Abstract
Objective:
Bladder injury is one of the complications of cesarean section (CS). It is reported that the overall incidence of bladder injury is 0.22-0.44% of CS. It is, however, unclear what factors influence this rate. The aim of this study was to determine if there is a difference in bladder injury rate between scheduled and emergency CS, as well as in primary and repeat CS at a large metropolitan hospital that serves a population at high risk for obstetric complications. In addition, the use of urology consultation following bladder injury and whether demographic factors and labor characteristics affect the rate of bladder injury were investigated.
Material and Methods:
A total of 8,488 records were reviewed (4,292 primary CS and 4,196 repeat CS) from January 1, 2013 to December 31, 2020. The incidence of bladder injury was calculated and the rate of intraoperative urology/urogynecology consultation was recorded. Then the association between bladder injury and intraoperative urology/urogynecology consultation and between bladder injury and maternal age, body mass index (BMI), and gestational age were compared.
Results:
There was a significant increase in risk of bladder injury in repeat CS versus primary CS (p=0.01). There was also a significant increase in risk of bladder injury in emergency CS versus scheduled CS (p=0.04). Intraoperative urogynecology/urology consultations were significantly higher in the bladder injury versus no bladder injury groups (p<0.0001). Both emergency CS and repeat CS are predictors of bladder injury with odd ratios of 5.7 and 7.4, respectively.
Conclusion:
These results add to the existing evidence that bladder injury is a rare complication in CS that may occur more often in women undergoing repeat or emergency CS than primary or scheduled CS. Given that the risk increases with repeat or emergency CS, patients should be made aware of such risks and surgeons should make careful intraoperative considerations with close postoperative follow-ups.
Keywords: Bladder, cesarean, urogynecology
Introduction
According to the National Center for Health Statistics, the cesarean section (CS) delivery rate in the United States was 31.9% for 2020, representing a steady increase since 1996 with a brief decline in 2008 and 2009 (1). As the CS rate has increased, maternal mortality and morbidity have also risen steadily over the last three decades (2). In 2004 it was reported that the overall complication rate from CS was 21.4% (3). In recent literature these complications are widely discussed. Uterine rupture, abnormal placentation, ectopic pregnancy, and preterm birth are most common (4). In a meta-analysis, emergency CS was associated with significantly more maternal and fetal complications and mortality than elective CS (5).
During a CS, the most common approach is to make a low transverse incision across the lower uterine segment. Anterior to this location is the bladder. Creating a bladder flap depends on the physician’s preference and the time available for the procedure. Most physicians avoid creating a bladder flap since there is no evidence that supports the bladder flap as a method to reduce bladder injury (6). On the contrary, there is evidence showing that bladder flap formation is associated with short-term urinary complaints, such as urinary retention and dysuria (7,8,9). There is, however, an increased operative time in CS deliveries when a bladder flap was created versus those when bladder flap was omitted (9,10).
The overall bladder injury incidence is reported to be 0.22-0.44%. Furthermore, these rates are 0.11-0.42% for primary CS and 0.27-0.81% for repeat CS (11,12,13,14). Repeat CS is the primary risk factor for bladder injury (12). The reason is attributed to the formation of adhesions postoperatively and it is shown that the incidence of adhesive disease following a primary CS ranges from 46-65% (15). In patients with repeat CS, the bladder may be adherent to the lower uterine segment where the hysterotomy is commonly made. Bladder injuries can occur at the time of bladder flap creation, hysterotomy and even closure of the hysterotomy because of the proximity of the bladder to the inferior aspect of the hysterotomy. Unfortunately, in emergency CS, diligent and careful dissection is not the most important priority. Failed vaginal delivery continues to be the major cause of emergency CS, primarily due to fetal distress and abnormal fetal position (16). Emergency CS was reported to be accompanied by significantly more maternal and fetal complications and mortality than elective CS in a meta-analysis (5). Although there are case reports of bladder injury during emergency CS, there is no clear data showing whether there is an association or not.
