Abstract
Background
Dietary intake during early childhood can have implications on child health and developmental trajectories. Early childhood education and care (ECEC) services are recommended settings to deliver healthy eating interventions as they provide access to many children during this important period. Healthy eating interventions delivered in ECEC settings can include strategies targeting the curriculum (e.g. nutrition education), ethos and environment (e.g. menu modification) and partnerships (e.g. workshops for families). Despite guidelines supporting the delivery of healthy eating interventions in this setting, little is known about their impact on child health.
Objectives
To assess the effectiveness of healthy eating interventions delivered in ECEC settings for improving dietary intake in children aged six months to six years, relative to usual care, no intervention or an alternative, non‐dietary intervention. Secondary objectives were to assess the impact of ECEC‐based healthy eating interventions on physical outcomes (e.g. child body mass index (BMI), weight, waist circumference), language and cognitive outcomes, social/emotional and quality‐of‐life outcomes. We also report on cost and adverse consequences of ECEC‐based healthy eating interventions.
Search methods
We searched eight electronic databases including CENTRAL, MEDLINE, Embase, CINAHL, PsycINFO, ERIC, Scopus and SportDiscus on 24 February 2022. We searched reference lists of included studies, reference lists of relevant systematic reviews, the World Health Organization International Clinical Trials Registry Platform, ClinicalTrials.gov and Google Scholar, and contacted authors of relevant papers.
Selection criteria
We included randomised controlled trials (RCTs), including cluster‐RCTs, stepped‐wedge RCTs, factorial RCTs, multiple baseline RCTs and randomised cross‐over trials, of healthy eating interventions targeting children aged six months to six years that were conducted within the ECEC setting. ECEC settings included preschools, nurseries, kindergartens, long day care and family day care. To be included, studies had to include at least one intervention component targeting child diet within the ECEC setting and measure child dietary or physical outcomes, or both.
Data collection and analysis
Pairs of review authors independently screened titles and abstracts and extracted study data. We assessed risk of bias for all studies against 12 criteria within RoB 1, which allows for consideration of how selection, performance, attrition, publication and reporting biases impact outcomes. We resolved discrepancies via consensus or by consulting a third review author. Where we identified studies with suitable data and homogeneity, we performed meta‐analyses using a random‐effects model; otherwise, we described findings using vote‐counting approaches and via harvest plots. For measures with similar metrics, we calculated mean differences (MDs) for continuous outcomes and risk ratios (RRs) for dichotomous outcomes. We calculated standardised mean differences (SMDs) for primary and secondary outcomes where studies used different measures. We applied GRADE to assess certainty of evidence for dietary, cost and adverse outcomes.
Main results
We included 52 studies that investigated 58 interventions (described across 96 articles). All studies were cluster‐RCTs. Twenty‐nine studies were large (≥ 400 participants) and 23 were small (< 400 participants). Of the 58 interventions, 43 targeted curriculum, 56 targeted ethos and environment, and 50 targeted partnerships. Thirty‐eight interventions incorporated all three components. For the primary outcomes (dietary outcomes), we assessed 19 studies as overall high risk of bias, with performance and detection bias being most commonly judged as high risk of bias.
ECEC‐based healthy eating interventions versus usual practice or no intervention may have a positive effect on child diet quality (SMD 0.34, 95% confidence interval (CI) 0.04 to 0.65; P = 0.03, I2 = 91%; 6 studies, 1973 children) but the evidence is very uncertain. There is moderate‐certainty evidence that ECEC‐based healthy eating interventions likely increase children's consumption of fruit (SMD 0.11, 95% CI 0.04 to 0.18; P < 0.01, I2 = 0%; 11 studies, 2901 children). The evidence is very uncertain about the effect of ECEC‐based healthy eating interventions on children's consumption of vegetables (SMD 0.12, 95% CI −0.01 to 0.25; P =0.08, I2 = 70%; 13 studies, 3335 children). There is moderate‐certainty evidence that ECEC‐based healthy eating interventions likely result in little to no difference in children's consumption of non‐core (i.e. less healthy/discretionary) foods (SMD −0.05, 95% CI −0.17 to 0.08; P = 0.48, I2 = 16%; 7 studies, 1369 children) or consumption of sugar‐sweetened beverages (SMD −0.10, 95% CI −0.34 to 0.14; P = 0.41, I2 = 45%; 3 studies, 522 children).
Thirty‐six studies measured BMI, BMI z‐score, weight, overweight and obesity, or waist circumference, or a combination of some or all of these. ECEC‐based healthy eating interventions may result in little to no difference in child BMI (MD −0.08, 95% CI −0.23 to 0.07; P = 0.30, I2 = 65%; 15 studies, 3932 children) or in child BMI z‐score (MD −0.03, 95% CI −0.09 to 0.03; P = 0.36, I2 = 0%; 17 studies; 4766 children). ECEC‐based healthy eating interventions may decrease child weight (MD −0.23, 95% CI −0.49 to 0.03; P = 0.09, I2 = 0%; 9 studies, 2071 children) and risk of overweight and obesity (RR 0.81, 95% CI 0.65 to 1.01; P = 0.07, I2 = 0%; 5 studies, 1070 children).
ECEC‐based healthy eating interventions may be cost‐effective but the evidence is very uncertain (6 studies). ECEC‐based healthy eating interventions may have little to no effect on adverse consequences but the evidence is very uncertain (3 studies).
Few studies measured language and cognitive skills (n = 2), social/emotional outcomes (n = 2) and quality of life (n = 3).
Authors' conclusions
ECEC‐based healthy eating interventions may improve child diet quality slightly, but the evidence is very uncertain, and likely increase child fruit consumption slightly. There is uncertainty about the effect of ECEC‐based healthy eating interventions on vegetable consumption. ECEC‐based healthy eating interventions may result in little to no difference in child consumption of non‐core foods and sugar‐sweetened beverages. Healthy eating interventions could have favourable effects on child weight and risk of overweight and obesity, although there was little to no difference in BMI and BMI z‐scores. Future studies exploring the impact of specific intervention components, and describing cost‐effectiveness and adverse outcomes are needed to better understand how to maximise the impact of ECEC‐based healthy eating interventions.
Plain language summary
How successful are healthy eating programmes in preschools, kindergartens and childcare settings?
Key messages
• Healthy eating programmes delivered in early childhood education and care (ECEC) settings (e.g. preschools, kindergarten, family day care) may improve child diet quality, likely increase fruit consumption, may have favourable effects on vegetable consumption, and likely have no impact on consumption of less healthy foods and sugar‐sweetened drinks. They may have favourable effects on child weight and may reduce the risk of being overweight or obese.
• We don't know if healthy eating interventions save money or cause unwanted effects because very few studies provided information about these points.
• We found little evidence from low‐ and middle‐income countries, but healthy eating programmes in high‐income countries may benefit child health. We don't know how to support educators and staff to implement these programmes in practice. We need more research about delivering programmes and about their effect in low‐income countries.
Why is it important to improve young children's diet?
Having a poor diet puts people at risk of many long‐term diseases including heart disease, type 2 diabetes and certain types of cancers. Research estimates that over 11 million deaths worldwide are caused by having an unhealthy diet. Dietary behaviours and preferences are established early in life and persist into adulthood.
What are healthy eating programmes?
Healthy eating programmes aim to encourage children to eat a healthier diet. They may involve changes to lessons and the culture in preschools, kindergartens and day care centres (early childhood education and care (ECEC) settings), and working with children's families, teachers and healthcare staff. For example, introducing new fruits and vegetables to children, changing the menu to include healthier options or providing families with information about child healthy eating. Healthy eating programmes may establish lifelong healthy eating patterns, reduce excessive weight gain and improve overall health.
What did we want to find out?
We wanted to find out what impact healthy eating interventions have on child diet and health. We were interested in changes to diet, weight, language and cognitive performance, social, emotional and quality of life outcomes in children aged six months to six years attending preschool, long day care, nurseries, kindergartens and family day care services. We also wanted to know the cost of interventions and whether they had any potential unwanted effects.
What did we do?
We searched for studies that compared healthy eating programmes against no action, delayed delivery of the programme, or a programme that did not aim to change child diet.
We compared and summarised the results of the studies and rated our confidence in the evidence, based on factors such as study methods and sizes.
What did we find?
We found 52 studies that looked at the effects of 58 healthy eating programmes in ECEC settings for children aged six months to six years. All studies were published in high and high‐middle‐income countries. The programmes were very different from each other. They:
• lasted from 4 weeks to 3 years;
• were delivered by a range of people including healthcare providers, ECEC staff, and researchers;
• used different delivery methods (telephone, face‐to‐face, online, printed materials); and
• measured results in a variety of ways (e.g. parent or staff surveys, observations of children's eating, and weighing foods before and after meals).
Overall, the programmes aimed to:
• change the ECEC environment (e.g. staff demonstrated healthy eating to children, and provided healthier foods);
• change the curriculum (e.g. they provided lessons about foods and healthy eating); and
• establish partnerships (e.g. they provided educational resources to families); and
• increase children's physical activity (e.g. by structured physical activity lessons and encouraging less screen time).
Healthy eating programmes may lead to small improvements in child diet quality, increase fruit consumption by 0.11 servings, potentially improve vegetable consumption by 0.12 servings and may have no effect on consumption of less healthy foods and sugar‐sweetened drinks. Further, we found child weight is potentially reduced by 230 g and for every 100 children, 19 would have better weight status. However, we found no evidence of impact on body mass index. The programmes may be cost‐effective and likely to have no unwanted effects, although few studies reported these points. Few studies reported on other learning, social and developmental outcomes.
What are the limitations of the evidence?
