Abstract
Background and Objectives:
Falls are a leading cause of injuries and injury deaths for older adults. The Centers for Disease Control and Prevention’s Stopping Elderly Accidents Deaths and Injuries (STEADI) initiative, a multifactorial approach to fall prevention, was adapted for implementation within the primary care setting of a health system in upstate New York. The purpose of this article is to: (a) report process evaluation results for this implementation using the Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework and (b) examine the utility of RE-AIM for assessing barriers and facilitators.
Research Design and Methods:
This evaluation used mixed methods. Qualitative evaluation involved semistructured interviews with key stakeholders and intercept interviews with health care providers and clinic staff. Quantitative methods utilized surveys with clinic staff. Process evaluation tools were developed based on the AIM dimensions of the RE-AIM framework. The study was conducted over a 2-month period, approximately 18 months postimplementation, and complements previously published results of the program’s reach and effectiveness.
Results:
Primary barriers by RE-AIM construct included competing organizational priorities (Adoption), competing patient care demands (Implementation), and staff turnover (Maintenance). Primary facilitators included having a physician champion (Adoption), preparing and training staff (Implementation), and communicating about STEADI and recognizing accomplishments (Maintenance).
Discussion and Implications:
Results revealed a high degree of concordance between qualitative and quantitative analyses. The framework supported assessments of various stakeholders, multiple organizational levels, and the sequence of practice change activities. Mixed methods yielded rich data to inform future implementations of STEADI-based fall prevention.
Keywords: Analysis—mixed methods, Barriers and facilitators, Evaluation, Falls, STEADI
Background and Objectives
Falls are a leading cause of injuries and deaths among older adults (aged ≥65 years) resulting in over 36,000 deaths, 1.8 million treat and release emergency department visits, and almost one million hospitalizations in 2020 (Centers for Disease Control and Prevention [CDC], 2022). Over one fourth of older adults reported at least one fall in the previous year, with more than a third of them having an injury that required medical treatment or limited their activity for at least a day (Moreland et al., 2020). Less than half of older adults who fall inform their health care provider (Stevens et al., 2012). And over 60% of physicians reported that they conducted falls screening only if the patient expressed concern about falling (Jones et al., 2011). Factors identified as barriers to fall risk evaluation and management in the practice setting include contending priorities, competing for patient care demands, lack of time during visit, training deficiencies, and inadequate or inappropriate referrals (Baker et al., 2005; Chou et al., 2006; Smith et al., 2015).
CDC developed the Stopping Elderly Accidents, Deaths and Injuries (STEADI) initiative to assist health care providers to incorporate fall risk assessment into routine clinical practice (Phelan et al., 2015; Stevens & Phelan, 2013) and was based on American Geriatric and British Geriatrics Societies’ Clinical Practice Guideline and health behavior theory (Panel on Prevention of Falls in Older Persons, 2011). STEADI advocates a multifactorial approach to fall prevention, including (a) screening older adults to determine their fall risk, (b) assessing for modifiable fall risk factors such as gait or balance issues for those at-risk, and (c) intervening with evidence-based programs such as strength and balance exercises to address identified risk factors (Phelan & Ritchey, 2018). The CDC website (www.cdc.gov/STEADI/) offers resources and materials such as a clinical algorithm, fact sheets, and training videos to assist health care providers with conducting clinical fall risk assessments (CFRAs) and providing fall prevention interventions in the primary care setting. These resources have been widely distributed (Sarmiento & Lee, 2017).
The New York State Department of Health received funding from CDC for a fall prevention initiative based on STEADI, which was implemented across all primary care practice locations of United Health Services (UHS) beginning in September 2012 (Stevens, Smith et al., 2017).
In their workflow, tasks were split between the nurse or clinical support staff and the health care provider (Supplementary Figure 1). The nurse or a clinical support staff conducted the initial screening, and results were entered into the electronic medical record (EMR). If the older adult was at-risk, then a Timed Up and Go (TUG) test was administered, and a paper-based referral form was left on the keyboard for the health care provider. Next, the health care provider conducted a multifaceted risk, discussed fall risk with the patient, and developed a fall plan of care.
The Oregon Health & Science University concurrently implemented STEADI-based fall prevention into their primary care practice and reported facilitators, including identifying a physician champion, using the EMR to prompt fall prevention, and modifying STEADI to fit into the clinical workflow (Casey et al., 2017). The major barrier identified was physician concerns about sufficient time during an office visit to conduct fall prevention. This process evaluation for UHS STEADI initiative builds on the previous Oregon one by examining implementation using the RE-AIM Framework in a second setting.
From 2012 to 2014 STEADI was rolled out at 19 UHS primary care practices (Stevens, Smith et al., 2017). Among practices with at least 2 years of data in 2014, 79% of patients aged 65 and older were screened for fall risk in the first year, and 18% of those screened at-risk. Screening declined to 49% during the second year, with rates improving during the third year (Stevens, Smith et al., 2017). An outcome evaluation, based on the Reach and Effectiveness elements of the RE-AIM framework, found that 90% of older adult patients were screened for fall risk at least once, and 61% of at-risk patients received a fall plan of care. Older adults at-risk for fall with a fall plan of care were 0.6 times less likely to have a fall-related hospitalization than those without one (p = .041), and their postintervention odds were similar to those who were not at-risk (Johnston et al., 2019).
Due to the success of the STEADI-based fall prevention initiative in primary care practices at UHS, reporting on the process evaluation may be informative for other health care systems wanting to adopt clinical fall prevention programs. This article reports on barriers and facilitators of the adoption, implementation, and maintenance (AIM) dimensions of the STEADI implementation at UHS with the goal of identifying opportunities for improvement and potentially informing future implementations in clinical settings as well as lessons learned from using the RE-AIM framework.
Research Design and Methods
The RE-AIM Framework
The RE-AIM Framework is a comprehensive model for planning and evaluation of health promotion programs that can inform both research and practice (Glasgow et al., 2004; Kessler et al., 2013; Klesges et al., 2005). This framework conceptualizes the impact of public health interventions as a function of five key dimensions: Reach, Effectiveness, Adoption, Implementation, and Maintenance (Glasgow et al., 1999, 2019). Reach refers to the number, proportion, and characteristics of intervention-exposed individuals (Glasgow et al., 1999). Effectiveness focuses on outcomes, both positive and negative, and can encompass behavioral, functional, and clinical effects (Glasgow et al., 1999). Reach and effectiveness are typically assessed at the individual level; whereas adoption, implementation, and maintenance characterize the intervention setting, address contextual factors, and are often multilevel (Glasgow et al., 1999, 2019). Adoption refers to the characteristics of both the intervention setting and the program agents (Glasgow et al., 1999, 2019). Implementation is concerned with fidelity, or the extent to which an intervention is implemented as intended and any adaptations (Glasgow et al., 1999, 2019). Finally, maintenance represents the institutionalization of the intervention, or the extent to which the intervention becomes a routine part of organizational culture and norms (Glasgow et al., 1999, 2019).
