Objective
The aim of the study is to identify differences in demographics, severity of disease, and rates of hospital readmission among adults discharged to skilled nursing facilities and inpatient rehabilitation facilities after hospitalization for coronavirus 2019.
Design
This is a retrospective cohort study of adults hospitalized with coronavirus 2019 infection at academic medical centers participating in the Vizient Clinical Data Base between April 1, 2020, and June 30, 2021, who were discharged to skilled nursing facilities or inpatient rehabilitation facilities (N = 39,882). Data from the Clinical Data Base are used with permission of Vizient, Inc. All rights reserved.
Results
Among adults hospitalized with coronavirus 2019 infection, those discharged to skilled nursing facilities were 1.4 times more likely to require hospital readmission than those discharged to inpatient rehabilitation facilities. They were, on average, older (73 vs. 61 yrs, P < 0.001) and had shorter hospital lengths of stay (15 vs. 26 days, P < 0.0001) than the patients discharged to inpatient rehabilitation facilities. Persons discharged to inpatient rehabilitation facilities were more likely to have received intensive care and mechanical ventilation while hospitalized (P < 0.001).
Conclusions
Individuals discharged to inpatient rehabilitation facilities after hospitalization for coronavirus 2019 differ from those discharged to skilled nursing facilities on a number of key variables, including age, hospital length of stay, having received intensive care, and odds of hospital readmission.
Key Words: COVID-19, Pandemics, Patient Readmission, Rehabilitation Centers
What Is Known
Survivors of severe COVID-19 infections often require rehabilitation services in postacute care settings after hospitalization. Early reports indicated high rates of hospital readmission among persons discharged to rehabilitation facilities.
What Is New
Among patients discharged from academic medical centers to postacute care settings, those discharged to inpatient rehabilitation facilities had significantly lower odds of hospital readmission than did those discharged to skilled nursing facilities, despite having longer average hospital lengths of stay, a higher average case mix index, and greater likelihood of having received intensive care.
The coronavirus 2019 (COVID-19) pandemic has resulted in tremendous demand for both hospitalization and postacute care. Survivors of severe acute respiratory syndrome coronavirus 2 infections who have required hospital admission are often left with functional impairments, which may in turn result in the need for postacute rehabilitation care in either the home or an inpatient setting.1 At the time of writing, thousands of Americans have been discharged to skilled nursing facilities (SNFs) or inpatient rehabilitation facilities (IRFs) after hospitalization for COVID-19.2 Little is known, however, as to how the groups of individuals discharged to these two settings after COVID-19 hospitalization differ in terms of demographics, severity of disease, and likelihood of hospital readmission.
Skilled nursing facilities are the most commonly used postacute care setting in the United States. Before the pandemic, in 2019, 18.7% of inpatient hospital discharges were to such facilities.3 Short-term care in SNFs for skilled nursing and rehabilitation services after a qualifying inpatient hospital stay is a covered benefit for persons enrolled in Medicare, the federal health insurance program for individuals 65 yrs and older, those with end-stage renal disease, and some persons with chronic disabilities. Many other health insurance plans also cover short-term SNF care. The majority of SNFs also provide long-term care services, which are not a covered Medicare benefit but are covered by Medicaid, the joint federal, and state health insurance program for low-income Americans.4
Far fewer inpatient hospitalizations result in discharges to IRFs. Discharges to IRFs occur after less than 5% of hospitalizations among Medicare beneficiaries.3 Inpatient rehabilitation facilities provide intensive multidisciplinary inpatient rehabilitation care under the supervision of a rehabilitation physician. This physician must see their patients face-to-face at least 2–3 times weekly, although many do so with greater frequency. Inpatient rehabilitation facility patients typically receive 3 hrs of therapy daily, at least 5 days a week, and they must require at least two therapy disciplines. To qualify as an IRF, at least 60% of patients admitted must have 1 of 13 conditions identified by the Centers for Medicare and Medicaid Services.5
The IRFs and SNFs differ with regard to a number of key patient outcomes, as evidenced by data on Medicare beneficiaries who received postacute care in 2020, not limited to those who had COVID-19. Lengths of stay are typically longer among persons receiving SNF care. The average number of covered days per SNF admission was 26.5 days, whereas the average length of stay in IRFs was 12.9 days. Those who received care in SNFs were successfully discharged to a community setting at a lower rate (38.6%) than those who were admitted to IRFs (67.3%). Of note, unplanned hospitalization rates were also higher from SNFs (14.2%) than from IRFs (7.8%).4,5
Hospital readmission rates, long a target of cost-containment strategies, are a particularly important outcome of interest during a pandemic, when there is considerable need to preserve hospital capacity. Survivors of COVID-19 hospitalizations most often are readmitted to the hospital within 30 days of their discharge due to hypoxia, thromboembolism, or sepsis.6 Lavery et al.7 reported that 9% of surviving patients who were hospitalized for COVID-19 in the United States between March and July 2020 were readmitted to the same hospital within 2 mos of discharge.