Our confidence in the evidence is low because the healthy eating programmes were conducted, delivered and assessed in different ways. Also, many of the people who received the healthy eating programmes were aware that they were being assessed and this can sometimes influence how they report their effects. For example, parents who reported their child's diet may have been more inclined to give positive answers because they felt they were doing what society expected or because they were grateful for the support and wanted to please the researchers. Also, not all studies provided information about everything we were interested in and there was often missing data when children were followed up after the study.
How up‐to‐date is the evidence?
The evidence is up‐to‐date to February 2022.
Summary of findings
Summary of findings 1. Comparison of early childhood education and care‐based healthy eating interventions for improving the diet of children aged six months to six years.
| Comparison of early childhood education and care‐based healthy eating interventions for improving the diet of children aged six months to six years | ||||||
| Patient or population: children aged six months to six years Setting: ECEC services (including centre‐based and family day care) Intervention: healthy eating interventions Comparison: no intervention (including usual care, minimal support or delayed intervention) or alternative, non‐dietary intervention | ||||||
| Outcome | Anticipated absolute effects (95% CI)* | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | What happens | |
| Risk with control | Risk with healthy eating interventions | |||||
| Diet quality | Mean score (SD) of 57.80 (10.82)a on the Healthy Eating Index (scale 0–100 points; higher scores = better diet quality) | SMD of 0.34 is equivalent to a score 3.68 points better in diet quality | SMD 0.34 SD higher (0.04 higher to 0.65 higher) | 1973 children (6 RCTs) | ⨁◯◯◯ Very lowb | ECEC‐based healthy eating interventions may increase diet quality slightly but the evidence is very uncertain. |
| Fruit consumption | Mean (SD) servings of fruit 2.06 (1.15)c | SMD of 0.11 is equivalent to an increase of 0.13 servings of fruit | SMD 0.11 SD higher (0.04 higher to 0.18 higher) | 2901 children (11 RCTs) |
⨁⨁⨁◯ Moderated | ECEC‐based healthy eating interventions likely increase fruit consumption slightly. This increase corresponds to approximately 20% of the daily in‐care fruit requirements for this age group. We were unable to pool 7 studies in the meta‐analysis; 4 studies reported positive effects of the intervention, while 3 studies reported negative effects. |
| Vegetable consumption | Mean (SD) servings of vegetables 1.50 (1.18)c | SMD of 0.12 is equivalent to an increase of 0.14 servings of vegetables | SMD 0.12 SD higher (0.01 lower to 0.25 higher) | 3335 children (13 RCTs) |
⨁◯◯◯ Very lowe | The evidence is very uncertain about the effect of ECEC‐based healthy eating interventions on child consumption of vegetable servings. We were unable to pool 8 studies in the meta‐analysis 7 studies reported positive effects of the intervention, while 1 study reported negative effects. |
| Non‐core foods (i.e. less healthy or discretionary) consumption | Times non‐core foods were consumed: mean 0.6; SD 0.85f | SMD of −0.05 is equivalent to 0.04 less times non‐core foods were consumed | SMD 0.05 SD lower (0.17 lower to 0.08 higher) | 1369 children (7 RCTs) | ⨁⨁⨁◯ Moderateg | ECEC‐based healthy eating interventions likely result in little to no difference in non‐core foods consumption. We were unable to pool 3 studies in the meta‐analysis; 2 studies reported favourable effects of the intervention, while 1 study reported unfavourable effects. |
| Sugar‐sweetened beverage consumption | Portions or servings: mean 1.85; SD 1.60c | SMD of −0.10 is equivalent to 0.16 fewer portions or servings of sugar‐sweetened beverages | SMD 0.10 SD lower (0.34 lower to 0.14 higher) | 522 children (3 RCTs) |
⨁⨁⨁◯ Moderateh | ECEC‐based healthy eating interventions likely result in little to no difference in sugar‐sweetened beverage consumption. We were unable to pool 3 studies in the meta‐analysis; 2 studies reported favourable effects and 1 study reported unfavourable effects of the intervention. |
| Cost‐effectiveness | 6 studies reported on various intervention costs (i.e. total cost of intervention, projected lifetime savings, cost for participants, average cost‐effectiveness ratio, and relative value index) as measured via surveys, records or logs. 1 study reported that healthy eating interventions were cost‐effective, 2 studies reported cost per child, and 3 studies reported intervention delivery costs, all of which varied across studies. | ‐ | 101 services (6 RCTs) |
⨁◯◯◯ Very lowi | ECEC‐based healthy eating interventions may be cost‐effective but the evidence is very uncertain. | |
| Adverse consequences | 3 studies reported no additional adverse consequences (i.e. incidents, negative feedback or parent complaints) as measured via staff self‐report. | ‐ | 62 services (3 RCTs) |
⨁◯◯◯ Very lowj | ECEC‐based healthy eating interventions may have little to no effect on adverse consequences but the evidence is very uncertain. | |
| * The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% confidence interval). The basis of assumed risk is provided in footnotes. CI: confidence interval; ECEC: early childhood education and care; RCT: randomised controlled trial; SD: standard deviation; SMD: standardised mean difference | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aBaseline estimates and standard deviation used from Vaughn 2021. bDowngraded one level for risk of bias: three RCTs were assessed as high risk of bias across three domains and one RCT was assessed a high risk of bias across one domain. Downgraded two levels for heterogeneity: I2 = 91%; > 75% considered considerable heterogeneity. Downgraded one level as publication bias was strongly detected via visual inspection of funnel plots, which indicated two outliers. cBaseline estimates and standard deviation used from Kornilaki 2021. dDowngraded one level for risk of bias: seven RCTs were assessed as high risk of bias across three or more domains, two RCTs were assessed high risk of bias across two domains. eDowngraded one level for risk of bias: eight RCTs were assessed as high risk of bias across three or more domains, three RCTs were assessed high risk of bias across two domains. Downgraded one level for heterogeneity: I2 = 70%; 50%‐75% considered substantial heterogeneity. Downgraded one level as publication bias was strongly suspected from visual inspection of funnel plots, which indicated an outlier. fBaseline estimates and standard deviation used from Yoong 2020a. gDowngraded one level for risk of bias: five RCTs were assessed as high risk of bias across three or more domains, two RCTs were assessed high risk of bias across two domains. hDowngraded one level for risk of bias: two RCTs were assessed as high risk of bias across three or more domains. iDowngraded one level for heterogeneity as there was some degree of heterogeneity of the measures used to assess this outcome. Downgraded two levels for indirectness as RCTs did not directly answer this research question, with different outcomes assessed. Downgraded two levels for imprecision due to small number of services analysed: 101 services were included in cost analysis. Downgraded one level for publication bias as RCTs were relatively small, all including fewer than 50 services; publication bias may be present. jDowngraded one level for indirectness as RCTs did not directly answer this research question, although similar outcomes were assessed. Downgraded two levels for imprecision due to small number of services analysed: 62 services were included in the analysis of this outcome. Downgraded one level for publication bias: all four RCTs were relatively small, all including fewer than 40 services for this outcome analysis; publication bias may be present.
Background
Description of the condition
Dietary risk factors, including low fruit and vegetable consumption and consumption of non‐core foods high in sodium, are the primary causes of death and disability globally (GBD 2017 Diet Collaborators). In 2017, dietary risk factors were collectively responsible for 11 million deaths and 255 million disability adjusted life years (DALYs) among adults (GBD 2017 Diet Collaborators). Extensive epidemiological evidence documents the association between poor diet and a range of chronic conditions including ischaemic heart disease, diabetes, respiratory diseases and certain types of gastrointestinal cancers (World Cancer Research Fund 2018). Internationally, both adults and children from low‐, medium‐ and high‐income countries do not meet population dietary recommendations for fruit, vegetables and whole‐grain foods, and overconsume non‐core foods (i.e. less healthy/discretionary foods) including sugar‐sweetened beverages, processed meats and sodium (Development Initiatives 2018; GBD 2017 Diet Collaborators).
Early childhood is a foundational period for establishing healthy eating patterns that track into later life. A number of longitudinal studies show that dietary intake in early childhood can influence child growth, general health and developmental trajectories (Guerrero 2016; Koning 2016; Shrestha 2015; Waxman 2003). For example, unhealthy dietary intake in children as young as three years of age has been found to influence cardiovascular disease markers, including obesity, dyslipidaemia and high blood pressure, which can persist into adulthood (Berenson 1998; Castellano 2014; Rodrigues 2013; Turco 2018). Additionally, longitudinal studies demonstrate that the consumption of fruit and vegetables in childhood persist into later childhood and is associated with reductions in non‐communicable diseases in adulthood (Maynard 2003; Ness 2005).
Description of the intervention
Leading health authorities, including the World Health Organization (WHO), have identified early childhood and education care (ECEC) services as important settings for public health action to promote child healthy eating (WHO 2012). These settings typically provide care, education and developmental activities for children outside their home, prior to formal compulsory schooling. ECEC services reach a large number of children aged up to six years (approximately 80% to 90% of young children in high‐income countries) for prolonged periods of time (up to 30 hours per week; Baxter 2015; European Commission 2021; Kamerman 2007; OECD 2019). In many countries, children attend such services for the majority of the day, where they consume up to 70% of their daily energy requirements (Soanes 2001). In addition, authorities in many countries have developed regulations and guidelines for the sector that recommend that ECEC services create health‐promoting environments to support young children with achieving recommendations outlined in national dietary guidelines (Australian Government 2009; Benjamin‐Neelon 2011; Jackson 2021).