Strategies Used to Support Adoption, Implementation, and Maintenance of STEADI
Specific strategies were used to address key aspects of the AIM dimensions to ensure the success of the STEADI initiative (Figure 1).
Figure 1.
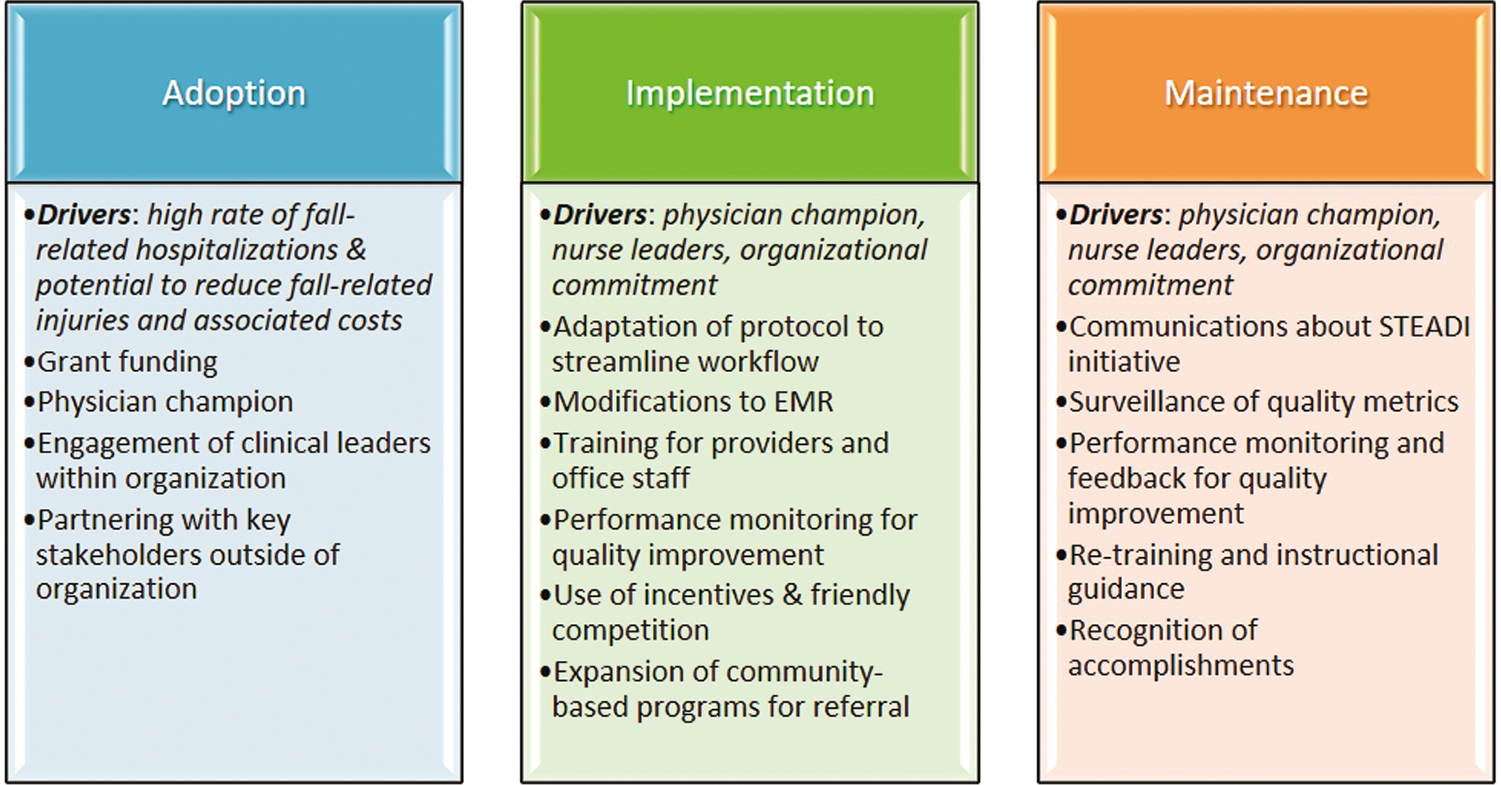
Strategies employed for the STEADI initiative by the adoption, implementation, and maintenance dimensions of the RE-AIM framework.
Notes: RE-AIM = Reach, Effectiveness, Adoption, Implementation, Maintenance; STEADI = Stopping Elderly Accidents Deaths and Injuries; EMR = electronic medical record.
Adoption strategies
The decision to adopt STEADI was twofold: (a) the high rate of fall-related hospitalizations in the region and (b) the potential to reduce fall-related injuries and associated costs (Johnston et al., 2019). The initiative received funding through CDC’s Core Violence and Injury Prevention Program to implement STEADI-based fall prevention in Broome County and was driven by a physician champion who led: (a) development of the clinical workflow protocol, (b) modifications to the EMR to facilitate fall-risk screening, (c) incorporation of fall-risk screening as a quality metric, and (d) planned to roll out for training and system-wide adoption. Dr. Frank Floyd spearheaded the initiative at UHS and engaged physician peers within the organization to help generate buy-in at both the organization and practice levels (Stevens, Smith et al., 2017). The decision to adopt had full administrative support and involved a top–down approach with two nurse leaders who directed and managed the implementation through unit coordinators within the practice sites.
Initial efforts involved significant information technology (IT) support to plan EMR modifications, including placement of screening questions on the intake screen, mechanism for verifying aged 65 or older, and system prompt for providers if the patient had not been screened in the past year. In addition, IT developed diagnostic coding protocols, data extraction and analysis methods, and prototype reports for unit- and provider-level screening rates.
Implementation strategies
The STEADI algorithm was adapted for this implementation. Leadership at UHS worked with providers to modify or remove elements of STEADI-based on provider feedback. To fit the UHS clinical workflow, the TUG test serving as the single gait and balance assessment (Stevens, Smith et al., 2017). Due to limited time during visits, providers did not take orthostatic blood pressures unless the patient reported dizziness or had an undetermined cause of gait or balance difficulty (Stevens, Smith et al., 2017). Removal of this element helped generate provider buy-in.
