Abstract
The effects of diet and nutritional habits on reproductive cells can be categorized in a variety of ways. In this review, the literature is divided, based on the dietary consumption effects on oocytes and sperm. Topics on dietary patterns and the intrauterine effect of maternal nutrition are covered. In general fruits, vegetables, whole greens, fish, legumes, and also dietary sources containing unsaturated fats can improve reproductive germ cell quality. In epidemiological studies, the food intake frequency questionnaire is one of the most common methods to assess diet. Due to methodological heterogeneity in dietary assessment and inadequacy in the measurement of dietary intake in the questionnaires used, several unreliable results may be reported. Thus, the quality of evidence needs to be improved, since nutritional diets may not be so simply objective and they are inadequate to explain obvious underlining mechanisms. In addition, various compounds that may be ingested can affect molecular mechanisms, influenced by other external factors (drugs, pesticides, smoking, alcohol) and changes in human nutritional parameters. Artificial Intelligence has recently gained widespread interest and may have a role in accurate analysis of dietary patterns for optimal nutritional benefit. Therefore, future prospective randomized studies and objective measurements, consisting of molecular level analysis of the impact on cells and clear-cut methods are needed for accurate assessment of the effect of dietary habits on reproductive treatment.
Keywords: Sperm quality, oocyte quality, dietary pattern
Introduction
Diet in particular can affect oocyte and sperm quality in three ways. First, maternal nutrition is one of the most important causes affecting the gametes in utero (1). Second, an increase in body mass index (BMI) resulting from excessive dietary intake affects associated systemic and inflammatory processes (2). Finally, abrupt changes in the metabolic environment in the sperm/follicular fluid due to a variety of nutritional factors has also been shown to affect the quality of the gametes (3). Eating patterns, BMI, and nutritional consumption are among the modifiable factors known to affect infertility (4). Dietary patterns have also a substantial influence on metabolism through various regulatory mechanisms that lead to local and systemic hormonal changes.
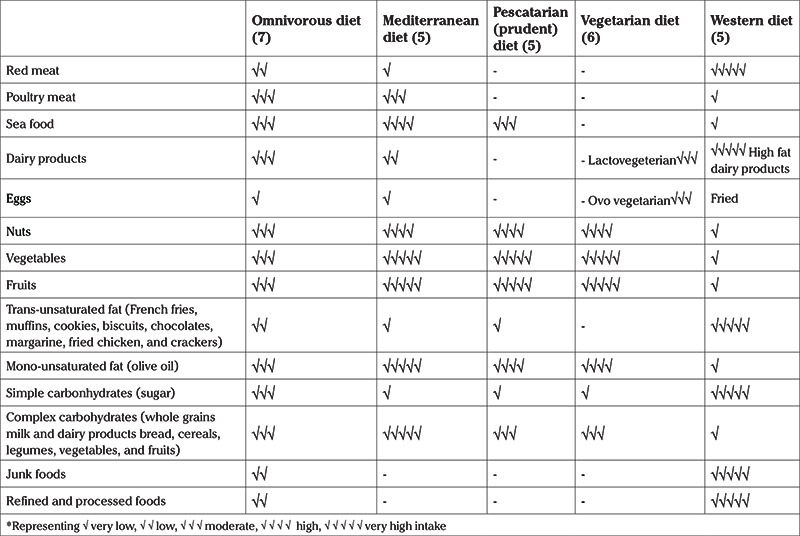
Global diets have been classified into four types based on different compositions, which include omnivorous, mediterranean, pescatarian (prudent), and vegetarian diets (5). A vegetarian diet excludes all meat, poultry, and seafood and includes a higher intake of fiber and usually a lower consumption of total and saturated fat, protein, vitamin B12, vitamin D, and calcium (6). However, the vegetarian diet may be sub-categorized into the Lacto-vegetarian diet, consisting of vegetarian diets and dairy products (milk, cheese, yogurt, and butter), Ovo-vegetarian diets allowing eggs but excluding dairy products, and Lacto-Ovo vegetarian diets that allow dairy products and eggs. Furthermore, vegan diets exclude all animal products, thus excludes meat, poultry, fish, eggs, and dairy products — and foods that contain these products. A pescatarian diet is largely vegetarian but includes seafood. A pescatarian diet may also completely or partially avoid meat and poultry, dairy and eggs in which case it is also known as a prudent diet. The Mediterranean diet is notable for increased consumption of fruits and vegetables, whole grains, sugars, oils, eggs, milk products, seafood, nuts, and moderate amounts of meat foods (poultry, pork, beef, lamb). Finally, the omnivorous diet includes all types of foods (7). The results of diet on oocyte and sperm quality, considering the amounts of macronutrients and vitamins and the role of essential fatty acids, proteins, vitamins, and minerals have been investigated. Studies have mostly compared Mediterranean and Western diets, whether healthy diet typified by the prudent or Mediterranean diet pattern is beneficial compared with the Western diet pattern that consists of richer saturated fats, red meat, junk foods, sweets, and excessive amounts of refined and processed foods (Table 1).
Table 1. Characteristics of different diet types.
Nutrients, including carbohydrates, fats, and proteins, provide energy for growth and repair of tissues and the production of enzymes, hormones, and fat-soluble vitamins (7). A usual diet consists of 55-65% carbohydrates, 30% fat, and 10-20% protein. All macronutrients obtained from energy and nutrients source rates show diversity (7).
Proteins
According to the European Food Safety Authority, for nitrogen balance, the recommended average daily protein intake is 0.66 g/kg body weight (8). Animal protein sources, such as red meat, poultry (usually chicken and turkey), various types of eggs, and dairy products (cheese, milk, whey) contain significant amounts of protein, micronutrients, and vitamins. Meat products are one of the most widely consumed and heavily investigated sources of protein. Several potential mechanisms could be mentioned to explain the reason behind meat consumption. In addition, a high intake of red meat may raise dietary iron intake. Studies of esophageal, stomach, and colon cancers have reported that excessive iron intake can increase oxidative stress that can promote chronic inflammatory processes and affect the immune system and may also damage tumor suppressor genes (9). Processed meat, such as salami and sausage, are modified by several methods, some of which involve the use of preservatives and flavourings that are used to extend shelf life and alter the flavor, respectively. Large epidemiological studies have shown that processed red meat consumption is associated with negative effects on sperm and oocyte quality by increased oxidative stress and production of reactive oxygen species (ROS) radicals (10).
Fatty acids
Fatty acids have a significant role in nutrition as they are high energy sources, contain fat-soluble vitamins and essential fatty acids, and are important for oxidative stability (11). Saturated fats account for approximately 10% of the energy in the American diet. The main sources of saturated fatty acids (SFA) in foods of animal origin are butter, cow's milk, meat, salmon, egg yolk, etc. Examples of plant product sources include chocolate and cocoa butter, coconut, and palm kernel oils. Transunsatured oil, contributing about 1-2% of the energy in the American diet, is produced commercially using a metal catalyst to partially hydrogenate vegetable oils in the presence of vacuum and high heat or may occur naturally in meat and dairy products where ruminants hydrogenize unsaturated fatty acids via bacterial enzymes (11).
Olive oil is a major source of monounsaturated fats and contains a wide range of valuable antioxidants and including superoxide and other reactive species (12). A major benefit of dietary fat intake is to increase the amount of long-chain omega-3 fatty acid (OM-3FAs) because they cannot be synthesized directly by the human body and must be obtained through diet. OM-3FAs are also potential precursors of lipid mediators that impact the inflammatory process, such as prostaglandin E3 (PGE3) and leukotriene B5 (LTB5) (12). Major dietary sources of OM-3FAs cold-water fishes, mussels, oysters, shrimps, oilseeds (almonds, walnuts, and hazelnuts), sesame, flaxseed, and canola (13). Studies have shown that increasing the ratio of long-chain omega-6 fatty acid (OM-6FA) to OM-3FA in the diet promotes chronic inflammatory diseases, including inflammatory bowel disease, asthma, rheumatoid arthritis and atherosclerosis. It has been suggested that the optimal ratio of omega-6 polyunsaturated fatty acid (6-PUFA) to omega-3 polyunsaturated fatty acid (3-PUFA) was 1:1, while in Western diets this ratio may be 16:1 (13). It has been demonstrated that consuming the Western diet for long periods promotes the production of ROS that may lead to insulin resistance and inflammation in various tissues, as well as overproduction of eicosanoids and proinflammatory cytokines (14).
