Abstract
Objective
This study provided a content analysis of English and Chinese YouTube videos related to dental radiation safety.
Method
The search string, entered in English and Chinese respectively, was: (dental x-ray safe). The searches were performed and exported with Apify YouTube scraper. By screening the resultant videos and their related videos (as recommended by YouTube), a total of 89 videos were screened. Finally, 45 videos (36 English and nine Chinese) were included and analyzed. The specific information regarding dental radiation was evaluated. The Patient Education Material Assessment Tool for Audiovisual Materials was used to assess understandability and actionability.
Results
There was no significant difference between the English and Chinese videos in terms of view count, like count, comment count, and video duration. Half of the videos explicitly reassured the audience that dental x-rays are safe. Two of the English videos specifically stated that dental x-rays do not cause cancers. Numerous analogies were made in regard to radiation dose, such as equivalence to taking a flight or eating some bananas. About 41.7% of the English videos and 33.3% of the Chinese videos mentioned that patients could be further protected from scatter radiation by wearing a lead apron and thyroid collar. Videos had a good understandability score (91.3) but a poor actionability score (0).
Conclusions
Some of the analogies and the claimed radiation dose were questionable. One Chinese video even wrongly stated that dental x-rays are nonionizing radiation. The videos generally did not mention their information sources or the underlying radiation protection principles.
Keywords: YouTube, radiation safety, ALARA, health, internet, media, information, quality
Introduction
Taking dental radiographs is a very common procedure that a dentist performs multiple times on a daily basis. Dental radiographs are crucial for diagnosis and treatment planning, as many conditions cannot be readily assessed by visual examination, such as interproximal caries in the posterior teeth (i.e. tooth decay between the posterior teeth), extent of alveolar bone loss in periodontal disease, and benign/malignant lesions within the jaw bones. Prior survey data from Europe showed that there were approximately 200–300 dental radiographic examinations taken per 1000 persons per year. 1 More recent figures from the United States showed that there were 22 million panoramic examinations, 5 million dental CBCT scans, and 300 million intraoral radiographs taken during 2014–2015. 2 Meanwhile, China is the country with the largest population. Such nationwide data on dental radiographic examinations seemed to be unavailable in the literature, but it was reported that over 0.5 million dental radiographic examinations were performed in a single city (Shanghai) in a single year (2016), which was equivalent to 105 examinations taken per 1000 persons. 3 Whereas dental x-rays are invaluable tools for diagnosis and treatment evaluation by dentists, there exists an x-ray hesitancy among some of the populations with recurring themes such as all x-rays are harmful and radiation exposures are cumulative. 4 To clear the doubts, patients can ask their dentists directly or online search for the answers, such as on YouTube. Previous studies have reported that YouTube videos were frequently watched by adults with health problems 5 but generally had subpar quality and actionability.6–11 Previous studies have evaluated the YouTube videos of dental radiography targeted for the professionals, such as radiographic procedures and radiographic anatomy.12–14 However, it was of paramount importance to evaluate the videos dealing with the safety issue of dental x-rays targeted at the public. Therefore, this study aimed to reveal whether the videos reassured the public about the safety of dental radiographic examinations, assess the content covered by them and check for the presence of any inaccurate information. We hypothesized that most videos would have a reassuring tone regarding safety concerns, and would mention authoritative bodies as their information source. Because of the large English- and Chinese-speaking populations, this study evaluated videos of both languages.
Materials and methods
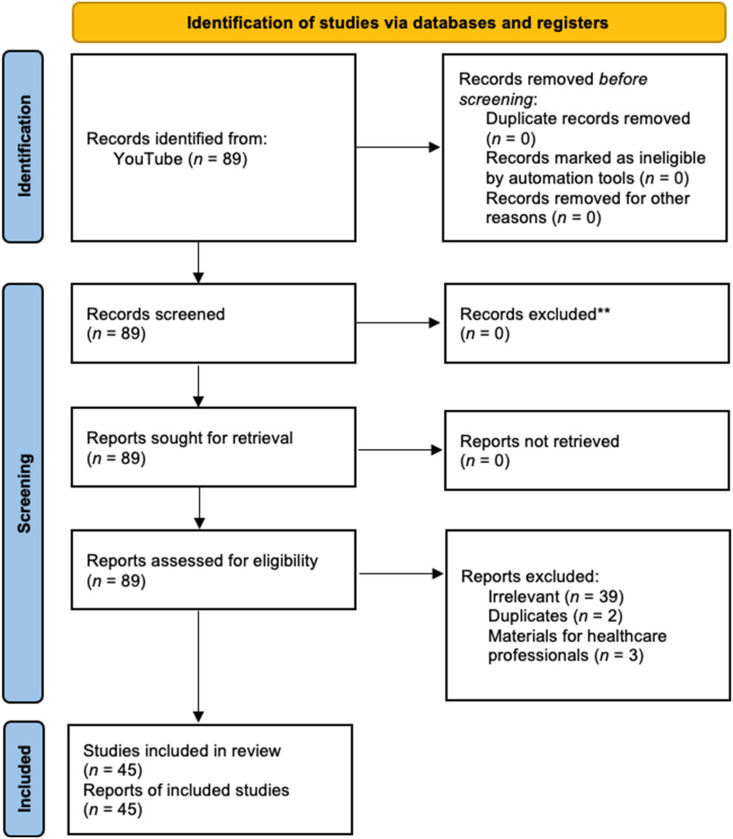
On 12th August 2022, a search was performed on YouTube for English videos. The search string was: (dental x-ray safe). On 28th November 2022, an additional YouTube search was performed per reviewer's request for Chinese videos. The search string was: (牙科X光安全) [In English: “dental x-ray safety”]. The searches were performed and exported with Apify YouTube scraper (https://apify.com/bernardo/youtube-scraper). Apify can extract the following metrics for each video resulting from the scrape: Channel name, channel URL, number of subscribers, view count, number of likes, comment count, video upload date, duration, video URL, and video title. By screening the resultant videos and their related videos (as recommended by YouTube), a total of 61 English videos and 28 Chinese videos were screened. Videos were excluded if they were irrelevant, duplicate videos, lectures for healthcare professionals, and plain explanations of radioprotection measures. Finally, 45 videos (36 English and nine Chinese) were included and analyzed (Figure 1).
