Abstract
Background
Plasmodium falciparum infection in pregnant women in sub-Saharan Africa is often asymptomatic. As these forms of malaria are often submicroscopic and difficult to diagnose by conventional methods (microscopy and/or rapid diagnostic test), diagnosis requires the use of molecular techniques such as polymerase chain reaction (PCR). This study analyses the prevalence of subclinical malaria and its association with adverse maternal and neonatal outcomes, a topic that has been scarcely evaluated in the literature.
Methods
A cross-sectional study was conducted using semi-nested multiplex PCR to assess the presence of P. falciparum in placental and peripheral blood of 232 parturient pregnant women at the Hospital Provincial de Tete, Mozambique between March 2017 and May 2019. Multivariate regressions were performed to assess the associations of maternal subclinical malaria with several maternal and neonatal outcomes after controlling for the presence of preeclampsia/eclampsia (PE/E) and HIV infection, as well as for other maternal and pregnancy characteristics.
Results
In total, 17.2% (n = 40) of the women studied had positive PCR for P. falciparum (7 in placental blood only, 3 in peripheral blood only). We found a significant association between subclinical malaria and a higher peripartum mortality risk, which persisted after controlling for maternal comorbidity and maternal and pregnancy characteristics (adjusted odds ratio: 3.50 [1.11–10.97]). In addition, PE/E and HIV infections were also significantly associated with several adverse maternal and neonatal outcomes.
Conclusion
This study demonstrated the association of subclinical malaria, as well as of PE/E and HIV, in pregnant women with adverse maternal and neonatal outcomes. Therefore, molecular methods may be sensitive tools to identify asymptomatic infections that can reduce the impact on peripartum mortality and their contribution to sustained transmission of the parasite in endemic countries.
Keywords: Subclinical malaria, Pregnancy, Preeclampsia/eclampsia, HIV, Mozambique
Background
According to the latest World Health Organization report on malaria [1], the incidence of malaria was estimated at 241 million cases worldwide in 2020, approximately 95% of which were in Africa. Indeed, six African countries accounted for 55% of all cases worldwide, with Mozambique ranked fourth after Nigeria, the Democratic Republic of Congo and Uganda.
Approximately 12 million pregnant women in 33 African countries have been exposed to Plasmodium spp. infection during pregnancy [1]. In this population, malaria has some special features. A significant percentage of pregnant women with malaria often remain asymptomatic and may act as reservoirs of Plasmodium, especially Plasmodium falciparum, favouring transmission to the rest of the population. At the same time, these infections are often submicroscopic and have low parasite loads, making them difficult to diagnose by conventional tests (microscopy and/or rapid diagnostic test). Hence, molecular diagnosis by polymerase chain reaction (PCR) is of particular importance for the diagnosis of subclinical infection [2–5].
In sub-Saharan Africa, the main causes of maternal and neonatal morbidity and mortality, are malaria, preeclampsia/eclampsia (PE/E) and HIV infection [6–8]. There are multiple interactions between these three diseases, well described by other authors [9, 10]. However, there is little information on the relationship between subclinical malaria in pregnant women [11–13]. In addition, the potential consequences of subclinical malaria on maternal and neonatal outcomes have not been extensively studied to date.
The two main objectives of this study therefore were to determine the prevalence of asymptomatic P. falciparum infection in pregnant women and the associations of asymptomatic P. falciparum with adverse maternal and neonatal outcomes. A secondary objective includes the assessment of the associations of PE/E and HIV infection with maternal and neonatal outcomes.
Methods
Study site
The study was conducted in the Maternity Services Unit of Tete Provincial Hospital (HPT). The province of Tete, with an area of 100,724 km2, is located in central Mozambique and is bound by Zambia to the north and Zimbabwe to the west (Fig. 1). The average temperature ranges between 23.4º and 32.9º. It is the third most populated province in the country and has a population of 2,829,594 inhabitants, 1,442,880 (50,1%) of whom are women [14].
Fig. 1.