Carbohydrates
Carbohydrates are the primary source of energy for the body, which include dietary fiber (soluble and insoluble), polysaccharides (starch found in plant food, such as bread and rice), monosaccharides (fructose, galactose, and glucose), and disaccharides (lactose, maltose, and sucrose) (15). Carbohydrate quality indicators are glycemic index (an index that shows the effect of carbohydrates on blood sugar), glycemic load (glycemic index times carbohydrate amount), and the extent of refined carbohydrate (whole grains versus refined grains), and the amount of dietary fiber (16).
Food products containing white flour increase the risk of obesity; therefore, it is important to not eat too many refined carbohydrates or too much food with a high glycemic index (17). It has been reported that very high sugar intake is related to elevated levels of estrogen in both animal and human models in males (18). Dietary carbohydrate intake can also have an important effect on inflammatory markers (19). Chronic exposure to postprandial hyperglycemia may induce oxidative damage by reducing plasma antioxidant defenses and increasing inflammation through free radical production (19).
Monoglutamate is the sole absorbable form of polyglutamate is converted from dietary folate with g-glutamyl hydrolase in the jejunum, and the activity of this enzyme is zinc-dependent (20). Moreover, zinc is a cofactor for homocysteine synthetase, which converts homocysteine to methionine and reduces homocysteine levels. The beneficial effects of zinc in interventional diet research are supported by randomized, placebo-controlled studies, where the administration of zinc and/or folic acid to sub-fertile patients has been shown to lead to a significant increase in semen concentration, from 18% to 74% (20). In addition, zinc, manganese, and selenium, all sourced from the diet, are cofactors for enzymes, including glutathione peroxidase or superoxide dismutase which are important protective enzymes against oxidative stress in reproductive cells (21).
The etiology of infertility factors remains unclear. Infertility can be associated with many physiological, environmental, and genetic factors, including chronic inflammation and oxidative stress. As far as nutrition is concerned, various components and nutrients have been proposed as possible determinants of normal functioning reproductive system over the last two decades (22). Similarly, several cross-sectional, case-control, retrospective, and prospective observational studies with large samples have investigated the relationship between diet and ovarian/semen quality and/or reproductive system with controversial results. Although there is a systematic review with meta-analysis of cohort studies that has carefully evaluated the contribution of the Mediterranean diet in improving sperm and oocyte quality, to the best of our knowledge there is no study that compares the results of both diets with a detailed information on the diet content (23).
The aim of this article was to discuss the effects of diet types, especially the Mediterranean and Western diets, on sperm and oocyte characteristics in the reproductive system and their impact on reproductive success in Assisted Reproductive Technologies (ART) treatments.
1. In utero impact of dietary patterns
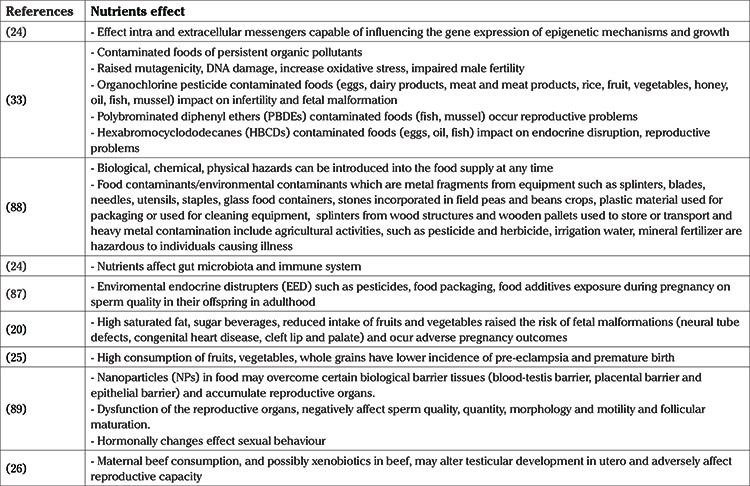
Nutrient patterns affect intracellular and extracellular messengers, which in turn affect epigenetic mechanisms that may alter gene expression in the future (24). Severe obstetric illnesses, such as preeclampsia and preterm birth, have a lower incidence in patients whose diets are rich in fruits, vegetables, and whole grains (25). In addition, increased intake of saturated fat and sugar-sweetened beverages increased the risk of fetal malformations (neural tube defects, congenital heart disease, cleft lip and/or palate) and adverse pregnancy outcomes (20). Furthermore, dietary patterns play an important role in the maturation of the fetal immune system and in the composition of the fetal gut microbiota, which is a metabolically and immunologically active system (24).
In a study by Swan et al. (26), weekly maternal beef consumption was inversely related to sperm concentration in the male offspring. High beef consumers (who consumed more than 7 grams of beef per week) were at greater risk of problems with sperm quality in their sons and that their sons had 24.3% lower sperm concentration in adulthood than those who consumed less beef (26). However, there are possible confounders for this so-called nutritional effect. It has been experimentally demonstrated that various environmental drugs and chemicals ingested with certain nutrients in foods during pregnancy and lactation may affect subsequent metabolic and reproductive function in the offspring (27,28,29). Swan et al. (26) also suggested that maternal beef consumption, possibly due to the effects of xenobiotics in red and processed meat, could transform fetal testicular development (26). They showed the effects of anabolic steroids (a xenobiotic agent) in red and processed meat, could transform fetal testicular development and negatively influence reproductive capacity. They also noted that regional variations in nutrition may alter the results, because most mothers in their study were living in North America and findings may not apply to other regions of the world where other agricultural methods may be used (26). Furthermore, environmental estrogens from polycarbonate plastic and metal cans containing antiandrogenic chemicals [bisphenol A (BPA) and PVC plastics in the resin coatings], and phytates used in many other products can cause abnormalities, including cryptorchidism and hypospadias, that affect sperm quality and reproductive ability in males (28). Another confounding factor for in utero impact of dietary patterns is recall error of maternal food consumption (Table 2).
Table 2. Nutritional factors affecting in utero reproductive cells.
2. The effect of dietary patterns on sperm quality
Human sperm quantitative and qualitative parameters decreased worldwide even though this situation caused a change in the normal values of WHO sperm parameters. A meta-analysis shows a global 32.5% deterioration in sperm concentration over a period of 50 years (30). Various and diverse environmental and dietary factors that have become a part of modern life may be responsible for this deterioration of sperm quality.
2.1. Dietary effects on hormonal parameters
Dietary patterns affect the hormonal axis in male reproductive function. Consumption of excess high-calorie foods, leading to increased adiposity and possibly obesity, results in increased aromatase enzyme activity and higher levels of systemic 17-oestradiol (E2) in the body. Increased E2 levels affect the hypothalamic-pituitary axis through negative feedback, which inhibits gonadotropin releasing hormone secretion and thus and pituitary gonadotropins secretions (31). Studies considering diet type show that high-energy foods (Western diet) not only reduce sperm quality but also lead to chronic illnesses, such as obesity and diabetes mellitus (32). Also, damage to sperm DNA mitochondrial activity and sperm quality, testosterone deficiency is associated with erectile dysfunction. Sex hormone-binding globulin also decreases due to obesity, increasing serum oestradiol levels, reducing the frequency of pulsatile luteinizing hormone levels. Increased adiposity also has some physical consequences, including increased scrotal temperatures which are known to decrease sperm quality (33). Furthermore, the disruption of antioxidant mechanisms seen in obesity because of high-calorie intake, impair sperm quality through impaired testosterone secretion and altered sperm DNA (4). Similarly, excessive trans fatty acids (TFA), saturated fat, cholesterol, or simply a high-calorie diet lead to gonadotoxicity and impair testicular physiology, disrupting spermatogenesis (31,32).
