Abstract
Introduction
The basic method of treating food hypersensitivity is the elimination diet, which is difficult for the patient in many ways.
Aim
To identify the main problems faced by patients with symptoms of food intolerance.
Material and methods
The survey was conducted from February 2021 to December 2021. The survey was posted in Polish thematic groups on Facebook, dedicated to people with food intolerances. The survey contained 34 questions about food intolerances and the use of elimination diets. Questions about the cost of the diet and difficulties in applying the elimination diet were included.
Results
There was no statistically significant relationship between the type of food intolerance and the body mass index of patients. It was found that people with lactose intolerance had a lower increase in food expenditure since the introduction of the diet than those without lactose intolerance. Almost half of the respondents did not find a difference in expenses. 21% of respondents noticed an increase of PLN 50–100/month, 19% – PLN 10–50/month, and only 6% above PLN 200/month. Circumstances where following an elimination diet is a particular challenge included intense private and professional lifestyle, prolonged stay away from home, and lack of time to prepare meals at home.
Conclusions
The difficulties in maintaining an elimination diet are dependent on the patient’s work and lifestyle. The cost of equivalents of intolerant products is also an important factor to consider when analysing the source of problems in maintaining the diet.
Keywords: food intolerance, lactose intolerance, celiac disease, gluten, hypersensitivity
Introduction
Food hypersensitivity is a significant problem in developed countries. Food allergy is a hypersensitivity of immunological etiopathogenesis, and non-immunological mechanisms play a key role in food intolerance. The relatively late diagnosis of the cause of the patient’s disturbing symptoms remains a problem.
Still, the basic method of treating food hypersensitivity is the elimination diet, which is in many ways difficult for the patient.
Aim
The aim of the study was to identify the main problems faced by patients with symptoms of food intolerance.
Material and methods
The survey was conducted from February 2021 to December 2021. The survey was posted in Polish thematic groups on Facebook, dedicated to people with food intolerances. The groups in which the survey was made available are: “Food intolerances”, “Candida, parasites, SIBO-treatment diet”, “Histamine intolerance”, and “Lactose intolerance”.
During the study, complete anonymity of personal data was maintained. The questionnaires were filled in by 146 people diagnosed with food intolerance or suspected of having such an intolerance. Four people were disqualified because they did not meet the inclusion criterion of age over 18 years.
The survey contained 34 questions about food intolerances and the use of elimination diets. Questions about the cost of the diet and difficulties in applying the elimination diet were included.
The study was approved by the Bioethics Committee of the Collegium Medicum in Bydgoszcz, number KB 38/2021
Statistical analysis
Statistical analysis of the obtained results was carried out in Microsoft Excel 365 and the R software, version 4.1.3. The analysis of the survey questions was carried out by calculating the number and percentage of occurrences of each answer. Comparison of responses in groups was performed using the χ2 test (with Yates’ correction for 2x2 tables) or Fisher’s exact test where low expected frequencies appeared in the tables. The analysis adopted a significance level of 0.05. Thus, all p-values below 0.05 were interpreted as significant associations.
Results
The study group consisted of 142 people. Sixty-five (46%) people were men and 77 (54%) were women. The youngest person was 18 years old and the oldest person was 66 years old at the time of the study, the mean age was 27.6 ±7.4.
The declared body weight was 43.5–120 kg (mean: 71.5 ±16.1 kg) and height 153–202 cm (mean: 172.5 ±7.8 cm). The body mass index (BMI) in the study population was 16.5–40.1 kg/m2 (mean: 23.9± 4.4). Six people were underweight (BMI < 18.5 kg/m2), 87 people were of normal weight (BMI 18.5–25 kg/m2), 37 people were overweight (BMI 25–29.9 kg/m2) and 12 were obese (BMI > 30 kg/m2).
Ninety-four (66%) of the respondents declared that they do not suffer from any chronic diseases. Among the 48 patients who declared chronic diseases, hypothyroidism and irritable bowel syndrome prevailed.
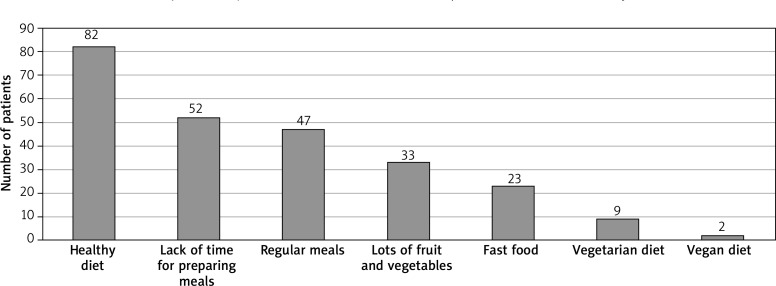
Respondents were asked to describe their current diet.