Given this, healthy eating interventions delivered in ECEC present a significant opportunity to improve population dietary intake and reduce the burden of disease associated with dietary risk factors. A Cochrane systematic review examining interventions to improve fruit and vegetable intake in preschool‐aged children (including both in attendance at ECEC and at home) found some evidence that child‐feeding interventions and multicomponent interventions significantly increased child fruit and vegetable intake (Hodder 2020). Previous reviews, which have included a range of study designs, have also explored characteristics of ECEC settings associated with child diet (Matwiejczyk 2018; Van de Kolk 2019; Ward 2015; Yoong 2020b). These reviews report that several ECEC policies and practices, including: ECEC educator feeding practices (Ward 2015); increasing the availability and exposure to healthier options; increasing knowledge of educators and children via healthy eating education; parental/carer involvement; and supportive healthy eating policies (Matwiejczyk 2018; Van de Kolk 2019), may be associated with improved child dietary intake within the setting.
How the intervention might work
A number of theories and models have been used to explain how ECEC‐based healthy eating interventions may work to influence child dietary intake. These include the socio‐ecological model, social cognitive theory and social learning theory (Matwiejczyk 2018). Collectively, these theories posit that behaviour (e.g. child dietary intake) is influenced by a combination of personal and environmental factors and the social interactions and context in which these experiences occur, and are important determinants of child behaviour in the early years (Korin 2016; Nixon 2012). They suggest that interventions delivered in ECEC may influence child diet through targeting children and their parents, carers, educators and family (as key social influences), as well as the environmental characteristics that facilitate behaviour change (e.g. food availability). Healthy eating intervention strategies delivered in ECEC might include: the provision of healthy eating education and training to educators and parents/carers (to target knowledge and self‐efficacy); supporting educators to implement positive feeding practices and role model healthy eating (to create a positive environment); modifying the environment of ECEC settings (including interventions to increase the availability of healthier foods and increasing implementation of healthy eating policies); or building partnerships between the service and parents/carers via the provision of resources or family participation in curriculum planning or interactive hands‐on activities (Matwiejczyk 2018; Stacey 2017). Such theories are consistent with the three main components highlighted within the WHO Health Promoting Schools Framework: health curriculum; ethos and environment of schools; and partnerships/engagement with healthcare, community, families or a combination of these (Langford 2014). Although this framework was developed for the school setting, there are similarities in the context, structure and operational characteristics of ECEC settings and schools, and as such will be used to characterise interventions included within this review.
Why it is important to do this review
Despite recommendations to implement healthy eating programmes in ECEC, little is known about the impact of ECEC‐based interventions on child dietary outcomes. An umbrella review of 12 systematic reviews describing healthy eating interventions in the ECEC setting reported mixed findings surrounding the effectiveness of such interventions on child diet (Matwiejczyk 2018). The most recent review describing ECEC‐specific healthy eating interventions included 71 studies of any design published up to April 2015, and undertook a narrative synthesis of included studies (Sisson 2016). Using vote‐counting approaches, the review found that 87% of included healthy eating interventions (n = 39) delivered in ECEC had the intended effect on the target behaviour. Although more recent systematic reviews that include ECEC‐based healthy eating interventions have been published (Morgan 2020; Nathan 2019; Van de Kolk 2019), none have summarised the evidence from randomised controlled trials (RCTs), which provide the most direct evidence of intervention effectiveness. Further, many previous reviews have lacked important information relevant to support decision‐making and guide future practice, including cost‐effectiveness of such interventions, their broader co‐benefits (e.g. social/emotional and language and cognition), the presence of any unintended adverse consequences or their impacts on health equity (Wolfenden 2009). Such information is considered to be particularly important to support healthcare decision‐making and allow for optimal allocation of resources.
As such, there remains considerable uncertainty overall regarding the impact of healthy eating interventions delivered in the ECEC setting, the components that may be associated with child dietary intake, the potential benefits on other child outcomes and limited detail on outcomes of interest (e.g. adverse consequences, economic analysis) to guide policy makers and practitioners in deciding to invest in such programmes for population‐level implementation.
Objectives
To assess the effectiveness of healthy eating interventions delivered in ECEC settings for improving dietary intake in children aged six months to six years, relative to usual care, no intervention or an alternative, non‐dietary intervention. The specific primary dietary outcomes included were: i) diet quality; ii) fruit consumption; iii) vegetable consumption; iv) fruit and vegetable consumption combined; v) non‐core foods (i.e. less healthy/discretionary foods) consumption; and vi) sugar‐sweetened beverage consumption.
Secondary objectives were to assess the impact of ECEC‐based healthy eating interventions on child physical outcomes (e.g. child BMI, BMI z‐score, weight, risk of overweight and obesity); language and cognitive outcomes (e.g. assessment of general development, early executive function); social/emotional outcomes (e.g. outcomes related to mental and behavioural outcomes); and quality‐of‐life outcomes. The review also summarised any cost/economic analysis and related adverse consequences of ECEC‐based healthy eating interventions.
Methods
Criteria for considering studies for this review
Types of studies
This review included RCTs (including cluster‐RCTs, stepped‐wedge RCTs, factorial RCTs, multiple baseline RCTs, and randomised cross‐over trials) as these designs are considered the highest quality to establish causality and quantify intervention effects (McKenzie 2022b).
We excluded cluster‐RCTs with fewer than two intervention sites and two control sites, as per Cochrane Effective Practice and Organisation of Care (EPOC) recommendations (EPOC 2021).
Types of participants
The primary targets of the interventions of the included studies were children aged between six months and six years (inclusive). Theories and models, such as the social ecological model, posit that child behaviour is influenced by individual, interpersonal, organisational, community and public policy factors (Korin 2016). As such, interventions that target parents, carers and ECEC staff as part of healthy eating interventions were also included as they are the primary providers of food to children and strongly influence child behaviour in the early years.
Participants in the studies included:
children aged between six months to six years (inclusive) attending the ECEC service. Studies including children older than six years were included if the mean age of the study sample at baseline was six years or under or if more than 50% of the included population were aged six months to six years;
parents, guardians or carers responsible for the care of children aged six months to six years; and
professionals responsible for care provided to children attending the ECEC service, including service directors, educators, volunteers, cooks, or other employed staff.
We excluded studies that exclusively targeted children aged between zero and six months, as dietary interventions are likely different for this group, who rely solely on breast milk/human milk substitutes as their primary sources of nutrients. Studies targeting children with special needs or clinical conditions (e.g. those with a diagnosed disease or health condition) were also excluded due to potential differences in feeding practices or nutrition requirements.
Types of interventions
The review included healthy eating interventions that were delivered within an ECEC service to facilitate healthy eating for young children. The ECEC setting consists of formal paid or government‐subsidised services such as preschools, nurseries, long day‐care centres and kindergartens, as well as family day‐care services (also known as family child‐care homes and child minding, in which a small group of children is offered care within the educator’s home), that offer care for children six years and under, prior to compulsory schooling (OECD 2014). We included interventions that targeted both the ECEC and other settings, such as the home, as long as the intervention was primarily delivered in ECEC (i.e. assessed as more than 50% of the intervention strategies were delivered within ECEC services or influenced the operation of ECEC services, or both).
For this review, healthy eating interventions could target children, parents, caregivers or educators' behaviour, centre environments, or broader policy context or other environments, or a combination of any of the above, that aimed to influence child diet. The WHO Health Promoting Schools Framework highlights three components that are integral to supporting settings‐based health promotion, including: health curriculum; ethos and environment of schools; and partnerships/engagement with healthcare, community, families or a combination of these (Langford 2014). Specifically, the type of interventions are likely to include health curriculum (e.g. healthy eating education, formal and informal teaching and learning experiences to children), ethos and environment (e.g. healthy eating policies, food availability, food service modification, staff training, nudge interventions) and partnerships or engagement (e.g. working with other organisations in the community, parents, families, healthcare providers).
To be eligible, interventions were required to include at least one Health Promoting Schools' component targeting child diet in the ECEC setting. Interventions that targeted other risk factors were included as long as there was a clear intervention component that sought to influence child diet. Both single‐ and multi‐component interventions (i.e. interventions that include more than one component to influence child diet) were included. There were no restrictions on intervention duration.
We excluded interventions that focused specifically on examining malnutrition or malnourishment, as well as those focusing on obesity‐management interventions (i.e. those that only included children classified as overweight or obese).
Control
We included studies that reported the outcomes of an intervention versus no intervention (control), delayed intervention (wait‐list control), an active, alternative intervention that did not directly seek to influence child diet, or usual care. Some examples of usual care include the delivery of specific jurisdiction‐funded health promotion programmes that target healthy eating in ECEC services (e.g. Munch & Move within New South Wales, Australia (Hardy 2010)), and subsidised programmes specifically targeting low‐income populations (e.g. the Child and Adult Care Food Program in the USA (Chriqui 2020)). These programmes typically include training and support for ECEC providers to promote healthier food environments. We excluded studies that compared two healthy eating interventions only (with no control) as the review was primarily focused on understanding the effect of ECEC‐based healthy eating interventions overall relative to a control, usual care or non‐healthy eating intervention.
Types of outcome measures
We included studies only if they measured at least one dietary or physical (i.e. anthropometric) outcome. We only included studies that had a follow‐up assessment that was at least three months or longer from baseline, regardless of active intervention length, as we were interested in understanding the longer‐term impact of healthy eating interventions delivered in the ECEC setting.
Primary outcomes
Given the number of dietary outcomes examined within the studies, we limited our analysis of child dietary intake outcomes to those outlined in a core outcome set for early intervention studies to prevent obesity in early childhood (Brown 2022). Such measures included assessments of child intake that occurred during attendance at ECEC or overall dietary intake.
This included:
overall diet quality (typically diet scores measuring the amount, quality and variety of foods consumed in a child's diet);
consumption of fruit or vegetables, or fruit and vegetables combined (g/servings, percentage of children consuming);
consumption of non‐core foods as defined by the study (g/servings/times, percentage of children consuming); and
consumption of sugar‐sweetened beverages (g/ounces/mL).