2.2. Dietary effects on sperm parameters
Various human diets can influence many biological pathways in a number of ways. Semen quality is affected by various antioxidants (coenzyme Q10, carnitine), homocysteine, vitamins B6 and B12, folic acid, zinc, and OM-3FA levels, the levels of all of which are at least partly dependent on diet. Assessment of food consumption as well as dietary patterns (the Mediterranean, prudent or Western diet) include modifiable factors (34,35) (Figure 1).
Figure 1.
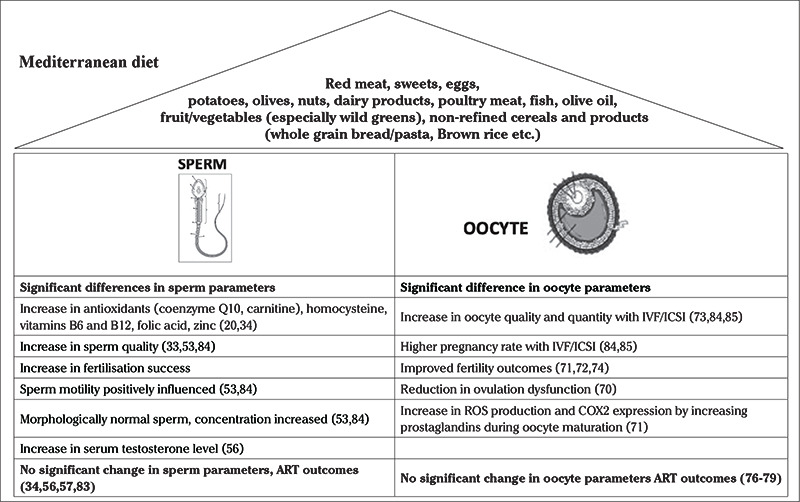
Impact of Mediterranean dietary patterns on female and male reproductive health
ART: Assisted Reproductive Technologies, IVF: In vitro fertilization, ICSI: Intracytoplasmic Sperm Injection, ROS: Reactive oxygen species
2.2.1. The effect of the Western diet on sperm parameters
Higher consumption of unhealthy dietary components, such as rich full-fat dairy food, sweets, and processed meat, that are characteristic of the Western diet has been associated with decreased semen quality, evaluated by various parameters including volume of the ejaculate, sperm concentration, total sperm count, progressive motility, total non-motile and total motile sperm count, DNA fragmentation index, and poor fertilization rate or pregnancy rate (36). In addition, the Western diet can lead to mitochondrial dysfunction and can induce oxidant/antioxidant imbalance in testicular tissue, amongst others. This may lead to cellular destruction because of directly damaged lipid membranes, and damage to amino acids, and nucleic acids through sperm peroxidation. ROS occur as a consequence of natural spermatogenesis, which is qualified as a response to the acrosome formation field (4). Also, ROS can lead to insulin resistance, oxidative stress, and inflammation in viscous tissues as well as the overproduction of eicosanoids and proinflammatory cytokines (37). In addition, ROS reduces the presence of adenosine triphosphate in sperm while increasing the risk of agglutination and decreasing mobility. This also prevents sperm from fertilizing oocytes, leading to increased apoptosis, reduced sperm acrosomal function, and lower chances of fertilization by direct damage to the sperm DNA (4). In general, data from animal models suggest that the Western diet generally correlates with decreased sperm quality, especially in terms of diminished motility and impaired sperm capacity, along with reduced sperm binding capacity to oocytes (38,39). Western diet increases testicular fatty acid and cholesterol content while altering sperm plasma membrane composition and sperm membrane-related events (40). Remarkably, sperm quality depends on high percentage of SFA and TFA which are common in the Western diet (34,41). In particular, studies have shown that consumption of high-energy diets disrupts mitochondrial function in the testicular bioenergetic state (39). Since these fatty acids are not endogenously produced in the body, excessive consumption contributes to the accumulation of fat in various organs such as testicular tissue, and the amount is inversely related to sperm counts (41,42). In conclusion, research has shown that the Western diet is directly related to diminished sperm concentration, altered sperm morphology, and asthenozoospermia (43,44,45,46) (Figure 2).
Figure 2.
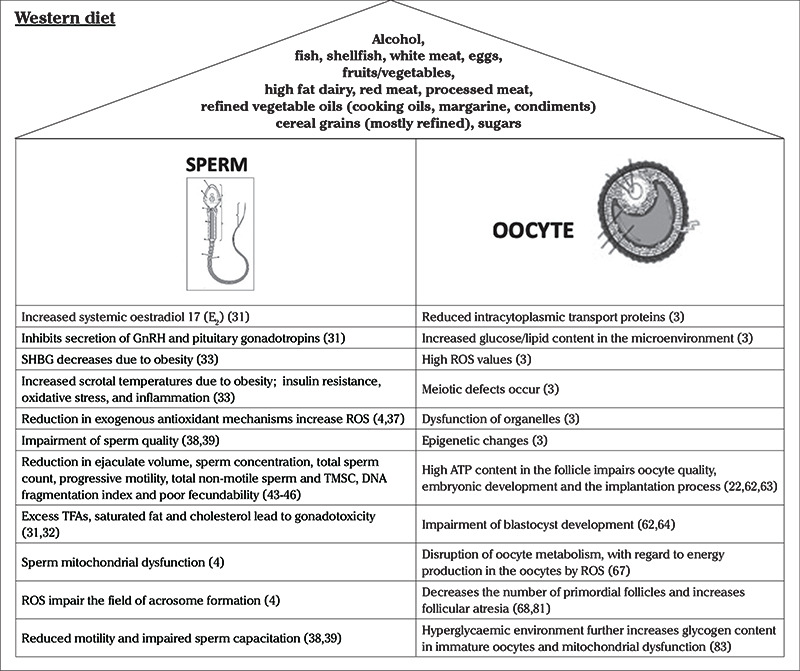
Impact of Western dietary patterns on female and male reproductive health
GnRH: Gonadotropin releasing hormone, SHBG: Sex hormone-binding globülin, ROS: Reactive oxygen species, TMSC: Total motile sperm count, TFA: Trans fatty acids
2.2.2. The effect of a Mediterranean diet on sperm parameters
In a review of 23 studies from 502 articles, the results confirmed the relationship between improved semen parameters and maintaining a healthy diet, while diets rich in lipophilic foods, soy isoflavones, and sweets resulted in impaired semen quality. The same authors report that despite the lack of underlying mechanisms and randomized controlled trials, dietary quality, and assessment of nutrient intake are important in the diagnosis and treatment of male factor infertility (47). Attaman et al. (48) showed a moderately significant association between dietary fatty acids and semen quality. They found that the total number and concentration of sperm depended on daily consumption of saturated fat and TFA (48). Although sperm membranes consist of cholesterol, rising ratios in sperm membranes disrupt membrane structure and fluidity. Moreover, minimal changes in dietary cholesterol levels can result in differences in membrane cholesterol concentrations that are reflected in acrosome reaction and a decrease in capacitance in an animal study (49). Several studies have shown that higher intake of components such as legumes, vegetables, especially dark green vegetables, cereals, fruits, and PUFAs from olive oil in a balanced diet are associated with high sperm concentration and progressive mobility (20,50,51,52,53). Additionally, folate-rich fruits and vegetables, along with antioxidants such as b-carotene, lutein, and lycopene, can improve sperm quality (21,45,54). A case study comparing dietary habits in normozoospermic and oligoasthenoteratospermic patients showed that the former group were more likely to regularly consume certain fruits and vegetables, such as lettuce, tomatoes, peaches, and apricots (45). Consumption of fruits and vegetables is important for males when considering the successful fertilization with in vitro fertilization (IVF) (52). In an observational study of 250 patients undergoing Intracytoplasmic Sperm Injection (ICSI), sperm motility was positively influenced by fruit and cereal consumption (50). In addition, it has been shown that pesticides, which may be present in fruits and vegetables, can lead to less morphologically normal spermatozoa and lower sperm concentration and motility (45,50).