Eighty-two (57.7%) patients declared that they followed a healthy diet. At the same time, 36.6% of the respondents stated that being too busy was the reason for improper composition of the diet. 33.1% of patients eat regularly, 23.2% eat a lot of fruit and vegetables, and only 16.2% say they eat fast food. Vegetarian and vegan diets were relatively uncommon in the study population (6.3% and 1.4% of respondents, respectively).
A food intolerance was declared in the study by 109 patients, 18 took part in the survey despite the lack of food intolerance, and the remaining respondents were not sure whether they had symptoms of food intolerance. For this purpose, a multiple-choice question was used. The results are shown in Figure 1.
Figure 1.
Diet declared by the respondents
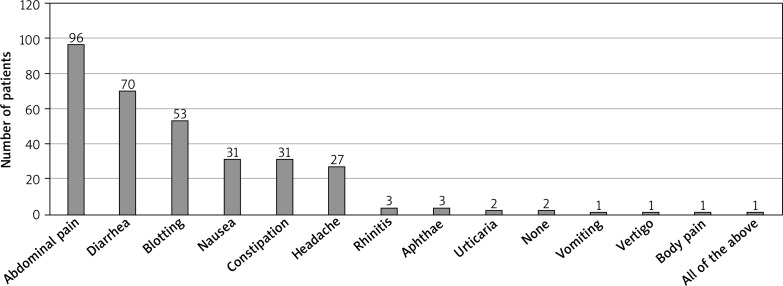
The nature of the symptoms of food intolerance declared by the patients differed significantly, but abdominal pain and diarrhoea were by far the most common. The declared symptoms are shown in Figure 2.
Figure 2.
Clinical signs of food intolerance declared in the survey
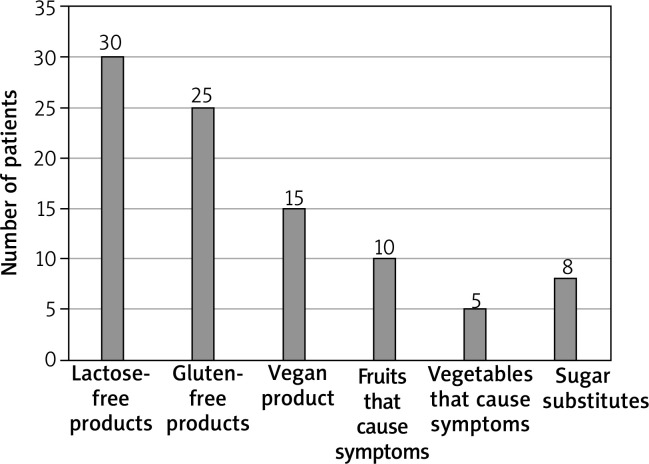
The foods that were responsible for causing intolerance symptoms in the study population were mainly lactose and gluten. The number of patients reporting symptoms after eating certain food groups is shown in Figure 3.
Figure 3.
Food products causing symptoms of intolerance in the study population
The respondents were asked whether they followed an elimination diet. A hundred and nine (76.8%) patients answered affirmatively. What is particularly important, as many as 104 people (95.4% of the group of people using the elimination diet) stated that the elimination diet had a positive impact on their well-being and quality of life, resulting in a reduction or complete disappearance of bothersome symptoms. Other people did not notice any difference in their well-being after introducing the diet.
An important aspect of the use of elimination diets is the introduction of a substitute in place of the eliminated product, which is designed to, on the one hand, ensure a variety of flavours in the diet, and on the other hand, in optimal conditions, prevent nutritional deficiencies. 66 respondents stated that they used substitutes in the elimination diet. 43 people using the elimination diet did not introduce substitutes to the diet.
According to the nature of the diagnosed intolerance, the vast majority of patients used lactose-free and gluten-free substitutes. The type of substitutes used, detailing the number of patients who introduced them to the diet, is presented in Figure 4.
Figure 4.
Substitutes for intolerant food products used by Patients
The respondents were asked whether the food substitutes they used, in their subjective opinion, were expensive. Fifty-seven people said that these products were expensive, and only 23 people said that they did not constitute a significant burden on the household budget.
The respondents were asked how much the expenses in their monthly household budget increased after the introduction of the elimination diet. Almost half of the respondents did not find a difference in expenses. 21% of respondents noticed an increase of PLN 50–100/month, 19% – PLN 10–50/month, and only 6% above PLN 200/month.
Another key aspect of using an elimination diet is its strict adherence to it. The respondents were asked whether there were situations in which they did not follow the diet while on a diet. Forty-five respondents confirmed that they sometimes consumed “forbidden” food. Moreover, another 40 people consumed these products unknowingly despite the fact that they wanted to follow the diet. Only 22% (32 people) of the respondents managed to maintain an elimination diet.
Occurring errors in the use of the diet prompt the respondents to ask the question whether, in their subjective opinion, the use of an elimination diet is difficult. As many as 80 respondents gave an affirmative answer, which is as much as 73.4% of those using the elimination diet.
