ABSTRACT
Isolated extramedullary plasmacytomas (IEMPs) are rare. Extramedullary plasmacytomas (EMPs) are uncommon and mostly occur in the nasopharynx or upper respiratory tract. EMP involvement of the gastrointestinal tract occurs in approximately 10% of cases, more often in the small bowel than the colon. Less than 40 cases of colonic IEMP have been reported. Asymptomatic colonic IEMPs are extremely rare with few reported cases. We present a 57-year-old asymptomatic man with a colonic IEMP found during screening colonoscopy. A sigmoid colon polyp was removed and diagnosed as a plasmacytoma. Further investigation revealed it to be an isolated lesion.
KEYWORDS: isolated, asymptomatic, colonic, plasmacytoma, colonoscopy
INTRODUCTION
The World Health Organization classifies plasma cell tumors as plasmacytoma, plasma cell myeloma/multiple myeloma, or plasma cell neoplasms with associated paraneoplastic syndrome.1,2 Plasmacytomas are classified as solitary plasmacytoma of bone (SPB) or extramedullary plasmacytoma (EMP). EMPs occur mostly in the nasopharynx or upper respiratory tract.3 EMPs are located in the gastrointestinal tract in 10% of cases,4–6 most frequently in the small bowel.4 IEMPs of the colon are very rare with less than 40 cases reported.7 In most cases, IEMPs of the colon present symptomatically with anemia, gastrointestinal bleeding, pain, diarrhea, and stricture.4,8,9 Few cases report IEMPs of the colon that are asymptomatic.10–12
CASE REPORT
A 57-year-old man presented for a screening colonoscopy. The patient had a history of well-controlled hypertension, diabetes mellitus, and hyperlipidemia. He had an average risk of colon cancer and elected to proceed. The patient had no subjective complaints, and physical examination was normal. The findings on his colonoscopy indicated a very good preparation and, in the proximal sigmoid colon, a polyp estimated endoscopically to be 12 mm in size. The polyp was smooth and semipedunculated (Figure 1). It was removed using a hot snare polypectomy device and retrieved. The postpolypectomy endoscopic appearance was satisfactory and excision was complete (Figure 2). On histopathological examination, the findings were consistent with a plasmacytoma. Histological sections showed colonic mucosa with a mass-like lesion composed of sheets of plasma cells. Immunohistochemistry (IHC) stains highlighted plasma cells expressing CD138 and BCL2 and showing kappa light chain restriction; they were negative for CD3, CD5, CD10, CD43, BCL1, BCL6, and pan keratin (Figures 3 and 4). Further investigations included a positron emission tomography (PET) scan, bone marrow biopsy, serum protein electrophoresis (SPEP), esophagogastroduodenoscopy, capsule enteroscopy, and serum kappa and lambda light chains. These studies were normal and did not reveal the presence of multiple myeloma.
Figure 1.
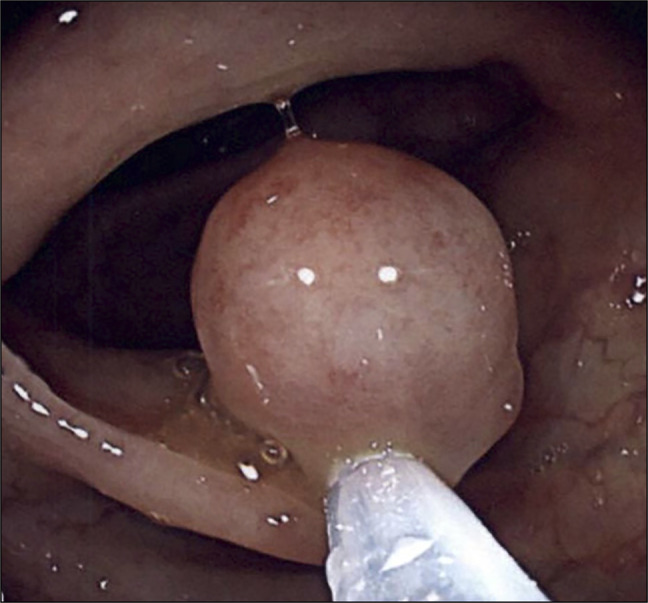
Smooth and semipedunculated polyp, estimated visually at 12 mm.
