Abstract
Introduction:
We report a case of a patient who presented with incarceration of the epiploic appendix in a spigelian hernia, subsequently treated by a robotic-assisted surgical approach.
Case Description:
This is a case of a 52 year-old male patient who presented with nausea and two-week history of worsening left lower quadrant pain. On examination, the patient had an irreducible left lower quadrant mass. Computed tomography scan showed an epiploic appendagitis in a left Spigelian hernia. The patient underwent a robotic transabdominal preperitoneal hernia repair successfully and was discharged home the same day.
Conclusion:
The robotic platform was a safe and effective approach to treating the patient with no postoperative complications.
Keywords: Hernias, Incarcerated hernia, Robotic surgery, Spigelian hernia, TAPP technique, Transabdominal preperitoneal
INTRODUCTION
Spigelian hernia (SH) is a rare intraparietal abdominal wall hernia occurring medial to the semilunar line, comprising 0.1% – 1% of all hernias.1–3 The main etiologies are defects in the aponeurosis of transversus abdominus muscle inferior to the arcuate line. Due to the rectus muscle and its sheath, the sac may expand caudally and laterally along the intraparietal plane between the external and internal oblique muscles.1
Moreno-Egea et al. published the first randomized controlled trial of laparoscopic versus open SH repair showing shorter recovery and lower complications rates.4 Different subsequent authors demonstrated the feasibility and safety of the minimally invasive approach for SHs. There are few published cases of SHs performed using a robotic platform.1,2
Epiploic appendagitis is a rare entity, with an incidence of 8.8 per million patients.5 It predominantly occurs as a primary event due to torsion of the appendix epiploica with obstruction of venous outflow.6 It can ultimately result in ischemia and infarction with catastrophic outcomes for patients if not addressed in a timely manner. Incarceration within a hernia sac can also result in obstruction of the venous outflow. We report a case of a patient who presented with incarceration of the epiploic appendix in a spigelian hernia, subsequently treated by a robotic-assisted surgical approach.
CASE REPORT
Patient is a 52-year-old male with past medical history of hyperlipidemia and past surgical history of open appendectomy in his 30s. The patient presented to the emergency department (ED) with nausea and left lower quadrant pain that had been worsening for two weeks, in the setting of six months of pain. On examination he had a left lower quadrant mass, tender to palpation, that was unable to be reduced. The patient had no signs of peritonitis, no fever, and all vital signs were normal in the ED. White blood cell count was normal, 7.3 k/uL (4.8 – 10.8 k/uL), hemoglobin 15 g/dL (14 – 17.4 g/dL), and normal kidney function.
A computed tomography (CT) scan of the abdomen and pelvis showed a focal area of fatty infiltration adjacent to the junction of sigmoid and left colon, which extended out of the abdominal cavity through a small left sided spigelian hernia. On the scan, the fascial defect appeared to be approximately 2.8 cm. The inflammation extended onto the abdominal wall. Findings were consistent with epiploic appendagitis. (Figure 1).
Figure 1.
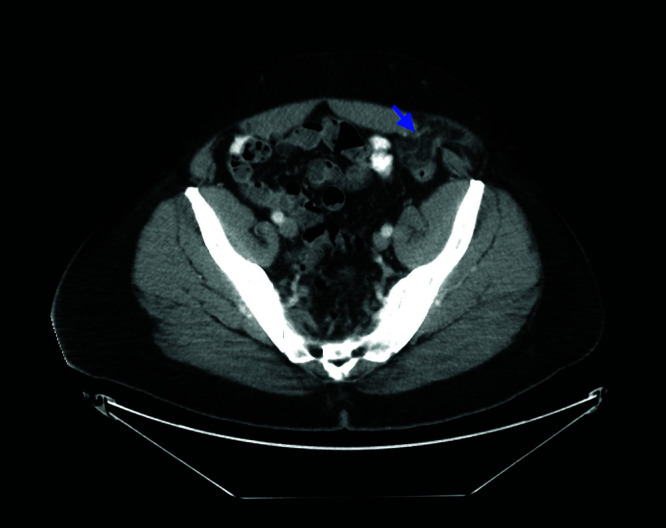
Computed tomography scan of the abdomen showing a focal area of fatty infiltration adjacent to junction of sigmoid and left colon that extended out of the abdominal cavity through a small left-sided spigelian hernia measuring 2.8 centimeters in diameter.
