Abstract
Background and Aim
Nursing reports are necessary for clinical communication and provide an accurate reflection of nursing assessments, care provided, changes in clinical status, and patient‐related information to support the multidisciplinary team to provide individualized care. Nurses always face challenges in recording and documenting nursing reports. Speech recognition systems (SRS), as one of the documentation technologies, can play a potential role in recording medical reports. Therefore, this study seeks to identify the barriers, benefits, and facilitators of utilizing speech recognition technology in nursing reports.
Materials and Methods
This cross‐sectional was conducted through a researcher‐made questionnaire in 2022. Invitations were sent to 200 ICU nurses working in the three educational hospitals of Imam Reza (AS), Qaem and Imam Zaman in Mashhad city (Iran), 125 of whom accepted our invitation. Finally, 73 nurses included the study based on inclusion and exclusion criteria. Data analysis was performed using SPSS 22.0.
Results
According to the nurses, “paperwork reduction” (3.96, ±1.96), “performance improvement” (3.96, ±0.93), and “cost reduction” (3.95, ±1.07) were the most common benefits of using the SRS. “Lack of specialized, technical, and experienced staff to teach nurses how to work with speech recognition systems” (3.59, ±1.18), “insufficient training of nurses” (3.59, ±1.11), and “need to edit and control quality and correct documents” (3.59, ±1.03) were the most common barriers to using SRS. As well as “ability to fully review documentation processes” (3.62, ±1.13), “creation of integrated data in record documentation” (3.58, ±1.15), “possibility of error correction for nurses” (3.51, ±1.16) were the most common facilitators. There was no significant relationship between nurses' demographic information and the benefits, barriers, and facilitators.
Conclusions
By providing information on the benefits, barriers, and facilitators of using this technology, hospital managers, nursing managers, and information technology managers of healthcare centers can make more informed decisions in selecting and implementing SRS for nursing report documentation. This will help to avoid potential challenges that may reduce the efficiency, effectiveness, and productivity of the systems.
Keywords: barriers, benefits, documenting nursing reports, facilitators, speech recognition system
1. BACKGROUND
Documentation is one of the processes in the field of nursing care that is planned and provided by nurses or with their help. 1 Nurses, as one of the most important groups in the field of healthcare, face barriers in terms of clinical information, diversity, and a large amount of data in the documentation of clinical records. 2 , 3 Other barriers reported by nurses include insufficient time, shortage of nurses in clinical wards, insufficient knowledge about the importance of documents, insufficient document sheets, patient burden, and lack of in‐service training on clinical documents. 5 , 6 , 7 Although nurses spend more than 30% of their time documenting clinical records, 8 nursing records are often incomplete 9 , 10 and do not have sufficient, accuracy and quality. 11 , 12
Using speech recognition (SR) systems is one way to overcome the barriers to recording clinical reports. They are a subset of artificial intelligence that automatically detect sound and translate it into text. 13 , 14 , 15 , 16 SR systems can be used to easily generate medical reports, reduce their rotation time and cost of transcribing, and improve the productivity of medical records. 17 In addition, the use of these technology can help nurses record and access verbal data in a timely manner, prevent information loss, simultaneously document care processes, data better sending, improve workflow (save and reduce documentation time), and help reduce the registration of incorrect information. 18 , 19 , 20 , 21 A study by Migowa et al., 22 showed that the SR system reduces medication errors and it has the greatest effect on reducing incorrect drug doses. Another study 23 demonstrated that clinical records documentation with a SR system saves time, increases efficiency, and speeds up the recording of more detailed information.
These systems in addition to many benefits of nursing reports documentation may have barriers. Software failure, inaccuracy in audio transcription, variety of equipment, unstructured training approaches, and nurse doubts about using this technology are among the barriers of using this system. 18 , 21 , 24 In addition to the benefits and barriers, SR systems have facilitators that can make it easier and more user‐friendly to use these systems. 18 , 25
In Iran in 2003, nursing documentation quality was found to be high in some cases when using hospital information systems (HIS). To further improve it, a SR system was suggested and implemented in some clinical departments using professional software such as Nevisa and Speechtexter. Although these software programs had higher accuracy, they generated more errors than the paper‐based method. The errors were subsequently reduced by optimizing and upgrading the software. 26 Currently, nursing documentation and reporting tools are used as a part of HIS to record nursing reports and documents.
To our knowledge, various studies have been conducted in the field of SR systems, 27 , 28 , 29 but none of these studies have specifically focused on the benefits, barriers, and facilitators of the use of SR technology nursing documentation and reporting. Hayt et al. 30 investigated the advantages and disadvantages of implementing PACS and SR systems. They concluded that using SR systems for documentation can help reduce wait times for doctors and patients. By studying the impact of SR technology in healthcare departments, Parente et al. 31 found that SR technology can be highly advantageous for healthcare providers who need to create documents at the patient's bedside. Moreover, a Persian article discussed some benefits, barriers, and facilitators of SR technology in nursing documentation, although the study focused on a limited number of these factors. 32 Therefore, this study aimed to identify the barriers, benefits, and facilitators of using SR technology in documenting nursing reports.
2. MATERIALS AND METHODS
2.1. Study design and settings
This cross‐sectional was conducted in the educational hospitals of Imam Reza (AS), Qaem, and Imam Zaman affiliated with Mashhad University of Medical Sciences in Khorasan Razavi Province, Iran. The study was reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline (see Supporting Information: File 1).
2.2. Participants
A convenience sampling method was used to data collection. Two hundred ICU nurses working in the three selected hospitals were invited to participate in the study. Convenience sampling is a type of nonrandom or non‐probability sampling method that involves selecting members of a target population who meet certain practical criteria, such as easy accessibility, availability at a specific time, geographic proximity, or willingness to participate, for inclusion in a study. This method is often used in social research to select subjects who are readily available to the researcher, and who can all be included in the study study. 33
In order for nurses to participate in the study, an invitation was sent to all 200 nurses through social networks (WhatsApp or Telegram). Out of the 200 nurses, 125 accepted our invitation. Finally, 73 nurses were selected to participate in the study based on the inclusion and exclusion criteria (as shown in Figure 1).
Figure 1.
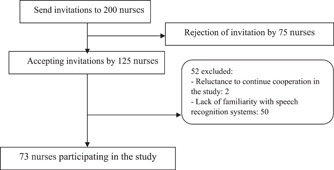
Study recruitment flow diagram.
2.3. Inclusion and exclusion criteria
The inclusion criteria for the study were as follows: having at least a bachelor's degree in nursing, being able to work with computers and having familiarity with SR systems, and providing informed consent to participate in the study. Furthermore, the exclusion criterion was reluctance to continue cooperation in the study.
2.4. Data collection tools
To collect data, we designed a questionnaire. To create a questionnaire, first, the sources related to the barriers, benefits, and facilitators of using SR technology in documenting nursing reports were studied. 18 , 19 , 21 , 34 , 35 , 36 , 37 , 38 , 39 , 40 Then, a questionnaire was designed by extracting information from studies and using the experiences and opinions of two nurses with a history of using SR systems. The questionnaire was divided into three parts. The first part included four questions about demographic information. The second part consisted of a single question about the participants' level of familiarity with the SR system. The third part was composed of 52 questions about the benefits, barriers, and facilitators of the SR system. Additionally, an open‐ended question was included to allow participants to provide any additional comments.