Consumption of fresh fruits, vegetables, chicken, light dairy products, and seafood decreases the risk of asthenozoospermia, while red meat consumption and high blood glucose levels increase this risk (45,51,55). Jurewicz et al. (56) reported on 336 patients attending the infertility clinic with slight oligoastenospermia (20 to 300 mln/mL sperm concentration) after sub-dividing the men into three groups based on the diet: Western; prudent; or mixed. In the prudent diet group, the relationship between serum testosterone levels and sperm concentration was significant. Additionally, they showed that a prudent diet prevents sperm DNA from fragmentation (34,56).
However, such an association of better sperm parameters with dietary pattern was not found in various other studies (34,57,58). Some studies have reported that nutritional factors do not affect live birth rate, while others show data on improving sperm parameters. The evidence is not entirely consistent, and different findings from different studies may be due to a number of reasons including that various populations were studied, study designs were different, and variable quality of the studies (33). The studies suggest that the relationship between diet and semen quality does not affect ART outcomes, such as fertilization rate, implantation, clinical pregnancy, and live birth rate (57,58). Li et al. (59) showed that vitamin C and β-carotene intake and ART treatment were positively related with fertilization rates in men attending infertility clinics, although no association was found with pregnancy or live birth rate (59). The relationship between lifestyle factors and semen quality remains unclear due to methodological differences (60).
3. The effect of dietary patterns on oocyte quality
Oocyte growth and maturation are affected by endocrine, nutritional, and chemical factors. There is a variety of dietary effects on oocyte function and ovulation, such as glycemic load, antioxidant and anti-inflammatory processes, pro-estrogenic and anti-estrogenic hormonal effects, and the impact of fatty acids (16). Reduced intracytoplasmic transport proteins, raised glucose/lipid ratio, and elevated ROS levels in oocytes can result in meiotic defects, organelle dysfunction, and epigenetic changes (3). Oxidative damage to gametes can lead to the rearrangement of DNA through various enzymatic changes.
3.1. Hormonal effects on oocyte quality and embryo production
At the cellular level, high BMI-related hyperinsulinemia, lipotoxicity, oxidative stress on the endoplasmic reticulum (ER) and mitochondria, leptin, and adiponectin reduce insulin sensitivity and activate related inflammatory systems in obese women (61). In addition, animal studies suggest that hyperinsulinemia (as a result of a high-fat diet) and high follicular ATP content affect oocyte quality, embryonic development, and the implantation process (22,62,63). In animal studies, maternal hyperglycemia, high-fat diet, and obesity have been shown to adversely affect the progression of the blastocyst (62,64). Furthermore, a high BMI is unlikely to affect endometrial receptivity and cause an implantation failure, compared to its effect on oocyte quality, which is diminished in people who have obesity (61,65). These findings suggest that exposure to abnormal metabolic conditions during oogenesis and fertilization causes morphological changes in the programming of fetal tissues (66). Also, some studies have shown that high-fat diets (Western diet) are related to elevated serum estradiol, estrone sulfate, and estrone levels in premenopausal women (67). For example, mice studies demonstrated that a Western diet reduces primordial follicle numbers and increased follicular atresia that may shorten the reproductive life span of women (68), and this has been associated with the development of inflammation (69).
3.2. Dietary effects on oocyte quality and ART parameters
3.2.1. The effect of a Mediterranean diet on oocyte quality and ART outcomes
The Nurses’ Health Study 2 evaluated the effectiveness of an investigator-defined “fertility diet”, which showed that consumption of monounsaturated fats, low-glycemic carbohydrates, high-fat dairy products, multivitamins, and plant-derived iron and “fertility diet” supplements was associated with a lower risk of infertility due to ovulatory dysfunction (relative risk: 0.34; 95% confidence interval: 0.23-0.48) (70). The effect of a Mediterranean diet on oocyte function was found to increase ROS production and COX2 expression by increasing prostaglandins in oocyte maturation (71). In a review of 62 articles regarding lifestyle and ART, it was concluded that the success of ART is dependent on the implementation of healthy lifestyle counseling programs, especially by implementing fruits, vegetables, and unsaturated fat in a healthy balanced diet (72). A recent prospective cohort study by Jahangirifar et al. (73) analyzed the connection between maternal nutritional patterns and reproductive status in infertile women. They analyzed 140 primary infertility patients who underwent gonadotropin antagonist protocol treatment. In the study, total oocyte and metaphase II oocyte count, fertilization rate, embryo quality, and biochemical and clinical pregnancy rates were compared between a healthy diet and a Western diet. The authors showed that healthy nutrition may increase the quality and quantity of oocytes through high levels of antioxidant in fresh vegetables, fruits, and nuts in a healthy diet. An unhealthy diet can adversely affect the chances of getting pregnant. However, the fertilization rate and quality of embryo were not affected by diet. Toledo et al. (74) report a prospective cohort study with 161 infertile couples who received IVF/ICSI therapy and showed that patients who followed the Mediterranean diet had a 40% higher pregnancy rate. The authors suggested that the reason for this was due to the fact that the Mediterranean diet is high in vegetable oils which are rich in linoleic acid (74). In a review of 351 couples undergoing IVF treatment, consumption of fruits and vegetables was examined. It was shown that healthy eating patterns that include whole grains, fish, fruits, vegetables, and olive oil, not only improve overall health but also fertility outcomes (75). Also, in their prospective cohort study, Ricci et al. (76) concluded that the Mediterranean diet affected oocyte numbers and clinical pregnancy rates in women over 35 years of age, but not live birth rates. On the other hand, a meta-analysis by Sanderman et al. (77) suggested not recommending a single dietary pattern to improve pregnancy or live birth rates in female infertility undergoing IVF treatment. Such dietary pattern associations and conclusions were not revealed in other studies (76,78,79).
3.2.2. The effect of Western diet on oocyte quality and ART outcomes
Graier et al. (80) showed that triglyceride droplets and free fatty acids accumulate when the oocyte was exposed to a high lipid environment, and this caused significant damage to the ER and mitochondria, leading to lipotoxicity. Furthermore, Nehra et al. (81) demonstrated that increased OM-3FA consumption improved maternal reproductive function in rats compared to OM-6FA, which was associated with very poor reproductive success in older ages. These data suggest that the Western diet may disrupt oocyte metabolism, in terms of energy production in oocytes through ROS. Furthermore, a high glycemic index diet induced an inflammatory process and increased the formation and persistence of bacterial vaginosis (82). Mtango et al. (83) showed that during the fertilization and implantation process, female mice following a normal diet for 4-5 days, with low-protein diets, had fewer embryos, lower birth weight, and compensatory post-natal weight gain, hypertension, and changes in organ/body weight ratios in the adulthood. This increased free glucose levels in mouse oocytes, hence the hyperglycaemic environment further increased glycogen content in immature oocytes and mitochondrial dysfunction occured (Figure 2).
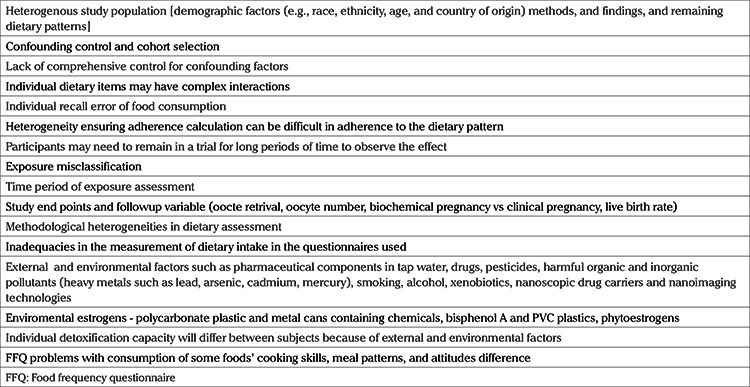
The limitations of nutritional studies
Epidemiologic and observational studies are considered the sole evidence for nutrition studies but are associated with various limitations, including methodological differences and design faults, tiny groups, short-term follow-ups, poorly conceived endpoints, confounding circumstances, understandably limited numbers of interventional studies, the absence of placebo, poor matching of subjects and non-standardized dosing (4). Recording of dietary habits of individuals include foods regularly consumed over a certain period of time (months or years) and usually do not include specific irregularities that are consumed only for a few days/weeks. In addition, dietary adherence (low, moderate, high) is modified when considering the dietary effect calculated in frequency questionnaire (FFQ). Sun et al. (84) found in a study of 590 patients that significant increase in embryo numbers with ART were achieved in patients who adhered more to the Mediterranean diet model (84). However, it cannot be generalized for all reproductive population or for those attending infertility clinics (84,85). A FFQ with a verified semi-quantitative 165-item was utilized to collect dietary data. The use of FFQs to measure nutritional habits in studies is a major confounder for study comparability, as FFQs do not record the consumption of some specific but possibly key food items, variability in cooking skills, meal patterns, and differences in attitudes to food. Artificial intelligence (AI) may be adapted for dietary pattern analysis and detection of nutritional problems, image diagnosis, and personalized nutrition for solving this problem (86).