Figure 1.
The screening process of YouTube videos on dental x-ray safety.
The following parameters were recorded for each video: (1) explicit statement on whether dental x-ray is safe, (2) stating that the benefits should outweigh the risks, (3) introduction of the concept of “as low as reasonably achievable” (ALARA) and/or its variants, (4) concept of deterministic versus stochastic effects, (5) concept of linear no-threshold (LNT) model, (6) notion that modern digital x-ray has less radiation than traditional analog film x-ray, (7) use of lead apron/thyroid collar, (8) other sources of radiation and comparisons, and (9) sources of information. The rationale for including these radiology-specific concepts is explained below.
The concept of the ALARA principle originated in the early 20th century following the discovery of x-ray. 15 It is an important principle as it reminds clinicians to try their best efforts to reduce radiation exposure to their patients. In other words, clinicians should not always attempt to produce the best-quality radiographs (e.g. through re-taking or increasing the radiation dose) as long as the radiographs have adequate diagnostic value. Meanwhile, the biological effects of radiation have been traditionally classified into either deterministic or stochastic. 16 For the former, the severity of the effect increases with increasing radiation dose, when the dose surpasses a safety threshold. Examples included graying of hair and lens opacification. For the latter, the probability of producing the effect (but not its severity) increases with increasing radiation dose. Examples included cancers. It is important to understand that dental radiography uses very small radiation doses that deterministic effects should not occur. The LNT model assumes that the risk of stochastic effects (e.g. cancers) holds a positive, linear relationship with radiation dose without any safety threshold. This concept should better inform the audience about the context of radiation safety. Finally, the use of a lead apron/thyroid collar can physically block x-ray that directs toward various parts of the patient's body that are not (and do not need to be) visualized in the radiographs. In certain occasions, their usage can better safeguard the patients.
Mann-Whitney U tests were performed to evaluate if there were significant differences between English and Chinese videos in terms of viewing metrics, such as view count, like count, comment count, video duration, channel subscriber count, and age of video. Tests were conducted by SPSS 26.0 (IBM, NY, USA).
Following previous studies on YouTube videos,9,17 the validated Patient Education Materials Assessment Tool for Audiovisual Materials (PEMAT A/V) 18 was used to evaluate the understandability and actionability of the YouTube videos. There were 17 evaluation items that assessed the content, word choice and style, organization, layout and design, use of visual aids, and actionability. The outcome of the assessment resulted in an Understandability score (0–100%) and an Actionability score (0–100%) for comparison between videos. In brief, understandability refers to the ability of the audience to process and explain key messages conveyed in the videos, whereas actionability refers to the ability of the audience to identify what they can do according to the information presented in the videos. 18 Ethical approval was not applicable to this study. The first author (AY), a dental radiologist with 11 years of working experience and both English and Chinese as his native languages, was responsible for reviewing the content of these videos. He watched each video twice to ensure the accuracy of the coded data. He has also previously published three articles that analyzed YouTube videos of dental radiography on radiographic procedures and radiographic anatomy.12–14
Results
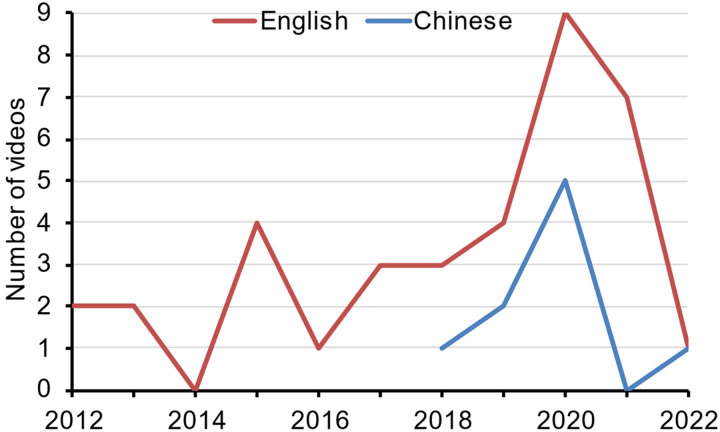
The details of the 45 videos on dental x-ray safety are listed in Table S1. The oldest one was uploaded on 12th November 2012 whereas the most recent one was uploaded on 24th January 2022. The year 2020 had the highest number of videos uploaded (n = 14). If the year 2022 was omitted, there seemed to be an overall upward trend in the number of English videos uploaded across the years, whereas Chinese videos began to appear only in 2018 (Figure 2).
