ABSTRACT
Zenker's diverticulum develops because of a weakness in Killian's triangle, leading to a mucosal and submucosal herniation. Its treatment has evolved from morbid surgical interventions to safer endoscopic techniques such as peroral endoscopic myotomy (Z-POEM). Despite being a safe technique, Z-POEM is not free of complications such as perforations, bleeding, pneumoperitoneum, and pneumothorax, for which new endoscopic techniques have been developed. We present the case of a 53-year-old man taken to a Z-POEM who postoperatively presented dehiscence of the mucosotomy and a mediastinal collection, managed with a vacuum-assisted endoscopic closure device.
KEYWORDS: Zenker's diverticulum, Z-POEM, esophageal perforation, abscess
INTRODUCTION
Esophageal diverticulum is a relatively rare entity that cause dysphagia, regurgitation, and chest pain. They can be found distally, in the middle esophagus (Rokitansky diverticulum), or pharyngoesophageal (Zenker diverticulum).1,2 Surgical management was considered the only curative intervention for years, however, associated with high mortality rates (up to 3%, especially in proximal diverticulum), leading to the development of new endoscopic options for its management.3
Because the development of third-space endoscopy for achalasia and the use of peroral endoscopic myotomy (POEM) in the treatment of Zenker's diverticulum (Z-POEM), Z-POEM has been considered an excellent option for symptomatic diverticulum patients.4,5 Although it is considered a safer procedure with low recurrence rates compared with other endoscopic techniques such as flexible endoscopic septotomy, endoscopic stapler-assisted diverticulotomy, and harmonic scalpel endoscopy, it is not free of complications such as perforations, bleeding, pneumoperitoneum, and pneumothorax, which can occur in up to 10% of patients with overall mortality rates of 0.025%; many of these susceptible to endoscopic and conservative management.6,7
CASE REPORT
We present the case of a 53-year-old man referred to the gastroenterology department for a 3-year progressive dysphagia, for solids and liquids. An esophagogram and upper endoscopy were performed, and a Zenker's diverticulum of approximately 15 mm was documented. With these findings, the patient was taken to a Z-POEM, and in the immediate postoperative period, the patient presented cervical subcutaneous emphysema. An esophagogram was then performed ruling out leaks (Figure 1), with subsequent hospital discharge 2 days later.
Figure 1.

Z-POEM immediate postoperative esophagogram; no evidence of water-soluble contrast leaks. (Z-POEM), peroral endoscopic myotomy in the treatment of Zenker's diverticulum.
A week later, the patient was readmitted because of persistent chest pain and dysphagia. Computed tomography of the chest showed a collection of 0.4 × 16 × 31 mm in the upper mediastinum compromising the prevertebral space (Figure 2). An upper endoscopy showed the complete dehiscence of the mucosotomy and a tunnel over the submucosa that extended deeply over the muscularis propria, allowing for the passage of the endoscope through the prevertebral space where abundant purulent material and fibrinous membranes were observed. An endoscopic lavage was performed, and a Jackson-Pratt drain was positioned in the abscess cavity through a nasomediastinal tract and then connected to a Blake device (Figure 2). In addition, antibiotic therapy was prescribed, and a nasogastric tube was placed for enteral nutrition. Seventy-two hours after, a follow-up endoscopy showed persistent purulent material, so a new endoscopic lavage and drainage were performed; the Jackson-Pratt drain was removed and replaced for a polyurethane sponge that was implanted in the cavity over the nasogastric tube, and then connected to a vacuum-assisted closure (VAC) device through a 14–16 Levin probe, with a negative pressure at −125 mm Hg (Figure 3).
Figure 2.
(A) Collection on the posterior wall of the esophagus and the prevertebral cortical bone that extended from C7 to T5 at the level of the carina of 104 × 16 × 31 mm (white arrow). (B) Endoscopic positioning of the drainage tube with the distal end at the bottom of the mediastinal abscess.
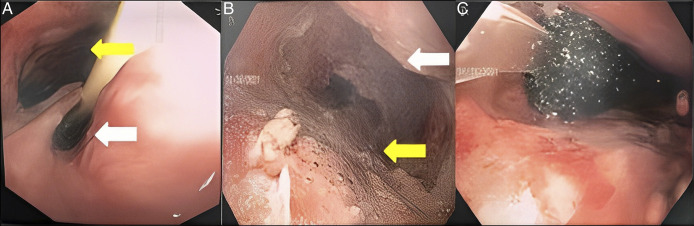
Figure 3.