Studies captured dietary intake using objective methods, such as plate waste audits or direct observations (Ball 2007), as well as subjective methods (e.g. parent‐reported dietary intake), such as short diet questions, food frequency questionnaires, food diaries and 24‐hour recalls. We excluded measures of foods or beverages that did not directly assess child consumption such as food provided to children (i.e. served or listed on ECEC menus), purchasing and selection of food and beverages.
Secondary outcomes
We included the following secondary outcomes.
Physical outcomes
We focused primarily on child anthropometry as outlined in the core outcome set for early childhood obesity prevention studies (Brown 2022). We included both objective (measured by trained researchers or ECEC staff) and subjective (parent‐reported) measures of anthropometry.
This included:
absolute weight in kilograms (kg);
Body mass index (BMI);
BMI z‐score (using age‐appropriate cut‐offs (WHO 2021));
risk of overweight and obesity; and
waist circumference.
Language and cognitive performance outcomes
We included any measure of child language and cognitive performance (Lichtenberger 2005). This was likely to be subjective measures related to academic performance and cognitive function (parent‐ or ECEC staff‐reported assessments) and could include:
Kaufman Assessment Battery for Children (Lichtenberger 2009);
Wechsler Preschool and Primary Scale of Intelligence (Wechsler 1989); and
The Early Years Toolbox for Assessing Early Executive Function, Language, Self‐Regulation, and Social Development (Howard 2017).
Social/emotional outcomes
We included any measure of child social and emotional outcomes. This was likely to be subjective measures (e.g. parent‐ or ECEC staff‐reported assessments) related to mental health, emotional regulation and social behaviour (e.g. Child Social Behavior Questionnaire (Warden 2003)).
Quality‐of‐life outcomes
We included any measure of child quality of life. This was likely to be subjective measures reported by parents or ECEC staff (e.g. the Paediatric Quality of Life Inventory (Varni 2001)).
Cost
We included any estimates of the intervention absolute cost or assessment of the intervention cost‐effectiveness, as assessed via internal project records, questionnaires or other measures. This could include:
crude cost of programme to service;
cost‐effectiveness ratio;
intervention delivery costs;
average cost‐effectiveness ratio; and
relative value index.
Adverse consequences
We included any unintended adverse consequences of the interventions that could be assessed via questionnaires, surveys, direct observations, or ECEC service audits, and may be related to:
child health (e.g. potential child injury (burns, cuts) during experiential learning activities); and
staff or parent attitudes (e.g. complaints about healthy eating policies, feedback).
We excluded adverse consequences related to participation in the non‐healthy eating component of interventions (e.g. injuries from participation in physical activity lessons).
Search methods for identification of studies
We undertook a search based on the search strategy used in a previously conducted Cochrane Review (Wolfenden 2020), adapted by a research librarian (DB) to suit our research question. The search was based on the following domains using Medical Subject Headings (MeSH) for ‘diet/nutrition’ and ‘ECEC’ and ‘RCT’ and ‘humans’ (Glanville 2020). Our search terms for each electronic database are outlined in Appendix 1.
Electronic searches
We undertook a systematic search using the following databases on 24 February 2022:
Cochrane Central Register of Controlled Trials (CENTRAL; 2022, Issue 2) in the Cochrane Library;
MEDLINE (OVID) (1946 to present);
Embase (OVID) (1947 to present);
CINAHL Complete (EBSCO) (Cumulative Index to Nursing and Allied Health Literature; 1937 to present);
PsycINFO (OVID) (1806 to present);
ERIC (Proquest) (1966 to present);
SCOPUS (Scopus) (1996 to present); and
SPORTDiscus (EBSCO) (1930 to present).
We placed no language or time restrictions on the searches.
Searching other resources
Unpublished or grey literature searches
In addition to electronic database searches, we searched for relevant unpublished or grey literature publications using the following terms; 'childcare centre and/or center' and 'nutrition intervention':
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch);
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov); and
Google Scholar (scholar.google.com.au) (first 100 results).
Searching other resources
Additional searches included:
handsearching reference lists of included studies;
handsearching reference lists of relevant systematic reviews identified in the electronic search strategy; and
contacting authors of relevant protocol papers identified by the electronic database searches.
Data collection and analysis
Selection of studies
Pairs of review authors (SY, ML, AL, JJ, CB, NP, SMc, LD, AG, TMcD) independently screened titles and abstracts of all studies using Covidence software. We resolved conflicts via consensus and via discussion with a third review author where necessary.
We obtained full‐text articles for any study that could not clearly be excluded on the basis of study title and abstract. Pairs of review authors (SY, ML, AL, JJ, CB, LD, AG, TMcD) independently reviewed full‐text articles in Covidence for their eligibility. Where we were unable to resolve discrepancies by consensus, we consulted a third review author to inform study inclusion. Authors of potentially relevant studies (SY, LW, CB, NP, JZJ, AG) were not involved in screening and adjudication for studies in which they were involved at title or full‐text stage.
Data extraction and management
Pairs of independent, unblinded review authors (SY, ML, CB, JZJ, CL, JJ, AL, NP, SMc, TMcD) extracted data independently for included studies, using Microsoft Excel. A third review author (SY, AG, JJ) assessed any discrepancies for final decision‐making.
For included studies, we used a piloted and adapted version of the Cochrane Public Health data extraction template to extract data on the following.
Study characteristics: first author, publication year, country, study design, sample size
ECEC characteristics: type of service (centre‐based (preschool or long day care) or family day care), operational characteristics (public or private; full‐time or part‐time), location (urban or rural), socioeconomic characteristics (low‐, middle‐ or high‐income)
Participant characteristics: age, gender, ethnicity, socioeconomic status
Intervention characteristics: name of the programme, intervention description, duration, intensity of the intervention, intervention components, settings, dose and where they are implemented, statistical analysis, and classification according to the WHO Health Promoting Schools Framework
Outcome definitions and time points of outcome measurement
Study results relevant to our review outcomes
Dropout rate
Financial cost of the intervention
Unintended adverse consequences of the intervention
Funding source
Conflict‐of‐interest statements
When data were only available in graph form, we extracted them using an online graph reader (automeris.io/WebPlotDigitizer).
We extracted data on all relevant outcomes, however, limited our analysis to that described above.
Authors of included studies (SY, LW, CB, NP, JZJ, AG) were not involved in the data extraction or risk of bias assessments for these studies.
Assessment of risk of bias in included studies
Two review authors (LD, ML, TD, AG, JJ) independently assessed risk of bias for individual studies, using the Cochrane risk of bias tool (RoB 1), described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), consistent with that outlined in the review protocol (Yoong 2021). Where required, a third review author (SY, ML for where SY was an author) adjudicated discrepancies regarding risk of bias that could not be resolved via consensus. We undertook data extraction in Microsoft Excel and assessed the following domains.
random sequence generation (selection bias);
allocation concealment (selection bias);
blinding of participants and research personnel by each outcome (detection bias);
blinding of outcome assessment for each outcome (detection bias);
incomplete outcome data reporting for each outcome (attrition bias);
selective outcome reporting (reporting bias); and
other sources of bias.
Where applicable, we also assessed risk of bias domains that are specific to cluster‐RCTs, including:
recruitment bias;
baseline imbalance;
loss of clusters;
incorrect analysis; and
contamination.
For studies that reported data on cost or adverse consequences in the intervention groups only, we assessed the following risk of bias domains, as we decided that other types of bias would not impact on these outcomes due to the nature of the design:
random sequence (selection bias);
allocation (selection bias);
performance bias;
detection bias;
attrition bias; and
reporting bias.
Based on risk of bias assessment, we judged risk of bias as ‘low’, ‘high’, or ‘unclear’ for each domain (Higgins 2011). We defined high overall study risk of bias as scoring high risk on three or more of the assessed risk of bias domains for the primary outcome. We conducted risk of bias assessments at the individual outcome level, as well as by overall study risk of bias (Higgins 2011). The risk of bias outcomes for all outcomes is presented in table form. For the primary outcomes (dietary outcomes), we included these results narratively in text.
Measures of treatment effect
We focused on estimating the main effect of randomisation (i.e. intention to treat). Where two or more studies measured outcomes in the same way, we pooled quantitative measures of the primary and secondary outcomes in either a meta‐analysis or a narrative synthesis. We selected the primary and secondary outcomes that allowed us to best answer the primary review aim.
Where all studies assessed an outcome using the same measure and metric (e.g. BMI, kg) we reported the measure of effect as the mean difference (MD). If studies used different measures or metrics to report the same outcome, we used the standardised mean difference (SMD) as the measure of effect. Where outcomes were binary, we estimated risk ratios (RR). We calculated 95% confidence intervals (CIs) and reported them with all measures of intervention effects (Deeks 2022). We used postintervention values in preference to change‐from‐baseline data, consistent with recommendations in the Cochrane Handbook for Systematic Reviews of Interventions and to maximise the number of studies that could be pooled (Deeks 2022). As all included studies were cluster‐RCTs, we used cluster‐adjusted estimates in our analysis.
Where studies did not provide standard deviations (SDs), we used other measures of variance provided including standard errors, CIs and P values to calculate SDs using the formulas outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2022). For economic outcomes, we undertook a brief economic commentary consistent with that outlined in the Cochrane Handbook for Systematic Reviews of Interventions where sufficient data existed (Aluko 2022).
Unit of analysis issues
We extracted data from all included studies. For all studies, we assessed data at the level of individuals within a cluster level. For cluster‐RCTs that did not appropriately account for clustering, we imputed missing intracluster correlation coefficient (ICC) values with the median ICC of other included studies in this review (median ICC = 0.02; Higgins 2022).
For multi‐arm studies where multiple interventions were relevant to the aims of the review, we combined the estimates from multiple arms as we were interested in the overall impact of healthy eating interventions on child outcomes. We combined these data with data from parallel‐arm studies in the meta‐analyses. For factorial studies, we included only the main effect estimates of the intervention.