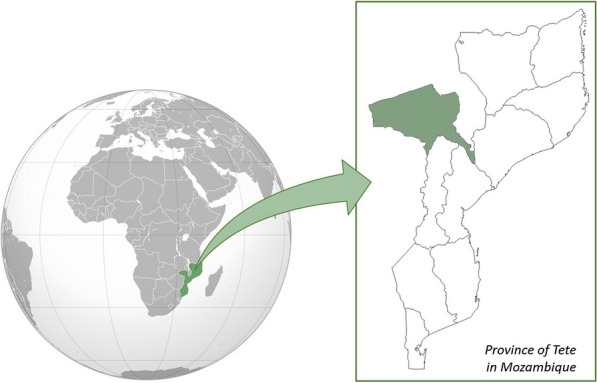
Political map of Tete (Mozambique)
Study population and procedures
Between 1 March 2017 and 30 May 2019, 232 women were recruited during delivery. For the selection, the criterion was only to recruit women when the researchers were present at the delivery. Women who refused to participate in the study or when the data could not be completed in the questionnaire were excluded. A cross-sectional study was carried out involving completion of a structured questionnaire that included demographic data and information about the current pregnancy, delivery, and the newborn. Each interview lasted between 10 and 15 min. The data collection instruments were the pregnancy cards of the National Health Service of the Republic of Mozambique and the clinical delivery records.
The Sysmex® autoanalyzer and Cellpack® reagents were used to provide hemoglobin values. Due to the cost of the study, haematometry was only performed when indicated by the obstetrician. HIV serostatus was assessed using a rapid test (Determine, Abbot Laboratories, USA) and positive results were confirmed using the Uni-gold rapid test (TM HIV, Trinity Biotech, Ireland). The Multistix® 10 SG reagent strip was used to measure protein in urine.
In parallel to data collection, samples of peripheral blood and placenta were collected at delivery for the detection of P. falciparum by multiplex PCR. Within 30 min of delivery, attending staff collected placental blood via the incision method and prepared filter paper samples [15]. In brief, staff made a shallow incision into the maternal side of the placenta using sterile scissors and collected the accumulated blood in the intervillous space with the help of a syringe. Peripheral blood was also collected by venipuncture and stored on filter papers. Filter paper samples were collected on FTA™ Classic Card (GE Healthcare UK Limited, UK) and stored in individual sterile plastic envelopes with desiccant.
DNA extraction and multiplex PCR development
Parasite DNA was isolated from the blood samples on filter paper with Chelex, as previously described [16], and samples were tested in duplicate by species-specific nested PCR for P. falciparum [17]. Amplifications were performed in 25 µl reactions containing 1 µl of template DNA, 0.4 µg of each primer, 2.5 U of Taq DNA polymerase (Promega, Madison, Wis.), and each deoxynucleotide triphosphate at a concentration of 0.2 mM. All amplifications were performed in a conventional thermocycler (Applied Biosystems™), the template DNA was denatured at 94 ºC for 7 min, followed by 40 cycles of amplification (melt at 94ºC for 20 s, anneal/extend at 62 ºC for 20 s, and 72 ºC for 30 s) and final extension at 72 ºC for 10 min. For the second round of amplification, 1 µl of the PCR product from the initial amplification was used as the template in 25 µl final volume. Amplified DNA was run on 2.5% agarose gels containing ethidium bromide and analyzed under UV light. A positive PCR of placental blood was defined as the presence of a species-specific band of amplified DNA.
Definitions
Subclinical malaria: characterized by low levels of parasitemia and absence of symptoms. The adolescent population includes individuals in the 10–19 years group.
The following variables were analysed:
Maternal and pregnancy characteristics: age (in years and = 1 if women were under 20-year-old), weight (in kilograms); pregnancy number (primigravida versus multigravida); pregnancy type (single versus multiple); malaria prophylactic treatment [defined as intermittent preventive treatment with sulfadoxine-pyrimethamine (IPTp)]; and pregnancy follow-up [assessed on the basis of completion of at least four or more antenatal care visits (ANC)].
Maternal comorbidity: the presence of hypertensive disorders induced by pregnancy (preeclampsia and eclampsia) and HIV infection. For the diagnosis of preeclampsia, current criteria were used [18, 19], which included (a) the presence of arterial hypertension (systolic blood pressure (SBP) ≥ 140 mm Hg and/or diastolic blood pressure (DBP) ≥ 90 mm Hg, determined on two occasions at least 4 h apart; (b) onset after the 20th week of pregnancy and (c) associated with proteinuria > 300 mg/24 h and/or adverse conditions that increase the risk of severe complications and/or severe complications that warrant delivery. The diagnosis of eclampsia was made if seizures appeared in patients with preeclampsia criteria.
Maternal and neonatal outcomes (dependent variables in multivariate models): delivery type (vaginal versus caesarean); the haemoglobin level (g/dL); gestational age at delivery (defined as preterm when occurring before week 37), newborn weight (in kilograms) and as low birth weight (LBW) = 1 if weight was less than 2500 g at birth; Apgar score < 7 at 1 and 5 min after birth [17]; neonatal resuscitation (defined as cardiopulmonary resuscitation maneuvers); and stillbirth (defined as fetal death occurring after 28 complete weeks of gestation).