The questions were based on a 5‐point Likert scale ranging from “strongly disagree” to “strongly agree.” The validity of the questionnaire was evaluated and confirmed by 5 health information management (2 people) and medical informatics (3 people). To confirm the reliability of the questionnaire, we asked 30 ICU nurses to complete it. We then used Cronbach's ⍺ to assess the questionnaire's reliability, which was determined to be 0.93. Notably, these nurses were distinct from the main sample used in the study.
After confirming the validity and reliability, the questionnaire was copied in a paper. Also, for those nurses who could not distribute the questionnaire in the paper, the questionnaire was designed electronically by Google Forms.
To collect information, first, the researcher went to the hospitals to provide the necessary explanations on how to complete the questionnaire and the objectives of the study for each participant. Then, the questionnaire was distributed and collected among them by the researcher. For nurses who could not be accessed to distribute the questionnaire, after providing a full explanation of the various sections of the questionnaire by phone, the questionnaire was sent electronically. The process of distributing and completing questionnaires took from February 2022 to May 2022.
2.5. Statistical analysis
Descriptive statistics indices (mean and standard deviation and percentage) were used for qualitative variables to examine the relationship between demographic information (age, gender, level of education, work experience). Also, to analyze the relationship between nurses' demographic information and the benefits, barriers, and facilitators of using SR system, T‐test and Kruskal−Wallis tests were used at a significant level (p > 0.05). Data analysis was performed using SPSS version 22.0.
3. RESULTS
Table 1 shows the demographic information of the nurses participating in the study. The frequency of men was higher than women (58.9%). More than half of the nurses were 25−35 years old (52.1%). Most of them had a bachelor's degree (90.4%).
Table 1.
Participants' demographics.
| Variables | Frequency (percent) | |
|---|---|---|
| Sex | Male | 43 (58.9) |
| Female | 30 (41.1) | |
| Age | 25−35 | 38 (52.1) |
| 36−45 | 26 (35.6) | |
| >45 | 9 (12.3) | |
| Education level | Associate | 3 (4.1) |
| Bachelor | 66 (90.4) | |
| Master and doctoral | 4 (5.5) | |
| Work experience | <5 | 23 (31.5) |
| 5−15 | 34 (46.6) | |
| >15 | 16 (21.9) | |
According to Table 2, there was no significant relationship between nurses' demographic information and the advantages, disadvantages, and facilitators of the SR system. However, nurses aged 45−36 (3.92, ±0.65), female nurses (3.88, ±0.70), married nurses (3.79, ±0.79), those with a postgraduate degree (4.07, ±0.54), and those with less work experience (3.98, ±0.65) benefited more from these systems compared to other age groups, male nurses, single nurses, nurses with diploma qualifications, and those with more work experience.
Table 2.
Advantages, barriers, and facilitators of using speech recognition system based on demographic information.
| Variables | Advantages mean (±SD) | p Value | Barriers mean (±SD) | p Value | Facilitators mean (±SD) | p Value |
|---|---|---|---|---|---|---|
| Age group | ||||||
| 25−35 | 3.70 (±0.77) | 0.418 | 3.35 (±0.94) | 0.525 | 3.44 (±1.08) | 0.552 |
| 36−45 | 3.92 (±0.65) | 3.35 (±0.74) | 3.41 (±1.00) | |||
| >45 | 3.62 (±0.91) | 3.71 (±0.90) | 3.83 (±1.03) | |||
| Sex | ||||||
| Male | 3.70 (±0.77) | 0.386 | 3.49 (±0.75) | 0.103 | 3.57 (±0.88) | 0.040 |
| Female | 3.88 (±0.70) | 3.27 (±1.01) | 3.34 (±1.23) | |||
| Marital status | ||||||
| Single | 3.71 (±0.51) | 0.195 | 3.45 (±0.55) | 0.092 | 3.53 (±0.71) | 0.159 |
| Married | 3.78 (±0.79) | 3.38 (±0.92) | 3.47 (±1.10) | |||
| Education level | ||||||
| Associate degree | 3.09 (±1.00) | 0.215 | 3.09 (±1.01) | 0.753 | 2.96 (±1.32) | 0.575 |
| Bachelor's degree | 3.78 (±0.74) | 3.40 (±0.87) | 3.48 (±1.03) | |||
| Master's degree | 4.07 (±0.54) | 3.60 (±0.74) | 3.80 (±1.18) | |||
| Work experience | ||||||
| <5 | 3.98 (±0.65) | 0.248 | 3.37 (±0.67) | 0.722 | 3.80 (±0.77) | 0.061 |
| 5−15 | 3.73 (±0.75) | 3.35 (±0.94) | 3.18 (±1.01) | |||
Nurses older than 45 years (3.71, ±0.90), male nurses (3.49, ±0.75), single nurses (3.45, ±0.55), and nurses with postgraduate education (3.60, ±0.74) with more than 15 years of experience (3.56, ±0.99) mostly were faced with barriers of the SR system.
Nurses older than 45 years (3.83, ±1.03), male nurses (3.57, ±0.88), single nurses (3.53, ±0.71), nurses with postgraduate level (3.80, ±1.18), and nurses with less than 5 years of experience (3.80, ±0.77) were more familiar with the SR system facilitators than other people.
As shown in Table 3, nurses believed that the most common benefits of using SR systems were “paperwork reduction” (3.96, ±1.03), “performance improvement (efficiency, speed, and accuracy in work)” (3.96, ±0.93), and “cost reduction” (3.95, ±1.07).
Table 3.
The most common benefits of using speech recognition systems in nursing reports documentation from the nurses' perspective.
| Row | Advantages | Mean (±SD) |
|---|---|---|
| 1 | Paperwork reduction | 3.96 (±1.13) |
| 2 | Performance improvement (efficiency, speed, and accuracy in work) | 3.96 (±0.93) |
| 3 | Cost reduction | 3.95 (±1.07) |
| 4 | Saving and reduce documentation time | 3.90 (±0.96) |
| 5 | Better programming for shift delivery | 3.88 (±1.11) |
| 6 | better sharing of clinical data and information | 3.88 (±0.99) |
| 7 | Increase the accuracy and precision in documenting | 3.86 (±1.05) |
| 8 | Quick access of nurses and other treatment staff to patients' clinical records | 3.82 (±1.07) |
| 9 | Improve communication between different departments inside and outside the organization through easy exchange of documents and easy communication between medical staff | 3.81 (±1.08) |
| 10 | Accelerate in care process | 3.79 (±0.94) |
| 11 | finding information among medical reports with fast search capability | 3.77 (±0.92) |
| 12 | Nurses' satisfaction of system using | 3.77 (±0.92) |
| 13 | Real‐time registration of medical information (documentation and collection of medical care data at the time of care delivery) | 3.75 (±0.99) |
| 14 | Quick and timely decision making (improving productivity) | 3.73 (±0.99) |
| 15 | Reminding nurses of various processes and giving them specific instructions | 3.67 (±0.88) |
| 16 | Saving data entry time | 0.84 (±2.95) |
The most common barriers in using SR systems from the nurses' point of view are “lack of specialized, technical, and experienced staff to teach nurses how to work with SR systems” (3.59, ±1.18), “inadequate training of nurses” (3.59, ±1.11), and the “need to edit and control the quality and modification of documents” (3.59, ±1.03). These barriers are shown in Table 4.