In the instance where a single study contributed multiple outcomes for the same group (i.e. one study reporting on two measures of fruit consumption), we selected the measure with the highest quality assessment methods (i.e. validated over non‐validated scale). For studies that used the same questionnaire or measurement method to assess outcomes within the same group (e.g. they used the same questionnaire to assess servings of fruit and proportion of children meeting guidelines for fruit), we selected the measure that allowed for direct comparison with population‐level guidelines (e.g. servings of fruit consumed overall rather than proportion of children consuming fruit) or were most commonly reported in the studies. For studies with multiple follow‐up periods, we used outcome data immediately postintervention where the follow‐up time point was at least three months post‐baseline.
Dealing with missing data
We assessed and reported missing outcome data and dropouts as reported by individual studies, including numbers, characteristics and reasons for dropout, in the included studies. For data that were not reported by individual studies and are essential for the calculation of an effect estimate, variability (e.g. SD) or other values important for inclusion in the meta‐analysis (e.g. ICC), we took the following measures. If possible, we calculated missing values using other reported data in the study (e.g. 95% CIs). Where only the total sample size was reported, we assumed that the groups had equal sizes. We assumed missing ICC values to be 0.02 as this was the median of other studies included in the review. Where additional data were required for inclusion in the meta‐analysis, we contacted the study authors and requested provision of the unpublished data. We documented evidence of potential reporting bias in the risk of bias tables.
Assessment of heterogeneity
We undertook meta‐analysis for our primary and secondary outcomes. We evaluated heterogeneity using forest plots and examined them for asymmetry. In addition, we quantified statistical heterogeneity by calculating the I2 statistic (Higgins 2003). Where study heterogeneity was considerable (defined as I2 > 75%), we carried out prespecified subgroup analyses to explore its causes and present a narrative description of study characteristics to explain heterogeneity (Deeks 2022).
Assessment of reporting biases
We assessed reporting bias by comparing published reports with information provided in trials registers and protocols. We explored reporting bias in each of the meta‐analyses that we conducted by plotting contour‐enhanced funnel plots and visually assessing them for asymmetry and outliers. We also evaluated the presence of reporting bias by undertaking a subgroup analysis comparing smaller (< 400 participants) and larger studies (≥ 400 participants) where there was more than one study in the subgroup.
Data synthesis
The primary analysis included all interventions, as the primary purpose of the review was to assess the impact of healthy eating interventions delivered in ECEC settings on child outcomes. For both primary and secondary review outcomes, we used a random‐effects meta‐analysis to calculate pooled effects due to variation in key study characteristics, including differences in interventions and target participants. A mix of change‐from‐baseline and postintervention measurements were reported across studies and we combined these measurements. For outcomes where studies used the same outcome measure and metric, we estimated the treatment effect as the MD and combined it in one meta‐analysis. This included the following outcomes: BMI, BMI z‐score, absolute weight and waist circumference. For outcomes where studies used different outcome measures or metrics, we calculated the treatment effect as the SMD, and conducted separate meta‐analyses for postintervention scores and change‐from‐baseline scores. We did this for all dietary outcomes, language and cognitive outcomes and social/emotional outcomes. For binary outcomes including risk of overweight and obesity, we reported risk ratios. We completed the analysis using Review Manager Web (RevMan Web 2023) software. Where SMDs were used, we presented the results directly as well as re‐expressed the SMDs to represent more clinically significant outcomes (e.g. servings of foods; Schünemann 2022a).
In instances where studies examined the same underlying constructs (i.e. fruit servings) but we could not combine data in a meta‐analysis (due to insufficient/missing data or outcomes not described in the same way), we conducted a narrative synthesis using vote‐counting approaches based on direction of effect in accordance with the procedures outlined in the Cochrane Handbook for Systematic Reviews of Interventions (McKenzie 2022a). We classified effects based on direction of effect only. An intervention was 'positive' if the effect favoured the intervention and 'negative' if it did not favour the intervention, regardless of whether the effect crossed the null. We also generated harvest plots to provide a visual representation of direction of effect for all relevant dietary outcomes where there were more than two studies using recalculated SMDs where data were available. We presented this by service socioeconomic status and high or low risk of bias, consistent with that prespecified in the protocol (Yoong 2021). For these studies, we calculated SMDs, MDs and relative risks, where sufficient data existed to do so, and described direction of effect where it was not possible to calculate effects (Campbell 2020). For the narrative synthesis, we used vote‐counting approaches to assess the consistency of effects to allow for assessment of certainty.
Subgroup analysis and investigation of heterogeneity
Where there were five or more studies overall and more than one study in each arm, we undertook subgroup analyses by the WHO Health Promoting Schools' components (i.e. health curriculum versus usual care/no intervention, ethos and environment versus usual care/no intervention, and partnerships versus usual care/no intervention) as long as the intervention included the component (regardless of whether it was a multicomponent intervention).
We undertook a subgroup analysis by high‐ and low‐socioeconomic status where there were five or more studies included in the meta‐analysis and more than one study in a subgroup, regardless of level of heterogeneity. Low socioeconomic status was as defined by the primary studies, including: where the majority of participants were located in areas of low socioeconomic status, as reported by the authors in the table of characteristics; only recruiting ECECs participating in programmes targeted at low‐socioeconomic status populations (e.g. Head Start, Child and Adult Care Food Program); or where targeting populations frequently affected by systemic inequities (e.g. African Americans).
We conducted a number of subgroup analyses to explore the potential causes of heterogeneity, where the I2 statistic was more than 75%. Where sufficient data were available (five studies or more studies included and more than one study in each arm), we undertook the following subgroup analyses (all specified a priori):
population: child age (six months to two years (inclusive), and over two years);
intervention: delivery using different modalities (such as telephone, internet, face‐to‐face combined) and delivery by different personnel (research, ECEC staff, healthcare professionals, other experts) and setting (family day care or centre‐based ECEC); and
outcome: outcome assessed at 3 to 12 months from baseline (inclusive) and more than 12 months from baseline.
We did not undertake subgroup analyses by high‐income and low‐/middle‐income countries as no studies took place in low‐ or lower‐middle‐income countries. We conducted subgroup analyses via statistical comparison as recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2022). In this instance, we only interpreted between‐subgroup differences.
Sensitivity analysis
For all outcomes, we undertook a sensitivity analysis excluding studies that we had classified as high risk of bias (defined as assessed as high risk of bias on three or more domains). We also undertook sensitivity analyses excluding any industry‐funded study.
Summary of findings and assessment of the certainty of the evidence
We used GRADE (Guyatt 2011; Schünemann 2022b) to assess the overall certainty of the available evidence for the following review outcomes (i.e. overall diet quality, fruit consumption, vegetable consumption, non‐core foods consumption, sugar‐sweetened beverage consumption; and key anthropometric outcomes including BMI, BMI z‐score, prevalence of overweight and obese, and weight. Additionally, we summarised assessments related to cost data and adverse consequences. We presented these results in the summary of findings table using GRADEpro GDT software. Based on GRADE assessments, we considered level of certainty to be high, moderate, low or very low. This table also reports the number of included studies and participants, the treatment effect estimate and the assessment of the overall certainty of the body of evidence for that outcome. We also converted the SMDs to a common metric for all dietary outcomes. For diet quality, this was the Healthy Eating Index (scale of 0 to 100), for fruit, vegetables and sugar‐sweetened beverages this was servings or portions, and for non‐core foods this was times consumed. Two review authors independently made these assessments (SY, ML, SMc). We involved a third review author where we were unable to reach a consensus.
As per GRADE recommendations, we assessed the outcome measures against five relevant GRADE criteria to obtain an overall GRADE rating and provided an overall level of certainty of the evidence.
We considered the following criteria for lowering the level of certainty:
risk of bias (serious defined as more than 50% of studies with a rating of high risk of bias on three or more domains and very serious as more than 75% of studies with a rating of high risk of bias on three or more domains);
inconsistency (serious defined as I2 statistic ranged between 50% to 75% (inclusive), very serious defined as I2 statistic more than 75%);
indirectness;
imprecision (small total analysed sample in meta‐analysis defined as < 400 participants); and
publication bias.
As all studies were randomised trials, all outcomes began with a rating of high‐certainty evidence and we downgraded them as applicable according to the above criteria. For the outcomes that were summarised and not synthesised via meta‐analysis (i.e. cost and adverse consequences), we used the guidance outlined by Murad 2017 to assess the certainty of the evidence for these outcomes as well as the risk of bias domains described above. We documented our decisions to downgrade the certainty of the evidence for each criterion in the summary of findings table footnotes. In the summary of findings table we included all interventions compared to no intervention, usual‐care control or an alternative, non‐dietary intervention, with a time‐period of three months or more following baseline data collection.
Results
Description of studies
See Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies.
Results of the search
We searched databases from their inception up to 24 February 2022. Results from the electronic search found 31,165 citations (see Figure 1 (Moher 2009)). We identified an additional 470 records from our screening of reference lists of relevant reviews and included studies, and handsearching key journals. Following the removal of duplicates, we screened 20,528 titles and abstracts. Following title and abstract screening, we obtained 203 full texts for full‐text screening.
1.
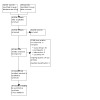
Figure 1: Flow diagram
We included 52 studies that included 58 interventions (described across 96 articles), in this review (Alkon 2014; Başkale 2011; Blomkvist 2021; Céspedes 2013; Davis 2016; De Bock 2011; De Coen 2012; Eliakim 2007; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Grummon 2019; Hodgkinson 2019; Hu 2009; Iaia 2017; Jones 2015; Kipping 2019; Kobel 2019; Kornilaki 2021; Kristiansen 2019; Leis 2020; Lerner‐Geva 2014; Lumeng 2017; Morris 2018; Namenek Brouwer 2013; Natale 2014a; Natale 2014b; Natale 2021; Nekitsing 2019a; Nemet 2011a; Nemet 2011b; Pearson 2022; Peñalvo 2015; Pinket 2016; Puder 2011; Ray 2020; Reyes‐Morales 2016; Roberts‐Gray 2018; Seward 2018; Stookey 2017; Toussaint 2021; Vaughn 2021; Vereecken 2009; Ward 2020a; Witt 2012; Yeh 2018; Yoong 2020a; Zask 2012; Zeinstra 2018).