Statistical analysis
Categorical variables are summarized as absolute numbers and percentages, and continuous variables as means and 95% confidence intervals. In univariate analyses, categorical data were analysed for associations with subclinical P. falciparum infection using the Chi-square test, while means of continuous variables were compared using Student's t-tests. Multivariate analyses were performed to assess associations between subclinical P. falciparum infection and each maternal and neonatal outcome, after controlling for maternal comorbidity (presence of E, PE and HIV) and maternal and pregnancy characteristics available for most women (i.e., mother’s age, pregnancy number and pregnancy type). Logistic regressions were performed for binary outcomes (i.e., cesarean delivery, pre-term birth, LBW, Apgar < 7 at 1 and 5 min, neonatal resuscitation, and still birth) and linear regressions for continuous outcomes (i.e., hemoglobin level and neonatal weight). For each model, odds ratios and 95% confidence intervals are presented. Statistical significance was set at p-value < 0.05. Data were analysed with Stata version 15 (StataCorp®).
Results
A total of 232 pregnant women between 14 and 43 years of age were evaluated, with a mean age of 23 years (interquartile range 18–28). Among them, 137 (59.3%) had attended at least 4 antenatal care visits.
Subclinical P. falciparum infection was detected in 40 women (17.2%) (7 exclusively in placental blood, 3 only in peripheral blood and 30 in both). Among the infected cases, 30 (79%) stated that they received IPTp at least 3 doses against Plasmodium sp. (Table 1).
Table 1.
Distribution of maternal and pregnancy characteristics, maternal comorbidity and maternal and neonatal outcomes according to the presence of subclinical P. falciparum infection
| No Pf n = 192 |
Yes Pf n = 40 |
Total 232 |
p-value | |
|---|---|---|---|---|
| Maternal and pregnancy characteristics | ||||
|
Age (years) N = 231 |
23.6 [22.7–24.6] |
21.8 [19.7–23.9] |
23.31 [22.5–24.2] |
0.109 |
|
Adolescent (< 20 year-old) N = 231 |
65/191 (34.03%) |
21/40 (52.5%) |
86/231 (37.23%) |
0.028 |
|
Weight (Kg) N = 134 |
67.05 [64.7–69.4] |
68.66 [58.3–79.0] |
67.25 [64.9–69.6] |
0.661 |
|
ANC ≥ 4 N = 231 |
116/191 (60.7%) |
21/40 (52.5%) |
137/231 (59.3%) |
0.335 |
|
Number of pregnancies N = 232 |
0.087 | |||
| Primigravida |
82/192 (42.7%) |
23/40 (57.5%) |
105/232 (45.3%) |
|
| Multigravida | 110/192 (57.3%) |
17/40 (42.5%) |
127/232 (54.7%) | |
|
Type of pregnancy N = 232 |
0.855 | |||
| Single |
181/192 (94.2%) |
38/40 (95.0%) |
219/232 (94.4%) |
|
| Multiple |
11/192 (5.7%) |
2/40 (5.0%) |
13/232 (5.6%) |
|
|
Profilaxis (IPTp) ≥ 3 N = 203 |
136/165 (82.4%) |
30/38 (79.0%) |
166/203 (81.8%) |
0.617 |
| Maternal comorbidity | ||||
|
PE N = 232 |
84/192 (43.8%) |
10/40 (25.0%) |
94/232 (40.5%) |
0.028 |
|
E N = 232 |
29/192 (15.1%) |
7/40 (17.5%) |
36/232 (15.5%) |
0.703 |
|
PE/E N = 232 |
113/192 (58.9%) |
17/40 (42.5%) |
130/232 (56.0%) |
0.058 |
|
HIV-positive N = 228 |
33/188 (17.5%) |
3/40 (7.5%) |
36/228 (15.5%) |
0.113 |
| Maternal and neonatal outcomes | ||||
|
Cesarean-section N = 224 |
55/187 (29.4%) |
13/37 (35.1%) |
68/224 (30.4%) |
0.489 |
|
Hemoglobin (g/dL) N = 167 |
10.9 [10.7–11.2] |
11.4 [10.7–12.0] |
11.0 [10.8–11.3] |
0.229 |
|
Pre-term birth N = 228 |
24/188 (12.8%) |
7/40 (17.5%) |
31/228 (13.6%) |
0.428 |
|
Neonatal weight, (g) N = 226 |
2800.5 [2710–2891] |
2679.5 [2480–2879] |
2779.6 [2698–2862] |
0.272 |
|
LBW N = 226 |
44/187 (23.5%) |
10/39 (25.6%) |
54/226 (23.9%) |
0.778 |
|
Apgar < 7 (1 m) N = 232 |
47/192 (24.5%) |
10/40 (25.0%) |
57/232 (24.6%) |
0.945 |
|
Apgar < 7 (5 m) N = 232 |
25/192 (13.5%) |
6/40 (15.0%) |
31/232 (13.4%) |
0.738 |
|
Neonatal resuscitation N = 223 |
34/185 (18.4%) |
8/38 (21.1%) |
42/223 (18.8%) |
0.701 |
|
Stillbirth N = 227 |
14/187 (7.5%) |
7/40 (17.5%) |
21/227 (9.3%) |
0.047 |
The data have been expressed as means [95% CI] for continuous data and absolute numbers (%) for categorical data