Another strategy to assimilate STEADI into the existing workflow was the modification to the existing EMR to incorporate STEADI screening questions (Supplementary Figure 1), including prompts for when an older adult was due for their annual fall risk screening. Screening questions and reminders in the EMR contributed to the integration of STEADI into the overall office workflow.
The STEADI initiative was implemented over a 2-year period across primary care or internal medicine practice sites with the majority occurring within the first year. All sites received training in relation to the screening protocol, documentation in the EMR, and the process for making referrals to community-based fall prevention programs. The training addressed specific responsibilities for both health care providers and clinical support staff. The physician champion and nurse leaders visited each primary care site to train providers and staff. Unit coordinators at each site were tasked with monitoring quality metrics and improving performance at the practice and provider levels. Unit coordinators reviewed screening rates to determine if refresher training was needed to maintain screening rates above the 90% benchmark.
With a portion of the funding, the Broome County Health Department (BCHD) simultaneously expanded the availability of community-based fall prevention programs such as the Tai Chi, Better Balance for Broome, and Stepping On. Referrals were made using a duplicate form, with one copy going to the older adult and one retained for upload to the EMR.
Maintenance strategies
Many of the implementation strategies also contributed to the maintenance phase, such as streamlining the process for efficient workflow and on-screen computer prompts in the EMR, as well as performance monitoring through surveillance of quality indicators. Other key strategies employed to ensure institutionalization of the STEADI initiative were communications about the STEADI initiative and recognition of accomplishments.
At the organizational level, performance monitoring kept both administrators and providers focused on operational aspects of the STEADI initiative. Unit coordinators received reports each month on STEADI screening rates and identified practices and providers with low performance. As staff turnover occurred in offices, retraining was conducted by nurse leaders, unit coordinators, or office-level staff. Providers were encouraged to follow-up on referrals at the next patient visit to determine whether patients had attended a community-based program and to inquire about its effect. Unit coordinators were responsible for scanning the referral form into the EMR, and conducting follow-up for at-risk patients. All providers attended quarterly meetings in which UHS administration provided updates and feedback on progress. Project accomplishments and national recognitions were highlighted at these meetings and in newsletters.
STEADI Process Evaluation Methods
The process evaluation used a mixed methods design, including semistructured key informant interviews, intercept interviews, and surveys approximately 18 months postimplementation in the last primary care practice. At the time of the evaluation, all UHS primary care practices in Broome County were continuing to implement STEADI. The process evaluation was conducted by the BCHD over a 2-month period from June to July 2016 and received expedited review and approval from the Institutional Review Board of UHS. The Human Subjects Research Review Committee at Binghamton University deferred to this review.
Setting
The STEADI initiative was implemented within a large not-for-profit health care organization in rural upstate New York, including 14 primary care practices that were located in Broome County. The roll out of the STEADI initiative in the UHS system is described in detail elsewhere (Stevens, Smith et al., 2017). Between initial implementation and the present study, two practices closed or were consolidated. The present evaluation, therefore, included only 12 primary care practices in Broome County, which was the target area for our previous outcome evaluation.
Participants
Participants were drawn from three stakeholder groups: (a) key stakeholders, who included a physician and nurse leaders, administrators, lead providers within practices, site supervisors, and IT personnel; (b) health care providers, comprised of physicians, nurse practitioners, and physician assistants; and (c) clinical support staff, consisting of registered nurses, licensed practical nurses, and medical office assistants.
Data collection tools
Interview protocols and surveys were developed for distinct stakeholder groups (Supplementary Table 1). The RE-AIM framework was used to guide question development for these assessments with a focus on the AIM dimensions.
Key informant interviews.—
The semistructured interview questionnaire for key stakeholders included open-ended questions about facilitators and barriers associated with the adoption, implementation, and maintenance of STEADI at UHS. The content of the semistructured key informant interviews was based on the key stakeholder’s role.
Intercept interviews.—
The intercept interview questionnaire included open-ended questions for which a brief response could be provided. The topics covered included: (a) workflow and tasks, (b) documentation of the TUG test, (c) recommendations for improvements, and (d) suggestions for others adopting STEADI. The protocol and questions comprising the intercept interviews with health care providers and clinical support staff were similar, though again with minor differences based on their specific roles.
Surveys.—
Two survey instruments were developed, one for health care providers and one for clinical support staff. Providers and clinical support staff received slightly different versions of the survey, which reflected their different roles. For example, health care providers were asked to rate their agreement to the statement, “Clinical Fall Risk Assessment with older adults is a high priority for me in my clinical practice” whereas for clinical support staff this item read, “Ensuring that Clinical Fall Risk Assessments with older adults are routinely completed is a high priority for me.” Both versions asked for scaled responses to items in the same areas: (a) attitudes and beliefs, (b) time to complete screening components, (c) facilitators and barriers, (d) feedback received, and (e) demographics.
Data collection process
The interviews and surveys were administered by project evaluators. All health care providers and clinical support staff received an e-mail 2 weeks prior to a site visit, notifying them that intercept interviews would be conducted on a specific date. Key informant interviews: individual, semistructured interviews were held with STEADI key informants, who were UHS administrators, clinic lead providers, unit coordinators and/or practice managers, IT personnel, and the nurse and physician project directors. Semistructured interviews were scheduled as face-to-face meetings or by phone at the convenience of the respondent. The interviews typically lasted 30–60 min each.
Intercept interviews.—
During the site visit, BCHD project staff conducted intercept interviews with available health care providers and clinical support staff as time allowed. To minimize workflow disruptions, the intercept interviews were designed to last no more than 5–10 min.
Surveys.—
All health care providers and clinical support staff from each of the 12 primary care practice locations were asked to complete the brief survey online. If a health care provider or clinical support staff had not completed the survey online, they were asked to complete a paper form during the site visit.
Analytic methods
Field notes taken during the key informant and intercept interviews were organized by participant type. Content analysis was conducted on transcribed field notes to examine the most commonly reported barriers and facilitators by stakeholder groups across the AIM dimensions. Interview responses were coded manually (without coding software), and related concepts were grouped into key themes for each participant type. Frequency counts were conducted on the key themes to identify the most commonly cited barriers and facilitators. The initial qualitative content analysis was performed by a single analyst and subsequently reviewed and validated by a second analyst.
Numerical data were analyzed using quantitative methods and narrative responses using qualitative methods. Descriptive statistics were conducted using Microsoft Excel and yielded frequency counts and percentages for each response item. Content analysis was conducted on open-ended items by grouping similar responses. Textual responses were conceptually coded and grouped to identify the most frequent themes.
Results
Participation
A total of 20 key informant interviews were conducted, representing 11 of the 12 primary care sites (92%) as well as organizational administration. These interviews included administrators (n = 3), practice site leaders (lead providers, n = 3; unit coordinators, n = 9), nurse leaders (n = 2), and IT personnel (n = 3). The key informant interview data for the physician champion were included under his administrative role.