Figure 2.

Postpolypectomy endoscopic appearance.
Figure 3.
Light microscopy and immunohistochemistry. (A) H&E, 20×. Polypoid submucosal mass. 0.7 × 0.6 × 0.5 cm, proximal sigmoid, completely excised. (B) H&E, 100×. Sheets of plasma cells and 2 residual germinal centers within the lamina propria. (C) H&E, 200×. Sheets of plasma cells. (D) CD138 (IHC) highlights sheets of plasma cells. (E and F) Kappa and lambda light chains (IHC) demonstrate kappa restriction. H&E, hematoxylin and eosin; IHC, immunohistochemistry.
Figure 4.

Light microscopy. Hematoxylin and eosin, 600×. Sheets of pleomorphic plasma cells show irregular nuclear contours, coarse chromatin, inconspicuous nucleoli, and abundant eosinophilic cytoplasm with a perinuclear hof.
DISCUSSION
Isolated plasmacytoma is extremely rare with fewer than 450 cases per year.13 Seventy percent of people with isolated plasmacytoma develop multiple myeloma.14 Extramedullary plasmacytoma (EMP) has an incidence rate of 0.09 per 100,000 adults per year, and solitary plasmacytoma of bone (SPB) has an incidence rate of 0.45 per 100,000 adults per year.15 EMPs most frequently occur in the nasopharynx or upper respiratory tract,3 and involvement of the gastrointestinal tract occurs in approximately 10% of cases,4–6 more often in the small bowel than in the colon.4 Less than 40 cases of isolated EMP of the colon have been reported.7 In most cases, IEMPs of the colon present symptomatically, with anemia, gastrointestinal bleeding, pain, diarrhea, and stricture.4,8,9 Asymptomatic IEMPs of the colon are extremely rare with very few reported cases, our own literature review revealing 3 reports.10–12
Plasmacytomas, when associated with a multiple myeloma, may precede, accompany, or follow the multiple myeloma.4 To confirm the diagnosis of IEMPs, exclusion of a concurrent multiple myeloma or plasmacytoma of another site is necessary. In our reported case, the diagnostic modalities used to do so included SPEP, serum kappa and lambda light chains, bone marrow biopsy, and position emission tomography scan. Imaging of other segments of the digestive tract was necessary because small bowel involvement is more common than colonic involvement in EMP and included an esophagogastroduodenoscopy and a capsule enteroscopy.
Histopathologically, plasmacytomas are defined by a tumorous proliferation of monoclonal plasma cells that are demonstrated by biopsy. Plasma cells show round-to-oval nuclei with coarse chromatin, inconspicuous nucleoli, abundant eosinophilic cytoplasm, and a perinuclear hof. The cells of plasmacytoma have an immunophenotype similar to plasma cell myeloma, expressing markers such as CD138 and showing evidence of clonality by light chain restriction. Plasma cell neoplasms are clinicopathologic diagnoses, requiring the integration of pathologic and clinical information; to render a diagnosis of plasmacytoma (such as EMP), multiple myeloma must be ruled out by demonstrating no end-organ damage (by CRAB); and subsequent bone marrow biopsy must not show 10% or more monoclonal plasma cells. Furthermore, no clonal B-cell population should be present in plasmacytoma.2 The differential diagnosis also includes reactive plasmacytosis, which would generally fail to show monoclonality.
Because of the very few numbers of asymptomatic IEMPs of the gastrointestinal tract, especially the colon, there are no well-defined treatment guidelines, prognostic studies, or established guidelines for continued surveillance and screening for future occurrence of multiple myeloma. However, parallels can be drawn from cases of EMP and IEMP that provide more data and seem to indicate an overall good prognosis.3
In this case report, adequate colonic preparation that allowed the polyp retrieval and characterization proved essential. Longitudinal follow-up to confirm the adequacy of the complete polyp resection as the sole treatment of the IEMP, and the lack of emergence of multiple myeloma in the future, will be paramount.
Colonic IEMPs are rare, especially presenting asymptomatically as a polyp at screening colonoscopy. Physicians should be aware of this entity to confirm the lack of association with a concurrent multiple myeloma. Continued follow-up and monitoring are necessary, yet not well-established because progression and outcomes data lack. This case also underscores the importance of a good colonic preparation allowing polyp retrieval and characterization.