Previous studies of survivors of COVID-19 hospitalizations have reported elevated readmission rates among persons discharged to rehabilitation facilities, without differentiating between the types of facilities. In their study on hospital readmissions among COVID-19 patients discharged from two New York City hospitals, Choi et al.8 reported that 13% of those who were readmitted within 30 days had been discharged to a rehabilitation facility, but they did not differentiate between SNFs and IRFs. Yeo et al.6 similarly combined SNFs and IRFs, as well as intermediate care facilities, in evaluating discharge disposition among persons with a readmission within 30 days of discharge after hospitalization for COVID-19. Their single-center study reported that more than a quarter of patients readmitted came from a facility rather than a community setting.
There have been few published studies reporting readmission rates among COVID-19 survivors specifically discharged to IRFs. Maltser et al.9 reported a wide range of readmission rates among COVID-19 patients discharged to the seven IRFs participating in the New York–New Jersey Rehabilitation Consortium, ranging from 0% to 25%. Their study, however, was completed early in the pandemic (May–June 2020) in a particularly hard-hit region. Olezene et al.10 reported three hospital readmissions among 29 consecutive patients admitted to an IRF after hospitalization for COVID-19, although it was noted that two of these cases were planned readmissions for surgical procedures to address pressure injuries. Piquet et al.11 reported that among 100 consecutive patients with COVID-19 admitted to an inpatient rehabilitation unit, only eight required transfer to acute care, despite a median age of 66 yrs and a high prevalence of comorbid conditions, including hypertension and diabetes mellitus. Abramoff et al.12 reported that 5 of 43 consecutive patients (12%) recovering from COVID-19 at their IRF required acute care rehospitalization. These observational studies included relatively small numbers of patients admitted to IRFs within the first year of the pandemic.
Unfortunately, there are limited national data that may be used to make comparisons between the groups of COVID-19 survivors discharged to SNFs and IRFs in the United States at this time. Nevertheless, such comparisons are necessary to better understand the utilization of these two types of postacute facilities by this patient population. They are also needed to inform future decisions regarding the optimal discharge location for persons hospitalized for COVID-19 infection in need of rehabilitation, particularly for those who are medically complex and/or survived critical illness.
The primary aim of this study was to test the hypothesis that persons hospitalized for COVID-19 infection discharged to IRFs are less likely than those discharged to SNFs to require hospital readmission, despite being more likely to have experienced more severe infections, as evidenced by the need for mechanical ventilation and/or intensive care. Accordingly, a key goal was to compare rates of hospital readmission among COVID-19 patients discharged to IRFs and SNFs. A secondary objective was to demonstrate important differences between the groups of patients discharged to these two different settings with regard to age, race, sex, and indicators of medical complexity and severity of illness. To evaluate these differences among a more representative sample of persons who were hospitalized for COVID-19, group statistics of persons discharged to the two settings from a convenience cohort of US academic medical centers (AMCs) and their affiliates were used for this preliminary study.
METHODS
Data Set
Data were retrospectively collected from 132 AMCs and their affiliate hospitals across the United States participating in the Vizient Clinical Data Base (CDB). Vizient CDB is a healthcare analytic platform designed to facilitate participating institutions’ performance improvement. It provides hospital-level data on patient demographics and on a number of key patient outcomes, including hospital readmission rates.13 Data were collected as part of an ongoing quality improvement (QI) initiative at the study team’s institution aimed at reducing hospital readmissions, in which the institution benchmarks itself against similar AMCs.
This study was approved by the authors’ institutional review board, and consent of patients whose data were extracted from the CDB was not required. The data from the CDB were used with permission of Vizient, Inc.
Study Population
All consecutive adult patients hospitalized for COVID-19 infection at hospitals participating in the Vizient CDB discharged to any SNF or IRF between April 1, 2020, and June 30, 2021 (total N = 39,882) were included.