Seventy intercept interviews were conducted across all 12 primary care sites. For the intercept interviews, participation rates were 63% among health care providers (n = 24) and 77% among clinical support staff (n = 46). The reported percentages by personnel type were based on the number of employees at the time of the evaluation and represent workforce estimates due to the dynamic nature of personnel.
A total of 89 surveys were collected from 10 of 12 primary care sites (83%) within Broome County (Supplementary Table 2). Of these, 48 were submitted on paper (54%) and 41 online (46%). An estimated 82% of health care providers (n = 31) and 97% of clinical support staff (n = 58) provided survey responses. For health care providers, 50% were physicians, 36% were nurse practitioners, and 14% were physician assistants. For clinical support staff who responded online (n = 30), 43% were registered nurses, 40% were certified medical assistants or medical office assistants, and 13% were licensed practical nurses. A unit coordinator accounted for the final 4%. Data for role type were not collected for 28 clinical support staff who responded via paper survey.
Qualitative Results: Barriers and Facilitators From Key Informant and Intercept Interviews
Qualitative findings from a key informant and intercept interviews, presented in Table 1, detail the most frequently cited barriers and facilitators for each AIM dimension. Notably, some items identified as barriers or facilitators were relevant to more than one of the AIM dimensions.
Table 1.
Facilitators and Barriers of Clinical Fall Risk Assessments in Primary Care
| RE-AIM | Barriers | Facilitators |
|---|---|---|
|
| ||
| Adoption | Need to modify EMR to include fall screening (KI) Competing demands for IT personnel (KI) Determining case definitions (II, KI) Complexity of IT systems (KI) |
Role of physician project leader as a “champion” (KI) Support of highest level of administration (II, KI) Recognition in working with the CDC (KI) Involvement of staff for buy-in (KI) Ability to alter STEADI to fit workflow (KI) Implementation would not require additional staff (KI) Collaboration with IT to identify appropriate indicators (KI) |
| Implementation | Resistance to administratively imposed change (KI) Top–down implementation (II, KI) Competing demands of other work (II, KI, SU) Complexity of patient needs (II, SU) Documentation burden (II, KI, SU) Time and space required for TUG test (II, KI) Narrative documentation for fall risk plan of care (II) Lack of efficiency using referral form (II) Access to/availability of fall prevention interventions in rural areas (II, KI) Lack of feedback related to follow-through on fall prevention interventions (II, SU) |
Role of physician project leader as a “champion” (KI) Favorable view of nurse leaders who garnered “buy-in” (KI) Commitment to improving health and quality of life (KI, SU) Organizational feedback on falls screening rates (KI) Organizational capacity to do data-driven analyses (KI) Adequate preparation and training (II, KI, SU) EMR screen layout quick and easy to use (KI, SU) Use of referral form for fall-risk interventions (SU) Team approach to implementation (SU) Communication among office staff (KI, SU) Belief that CFRAs reduced falls and health care costs (SU) Incentives for screening (friendly competition) (KI) Recognition and publicity (KI) |
| Maintenance | Staff turnover and training of new staff (II, KI) Need for surveillance monitoring of performance (KI) Limited resources (KI) Documentation considered time-consuming (II, KI) Systematic feedback on referrals to community-based fall-prevention programs (II, KI) Reliance on a physician champion with program success vested in one person (KI) |
Use of unit coordinators in maintaining screening rates (KI) Testimonials from patients about their participation (KI) Organizational feedback on falls screening (KI, SU) National recognition of work (KI) Perceived reduction in fall-related injuries and costs (SU) Meaningful use of health information (KI) |
Notes: II = intercept interviews; KI = key informant interviews; SU = survey; CDC = Centers for Disease Control and Prevention; STEADI = Stopping Elderly Accidents Deaths and Injuries; IT = information technology; EMR = electronic medical record; TUG = Timed Up and Go; CFRAs = clinical fall risk assessments, RE-AIM = Reach, Effectiveness, Adoption, Implementation, and Maintenance.
Adoption barriers
From the perspective of UHS administration and project leadership, implementing the STEADI protocol in its initial form would have potentially impeded the clinical workflow. The need for modification of the screening algorithm to streamline workflow and minimize adverse affects was seen as a critical barrier to adoption. Administrators and IT personnel indicated that modification of the EMR to prompt screenings and document CFRAs was a barrier to adoption. Findings from key informant interviews revealed that the variety of data systems in use over time, the lengthy process for modifying the user interface, the complexity of extracting precisely defined indicators to populate reports, and the level of sophistication required to create a surveillance system for quality monitoring posed significant challenges and prolonged the adoption period.
Adoption facilitators
Administrators and other project personnel indicated that having a physician who served as a “champion” and provided critical leadership across all phases of the project was one of the most important factors for initial adoption. This person was noted for his visibility in the community, his authority within the organization, and his clear vision for how to effectively manage clinical practice change. The physician champion was also a driving force in aligning the STEADI initiative with organizational priorities and mobilizing necessary resources.
Administrators cited the potential to reduce health care costs as an important factor in their decision to adopt STEADI. From their standpoint, the anticipated cost–benefit ratio of the proposed intervention was considered to be favorable as no additional staff would be hired, and the potential cost savings from reduced health care utilization was appealing. Furthermore, the STEADI initiative leveraged expertise and funding from the CDC with the added benefit of networking with other fall prevention researchers and expanding the development of clinical-community partnerships. The administration also believed that they had sufficient technical capacity to make the IT modifications and could make use of their wellness coordinators to facilitate the roll out.
Implementation barriers
Barriers to implementation identified by health care providers and clinical support staff during intercept interviews included factors that increased workload, including time to conduct clinical assessments such as the TUG test and increased documentation burden. Some practice locations indicated that they did not have space for conducting the TUG test. The TUG test was seen as time-consuming, difficult to perform in many offices, and an impediment to workflow. Consequently, this element of the STEADI protocol, by self-report, was often not completed.
The resistance to administratively imposed change was a concern raised by health care providers in particular. Some health care providers saw STEADI-based fall prevention as another mandate that placed additional demands on their clinical time. Further health care providers saw conducting CFRAs as competing with clinical care. While the check boxes for assessments in the EMR were seen as efficient, health care providers saw the narrative documentation for the Fall Plan of Care (FPOC) as burdensome and the paper form for referral to community-based fall prevention interventions as inefficient. This paper form, which was scanned into the chart, was cited as being more cumbersome than the established electronic system for referrals to physical therapy.