(A) Endoscopic view of the true esophageal lumen (white arrow) and the prevertebral space between the posterior wall of the esophagus and the cortex of the vertebral column at the level of C5 (yellow arrow). (B) Light photography of the prevertebral space during lavage (yellow arrow: posterior wall of the esophagus; white arrow: cortical bone of the thoracic spine). (C) Polyurethane sponge and negative pressure device connection probe occupying the prevertebral space.
Four days later, the VAC was removed showing a smaller esophageal defect with a clean base. At this moment, a fibrin sealant was applied, and the patient was discharged continuing enteral nutrition. An endoscopic control performed 3 weeks after showed a smaller esophageal wall defect (Figure 4), so the nasogastric tube was then removed, and liquid diet indicated. A control endoscopy 3 weeks later showed a complete closure of the sinus tract (Figure 4), and an esophagogram performed 1 month later showed correction of Zenker's diverticulum with no evidence of a fistulous tract (Figure 5).
Figure 4.
(A) Residual esophageal defect 3 weeks after VAC removal (white arrow: esophageal lumen; yellow arrow: fistula tract). (B) Esophageal lumen with normal caliber 6 weeks after VAC removal, scar from the closure of the defect (yellow arrow). VAC, vacuum-assisted closure.
Figure 5.

Post-treatment esophagogram.
DISCUSSION
Zenker's diverticulum is a pharyngoesophageal pseudodiverticulum caused by herniation of the mucosa and submucosa of the posterior wall of the proximal esophagus through Killian's triangle.8 It has a low prevalence in the general population, between 0.01% and 0.11%, being more frequent in males (58%) and in patients older than 65 years (78%). Dysphagia, regurgitation, and chest pain are caused by incomplete opening of the upper esophageal sphincter and extrinsic compression by the pseudodiverticulum.9 Its treatment is based on a septotomy that can be surgical or endoscopic; however, its predominance in elderly patients limits the use of surgical techniques because of its invasiveness and higher mortality, which is why, in recent years, peroral endoscopic myotomy has proven to be a safe technique, with high success rates and lower complications.10 A recent systematic review and meta-analysis found a Z-POEM success rate of 95% and an adverse event rate of 6%.11 Among the complications described in a study of 75 patients, bleeding presented in 1 patient and 4 cases of perforations were described, 3 managed endoscopically with cyanoacrylate and metal clips; 1 required conservative treatment, and no mortality cases were reported.12
Z-POEM–associated mediastinal abscess has not been described, however, esophageal perforations are the main risk factor for presenting them.13 In POEM in achalasia, mediastinitis, abscesses, and fistula are present in less than 0.1%, although the rate of mediastinal exposure can be greater than 10%.14 Vacuum therapy involves the placement of a sterile polyurethane sponge fixed with a surgical suture in the fenestrated tip of a nasogastric tube, positioned over the lumen of the defect on the esophageal wall and directed with a flexible overtube to the cavity, connected to an external suction device,15 and has been described effective in the treatment of esophageal perforations that already have a mediastinal track, with closure rates of 92% (Figure 6).16–18
Figure 6.
(A) Elements used: Endoscope, endoscopic forceps, and EndoVac. (B, C) Perforated polyurethane sponge fixed on the fenestrated tip of the nasogastric tube and size comparison with the endoscope tip.
We present a young man with an esophageal perforation after a Z-POEM, which developed an abscess in the anterior mediastinum, needing nasomediastinal drainage, endoscopic lavage and drainage of the abscess, and placement of a vacuum-assisted closure system with successful closure of the defect. Our patient's age stands out, being younger than the average age of presentation of Zenker's diverticulum described in the literature. A total of 3 VAC device replacements were needed, 2 of which were performed in an outpatient setting. The patient completed 14 days of antibiotic treatment with ureidopenicillin and received concomitant analgesic and prokinetic medication. He was managed together with nutritional support, which favored early hospital discharge, requiring only 15 days of hospitalization.
All these findings suggest that vacuum-assisted system is useful as closure therapy for esophageal perforations because of multiple causes and that endoscopic management should be considered as the first treatment option in most patients.