Surgical Technique
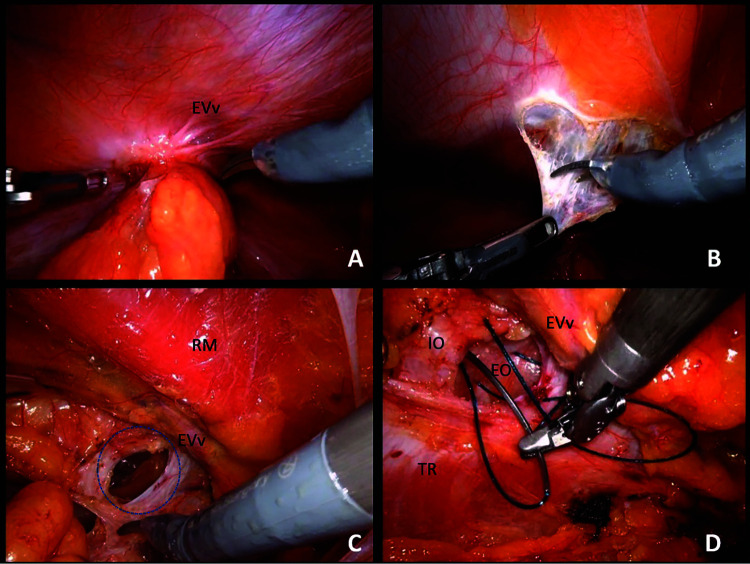
The patient was positioned in a supine position and the abdomen was prepped and draped in the usual sterile surgical fashion. After 15 mmHg was established with a Veress needle, we positioned an 8-mm robotic optical trocar in the right upper quadrant with no injury during entry and positioned two additional 8-mm ports on the right flank, each three inches apart. We docked the robot from the left side of the patient and could observe incarcerated epiploic appendages in the small left sided spigelian hernia (Figure 2a). We created a large preperitoneal dissection pocket (Figure 2b). We were able to reduce the incarcerated visceral content and a large amount of preperitoneal fat.
Figure 2.
A) Incarcerated epiploic appendages in the small left-sided spigelian hernia. B) Creating a large preperitoneal dissection pocket. C) True spigelian defect measuring around 2 × 2 centimeters. D) A 3–0 barbed suture was used to close the defect. Abbreviations: EVV, epigastric vessels; RM, rectus muscle; EO, external oblique; IO, internal oblique; TR, transverse muscle; blue dotted circle, hernia defect.
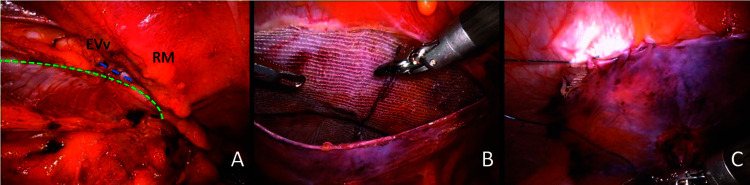
The defect measured around 2 × 2 cm (Figure 2c). We could appreciate the interparietal hernia space with intact external oblique muscle, typical of SH. We closed the defect with a 3–0 slow-absorbable barbed suture (Figures 2d and 3a). An additional defect of 1 × 1 cm was found just caudal to the larger one. We dissected posteriorly until the psoas muscle was identified as well as the area medial to Cooper's ligament. We safely preserved and dissected the vas deferens and the spermatic vessels on the left side and reduced a small cord lipoma. No inguinal hernia was identified. We obtained hemostasis and trimmed a self-gripping mesh to be 15 × 15 cm (Figure 3b) and centered it into the defect that provided coverage of the deep inguinal ring as well. The mesh was completely opened with no significant wrinkles or folds and we then closed the peritoneal flap with a running suture of 3-0 barbed suture (Figure 3c). The patient had an uncomplicated recovery and was discharged home with oral pain medication from the post-anesthesia care unit. He was seen in clinic the following week with a well healing surgical incision and with no specific complaints.
Figure 3.
A) The closed defect with a 3–0 barbed suture. B) A self-gripping mesh measuring 15 × 15 centimeters was trimmed with no wrinkles or folds. C) The peritoneal flap was closed with a running suture of 3–0 barbed suture. Abbreviations: Evv, epigastric vessels; RM, rectus muscle; green dotted line, semilunar line; small blue dotted line, closed hernia defect.
DISCUSSION
Our patient presented to the ED with nausea, abdominal pain, and the presence of a tender and irreducible mass in the left lower quadrant. Epiploic appendagitis symptoms vary in the literature. It may mimic appendicitis if on the right side, or sigmoid diverticulitis if on the left when there is no palpable mass.7 Also, patients may present with symptoms of small bowel obstruction. There are only four cases published in the literature regarding an epiploic appendagitis in SHs and there is only one case with a confirmed diagnosis by ultrasound and CT scan prior to the operation. Our patient was the second in the literature to have a pre-operative diagnosis confirmed by CT scan.7 There are two cases published in the literature regarding an epiploic appendage incarcerated in a femoral hernia.8,9
There are many studies showing the safety and feasibility of the minimally invasive approach for the treatment of SHs. As SH is a rare disease, most publications are case reports. Recently, two authors published a case series of a robotic approach for the treatment of SH.1,2 Pirolla et al. (2015), published his 20 years’ experience with five cases treated laparoscopically and two cases treated with robotic surgery. Jamshidian et al. (2017) published his case series with three patients who underwent robotic transabdominal preperitoneal SH repair. Mean operative time was 88 min (range 48 – 130 min) and mean hospital length of stay was 0.3 d (range 0 – 1 d).