Data Collection and Outcomes
The study team was provided summary statistics from their institution’s QI team, who extracted key elements from the Vizient CDB, for the two groups of patients, categorized by the type of postacute setting to which they were discharged (SNF or IRF). Data provided included the total number of patients discharged to the two types of settings during the period of interest, as well as the percentage who had been placed on mechanical ventilation, the percentage who received intensive care, and the percentage who were readmitted to acute care within 30 days of their hospital discharge.
Demographic data provided were limited to the age, sex, and racial composition of each group. It was not possible to determine the percentage of each group with Hispanic or Latino ethnicity. Individual-level data were not available to the study team; however, the mean age and hospital length of stay by participating AMC enabled determination of the median and SD among AMCs for these variables.
Determination of “Readmission”
Patients were considered to have had a hospital readmission if they were readmitted to the same hospital within 30 days of discharge.
Determination of Average Case Mix Index
The case mix index (CMI) was calculated by dividing the sum of the Medicare Severity-Diagnosis Related Group weights for each hospital inpatient discharge by the total number of these discharges.14
Statistical Analysis
Comparisons of the proportions of patients requiring readmission among the groups of interest were evaluated by χ2 analyses. χ2 analyses were also used to determine differences in the proportions of patients in each group (IRF vs. SNF) who required mechanical ventilation and/or intensive care during their acute care index hospitalizations. T tests were performed to compare age and hospital length of stay between the two groups of patients. A P value less than 0.05 was considered statistically significant. Statistical analyses were conducted using SPSS Version 25.0.15
RESULTS
A total of 301,330 individuals were hospitalized with COVID-19 infection at the participating medical centers between April 1, 2020, and June 30, 2021. Of these, 10.6% (31,941) were discharged to SNFs and 2.6% (7941) were discharged to IRFs. As seen in Table 1, the average age of patients discharged to SNFs (73 yrs, [95% confidence interval {CI}, 65.3–80.7]) was significantly higher than that of those discharged to IRFs (61 yrs [95% CI, 49.0–73.0], t = −214.2, P < 0.001). Accordingly, a greater percentage of patients discharged to SNFs (45%) had Medicare as their payer source compared with patients discharged to IRFs (27%). Males comprised 50% of the COVID-19 patients discharged to SNFs and 60% of those discharged to IRFs. The racial composition of the groups discharged to SNFs and IRFs was similar.
TABLE 1.
Characteristics of COVID-19 patients discharged to postacute care settings
| Discharge Location | |||
|---|---|---|---|
| Discharge Date—April 1, 2020–June 30, 2021 | SNF | IRF | T Test for Variable |
| No. cases | 31,941 | 7941 | |
| % of cases out of all COVID cases | 10.6% | 2.6% | |
| Age | |||
| Average | 73 yrs | 61 yrs | t = −214.24 |
| Median | 73.03 | 60.71 | P < 0.001 |
| SD | 3.95 | 6.12 | |
| 95% CI | 65.26–80.74 | 49.00–73.00 | 12.11–11.89 |
| Sex (% of male/female) | 50% M | 60% M | |
| 50% F | 40% F | ||
| Racial/ethnic background (% of race) | 2% Asian | 2% Asian | |
| 22% Black | 20% Black | ||
| 67% White | 68% White | ||
| 7% other | 7% other | ||
| 1% unavailable | 1% unavailable | ||
| 1% declined | 1% declined | ||
| Acute care case mix index (average) | 2.63 | 5.56 | |
| Hospital length of stay | |||
| Average days | 15.38 | 26.47 | t = 144.0 |
| Median | 14.98 | 25.17 | P < 0.001 |
| SD | 5.31 | 8.72 | |
| 95% CI | 4.97–25.79 | 9.38–43.56 | 10.94–11.24 |
| Payer (% of Medicare) | 45% | 27% | |
A number of metrics provide evidence that the group discharged to IRFs experienced more severe disease than those discharged to SNFs. As seen in Figure 1 and Table 2, a significantly higher percentage of patients discharged to IRFs required mechanical ventilation during their acute care index admission (χ2(1, 39,882) = 4169, P < 0.001) compared with those discharged to SNFs (45% and 13%, respectively). The group discharged to IRFs also demonstrated a higher likelihood of having received intensive care (χ2(1, 39,882) = 2919, P < 0.001) compared with their SNF counterparts (52.6% and 22.5%, respectively). The average acute hospital length of stay was significantly longer among patients discharged to IRFs (26.5 days, [9.4–43.6]) than among those discharged to SNFs (15.4 days, [CI, 5.0–25.8], t = 144, P < 0.001). The mean acute care case mix index of the IRF cohort (5.56) was more than twice as high as that of the SNF cohort (2.63), representing greater medical complexity among persons discharged to IRFs.