Finally, a few health care providers felt there was limited evidence to support CFRAs, and many health care providers indicated that there was limited feedback related to follow-through on fall prevention interventions. Health care providers expressed concerns about the limited availability of fall prevention interventions, especially in rural areas, as well as costs of programs and transportation. Providers did not see the benefit of screening if resources were not accessible.
Implementation facilitators
Implementation facilitators cited by key informants included the role of the physician champion as project lead and their service orientation as a “community hospital.” The nurse leaders were viewed favorably by their peers and seen as being responsible for achieving “buy-in.” Their established relationships with the various sites and their ability to oversee operations and coordinate training were viewed as an asset by administrators, health care providers, and clinical staff. Project leads felt that the extended time over which the roll out occurred and the engagement of “early adopter” sites allowed them to streamline instructional content, training delivery, and technical assistance. Administrators also cited their ability to extract and analyze data for real-time monitoring of quality metrics and to provide feedback on falls screening rates at the practice and provider levels as being essential for achieving high screening rates. Another implementation facilitator identified by key informants was the use of friendly competition within and between practices which they felt increased screening rates in a fun way. From the health care provider and clinical support staff perspective, most felt that the training and preparation were adequate, that the EMR layout was quick and easy to use, and that the prompts to conduct CRFA based on patient age and date of last screening were useful. Finally, both health care providers and clinical support staff felt that the efficient communication and workflow patterns within their practices facilitated the implementation of the STEADI protocol.
Maintenance barriers
Health care providers noted that the turnover in clinical support staff was difficult from a training perspective and adversely affected the maintenance of the STEADI protocol. Staff turnover was identified as the most common reason for observed declines in screening rates. Concern was also expressed about the ability to maintain the initiative in the future when the physician champion was no longer in that role, as well as the resources required to maintain ongoing surveillance given competing organizational priorities. From the health care provider and clinical support staff perspective, two factors that were considered barriers to implementation also were cited as longer-term impediments to maintenance. These factors included the time required for documentation and the lack of a formal mechanism for feedback after making referrals to community-based fall prevention programs.
Maintenance facilitators
The advocacy of a physician champion, the detailed orientation of the nurse leaders, and the use of wellness coordinators were seen as significant facilitators of project success. Furthermore, the team approach contributed to a sense of common purpose that aligned well with professional values. Finally, the belief that conducting CFRAs among older adults and intervening to reduce risk could improve health outcomes and lower health care costs served as a compelling motivator. Use of the EMR expanded health system capacity for conducting data driven analytics related to the STEADI fall prevention initiative. Seeing data that showed success in one site helped in expanding to other sites.
Administrators cited the meaningful use of quality indicators to improve clinical care as meeting an organizational goal and reason for continuation. For health care providers and clinical support staff, the positive informal feedback from their patients about participation in recommended fall prevention interventions and organizational feedback regarding fall screening rates were identified as facilitators in the maintenance phase. For both administrative personnel and health care providers, the national recognition that the STEADI initiative brought to the organization was seen as contributing to ongoing support for CFRAs in primary care.
Quantitative Results: Health Care Provider and Office Staff Surveys
Results of the health care provider and office staff survey are useful for contextualizing the facilitators and barriers identified from the key informant and intercept interviews and for understanding the impact on those who provide clinical care.
Attitudes and beliefs about STEADI
Overall, the STEADI program was perceived positively (Supplementary Tables 3 and 4). The majority of health care providers (70%) and clinical support staff (91%) agreed or strongly agreed that the training they received prepared them to conduct CFRAs with older adults. Most health care providers (83%) and clinical support staff (98%) agreed or strongly agreed that CFRAs was a high priority for them in their clinical practice. Furthermore, 90% of health care providers and 95% of clinical support staff indicated that they worked as a team to complete the CFRAs. Also, 90% of health care providers and 91% of clinical support staff believed that conducting CFRAs and developing a FPOC for at-risk older adults results in (a) fewer falls and fall-related injuries and (b) lower overall costs for their health care organization. These survey results demonstrate the high level of support for STEADI implementation in the primary care setting.
Attitudes toward documentation in the EMR were generally positive though health care providers had somewhat less favorable perceptions than clinical support staff. Only 61% of health care providers, compared to 86% of clinical support staff, reported that the screen layout made it quick and easy to document CFRAs. Just over 58% of health care providers indicated that documenting CFRAs in the EMR was time-consuming, and only 52% of health care providers reported that the screen layout made it quick and easy to document a FPOC. Documentation in the EMR appeared to present a greater challenge for health care providers than for clinical support staff.
The referral form used for at-risk older adults was viewed as a quick and easy way to refer patients for fall prevention by 90% of clinical support staff, but by only 72% of health care providers. A similar difference was noted for specific interventions with 89% of clinical support staff indicating that the form had all of the interventions to which they would refer a patient when compared with only 61% of health care providers.
Facilitators and barriers of STEADI
Approximately two third of health care providers identified competing demands of other work and the complexity of patient care needs as the two most significant barriers to conducting CFRAs in their practice (Supplementary Tables 5 and 6) compared to clinical support staff with only 26% identifying competing demands and 21% complexity of care needs as barriers. The most commonly cited facilitator of CFRAs for both health care providers (67%) and clinical support staff (60%) was “professional/personal commitment.” Coordination of office workflow and communication among staff were identified as facilitators by more than half of health care providers and nearly half of the clinical support staff. On-screen computer prompts were identified as facilitators by more than half of clinical support staff and nearly half of health care providers. Of note, more than half of health care providers and clinical support staff indicated that administrative leadership was neither a barrier nor a facilitator. A greater proportion of health care providers viewed staffing levels as a barrier, while the modal category for clinical support staff was neutral.
Frequency of feedback
Fifty-five percent of health care providers and 48% of clinical support staff reported frequently or always receiving organizational feedback on their performance (Supplementary Tables 7 and 8). More than half of health care providers and clinical support staff reported that they rarely or never received feedback from patients about the impact of fall risk screening on their overall well-being or on their participation in community-based falls prevention programs. Approximately 46% of health care providers reported that they frequently or always received patient feedback about their participation in physical therapy, however, clinical support staff received feedback about physical therapy only 26% of the time.
Discussion and Implications
The process evaluation of STEADI-based fall prevention revealed several factors that either facilitated or inhibited successful implementation (Figure 2). Key success factors related to adoption included: (a) use of respected leaders as champions, (b) modification of the STEADI workflow for efficiency, (c) early engagement with IT personnel to adapt the EMR, and (d) building organizational capacity to support the planned intervention. These success factors were similar to those cited in an implementation of STEADI-based fall prevention in an academic setting: using clinical champions, adapting STEADI to the clinical workflow, and leveraging EMR tools (Casey et al., 2017; Eckstrom et al., 2017).