It has been reported that repeat CS is a risk factor for bladder injury (13). In this study, the aim was to determine if there is a difference in bladder injury rates between scheduled and emergency CS, and between primary and repeat CS at a large metropolitan hospital that serves a population at high risk for obstetric complications. In addition, the use of urology consultation following bladder injury and whether demographic factors and labor characteristics affect the rate of bladder injury were investigated. Recommendations will be made, based on the findings of this study.
In a major study, the overall incidence of bladder injury was 0.28%, with an incidence of 0.56% during repeat CS and 0.14% during primary CS (13). To show such an effect, at least 3,103 cases per group needed to be reviewed. Despite fast-paced developments in this medical field, there is no large and recent study investigating bladder injury in repeat and emergency CS in the last two decades. In the present study, 8,488 records were reviewed, consisting of 4,292 primary CS and 4,196 repeat CS from January 1, 2013 to December 31, 2020. This study is the first to investigate the association between bladder injury and intraoperative urology/urogynecology consultation and between bladder injury and maternal age, body mass index (BMI), and gestational age.
Material and Methods
This was a retrospective cohort study that received Ascension St. John Hospital Institutional Review Board exemption (approval number: 1790154) and exemption for informed consent. A chart review was performed of women who underwent either a scheduled or emergency CS delivery at a large urban metropolitan hospital. The inclusion criterion was women (18 years and older) who underwent a scheduled or emergency CS delivery from January 1, 2013, to December 31, 2020. The billing data was queried for cases using the ICD-9 codes of 740, 741, 742, and 744 as well as ICD-10 codes of 10D00Z1, 10D00Z2 and 10D00Z0. Once the cases were identified, the operative reports were reviewed for surgical details, as well as the anesthesia and nursing reports, to identify the pertinent variables. The following variables were collected from these charts: patient demographics, BMI, gestational age at delivery, primary or repeat CS, reason for CS, bladder injury noted at the time of surgery, if the patient had been in labor, and the type of anesthesia. The primary outcome was the incidence of bladder injury. The secondary outcomes were intraoperative urology/urogynecology consultation, demographic characteristics, and the nature of the CS (repeat or emergency).
Statistical analysis
Statistical analysis was done using SPSS version 25.0 (IBM Inc., Armonk, NY, USA) and a p-value of less than 0.05 was considered to indicate statistical significance.
Comparisons were made between the group that had no bladder injury and the group that had bladder injury. Continuous variables were analyzed using the mean with standard deviation or median with range or interquartile range. Categorical variables were analyzed using frequency distributions and chi-squared test. Univariable analysis of factors associated with bladder injury were assessed using Student’s t-test and the chi-squared analysis. Non-parametric tests were used for data that are non-normally distributed. A Mann-Whitney U test was used for analysis of the cervical dilation due to the skew and variability. Multivariable analysis of bladder injury was performed using logistic regression.
Results
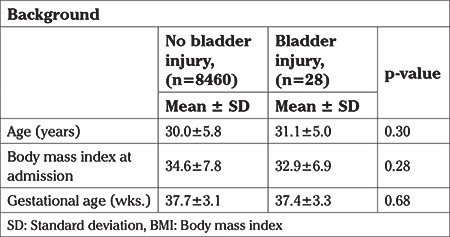
A total of 8,488 CS reports were reviewed, dating from January 1, 2013, to December 31, 2020. There were 3,838 emergency CS (45%) and 4,650 (55%) scheduled CS. There were also 4,292 primary CS (51%) and 4,196 repeat CS (49%). There was a total of 28 cases of bladder injury identified including 18 (64%) during emergency CS versus ten (36%) during scheduled CS (p=0.04). Furthermore, seven (25%) of bladder injury cases were primary CS versus 21 (75%) in repeat CS (p=0.01). Intraoperative urology/urogynecology consultation was made in 24/28 (86%) of bladder injury cases versus 0% in the “No Bladder Injury” group (p<0.0001) (Table 1). The mean gestational age in weeks in the No Bladder Injury group was 37.7±3.1 versus 37.4±3.3 in the “Bladder Injury” group (p=0.68) (Table 2). There was a significant difference in the proportion of women in “No Bladder Injury” group (32%) being in labor versus 57% in “Bladder Injury” group (p=0.004).