FIGURE 1.
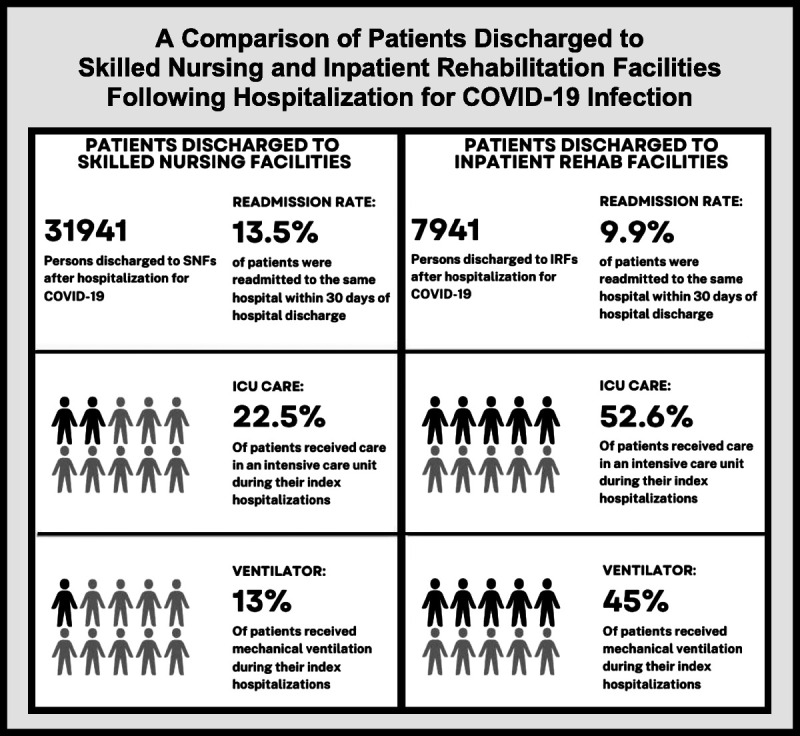
The percentages of patients discharged to rehabilitation facilities from participating AMCs after hospitalization with COVID-19 to IRFs who required mechanical ventilation, intensive care, and 30-day hospital readmission.
TABLE 2.
Contingency tables
| SNF (n = 31,941) | IRF (n = 7941) | χ2 (df) | |
|---|---|---|---|
| No. readmitted | 4296 (13.5%) | 783 (9.9%) | 73.7a (1) |
| No. not readmitted | 27,645 (86.5%) | 7158 (90.1%) | |
| No. ventilator | 4152 (13.0%) | 3573 (45.0%) | 4168.7a (1) |
| No. no ventilator | 27,789 (87.0%) | 4368 (55.0%) | |
| No. ICU | 7190 (22.5%) | 4174 (52.6%) | 2819.1a (1) |
| No. no ICU | 24,751 (77.5%) | 3767 (47.4%) |
a All analyses P < 0.001.
ICU, intensive care unit.
A χ2 test of independence was performed to examine the relationship between the type of postacute care setting and the likelihood of readmission after hospitalization for COVID-19. The relationship between these variables was significant, χ2(1, 39882) = 74, P < 0.001. Patients discharged to SNFs were 1.4 times [CI, 1.3–1.5] more likely to readmit to the same acute care hospital within 30 days than were patients discharged to IRFs.
DISCUSSION
This study is novel in that it makes use of a national, representative data set of persons hospitalized with COVID-19 in the United States who were discharged to SNFs and IRFs. Although the data provided to the study team did not include individual-level data that would enable multivariate analyses, it has yielded important information regarding the utilization of these facilities by survivors of COVID-19 as well as hospital readmission rates among those discharged to SNFs and IRFs. It also provides descriptive epidemiology of COVID-19 survivors receiving care in these facilities and enables a comparison between these populations.