Confounding factors
In this industrial millennial age, uncontaminated food stuffs are an increasing rarity. One should always keep in mind that food, especially processed food, is under direct contamination by various intentional and unintentional factors, such as environmental supplemental chemicals, classified into different functional categories including pesticides, food packaging, food additives, hormones, polycarbonate plastic and metals (29). At present, one of the most common intentional but unnatural processes in meat production is the administration of estrogen-containing anabolic supplements to farm animals and animal feeds in order to increase animal weight (87). Hence, when we talk about the downside of meat consumption and its fertility effects, we can actually never talk about pure meat.
Some of the factors affecting human reproduction include air pollution, smoking, lack of exercise, obesity, drug use, additives in beverages, phthalates, a group of chemicals used to make plastics more durable, organochlorine pollutants, and stress (33) but evidence linking chronic low-dose environmental exposures and fertility is weak. However, with the growing industry and lifestyle changes, new chemicals and compounds are emerging as threats to reproductive cells. Among these, compounds include pharmaceutical contamination of tap water, organochlorine pollutants in fruit and vegetables, BPA in plastic bottles, phthalates in skin care products, heavy metals and xenobiotics, such as antibiotics, herbicides, pesticides in various foods and food additives like flavor enhancers (monosodium glutamate) are all the focus of research into reproductive cells (88). Indeed, in the EARTH study conducted in 799 women and 487 men (89), some phthalate metabolites were associated with lower oocyte yield, lower clinical pregnancy likelihood, increased risk of pregnancy loss, and lower likelihood of live birth after infertility treatment in women. Certain urinary concentrations of phthalate metabolites have also been associated with lower implantation and live birth rates in men. Maternal soy and folic acid intake significantly altered the association between BPA and IVF outcomes in women (89). There are other harmful organic and inorganic pollutants, such as metal parts in ground meat, bone fragments, product packaging pieces, stones, insects, or other personal items, and heavy metals (lead, arsenic, cadmium, mercury) can have detrimental effects on reproductive cells (88). Considering the fertility impact, various issues should be regarded as confounding factors, not only health related maternal problems but also the detoxification capacity of the mother and the offspring. Additionally, lifestyle factors, such as smoking and lack of exercise can alter the balance between ROS and antioxidant protection. Gene expression of epigenetic mechanisms and growth may also be altered.
In addition, the recent development of nanometre-sized materials in medicine is another point that needs to be addressed. Nanoparticles are used in all fields of life, including pharmacology, medicine, chemistry, physics, materials science, engineering and industry, cosmetics and clothing, and food. Nanoscopic drug carriers and nanoimaging technologies can overcome certain biological barriers, such as the blood-testis barrier, placental barrier and epithelial barrier, and accumulate in reproductive organs. This accumulation affects Sertoli and Leydig cell function, the epididymis, ovaries and uterus, and may lead to dysfunction of the reproductive organs, adversely affecting sperm quality, quantity, morphology and motility, and reducing the number of mature eggs and follicular development. Hormonally induced changes in sexual behavior may also be altered (90).
While some researchers have examined the effects of diet on sperm parameters in the general population (32,34,91), others evaluated the effects of diet only on infertile patients who are admitted to the fertility outpatient clinics (20,21,43,45,48,50,51,54,56,92). The results showed that some discrepancies occur in the differential effects of diet in fertile and infertile men, but in short, diets containing fruits and vegetables, fish, or low-fat dairy products are associated with better semen quality. Another problem is that some studies compare the diet effects on IVF success rates that include biochemical pregnancies, that is pregnancy diagnosed only by detection of human β-choriongonadotropin in serum or urine (20,78,84,85), while others compare clinical pregnancies, defined as pregnancy diagnosed by ultrasound examination of one or more gestational sacs or by clear clinical signs of pregnancy or live births (after 22 completed weeks of gestation) (76,78,85). Many beneficial effects of a healthy diet, and recommendations can be provided with confidence, but more studies are currently needed to clarify the findings of underlying mechanisms (33) (Table 3).
Table 3. Confounding factors in nutrition studies.
Conclusion
Research in this field has shown that foods rich in fibers, folate, fruits and vegetables, seafood, poultry, nuts, whole grains, and PUFAs can increase sperm quality. Furthermore, animal proteins, unsaturated fats, and vegetable proteins can improve fertility and induce ovulation. Current studies are based mostly on animal models and the exact effects on humans are still yet to be discovered. Therefore, the dietary effects on human infertility are not conclusive. The evidence of the role of the diet on male and female fertility is weak or of very low quality. In addition, well-constructed, randomized controlled trials into diet models are needed to define the effect of a healthy diet on the quality of reproductive cells. As dietary habits vary from society to society and even from person to person obtaining clear evidence into this topic is challenging. Improved nutrition may be possible through more effective public health intervention programs that are tailored by specific nutrition characteristics and the health concerns closely associated with family planning.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Surgical and Medical Practices: N.A., J.B.P.; Concept: N.A., M.N.C.K., J.B.P.; Design: N.A., J.B.P.; Data Collection or Processing: N.A.; Analysis or Interpretation: N.A.; Literature Search: N.A., M.N.C.K.; Writing: N.A., M.N.C.K., J.B.P.
Conflict of Interest: No conflict of interest is declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.
