Abstract
Prostate-specific membrane antigen (PSMA) PET/CT is a highly reliable nuclear tracer for diagnostic imaging of prostate cancer. However, PSMA is also expressed by some nonprostatic tissues such as benign tumors, inflammatory processes, and malignant neoplasms. This case presents a patient with prostate cancer and follicular lymphoma undergoing PSMA PET/CT. Remarkably, both tumor entities were clearly detected in the scan. Yet, the 2 malignancies demonstrated rather different ranges in terms of SUVmax uptake values and therefore still enabled precise and accurate discrimination of prostate cancer and follicular lymphoma.
Keywords: PSMA PET/CT, prostate cancer, follicular lymphoma
FIGURE 1.
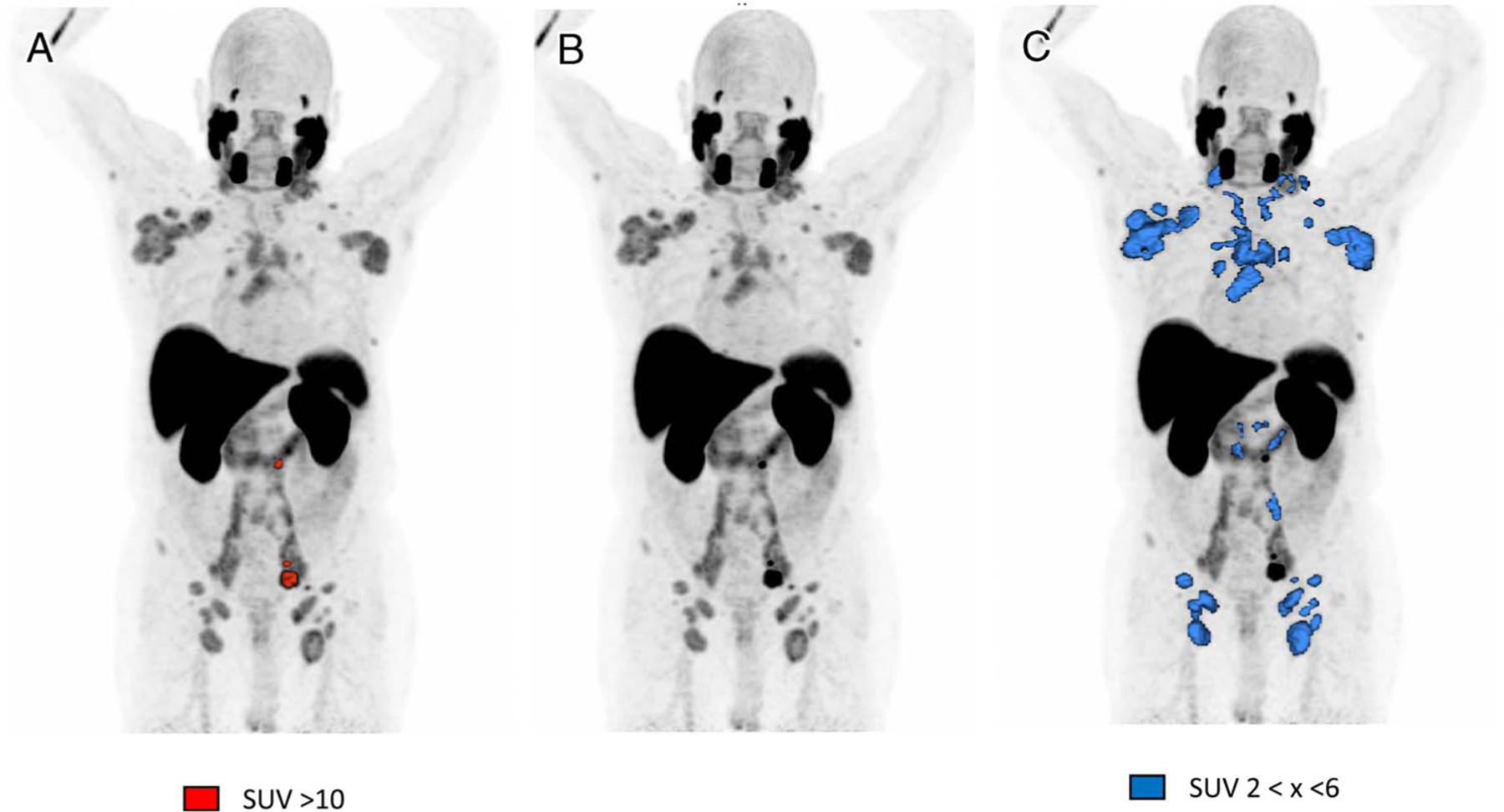
Prostate-specific membrane antigen (PSMA) is overexpressed by prostate epithelial cells.1,2 However, moderate or even high PSMA expression can also be observed in a variety of conditions including inflammatory processes, benign tumors, and malignant neoplasms.3,4 This image depicts a case of a 79-year-old man with a previously treated histologically confirmed prostate cancer (10/2015) referred for a 18F-PSMA-1007 PET/CT due to a rising PSA value (3.96 ng/mL) after definitive radiotherapy in 2016 (GSc 7b, pT1c, iPSA 6.0 ng/mL). In November 2018, follicular non-Hodgkin lymphoma (IIa Ann Arbor) was additionally diagnosed in a CT scan and histologically confirmed by lymph node excisional biopsy. A follow-up 18F-PSMA-1007 PET/CT scan (07/2020) unveiled a relapse of the prostate carcinoma with 2 lymph node metastases located in the left paravesical space (SUVmax, 19.2) and left para-aortic space (SUVmax, 15.3), as well as 1 bone metastasis in the left sacrum (SUVmax, 15.4), all highlighted in A. Remarkably, the scan also clearly demonstrated moderate PSMA uptake in the follicular lymphoma, presented as large symmetric lymph nodes with an apparent worsening to Ann Arbor III. The SUVmax of the delineated lesions ranged from 2 to 6 (C). Thus, in this special case, both prostate cancer and follicular lymphoma emerged as PSMA positive. In terms of SUVmax, the follicular lymphoma showed rather moderate uptake values when compared with the prostate cancer lesions. Therefore, a precise identification of each disease can, in accordance with the SUV value, be performed based on the Syngo via MM Oncology VB50 (A–C). This case demonstrates that PSMA-positive lesions may not be due to prostate cancer alone, and thus different diagnoses should be considered in atypical cases as well.3 Nevertheless, apart from occasional challenges with other neoplasms, PSMA PET/CT remains a highly reliable and precise tracer for diagnosing and monitoring of prostate cancer.5–8
Sources of funding:
Patent application for PSMA-1007 for F.L.G., U.H., and J.C. and for PSMA-617 for C.Kr. and U.H. F.L.G. is an advisor at SOFIE Biosciences, Telix, and ABX pharmaceutical.
Footnotes
Conflicts of interest:
The remaining authors declare no conflicts of interest.
Ethics approval and consent to participate: The radiopharmaceutical was used on an individual patient basis according to German Pharmaceuticals Act §13 (2b). The patient gave written informed consent to receive the novel diagnostics and permitted anonymized publication of related medical data. The ethical committee of Heidelberg University approved this retrospective evaluation to be in accordance with the Helsinki declaration. For case reports from clinical practice, no trial registration is required.
REFERENCES
- 1.Giesel FL, Hadaschik B, Cardinale J, et al. F-18 labelled PSMA-1007: biodistribution, radiation dosimetry and histopathological validation of tumor lesions in prostate cancer patients. Eur J Nucl Med Mol Imaging 2017;44: 678–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Will L, Sonni I, Kopka K, et al. Radiolabeled prostate-specific membrane antigen small-molecule inhibitors. QJ Nucl Med Mol Imaging 2017;61:168–180. [DOI] [PubMed] [Google Scholar]
- 3.Sheikhbahaei S, Afshar-Oromieh A, Eiber M, et al. Pearls and pitfalls in clinical interpretation of prostate-specific membrane antigen (PSMA)-targeted PET imaging. Eur J Nucl Med Mol Imaging 2017;44:2117–2136. [DOI] [PubMed] [Google Scholar]
- 4.Silver DA, Pellicer I, Fair WR, et al. Prostate-specific membrane antigen expression in normal and malignant human tissues. Clin Cancer Res 1997;3:81–85. [PubMed] [Google Scholar]
- 5.Perera M, Papa N, Roberts M, et al. Gallium-68 prostate-specific membrane antigen positron emission tomography in advanced prostate cancer-updated diagnostic utility, sensitivity, specificity, and distribution of prostate-specific membrane antigen-avid lesions: a systematic review and meta-analysis. Eur Urol 2020;77:403–417. [DOI] [PubMed] [Google Scholar]
- 6.Bagguley D, Ong S, Buteau JP, et al. Role of PSMA PET/CT imaging in the diagnosis, staging and restaging of prostate cancer. Future Oncol 2021;17: 2225–2241. [DOI] [PubMed] [Google Scholar]
- 7.Malaspina S, Anttinen M, Taimen P, et al. Prospective comparison of (18)F-PSMA-1007 PET/CT, whole-body MRI and CT in primary nodal staging of unfavourable intermediate- and high-risk prostate cancer. Eur J Nucl Med Mol Imaging 2021. [Online ahead of print]. doi: 10.1007/s00259-021-05296-1. [DOI] [PubMed]
- 8.Kuten J, Fahoum I, Savin Z, et al. Head-to-head comparison of 68Ga-PSMA-11 with 18F-PSMA-1007 PET/CT in staging prostate cancer using histopathology and immunohistochemical analysis as a reference standard. J Nucl Med 2020; 61:527–532. [DOI] [PubMed] [Google Scholar]