More than 12% of persons hospitalized with COVID-19 infection at participating medical centers were discharged to rehabilitation facilities. Only a small percentage of patients in this cohort (2.6%) were discharged to IRFs. Anesi et al.16 reported that among their cohort of patients with COVID-19–related critical illness from a single multihospital health system, 12.2% were discharged to IRFs. Our finding of a much smaller percentage of patients discharged to IRFs in this cohort is likely due, in part, to broader inclusion criteria, not limited to survivors of critical illness. In addition, there may be geographical variation in referral patterns to IRFs, which are far fewer in number than SNFs in the United States.3 A number of other factors may have also contributed to a relatively low percentage of patients discharged to IRFs. The closure of hospital-based rehabilitation units to make room for surges of infected patients may have resulted in limited access to postacute care. Moreover, some patients may have declined services because of fears of reinfection, the need to remain masked, and/or visitor restrictions in rehabilitation facilities. In addition, early in the pandemic, some facilities did not accept patients who continued to test positive for COVID-19 despite no longer having symptoms due to infection control concerns. Particularly, deconditioned patients may also have been denied admission to IRFs because of their inability to tolerate the intensity of therapy services they provide.
As previously mentioned, reports have called attention to higher rates of hospital readmission among COVID-19 survivors discharged to rehabilitation facilities without differentiating between the types of such facilities.6,8 This preliminary exploration has demonstrated that key differences exist between the groups of patients discharged to SNFs and those discharged to IRFs. Accordingly, it is essential that future studies consider these discharge locations separately when evaluating patient outcomes, including readmission rates, among those recovering from COVID-19.
The average age of the group of patients discharged to SNFs was higher than that of the group discharged to IRFs. This may have been influenced by patients’ insurance benefits, as Americans 65 years and older are usually eligible for Medicare, which covers short-term SNF care after a hospital stay. An increased odds of readmission has been observed among persons 65 yrs or older after hospitalization for COVID-19.7 This may at least partially account for the higher readmission rate observed in the group of patients who received SNF care.
Another finding of note was that readmission rates among COVID-19 survivors from both postacute facility types compared favorably with previous available data concerning readmissions after hospitalization for influenza. Dobrzynski et al.17 reported a 14% readmission rate within 30 days of hospital discharge in their cohort of persons with influenza, which exceeds the readmission rates observed in COVID-19 survivors in both groups included in this study.
Most significantly, this study has shown that individuals admitted to IRFs after hospitalization with COVID-19 were more critically ill, had longer length of stays in the acute hospital, and were more medically complex, as measured by the case mix index. Nevertheless, these patients demonstrated a 1.4 times lower odds of readmission within 30 days of hospital discharge as compared with those who discharged to an SNF. This may speak to the benefit that IRFs provide medically complex patients. However, it is important to note that individuals without the potential to tolerate and benefit from intensive therapies are unlikely to be admitted to IRFs and such persons may be at higher risk for readmission because of reduced physiological reserve. Moreover, previous COVID-19 studies have reported unexpected associations between a shorter length of stay during the index hospitalization and a higher risk for readmission, as well as between admission to the intensive care unit and lower risk of readmission.7,18,19 Thus, it is possible that the lower readmission rate among patients discharged to IRFs may be due, at least in part, to differences in the acute care they received during their hospitalizations.
The avoidance of preventable hospital readmissions among patients in rehabilitation facilities is an important goal. Readmissions are a key performance measure used in Medicare’s value-based purchasing program. Acute care facilities that perform poorly on this metric may be subject to payment reductions.20 Moreover, transitions in care increase risk for medical errors and may provoke anxiety among patients and their families.21 An interruption in one’s rehabilitation course may also be conducive to a loss of functional gains achieved.22 Readmissions are particularly problematic during times of limited hospital capacity, as occurred at times during the pandemic, because they potentially detract limited resources away from other patients in need. Thus, it is important to identify patients at high risk for readmission and provide them with close medical supervision. Inpatient rehabilitation facilities provide close supervision by a rehabilitation physician, which may contribute to the lower readmission rate from such facilities when compared with SNFs. As the greater average expenditure for a stay in an IRF relative to one in an SNF has been heavily scrutinized, it is important to demonstrate the value that IRFs provide. Additional research is necessary to determine whether provision of this level of care reduces one’s risk for readmission and the impact of fewer preventable readmissions on health expenditures and other significant patient outcomes.