References
- 1.Barker DJ. Fetal origins of coronary heart disease. BMJ. 1995;311:171–4. doi: 10.1136/bmj.311.6998.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Practice Committee of the American Society for Reproductive Medicine and the Practice Committee of the Society for Reproductive Endocrinology and Infertility. Electronic address: asrm@asrm.org. Optimizing natural fertility: a committee opinion. Fertil Steril. 2022;117:53–63. [Google Scholar]
- 3.Gu L, Liu H, Gu X, Boots C, Moley KH, Wang Q. Metabolic control of oocyte development: linking maternal nutrition and reproductive outcomes. Cell Mol Life Sci. 2015;72:251–71. doi: 10.1007/s00018-014-1739-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alom M, Wymer K, Trost L. The Impact of Lifestyle Factors on Male Reproduction: Body Composition, Diet, Exercise, and Recreational Drug Use. Bioenvironmental Issues Affecting Men's Reproductive and Sexual Health: Elsevier. 2018;. p.:85–105. [Google Scholar]
- 5.Tilman D, Clark M. Global diets link environmental sustainability and human health. Nature. 2014;515:518–22. doi: 10.1038/nature13959. [DOI] [PubMed] [Google Scholar]
- 6.Turner-McGrievy GM, Wirth MD, Shivappa N, Wingard EE, Fayad R, Wilcox S, et al. Randomization to plant-based dietary approaches leads to larger short-term improvements in Dietary Inflammatory Index scores and macronutrient intake compared with diets that contain meat. Nutr Res. 2015;35:97–106. doi: 10.1016/j.nutres.2014.11.007. [DOI] [PubMed] [Google Scholar]
- 7.Berdanier CD. Advanced nutrition: macronutrients. CRC press. 2018. [Google Scholar]
- 8.EFSA Panel on Dietetic Products, Nurtrition and Allergies. Scientific opinion on dietary reference values for protein. EFSA Journal. 2012;10:2557. [Google Scholar]
- 9.Ward MH, Cross AJ, Abnet CC, Sinha R, Markin RS, Weisenburger DD. Heme iron from meat and risk of adenocarcinoma of the esophagus and stomach. Eur J Cancer Prev. 2012;21:134–8. doi: 10.1097/CEJ.0b013e32834c9b6c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tremellen K. Treatment of sperm oxidative stress: a collaborative approach between clinician and embryologist. Oxidants, Antioxidants and Impact of the Oxidative Status in Male Reproduction: Elsevier. 2019;. p.:225–35. [Google Scholar]
- 11.de Souza RJ, Mente A, Maroleanu A, Cozma AI, Ha V, Kishibe T, et al. Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. BMJ. 2015;351:h3978. doi: 10.1136/bmj.h3978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Psaltopoulou T, Kosti RI, Haidopoulos D, Dimopoulos M, Panagiotakos DB. Olive oil intake is inversely related to cancer prevalence: a systematic review and a meta-analysis of 13,800 patients and 23,340 controls in 19 observational studies. Lipids Health Dis. 2011;10:127. doi: 10.1186/1476-511X-10-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wall R, Ross RP, Fitzgerald GF, Stanton C. Fatty acids from fish: the anti-inflammatory potential of long-chain omega-3 fatty acids. Nutr Rev. 2010;68:280–9. doi: 10.1111/j.1753-4887.2010.00287.x. [DOI] [PubMed] [Google Scholar]
- 14.Attaman JA, Stanic AK, Kim M, Lynch MP, Rueda BR, Styer AK. The anti-inflammatory impact of omega-3 polyunsaturated Fatty acids during the establishment of endometriosis-like lesions. Am J Reprod Immunol. 2014;72:392–402. doi: 10.1111/aji.12276. [DOI] [PubMed] [Google Scholar]
- 15.Ludwig DS, Hu FB, Tappy L, Brand-Miller J. Dietary carbohydrates: role of quality and quantity in chronic disease. BMJ. 2018;361:k2340. doi: 10.1136/bmj.k2340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chiu YH, Chavarro JE, Souter I. Diet and female fertility: doctor, what should I eat? Fertil Steril. 2018;110:560–9. doi: 10.1016/j.fertnstert.2018.05.027. [DOI] [PubMed] [Google Scholar]
- 17.Drewnowski A, Kurth C, Holden-Wiltse J, Saari J. Food preferences in human obesity: carbohydrates versus fats. Appetite. 1992;18:207–21. doi: 10.1016/0195-6663(92)90198-f. [DOI] [PubMed] [Google Scholar]
- 18.El Hafidi M, Pérez I, Carrillo S, Cardoso G, Zamora J, Chavira R, et al. Effect of sex hormones on non-esterified fatty acids, intra-abdominal fat accumulation, and hypertension induced by sucrose diet in male rats. Clin Exp Hypertens. 2006;28:669–81. doi: 10.1080/10641960601013617. [DOI] [PubMed] [Google Scholar]
- 19.Galland L. Diet and inflammation. Nutr Clin Pract. 2010;25:634–40. doi: 10.1177/0884533610385703. [DOI] [PubMed] [Google Scholar]
- 20.Vujkovic M, de Vries JH, Dohle GR, Bonsel GJ, Lindemans J, Macklon NS, et al. Associations between dietary patterns and semen quality in men undergoing IVF/ICSI treatment. Hum Reprod. 2009;24:1304–12. doi: 10.1093/humrep/dep024. [DOI] [PubMed] [Google Scholar]
- 21.Benatta M, Kettache R, Buchholz N, Trinchieri A. The impact of nutrition and lifestyle on male fertility. Arch Ital Urol Androl. 2020;92. doi: 10.4081/aiua.2020.2.121. [DOI] [PubMed] [Google Scholar]
- 22.Van Blerkom J, Davis PW, Lee J. ATP content of human oocytes and developmental potential and outcome after in-vitro fertilization and embryo transfer. Hum Reprod. 1995;10:415–24. doi: 10.1093/oxfordjournals.humrep.a135954. [DOI] [PubMed] [Google Scholar]
- 23.Muffone ARMC, de Oliveira Lübke PDP, Rabito EI. Mediterranean diet and infertility: a systematic review with meta-analysis of cohort studies. Nutr Rev. 2022;nuac087. doi: 10.1093/nutrit/nuac087. [DOI] [PubMed] [Google Scholar]
- 24.Indrio F, Mestrovic J, Carrasco-Sanz A, Vural M, Namazova-Baranova L, Giardino I, et al. Overview on child health, nutrition and food hazards during the first thousand days of life. Global Pediatrics. 2022;2:100018. [Google Scholar]
- 25.Englund-Ögge L, Brantsæter AL, Sengpiel V, Haugen M, Birgisdottir BE, Myhre R, et al. Maternal dietary patterns and preterm delivery: results from large prospective cohort study. BMJ. 2014;348:g1446. doi: 10.1136/bmj.g1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Swan SH, Liu F, Overstreet JW, Brazil C, Skakkebaek NE. Semen quality of fertile US males in relation to their mothers’ beef consumption during pregnancy. Hum Reprod. 2007;22:1497–502. doi: 10.1093/humrep/dem068. [DOI] [PubMed] [Google Scholar]
- 27.vom Saal FS. Could hormone residues be involved? Hum Reprod. 2007;22:1503–5. doi: 10.1093/humrep/dem092. [DOI] [PubMed] [Google Scholar]
- 28.vom Saal FS, Hughes C. An extensive new literature concerning low-dose effects of bisphenol A shows the need for a new risk assessment. Environ Health Perspect. 2005;113:926–33. doi: 10.1289/ehp.7713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Istvan M, Rahban R, Dananche B, Senn A, Stettler E, Multigner L, et al. Maternal occupational exposure to endocrine-disrupting chemicals during pregnancy and semen parameters in adulthood: results of a nationwide cross-sectional study among Swiss conscripts. Hum Reprod. 2021;36:1948–58. doi: 10.1093/humrep/deab034. [DOI] [PubMed] [Google Scholar]
- 30.Sengupta P, Dutta S, Krajewska-Kulak E. The Disappearing Sperms: Analysis of Reports Published Between 1980 and 2015. Am J Mens Health. 2017;11:1279–304. doi: 10.1177/1557988316643383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rato L, Alves MG, Cavaco JE, Oliveira PF. High-energy diets: a threat for male fertility? Obes Rev. 2014;15:996–1007. doi: 10.1111/obr.12226. [DOI] [PubMed] [Google Scholar]
- 32.Morgan DH, Ghribi O, Hui L, Geiger JD, Chen X. Cholesterolenriched diet disrupts the blood-testis barrier in rabbits. Am J Physiol Endocrinol Metab. 2014;307:E1125–30. doi: 10.1152/ajpendo.00416.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ricci E, Al-Beitawi S, Cipriani S, Alteri A, Chiaffarino F, Candiani M, et al. Dietary habits and semen parameters: a systematic narrative review. Andrology. 2018;6:104–16. doi: 10.1111/andr.12452. [DOI] [PubMed] [Google Scholar]