There are circumstances where following an elimination diet is a particular challenge. They are usually associated with an intense private and professional life, prolonged stay away from home and lack of time to prepare meals on their own. The circumstances declared by the respondents in which errors in the use of the elimination diet most often occurred are presented in Figure 5.
Figure 5.
Circumstances during which respondents experience the most difficulties in maintaining the elimination diet
There was no statistically significant relationship between the type of food intolerance and BMI of patients.
In general, analysing the entire study population, it was found that dietary errors occurred most often in the group of respondents aged over 30 years (Figure 6).
Figure 6.
Dietary errors and the age of respondents
It was found that in people with gluten intolerance, the increase in food expenditure since the introduction of the diet was greater than in people without this intolerance (Table 1). In this group, the consumption of products causing intolerance, despite the use of an elimination diet, occurred less frequently than in people without this intolerance, but there were cases of accidental consumption of food containing a given product. Interestingly, it turned out that going to parties, social gatherings or restaurants did not make it difficult to follow a gluten-free diet.
Table 1.
Statistical analysis of survey data on difficulties in using a gluten-free diet
| Parameter | Gluten intolerance | P-value | ||
|---|---|---|---|---|
| Yes (N = 37) | No (N = 105) | |||
| Current diet** | Lack of time for proper composition of meals | 5 (13.51%) | 30 (28.57%) | 0.108 |
| Vegan diet | 2 (5.41%) | 1 (0.95%) | 0.166 | |
| Vegetarian diet | 2 (5.41%) | 7 (6.67%) | 1 | |
| Lots of vegetables and fruits | 9 (24.32%) | 24 (22.86%) | 1 | |
| Fast food | 2 (5.41%) | 21 (20.00%) | 0.07 | |
| Regular meals | 16 (43.24%) | 51 (48.57%) | 0.714 | |
| Healthy diet | 22 (59.46%) | 49 (46.67%) | 0.251 | |
| Increase in food spending since the introduction of the diet | PLN 10–50 | 1 (2.70%) | 18 (17.14%) | < 0.001* |
| PLN 50–100 | 9 (24.32%) | 20 (19.05%) | ||
| PLN 100–200 | 10 (27.03%) | 6 (5.71%) | ||
| More than PLN 200 | 5 (13.51%) | 3 (2.86%) | ||
| Not applicable | 12 (32.43%) | 58 (55.24%) | ||
| Consumption of products that cause intolerance despite the use of an elimination diet | Yes | 6 (16.22%) | 39 (37.14%) | 0.003* |
| Unintentionally | 18 (48.65%) | 22 (20.95%) | ||
| No | 10 (27.03%) | 22 (20.95%) | ||
| Not applicable | 3 (8.11%) | 22 (20.95%) | ||
| Circumstances hindering the maintenance of the diet** | Events | 6 (16.22%) | 42 (40.00%) | 0.015* |
| Numerous responsibilities – lack of time | 2 (5.41%) | 19 (18.10%) | 0.109 | |
| Business trips | 8 (21.62%) | 20 (19.05%) | 0.922 | |
| Accidental ingestion of food containing the product | 23 (62.16%) | 43 (40.95%) | 0.042* | |
| Social gatherings | 6 (16.22%) | 41 (39.05%) | 0.02* | |
| Stressful situations in life | 5 (13.51%) | 18 (17.14%) | 0.798 | |
| Vacation | 9 (24.32%) | 36 (34.29%) | 0.36 | |
| Eating in a restaurant | 7 (18.92%) | 41 (39.05%) | 0.043* | |
| Do you find it difficult to follow an elimination diet? | Yes | 25 (67.57%) | 55 (52.38%) | 0.459 |
| No | 9 (24.32%) | 33 (31.43%) | ||
| I have no opinion | 3 (8.11%) | 12 (11.43%) | ||
| No data available | 0 (0.00%) | 5 (4.76%) | ||
p – for quantitative variables – the Mann-Whitney test, for qualitative variables – the c2 test or the Fisher’s exact test.
Statistically significant difference (p < 0.05).
Multiple choice question – interest does not add up to 100.
It was found that people with lactose intolerance had a lower increase in food expenditure since the introduction of the diet than those without lactose intolerance (Table 2). What is more, the consumption of products causing intolerance despite the use of an elimination diet occurred more often than in people without this intolerance. In this type of diet, parties and social gatherings were a factor that made it difficult to maintain the diet.
Table 2.