Figure 2.
Number of YouTube videos uploaded each year on dental x-ray safety.
The 36 English videos had a median view count of 350 times, with a median duration of 161.5 seconds (Table 1). Meanwhile, the nine Chinese videos had a median view count of 2021 times, with a median duration of 113.0 seconds. Comments were turned off for one English video. Notwithstanding, the median comment count was only one for English videos and 0 for Chinese videos. There was no significant difference in the viewing metrics between English and Chinese videos.
Table 1.
Viewing metrics of the 36 videos.
| Metric | Median; IQR | Min; Max | p-value | |||
|---|---|---|---|---|---|---|
| English | Chinese | English | Chinese | |||
| View count | 350.0; 3870.3 | 2021.0; 1596.0 | 9; 23021 | 1; 8588 | 0.590 | |
| Like count | 7.0; 31.3 | 11.0; 10.0 | 0; 472 | 0; 41 | 0.754 | |
| Comment count | 1.0; 9.5 | 0; 2.0 | 0; 138 | 0; 2 | 0.178 | |
| Duration (s) | 161.5; 197.0 | 113.0; 148.0 | 32; 587 | 15; 256 | 0.233 | |
| Channel subscriber | 303.5; 21839.3 | 503.0; 1683.0 | 10; 1590000 | 30; 12800 | 0.712 | |
| Age of video (y) | 2.8; 3.8 | 2.8; 0.9 | 0.6; 9.8 | 0.9; 4 | 0.712 |
Regarding the question of whether dental x-rays are safe, exactly half of the 36 English videos explicitly reassured the audience that they are safe (n = 18). For the relevant excerpts, please see Table 2. Two of these videos (Videos #E14 and #E20) went beyond general safety and specifically stated that dental x-rays do not cause cancers. Meanwhile, nearly half of the nine Chinese videos explicitly reassured the audience that dental x-rays are safe (n = 4).
Table 2.
Excerpts from the 18 English and four Chinese videos that explicitly said dental x-rays are safe.
| Video number | Excerpts |
|---|---|
| #E1 | “Yes. First off, today's digital x-rays do not use near as much radiation as what traditional radiographs (x-rays) did a couple of decades ago. But even then, they were still safe!” (In video description) |
| #E2 | (After saying that digital x-rays have lower radiation dose than film x-rays) “Film radiographs still use very low radiation exposure and are still considered very safe.” |
| #E5 | “Digital x-rays that we use today do not use nearly as much radiation as the traditional x-rays did decades ago, but even then they were still safe.” |
| #E7 | “Yes, dental x-ray are safe.” |
| #E11 | “The good thing about dental x-rays is that, just by being below levels that are considered dangerous, because the way radiation works, they are completely safe.” |
| #E14 | “Dental x-ray can never cause cancer!” and “You are safe!” |
| #E15 | “Dental x-rays are not at all harmful because their exposure time is very less coming to new systems of x-rays.” |
| #E20 | “Our dental x-ray is dangerous because of the radiation? No.” and “There are no documented cases of anyone having cancers from dental x-rays.” |
| #E21 | “Yes, our x-rays are safe.” |
| #E22 | “Dental x-rays today are actually very safe.” |
| #E23 | “Are they safe? And I want to assure you that they are.” And “In my opinion there really is no risk.” |
| #E25 | “Studies confirmed that radiation doses below 50,000 μSv are safe to the patient.” |
| #E26 | “Yes, dental x-ray are safe.” |
| #E28 | “Doing regular x-rays will not harm your overall body.” |
| #E29 | “Dental x-rays are safe.” |
| #E30 | “Yes! Dental x-rays are safe.” |
| #E31 | “Modern dental x-rays […] is exceedingly safe.” |
| #E33 | “They are very safe.” |
| #C1 | “The radiation dose of dental x-rays is very safe indeed.” (In video description) |
| #C3 | “The radiation dose of dental x-rays is very low and very safe.” |
| #C4 | “Normally, dental x-rays are very safe.” |
| #C9 | “Dental x-rays are safe and have no problem.” |
Please see Table S1 for the URLs and video titles of these videos. The excerpts from Chinese videos were translated into English.
The other 18 English videos mostly did not directly answer the question of whether dental x-rays are safe. Three of these 18 had a cautious tone (Table 3). Besides, five Chinese videos did not directly address if dental x-rays are safe. One of them had a cautious tone.
Table 3.