Pf: Plasmodium falciparum; Kg: kilograms, ANC: antenatal care visits, IPTp: Intermitent Preventive Treatment of malaria for pregnant women, mmHg: milimetres of mercury, PE: preeclampsia, E: eclampsia, PE/E: preeclampsia/eclampsia, HIV: Human Immunodeficiency Virus, Pre-term birth: pre-term delivery (< 37 weeks), LBW: low birth weight, g: gram. dl: decilitre, m: minute
Of the total number of pregnant women, 94 (40.5%) had preeclampsia and 36 (15.5%) had eclampsia. 36 (15.5%) of the pregnant women were infected with HIV. Univariate analyses show a negative and significant association of subclinical P. falciparum infection and being under 20-year-old and with the presence of eclampsia, and a positive and significant association of subclinical P. falciparum infection with peripartum neonatal death.
Table 2 shows the results of the multivariate analyses of each maternal and neonatal outcome. Each of these models include as covariates: the presence of subclinical P. falciparum infection, the presence of PE, E and HIV infection, and maternal and pregnancy characteristics (i.e., mother’s age, pregnancy type and pregnancy number). Odd ratios/coefficients of subclinical P. falciparum infection, PE, E and HIV infection are reported in Table 2. Subclinical P. falciparum infection was significantly associated with peripartum neonatal mortality, even after controlling for maternal comorbidity and maternal and pregnancy characteristics. In addition, eclampsia was significantly associated with all adverse maternal and neonatal outcomes analysed in this study (with the only exception of haemoglobin level), while preeclampsia was significantly associated with having a cesarean delivery and requiring neonatal resuscitation. HIV infection was significantly associated with low neonatal weight, having Apgar < 7 at 5 min and with peripartum neonatal mortality.
Table 2.
Multivariate models of maternal and neonatal outcomes on the presence of subclinical P. falciparum infection, PE,E and HIV infections
| Logistic models * | ||
|---|---|---|
| Odd Ratio | 95% CI | |
| Cesarean delivery (N = 219) | ||
| Subclinical Malaria | 1.69 | [0.71; 4.01] |
| PE | 3.69 | [1.69; 8.03] |
| E | 15.38 | [5.66; 41.83] |
| HIV | 1.63 | [0.63; 4.21] |
| Pre-term birth (N = 223) | ||
| Subclinical Malaria | 1.38 | [0.50; 3.80] |
| PE | 2.17 | [0.78; 5.97] |
| E | 5.64 | [1.87; 17.01] |
| HIV | 1.25 | [0.36; 4.26] |
| Low birth weight (N = 221) | ||
| Subclinical Malaria | 1.41 | [0.56; 3.59] |
| PE | 2.08 | [0.91; 4.74] |
| E | 3.13 | [1.16; 8.46] |
| HIV | 3.14 | [1.19; 8.29] |
| Apgar < 7 1 m (N = 227) | ||
| Subclinical Malaria | 1.26 | [0.53; 3.00] |
| PE | 2.01 | [0.95; 4.24] |
| E | 4.59 | [1.79; 11.79] |
| HIV | 1.68 | [0.69; 4.06] |
| Apgar < 7 5 m (N = 227) | ||
| Subclinical Malaria | 1.53 | [0.51; 4.59] |
| PE | 2.08 | [0.74; 5.85] |
| E | 4.96 | [1.55; 15.85] |
| HIV | 4.36 | [1.51; 12.57] |
| Neonatal resuscitation (N = 218) N = 223 | ||
| Subclinical Malaria | 1.51 | [0.60; 3.79] |
| PE | 3.04 | [2.19; 7.16] |
| E | 4.68 | [1.64; 13.4] |
| HIV | 1.31 | [0.48; 3.58] |
| Stillbirth (N = 222) | ||
| Subclinical Malaria | 3.50 | [1.11; 10.97] |
| PE | 1.59 | [0.46; 5.56] |
| E | 4.80 | [1.30; 17.69] |
| HIV | 3.82 | [1.05; 13.88] |
| OLS models* | ||
| Coefficient | 95% CI | |
| Haemoglobin (N = 167) | ||
| Subclinical Malaria | 0.40 | [− 0.38; 1.17] |
| PE | 0.13 | [− 0.52; 0.77] |
| E | 0.87 | [− 0.002; 1.74] |
| HIV | − 0.13 | [− 0.95; 0.68] |
| Neonatal weight (N = 221) | ||
| Subclinical Malaria | − 147.70 | [− 343.46; 48.06] |
| PE | − 141.26 | [− 305.31; 22.80] |
| E | − 354.94 | [− 581.43; − 128.44] |
| HIV | − 255.94 | [− 465.18; − 46.69] |
* Each model includes additional covariates for adolescence, primigravity and multiple pregnancy
PE: preeclampsia, E: eclampsia, HIV: Human Immunodeficiency Virus, OLS: Ordinary Least Squared
Discussion
Pregnant women in sub-Saharan Africa suffer subclinical P. falciparum infections more frequently than symptomatic infections [4]. These infections can cause placental infection [2, 21] and adverse health effects in mothers and newborns [3, 4].