Statistical analysis of survey data on difficulties in using a lactose-free diet
| Parameter | Lactose intolerance | P-value | ||
|---|---|---|---|---|
| Yes (N = 67) | No (N = 75) | |||
| Current diet** | Lack of time for proper composition of meals | 17 (25.37%) | 18 (24.00%) | 1 |
| Vegan diet | 2 (2.99%) | 1 (1.33%) | 0.602 | |
| Vegetarian diet | 5 (7.46%) | 4 (5.33%) | 0.735 | |
| Lots of vegetables and fruits | 20 (29.85%) | 13 (17.33%) | 0.118 | |
| Fast food | 14 (20.90%) | 9 (12.00%) | 0.227 | |
| Regular meals | 32 (47.76%) | 35 (46.67%) | 1 | |
| Healthy diet | 33 (49.25%) | 38 (50.67%) | 1 | |
| Increase in food spending since the introduction of the diet | PLN 10–50 | 15 (22.39%) | 4 (5.33%) | < 0.001* |
| PLN 50–100 | 20 (29.85%) | 9 (12.00%) | ||
| PLN 100–200 | 10 (14.93%) | 6 (8.00%) | ||
| More than PLN 200 | 6 (8.96%) | 2 (2.67%) | ||
| Not applicable | 16 (23.88%) | 54 (72.00%) | ||
| Consumption of products that cause intolerance despite the use of an elimination diet | Yes | 32 (47.76%) | 13 (17.33%) | < 0.001* |
| Unintentionally | 18 (26.87%) | 22 (29.33%) | ||
| No | 12 (17.91%) | 20 (26.67%) | ||
| Not applicable | 5 (7.46%) | 20 (26.67%) | ||
| Circumstances hindering the maintenance of the diet** | Events | 30 (44.78%) | 18 (24.00%) | 0.015* |
| Numerous responsibilities – lack of time | 9 (13.43%) | 12 (16.00%) | 0.847 | |
| Business trips | 14 (20.90%) | 14 (18.67%) | 0.903 | |
| Accidental ingestion of food containing the product | 26 (38.81%) | 40 (53.33%) | 0.118 | |
| Social gatherings | 31 (46.27%) | 16 (21.33%) | 0.003* | |
| Stressful situations in life | 11 (16.42%) | 12 (16.00%) | 1 | |
| Vacation | 23 (34.33%) | 22 (29.33%) | 0.647 | |
| Going to the restaurant | 25 (37.31%) | 23 (30.67%) | 0.51 | |
| Do you find it difficult to follow an elimination diet? | Yes | 37 (55.22%) | 43 (57.33%) | 0.923 |
| No | 21 (31.34%) | 21 (28.00%) | ||
| I have no opinion | 7 (10.45%) | 8 (10.67%) | ||
| No data available | 2 (2.99%) | 3 (4.00%) | ||
p – for quantitative variables – the Mann-Whitney test, for qualitative variables – the c2 test or the Fisher’s exact test.
Statistically significant difference (p < 0.05).
Multiple choice question – interest does not add up to 100.
Discussion
The problem of food intolerance in the Polish population is growing. At the same time, the therapy proposed to patients, mainly based on elimination diets, often negatively affects the lifestyle of patients.
The respondents were asked what diet they followed. The majority (57.7%) of the respondents declared that they ate in a healthy way. This is a subjective feeling of patients, which should be verified by a dietician in optimal conditions. Research shows that knowledge about the principles of healthy eating is generally relatively low. At the same time, interest in a healthy diet and the principles of proper nutrition is growing [1]. A proper, healthy diet and physical activity are of key importance for the well-being of the body and reduce the risk of cardiovascular diseases. Proper nutrition and weight maintenance lowers blood glucose levels and prevents the development of type 2 diabetes [2].
It is worth noting that 36.6% of the respondents stated that being too busy was the reason for improper composition of the diet. This is certainly one of the serious problems associated with the modern lifestyle. Among the respondents, 33.1% eat regularly, and only 23.2% eat a lot of vegetables and fruits. On the other hand, only 16.2% report eating fast food. Identification of the factors causing an incorrect, irregular diet, which includes highly processed products, is of key importance in the context of conducting a correct and effective intervention leading to the reduction and maintenance of normal body weight [1]. The professional work performed, the multitude of duties, often make it difficult or even impossible to follow a proper diet. In 2019, an interesting meta-analysis of the nutrition of nurses working in shifts compared to those working regular hours was published. In this group, higher consumption of coffee (and other caffeinated beverages), lower alcohol consumption, lower consumption of vegetables and fruits, increased frequency of snacking, later time of the last meal, irregular consumption of meals and generally lower quality of diet were found [3]. Problems in personal and professional life, as well as mental disorders can also have a negative impact on the way of eating, and interventions in such cases must be interdisciplinary. It is necessary to identify and comprehensively treat the problems that cause the patient’s poor diet [4].
It is worth noting that in the analysed population, people over 30 had the greatest problem with maintaining an elimination diet. This may be related to the fact that at this age most people already have a job, family responsibilities, children, and loans. This often causes a reduction in attention to one’s health and physical condition. Studies show that married people have a higher body mass than single people, which most likely indicates shifting attention to other areas of life [5, 6].