Excerpts from the three English and one Chinese videos that had a cautious tone.
| Video number | Excerpts |
|---|---|
| #E3 | “There actually is some risk while it is incredibly low. There is a risk to taking any sort of x-ray.” |
| #E18 | “Any kind of exposure to radiation can damage cells and tissues and can lead to the development of cancer in rare instances.” |
| #E27 | “There is always a slight risk of damage to your cells or tissue from being exposed to any radiation.” |
| #C2 | “The risk of causing pathology by the radiation dose of dental x-rays is not high. The risk of causing cancers is very small.” |
Meanwhile, half of the English videos (n = 18) and 11.1% of Chinese videos (n = 1) mentioned that modern digital imaging has less radiation than traditional analog film imaging and hence patients are now safer than before. About 41.7% of the English videos (n = 15) and 33.3% of the Chinese videos (n = 3) mentioned that patients could be further protected from scatter radiation by wearing lead apron and thyroid collar. One-third of the English videos (n = 12) but none of the Chinese videos mentioned that dentists would only take dental x-rays for patients when the benefits should outweigh the risks. The concept of the ALARA principle was mentioned in 19.4% of the English videos (n = 7) but none of the Chinese videos. Only one English video (2.8%) but no Chinese video elaborated on the concepts of deterministic versus stochastic effects (Video #E9). No English or Chinese video mentioned the concept of the LNT model.
Radiation sources other than dental x-rays were mentioned by 63.9% of the English videos (n = 23). On top of the list were walking under the sun (n = 15, 41.7%), taking a flight (n = 13, 36.1%), and eating foods (n = 8, 22.2%) (Table 4). Readers should be aware that cellphone, computer, and microwave are different from radiographic procedures as they emit nonionizing radiation. Meanwhile, some fluorescent lamps manufactured in the past might contain radioactive materials.
Table 4.
Radiation sources (other than dental x-rays) mentioned by the videos.
| Source | Frequency (% of 36) of English videos | Frequency (% of nine) of Chinese videos |
|---|---|---|
| Ionizing radiation | ||
| Walking under the sun | 15 (41.7) | 2 (22.2) |
| Taking a flight | 13 (36.1) | 3 (33.3) |
| Eating foods (e.g. bananas) | 8 (22.2) | 2 (22.2) |
| Living in a brick house | 5 (13.9) | 0 |
| Sleeping next to someone | 3 (8.3) | 0 |
| Medical radiographic procedures | 3 (8.3) | 0 |
| Radon gas | 3 (8.3) | 0 |
| Soil | 2 (5.6) | 1 (11.1) |
| Smoking | 2 (5.6) | 1 (11.1) |
| Heating/cooking with natural gas | 1 (2.8) | 0 |
| Fluorescent lamp | 1 (2.8) | 0 |
| Air | 1 (2.8) | 0 |
| Water | 1 (2.8) | 0 |
| Nonionizing radiation | ||
| Using cellphone | 3 (8.3) | 0 |
| Computer | 1 (2.8) | 0 |
| Microwave | 1 (2.8) | 0 |
It would be helpful for the audience to comprehend if the videos compared the radiation dose received from dental x-rays with examples from daily life. 66.7% of the English videos (n = 24) and 88.9% of the Chinese videos (n = 8) attempted to make such comparisons and they are listed in Table 5. In Table 5, a “dental x-ray” means an intraoral radiograph and the abbreviations used are as follows. BGR, background radiation; FAA, Federal Aviation Administration; FMX, full mouth series (approximately 15–20 dental x-rays); IAEA, International Atomic Energy Agency; and ICRP, International Commission on Radiological Protection.
Table 5.
Comparisons of radiation dose received from dental x-rays with daily life examples extracted from the videos.
| Video number | Comparisons made and the claimed dose (converted into μSv) | Comments |
|---|---|---|
| #E1, #E5, #E6 |
|
The claimed radiation dose of 1 dental x-ray (0.2 μSv) and hence FMX (3.9 μSv) was only 2.5%–20% of the figure listed by IAEA. 19 |
| #E3 |
|
The speaker said that his clinic would take 1 FMX (18 x-rays) for every patient at the initial visit if they could not access the record from the patient's previous dentist. However, the practice of routine pre-treatment FMX is debatable. 2 |
| #E7 |
|
|
| #E8 | 1 FMX = being out in the sun for a few hours for a few days, or 1 cross-country flight. | NA. |
| #E9 |
|
The speaker reported figures that should be in μSv but wrongly in mSv, hence all the claimed figures were about 1000x of those listed by IAEA. 19 |
| #E11 |
|
NA. |
| #E12 | 1 dental x-ray (0.2 μSv) = eating 2 bananas, or < daily BGR (8 μSv), or < 1 flight from NY to LA (40 μSv). | The claimed radiation dose of 1 dental x-ray (0.2 μSv) was only 2.5%–20% of the figure listed by IAEA. |
| #E19 | Dental x-rays taken during an annual check-up = 50% of dose received from daily activities on a day. | The comparison had unclear context. |
| #E20 | 1 FMX < 1 flight for 1–2 h. | The speaker mentioned that 1 dental x-ray = 5 μSv. According to FAA-based formula, 21 2-h flight roughly = 6 μSv, hence the claim that 1 FMX (15-20 dental x-rays) < 1 flight for 1-2 h seemed questionable. |
| #E22 | Dental x-rays < dose received on a normal day outside. | The comparison had unclear context. |
| #E23 | Dental x-rays taken during an annual check-up = driving a car for 15–20 min. | The comparison had unclear context. |