We contacted authors of 13 included studies (Başkale 2011; De Bock 2011; De Coen 2012; Hodgkinson 2019; Kobel 2019; Lumeng 2017; Morris 2018; Natale 2014a; Natale 2014b; Natale 2021; Peñalvo 2015; Pinket 2016; Stookey 2017) to obtain additional data needed for inclusion in the meta‐analysis and authors from six (46.2%) studies provided such data (Başkale 2011; Kobel 2019; Kornilaki 2021; Lumeng 2017; Morris 2018; Pinket 2016).
Included studies
See Characteristics of included studies.
Most included studies were undertaken in the USA (20 studies; Alkon 2014; Davis 2016; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Grummon 2019; Lumeng 2017; Namenek Brouwer 2013; Natale 2014a; Natale 2014b; Natale 2021; Roberts‐Gray 2018; Stookey 2017; Vaughn 2021; Ward 2020a; Witt 2012; Yeh 2018), Australia (6 studies; Jones 2015; Morris 2018; Pearson 2022; Seward 2018; Yoong 2020a; Zask 2012) and Israel (4 studies; Eliakim 2007; Lerner‐Geva 2014; Nemet 2011a; Nemet 2011b). There were three studies in the UK (Hodgkinson 2019; Kipping 2019; Nekitsing 2019a), two each in Belgium (De Coen 2012; Vereecken 2009), Germany (De Bock 2011; Kobel 2019), the Netherlands (Toussaint 2021; Zeinstra 2018) and Norway (Blomkvist 2021; Kristiansen 2019), and one each in Greece (Kornilaki 2021), Spain (Peñalvo 2015), Colombia (Céspedes 2013), China (Hu 2009), Italy (Iaia 2017), Turkey (Başkale 2011), Canada (Leis 2020), Switzerland (Puder 2011), Finland (Ray 2020), and Mexico (Reyes‐Morales 2016). One study was based in several European countries including Belgium, Bulgaria, Germany, Greece, Poland and Spain (Pinket 2016).
Four studies were conducted in countries classified as upper‐middle‐income (Başkale 2011; Céspedes 2013; Hu 2009; Reyes‐Morales 2016). One cross‐country study was conducted in five high‐income countries and one upper‐middle‐income country (Pinket 2016). The remaining studies were conducted in high‐income countries.
All studies were cluster‐RCTs, with one being a 2 x 2 factorial trial (Nekitsing 2019a).
Forty‐seven studies included one intervention group and one control group (Alkon 2014; Başkale 2011; Céspedes 2013; Davis 2016; De Bock 2011; De Coen 2012; Eliakim 2007; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Grummon 2019; Hodgkinson 2019; Hu 2009; Iaia 2017; Jones 2015; Kipping 2019; Kobel 2019; Kornilaki 2021; Kristiansen 2019; Leis 2020; Morris 2018; Namenek Brouwer 2013; Natale 2014a; Natale 2014b; Natale 2021; Nemet 2011a; Nemet 2011b; Pearson 2022; Peñalvo 2015; Pinket 2016; Puder 2011; Ray 2020; Reyes‐Morales 2016; Roberts‐Gray 2018; Seward 2018; Stookey 2017; Toussaint 2021; Vaughn 2021; Vereecken 2009; Ward 2020a; Witt 2012; Yoong 2020a; Zask 2012; Zeinstra 2018).
Four studies included two intervention groups and one control group (Blomkvist 2021; Lerner‐Geva 2014; Lumeng 2017; Yeh 2018)
One study reported on three intervention groups and one control (Nekitsing 2019a).
Of the 52 control groups:
14 were delayed intervention (Alkon 2014; Céspedes 2013; De Bock 2011; Fernandez‐Jimenez 2019; Grummon 2019; Kornilaki 2021; Kristiansen 2019; Leis 2020; Morris 2018; Namenek Brouwer 2013; Ray 2020; Roberts‐Gray 2018; Vaughn 2021; Zask 2012);
nine were alternative interventions that did not seek to influence child diet (Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Natale 2014a; Natale 2014b; Natale 2021; Ward 2020a); and
29 were usual care (Başkale 2011; Blomkvist 2021; Davis 2016; De Coen 2012; Eliakim 2007; Hodgkinson 2019; Hu 2009; Iaia 2017; Jones 2015; Kipping 2019; Kobel 2019; Lerner‐Geva 2014; Lumeng 2017; Nekitsing 2019a; Nemet 2011a; Nemet 2011b; Pearson 2022; Peñalvo 2015; Pinket 2016; Puder 2011; Reyes‐Morales 2016; Seward 2018; Stookey 2017; Toussaint 2021; Vereecken 2009; Witt 2012; Yeh 2018; Yoong 2020a; Zeinstra 2018).
Usual‐care control services continued their ECEC programme as usual, which may have included receiving training to implement health promotion programmes, which may have been broadly funded within a particular jurisdiction (e.g. Munch & Move in New South Wales, Australia, Sure Start in the UK, Head Start in the USA, Child and Adult Care Food Program in the USA, Mexican Social Security Institute in Mexico).
Two studies were conducted in family day care (Gans 2022; Ward 2020a), while the remaining studies took place in centre‐based care (e.g. preschool, long day care, kindergarten, nurseries). The unit of randomisation was most frequently the ECEC service (e.g. centre‐based care or family day care; 45 studies; Alkon 2014; Başkale 2011; Blomkvist 2021; Céspedes 2013; Davis 2016; De Bock 2011; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Grummon 2019; Hodgkinson 2019; Hu 2009; Iaia 2017; Jones 2015; Kipping 2019; Kobel 2019; Kornilaki 2021; Kristiansen 2019; Leis 2020; Lerner‐Geva 2014; Morris 2018; Namenek Brouwer 2013; Natale 2014a; Natale 2014b; Natale 2021; Nekitsing 2019a; Pearson 2022; Peñalvo 2015; Ray 2020; Reyes‐Morales 2016; Roberts‐Gray 2018; Seward 2018; Stookey 2017; Toussaint 2021; Vaughn 2021; Vereecken 2009; Ward 2020a; Witt 2012; Yeh 2018; Yoong 2020a; Zask 2012; Zeinstra 2018), followed by rooms within an ECEC service (5 studies; Eliakim 2007; Lumeng 2017; Nemet 2011a; Nemet 2011b; Puder 2011), and communities/municipalities (2 studies; De Coen 2012; Pinket 2016).
The majority of studies (n = 48) reported on funding sources.
Two studies reported that they received no funding support (Başkale 2011; Lerner‐Geva 2014).
One study received funding support from industry (Iaia 2017).
Forty‐two studies received funding support from government or charity organisations (Alkon 2014; Blomkvist 2021; Céspedes 2013; Davis 2016; De Bock 2011; De Coen 2012; Eliakim 2007; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Grummon 2019; Hodgkinson 2019; Hu 2009; Jones 2015; Kipping 2019; Kobel 2019; Kristiansen 2019; Leis 2020; Lumeng 2017; Natale 2014a; Natale 2014b; Natale 2021; Nemet 2011a; Nemet 2011b; Pearson 2022; Peñalvo 2015; Pinket 2016; Ray 2020; Reyes‐Morales 2016; Roberts‐Gray 2018; Seward 2018; Stookey 2017; Toussaint 2021; Vaughn 2021; Vereecken 2009; Ward 2020a; Yeh 2018; Yoong 2020a; Zask 2012).
Three studies reported receiving funding support from government or charity organisations and additional funding or in‐kind support from industry (Nekitsing 2019a; Puder 2011; Zeinstra 2018).
Four studies did not report on funding sources (Kornilaki 2021; Morris 2018; Namenek Brouwer 2013; Witt 2012).
Participants
We considered 29 studies to be large, with 400 or more participants (Alkon 2014; Céspedes 2013; Davis 2016; De Coen 2012; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Hu 2009; Iaia 2017; Kobel 2019; Kristiansen 2019; Leis 2020; Lumeng 2017; Natale 2014b; Natale 2021; Nemet 2011a; Peñalvo 2015; Pinket 2016; Puder 2011; Ray 2020; Reyes‐Morales 2016; Roberts‐Gray 2018; Stookey 2017; Vaughn 2021; Vereecken 2009; Ward 2020a; Yoong 2020a; Zask 2012).
Twenty‐three studies were small, with fewer than 400 participants (Başkale 2011; Blomkvist 2021; De Bock 2011; Eliakim 2007; Fitzgibbon 2013; Gans 2022; Grummon 2019; Hodgkinson 2019; Jones 2015; Kipping 2019; Kornilaki 2021; Lerner‐Geva 2014; Morris 2018; Namenek Brouwer 2013; Natale 2014a; Nekitsing 2019a; Nemet 2011b; Pearson 2022; Seward 2018; Toussaint 2021; Witt 2012; Yeh 2018; Zeinstra 2018).
The largest study recruited 4964 children from 309 centre‐based ECEC services (Pinket 2016). All studies, excluding one (Blomkvist 2021), included a sample of children over the age of two years.