Food intolerance was declared by 109 patients. Among these subjects, lactose intolerance was the most common (68 subjects, 62.4%), followed by gluten intolerance (37 subjects, 33.9% of people with intolerance). Intolerance to some fruits occurred in 33 patients, vegetables in only 15 patients, honey in 6 patients. Four people declared food allergy. These results are understandable from an epidemiological point of view. Lactose intolerance is very common in the adult population, although its prevalence varies from population to population. It is the most common food intolerance in the practice of a family doctor, it is estimated that it affects about 50 million citizens of the United States of America [7]. In Indonesia, a country where milk and dairy products are generally not a significant part of the adult diet, new epidemiological studies have estimated the prevalence of lactose intolerance to be 66% in the population [8]. In Poland, it is estimated that up to 37% of the population struggles with adult hypolactasia [9].
Abnormal symptoms after eating gluten can have different aetiologies. Gluten intolerance in the form of celiac disease, a serious, genetic disease in which autoimmunity plays a key role, occurs in about 1% of the population [10].
Allergy to wheat flour, hypersensitivity of immunological aetiology, has symptoms slightly different than celiac disease, but many ailments may be non-specific for these two diseases. To differentiate them, it is necessary to perform additional diagnostic tests [11]. The most controversial form of gluten intolerance is NCGS (Non-Celiac Gluten Sensitivity). In this intolerance there are non-specific symptoms: flatulence, abdominal discomfort, diarrhoea and excessive intestinal gas. Symptoms of NCGS may suggest the presence of irritable bowel syndrome, but also other food intolerances. Moreover, severe, debilitating diseases, such as Crohn’s disease, also have such symptoms in their spectrum [12]. In recent years, a gluten-free diet has become for many patients the answer to many other disease entities. Popular theories say that its effect is beneficial in patients with autism, neurological, rheumatological and psychiatric diseases [13]. These controversial views may lead to unjustified use of gluten-free diets, which is unfavourable for the patient for many reasons, including the increased cost of such a diet or social and professional limitations associated with the need for intensive modification of the diet [11]. There is no doubt that gluten is relatively hard to digest, which can cause abdominal discomfort in some people, even completely healthy [14].
Another group of products that are not tolerated by many patients is fruit. Several mechanisms may be responsible for this. On the one hand, fruits are a source of fructose. Fructose intolerance is a problem that is often underestimated. The recessive form is a serious metabolic disease diagnosed in early childhood, associated with insufficient production of aldolase B. It is a rare disease in which a diet low in fructose allows patients to function normally [15]. The condition that should be considered in the study population, among people declaring fruit intolerance, is intolerance of fructose present in the diet or, more broadly, intolerance of fermentable carbohydrates. This is a problem characteristic of patients with symptoms of irritable bowel syndrome who benefit from a low-FODMAP diet [16].
Concerns after eating food reported by the respondents were typical of food intolerances. First of all, they involved the digestive system: abdominal pain, diarrhoea, bloating, sometimes nausea, less often constipation. Symptoms from other systems occurred much less frequently in the study population. Food intolerances mainly manifest themselves in this way [17].
In a study of 109 people diagnosed with food intolerance, all of them followed an elimination diet. What is particularly important, as many as 104 people (95.4% of the group of people using the elimination diet) stated that the elimination diet had a positive impact on their well-being and quality of life, resulting in a reduction or complete disappearance of bothersome symptoms. Other people did not notice any difference in their well-being after introducing the diet. An elimination diet, when used correctly, is effective in eliminating symptoms. A properly selected diet should be nutritious and tasty at the same time, in line with the patient’s lifestyle, and easy to prepare. It must also be calorically balanced so as not to cause unintended weight gain or loss [18].
An important aspect of the use of elimination diets is the introduction of a substitute in place of the eliminated product, which is designed to, on the one hand, ensure a variety of flavours in the diet, and on the other hand, in optimal conditions, prevent nutritional deficiencies. 66 respondents stated that they used substitutes in the elimination diet. Forty-three (39.4%) people using the elimination diet did not introduce any substitutes to the diet. It is puzzling why almost 40% of the studied population, despite the elimination of the nutrient, did not replace it with a substitute. There may be several reasons for this phenomenon. On the one hand, the problem may be the lack of sufficient knowledge about food substitutes, lack of proper education and diet preparation by a dietitian. Another problem may be the cost of substitutes, and yet another problem is their availability or taste, which is not accepted by the patient.
A healthy diet in general can be a significant financial burden. Both healthy food products and specialist consultations, including dietary consultations, may be beyond the financial reach of many patients. A meta-analysis from 2017, published by Sun et al., estimated, based on the available studies, that the mean cost of a dietary intervention leading to a loss of 1 kg of body weight ranged from $34.06 for 6 months to $1,005.36 for 12 months [19]. In Polish conditions, these costs are probably lower, but still important for the household budget.