Conventional diagnostic methods [light microscopy and rapid diagnostic test (RDT)] have limited sensitivity for the diagnosis of subclinical infections. Low-density infections are more likely to be missed [22]. In the last decade, the use of PCR-based molecular methods for the diagnosis of these infections has emerged, especially in pregnant women [3, 4]. After performing semi-nested PCR, the prevalence of subclinical P. falciparum infection in this study was 17.2%. These figures are similar to those of other studies conducted in Africa (Benin: 20.5%, Ethiopia 18.1% and the Democratic Republic of Congo 19%) [2, 4, 23].
A high incidence of subclinical malaria was observed despite the fact that 79% of women with malaria reported taking preventive treatment of malaria for pregnant women (IPTp). There could be several reasons for this. First, since IPTp with sulfadoxine-pyrimethamine is contraindicated in the first trimester due to its possible teratogenic effects, the pregnant women in this study may not have been protected during this period [5]. Second, a high prevalence of P. falciparum resistance to sulfadoxine-pyrimethamine has been reported in most malaria-endemic areas [24, 25]. Finally, it is likely that women with HIV infection took less IPTp because they were on prophylactic treatment with trimethoprim-sulfamethoxazole against Pneumocystis jirovecii and IPTp is contraindicated because of the potential additional risk of adverse effects associated with taking two antifolate drugs simultaneously [26, 27].
In general, most studies suggest that, in malaria-endemic regions, women exposed to placental parasites may be at higher risk of preeclampsia compared to those in malaria-free regions [9, 28–31]. In this study, however a negative association was observed. This could be explained by the inclusion of women with subclinical infections and low parasite loads at the end of their pregnancies (end of the 3rd trimester), as it is the first and second trimester that is associated with increased risk of placental malaria and maternal morbidity [4, 21].
A significant and positive association between peripartum newborn mortality was observed in mothers with subclinical malarial infection. This finding persisted even after controlling for maternal comorbidity and other maternal and pregnancy characteristics. This association is novel and has a high impact, highlighting the importance of diagnosing subclinical P. falciparum infection in antenatal care. In a study in Ghana, they detected a great number of anaemia-associated malaria infections were observed under microscope to have less than 1000 parasite count per microlitre of blood [32]. Therefore, asymptomatic malaria could be detected with a malaria and anemia screening intervention during early antenatal care visits [33], improving the chances of missing asymptomatic malaria at antenatal care visits as a possibility in cases where molecular methods cannot be used.
In addition, eclampsia was significantly associated with most adverse maternal and neonatal outcomes analysed in this study. Preeclampsia was significantly associated with having a cesarean delivery and requiring neonatal resuscitation, while HIV infection was significantly associated with low neonatal weight, having Apgar < 7 at 5 min and peripartum neonatal mortality. The effects of these diseases in the newborn have been widely described by other authors [34–37].
Among the limitations of the study, the pregnant women were evaluated only at the time of delivery, with no opportunity to assess the impact of subclinical parasitemia during the first and second trimesters, nor to follow up on both maternal and neonatal complications in the post-partum period. In addition, the multivariate models used were conducted to assess the relationship between subclinical P. falciparum infection with maternal and neonatal outcomes after controlling for maternal comorbidities and characteristics. However, given the nature and the size of the sample used, it is difficult to establish causal relationships and assess potential interactions between comorbidities. Further research should focus on studying pregnant women from the first trimester and performing postpartum follow-up and continue with future studies to demonstrate the effect of subclinical parasitemia on maternal and neonatal outcomes.