Table 4.
The most common barriers of using speech recognition systems in nursing reports documentation from the nurses' perspective.
| Row | Barriers | Mean (±SD) |
|---|---|---|
| 1 | Lack of specialized, technical, and experienced staff to teach nurses how to work with speech recognition systems | 3.59 (±1.18) |
| 2 | Inadequate training of nurses | 3.59 (±1.11) |
| 3 | Need to edit and control the quality and modification of documents | 3.59 (±1.03) |
| 4 | Hardware and software problems (systemic and technical issues and errors, low system speed, etc.) | 3.52 (±1.04) |
| 5 | Infrastructure problems related to network and Internet | 3.51 (±1.06) |
| 6 | Negative attitudes of policymakers, senior managers, and nurses about speech recognition technology | 3.51 (±1.06) |
| 7 | Cost of implementation and application of these systems in health organizations | 3.49 (±1.15) |
| 8 | Lack of interaction between providers and patients | 3.48 (±1.14) |
| 9 | Insufficient support of senior managers of using the system in health organizations | 3.48 (±1.11) |
| 10 | Concerns about insufficient transcript accuracy (error increase) | 3.45 (±1.15) |
| 11 | Lack of time for nurses to use the system because of clinical workload | 3.43 (±1.11) |
| 12 | Decrees of accuracy of speech recognition software (effect of accent, slang, and women's voice) | 3.41 (±1.03) |
| 13 | Nurses' resistance to using speech recognition systems | 3.40 (±1.11) |
| 14 | Environmental noise when nurses use the system | 3.40 (±1.07) |
| 15 | Problem accessing clinical information and reported clinical records and searching for information after registration | 3.39 (±1.11) |
| 16 | Incompatibility of speech recognition systems with hospital information system (HIS) and its subsystems | 3.37 (±1.11) |
| 17 | Delay in documentation (increase the time) | 3.33 (±1.20) |
| 18 | Lack of participation of nurses in designing of speech recognition systems | 3.32 (±1.09) |
| 19 | Using abbreviations in system | 3.29 (±1.13) |
| 20 | Dissatisfaction in meeting expectations | 3.29 (± 1.08) |
| 21 | Increase in nurses' workload | 3.14 (±1.24) |
| 22 | Insufficient users' skills to work with speech recognition systems | 2.92 (±0.86) |
| 23 | Nurses' uncertainty about the usefulness of speech recognition systems | 2.23 (±1.07) |
As Table 5 shows, “ability to fully review documentation processes in system” (3.62, ±1.13), “integrated data creation in documentation” (3.58, ±1.15), and “error correction for nurses” (3.51, ±1.16) were the most common facilitators of using SR systems in documenting nursing reports from nurses' perspective.
Table 5.
The most common facilitators of using speech recognition systems in documenting nursing reports from the nurse's perspective.
| Row | Facilitators | Mean (±SD) |
|---|---|---|
| 1 | Ability to fully review the documentation processes in system | 3.62 (±1.13) |
| 2 | Create integrated data in documentation | 3.58 (±1.15) |
| 3 | Correct errors for nurses | 3.51 (±1.16) |
| 4 | Adaptation to nurses' speech | 3.48 (±1.18) |
| 5 | Adequate training on how to work with speech recognition systems for nurses | 3.48 (±1.13) |
| 6 | Backing up data and the ability to recover and edit of data | 3.47 (±1.15) |
| 7 | Strong technical support team | 3.44 (±1.29) |
| 8 | Use of suitable recording equipment (portable and noise absorber) | 3.40 (±1.17) |
| 9 | Improve nurses' understanding of system (benefits and experience) | 3.38 (±1.17) |
4. DISCUSSION
The present study examines the advantages, barriers, and facilitators of using SR technology in the documentation of nursing reports from the perspective of nurses.
4.1. Advantages of using SR technology in documentation of nursing reports
Findings of the present study and other studies 18 , 19 , 21 , 35 , 36 , 41 have shown that SR systems offer advantages in documenting clinical documents. These benefits include improved performance (efficiency, speed, and accuracy of work), continuity of care, nurses' willingness to use, timely and improved decision making, improved productivity (improved communication, improved shift delivery, reduced costs, and availability of documents), simultaneous documentation, transfer, and transmission of data, and improved and accurate documentation. Another advantage of using SR systems in clinical departments and document registration is the improvement of performance (efficiency, speed, and accuracy in doing work). 42 , 43 It seems that if the registration of clinical documents by this system is done faster than manual typing, the overall performance of clinical care systems will be improved because healthcare system staff will have more time to handle patients' clinical affairs. 43
Rana et al. 44 proposed SR system as a suitable method for recording clinical documents by radiologists and concluded that SR system can increase the speed of clinical document production and save radiologists time (time). Vogel et al. 45 also introduced the SR system as a meaningful and effective tool for the clinical documentation process. They also believed that the SR system speeds up the clinical documentation process compared to manual typing. Another study 29 examined the role of SR technology in documenting physicians. The results of this study showed that physicians had positive opinions about the effect of the SR system on workflow and the efficiency of clinical document registration. 78.8% of physicians were satisfied with the SR system and 77.2% agreed that the SR system has improved the performance and efficiency of recording their clinical records. 29
“Saving and reducing documentation time” is another advantage of SR systems. Hodgson et al. 46 showed that for recording clinical documents, such as radiological results reporting, a SR system can reduce the overall time of recording clinical documents compared to manual typing. Singh et al. 47 also proved that the SR system saves time in documenting clinical documents in Surgical Pathology. Thus, if it took 4 days to register clinical documents in the usual way, this time was reduced to 3 days by using this system. “increasing nurses' satisfaction with the use of the system” is another benefit of SR systems. In another study, 48 physicians' expectations and experience before and after of using SR technology were examined. According to a survey conducted before the study, 82% of physicians were optimistic about using this technology. After using this technology for 6 months, 87% of physicians agreed that SR technology is a good idea and meets expectations. More than half of the doctors agreed that this system could save time. They also believed that implementing a cost‐effective SR system would remove the additional financial burden from healthcare systems. Some studies 17 , 49 have also shown that the design and implementation of SR systems for documenting clinical records in healthcare systems are cost‐effective, as accurate as traditional transcriptions, and greatly shorten the recording time of various clinical processes. Koivikko et al. 50 also concluded that after the use of SR system by radiologists to record radiology reports, the SR system accelerates the process of patient care, saves and reduces documentation time, improves productivity and efficiency, and increase end user satisfaction.