In the surveyed population, as many as 57 (52.3%) people stated that substitutes used in the elimination diet were expensive products, and only 23 (21%) people said that they did not constitute a significant burden on the household budget. The introduction of a professionally planned diet is often associated with a financial burden for the patient. Even a slimming diet based on a reduced calorie supply can be relatively expensive. The inclusion of high-quality products in the diet, as well as dietary advice, represent a significant burden on the household budget. It should also be borne in mind that the availability of food varies significantly in different parts of the world. In 2019, an analysis by the EAT-Lancet commission was published. The goal of the researchers was to create a universal, healthy diet that could be used around the world. The cheapest, wholesome diet proposed by the EAT-Lancet, on a global scale, is still beyond the reach of 1.58 billion people [20]. The Mediterranean diet is considered to be one of the cheapest and, at the same time, nutritious diets [21]. Fortunately, Poland is one of the countries where the vast majority of citizens can afford a proper diet.
The subjective feeling of the scale of the financial burden depends on the individual situation of the patient, and when composing the diet, the financial capabilities of the patient should be taken into account. Even in highly developed countries with a high overall level of income among citizens, such as Denmark, differences in diet are noticeable depending on the level of income. Interestingly, these differences often concern access to healthy food, including the so-called superfoods, such as chia seeds, quinoa or goji berries [22].
Respondents in the current study most often used lactose-free products (30 respondents), followed by gluten-free products (25 respondents). In addition, the respondents chose fruits and vegetables that did not cause intolerance symptoms, which also affected their overall diet. The respondents answered the question of how much their expenses increased during the elimination diet. Twenty-one percent of respondents stated an increase in expenses at the level of PLN 50–100/month, 13% at the level of PLN 10–50/month, 11% at the level of PLN 100–200/month, and only 6% stated that they had to spend even more on replacements. The scale of the budget burden does not seem large, however, if one also takes into account dietary consultations, professional literature, and possible additional research aimed at determining possible food deficiencies, it could turn out that lifestyle changes forced by a food intolerance are for many people in a serious burden on our country’s budget.
In the case of food intolerances, one of the key directions of development for the food industry is the creation of widely available, tasty and cheap equivalents of intolerant products, such as vegetable milk, used by patients with lactose intolerance [23]. Please note that the substitute may be, like lactose-free cow’s milk, simply devoid of intolerant sugars. However, sometimes it is a substance with similar culinary properties, similar appearance and taste, but with a completely different composition, which must be taken into account when composing a diet [24].
Research shows that gluten-free products are definitely less available and much more expensive than their gluten counterparts. Gluten-free products of all types can be purchased online, and they are also widely available in health food stores. In typical grocery stores, unfortunately, it is not always possible to buy the product you need. The price of products for many patients is prohibitive. For example, gluten-free pasta costs about 2× more than standard pasta [25].
When preparing a diet for a patient, a dietitian must take into account the patient’s financial capabilities. It is possible to use substitutes that will not significantly increase the cost of the diet. You can, by including seeds in your diet, choose the cheaper ones, which still contain a high concentration of unsaturated omega-3 fatty acids [26]. However, this requires knowledge and recognition of the patient’s needs, as well as an honest conversation with him/her. Our study confirmed that a gluten-free diet is associated with a significant increase in expenses, while lactose intolerance causes a relatively less burden on the budget. Going out to restaurants and socializing are especially difficult for people with lactose intolerance. People on a gluten-free diet fare relatively better in these circumstances.
Unfortunately, patients quite often do not follow the recommended diet, even if it is the most perfect and best suited to their needs. Although the respondents do not make daily dietary mistakes often, the majority of patients consume illegal products regularly, weekly or monthly. The reason for this phenomenon is a lifestyle that is very demanding nowadays. Young, active people often travel, have business dinners, go on vacation, and meet friends. All these situations complicate the diet. The most comfortable for a person who uses an elimination diet is certainly staying at home and preparing meals on their own. Research shows that eating healthy meals together as a family has a positive effect on the diet of children and adults [27].
The respondents most often indicated that the situations in which they consume prohibited food were, on the one hand, going out to restaurants, parties, social and business meetings. On the other hand, as many as 66 patients indicated that they ate forbidden food accidentally. For patients on an elimination diet, proper labelling of food products is of key importance. Access to information on the composition of food has been significantly improved by currently applicable Regulation (EU) No. 1169/2011 of the European Parliament and of the Council of 25 October 2011 on the provision of food information to consumers. It lists the food ingredients that must be enumerated in the composition of foods if they were used during production and are still present in the product (gluten-containing cereals, shellfish, eggs, fish, peanuts, soybeans, milk, nuts, celery, mustard, sesame, sulfur dioxide and sulphites above 10 mg/kg, lupine and molluscs).