Conclusion
In conclusion, this study demonstrated the significant association between subclinical malaria in pregnant women and peripartum neonatal mortality. In order to reduce the impact on newborn mortality and its role in maintaining parasite transmission in endemic area countries, it could be necessary to apply molecular methods able to detect extremely low parasite densities.
Acknowledgements
This study has had the support of the Medical Training Cooperation Project of the Faculty of Health Sciences of the University of Zambeze (Tete, Mozambique) directed by Dr. Luis Lopez Rivero and the University Center for International Development Cooperation (CUCID) of the University of Las Palmas de Gran Canaria (ULPGC). We would like to thank Ms. Janet Dawson for her help in reviewing the English version of the manuscript.
Abbreviations
- PCR
Polymerase chain reaction
- PE/E
Preeclampsia/eclampsia
- HIV
Human Immunodeficiency Virus
- HPT
Provincial Hospital of Tete
- DNA
Deoxyribonucleic acid
- UV
Ultraviolet
- SFH
Symphysis fundal height
- ANC
Antenatal care visits
- SBP
Systolic Blood Pressure
- DBP
Diastolic Blood Pressure
- LBW
Low birth weight
- SD
Standard deviation
- RDT
Rapid diagnostic test
- IPTp
Intermittent preventive treatment of malaria for pregnant women
- WHO
World Health Organization
- CUCID
Centro Universitario de Cooperación Internacional al Desarrollo
- ULPGC
Universidad de Las Palmas de Gran Canaria
Author contributions
NJS, GGA, LVT, CCR, PGS, JLPA: conceptualization, methodology, software; NJS, GGA, LVT, NM, CCR: data curation, writing—original draft preparation; NJS, GGA, CCR, JLPA: visualization, investigation; GGA, CCR, JLPA: supervision. NJS, CCR, LVT: software, validation; NJS, GGA, CCR, JLPA: writing—reviewing and editing. All authors read and approved the final manuscript.
Funding
This research has not received any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Study protocols and informed consent forms for trials were reviewed and approved by the National Ethics Review Committee in Mozambique 432/CNBS/16 and the number of the CEIm of the CHUIMI (Spain) is CEIm-CHUIMI-2016/848. The study was conducted in accordance with the provisions of the Declaration of Helsinki and the Good Clinical Practice guidelines established by the WHO and the International Conference on Harmonization. Participation in the study was completely voluntary. All study participants were informed of the purpose of the study and written informed consent was obtained from each study participant. The consent form was signed by the parent/guardian if the participant was under 18 years of age. Illiterate women had the consent form and patient information sheet read and explained to them, and those who verbally agreed to participate in the study signed the consent form with their finger.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO . World malaria report 2021. Geneva: World Health Organization; 2021. [Google Scholar]
- 2.Tilahun A, Yimer M, Gelaye W, Tegegne B. Prevalence of asymptomatic Plasmodium species infection and associated factors among pregnant women attending antenatal care at Fendeka town health facilities, Jawi District, North West Ethiopia: a cross-sectional study. PLoS ONE. 2020;154:e0231477. doi: 10.1371/journal.pone.0231477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cottrell G, Moussiliou A, Luty AJ, Cot M, Fievet N, Massougbodji A, et al. Submicroscopic Plasmodium falciparum infections are associated with maternal anemia, premature births, and low birth weight. Clin Infect Dis. 2015;60:1481–1488. doi: 10.1093/cid/civ122. [DOI] [PubMed] [Google Scholar]