DISCLOSURES
Author contributions: EM Daza Castro, CF Fuentes, and AC Córdoba Guzmán wrote and approved the article. D. Aponte, JN Rocha, C. Gonzalez, and LC Sabbagh reviewed the literature. All authors edited and revised the article for intellectual content. AC Córdoba Guzmán is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
REFERENCES
- 1.Sato H, Takeuchi M, Hashimoto S, et al. Esophageal diverticulum: New perspectives in the era of minimally invasive endoscopic treatment. World J Gastroenterol. 2019;25(12):1457–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Law R, Katzka DA, Baron TH. Zenker's diverticulum. Clin Gastroenterol Hepatol. 2014;12(11):1773–82. [DOI] [PubMed] [Google Scholar]
- 3.Budnicka A, Januszewicz W, Białek AB, Spychalski M, Reguła J, Kaminski MF. Peroral endoscopic myotomy in the management of Zenker's diverticulum: A retrospective multicenter study. J Clin Med. 2021;10(2):187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gonzalez JM, Benezech A, Barthet M. Complications of submucosal endoscopy. Best Pract Res Clin Gastroenterol. 2016;30(5):783–91. [DOI] [PubMed] [Google Scholar]
- 5.Miutescu BP, Khan S, Mony S, Khashab MA. Role of peroral endoscopic myotomy (POEM) in the management of esophageal diverticula. Clin Endosc. 2020;53(6):646–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krutsri C, Hiranyatheb P, Sumritpradit P, Singhatas P, Choikrua P. Z-per-oral endoscopic myotomy as definitive prevention of a bleeding ulcer in Zenker's diverticulum: A case report. World J Gastrointest Endosc. 2022;14(3):183–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeng X, Bai S, Zhang Y, Ye L, Yuan X, Hu B. Peroral endoscopic myotomy for the treatment of esophageal diverticulum: An experience in China. Surg Endosc. 2021;35(5):1990–6. [DOI] [PubMed] [Google Scholar]
- 8.Altintoprak F, Gundogdu K, Eminler AT, Parlak E, Cakmak G, Uzunoglu Mustafa Y. An endoscopic nasomediastinal approach to a mediastinal abscess developing after Zenker's diverticulectomy. Case Rep Gastrointest Med. 2017;2017:8726706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nuño-Guzmán CM, García-Carrasco D, Haro M, Arróniz-Jáuregui J, Corona JL, Salcido M. Zenker's diverticulum: Diagnostic approach and surgical management. Case Rep Gastroenterol. 2014;8(3):346–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miutescu BP, Khan S, Mony S, Khashab MA. Role of peroral endoscopic myotomy (POEM) in the management of esophageal diverticula. Clin Endosc. 2020;53(6):646–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kamal F, Khan MA, Lee-Smith W, et al. Peroral endoscopic myotomy is a safe and feasible option in management of esophageal diverticula: Systematic review and meta-analysis. Dig Dis Sci. 2021;66(10):3242–9. [DOI] [PubMed] [Google Scholar]
- 12.Yang J, Novak S, Ujiki M, et al. An international study on the use of peroral endoscopic myotomy in the management of Zenker's diverticulum. Gastrointest Endosc. 2020;91(1):163–8. [DOI] [PubMed] [Google Scholar]
- 13.Babür T. Iatrogenic Zenker's diverticulum perforation: A conservatively treated case. Ulus Cerrahi Derg. 2013;30(4):234–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stavropoulos SN, Desilets DJ, Fuchs KH, et al. Per-oral endoscopic myotomy white paper summary. Surg Endosc. 2014;28(7):2005–19. [DOI] [PubMed] [Google Scholar]
- 15.Kuehn F, Loske G, Schiffmann L, Gock M, Klar E. Endoscopic vacuum therapy for various defects of the upper gastrointestinal tract. Surg Endosc. 2017;31(9):3449–58. [DOI] [PubMed] [Google Scholar]
- 16.Gurwara S, Clayton S. Esophageal perforations: An endoscopic approach to management. Curr Gastroenterol Rep. 2019;21(11):57. [DOI] [PubMed] [Google Scholar]
- 17.de Moura DTH, de Moura BFBH, Manfredi MA, et al. Role of endoscopic vacuum therapy in the management of gastrointestinal transmural defects. World J Gastrointest Endosc. 2019;11(5):329–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Laukoetter MG, Mennigen R, Neumann PA, et al. Successful closure of defects in the upper gastrointestinal tract by endoscopic vacuum therapy (EVT): A prospective cohort study. Surg Endosc. 2017;31(6):2687–96. [DOI] [PubMed] [Google Scholar]