- 34.Gaskins AJ, Colaci DS, Mendiola J, Swan SH, Chavarro JE. Dietary patterns and semen quality in young men. Hum Reprod. 2012;27:2899–907. doi: 10.1093/humrep/des298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dcunha R, Hussein RS, Ananda H, Kumari S, Adiga SK, Kannan N, et al. Current Insights and Latest Updates in Sperm Motility and Associated Applications in Assisted Reproduction. Reprod Sci. 2022;29:7–25. doi: 10.1007/s43032-020-00408-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oostingh EC, Steegers-Theunissen RP, de Vries JH, Laven JS, Koster MP. Strong adherence to a healthy dietary pattern is associated with better semen quality, especially in men with poor semen quality. Fertil Steril. 2017;107:916–23. doi: 10.1016/j.fertnstert.2017.02.103. [DOI] [PubMed] [Google Scholar]
- 37.Farooqui AA, Farooqui T. Effects of Western, Mediterranean, vegetarian, and Okinawan diet patterns on human brain. Role of the Mediterranean diet in the brain and neurodegenerative diseases: Elsevier. 2018;. p.:317–32. [Google Scholar]
- 38.Fernandez CD, Bellentani FF, Fernandes GS, Perobelli JE, Favareto AP, Nascimento AF, et al. Diet-induced obesity in rats leads to a decrease in sperm motility. Reprod Biol Endocrinol. 2011;9:32. doi: 10.1186/1477-7827-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rato L, Alves MG, Dias TR, Lopes G, Cavaco JE, Socorro S, et al. High-energy diets may induce a pre-diabetic state altering testicular glycolytic metabolic profile and male reproductive parameters. Andrology. 2013;1:495–504. doi: 10.1111/j.2047-2927.2013.00071.x. [DOI] [PubMed] [Google Scholar]
- 40.Diaz-Fontdevila M, Bustos-Obregón E. Cholesterol and polyunsaturated acid enriched diet: effect on kinetics of the acrosome reaction in rabbit spermatozoa. Mol Reprod Dev. 1993;35:176–80. doi: 10.1002/mrd.1080350211. [DOI] [PubMed] [Google Scholar]
- 41.Halton TL, Willett WC, Liu S, Manson JE, Stampfer MJ, Hu FB. Potato and french fry consumption and risk of type 2 diabetes in women. Am J Clin Nutr. 2006;83:284–90. doi: 10.1093/ajcn/83.2.284. [DOI] [PubMed] [Google Scholar]
- 42.Luiken JJ, Bonen A, Glatz JF. Cellular fatty acid uptake is acutely regulated by membrane-associated fatty acid-binding proteins. Prostaglandins Leukot Essent Fatty Acids. 2002;67:73–8. doi: 10.1054/plef.2002.0401. [DOI] [PubMed] [Google Scholar]
- 43.Eslamian G, Amirjannati N, Rashidkhani B, Sadeghi MR, Baghestani AR, Hekmatdoost A. Adherence to the Western Pattern Is Potentially an Unfavorable Indicator of Asthenozoospermia Risk: A Case-Control Study. J Am Coll Nutr. 2016;35:50–8. doi: 10.1080/07315724.2014.936983. [DOI] [PubMed] [Google Scholar]
- 44.Liu CY, Chou YC, Chao JC, Hsu CY, Cha TL, Tsao CW. The Association between Dietary Patterns and Semen Quality in a General Asian Population of 7282 Males. PLoS One. 2015;10:e0134224. doi: 10.1371/journal.pone.0134224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mendiola J, Torres-Cantero AM, Moreno-Grau JM, Ten J, Roca M, Moreno-Grau S, et al. Food intake and its relationship with semen quality: a case-control study. Fertil Steril. 2009;91:812–8. doi: 10.1016/j.fertnstert.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 46.Bakos HW, Mitchell M, Setchell BP, Lane M. The effect of paternal diet-induced obesity on sperm function and fertilization in a mouse model. Int J Androl. 2011;34:402–10. doi: 10.1111/j.1365-2605.2010.01092.x. [DOI] [PubMed] [Google Scholar]
- 47.Giahi L, Mohammadmoradi S, Javidan A, Sadeghi MR. Nutritional modifications in male infertility: a systematic review covering 2 decades. Nutr Rev. 2016;74:118–30. doi: 10.1093/nutrit/nuv059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Attaman JA, Toth TL, Furtado J, Campos H, Hauser R, Chavarro JE. Dietary fat and semen quality among men attending a fertility clinic. Hum Reprod. 2012;27:1466–74. doi: 10.1093/humrep/des065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saez Lancellotti TE, Boarelli PV, Monclus MA, Cabrillana ME, Clementi MA, Espínola LS, et al. Hypercholesterolemia impaired sperm functionality in rabbits. PLoS One. 2010;5:e13457. doi: 10.1371/journal.pone.0013457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Braga DP, Halpern G, Figueira Rde C, Setti AS, Iaconelli A Jr, Borges E Jr. Food intake and social habits in male patients and its relationship to intracytoplasmic sperm injection outcomes. Fertil Steril. 2012;97:53–9. doi: 10.1016/j.fertnstert.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 51.Eslamian G, Amirjannati N, Rashidkhani B, Sadeghi MR, Hekmatdoost A. Intake of food groups and idiopathic asthenozoospermia: a case-control study. Hum Reprod. 2012;27:3328–36. doi: 10.1093/humrep/des311. [DOI] [PubMed] [Google Scholar]
- 52.Chavarro JE. Healthy diets and men's contribution to fertility; is semen quality good enough? Fertil Steril. 2017;107:906–7. doi: 10.1016/j.fertnstert.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 53.Salas-Huetos A, James ER, Aston KI, Jenkins TG, Carrell DT. Diet and sperm quality: Nutrients, foods and dietary patterns. Reprod Biol. 2019;19:219–24. doi: 10.1016/j.repbio.2019.07.005. [DOI] [PubMed] [Google Scholar]
- 54.Chiu YH, Gaskins AJ, Williams PL, Mendiola J, Jørgensen N, Levine H, et al. Intake of Fruits and Vegetables with Low-to-Moderate Pesticide Residues Is Positively Associated with Semen-Quality Parameters among Young Healthy Men. J Nutr. 2016;146:1084–92. doi: 10.3945/jn.115.226563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hatch EE, Wesselink AK, Hahn KA, Michiel JJ, Mikkelsen EM, Sorensen HT, et al. Intake of Sugar-sweetened Beverages and Fecundability in a North American Preconception Cohort. Epidemiology. 2018;29:369–78. doi: 10.1097/EDE.0000000000000812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jurewicz J, Radwan M, Sobala W, Radwan P, Bochenek M, Hanke W. Dietary Patterns and Their Relationship with Semen Quality. Am J Mens Health. 2018;12:575–83. doi: 10.1177/1557988315627139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Salas-Huetos A, Mínguez-Alarcón L, Mitsunami M, Arvizu M, Ford JB, Souter I, et al. Paternal adherence to healthy dietary patterns in relation to sperm parameters and outcomes of assisted reproductive technologies. Fertil Steril. 2022;117:298–312. doi: 10.1016/j.fertnstert.2021.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mitsunami M, Salas-Huetos A, Mínguez-Alarcón L, Attaman JA, Ford JB, Kathrins M, et al. A dietary score representing the overall relation of men's diet with semen quality in relation to outcomes of infertility treatment with assisted reproduction. F S Rep. 2021;2:396–404. doi: 10.1016/j.xfre.2021.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Li MC, Chiu YH, Gaskins AJ, Mínguez-Alarcón L, Nassan FL, Williams PL, et al. Men's Intake of Vitamin C and β-Carotene Is Positively Related to Fertilization Rate but Not to Live Birth Rate in Couples Undergoing Infertility Treatment. J Nutr. 2019;149:1977–84. doi: 10.1093/jn/nxz149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Danielewicz A, Przybyłowicz KE, Przybyłowicz M. Dietary Patterns and Poor Semen Quality Risk in Men: A Cross-Sectional Study. Nutrients. 2018;10:1162. doi: 10.3390/nu10091162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bellver J, Busso C, Pellicer A, Remohí J, Simón C. Obesity and assisted reproductive technology outcomes. Reprod Biomed Online. 2006;12:562–8. doi: 10.1016/s1472-6483(10)61181-9. [DOI] [PubMed] [Google Scholar]
- 62.Luzzo KM, Wang Q, Purcell SH, Chi M, Jimenez PT, Grindler N, et al. High fat diet induced developmental defects in the mouse: oocyte meiotic aneuploidy and fetal growth retardation/brain defects. PLoS One. 2012;7:e49217. doi: 10.1371/journal.pone.0049217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ou XH, Li S, Wang ZB, Li M, Quan S, Xing F, et al. Maternal insulin resistance causes oxidative stress and mitochondrial dysfunction in mouse oocytes. Hum Reprod. 2012;27:2130–45. doi: 10.1093/humrep/des137. [DOI] [PubMed] [Google Scholar]