Twenty‐four studies were conducted in a low‐socioeconomic status sample (Alkon 2014; Céspedes 2013; Davis 2016; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Grummon 2019; Hodgkinson 2019; Jones 2015; Lumeng 2017; Natale 2014a; Natale 2014b; Natale 2021; Nemet 2011a; Nemet 2011b; Puder 2011; Stookey 2017; Toussaint 2021; Ward 2020a; Witt 2012; Yeh 2018), 11 studies were conducted in a sample that was not considered low‐socioeconomic status (Başkale 2011; De Coen 2012; Eliakim 2007; Kipping 2019; Lerner‐Geva 2014; Morris 2018; Pearson 2022; Peñalvo 2015; Ray 2020; Roberts‐Gray 2018; Seward 2018), and 17 studies did not provide sufficient information to permit clear judgement (Blomkvist 2021; De Bock 2011; Hu 2009; Iaia 2017; Kobel 2019; Kornilaki 2021; Kristiansen 2019; Leis 2020; Namenek Brouwer 2013; Nekitsing 2019a; Pinket 2016; Reyes‐Morales 2016; Vaughn 2021; Vereecken 2009; Yoong 2020a; Zask 2012; Zeinstra 2018).
Interventions
Of the 58 interventions 37 interventions included strategies that incorporated all three Health Promoting Schools' components (health curriculum, ethos and environment, and partnership).
Forty‐three interventions (in 39 studies) included curriculum strategies (Başkale 2011; Blomkvist 2021; Céspedes 2013; Davis 2016; De Bock 2011; De Coen 2012; Eliakim 2007; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Grummon 2019; Hu 2009; Iaia 2017; Kobel 2019; Kornilaki 2021; Lerner‐Geva 2014; Lumeng 2017; Morris 2018; Namenek Brouwer 2013; Natale 2014a; Natale 2014b; Natale 2021; Nekitsing 2019a; Nemet 2011a; Nemet 2011b; Peñalvo 2015; Pinket 2016; Puder 2011; Ray 2020; Reyes‐Morales 2016; Roberts‐Gray 2018; Stookey 2017; Vaughn 2021; Vereecken 2009; Witt 2012; Yeh 2018; Zask 2012).
Fifty‐six interventions (in 50 studies) included ethos and environment strategies (Alkon 2014; Blomkvist 2021; Céspedes 2013; Davis 2016; De Bock 2011; De Coen 2012; Eliakim 2007; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Grummon 2019; Hodgkinson 2019; Hu 2009; Iaia 2017; Jones 2015; Kipping 2019; Kobel 2019; Kornilaki 2021; Kristiansen 2019; Leis 2020; Lerner‐Geva 2014; Lumeng 2017; Morris 2018; Namenek Brouwer 2013; Natale 2014a; Natale 2014b; Natale 2021; Nekitsing 2019a; Nemet 2011a; Nemet 2011b; Pearson 2022; Peñalvo 2015; Pinket 2016; Puder 2011; Ray 2020; Reyes‐Morales 2016; Roberts‐Gray 2018; Seward 2018; Stookey 2017; Toussaint 2021; Vaughn 2021; Vereecken 2009; Ward 2020a; Witt 2012; Yeh 2018; Yoong 2020a; Zask 2012; Zeinstra 2018).
Fifty interventions (in 47 studies) included partnership strategies (Alkon 2014; Başkale 2011; Céspedes 2013; Davis 2016; De Bock 2011; De Coen 2012; Eliakim 2007; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Grummon 2019; Hodgkinson 2019; Hu 2009; Iaia 2017; Jones 2015; Kipping 2019; Kobel 2019; Kristiansen 2019; Leis 2020; Lumeng 2017; Namenek Brouwer 2013; Natale 2014a; Natale 2014b; Natale 2021; Nekitsing 2019a; Nemet 2011a; Nemet 2011b; Pearson 2022; Peñalvo 2015; Pinket 2016; Puder 2011; Ray 2020; Reyes‐Morales 2016; Roberts‐Gray 2018; Seward 2018; Stookey 2017; Toussaint 2021; Vaughn 2021; Vereecken 2009; Ward 2020a; Witt 2012; Yeh 2018; Yoong 2020a; Zask 2012).
All interventions occurred in the ECEC setting, however, 22 studies also included the home setting (Davis 2016; De Bock 2011; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Grummon 2019; Hodgkinson 2019; Kipping 2019; Kobel 2019; Kristiansen 2019; Lumeng 2017; Natale 2014a; Nemet 2011a; Nemet 2011b; Pearson 2022; Peñalvo 2015; Pinket 2016; Puder 2011; Reyes‐Morales 2016; Roberts‐Gray 2018; Vereecken 2009), and three included the community (Davis 2016; De Coen 2012; Iaia 2017).
Intervention components were delivered by:
the research team (43 interventions, 39 studies; Başkale 2011; Céspedes 2013; Davis 2016; De Bock 2011; De Coen 2012; Eliakim 2007; Fernandez‐Jimenez 2019; Fitzgibbon 2011; Grummon 2019; Hu 2009; Iaia 2017; Jones 2015; Kipping 2019; Kornilaki 2021; Kristiansen 2019; Leis 2020; Lerner‐Geva 2014; Lumeng 2017; Morris 2018; Namenek Brouwer 2013; Natale 2014a; Natale 2014b; Natale 2021; Nekitsing 2019a; Nemet 2011a; Nemet 2011b; Pinket 2016; Puder 2011; Ray 2020; Reyes‐Morales 2016; Roberts‐Gray 2018; Seward 2018; Toussaint 2021; Vaughn 2021; Vereecken 2009; Ward 2020a; Yeh 2018; Yoong 2020a; Zeinstra 2018);
ECEC staff (50 interventions, 44 studies; Blomkvist 2021; Davis 2016; De Coen 2012; Eliakim 2007; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Grummon 2019; Hodgkinson 2019; Iaia 2017; Jones 2015; Kobel 2019; Kornilaki 2021; Kristiansen 2019; Leis 2020; Lerner‐Geva 2014; Lumeng 2017; Morris 2018; Namenek Brouwer 2013; Natale 2014a; Natale 2014b; Natale 2021; Nekitsing 2019a; Nemet 2011a; Nemet 2011b; Pearson 2022; Peñalvo 2015; Pinket 2016; Puder 2011; Ray 2020; Reyes‐Morales 2016; Roberts‐Gray 2018; Seward 2018; Stookey 2017; Toussaint 2021; Vaughn 2021; Vereecken 2009; Ward 2020a; Witt 2012; Yeh 2018; Zask 2012; Zeinstra 2018)
ECEC staff or healthcare staff, or both (31 interventions, 28 studies; Alkon 2014; Başkale 2011; Davis 2016; De Bock 2011; De Coen 2012; Eliakim 2007; Gans 2022; Hodgkinson 2019; Iaia 2017; Jones 2015; Leis 2020; Lumeng 2017; Namenek Brouwer 2013; Natale 2014a; Natale 2014b; Natale 2021; Nekitsing 2019a; Nemet 2011a; Nemet 2011b; Pearson 2022; Peñalvo 2015; Puder 2011; Seward 2018; Stookey 2017; Ward 2020a; Yeh 2018; Yoong 2020a; Zask 2012).
Interventions were delivered via one or more modes, including:
face‐to‐face (57 interventions, 51 studies; Alkon 2014; Başkale 2011; Céspedes 2013; Davis 2016; De Bock 2011; De Coen 2012; Eliakim 2007; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Grummon 2019; Hodgkinson 2019; Hu 2009; Iaia 2017; Jones 2015; Kipping 2019; Kobel 2019; Kornilaki 2021; Kristiansen 2019; Leis 2020; Lerner‐Geva 2014; Lumeng 2017; Morris 2018; Namenek Brouwer 2013; Natale 2014a; Natale 2014b; Natale 2021; Nekitsing 2019a; Nemet 2011a; Nemet 2011b; Pearson 2022; Peñalvo 2015; Pinket 2016; Puder 2011; Ray 2020; Reyes‐Morales 2016; Roberts‐Gray 2018; Seward 2018; Stookey 2017; Toussaint 2021; Vaughn 2021; Vereecken 2009; Ward 2020a; Witt 2012; Yeh 2018; Yoong 2020a; Zask 2012; Zeinstra 2018);
telephone (12 interventions, 11 studies; Alkon 2014; De Coen 2012; Gans 2022; Jones 2015; Kipping 2019; Kornilaki 2021; Leis 2020; Lumeng 2017; Seward 2018; Ward 2020a; Yoong 2020a);
online (20 interventions, 20 studies; Alkon 2014; Blomkvist 2021; De Coen 2012; Gans 2022; Jones 2015; Kipping 2019; Kornilaki 2021; Kristiansen 2019; Leis 2020; Morris 2018; Nekitsing 2019a; Pearson 2022; Peñalvo 2015; Ray 2020; Seward 2018; Stookey 2017; Vaughn 2021; Vereecken 2009; Ward 2020a; Yoong 2020a); and
written communication (50 interventions, 46 studies; Alkon 2014; Blomkvist 2021; Céspedes 2013; Davis 2016; De Coen 2012; Eliakim 2007; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Grummon 2019; Hodgkinson 2019; Hu 2009; Iaia 2017; Jones 2015; Kipping 2019; Kobel 2019; Kornilaki 2021; Kristiansen 2019; Leis 2020; Lerner‐Geva 2014; Lumeng 2017; Morris 2018; Namenek Brouwer 2013; Natale 2014a; Natale 2014b; Natale 2021; Nekitsing 2019a; Nemet 2011a; Nemet 2011b; Pearson 2022; Peñalvo 2015; Pinket 2016; Puder 2011; Ray 2020; Reyes‐Morales 2016; Roberts‐Gray 2018; Seward 2018; Stookey 2017; Vaughn 2021; Vereecken 2009; Ward 2020a; Witt 2012; Yeh 2018; Zask 2012).