Finally, it should be noted that the benefits of SR systems in clinical wards for recording clinical documents make the system easier to use, better system acceptance, more willing of nurses to use and work with the system, reduce resistance to the use of systems, improve communication and thus improving the level of welfare, comfort as well as facilitating the clinical affairs of nurses.
4.2. Barriers of using SR technology in documenting nursing reports
Each technology, along with its benefits for users has some barriers. A SR system like other systems always faces barriers. Decreased accuracy of SR software (effect of accent, slang, and women's voice), environmental noise, hardware and software reliability problems, systemic and technical issues and errors (need to edit and control quality and modify documents), need to edit documents (inadequate training in data and information security issues), concerns about information confidentiality by using technology (dissatisfaction with meeting expectations, problems with the use of abbreviations), concerns about the accuracy of transcripts, implementation costs, lack of interaction between providers and patients, delays in documentation due to inappropriate tools, and lack of technology acceptance (resistance to audio recording, change of work style, and older age of the user) are among the barriers expressed in the present study and various other studies 18 , 20 , 21 , 35 , 36 , 41 , 51
Many studies 49 , 52 , 53 , 54 , 55 have shown that SR systems spend more time on “editing, quality control, and correction of documents” than when reports and clinical documents are written in a traditional, manual manner. Currently, the only standard for editing as well as ensuring the accuracy of clinical documents after using the SR system is editing by a third party (editor) (human transcriptionist). Editing by a third party (editor) must be done with great care. Moreover, after editing, the documents must be approved by experts. It should also be noted that text editing by a third party (editor) in addition to time, costs a lot of money for healthcare organizations. 56
Using of SR system should be able to estimate the expectations of users in clinical departments such as other information technology systems. If this system meets the expectations of users, people will be more inclined to use the system. In a study by Alapetite et al. 57 that examined physicians' expectations of a SR system, 33% of physicians identified the system as a suitable technology for documenting clinical documents. Thirty‐one percent thought it was not a good technology and would not meet expectations, and 36% did not comment specifically on the use of the system. But after months of using the system, doctors report a more negative view of the system. Because the system did not meet their expectations in practice, they spent much more time in documenting medical records, and correcting errors in documenting clinical records than before. Furthermore, the overall quality of clinical documents was reduced using the SR system.
One of the barriers for the SR system is “nurses' resistance to using SR systems.” Employees' resistance of using technology and insistence on using traditional methods cause the loss of data in clinical records and inconsistencies in setting up, implementing, and executing the new system, failing to meet information needs within the organization and outside the organization, and lack of proper response to patients and senior officials in healthcare systems. Various studies have shown 59 , 60 that training and support of senior managers are important for the successful implementation of new technologies and overcoming employee resistance to system use. Therefore, it is better, for hospital managers and senior executives, to hold training sessions of using of the SR systems, to justify nurses. In this way, they can offer solutions to the nurses' resistance in using new technologies, including SR systems, through multiple sessions. Managers can also provide incentives for nurses. Other barriers to SR systems include “reduction in the accuracy of SR software” (effect of accent, slang, and femininity). Accuracy of SR software depends on accent, tone of voice (male and female), spoken language, loudness and shortness of speech, as well as the complexity and simplicity of sentences, may vary. Suominen et al., 20 showed that recognition of speech and accent by SR system software is one of the barriers of these systems. Accent recognition in this study was more difficult than the mother tongue, and SR software usually recognized the male speaker better than the female speaker. By using simple and short sentences, we can overcome this barriers. 61 Artificial intelligence technology can also be used to identify different accents and dialects. Another barrier to implementing this system is the “concern about sufficient transcription accuracy (increased error).” Chang et al., 62 to understand the accuracy of SR systems radiological reports divided it into two categories: computer radiography (CR = plain film) and non‐CR (ultrasound, computed tomography, magnetic resonance imaging, nuclear medicine, and angiographic examinations). Of the 379 final CR reports and 631 final non‐CR reports, 11% of the CR group reports had errors. Two percent of these reports contained inappropriate phrases. Thirty‐six percent of the reports in the non‐CR group had errors, and of these, 5% contained inappropriate expressions. In this study, they stated that increasing the awareness of the error rate will help to reduce the error rate and also to balance the quality and speed of the reports produced. Another study 63 showed that reports recorded by radiologists using a SR system were associated with errors. But these errors decreased over time. The study by Clarke et al. 40 also showed that after documenting clinical documents, more than half of the participants experienced an increase in spelling and grammatical errors.
In the study of Pezzullo et al., 55 barriers were identified by radiologists after using the SR system. Radiologists say the system increases user fatigue. They concluded that recording clinical records by using this system for radiology reports was error‐prone and would increase costs compared to manual typing. In another study, 13 the effect of SR systems on the creation of electronic progress note (ePN) documents by physicians was investigated. Users stated that the SR system had no clear perceived advantages in terms of data entry time, quality of care, quality of documentation, or impact on clinical and administrative workflow. In general, barriers to SR systems in clinical wards for recording clinical documents cause additional costs, wasting nurses time, less system acceptance, less willingness of nurses to use, increasing nurses resistance to using the system, reducing communication, reducing efficiency and effectiveness, decreased security, and confidentiality. Therefore, if the barriers of this system are not removed in time, these systems may be abandoned and obsolete.
It should be noted that with the emergence of continuous real‐time voice recognition software, it is possible to draw charts related to patients' symptoms in an accurate, fast, legible, and complete manner with a very low cost for each chart. 29 , 49 However, one of the challenges of SR systems is the accuracy of recording charts and images that are in the clinical reports of patients' files. Some studies 64 , 65 , 66 have pointed out this challenge and stated that the reports of charts and images recorded using this technology have many errors. Robert et al. 49 showed that the error rate of drawing diagrams using a SR system is 1.3% higher than drawing diagrams by hand. Natural language processing and text mining can be used to solve this challenge. Other studies have shown 67 , 68 that the transfer of imaging reports and chart reports recorded by nurses to electronic medical record systems and HIS systems creates problems when updating, integrating, and sharing image data and charts. These problems include heterogeneity of the formats of recorded data in visual and graphical reports. One reason for the heterogeneity of these formats is that imaging reports and charts usually do not have a specific structure and use free language to record. Artificial intelligence engines are a computer‐based approach to analyzing text, charts, and images, and can be used to automate this task alongside SR systems. 67
Moreover, it is important to note that the charting process may vary between hospital departments, and should be taken into consideration when discussing the challenges faced by nurses in documenting patient information. 26 , 69 Overall, addressing these challenges and improving nursing documentation practices can lead to better patient care, increased accuracy in record‐keeping, and more efficient workflow for nurses.