- 64.Moley KH, Chi MM, Mueckler MM. Maternal hyperglycemia alters glucose transport and utilization in mouse preimplantation embryos. Am J Physiol. 1998;275:E38–47. doi: 10.1152/ajpendo.1998.275.1.E38. [DOI] [PubMed] [Google Scholar]
- 65.Bellver J, Pellicer A, García-Velasco JA, Ballesteros A, Remohí J, Meseguer M. Obesity reduces uterine receptivity: clinical experience from 9,587 first cycles of ovum donation with normal weight donors. Fertil Steril. 2013;100:1050–8. doi: 10.1016/j.fertnstert.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 66.Cardozo E, Pavone ME, Hirshfeld-Cytron JE. Metabolic syndrome and oocyte quality. Trends Endocrinol Metab. 2011;22:103–9. doi: 10.1016/j.tem.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 67.Kaneda N, Nagata C, Kabuto M, Shimizu H. Fat and fiber intakes in relation to serum estrogen concentration in premenopausal Japanese women. Nutr Cancer. 1997;27:279–83. doi: 10.1080/01635589709514538. [DOI] [PubMed] [Google Scholar]
- 68.Wang N, Luo LL, Xu JJ, Xu MY, Zhang XM, Zhou XL, et al. Obesity accelerates ovarian follicle development and follicle loss in rats. Metabolism. 2014;63:94–103. doi: 10.1016/j.metabol.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 69.Skaznik-Wikiel ME, Swindle DC, Allshouse AA, Polotsky AJ, McManaman JL. High-Fat Diet Causes Subfertility and Compromised Ovarian Function Independent of Obesity in Mice. Biol Reprod. 2016;94:108. doi: 10.1095/biolreprod.115.137414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC. Diet and lifestyle in the prevention of ovulatory disorder infertility. Obstet Gynecol. 2007;110:1050–8. doi: 10.1097/01.AOG.0000287293.25465.e1. [DOI] [PubMed] [Google Scholar]
- 71.Tian X, Diaz FJ. Acute dietary zinc deficiency before conception compromises oocyte epigenetic programming and disrupts embryonic development. Dev Biol. 2013;376:51–61. doi: 10.1016/j.ydbio.2013.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zeinab H, Zohreh S, Samadaee Gelehkolaee K. Lifestyle and Outcomes of Assisted Reproductive Techniques: A Narrative Review. Glob J Health Sci. 2015;7:11–22. doi: 10.5539/gjhs.v7n5p11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jahangirifar M, Taebi M, Nasr-Esfahani MH, Askari GH. Dietary Patterns and The Outcomes of Assisted Reproductive Techniques in Women with Primary Infertility: A Prospective Cohort Study. Int J Fertil Steril. 2019;12:316–23. doi: 10.22074/ijfs.2019.5373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Toledo E, Lopez-del Burgo C, Ruiz-Zambrana A, Donazar M, Navarro-Blasco I, Martínez-González MA, et al. Dietary patterns and difficulty conceiving: a nested case-control study. Fertil Steril. 2011;96:1149–53. doi: 10.1016/j.fertnstert.2011.08.034. [DOI] [PubMed] [Google Scholar]
- 75.Millen BE, Abrams S, Adams-Campbell L, Anderson CA, Brenna JT, Campbell WW, et al. The 2015 Dietary Guidelines Advisory Committee Scientific Report: Development and Major Conclusions. Adv Nutr. 2016;7:438–44. doi: 10.3945/an.116.012120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ricci E, Bravi F, Noli S, Somigliana E, Cipriani S, Castiglioni M, et al. Mediterranean diet and outcomes of assisted reproduction: an Italian cohort study. Am J Obstet Gynecol. 2019;221:627.e1–14. doi: 10.1016/j.ajog.2019.07.011. [DOI] [PubMed] [Google Scholar]
- 77.Sanderman EA, Willis SK, Wise LA. Female dietary patterns and outcomes of in vitro fertilization (IVF): a systematic literature review. Nutr J. 2022;21:5. doi: 10.1186/s12937-021-00757-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gaskins AJ, Nassan FL, Chiu YH, Arvizu M, Williams PL, Keller MG, et al. Dietary patterns and outcomes of assisted reproduction. Am J Obstet Gynecol. 2019;220:567.e1–18. doi: 10.1016/j.ajog.2019.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sugawa M, Okubo H, Sasaki S, Nakagawa Y, Kobayashi T, Kato K. Lack of a meaningful association between dietary patterns and in vitro fertilization outcome among Japanese women. Reprod Med Biol. 2018;17:466–73. doi: 10.1002/rmb2.12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Graier WF, Malli R, Kostner GM. Mitochondrial protein phosphorylation: instigator or target of lipotoxicity? Trends Endocrinol Metab. 2009;20:186–93. doi: 10.1016/j.tem.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nehra D, Le HD, Fallon EM, Carlson SJ, Woods D, White YA, et al. Prolonging the female reproductive lifespan and improving egg quality with dietary omega-3 fatty acids. Aging Cell. 2012;11:1046–54. doi: 10.1111/acel.12006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Thoma ME, Klebanoff MA, Rovner AJ, Nansel TR, Neggers Y, Andrews WW, et al. Bacterial vaginosis is associated with variation in dietary indices. J Nutr. 2011;141:1698–704. doi: 10.3945/jn.111.140541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mtango NR, Potireddy S, Latham KE. Oocyte quality and maternal control of development. Int Rev Cell Mol Biol. 2008;268:223–90. doi: 10.1016/S1937-6448(08)00807-1. [DOI] [PubMed] [Google Scholar]
- 84.Sun H, Lin Y, Lin D, Zou C, Zou X, Fu L, et al. Mediterranean diet improves embryo yield in IVF: a prospective cohort study. Reprod Biol Endocrinol. 2019;17:73. doi: 10.1186/s12958-019-0520-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Karayiannis D, Kontogianni MD, Mendorou C, Mastrominas M, Yiannakouris N. Adherence to the Mediterranean diet and IVF success rate among non-obese women attempting fertility. Hum Reprod. 2018;33:494–502. doi: 10.1093/humrep/dey003. [DOI] [PubMed] [Google Scholar]
- 86.Miyazawa T, Hiratsuka Y, Toda M, Hatakeyama N, Ozawa H, Abe C, et al. Artificial intelligence in food science and nutrition: a narrative review. Nutr Rev. 2022;80:2288–300. doi: 10.1093/nutrit/nuac033. [DOI] [PubMed] [Google Scholar]
- 87.Huhtinen K, Desai R, Ståhle M, Salminen A, Handelsman DJ, Perheentupa A, et al. Endometrial and endometriotic concentrations of estrone and estradiol are determined by local metabolism rather than circulating levels. J Clin Endocrinol Metab. 2012;97:4228–35. doi: 10.1210/jc.2012-1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Pettoello-Mantovani M, Mestrovic J, Namazova-Baranova Md PhD L, Giardino I, Somekh E, Vural M. Ensuring Safe Food for Infants: The Importance of an Integrated Approach to Monitor and Reduce the Risks of Biological, Chemical, and Physical Hazards. J Pediatr. 2021;229:315–6. doi: 10.1016/j.jpeds.2020.10.074. [DOI] [PubMed] [Google Scholar]
- 89.Messerlian C, Williams PL, Ford JB, Chavarro JE, Mínguez-Alarcón L, Dadd R, et al. The Environment and Reproductive Health (EARTH) Study: A Prospective Preconception Cohort. Hum Reprod Open. 2018;2018:hoy001. doi: 10.1093/hropen/hoy001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wang R, Song B, Wu J, Zhang Y, Chen A, Shao L. Potential adverse effects of nanoparticles on the reproductive system. Int J Nanomedicine. 2018;13:8487–506. doi: 10.2147/IJN.S170723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jensen TK, Priskorn L, Holmboe SA, Nassan FL, Andersson AM, Dalgård C, et al. Associations of Fish Oil Supplement Use with Testicular Function in Young Men. JAMA Netw Open. 2020;3:e1919462. doi: 10.1001/jamanetworkopen.2019.19462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Salas-Huetos A, Bulló M, Salas-Salvadó J. Dietary patterns, foods and nutrients in male fertility parameters and fecundability: a systematic review of observational studies. Hum Reprod Update. 2017;23:371–89. doi: 10.1093/humupd/dmx006. [DOI] [PubMed] [Google Scholar]