Figure 2.
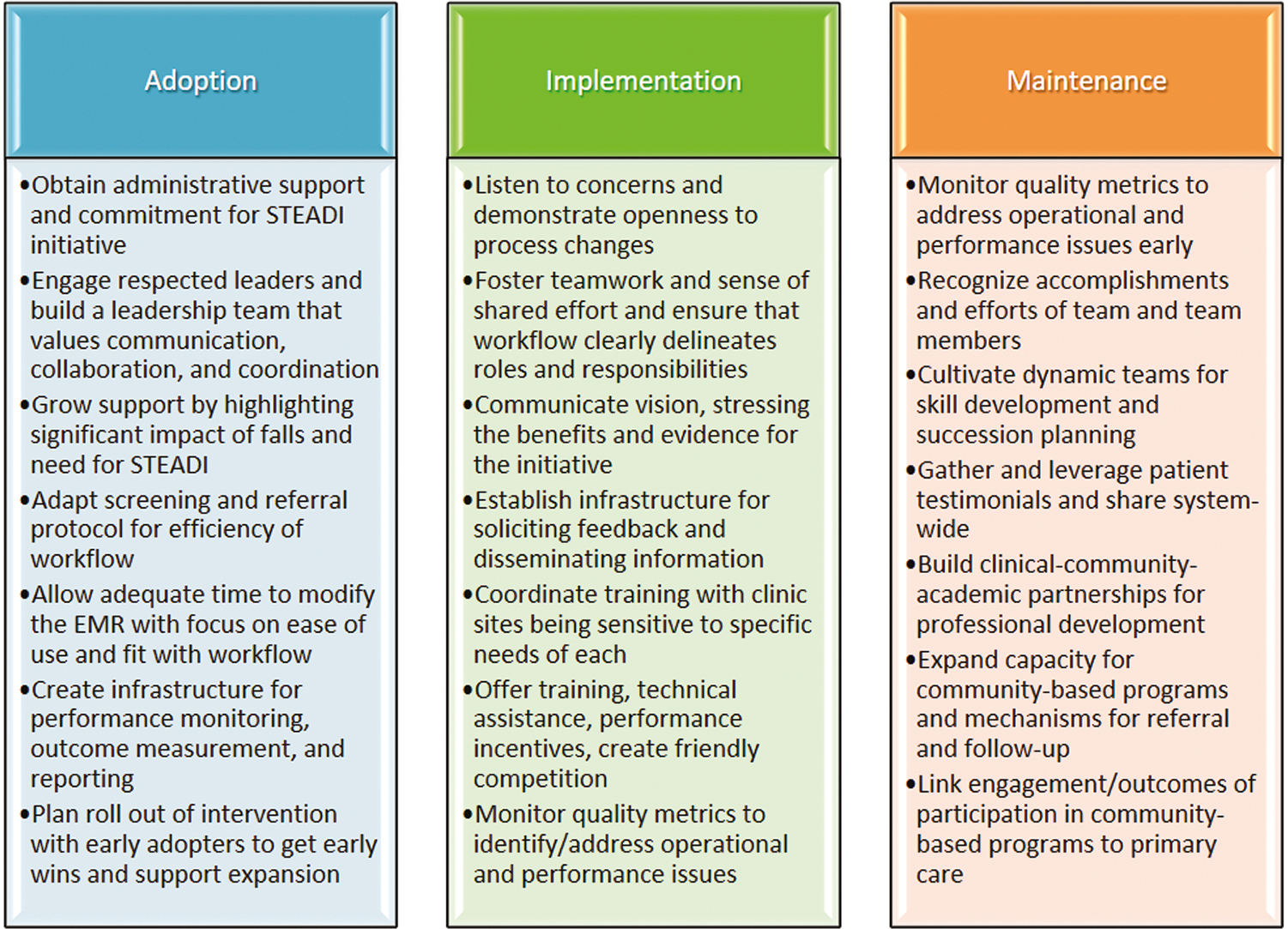
Success strategies specific to the adoption, implementation, and maintenance dimensions of STEADI using the RE-AIM framework.
Notes: RE-AIM = Reach, Effectiveness, Adoption, Implementation, Maintenance; STEADI = Stopping Elderly Accidents Deaths and Injuries; EMR = electronic medical record.
The strategies during implementation that supported success included: (a) workflow modifications, (b) emphasis on teamwork with clearly defined roles for clinical support staff and health care providers, (c) use of existing communication channels to disseminate implementation-related information, (d) custom training for each site while stressing key elements of the protocol, (e) availability of personnel for technical assistance, and (f) identifying and addressing performance issues using quality indicators. The central issue encountered during implementation was resistance to change, which seemed to be related to three factors: an administrative top–down approach, the complexity of patient care, and competing demands on clinical time. These factors have been similarly cited as barriers by Landis and Galvin (2014) and Liddle et al. (2018).
Facilitating change may be improved by highlighting the clinical benefit of the full range of program elements within STEADI, including the potential for fewer serious falls, and the impact on overall health that a serious fall can have. An outcome evaluation of the UHS STEADI-based fall prevention was conducted simultaneously with this process evaluation which showed that at-risk older adults who received a FPOC were 40% less likely to be hospitalized compared to at-risk older adults who did not receive one (Johnston et al., 2019). Health care providers may be persuaded by a short summary of the current clinical evidence as one element of implementing a change in clinical practice. Considering this intervention as a cultural change and ongoing commitment, rather than a short-term adjustment, may help improve perceptions about the value of fall risk prevention and help health care providers see CFRAs as a worthwhile demand on their time.
The process evaluation was conducted approximately 18 months after the last primary care site implemented the STEADI screening protocol. This time frame fell within the 6- to 24-month recommendation for assessing maintenance in the literature (Glasgow et al., 2019; Holtrop et al., 2021). Several considerations may be important for ongoing maintenance and sustainability. First, the use of quality indicators may be difficult to maintain. Across all stakeholder groups, creating an IT infrastructure for performance monitoring was cited as one of the most important factors contributing to success. Without surveillance, decreases in performance can easily go unrecognized. The maintenance phase, in particular, requires vigilance with sustained focus on identifying and addressing underlying performance issues. However, sustaining this capability represents a substantial commitment of resources.