4.3. Facilitators of the use of SR technology in documenting nursing reports
According to the findings of the present study and various studies 18 , 19 , 20 , 35 , 51 adequate training, integrated data creation, improving nurses understanding, adaptation to nurses' speech, the possibility of error correction, ability to fully review documentation processes, previous experience of using the system expresses that the strong support and management of senior executives are as facilitators of the SR system. A recent survey reported that more than 90% of hospitals plan to expand the use of front‐end SR systems, that is, direct dictation in the field of free text in electronic health records, 70 and extension in new years. 71 Therefore, it is better to use facilitators to improve the performance of these systems to increase their efficiency and effectiveness of these systems. Also, the quality of clinical documents is maintained by the expectations of individuals and organizations. Other studies 65 , 72 , 73 have shown that the performance of a SR system from a technology point of view can be facilitated by facilitators such as a good sound card and a good memory card, simple and fast loading of clinical documents and medical reports in the SR system software, use of clear dictionaries, repetitive vocabulary, thematic classification of vocabulary with semantic features in medical reports, adequate pronunciation speed and compound and structured sentences, a quiet room, and a good, high‐quality microphone (to prevent noise background) improved. Additionally, the use of portable hardware devices such as tablets and personal digital devices, along with user‐friendly interface systems (SR software), can facilitate the adoption of this technology across different departments of a hospital. 18
One of the stated facilitators for the SR system is “adequate training of nurses on how to work with SR systems.” It is better to form a strong support team and teach nurses the necessary exercises and training. Powder and Belmar 74 and Johnson et al. 72 noted that the time to learn to use a SR system can vary from a few minutes to 6 h for the first exercise. These exercises are necessary for several weeks to familiarize the user with the SR system and the SR system can store more new vocabulary in the database after receiving the users' speech. According to the same authors, the time required to familiarize, practice, and educate users with the SR system and achieve satisfactory results may take between 2 and 6 months. However, this time is directly related to the users' skills and the type of equipment used (such as SR system, microphone, or sound card). Hodgson et al., 28 showed that improving system data integration and workflow, along with enhancing accuracy and implementing user‐centric error correction strategies, may improve the performance of SR systems. Suominen et al. 20 also extracted data from 260 manually recorded reports to use integrated data to enhance the performance of the SR system. Reports were extracted from various work shifts and medical and surgical wards of hospitals in Sydney, Australia. The results of this study showed that information extraction stores all the required information and prevents misinterpretation of information by others. They also stated that this information is available more quickly to authorized personnel, and none of the required information will be lost.
Another facilitator for the SR system is to improve nurses' understanding (of system benefits and experience). Fratzke et al. 21 surveyed long‐term care centers to improve nurses' perceptions and demonstrated the benefits of a SR system in reducing the burden of documentation responsibility, improving financial performance due to increased reimbursement, and reducing overtime for nurses. In their study, they used a simulated nursing care environment using virtual reality technology to validate the SR system for documenting nursing care. The results showed that the successful adoption of technology in a simulated environment using virtual reality depends on the benefits perceived by nurses, timely access to training, and minimizing barriers to the use of technology.
4.4. Electronic systems for nursing documentation and reporting
In medical centers and hospitals, various electronic systems are used for nursing documentation and reporting, except for the SR system. According to Staggers et al., 75 documenting nursing reports in the patient file was done using computerized patient summary reports in an electronic health record after installing a computerized provider order entry system. Despite this technological advancement, nurses still had to print reports from the system, and patient case summary reports were often incomplete, making it difficult for nurses to access relevant information at a glance. EHRs are other computerized systems that allow nurses to enter patient data and generate reports. These systems can be accessed from various locations, including computers, tablets, and smartphones. In a study, Moody et al. 76 investigated the nurses' attitudes toward recording documents in electronic health records. Although 75% of nurses stated that EHRs have improved the quality of documentation, only 36% of nurses believed that using EHRs for reporting has resulted in reduced workload. Most of the nurses (64%) preferred to record the documents at the bedside. In another study, Yadav et al. 77 showed that the rate of incorrect documentation in EHR was significantly higher than in paper charts. Handheld devices are other technologies for recording nursing reports and documentation. Handheld devices, such as tablets or smartphones, can be used to record nursing reports. Some devices may also come equipped with software specifically designed for nurses, making it easier to input patient information and generate reports. 78 , 79 , 80 Despite the advantages of these devices, some studies 79 , 81 have shown that the use of handheld devices generally does not improve the documentation of doctors' and nurses' reports or the efficiency of workflow.
Wearable technology can also be used to record your reports and nursing documentation. Wearable technology, such as smartwatches or fitness trackers, can also be used to record nursing reports. Some devices may allow nurses to input patient data directly into the device or access electronic health records remotely. 82 , 83 Moreover, barcoding technology can also be used to scan patient information, such as medication labels, and record this information electronically. This can help to reduce errors and improve efficiency in the nursing report process. 84 , 85 , 86 , 87 Barcoding Technology like other technologies has benefits and challenges for implementation. The costs of equipment and training, increasing the implementing time, and preparing the coding of the tapes are among the challenge to the implementation of this technology. 88
4.5. Study limitations
Our study was conducted in a specific place and time range (on ICU nurses working in the three educational hospitals in Mashhad city). Consequently, the findings of this study cannot be extrapolated to nurses working in other healthcare facilities or the general population of nurses in Iran. Therefore, it is better to conduct future studies on a large national and even international level and on nurses working in non‐ICU departments. Another limitation of this study is the small sample size due to the lack of familiarity of many nurses with SR systems, so it is recommended to conduct studies with a larger population. The survey was conducted only on nurses and other clinical care providers and physicians were not included in the study. It is suggested that future studies examine the views of this group of people.
4.6. Implications and recommendations
Although SR technology holds vast potential for documenting nursing reports, different barriers hinder its effective implementation and usage. In this study, we tried to provide good insight to hospital executives, policymakers, designers, and health developers by introducing the benefits, facilitators, and barriers of this technology, so that they can choose SR system technology appropriately and efficiently and develop it. Because the basic issue regarding the implementation of new technologies such as the SR system in hospitals is the cost and justification of its benefits, barries, and challenges.
It is important for healthcare organizations to invest in high‐quality SR software and provide adequate training and support to ensure its proper use. In addition, healthcare providers should remain vigilant in reviewing and verifying the accuracy of documentation created through SR technology. As with any technological advancement in healthcare, proper implementation and oversight are critical to maximizing benefits while minimizing risks.
5. CONCLUSION
In this study, we identified the benefits, barriers, and facilitators of using SR technology in nursing documentation and reporting. Understanding nurses' experiences and perspectives on the benefits, barriers, and facilitators of this technology can lead to its acceptance, overcoming of barriers, and development of appropriate strategies to guide nurses toward its benefits in medical centers and health systems. Moreover, by providing information on the benefits, barriers, and facilitators of SR technology, hospital managers, nursing department managers, and IT managers can make more informed decisions when selecting and implementing SR systems for nursing documentation. They can also take courses on positive orientations to develop appropriate strategies and policies to improve acceptance of the system among nurses and other medical professionals. Furthermore, this information can aid the designers of the system in creating effective training programs.
By leveraging this technology, nursing schools can better prepare their students for the realities of the modern healthcare system while also promoting inclusivity and accessibility. Educational officials should consider the potential benefits of SR technology in nursing reports documenting, including increased efficiency, reduced errors, and improved patient care.