| #E24 | Digital X-rays < 1 coast-to-coast flight, or living in a concrete building. | The comparison had unclear context. |
| #E25 |
|
According to FAA-based formula, 21 7-h flight roughly = 36 μSv, 1.8x of the claimed figure. |
| #E26 | 1 dental x-ray = 8 units of radiation dose, 1 FMX = 25 units, and 1 medical CT scan = 1000 units. |
|
| #E27 | 1 dental x-ray < 0.3% of annual BGR. | NA. |
| #E28 | 1 dental x-ray (5 μSv) = 1 day of BGR. | NA. |
| #E30 | 1 dental x-ray (1 μSv) = from soil (1 μSv per day), or 4 days of cooking with natural gas (0.25 μSv per day), < 1 transcontinental flight (20–40 μSv), and < smoking (4 μSv per day). | The speaker wrongly said that the radiation dose for a transcontinental flight was per year, which did not make sense. The subtitle was correct. |
| #E31 | 1 dental xray (1 μSv) = 1.4% of living in a brick house for a year, 1.7–2% of a flight from NY to LA, or 30 bananas. | The commonly known banana equivalent dose = 0.1 μSv. Hence the claimed dose for 1 dental x-ray should only = 10 bananas. |
| #E32 | 1 dental x-ray = 1 day of BGR. | NA. |
| #E33 | 1 dental x-ray (5 μSv) = 1 cross-country flight. | Depending on the flight time, a cross-country flight should have much more radiation dose. |
| #E34 | 1 dental x-ray < 1 flight from NY to LA. | The video wrongly claimed that cellphone, microwave, and computers emitted more radiation than dental x-rays. The former group should emit non-ionizing radiation which is different from dental x-rays. |
| #E35 | Coming to the dentist (and get dental x-rays) < 1 flight. | The comparison had unclear context. |
| #C1 | 1 dental x-ray (5 μSv) < 1 day of BGR (8.2 μSv) < 1 panoramic (10 μSv). | NA. |
| #C2 | 1 dental x-ray (0.005 μSv) = 1 day of BGR. | The claimed radiation dose of 1 dental x-ray (0.005 μSv) was much lower than the figure listed by IAEA. 19 This was probably due to a typo mistake, as the displayed word correctly said milli but the SI unit was wrongly displayed as micro. |
| #C3 | 1 dental x-ray (2 μSv) < 1 day of BGR (2.7 μSv). | NA. |
| #C4 | 1 dental x-ray (1-2 μSv) < 1 day of BGR (6.6 μSv) < 1 panoramic (16 μSv) < 1 child CBCT (42 μSv) < radiation dose with increased cancer risk (100,000 μSv). | Cancer should be a stochastic effect without a safe threshold. |
| #C6 | 1 day of BGR (4.4 μSv) < 1 dental x-ray (5 μSv) < 1 panoramic (10 μSv) < smoking 30 pieces of cigarette in a day (35.6 μSv) < 1 Taiwan to USA West coast flight (90 μSv). | NA. |
| #C7 | 1 panoramic < radiation received by walking on the street. | This video wrongly claimed that dental x-ray is nonionizing radiation. |
| #C8 | 1 day of BGR (4.4 μSv) < 1 dental x-ray (5 μSv) < 1 panoramic (10 μSv) < 1 CBCT (60 μSv) < 1 Taiwan to USA West coast flight (90 μSv). | NA. |
| #C9 | 1 dental x-ray (5 μSv) < 1 panoramic (10 μSv) < 1 Taiwan to USA West coast flight (90 μSv). | The video claimed that ICRP said that radiation dose < 100,000 μSv is not harmful. This claim was not accurate. |
Though the sun was most frequently mentioned radiation source as seen in Table 4, the most common comparison was actually about taking a flight: one dental x-ray (or one full mouth series of 15–20 dental x-rays, FMX) had a lower radiation dose than a flight from the West Coast to the East Coast of the United States, or a flight between Taiwan and the West Coast of the United States. It is understandable that the radiation dose for one dental x-ray is variable depending on the radiographic equipment and its parameter settings. In the English videos, the claimed dose of one dental x-ray ranged from 0.2 to 5 μSv, which, according to the videos, equals to eating as few as two bananas up to as many as 30 bananas. The Chinese videos claimed that the dose of one dental x-ray ranged from 1 to 5 μSv, comparable to the English videos. However, the Chinese videos did not compare such doses with the dose from foods.
Only 22.2% of the English videos (n = 8) mentioned their source of information. The American Dental Association (ADA) was mentioned in five videos, one of which also mentioned the American Medical Association as well. The other three videos mentioned the United States Nuclear Regulatory Commission, the American Academy of Pediatric Dentistry, and the Radiological Society of North America/American College of Radiology once each. Meanwhile, 33.3% of the Chinese videos (n = 3) mentioned their information source, two of which quoted the Taiwan Atomic Energy Council together with ICRP, and one quoted the ADA.
Finally, the assessment by PEMAT A/V tool revealed that both English and Chinese videos were very understandable (Table 6). However, most of them did not identify actions the audience could take. For instance, the videos rarely mentioned that the patients might ask for copies of x-rays recently taken by their previous dentists. The videos also did not, as listed in PEMAT A/V tool, use charts or other visuals to explain how the audience should take actions. In this example of copying x-rays, a simple flow chart can suggest to the audience that perhaps they should copy x-rays taken in the last 1–2 years and bring them to their new dentist in case they have active dental diseases.