Second, a potential facilitator was feedback across the program life cycle—including whether patients engaged in and perceived benefits from the community-based falls prevention programming. Providers who received positive feedback on these interventions reported being more motivated to recommend these programs to other patients in the future, while lack of feedback was reported as a barrier. It may be helpful for health care systems seeking to implement STEADI-based fall prevention initiatives to ensure that health care providers are aware of community-based falls prevention programming and to formalize a feedback mechanism for referrals. The linkage between utilization of fall-prevention programs and outcomes of care has been identified as a major barrier, and researchers have advocated for community partnerships with data sharing as essential for determining the long-term affect of fall risk screening and referral (Casey et al., 2017; Coe et al., 2017).
Third, health care providers reported challenges related to access in rural areas and appropriate transportation when referring their patients to community-based programs. Many health care systems working within rural and frontier communities may have the same challenges (Balis et al., 2018). Offering transportation services or vouchers for transportation to community-based fall prevention programs could minimize these barriers. Even when services are accessible, older adults may experience barriers related to their acceptability (Stevens, Sleet et al., 2017). It may be beneficial to work with local public infrastructure, including adult service programs (e.g., Councils on Aging) to address these issues.
Finally, programs face many challenges to sustainability, including overreliance on respected individuals to maintain ongoing operations and turnover in leadership (Dixon-Woods et al., 2012). Assuming that interventions will take hold without a need for ongoing support can threaten existing progress as well as long-term sustainability of the initiative (Dixon-Woods et al., 2012). Staff turnover was identified as a reason for observed declines in screening rates and one of the nurse leaders retired. In both cases, the organization responded quickly and effectively with additional training or by filling the leadership role with a nurse who was already familiar with STEADI. Given the aging health care workforce, succession planning will likely play a critical role in the sustainability of the STEADI initiative.
Utility of the RE-AIM Model for Fall Prevention Planning and Evaluation
The RE-AIM framework provided the structure for examining process elements that served as facilitators of the STEADI initiative as well as contextual factors that acted as barriers. There was considerable concordance between the quantitative data collected through surveys and the qualitative information obtained via intercept and key informant interviews across the three AIM dimensions. The triangulation of these findings lends credibility to the results.
The RE-AIM framework also supported a developmental approach for the evaluation of the STEADI initiative by examining the three AIM dimensions, which occur sequentially over time. Strategies employed during adoption affected implementation. For example, the decision to adopt the STEADI initiative was an administrative one that created resistance from health care providers during the implementation phase. On the other hand, the physician champion modified the screening protocol during the adoption phase to minimize workflow disruptions, which facilitated implementation. In the same way, strategies employed during adoption and implementation affected long-term maintenance. For example, the modifications to the EMR that provided reminder prompts for screening were effective across both the implementation and maintenance phases. During the implementation phase, surveillance of quality measures offered concrete evidence of performance, which permitted corrective actions to be taken in order to maintain high screening rates. This feedback within the system was effective at keeping screening rates high during the maintenance period.
This process evaluation was limited to the time period during which performance monitoring was active. Unfortunately, we were not able to determine the extent to which conducting CFRAs was established as a behavioral norm without this inducement, which would have provided stronger evidence for the long-term assimilation of the STEADI initiative. The RE-AIM framework could serve as a useful framework to assess sustainability (Lovarini et al., 2013).
Implications
The successful results obtained in our previous evaluation of reach and effectiveness underscore the importance of evaluating the process by which the observed reductions in fall-related hospitalizations were achieved. The results of this evaluation were shared at a provider meeting and the feedback proved useful to the organization with respect to securing greater commitment for the STEADI initiative from providers across the organization and potentially increasing its sustainability. The use of the RE-AIM framework supported ascertainment of strategies for success. The insights gained from this process evaluation can facilitate the adoption, implementation, and maintenance of STEADI-based fall prevention programs by other health care organizations. Our initial aim addressed an identified gap between research and practice by focusing on a system-wide implementation (Noonan et al., 2011) and by disseminating success strategies that can be used to inform future implementations of STEADI in primary care (Harden et al., 2018). Our hope is that sharing these findings will increase the likelihood that the population-level affect of clinical fall prevention can be realized in other locations.
Supplementary Material
Acknowledgments
The authors wish to thank Dr. Frank Floyd, Amy Roma, Bridget Talbut, Leah Miller, Amy Booth, Srikanth Poranki, and Chris Alderman of United Health Services Hospitals, Inc.
The data and analytic methods are not available to other researchers for replication purposes, however the materials (i.e., survey tools and interview guides) are available from the corresponding author upon request. The program evaluation reported in this manuscript was not preregistered.
Funding
This study was funded by Centers for Disease Control and Prevention Cooperative Agreement 3U17CE001997.
Footnotes
Conflict of Interest
None declared.
Disclaimer
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Supplementary Material
Supplementary data are available at The Gerontologist online.
References
- Baker DI, King MB, Fortinsky RH, Graff LG, Gottschalk M, Acampora D, Preston J, Broan CJ, & Tinetti ME (2005). Dissemination of an evidence-based multicomponent fall risk-assessment and -management strategy throughout a geographic area. Journal of the American Geriatrics Society, 53(4), 675–680. doi: 10.1111/j.1532-5415.2005.53218.x [DOI] [PubMed] [Google Scholar]
- Balis LE, Strayer TE, Ramalingam N, & Harden SM (2018). Beginning with the end in mind: Contextual considerations for scaling-out a community-based intervention. Frontiers in Public Health, 6, 357. doi: 10.3389/fpubh.2018.00357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey CM, Parker EM, Winkler G, Liu X, Lamvert GH, & Eckstrom E (2017). Lessons learned from implementing CDC’s STEADI falls prevention algorithm in primary care. The Gerontologist, 57(4), 787–796. doi: 10.1093/geront/gnw074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. (2022). Web-based Injury Statistics Query and Reporting System (WISQARS): 2020 fatal and non-fatal injury statistics with fall as mechanism of injury [online]. https://www.cdc.gov/injury/wisqars