AUTHOR CONTRIBUTIONS
Fatemeh Dinari: Conceptualization; data curation; formal analysis; investigation; methodology; resources; writing—review and editing. Kambiz Bahaadinbeigy: Investigation; writing—review and editing. Somayyeh Bassiri: Data curation. Esmat Mashouf: Writing—original draft; writing—review and editing. Saiyad Bastaminejad: Data curation; formal analysis; writing—review and editing. Khadijeh Moulaei: Conceptualization; data curation; formal analysis; investigation; methodology; project administration; writing—original draft; writing—review and editing.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
For this research, ethics approval was obtained from the Ethics Committee of Kerman University of Medical Sciences (KUMS) with the code number IR.KMU.REC.1400.607. Participation of all nurses in this study was voluntary. In face‐to‐face referrals to hospitals to complete the questionnaires, all participants signed written informed consent. Additionally, the nurses who participated in the study online signed the written informed consent and emailed it to us.
TRANSPARENCY STATEMENT
The lead author Khadijeh Moulaei affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Supporting information
Supporting information.
ACKNOWLEDGMENTS
The authors would like to thank all nurses who participated in this study. This study was supported by Kerman University of Medical Sciences (Grant: 400000808). The funder had no roles in study design, data gathering, and analysis.
Dinari F, Bahaadinbeigy K, Bassiri S, Mashouf E, Bastaminejad S, Moulaei K. Benefits, barriers, and facilitators of using speech recognition technology in nursing documentation and reporting: a cross‐sectional study. Health Sci Rep. 2023;6:e1330. 10.1002/hsr2.1330
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Urquhart C, Currell R, Grant MJ, Hardiker NR. Nursing record systems: effects on nursing practice and healthcare outcomes. Cochrane Database Syst Rev. 2009;50(51):1‐40. [DOI] [PubMed] [Google Scholar]
- 2. Ahmadi M, Gorzin Z, Khoshgam M. Nurses needs assessment on methods of documentation in electronic health records. 2013.
- 3. Kahouei M, Babamohamadi H. Experiences of nurses in impact of nursing information system on nursing services efficiency. Health Inf Manage. 2013;10(2):1‐12. [Google Scholar]
- 4. Heidarizadeh K, Rassouli M, Manoochehri H, Tafreshi MZ, Ghorbanpour RK. Nurses' perception of challenges in the use of an electronic nursing documentation system. Comput Inform Nurs. 2017;35(11):599‐605. [DOI] [PubMed] [Google Scholar]
- 5. Sum MT, Chebor MA. Documentation: historical perspectives, purposes, benefits and challenges as faced by nurses. Int J Hum Soc Sci. 2013;3(16):236‐240. [Google Scholar]
- 6. Kebede M, Endris Y, Zegeye DT. Nursing care documentation practice: the unfinished task of nursing care in the University of Gondar Hospital. Inform Health Social Care. 2017;42(3):290‐302. [DOI] [PubMed] [Google Scholar]
- 7. Tasew H, Mariye T, Teklay G. Nursing documentation practice and associated factors among nurses in public hospitals, Tigray, Ethiopia. BMC Res Notes. 2019;12(1):612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Barr BJ. Managing change during an information systems transition. AORN J. 2002;75(6):1085‐1092. [DOI] [PubMed] [Google Scholar]
- 9. Broderick MC, Coffey A. Person‐centred care in nursing documentation. Int J Older People Nurs. 2013;8(4):309‐318. [DOI] [PubMed] [Google Scholar]
- 10. Jasemi M, Zamanzadeh V, Rahmani A, Mohajjel A, Alsadathoseini F. Knowledge and practice of Tabriz teaching hospitals' nurses regarding nursing documentation. Thrita. 2013;2(2):1‐6. [Google Scholar]
- 11. Gomes DC, Cubas MR, Pleis LE, Shmeil MA, Peluci AP. Terms used by nurses in the documentation of patient progress. Rev Gaucha Enferm. 2016;37:53927. [DOI] [PubMed] [Google Scholar]
- 12. Considine J, Trotter C, Currey J. Nurses' documentation of physiological observations in three acute care settings. J Clin Nurs. 2016;25(1‐2):134‐143. [DOI] [PubMed] [Google Scholar]
- 13. Derman YD, Arenovich T, Strauss J. Speech recognition software and electronic psychiatric progress notes: physicians' ratings and preferences. BMC Med Inform Decis Mak. 2010;10(1):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mehta A, Dreyer KJ, Schweitzer A, Couris J, Rosenthal D. Voice recognition—an emerging necessity within radiology: experiences of the Massachusetts General Hospital. J Digit Imaging. 1998;11(2):20‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Quint DJ. Voice recognition: ready for prime time? J Am Coll Radiol. 2007;4(10):667‐669. [DOI] [PubMed] [Google Scholar]
- 16. Weber J. Tomorrow's transcription tools: what new technology means for healthcare. Tomorrow's transcription tools: what new technology means for healthcare. AHIMA, American Health Information Management Association. 2003.
- 17. Callaway EC, Sweet CF, Siegel E, Reiser JM, Beall DP. Speech recognition interface to a hospital information system using a self‐designed visual basic program: initial experience. J Digit Imaging. 2002;15(1):43‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dawson L, Johnson M, Suominen H, et al. A usability framework for speech recognition technologies in clinical handover: a pre‐implementation study. J Med Syst. 2014;38(6):56. [DOI] [PubMed] [Google Scholar]
- 19. Carter‐Wesley J. Voice recognition dictation for nurses. JONA: J Nurs Administration. 2009;39(7/8):310‐312. [DOI] [PubMed] [Google Scholar]
- 20. Suominen H, Johnson M, Zhou L, et al. Capturing patient information at nursing shift changes: methodological evaluation of speech recognition and information extraction. J Am Med Inform Assoc. 2015;22(e1):e48‐e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fratzke J, Tucker S, Shedenhelm H, Arnold J, Belda T, Petera M. Enhancing nursing practice by utilizing voice recognition for direct documentation. JONA: J Nurs Administration. 2014;44(2):79‐86. [DOI] [PubMed] [Google Scholar]
- 22. Migowa AN, Macharia WM, Samia P, Tole J, Keter AK. Effect of a voice recognition system on pediatric outpatient medication errors at a tertiary healthcare facility in Kenya. Ther Adv Drug Saf. 2018;9(9):499‐508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Blackley SV, Schubert VD, Goss FR, Al Assad W, Garabedian PM, Zhou L. Physician use of speech recognition versus typing in clinical documentation: a controlled observational study. Int J Med Inform. 2020;141:104178. [DOI] [PubMed] [Google Scholar]
- 24. Hoyt R, Yoshihashi A. Lessons learned from implementation of voice recognition for documentation in the military electronic health record system. Perspect Health Inf Manag. 2010;7(Winter):1. [PMC free article] [PubMed] [Google Scholar]
- 25. Mubin O, Bartneck C, Feijs L, Hooft van Huysduynen H, Hu J, Muelver J. Improving speech recognition with the robot interaction language. Disruptive Sci Technol. 2012;1(2):79‐88. [Google Scholar]