Table 1. Cesarean section delivery characteristics in the study sample.
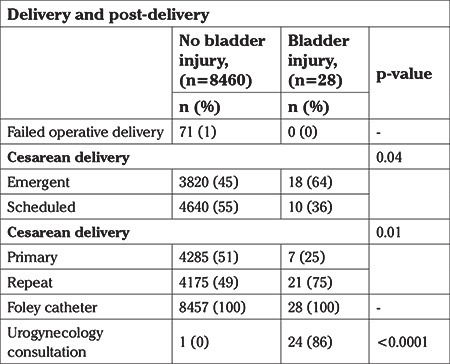
Table 2. Patients’ background characteristics.
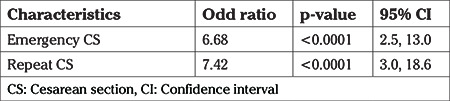
A significant increase was found in the risk of bladder injury in repeat CS versus primary CS (p=0.01). There was also a significant increase in the risk of bladder injury in emergency CS versus scheduled CS (p=0.04). Intraoperative urogynecology/urology consultations were significantly more common in the bladder injury group versus no bladder injury group (p<0.0001). Both emergency CS and repeat CS were predictors of bladder injury with odd ratios of 5.7 and 7.4, respectively (Table 3).
Table 3. Logistic regression analysis for the risk of bladder injury.
Discussion
This study shows an increased risk of bladder injury in the setting of emergency CS versus scheduled CS with a relative risk (RR) of 100%. In addition, a higher risk of bladder injury was associated with repeat CS versus scheduled CS (RR: 68%). In cases where bladder injury was suspected, urogynecology/urology was most likely to be consulted intraoperatively. There was no association between having a bladder injury and maternal age, BMI, and gestational age at the time of delivery.
CS increases the risk of postoperative adhesions at the surgical site (17). Since the bladder is in close proximity to the anterior uterus, it can be affected by nearby anatomical changes. Adhesions were present in 37% of patients with prior CS while these were only found in 10% of patients with no prior CS in a study that evaluated over 15 thousand patients (17). It was also reported that adhesions were found in 32% of women who had one CS, in 42% after two CSs, and 59% after three or more CSs (17). Tulandi et al. (18) studied the site and extent of adhesion post CS. They reported that dense adhesions between the uterus and the bladder were found in 29.8% of one-repeat CS patients group versus 46.3% in two-repeat CS patients (18). These authors also reported dense adhesions between the uterus and the abdomen in 25.6% of one-repeat CS versus 48.2% in two-repeat CS (18). In a study that presented transvaginal ultrasound findings following CS, there was obliteration of the anterior cul-de-sac in multiple cases and fibrosis between lower uterine segment and cervix with the bladder in others (19). These findings correlate to limited mobility of the bladder and therefore increase the risk of bladder injury.
There is no consensus on the most favorable method for opening or closure of CS. However, some studies evaluated the impact of different uterine closure techniques on lower uterine segment anatomy and formation of adhesions. Double-layer closure was associated with better but thicker uterine scar healing than single layer closure (20,21). In addition, increased uterine scar thickness was found to increase adhesions and compression effect on the bladder, seen as a bulging mass on cystoscopy and therefore, increase risk of bladder injury (22).
In addition to the formation of adhesions, changes to the natural position of the uterus can occur, thus increasing the risk of bladder injury in subsequent surgery. There is a statistically significant increase in antepartum and postpartum flexion angle of the uterus between cesarean and vaginal delivery (23).