Table 6.
Assessment outcome of the videos according to PEMAT A/V tool.
| Metric | Median; IQR | Min; Max | ||
|---|---|---|---|---|
| English | Chinese | English | Chinese | |
| Understandability score | 91.3; 20.6 | 90.0; 27.3 | 66.7; 100 | 72.7; 100 |
| Actionability score | 0; 100 | 0; 0 | 0; 100 | 0; 0 |
Discussion
This YouTube video survey analyzed 45 videos (36 English and nine Chinese) regarding the safety of dental x-rays. The majority of them had a very positive tone on this issue, with half of the videos explicitly stated that dental x-rays are safe. The rest of the videos usually did not directly address this issue, but stating that the radiation dose received from dental radiography is very low, and even lower by the use of modern digital x-rays. The most common analogies of receiving radiation from dental radiography were taking a flight and eating foods such as bananas. However, few videos mentioned their information source. One reassuring aspect resulted from the evaluation was that most videos had good understandability.
One common issue of these videos was the lack of references to the information sources. Some of the contents might be inaccurate or misleading. For instance, three videos compared taking one dental x-ray to eating two bananas (Videos #E1, E5, E6) and one video claimed that it was equivalent to eating 30 bananas (Video #E31). The audience might be explained the fact that a banana contains a small amount of radioactive isotope potassium-40 and hence is radioactive. However, the comparisons were very different. The audience may be able to imagine eating two bananas on a regular daily basis, but it would be virtually impossible to imagine a scenario of eating 30 bananas. Hence, the former might sound very casual and trivial, whereas the latter might relatively make a patient feel worried. In fact, one banana should carry approximately 0.1 μSv of radiation (also commonly known as one banana equivalent dose), whereas one dental x-ray should involve 1–8 μSv of radiation according to IAEA, 19 equivalent to 10–80 bananas. Interestingly, none of the Chinese videos made an analogy between taking dental x-rays and eating foods.
The same issue applied to the analogy of taking a flight. Some videos mentioned that one dental x-ray had less radiation than one coast-to-coast flight in the United States (e.g. Videos #E12, E31, E34), some said equal to one cross-country flight (e.g. Video #E33) or a flight between Taiwan and the United States (Videos #C6, C8, C9). Some videos were more affirmative by claiming that even 1 FMX (e.g. Videos #E1, E5, E6) or one panoramic radiograph (Videos #C6, C8, C9) had less radiation than one such flight.
Here, we recognized that FMX was only covered by English videos, whereas panoramic radiograph was covered by seven Chinese videos and only one English video. Perhaps this implied a differential radiographic practice between China and English-speaking regions. Meanwhile, the amount of cosmic radiation received on a flight depends on multiple factors such as solar activity, flight altitude, and latitude.22,23 A general coast-to-coast flight within the United States had approximately 35 μSv. 24 Hence, in reality, it may be very difficult to provide an accurate comparison with a flight.
Another issue was related to the nature of the radiation. Some videos mentioned that the public frequently received radiation from their cellphones, computers, and microwaves. The radiation emitted from these sources are nonionizing, meaning that they are not measured in μSv and cannot produce damage by removing electrons from atoms and molecules, but they can produce damage by heat. 25 Heat is produced as nonionizing radiation changes the rotational, vibrational, or electronic valence configurations of atoms and molecules that absorb the energy. Walking under the sun exposes a person to ultraviolet radiation, which also belongs to this category; and, to a lesser extent, cosmic radiation, which is ionizing. It should be noted that one Chinese video wrongly categorized dental x-rays into nonionizing radiation (Video #C7).
Besides the amount of the radiation dose, the distribution of the radiation dose over the exposure period (dose rate) should also be considered in radiation risk assessment. The mutagenic and carcinogenic effects of ionizing radiation are reduced when the dose rate is reduced.26,27 It is reasonable to expect that the same amount of radiation received within a fraction of one second (dental x-ray) and across several hours (flight) would affect cells differently, not to mention that the former focuses on the oral cavity whereas the latter is distributed across the entire body. However, none of the videos mentioned about this.
The cornerstone of radiation protection in dentistry and medicine is the ALARA principle. 15 It urges radiation workers and users to reduce the radiation dose as long as the radiographic procedures retain the acceptable diagnostic value. It is an implicit adherence to the LNT model, which assumes that the risk of stochastic health effects (called response, e.g. cancer risk) holds a positive, linear relationship with radiation dose. (Readers are referred to 28 for a comprehensive historical review of the development of the LNT model and its establishment as the default model for cancer risk assessment.) Within this model, there is not a threshold below which radiation is safe, and that the risk of having cancer (but not its severity) is proportional to the radiation dose. However, it should be noted that the model was only developed and supported by evidence in the moderate dose band (>100 mGy) and high dose band (>1 Gy) which is much higher than the dose involved in dental radiography, and the model does not consider the presence of biological defense mechanisms such as DNA repair. 29 Meanwhile, LNT model is unsuitable for deterministic effects (tissue reactions), for which the effect severity increases with radiation dose that exceeds a safe threshold.