- 26. Johnson M, Sanchez P, Suominen H, et al. Comparing nursing handover and documentation: forming one set of patient information. Int Nurs Rev. 2014;61(1):73‐81. [DOI] [PubMed] [Google Scholar]
- 27. Marjan GS, Reza S, Abdoljalil KH, Leila S, Fatemeh S. Advantages and limitations of using speech recognition systems in health care and practical means to solve their application. Payavard Salamat. 2014;8(1):1‐12. [Google Scholar]
- 28. Hodgson T, Magrabi F, Coiera E. Efficiency and safety of speech recognition for documentation in the electronic health record. J Am Med Inform Assoc. 2017;24(6):1127‐1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Goss FR, Blackley SV, Ortega CA, et al. A clinician survey of using speech recognition for clinical documentation in the electronic health record. Int J Med Inform. 2019;130:103938. [DOI] [PubMed] [Google Scholar]
- 30. Hayt DB, Alexander S. The pros and cons of implementing PACS and speech recognition systems. J Digit Imaging. 2001;14:149‐157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Parente R, Kock N, Sonsini J. An analysis of the implementation and impact of speech‐recognition technology in the healthcare sector. Perspec Health Inf Manag. 2004;1:5. [PMC free article] [PubMed] [Google Scholar]
- 32. Sheikhtaheri A. Documenting nursing reports using speech recognition technology: benefits, barriers, challenges and facilitators. J Health Biomed Infor. 2018;5(1):70‐82. [Google Scholar]
- 33. Etikan I. Comparison of convenience sampling and purposive sampling. Am J Theoretical Applied Statistics. 2016;5(1):1‐4. [Google Scholar]
- 34. Saxena K, Diamond R, Conant RF, Mitchell TH, Gallopyn G, Yakimow KE. Provider adoption of speech recognition and its impact on satisfaction, documentation quality, efficiency, and cost in an inpatient EHR. AMIA Jt Summits Transl Sci Proc. 2018;2018:186. [PMC free article] [PubMed] [Google Scholar]
- 35. Dunphy H, Finlay JL, Lemaire J, MacNairn I, Wallace JE. Hands‐free communication technology: a benefit for nursing? JONA: J Nur Administration. 2011;41(9):365‐368. [DOI] [PubMed] [Google Scholar]
- 36. Suominen H, Hanlen L, Goeuriot L, Kelly L, Jones GJ. In Task 1a of the CLEF eHealth Evaluation Lab 2015, 6th International Conference on Labs of the Evaluation Forum, CLEF 2015, CEUR Workshop Proceedings: 2015; pp 1‐18.
- 37. Blackley SV, Huynh J, Wang L, Korach Z, Zhou L. Speech recognition for clinical documentation from 1990 to 2018: a systematic review. J Am Med Inform Assoc. 2019;26(4):324‐338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Friedberg MW, Chen PG, Van Busum KR, et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. Rand Health Q. 2014;3(4):1. [PMC free article] [PubMed] [Google Scholar]
- 39. Payne TH, Alonso WD, Markiel JA, et al. Using voice to create inpatient progress notes: effects on note timeliness, quality, and physician satisfaction. JAMIA open. 2018;1(2):218‐226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Clarke MA, King JL, Kim MS. Toward successful implementation of speech recognition technology: a survey of SRT utilization issues in healthcare settings. South Med J. 2015;108(7):445‐451. [DOI] [PubMed] [Google Scholar]
- 41. Suominen H, Zhou L, Hanlen L, Ferraro G. Benchmarking clinical speech recognition and information extraction: new data, methods, and evaluations. JMIR Med Inform. 2015;3(2):e4321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ajami S. Use of speech‐to‐text technology for documentation by healthcare providers. Natl Med J India. 2016;29(3):148‐152. [PubMed] [Google Scholar]
- 43. Zhou L, Blackley SV, Kowalski L, et al. Analysis of errors in dictated clinical documents assisted by speech recognition software and professional transcriptionists. JAMA Network Open. 2018;1(3):e180530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Rana DS, Hurst G, Shepstone L, Pilling J, Cockburn J, Crawford M. Voice recognition for radiology reporting: is it good enough? Clin Radiol. 2005;60(11):1205‐1212. [DOI] [PubMed] [Google Scholar]
- 45. Vogel M, Kaisers W, Wassmuth R, Mayatepek E. Analysis of documentation speed using web‐based medical speech recognition technology: randomized controlled trial. J Med Internet Res. 2015;17(11):e5072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hodgson T, Coiera E. Risks and benefits of speech recognition for clinical documentation: a systematic review. J Am Med Inform Assoc. 2016;23(e1):e169‐e179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Singh M, Pal TR. Voice recognition technology implementation in surgical pathology: advantages and limitations. Arch Pathol Lab Med. 2011;135(11):1476‐1481. [DOI] [PubMed] [Google Scholar]
- 48. Lyons JP, Sanders SA, Fredrick Cesene D, Palmer C, Mihalik VL, Weigel T. Speech recognition acceptance by physicians: a temporal replication of a survey of expectations and experiences. Health Informatics J. 2016;22(3):768‐778. [DOI] [PubMed] [Google Scholar]
- 49. Zick RG, Olsen J. Voice recognition software versus a traditional transcription service for physician charting in the ED. Am J Emerg Med. 2001;19(4):295‐298. [DOI] [PubMed] [Google Scholar]
- 50. Koivikko MP, Kauppinen T, Ahovuo J. Improvement of report workflow and productivity using speech recognition—a follow‐up study. J Digit Imaging. 2008;21(4):378‐382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Suominen H, Ferraro G. Noise in speech‐to‐text voice: analysis of errors and feasibility of phonetic similarity for their correction. 2013.
- 52. Bradley Morrison J, Rudolph JW. Learning from accident and error: avoiding the hazards of workload, stress, and routine interruptions in the emergency department. Acad Emerg Med. 2011;18(12):1246‐1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Westbrook JI, Coiera E, Dunsmuir WT, et al. The impact of interruptions on clinical task completion. QSHC (Qual Saf Health Care). 2010;19(4):284‐289. [DOI] [PubMed] [Google Scholar]
- 54. Issenman RM, Jaffer IH. Use of voice recognition software in an outpatient pediatric specialty practice. Pediatrics. 2004;114(3):e290‐e293. [DOI] [PubMed] [Google Scholar]
- 55. Pezzullo JA, Tung GA, Rogg JM, Davis LM, Brody JM, Mayo‐Smith WW. Voice recognition dictation: radiologist as transcriptionist. J Digit Imaging. 2008;21(4):384‐389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. White KS. Speech recognition implementation in radiology. Pediatr Radiol. 2005;35(9):841‐846. [DOI] [PubMed] [Google Scholar]
- 57. Alapetite A, Boje Andersen H, Hertzum M. Acceptance of speech recognition by physicians: a survey of expectations, experiences, and social influence. Int J Hum Comput Stud. 2009;67(1):36‐49. [Google Scholar]
- 58. Ayani S, Sadoughi F, Jabari R, Moulaei K, Ashrafi‐Rizi H. Evaluation criteria for health websites: critical review. Front. Health Inform. 2020;9(1):44‐66. [Google Scholar]
- 59. Dawson L, Fisher J, Weeding S, Heslop L, Howard A. Action research in emerging technologies in health information systems: creating a mobile information environment in a hospital ward. 2009.