The Regulation prescribes that these ingredients must be indicated by a letter clearly distinguishing them from the rest of ingredients. The consumer must also have access to the composition of unpackaged food, although it is not specified in what form [28]. Please note that food labelling rules differ outside of the European Union. For example, Japan requires labelling of 7 food ingredients (eggs, cow’s milk, wheat, buckwheat, peanuts, shrimps and crabs), and recommends a further 21 [29]. Unfortunately, dishes can be contaminated with food from other sources, so it happens that a given dish may contain ingredients that generally should not be in it. This is particularly important for patients at risk of anaphylactic shock, but it can also cause troublesome symptoms in people struggling with food intolerance [30, 31]. It is extremely important to train people involved in gastronomy about allergies and food intolerances to avoid cases where a person using a specific elimination diet will be unknowingly exposed to a given food [28].
In addition, it is extremely important to train patients struggling with food intolerance. The aim of educating patients is not only to familiarize them with the principles of diet, but also to explain how to look for healthy and safe products, what food labelling to pay attention to, and how to prepare healthy dishes. Moreover, it is important to help identify situations that lead to non-compliance with the diet. Among the respondents in the presented study, 45% believe that their knowledge about food intolerances is insufficient. Certainly, an additional problem is that patients often use inappropriate sources of knowledge about food intolerance and use alternative, inappropriate diagnostic tests [32]. Providing patients with reliable sources of information on food intolerances and clarifying any doubts that may arise during treatment is an important aspect of a dietician’s work.
The study has some limitations that affect the interpretation of the results. The population was selected at random, but the results of the study may be affected by the fact that the respondents were members of thematic groups on Facebook. As a result, subjects are initially interested in the issue of food intolerance, mainly due to the presence of symptoms that may indicate such intolerance. A similar number of men and women took part in the study (46% vs. 54%), but the young age of the respondents is noteworthy (mean age: 27.6 ±7.4 years). This is determined by the methodology used, which, unfortunately, to some extent excludes a significant number of middle-aged and older patients who use social networking sites less frequently. In 2017, Whitaker et al. published a meta-analysis presenting the use of social networking sites in recruiting respondents for research in the field of biomedicine. Researchers found that this method is effective, inexpensive, and allows to reach a wide group of patients in a short time. However, the limitation is the overrepresentation of young people in the surveyed population, and people from environments where there is no access to a computer or the Internet are automatically excluded from the research [33]. The results obtained in the study should be interpreted taking into account the described methodological limitations.
Conclusions
The use of an elimination diet is often difficult, it affects the patient’s lifestyle, especially in the context of social and business occasions. What is more, the introduction of diet substitutes may be a burden on the household budget and not everyone will be able to fully use the possibilities available in composing the diet of people with food intolerances. An interesting conclusion from the study is the fact that patients with lactose intolerance report slightly different problems compared to people with gluten intolerance. The cost of the diet has been found to be less of an issue among people with lactose intolerance, and it is more difficult to stick to the diet during social gatherings. In the case of gluten intolerance, the cost of gluten-free products is a primary concern for patients.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.de Ridder D, Kroese F, Evers C, et al. Healthy diet: health impact, prevalence, correlates, and interventions. Psychol Health 2017; 32: 907-41. [DOI] [PubMed] [Google Scholar]
- 2.Patnode CD, Evans CV, Senger CA, et al. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults without known cardiovascular disease risk factors: updated systematic review for the U.S. Preventive Services Task Force [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2017. Jul. Report No.: 15-05222-EF-1. [PubMed] [Google Scholar]
- 3.Pepłoñska B, Nowak P, Trafalska E. The association between night shift work and nutrition patterns among nurses: a literature review. Med Pr 2019; 70: 363-76. [DOI] [PubMed] [Google Scholar]
- 4.Tessier JM, Erickson ZD, Meyer HB, et al. Therapeutic lifestyle changes: impact on weight, quality of life, and psychiatric symptoms in veterans with mental illness. Mil Med 2017; 182: e1738-44. [DOI] [PubMed] [Google Scholar]