- Chou WC, Tinetti ME, King MB, Irwin K, & Fortinsky RH (2006). Perceptions of physicians on the barriers and facilitators to integrating fall risk evaluation and management into practice. Journal of General Internal Medicine, 21(2), 117–122. doi: 10.1111/j.1525-1497.2005.00298.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coe LJ, St. John JA, Hariprasad S, Shankar KN, MacCulloch PA, Bettano AL, & Zotter J (2017). An integrated approach to falls prevention: A model for linking clinical and community interventions through the Massachusetts Prevention and Wellness Trust Fund. Frontiers in Public Health, 5, 38. doi: 10.3389/fpubh.2017.00038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon-Woods M, McNicol S, & Martin G (2012). Ten challenges in improving quality in healthcare: Lessons from the Health Foundation’s programme evaluations and relevant literature. BMJ Quality and Safety, 21(10), 876–884. doi: 10.1136/bmjqs-2011-000760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckstrom E, Parker EM, Lambert GH, Winkler G, Dowler D, & Casey CM (2017). Implementing STEADI in academic primary care to address older adult fall risk. Innovation in Aging, 1(2), 1–9. doi: 10.1093/geroni/igx028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Harden SM, Gaglio B, Rabin B, Smith ML, Porter GC, & Estabrooks PA (2019). RE-AIM planning and evaluation framework: Adapting to new science and practice with a 20-year review. Frontiers in Public Health, 7(64), 1–9. doi: 10.3389/fpubh.2019.00064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Klesges LM, Dzewaltowski DA, Bull SS, & Estabrooks P (2004). The future of health behavior change research: What is needed to improve translation of research into health promotion practice? Annals of Behavioral Medicine, 27(1), 3–12. doi: 10.1207/s15324796abm2701_2 [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Vogt TM, & Boles SM (1999). Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health, 89(9), 1322–1327. doi: 10.2105/AJPH.89.9.1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harden SM, Smith ML, Ory MG, Smith-Ray RL, Estabrooks PA, & Glasgow RE (2018). RE-AIM in clinical, community, and corporate settings: Perspectives, strategies, and recommendations to enhance public health impact. Frontiers in Public Health, 6, 71. doi: 10.3389/fpubh.2018.00071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtrop JS, Estabrooks PA, Gaglio B, Harden SM, Kessler RS, King DK, Kwan BM, Ory MG, Rabin BA, Shelton RC, & Glasgow RE (2021). Understanding and applying the RE-AIM framework: Clarifications and resources. Journal of Clinical and Translational Science, 5(1), e126. doi: 10.1017/cts.2021.789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston YA, Bergen G, Bauer M, Parker EM, Wentworth L, McFadden M, & Garnett M (2019). Implementation of the Stopping Elderly Accidents, Deaths, and Injuries initiative in primary care: An outcome evaluation. The Gerontologist, 59(6), 1182–1191. doi: 10.1093/geront/gny101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones TS, Ghosh TS, Horn K, Smith J, & Vogt RL (2011). Primary care physicians perceptions and practices regarding fall prevention in adults 65 years and over. Accident Analysis and Prevention, 43, 1605–1609. doi: 10.1016/j.aap.2011.03.013 [DOI] [PubMed] [Google Scholar]
- Kessler RS, Purcell EP, Glasgow RE, Klesges LM, Benkeser RM, & Peek C (2013). What does it mean to “employ” the RE-AIM model? Evaluation and the Health Professions, 36(1), 44–66. doi: 10.1177/0163278712446066 [DOI] [PubMed] [Google Scholar]
- Klesges LM, Estabrooks PA, Dzewaltowski DA, Bull SS, & Glasgow RE (2005). Beginning with the application in mind: Designing and planning health behavior change interventions to enhance dissemination. Annals of Behavioral Medicine, 29(2), 66–75. doi: 10.1207/s15324796abm2902s_10 [DOI] [PubMed] [Google Scholar]
- Landis SE, & Galvin SL (2014). Implementation and assessment of a fall screening program in primary care practices. Journal of the American Geriatrics Society, 62(12), 2408–2414. doi: 10.1111/jgs.13137 [DOI] [PubMed] [Google Scholar]
- Liddle J, Lovarini M, Clemson L, Mackenzie L, Tan A, Pit SW, Poulos R, Tiedemann A, Sherrington C, Roberts C, & Willis K (2018). Making fall prevention routine in primary care practice: Perspectives of allied health professionals. BMC Health Services Research, 18(1), 1–9. doi: 10.1186/s12913-018-3414-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovarini M, Clemson L, & Dean C (2013). Sustainability of community-based fall prevention programs: A systematic review. Journal of Safety Research, 47(2013), 9–17. doi: 10.1016/j.jsr.2013.08.004 [DOI] [PubMed] [Google Scholar]
- Moreland B, Kakara R, & Henry A (2020). Trends in nonfatal falls and fall-related injuries among adults aged ≥65 years—United States, 2012–2018. Morbidity and Mortality Weekly Report, 69(27), 875–881. doi: 10.15585/mmwr.mm6927a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noonan RK, Sleet DA, & Stevens JA (2011). Closing the gap: A research agenda to accelerate the adoption and effective use of proven older adult fall prevention strategies. Journal of Safety Research, 42(6), 427–430. doi: 10.1016/j.jsr.2010.12.002 [DOI] [PubMed] [Google Scholar]
- Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. (2011). Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. Journal of the American Geriatrics Society, 59(1), 148–157. doi: 10.1111/j.1532-5415.2010.03234.x [DOI] [PubMed] [Google Scholar]
- Phelan EA, Mahoney JE, Voit JC, & Stevens JA (2015). Assessment and management of fall risk in primary care settings. Medical Clinics of North America, 99(2), 281–293. doi: 10.1016/j.mcna.2014.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan EA, & Ritchey K (2018). Fall prevention in community-dwelling older adults. Annals of Internal Medicine, 169(11), ITC81–ITC96. doi: 10.7326/AITC201812040 [DOI] [PubMed] [Google Scholar]
- Sarmiento K, & Lee R (2017). STEADI: CDC’s approach to make older adult fall prevention part of every primary care practice. Journal of Safety Research, 63, 105–109. doi: 10.1016/j.jsr.2017.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ML, Stevens JA, Ehrenreich H, Wilson AD, Schuster RJ, Cherry CO, & Ory MG (2015). Healthcare providers’ perceptions and self-reported fall prevention practices: Findings from a large New York health system. Frontiers in Public Health, 3(17), 1–5. doi: 10.3389/fpubh.2015.00017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens JA, Ballesteros MF, Mack KA, Rudd RA, DeCaro E, & Adler G (2012). Gender differences in seeking care for falls in the aged Medicare population. American Journal of Preventive Medicine, 43(1), 59–62. doi: 10.1016/j.amepre.2012.03.008 [DOI] [PubMed] [Google Scholar]
- Stevens JA, & Phelan EA (2013). Development of STEADI: A fall prevention resource for health care providers. Health Promotion Practice, 14(5), 706–714. doi: 10.1177/1524839912463576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens JA, Sleet DA, & Rubenstein LZ (2017). The influence of older adults’ beliefs and attitudes on adopting fall prevention behaviors. American Journal of Lifestyle Medicine, 12(4), 324–330. doi: 10.1177/1559827616687263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens JA, Smith ML, Parker EM, Jiang L, & Floyd FD (2017). Implementing a clinically based fall prevention program. American Journal of Lifestyle Medicine, 14(1), 71–77. doi: 10.1177/1559827617716085 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