DISCLOSURES
Author contributions: C. Nassif and M. Crabtree collected data and wrote the manuscript. ST Pullarkat supervised and edited the manuscript. C. Nassif is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
Contributor Information
Matthew Crabtree, Email: mcrabtree@mednet.ucla.edu.
Sheeja T. Pullarkat, Email: spullarkat@mednet.ucla.edu.
REFERENCES
- 1.Harris NL, Jaffe ES, Diebold J, et al. World Health organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues: Report of the Clinical Advisory Committee Meeting-Airlie House, Virginia, 1997. J Clin Oncol. 1999;17:3835–49. [DOI] [PubMed] [Google Scholar]
- 2.Alaggio R, Amador C, Anagnostopoulos I, et al. The 5th edition of the World Health Organization classification of haematolymphoid tumours: Lymphoid neoplasms. Leukemia. 2022;36(7):1720–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liebross RH, Ha CS, Cox JD, Weber D, Delasalle K, Alexanian R. Clinical course of solitary extramedullary plasmacytoma. Radiother Oncol. 1999;52(3):245–9. [DOI] [PubMed] [Google Scholar]
- 4.Gupta V, Nahak B, Sakhuja P, Agarwal AK, Kumar N, Mishra PK. Primary isolated extramedullary plasmacytoma of colon. World J Surg Oncol. 2007;5:article 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hampton JM, Gandy JR. Plasmacytoma of the gastro-instestinal tract. Ann Surg. 1957;145(3):415–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Asselah F, Crow J, Slavin G, Sowter G, Sheldon C, Asselah H. Solitary plasmacytoma of the intestine. Histopathology. 1982;6(5):631–45. [DOI] [PubMed] [Google Scholar]
- 7.Alfar R, Kamal N, Abdel Razeq R, Omari Z, Bater R, Sharaf B. A durable response of primary advanced colonic plasmacytoma using a combination of surgical resection and adjuvant bortezomib: A case report and literature review. OncoTargets Ther. 2022;15:1347–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dalgic T, Bostanci EB, Cakir T, et al. Solitary plasmacytoma of the cecum and the ascending colon: Surgical resection as a treatment modality. Case Rep Surg. 2015;2015:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collado Pacheco D, Moran Ortiz de Solórzano M, Quintanilla Lázaro E, Chico Álvarez I, Rábago Torre L. Extramedullary plasmacytoma of the colon: A rare cause of gastrointestinal bleeding. Endoscopy. 2009;41(Suppl 02):E306–7. [DOI] [PubMed] [Google Scholar]
- 10.Sidani MS, Campos MM, Joseph JI. Primary plasmacytomas of the colon. Dis Colon Rectum. 1983;26(3):182–7. [DOI] [PubMed] [Google Scholar]
- 11.Allison JG, Getaz EP, Staples WG. Primary isolated extramedullary plasmacytoma of the colon: A case report. S Afr Med J. 1977;51(24):893–5. [PubMed] [Google Scholar]
- 12.Ajanaku F, Mekasha G, Scott V. Extramedullary plasmacytoma of the colon. Am J Gastroenterol. 2019;114:S908. [Google Scholar]
- 13.Iqbal QUA, Majid HJ. Plasmacytoma. StatPearls Publishing: Treasure Island (FL), 2022. [PubMed] [Google Scholar]
- 14.Solitary or Extramedullary Plasmacytoma. Memorial Sloan Kettering Cancer Center (https://www.mskcc.org/cancer-care/types/multiple-myeloma/other-plasma-cell-diseases/solitary-plasmacytoma#:∼:text=However%2C%2070%20percent%20of%20people,with%20a%20stem%20cell%20transplant). (1970, January 1). Accessed January 5, 2023. [Google Scholar]
- 15.Ellington TD, Henley SJ, Wilson RJ, Wu M, Richardson LC. Trends in solitary plasmacytoma, extramedullary plasmacytoma, and plasma cell myeloma incidence and myeloma mortality by racial-ethnic group, United States 2003-2016. Cancer Med. 2021;10(1):386–95. [DOI] [PMC free article] [PubMed] [Google Scholar]