- 4.Hounkonnou CPA, Briand V, Fievet N, Accrombessi M, Yovo E, Mama A, et al. Dynamics of submicroscopic Plasmodium falciparum infections throughout pregnancy: a preconception cohort study in Benin. Clin Infect Dis. 2020;71:166–174. doi: 10.1093/cid/ciz748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alkan ML. The importance of submicroscopic diagnosis of malaria. Clin Infect Dis. 2020;71:175–176. doi: 10.1093/cid/ciz752. [DOI] [PubMed] [Google Scholar]
- 6.Boene H, Vidler M, Augusto O, Sidat M, Macete E, Menéndez C, et al. CLIP feasibility working group. Community health worker knowledge and management of pre-eclampsia in southern Mozambique. Reprod Health. 2016;13(Suppl 2):105. doi: 10.1186/s12978-016-0220-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sacoor C, Payne B, Augusto O, Vilanculo F, Nhacolo A, Vidler M, et al. CLIP feasibility working group Health and socio-demographic profile of women of reproductive age in rural communities of southern Mozambique. PLoS ONE. 2018;13:e0184249. doi: 10.1371/journal.pone.0184249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Menéndez C, Romagosa C, Ismail MR, Carrilho C, Saute F, Osman N, et al. An autopsy study of maternal mortality in Mozambique: the contribution of Infectious Diseases. PLoS Med. 2008;5:e44. doi: 10.1371/journal.pmed.0050044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Obiri D, Erskine IJ, Oduro D, Kusi KA, Amponsah J, Gyan BA, et al. Histopathological lesions and exposure to Plasmodium falciparum infections in the placenta increases the risk of preeclampsia among pregnant women. Sci Rep. 2020;10:8280. doi: 10.1038/s41598-020-64736-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boyajian T, Shah PS, Murphy KE. Risk of preeclampsia in HIV-positive pregnant women receiving HAART: a matched cohort study. J Obstet Gynaecol Can. 2012;34:136–141. doi: 10.1016/S1701-2163(16)35156-8. [DOI] [PubMed] [Google Scholar]
- 11.Mahamar A, Andemel N, Swihart B, Sidibe Y, Gaoussou S, Barry A, et al. Malaria infection is common and associated with perinatal mortality and preterm delivery despite widespread use of chemoprevention in Mali: an observational study 2010 to 2014. Clin Infect Dis. 2021;73:1355–1361. doi: 10.1093/cid/ciab301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ategeka J, Kakuru A, Kajubi R, Wasswa R, Ochokoru H, Arinaitwe E, et al. Relationships between measures of malaria at delivery and adverse birth outcomes in a high-transmission area of Uganda. J Infect Dis. 2020;222:863–870. doi: 10.1093/infdis/jiaa156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gaoussou S, Attaher O, Swihart B, Traore M, Diarra S, Soumbounou IH, et al. Pregnancy outcomes in a malaria-exposed Malian cohort of women of child-bearing age. Front Med (Lausanne) 2022;9:1061538. doi: 10.3389/fmed.2022.1061538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.INE: Instituto Nacional de Estadística. Maputo, Mozambique: INE. 2018. Anuário Estatístico da Província de Tete, 2018. http://www.ine.gov.mz/estatisticas/publicacoes/anuario/provincia-de-tete/anuario-tete-2018.pdf/view. Accessed 11 Dec 2020.
- 15.Othoro C, Moore JM, Wannemuehler K, Nahlen BL, Otieno J, Slutsker L, et al. Evaluation of various methods of maternal placental blood collection for immunology studies. Clin Vaccine Immunol. 2006;13:568–574. doi: 10.1128/CVI.13.5.568-574.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Plowe CV, Djimde A, Bouare M, Doumbo O, Wellems TE. Pyrimethamine and proguanil resistance-conferring mutations in Plasmodium falciparum dihydrofolate reductase: polymerase chain reaction methods for surveillance in Africa. Am J Trop Med Hyg. 1995;52:565–568. doi: 10.4269/ajtmh.1995.52.565. [DOI] [PubMed] [Google Scholar]
- 17.Muucsf. Protocol for Plasmodium species determination by PCR. 2022. [http://www.muucsf.org/protocols/protocols_genotyping.html]. Accessed 13 Dec 2022.