LIMITATIONS
This retrospective study makes use of a limited data set of group summary statistics from a cohort from AMCs, and as such, it has a number of limitations. First and foremost, the impact of potentially significant confounding variables on readmission rates could not be assessed using data from this national sample. In their study of COVID-19 survivors, Yeo et al.6 reported higher readmission rates among individuals with an elevated peak serum creatinine level and those with a body mass index of less than 18.5. Neither serum laboratory values nor body mass index was reported in the data set used for this study. Moreover, they also found higher rates of readmission among COVID-19 patients with the comorbidities of hypertension, diabetes mellitus, and congestive heart failure. Lavery et al.7 similarly reported higher odds of readmission among those with heart failure or diabetes, as well as those with chronic obstructive pulmonary disease or chronic kidney disease. The prevalence analysis of these comorbidities among the patients was beyond the scope of this investigation.
The impact of demographic variables, including sex and race, on hospital readmission rates, similarly could not be assessed. Moreover, the utilization of rehabilitation facilities by COVID-19 survivors who identify as Hispanic or Latino could not be determined because of limitations in how data concerning race were reported in the data set used. Information regarding patients’ premorbid living environment was not obtained. Some persons discharged to SNF may have been receiving long-term care within an SNF before their hospitalizations.
Another potential limitation is the possibility of undercounting readmissions due to failure to capture those cases in which patients were admitted to a different hospital than the one from which they were discharged. Patients discharged to rehabilitation facilities may be transferred to the acute care facility nearest to their SNF or IRF in the event of a medical emergency, rather than the referring hospital. Readmission to a different hospital may also be likely in the event of the need to divert cases because of a lack of available hospital beds.
Another potential limitation is the use of the group CMI as a measure of medical complexity. A more complex and resource-intensive caseload is typically reflected in a higher CMI. Nevertheless, a number of other tools may be used to more comprehensively capture the complexity of a group of rehabilitation patients, including measures of functional independence.
It is also possible that there may be variability in the patient mix and/or outcomes among facilities falling within the same type of postacute care setting, which we were unable to evaluate. In urban and suburban regions, there are often multiple SNFs and IRFs from which a patient may choose. These may vary with regard to the services they provide and resources they have available. The frequency of physician visits, intensity of rehabilitation, and the availability of respiratory therapy all, for example, can vary from one facility to the next. Accordingly, while readmission rates among patients in this cohort discharged to SNFs are relatively high, the rate from an individual SNF may not be. Moreover, variability in rates of readmission among COVID-19 patients from IRFs was previously reported by Maltser et al.9
Lastly, it is unclear as to what role limited hospital bed capacity during local surges in cases may have played in suppressing hospital readmissions during the pandemic, particularly from IRFs. For example, the authors observed that physicians in a particular area code IRF faced difficulty transferring patients back to acute care because of limited bed availability during a local surge in cases in the summer of 2020. As such, the physicians managed some medical emergencies in the IRF that would usually have resulted in the patients’ return to acute care. The ability of IRFs to safely provide high acuity medical care during a pandemic is an important consideration when hospital bed capacity is limited and should be further evaluated.
CONCLUSIONS
Thousands of individuals have received postacute care services after hospitalization for COVID-19 infection in skilled nursing or IRFs in the United States. Those who received care in IRFs had, on average, longer hospitalizations than those discharged to SNFs and were more likely to have received intensive care, but had a lower rate of readmission to the hospital. This may be due in part to the younger average age among persons discharged to IRFs. This study highlights the importance of distinguishing between facility types in evaluating outcomes among those recovering from COVID-19 in postacute care settings. Additional research is necessary to determine whether care in an IRF may prevent hospital readmission after COVID-19 infection. The results of such studies may add to the growing body of literature demonstrating benefits of care in an IRF as part of ongoing care for survivors of severe COVID-19 infections. Moreover, they may inform planning for future pandemics with regard to optimal postacute care placement during times of limited available hospital capacity.
Footnotes
Presented as an e-poster at the Virtual Annual Assembly of the AAPM&R, November 2021.
This article makes use of a larger data set with data from multiple institutions across the country.
Financial disclosure statements have been obtained, and no conflicts of interest have been reported by the authors or by any individuals in control of the content of this article.
Contributor Information
Adriana D. Valbuena Valecillos, Email: ADV20@med.miami.edu.
Joslyn Gober, Email: jfg101@med.miami.edu.