- 5.Teachman J. Body weight, marital status, and changes in marital status. J Fam Issues 2016; 37: 74-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perelli-Harris B, Hoherz S, Lappegård T, Evans A. Mind the “happiness” gap: the relationship between cohabitation, marriage, and subjective well-being in the United Kingdom, Australia, Germany, and Norway. Demography 2019; 56: 1219-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rusynyk RA, Still CD. Lactose intolerance. J Am Osteopath Assoc 2001; 101: S10-2. [PubMed] [Google Scholar]
- 8.Dewiasty E, Setiati S, Agustina R, et al. Prevalence of lactose intolerance and nutrients intake in an older population regarded as lactase non-persistent. Clin Nutr ESPEN 2021; 43: 317-21. [DOI] [PubMed] [Google Scholar]
- 9.Zatwarnicki P. Nietolerancja laktozy – przyczyny, objawy, diagnostyka. Pielêgniarstwo i Zdrowie Publiczne 2014; 4: S273-6. [Google Scholar]
- 10.Lebwohl B, Sanders DS, Green PHR. Coeliac disease. Lancet 2018; 391: 70-81. [DOI] [PubMed] [Google Scholar]
- 11.Bartuzi Z, Ukleja-Sokołowska N. Alergia pokarmowa na mąkę i celiakia. Alergia 2014; 2: 4-10. [Google Scholar]
- 12.Roszkowska A, Pawlicka M, Mroczek A, et al. Non-celiac gluten sensitivity: a review. Medicina 2019; 55: 222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Palmieri B, Vadala’ M, Laurino C. Gluten-free diet in non-celiac patients: beliefs, truths, advantages and disadvantages. Minerva Gastroenterol Dietol 2019; 65: 153-62. [DOI] [PubMed] [Google Scholar]
- 14.Biesiekierski JR. What is gluten? J Gastroenterol Hepatol 2017; 32 Suppl 1: 78-81. [DOI] [PubMed] [Google Scholar]
- 15.Ali M, Rellos P, Cox TM. Hereditary fructose intolerance. J Med Genet 1998; 35: 353-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fedewa A, Rao SS. Dietary fructose intolerance, fructan intolerance and FODMAPs. Curr Gastroenterol Rep 2014; 16: 370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gargano D, Appanna R, Santonicola A, et al. Food allergy and intolerance: a narrative review on nutritional concerns. Nutrients 2021; 13: 1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Toca MDC, Fernández A, Orsi M, et al. Lactose intolerance: myths and facts. An update. Arch Argent Pediatr 2022; 120: 59-66. [DOI] [PubMed] [Google Scholar]
- 19.Sun Y, You W, Almeida F, et al. The effectiveness and cost of lifestyle interventions including nutrition education for diabetes prevention: a systematic review and meta-analysis. J Acad Nutr Diet 2017; 117: 404-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hirvonen K, Bai Y, Headey D, Masters WA. Affordability of the EAT-Lancet reference diet: a global analysis. Lancet Glob Health 2020; 8: e59-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Di Renzo L, Gualtieri P, de Lorenzo A, et al. The effective cost of healthy diet. Eur Rev Med Pharmacol Sci 2020; 24: 479-80. [DOI] [PubMed] [Google Scholar]
- 22.Oude Groeniger J, van Lenthe FJ, Beenackers MA, Kamphuis CB. Does social distinction contribute to socioeconomic inequalities in diet: the case of ‘superfoods’ consumption. Int J Behav Nutr Phys Act 2017; 14: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Silva ARA, Silva MMN, Ribeiro BD. Health issues and technological aspects of plant-based alternative milk. Food Res Int 2020; 131: 108972. [DOI] [PubMed] [Google Scholar]
- 24.Mäkinen OE, Wanhalinna V, Zannini E, Arendt EK. Foods for special dietary needs: non-dairy plant-based milk substitutes and fermented dairy-type products. Crit Rev Food Sci Nutr 2016; 56: 339-49. [DOI] [PubMed] [Google Scholar]
- 25.Lee AR, Ng DL, Zivin J, Green PH. Economic burden of a gluten-free diet. J Hum Nutr Diet 2007; 20: 423-30. [DOI] [PubMed] [Google Scholar]
- 26.Alasalvar C, Chang SK, Bolling B, et al. Specialty seeds: nutrients, bioactives, bioavailability, and health benefits: a comprehensive review. Compr Rev Food Sci Food Saf 2021; 20: 2382-427. [DOI] [PubMed] [Google Scholar]
- 27.Fulkerson JA, Friend S, Horning M, et al. Family home food environment and nutrition-related parent and child personal and behavioral outcomes of the Healthy Home Offerings via the Mealtime Environment (HOME) Plus Program: a randomized controlled trial. J Acad Nutr Diet 2018; 118: 240-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rozporządzenie Parlamentu Europejskiego i Rady (UE) Nr 1169/2011 120 z dnia 25 października 2011 r. Available at: https://eur-lex.europa.eu/legal-content/PL/TXT/HTML/?uri=CELEX:32011R1169&from=PL [Accessed: 20.05.2022].
- 29.Ukleja-Sokołowska N, Bartuzi Z. Alergia pokarmowa: sytuacja społeczna i prawna. Alergia Astma Immunologia 2015; 20: 88-93. [Google Scholar]
- 30.Akiyama H, Adachi R. Japanese Food Allergy-Labeling System and Comparison with the International Experience; Detection and Thresholds. Food Saf 2021; 9: 101-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boden M, Dadswell R, Hattersley S. Review of statutory and voluntary labelling of food allergens. Proc Nutr Soc 2005; 64: 475-80. [DOI] [PubMed] [Google Scholar]
- 32.Skypala IJ. Food-induced anaphylaxis: role of hidden allergens and cofactors. Front Immunol 2019; 10: 673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Whitaker C, Stevelink S, Fear N. The use of facebook in recruiting participants for health research purposes: a systematic review. J Med Internet Res 2017; 19: e290. [DOI] [PMC free article] [PubMed] [Google Scholar]