- 18.von Dadelszen P, Magee LA. Pre-eclampsia: an update. Curr Hypertens Rep. 2014;16:454. doi: 10.1007/s11906-014-0454-8. [DOI] [PubMed] [Google Scholar]
- 19.Mol BWJ, Roberts CT, Thangaratinam S, Magee LA, de Groot CJM, Hofmeyr GJ. Pre-eclampsia. Lancet. 2016;387:999–1011. doi: 10.1016/S0140-6736(15)00070-7. [DOI] [PubMed] [Google Scholar]
- 20.Academy A, of Pediatrics Committee on Fetus and Newborn. American college of obstetricians and gynecologists committee on obstetric practice. Apgar Score Pediatrics. 2015;136:819–822. [Google Scholar]
- 21.Briggs J, Ategeka J, Kajubi R, Ochieng T, Kakuru A, Ssemanda C, et al. Impact of microscopic and submicroscopic parasitemia during pregnancy on placental malaria in a high-transmission setting in Uganda. J Infect Dis. 2019;220:457–466. doi: 10.1093/infdis/jiz130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Okell LC, Ghani AC, Lyons E, Drakeley CJ. Submicroscopic infection in Plasmodium falciparum-endemic populations: a systematic review and meta-analysis. J Infect Dis. 2009;200:1509–1517. doi: 10.1086/644781. [DOI] [PubMed] [Google Scholar]
- 23.Ntoumi F, Bakoua D, Fesse A, Komboa M, Vouvoungui JC, Koukouikila-Koussounda F. Characterization of asymptomatic Plasmodium falciparum infection and its risk factors in pregnant women from the Republic of Congo. Acta Trop. 2016;153:111–115. doi: 10.1016/j.actatropica.2015.10.009. [DOI] [PubMed] [Google Scholar]
- 24.Gueneuc A, Deloron P, Bertin GI. Usefulness of a biomarker to identify placental dysfunction in the context of malaria. Malar J. 2017;16:11. doi: 10.1186/s12936-016-1664-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roux AT, Maharaj L, Oyegoke O, Akoniyon OP, Adeleke MA, Maharaj R, et al. Chloroquine and sulfadoxine-pyrimethamine resistance in sub-Saharan Africa—a review. Front Genet. 2021;12:668574. doi: 10.3389/fgene.2021.668574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tratamento Antiretroviral e Infecções Oportunistas do Adulto, Adolescente, Grávida e Criança 2016. Republica de Mozambique. Ministerio de Saúde. Direcção Nacional de Saúde Pública. https://comitetarvmisau.co.mz/docs/guiao_tarv/TARV_IO_adulto_adolescente_crianca_gravida.pdf
- 27.WHO . Guidelines for the treatment of malaria. 3. Geneva: World Health Organization; 2015. [PubMed] [Google Scholar]
- 28.Muehlenbachs A, Mutabingwa TK, Edmonds S, Fried M, Duffy PE. Hypertension and maternal–fetal conflict during placental malaria. PLoS Med. 2006;3:e446. doi: 10.1371/journal.pmed.0030446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ndao CT, Dumont A, Fievet N, Doucoure S, Gaye A, Lehesran JY. Placental malarial infection as a risk factor for hypertensive disorders during pregnancy in Africa: a case-control study in an urban area of Senegal. West Africa Am J Epidemiol. 2009;170:847–853. doi: 10.1093/aje/kwp207. [DOI] [PubMed] [Google Scholar]
- 30.Adam I, Elhassan EM, Mohmmed AA, Salih MM, Elbashir MI. Malaria and pre-eclampsia in an area with unstable malaria transmission in Central Sudan. Malar J. 2011;10:258. doi: 10.1186/1475-2875-10-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Etard JF, Kodio B, Ronsmans C. Seasonal variation in direct obstetric mortality in rural Senegal: Role of malaria? Am J Trop Med Hyg. 2003;68:503–504. doi: 10.4269/ajtmh.2003.68.503. [DOI] [PubMed] [Google Scholar]
- 32.Dosoo DK, Chandramohan D, Atibilla D, Oppong FB, Ankrah L, Kayan K, et al. Epidemiology of malaria among pregnant women during their first antenatal clinic visit in the middle belt of Ghana: a cross sectional study. Malar J. 2020;19:381. doi: 10.1186/s12936-020-03457-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mlugu EM, Minzi O, Kamuhabwa A, Aklillu E. Prevalence and correlates of asymptomatic malaria and anemia on first antenatal care visit among pregnant women in Southeast, Tanzania. Int J Environ Res Public Health. 2020;17:3123. doi: 10.3390/ijerph17093123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ndwiga C, Odwe G, Pooja S, Ogutu O, Osoti A, Warren CE. Clinical presentation and outcomes of pre-eclampsia and eclampsia at a national hospital, Kenya: a retrospective cohort study. PLoS ONE. 2020;15:e0233323. doi: 10.1371/journal.pone.0233323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Omotayo M, Dickin K, Stolzfus R. Perinatal mortality due to pre-eclampsia in Africa: a comprehensive and integrated approach is needed. Glob Health Sci Pract. 2016;4:350–351. doi: 10.9745/GHSP-D-16-00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Calvert C, Ronsmans C. HIV and the risk of direct obstetric complications: a systematic review and meta-analysis. PLoS ONE. 2013;4:e74848. doi: 10.1371/journal.pone.0074848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gonzalez R, Rupérez M, Sevene E, Vala A, Maculuve S, Bulo H, et al. Effects of HIV infection on maternal and neonatal health in southern Mozambique: a prospective cohort study. PLoS ONE. 2017;12:e0178134. doi: 10.1371/journal.pone.0178134. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.