Doug Johnson-Greene, Email: DJGreene@med.miami.edu.
Lauren T. Shapiro, Email: lxs973@med.miami.edu.
REFERENCES
- 1.Roberts P Wertheimer J Park E, et al. : Identification of functional limitations and discharge destination in patients with COVID-19. Arch Phys Med Rehabil 2021;102:351–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vizient : Clinical DATA BASE. Available at: https://www.vizientinc.com. Data approved for publication on February 15, 2022 [Google Scholar]
- 3.Medicare Payment Advisory Commission : Post-acute care, in: Health Care Spending and the Medicare Program. Washington, DC, MedPAC, 2022:95–111 [Google Scholar]
- 4.Medicare Payment Advisory Commission : Skilled nursing facility services, in: March 2022 Report to the Congress: Medicare Payment Policy. Washington, DC, MedPAC, 2022:233–66 [Google Scholar]
- 5.Medicare Payment Advisory Commission : Inpatient rehabilitation facility services, in: March 2022 Report to the Congress: Medicare Payment Policy. Washington, DC, MedPAC, 2022:303–29 [Google Scholar]
- 6.Yeo I Baek S Kim J, et al. : Assessment of thirty-day readmission rate, timing, causes and predictors after hospitalization with COVID-19. J Intern Med 2021;290:157–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lavery AM Preston LE Ko JY, et al. : Characteristics of hospitalized COVID-19 patients discharged and experiencing same-hospital readmission—United States, March–August 2020. MMWR Morb Mortal Wkly Rep 2020;69:1695–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choi JJ Contractor JH Shaw AL, et al. : COVID-19-related circumstances for hospital readmissions: a case series from 2 New York City hospitals. J Patient Saf 2021;17:264–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maltser S Trovato E Fusco HN, et al. : Challenges and lessons learned for acute inpatient rehabilitation of persons with COVID-19: clinical presentation, assessment, needs, and services utilization. Am J Phys Med Rehabil 2021;100:1115–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olezene CS Hansen E Steere HK, et al. : Functional outcomes in the inpatient rehabilitation setting following severe COVID-19 infection. PLoS One 2021;16:e0248824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Piquet V Luczak C Seiler F, et al. Covid Rehabilitation Study Group : Do patients with COVID-19 benefit from rehabilitation? Functional outcomes of the first 100 patients in a COVID-19 rehabilitation unit. Arch Phys Med Rehabil 2021;102:1067–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abramoff BA Dillingham TR Caldera FE, et al. : Inpatient rehabilitation outcomes after severe COVID-19 infections: a retrospective cohort study. Am J Phys Med Rehabil 2021;100:1109–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vizient : Clinical DATA BASE. Available at: https://www.vizientinc.com/what-we-do/operations-and-quality/clinical-data-base. Accessed October 9, 2022
- 14.Date.gov : Case mix index. Available at: https://catalog.data.gov/dataset/case-mix-index. Published August 7, 2021. Accessed October 9, 2022
- 15.IBM Corp : IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY, IBM Corp, 2017 [Google Scholar]
- 16.Anesi GL Jablonski J Harhay MO, et al. : Characteristics, outcomes, and trends of patients with COVID-19–related critical illness at a learning health system in the United States. Ann Intern Med 2021;174:613–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dobrzynski DM Ndi DN Zhu Y, et al. : Hospital readmissions after laboratory-confirmed influenza hospitalization. J Infect Dis 2020;222:583–9 [DOI] [PubMed] [Google Scholar]
- 18.Ramos-Martínez A Parra-Ramírez LM Morrás I, et al. : Frequency, risk factors, and outcomes of hospital readmissions of COVID-19 patients. Sci Rep 2021;11:13733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Somani SS Richter F Fuster V, et al. : Characterization of patients who return to hospital following discharge from hospitalization for COVID-19. J Gen Intern Med 2020;35:2838–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hospital Readmissions Reduction Program (HRRP) : Centers for Medicare & Medicaid Services. Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program. Published August 5, 2022. Accessed October 9, 2022
- 21.Coleman EA: Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc 2003;51:549–55 [DOI] [PubMed] [Google Scholar]
- 22.Shea CA Turcu R Wong BS, et al. : Variation in 30-day readmission rates from inpatient rehabilitation facilities to acute care hospitals. J Am Med Dir Assoc 2021;22:2461–7 [DOI] [PMC free article] [PubMed] [Google Scholar]