Study Limitations
There is no agreement in the literature on why bladder injury risk increases with emergency CS. It is likely that the emergency itself and the anatomical changes mentioned above increase the risk of errors and therefore, iatrogenic injuries in many different ways.
Conclusion
These results build on the existing evidence that bladder injury is a rare complication of CS that more often occurs in women undergoing repeat or emergency CS compared to primary or scheduled CS. Our study has several strengths, including the large sample volume and diverse demography. Also, the study data came from an urban institution that serves a diverse population making it applicable to a wider profile of cases. However, the generalizability of our study is limited by its retrospective nature and the single institution data source could be non-inclusive to other centers that practice different techniques. Additional analysis is needed to understand the association between different CS techniques and bladder injury and the additive effect of repeat and emergency CS on the risk of bladder injury.
Due to the rapid increase in the prevalence of CS deliveries, the risk of bladder injury during primary versus repeat CS and scheduled versus emergency CS was assessed. Given that the risk increases with repeat and emergency CS, patients should be made aware of such risk and surgeons should make careful intraoperative considerations with close postoperative follow-ups.
Footnotes
Ethics Committee Approval: This was a retrospective cohort study that received Ascension St. John Hospital Institutional Review Board exemption (approval number: 1790154).
Informed Consent: This was a retrospective cohort study that received exemption for informed consent.
Peer-review: Internally peer-reviewed.
Author Contributions: Surgical and Medical Practices: M.A., S.F., A.S.K.; Concept: M.A., S.F., A.S.K.; Design: M.A., S.F., A.S.K.; Data Collection or Processing: A.S.K.; Analysis or Interpretation: K.H., A.S.K.; Literature Search: A.S.K.; Writing: A.S.K.
Conflict of Interest: No conflict of interest is declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.
References
- 1.Osterman M, Hamilton B, Martin JA, Driscoll AK, Valenzuela CP. Births: Final Data for 2020. Natl Vital Stat Rep. 2021;70:1–50. [PubMed] [Google Scholar]
- 2.Antoine C, Young BK. Cesarean section one hundred years 1920-2020: the Good, the Bad and the Ugly. J Perinat Med. 2020;49:5–16. doi: 10.1515/jpm-2020-0305. [DOI] [PubMed] [Google Scholar]
- 3.Häger RM, Daltveit AK, Hofoss D, Nilsen ST, Kolaas T, Øian P, et al. Complications of cesarean deliveries: rates and risk factors. Am J Obstet Gynecol. 2004;190:428–34. doi: 10.1016/j.ajog.2003.08.037. [DOI] [PubMed] [Google Scholar]
- 4.Sandall J, Tribe RM, Avery L, Mola G, Visser GH, Homer CS, et al. Short-term and long-term effects of caesarean section on the health of women and children. Lancet. 2018;392:1349–57. doi: 10.1016/S0140-6736(18)31930-5. [DOI] [PubMed] [Google Scholar]
- 5.Yang XJ, Sun SS. Comparison of maternal and fetal complications in elective and emergency cesarean section: a systematic review and meta-analysis. Arch Gynecol Obstet. 2017;296:503–12. doi: 10.1007/s00404-017-4445-2. [DOI] [PubMed] [Google Scholar]
- 6.Tarney CM. Bladder Injury During Cesarean Delivery. Curr Womens Health Rev. 2013;9:70–6. doi: 10.2174/157340480902140102151729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gül DK, Kırca AS. Effects of creation of bladder flap during cesarean section on long-term residual urine volume and postoperative urinary retention. J Surg Med. 2020;4:1190–4. [Google Scholar]