Use of the robotic platform has increased for abdominal wall repair over the last years, especially in complex abdominal wall reconstruction. For inguinal hernias, the RIVAL trial showed that for primary and uncomplicated inguinal hernias, there was no advantage in using the robotic platform when compared with the traditional laparoscopic approach.10 Regarding SH, there are no ongoing trials comparing a laparoscopic approach to robotic surgery.
Regarding the imaging modalities to diagnose an incarcerated SH, CT findings are similar to ultrasound findings. However, ultrasound has specific advantages to diagnose the incompressibility of the lesion, visualize adherences to the parietal peritoneum, and establish a precise correlation between the location of the lesion and the tenderness.7 In our case, we opted to do a CT scan as it was readily available in the moment.
Our patient did not have a strangulated hernia and the surgical field did not show any sign of ischemia, infarction, infection, and normal white cell blood count. This guided the decision to use a synthetic mesh after closing the defect. Furthermore, we used a 15 × 15 cm mesh to guarantee a proper overlap and decrease the likelihood of recurrence.
CONCLUSION
This report presents an extremely rare surgical disease, with only five patients undergoing robotic repair of SH and four patients reported with epiploic appendagitis due to incarcerated SH.1,2,7 The robotic platform was a safe and effective method for treating the patient with no postoperative complications. Further studies comparing laparoscopic and robotic approaches should be performed in the future to evaluate the best surgical approach to benefit the patient.
Footnotes
Author contribution: Study design: F. Malcher, D.L. Lima, A. Alcabes; Data collection: V. Viscarret, D.L. Lima, A. Alcabes; Manuscript preparation and editing: F. Malcher, R. Nogueira, D.L. Lima.
Acknowledgements: none.
Disclosure: none.
Funding sources: none.
Conflict of interests: Dr. Malcher discloses consulting fees from BD, Intuitive, Integra, Allergan, DeepBlue, and Medtronic, outside the submitted work.
Informed consent: Dr. Diego L. Lima declares that written informed consent was obtained from the patient/s for publication of this study/report and any accompanying images.
Contributor Information
Diego L. Lima, Department of Surgery, Montefiore Medical Center, The Bronx, NY..
Analena Alcabes, Department of Surgery, Montefiore Medical Center, The Bronx, NY..
Valentina Viscarret, Department of Surgery, Montefiore Medical Center, The Bronx, NY..
Raquel Nogueira, Division of General Surgery, NYU Langone Health, New York, NY..
Flavio Malcher, Center for Abdominal Core Health, Division of General Surgery, NYU Langone Health, New York, NY..
References
- 1.Jamshidian M, Stanek S, Sferra J, Jamil T. Robotic repair of symptomatic Spigelian hernias: a series of three cases and surgical technique review. J Robot Surg. 2018;12(3):557–560. [DOI] [PubMed] [Google Scholar]
- 2.Pirolla EH, Fregni F, Godoy-Santos AL, Schraibman V. A feasibility report of a novel and unpublished surgical approach for Spiegel’s hernia reconstruction using robotics-assisted surgery. Adv Health Care Technol. 2015;1:3–12. [Google Scholar]
- 3.Bittner JG, Edwards MA, Shah MB, MacFadyen BV, Mellinger JD. Mesh-free laparoscopic spigelian hernia repair. Am Surg. 2008;74(8):713–7–20.. [PubMed] [Google Scholar]
- 4.Moreno-Egea A, Carrasco L, Girela E, Martín J-G, Aguayo JL, Canteras M. Open vs laparoscopic repair of spigelian hernia: a prospective randomized trial. Arch Surg Chic Ill (1960). 2002;137(11):1266–126–8.. [DOI] [PubMed] [Google Scholar]
- 5.de Brito P, Gomez MA, Besson M, Scotto B, Huten N, Alison D. Frequency and epidemiology of primary epiploic appendagitis on CT in adults with abdominal pain . J Radiol. 2008;89(2):235–2–43.. [DOI] [PubMed] [Google Scholar]
- 6.Singh AK, Gervais D, Rhea J, Mueller P, Noveline RA. Acute epiploic appendagitis in hernia sac: CT appearance. Emerg Radiol. 2005;11(4):226–22–7.. [DOI] [PubMed] [Google Scholar]
- 7.Coulier B, Broze B. Epiploic appendagitis within a Spigelian hernia. JBR-BTR. 2010;93(5):271. [DOI] [PubMed] [Google Scholar]
- 8.McArthur D, McArthur C. Epiploic appendagitis in a femoral hernia. J Radiol Case Rep. 2019;13(5):10–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Janež J. Epiploic appendix of the sigmoid colon incarcerated in the right femoral hernial sac – case report. Int J Med Pharm Case Rep. 2018;11(1):1–3.. [Google Scholar]
- 10.Prabhu AS, Carbonell A, Hope W, et al. Robotic inguinal vs transabdominal laparoscopic inguinal hernia repair: The RIVAL Randomized Clinical Trial. JAMA Surg. 2020;155(5):380–387. [DOI] [PMC free article] [PubMed] [Google Scholar]