- 60. Fernando J, Dawson L. Clinician assessments of workplace security training‐an informatics perspective. 2008.
- 61. Darcy R, Gallagher P, Moore S, Varghese D. In the potential of using voice recognition in patient assessment documentation in mountain rescue, IEEE 29th International Symposium on Computer‐Based Medical Systems (CBMS), IEEE. 2016; pp. 329‐332.
- 62. Chang CA, Strahan R, Jolley D. Non‐clinical errors using voice recognition dictation software for radiology reports: a retrospective audit. J Digit Imaging. 2011;24(4):724‐728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Ringler MD, Goss BC, Bartholmai BJ. Syntactic and semantic errors in radiology reports associated with speech recognition software. Health Informatics J. 2017;23(1):3‐13. [DOI] [PubMed] [Google Scholar]
- 64. Pezzullo JA, Tung GA, Rogg JM, Davis LM, Brody JM, Mayo‐Smith WW. Voice recognition dictation: radiologist as transcriptionist. J Digit Imaging. 2008;21:384‐389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Hammana I, Lepanto L, Poder T, Bellemare C, Ly M‐S. Speech recognition in the radiology department: a systematic review. Health Information Management Journal. 2015;44(2):4‐10. [DOI] [PubMed] [Google Scholar]
- 66. Basma S, Lord B, Jacks LM, Rizk M, Scaranelo AM. Error rates in breast imaging reports: comparison of automatic speech recognition and dictation transcription. Am J Roentgenol. 2011;197(4):923‐927. [DOI] [PubMed] [Google Scholar]
- 67. Cai T, Giannopoulos AA, Yu S, et al. Natural language processing technologies in radiology research and clinical applications. Radiographics. 2016;36(1):176‐191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Dreisbach C, Koleck TA, Bourne PE, Bakken S. A systematic review of natural language processing and text mining of symptoms from electronic patient‐authored text data. Int J Med Inform. 2019;125:37‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Kelley TF, Brandon DH, Docherty SL. Electronic nursing documentation as a strategy to improve quality of patient care. J Nurs Scholarsh. 2011;43(2):154‐162. [DOI] [PubMed] [Google Scholar]
- 70. Abd El‐Kafy EM, Alshehri MA, El‐Fiky AA‐R, Guermazi MA, Mahmoud HM. The effect of robot‐mediated virtual reality gaming on upper limb spasticity poststroke: a randomized‐controlled trial. Games Health J. 2022;11(2):93‐103. [DOI] [PubMed] [Google Scholar]
- 71. Stewart B. Front‐End Speech 2014: Functionality Doesn't Trump Physician Resistance. KLAS; 2014. [Google Scholar]
- 72. Johnson M, Lapkin S, Long V, et al. A systematic review of speech recognition technology in health care. BMC Med Inform Decis Mak. 2014;14(1):94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Alcantara‐Pla M, Declerck T. In Proceedings of SRSL, the 2nd Workshop on Semantic Representation of Spoken Language, Proceedings of SRSL 2009, the 2nd Workshop on Semantic Representation of Spoken Language. 2009.
- 74. Poder TG, Bellemare C. Émergence d'une nouvelle technologie au service de la gestion des hôpitaux: les systèmes de reconnaissance vocale. Journal de gestion et d'économie médicales. 2009;27(6):329‐339. [Google Scholar]
- 75. Staggers N, Clark L, Blaz JW, Kapsandoy S. Why patient summaries in electronic health records do not provide the cognitive support necessary for nurses' handoffs on medical and surgical units: insights from interviews and observations. Health Informatics J. 2011;17(3):209‐223. [DOI] [PubMed] [Google Scholar]
- 76. Moody LE, Slocumb E, Berg B, Jackson D. Electronic health records documentation in nursing: nurses' perceptions, attitudes, and preferences. Computers, Infor, Nurs: CIN. 2004;22(6):337‐344. [DOI] [PubMed] [Google Scholar]
- 77. Yadav S, Kazanji N, KC N, et al. Comparison of accuracy of physical examination findings in initial progress notes between paper charts and a newly implemented electronic health record. J Am Med Inform Assoc. 2017;24(1):140‐144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Killeen JP, Chan TC, Buono C, Griswold WG, Lenert LA. In a wireless first responder handheld device for rapid triage, patient assessment and documentation during mass casualty incidents, AMIA annual symposium proceedings, American Medical Informatics Association. 2006; p. 429. [PMC free article] [PubMed]
- 79. Stengel D, Bauwens K, Walter M, Köpfer T, Ekkernkamp A. Comparison of handheld computer‐assisted and conventional paper chart documentation of medical records: a randomized, controlled trial. J Bone Joint Surg. 2004;86(3):553‐560. [DOI] [PubMed] [Google Scholar]
- 80. Koban KC, Perko P, Etzel L, Li Z, Schenck TL, Giunta RE. Validation of two handheld devices against a non‐portable three‐dimensional surface scanner and assessment of potential use for intraoperative facial imaging. J Plastic, Reconstructive Aesthetic Surg: JPRAS. 2020;73(1):141‐148. [DOI] [PubMed] [Google Scholar]
- 81. Prgomet M, Georgiou A, Westbrook JI. The impact of mobile handheld technology on hospital physicians' work practices and patient care: a systematic review. J Am Med Inform Assoc. 2009;16(6):792‐801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Ip JE. Wearable devices for cardiac rhythm diagnosis and management. JAMA. 2019;321(4):337‐338. [DOI] [PubMed] [Google Scholar]
- 83. Reeder B, David A. Health at hand: a systematic review of smart watch uses for health and wellness. J Biomed Inf. 2016;63:269‐276. [DOI] [PubMed] [Google Scholar]
- 84. Edwards M, Moczygemba J. Reducing medical errors through better documentation. Health Care Manag (Frederick). 2004;23(4):329‐333. [DOI] [PubMed] [Google Scholar]
- 85. Turner CL, Casbard AC, Murphy MF. Barcode technology: its role in increasing the safety of blood transfusion. Transfusion. 2003;43(9):1200‐1209. [DOI] [PubMed] [Google Scholar]
- 86. Zheng WY, Lichtner V, Van Dort BA, Baysari MT. The impact of introducing automated dispensing cabinets, barcode medication administration, and closed‐loop electronic medication management systems on work processes and safety of controlled medications in hospitals: a systematic review. Res Social Administrative Pharmacy. 2021;17(5):832‐841. [DOI] [PubMed] [Google Scholar]
- 87. Cummings J, Ratko T, Matuszewski K. Barcoding to enhance patient safety. Agency for Healthcare Research and Quality Case and Commentary. 2005. http://www.psqh.com/sepoct05/barcodingrfid1.html
- 88. Fleischman, EK . Innovative application of bar coding technology to breast milk administration. J Perinat Neonatal Nurs. 2013;27(2):145‐150. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