- 8.Aslan Cetin B, Aydogan Mathyk B, Barut S, Zindar Y, Seckin KD, Kadirogullari P. Omission of a Bladder Flap during Cesarean Birth in Primiparous Women. Gynecol Obstet Invest. 2018;83:564–8. doi: 10.1159/000481283. [DOI] [PubMed] [Google Scholar]
- 9.Elsersy MA. Usefulness of bladder dissection in cesarean section: a randomized controlled trial. Int J Reprod Contracept Obstet Gynecol. 2016;5:4317–21. [Google Scholar]
- 10.Youssef YA, Farghaly TA, Elsenosy E, Youssef AA, Abbas AM. The Effect of Omission of the Bladder Flap Formation at Lower Segment Cesarean Delivery: A Randomized Controlled Trial. Open Journal of Obstetrics and Gynecology. 2019;9:1083–91. [Google Scholar]
- 11.Morris S, Turocy J, Dabney L, Hardart A. Bladder Injury During Cesarean Delivery. Obstet Gynecol. 2016;127:33. [Google Scholar]
- 12.Rahman MS, Gasem T, Al Suleiman SA, Al Jama FE, Burshaid S, Rahman J. Bladder injuries during cesarean section in a University Hospital: a 25-year review. Arch Gynecol Obstet. 2009;279:349–52. doi: 10.1007/s00404-008-0733-1. [DOI] [PubMed] [Google Scholar]
- 13.Phipps MG, Watabe B, Clemons JL, Weitzen S, Myers DL. Risk factors for bladder injury during cesarean delivery. Obstet Gynecol. 2005;105:156–60. doi: 10.1097/01.AOG.0000149150.93552.78. [DOI] [PubMed] [Google Scholar]
- 14.Cahill AG, Stout MJ, Stamilio DM, Odibo AO, Peipert JF, Macones GA. Risk factors for bladder injury in patients with a prior hysterotomy. Obstet Gynecol. 2008;112:116–20. doi: 10.1097/AOG.0b013e31817946f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.El-Mowafi DM, Diamond MP. Are pelvic adhesions preventable? Surg Technol Int. 2003;11:222–35. [PubMed] [Google Scholar]
- 16.Guan P, Tang F, Sun G, Ren W. Prediction of emergency cesarean section by measurable maternal and fetal characteristics. J Investig Med. 2020;68:799–806. doi: 10.1136/jim-2019-001175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hesselman S, Högberg U, Råssjö EB, Schytt E, Löfgren M, Jonsson M. Abdominal adhesions in gynaecologic surgery after caesarean section: a longitudinal population-based register study. BJOG. 2018;125:597–603. doi: 10.1111/1471-0528.14708. [DOI] [PubMed] [Google Scholar]
- 18.Tulandi T, Al-Sannan B, Akbar G, Miner L, Ziegler C, Sikirica V. Clinical relevance of intra-abdominal adhesions in cesarean delivery. Gynecol Surg. 2011;8:399–403. [Google Scholar]
- 19.Walid MS, Heaton RL. Uterine peaking--sonographic sign of vesicouterine adhesion. Ger Med Sci. 2011;9:Doc24. doi: 10.3205/000147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roberge S, Demers S, Girard M, Vikhareva O, Markey S, Chaillet N, et al. Impact of uterine closure on residual myometrial thickness after cesarean: a randomized controlled trial. Am J Obstet Gynecol. 2016;214:507.e1–6. doi: 10.1016/j.ajog.2015.10.916. [DOI] [PubMed] [Google Scholar]
- 21.Yasmin S, Sadaf J, Fatima N. Impact of methods for uterine incision closure on repeat caesarean section scar of lower uterine segment. J Coll Physicians Surg Pak. 2011;21:522–6. [PubMed] [Google Scholar]
- 22.Rosa F, Perugin G, Schettini D, Romano N, Romeo S, Podestà R, et al. Imaging findings of cesarean delivery complications: cesarean scar disease and much more. Insights Imaging. 2019;10:98. doi: 10.1186/s13244-019-0780-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaelin Agten A, Honart A, Monteagudo A, McClelland S, Basher B, Timor-Tritsch IE. Cesarean Delivery Changes the Natural Position of the Uterus on Transvaginal Ultrasonography. J Ultrasound Med. 2018;37:1179–83. doi: 10.1002/jum.14461. [DOI] [PubMed] [Google Scholar]


