P., Ernecoff N.C., Buddadhumaruk P., et al. Clinician-family communication about patients’ values and preferences in intensive care units. JAMA Intern Med. 2019;179(5):676–684. doi: 10.1001/jamainternmed.2019.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Knaus W.A., Draper E.A., Wagner D.P., Zimmerman J.E. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829. [PubMed] [Google Scholar]
- 35.Gries C.J., Engelberg R.A., Kross E.K., et al. Predictors of symptoms of posttraumatic stress and depression in family members after patient death in the ICU. Chest. 2010;137(2):280–287. doi: 10.1378/chest.09-1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.White D.B., Braddock C.H., III, Bereknyei S., Curtis J.R. Toward shared decision making at the end of life in intensive care units: opportunities for improvement. Arch Intern Med. 2007;167(5):461–467. doi: 10.1001/archinte.167.5.461. [DOI] [PubMed] [Google Scholar]
- 37.McDonagh J.R., Elliott T.B., Engelberg R.A., et al. Family satisfaction with family conferences about end-of-life care in the intensive care unit: increased proportion of family speech is associated with increased satisfaction. Crit Care Med. 2004;32(7):1484–1488. doi: 10.1097/01.ccm.0000127262.16690.65. [DOI] [PubMed] [Google Scholar]
- 38.Nelson J.E., Mulkerin C.M., Adams L.L., Pronovost P.J. Improving comfort and communication in the ICU: a practical new tool for palliative care performance measurement and feedback. Qual Saf Health Care. 2006;15(4):264–271. doi: 10.1136/qshc.2005.017707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mendez M.P., Patel H., Talan J., et al. Communication training in adult and pediatric critical care medicine: a systematic review. ATS Sch. 2020;1(3):316–330. doi: 10.34197/ats-scholar.2019-0017RE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Arnold R.M., Back A.L., Barnato A.E., et al. The Critical Care Communication project: improving fellows’ communication skills. J Crit Care. 2015;30(2):250–254. doi: 10.1016/j.jcrc.2014.11.016. [DOI] [PubMed] [Google Scholar]
- 41.Gustin J.L., Way D.P., Wells-Di Gregorio S., McCallister J.W. Validation of the family meeting behavioral skills checklist: an instrument to assess fellows’ communication skills. Ann Am Thorac Soc. 2016;13(8):1388–1393. doi: 10.1513/AnnalsATS.201601-021OC. [DOI] [PubMed] [Google Scholar]
- 42.Hope A.A., Hsieh S.J., Howes J.M., et al. Let’s talk critical: development and evaluation of a communication skills training program for critical care fellows. Ann Am Thorac Soc. 2015;12(4):505–511. doi: 10.1513/AnnalsATS.201501-040OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Heyland D.K., Dodek P., Rocker G., et al. What matters most in end-of-life care: perceptions of seriously ill patients and their family members. CMAJ. 2006;174(5):627–633. doi: 10.1503/cmaj.050626. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.