A prior in vitro study reported that dental CBCT (a form of 3D dental imaging with a much higher radiation dose than a plain dental x-ray) could induce DNA damage in dental mesenchymal stromal cells but seemed to exert a minimal final effect on cell cycle progression. 30 A recent clinical study found that the buccal cheek mucosal cells of children and adult patients undergoing CBCT scans reacted differently but found no dose-response relationship, and both groups did not suffer from DNA double-strand breaks. 31 Evidence from these preliminary studies seemed to suggest that dental radiation would indeed induce small molecular effects, but it was largely unclear if such effects would lead to any short- or long-term health effects after undergoing biological defense mechanisms. One of the surveyed video (Video #E7) indeed mentioned that the human body is able to recover from small doses of radiation without any lasting adverse events. Notwithstanding, prior to getting a clear conclusion from the scientific community, it is still reasonable to consider the ALARA principle, use low-dose imaging modes if possible, 32 and use the lead apron and thyroid collar to provide additional protection for patients deemed appropriate, following the guidance from the local authority. Some research groups modified the ALARA principle and suggested that the ALADAIP (“as low as diagnostically acceptable being indication-oriented and patient-specific”) principle should be observed. 33 However, international organizations such as ICRP or IAEA have not yet accepted it or included it in their glossary.
Overall, inaccurate information indeed existed in some of the videos. The inaccurate analogies of dental x-rays to daily life radiation sources might either impose a false impression of absolute safety or trigger unnecessary/exaggerated fear. Moreover, instead of being retained within the problematic videos, the misinformation may be spread out by the audience through social media. As the audience can be content creators by themselves, they may create infographics, their own videos/vlogs/blogs, or post a soundbite on Twitter, Reddit, etc. As a result, the misinformation can reach and affect a broader audience across platforms.
There were some limitations of this study. Only English and Chinese YouTube videos were considered. It should be noted that Spanish and Hindi were also among the most used languages in the world, but the authors were incompetent in these languages. Hence these languages were omitted. Private and unlisted videos posted on YouTube could not be accessed. Due to constrained resources, the posted comments on the videos were not analyzed in this study.
Conclusions
Within the limitation of analyzing English and Chinese language videos, we found that many of them had a positive and reassuring tone that dental x-rays are safe. Numerous analogies were made to help the audience to better comprehend the radiation dose received, such as equivalence to taking a flight or eating some bananas. However, some of these analogies and the claimed radiation dose were questionable. The videos generally did not mention their information sources or the underlying radiation protection principles, such as ALARA and LNT model, rendering them relatively superficial. There was no significant difference in the viewing metrics between English and Chinese videos. The radiation doses of dental x-rays claimed by English and Chinese videos were similar. However, English videos mentioned more radiation sources (other than dental x-rays) than Chinese videos. One Chinese video had a very serious mistake by claiming dental x-rays as nonionizing radiation. Future videos targeting the audience should provide accurate information and cite their information source. Meanwhile, the general public should be reminded that such existing videos available on YouTube may contain inaccurate information and thus cannot replace customized expert advice from their family doctor or dentist regarding radiation safety.
Acknowledgements
Not applicable.
Footnotes
Contributorship: AY contributed to the conceptualization, writing, data synthesis, and revision of this article. EP, JH, MKP, OK, HW, and AA contributed to the drafting and final revision of this article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, and authorship of this article. The publishing fee of this article was supported by Ludwig Boltzmann Institute for Digital Health and Patient Safety, Medical University of Vienna.
Ethical approval: Not applicable.
Guarantor: AY.
ORCID iD: Andy Wai Kan Yeung https://orcid.org/0000-0003-3672-357X
References
- 1.Regulla DF, Eder H. Patient exposure in medical X-ray imaging in Europe. Radiat Prot Dosim 2005; 114: 11–25. [DOI] [PubMed] [Google Scholar]
- 2.Benn DK, Vig PS. Estimation of x-ray radiation related cancers in US dental offices: is it worth the risk? Oral Surg Oral Med Oral Pathol Oral Radiol 2021; 132: 597–608. [DOI] [PubMed] [Google Scholar]
- 3.Yao J, Gao L, Qian A, et al. Survey on frequency of medical X-ray diagnosis in Shanghai (in Chinese). Chinese Journal of Radiological Medicine and Protection 2019; 39: 370–375. DOI: 10.3760/cma.j.issn.0254-5098.2019.05.009 [Google Scholar]
- 4.Oakley PA, Harrison DE. X-Ray hesitancy: patients’ radiophobic concerns over medical X-rays. Dose Response 2020; 18: 1559325820959542. DOI: 10.1177/1559325820959542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Langford AT, Orellana KT, Buderer N. Use of YouTube to watch health-related videos and participation in online support groups among US adults with heart disease, diabetes, and hypertension. Digital Health 2022; 8: 20552076221118822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hegarty E, Campbell C, Grammatopoulos E, et al. YouTube™ as an information resource for orthognathic surgery. J Orthod 2017; 44: 90–96. [DOI] [PubMed] [Google Scholar]
- 7.Ustdal G, Guney AU. YouTube as a source of information about orthodontic clear aligners. Angle Orthod 2020; 90: 419–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ward B, Ayyala HS, Zhang K, et al. YouTube for cosmetic plastic surgery: an effective patient resource? Aesthet Surg J 2020; 40: NP314–NP319. [DOI] [PubMed] [Google Scholar]
- 9.Bellon-Harn ML, Manchaiah V, Shashikanth S. A cross-sectional study of the portrayal of childhood speech and language disorders in YouTube videos. Digital Health 2020; 6: 2055207620929785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kallur A, Albalbissi A, Carillo-Martin I, et al. Doctor YouTube’s opinion on seasonal influenza: a critical appraisal of the information available to patients. Digital Health 2020; 6: 2055207620906968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meldrum S, Savarimuthu BT, Licorish S, et al. Is knee pain information on YouTube videos perceived to be helpful? An analysis of user comments and implications for dissemination on social media. Digital Health 2017; 3: 2055207617698908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grillon M, Yeung AWK. Content analysis of YouTube videos that demonstrate panoramic radiography. Healthcare 2022; 10: 1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yeung AWK. Content analysis of YouTube videos on radiographic anatomy on dental panoramic images. Healthcare 2022; 10: 1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grillon M, Yeung AWK. Content analysis of YouTube videos that demonstrate periapical radiography. Applied Sciences 2022; 12: 9602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yeung AWK. The “As Low As Reasonably Achievable” (ALARA) principle: a brief historical overview and a bibliometric analysis of the most cited publications. Radioprotection 2019; 54: 103–109. [Google Scholar]
- 16.Blakely EA. Biological effects of cosmic radiation: deterministic and stochastic. Health Phys 2000; 79: 495–506. [DOI] [PubMed] [Google Scholar]
- 17.Morra S, Napolitano L, Ruvolo CC, et al. Could YouTubeTM encourage men on prostate checks? A contemporary analysis. Archivio Italiano di Urologia e Andrologia 2022; 94: 285–290. [DOI] [PubMed] [Google Scholar]
- 18.Shoemaker SJ, Wolf MS, Brach C. Development of the Patient Education Materials Assessment Tool (PEMAT): a new measure of understandability and actionability for print and audiovisual patient information. Patient Educ Couns 2014; 96: 395–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.International Atomic Energy Agency. Radiation doses in dental radiology, https://www.iaea.org/resources/rpop/health-professionals/dentistry/radiation-doses#4(2022, accessed August 18, 2022).
- 20.International Commission on Radiological Protection. The 2007 recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Amsterdam, Netherlands: Elsevier, 2007. [Google Scholar]
- 21.Yuri K.Flight Radiation Exposure Calculator, https://www.translatorscafe.com/unit-converter/en-US/calculator/flight-radiation-exposure/(2022, accessed August 18, 2022).
- 22.Bottollier-Depois J-F, Chau Q, Bouisset P, et al. Assessing exposure to cosmic radiation during long-haul flights. Radiat Res 2000; 153: 526–532. [DOI] [PubMed] [Google Scholar]
- 23.Friedberg W, Copeland K, Duke FE, et al. Radiation exposure during air travel: guidance provided by the Federal Aviation Administration for air carrier crews. Health Phys 2000; 79: 591–595. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Radiation from Air Travel, https://www.cdc.gov/nceh/radiation/air_travel.html(2022, accessed November 14, 2022).
- 25.Centers for Disease Control and Prevention. The Electromagnetic Spectrum: Non-Ionizing Radiation, https://www.cdc.gov/nceh/radiation/nonionizing_radiation.html(2022, accessed August 18, 2022).
- 26.Vilenchik MM, Knudson AG. Radiation dose-rate effects, endogenous DNA damage, and signaling resonance. Proc Natl Acad Sci USA 2006; 103: 17874–17879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vilenchik MM, Knudson AG, Jr. Inverse radiation dose-rate effects on somatic and germ-line mutations and DNA damage rates. Proc Natl Acad Sci USA 2000; 97: 5381–5386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Calabrese EJ. From muller to mechanism: how LNT became the default model for cancer risk assessment. Environ Pollut 2018; 241: 289–302. [DOI] [PubMed] [Google Scholar]
- 29.Siegel JA, Greenspan BS, Maurer AH, et al. The BEIR VII estimates of low-dose radiation health risks are based on faulty assumptions and data analyses: a call for reassessment. J Nucl Med 2018; 59: 1017–1019. [DOI] [PubMed] [Google Scholar]
- 30.Belmans N, Gilles L, Welkenhuysen J, et al. In vitro assessment of the DNA damage response in dental mesenchymal stromal cells following low dose X-ray exposure. Front Public Health 2021; 9: 584484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Belmans N, Gilles L, Vermeesen R, et al. Quantification of DNA double strand breaks and oxidation response in children and adults undergoing dental CBCT scan. Sci Rep 2020; 10: 2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yeung AWK, Jacobs R, Bornstein MM. Novel low-dose protocols using cone beam computed tomography in dental medicine: a review focusing on indications, limitations, and future possibilities. Clin Oral Investig 2019; 23: 2573–2581. [DOI] [PubMed] [Google Scholar]
- 33.Oenning AC, Jacobs R, Pauwels R, et al. Cone-beam CT in paediatric dentistry: DIMITRA project position statement. Pediatr Radiol 2018; 48: 308–316. [DOI] [PubMed] [Google Scholar]