Thirty‐one studies described the theoretical basis of the interventions. Theoretical frameworks included:
Piaget’s Cognitive Development Theory (Başkale 2011);
Social Cognitive Theory (Céspedes 2013; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Kipping 2019; Kobel 2019; Lumeng 2017; Natale 2021; Ray 2020; Roberts‐Gray 2018; Vaughn 2021; Ward 2020a);
Transtheoretical Model (Céspedes 2013; Fitzgibbon 2005);
Socioecological Model (Davis 2016; De Coen 2012; Gans 2022; Grummon 2019; Kobel 2019; Natale 2014a; Puder 2011; Roberts‐Gray 2018; Vaughn 2021; Ward 2020a);
Social Learning Theory (De Bock 2011; Hodgkinson 2019);
Zajonc’s Exposure Effect (De Bock 2011);
Self‐Determination Theory (Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Ray 2020; Ward 2020a);
Health Belief Model (Fitzgibbon 2013; Zask 2012);
Damschroder’s Consolidated Framework for Implementation Research (Jones 2015);
Socioeconomic Framework (Kipping 2019);
Funds of Knowledge (Kornilaki 2021; Morris 2018);
Adult Learning Theory (Natale 2021);
Reach Effectiveness Adoption Implementation and Maintenance Framework (Natale 2014b; Natale 2021);
Behaviour Change Wheel (Pearson 2022);
PRECEDE‐PROCEED Model (Pinket 2016);
Theory of Planned Behaviour (Ray 2020);
Theory of Reasoned Action (Roberts‐Gray 2018);
Exchange Theory (Vaughn 2021);
Social Marketing Approach (Vaughn 2021);
Theoretical Domains Framework (Seward 2018; Yoong 2020a);
Technology Acceptance Model (Yoong 2020a); and
Competence Motivational Theory (Zask 2012).
Intervention duration ranged from between four to six weeks (Kornilaki 2021), and three years (Peñalvo 2015).
Outcomes
Thirty‐eight studies reported on at least one child dietary intake outcome (Başkale 2011; Blomkvist 2021; De Bock 2011; De Coen 2012; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Grummon 2019; Hu 2009; Iaia 2017; Jones 2015; Kipping 2019; Kobel 2019; Kornilaki 2021; Kristiansen 2019; Leis 2020; Lerner‐Geva 2014; Lumeng 2017; Morris 2018; Namenek Brouwer 2013; Natale 2014b; Natale 2021; Nekitsing 2019a; Pearson 2022; Pinket 2016; Puder 2011; Ray 2020; Reyes‐Morales 2016; Roberts‐Gray 2018; Seward 2018; Vaughn 2021; Vereecken 2009; Ward 2020a; Witt 2012; Yoong 2020a; Zeinstra 2018). Studies assessed a range of continuous dietary outcomes, including: consumption of food groups (e.g. fruit, vegetables, snacks, breads and cereals, dairy, meat and alternatives, non‐core foods); consumption of specific foods (e.g. carrots, pumpkin, grapes, yoghurt, French fries, biscuits); consumption of beverage types (e.g. sugar‐sweetened beverages, water); consumption of specific beverages (e.g. soft drink, tea, plain milk, 100% fruit juice); intake of macronutrients (e.g. fibre, fat, energy); intake of specific dietary components (e.g. sodium, sugars, saturated fatty acids); diet quality components (e.g. fruit, vegetables, whole grains); and overall diet quality.
The included studies assessed dietary outcomes using:
parent‐ or ECEC staff‐reported surveys, recall or diaries (19 studies; Başkale 2011; Blomkvist 2021; De Bock 2011; De Coen 2012; Fitzgibbon 2005; Fitzgibbon 2006; Grummon 2019; Hu 2009; Iaia 2017; Kobel 2019; Kornilaki 2021; Lerner‐Geva 2014; Morris 2018; Natale 2014b; Natale 2021; Pinket 2016; Puder 2011; Ray 2020; Reyes‐Morales 2016);
in‐care observations by researchers (6 studies; Gans 2022; Jones 2015; Kipping 2019; Namenek Brouwer 2013; Roberts‐Gray 2018; Ward 2020a);
weighed plate waste (5 studies; Leis 2020; Nekitsing 2019a; Pearson 2022; Witt 2012; Zeinstra 2018), or
a combination of two measures (8 studies; Fitzgibbon 2011; Fitzgibbon 2013; Kristiansen 2019; Lumeng 2017; Seward 2018; Vaughn 2021; Vereecken 2009; Yoong 2020a).
Fifteen studies reported that the measure used was validated (De Coen 2012; Gans 2022; Jones 2015; Kipping 2019; Kornilaki 2021; Leis 2020; Lerner‐Geva 2014; Morris 2018; Namenek Brouwer 2013; Natale 2014b; Natale 2021; Pearson 2022; Pinket 2016; Ray 2020; Roberts‐Gray 2018), one study reported that one of the two measures used was validated (Vereecken 2009), and the remaining studies did not report on the validity of the measure. We extracted all data relating to dietary outcomes.
Thirty‐six studies reported on at least one anthropometric outcome (Alkon 2014; Başkale 2011; Céspedes 2013; Davis 2016; De Bock 2011; De Coen 2012; Eliakim 2007; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Grummon 2019; Hodgkinson 2019; Hu 2009; Iaia 2017; Kipping 2019; Kobel 2019; Kornilaki 2021; Lerner‐Geva 2014; Lumeng 2017; Natale 2014a; Natale 2014b; Natale 2021; Nemet 2011a; Nemet 2011b; Peñalvo 2015; Puder 2011; Roberts‐Gray 2018; Stookey 2017; Toussaint 2021; Vaughn 2021; Ward 2020a; Witt 2012; Yoong 2020a; Zask 2012). Continuous anthropometric outcomes included: BMI and BMI z‐score; weight, weight z‐score and weight‐for‐age z‐score; body mass percentage; mid‐upper arm circumference; waist circumference; skinfold thickness (e.g. sum, triceps, subscapular); fat‐free index and fat‐free mass index. Dichotomous anthropometric outcomes (as reported by studies) included: children classified as overweight, obese, at risk of being overweight or obese, at a healthy weight or underweight; and children classified with mid‐upper arm circumference percentile (≤ 10, > 10 to < 85, or ≥ 85). Studies collected all anthropometric data using objective measures.
Language and cognitive outcomes were reported by two studies (Puder 2011; Ray 2020). All outcomes were continuous and included: cognitive self‐regulation; attention; and spatial working memory. Measures included the Konzentrations‐Handlungsverfahren für Vorschulkinder (Ettrich 2006), Intelligence and Development Scales (Grob 2009), and items from the Child Social Behavior Questionnaire (Warden 2003). One study reported that the measure was validated.
Social or emotional outcomes were reported by two studies (Fernandez‐Jimenez 2019; Ray 2020). The outcomes, emotional comprehension and emotional self‐regulation, were both continuous. Measures included the Test of Emotion Comprehension (Pons 2004), and items from the Child Social Behavior Questionnaire (Warden 2003). Neither study reported the validity of the measures.
Quality‐of‐life outcomes were reported by three studies (Kipping 2019; Puder 2011; Yoong 2020a). All were parent‐reported and validated. They included total quality of life and quality‐of‐life components (e.g. physical function, emotional function, social function, nursery function). Measures were Paediatric Quality of Life Inventory (Varni 2001), and parent proxy version of KIDSCREEN‐10 (Ravens‐Sieberer 2010).
Costs related to the intervention were available for six studies (Iaia 2017; Kipping 2019; Leis 2020; Natale 2014b; Stookey 2017; Yoong 2020a). Cost outcomes included: total cost of intervention; projected lifetime savings; cost for participants (e.g. cost per service, parental weekly food spend); average cost‐effectiveness ratio and relative value index. Measures included: detailed staffing and financial records; nursery logs; parent‐completed questionnaire; micro‐costing; and service questionnaire; or were not reported. No study reported on the validity of cost measures.
Adverse consequences outcomes were explicitly reported by three studies (Kipping 2019; Pearson 2022; Seward 2018), including: increased occurrence of injury among children or staff; (incident or) adverse event; negative feedback; parent complaints or concerns; and percentage of meal waste. A further four studies reported that no adverse consequences were reported (Eliakim 2007; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006), however, no specific measures or outcomes were reported. No study reported on the validity of adverse consequences measures.
Length of follow‐up from baseline ranged between three months (Blomkvist 2021; Grummon 2019; Kornilaki 2021; Morris 2018; Natale 2014a; Witt 2012), to three years (Peñalvo 2015), across outcomes.
Excluded studies
Following our review of 203 full texts, we excluded 81 articles for the following reasons: study design (n = 26), participants (n = 2), intervention (n = 9) and outcomes (n = 44). See Figure 1.
Studies awaiting classification
We identified one study that we were unable to classify due to limited study information (ChiCTR2200060958; Characteristics of studies awaiting classification).
Ongoing studies
We identified 13 relevant ongoing RCT protocols (Armstrong 2019; Barnes 2020; Beckerman 2019; Cosco 2021; Helland 2016; Lee 2019; Malden 2018; Mehdizadeh 2018; Reeves 2018; Sisson 2019; Watt 2014; Yin 2019; Zarnowiecki 2021), and 11 trial registrations, which did not have published or unpublished outcomes (ISRCTN33134697; NCT01890681; NCT02580123; NCT03575884; NCT03601299; NCT03668678; NCT04082247; NCT04140032; NCT04164277; NCT04711525; NCT05112185; Characteristics of ongoing studies).
Risk of bias in included studies
See Characteristics of included studies.
The risk of bias assessment for each study across all outcomes is summarised within Figure 2 and support for judgements are provided in the Characteristics of included studies table. The risk of bias assessments for the primary outcome are described in detail below. Risk of bias assessments are also summarised for each study in the main meta‐analysis for each outcome (see Analysis 1.1; Analysis 2.1; Analysis 3.1; Analysis 4.1; Analysis 5.1; Analysis 6.1; Analysis 7.1; Analysis 8.1; Analysis 9.1; Analysis 10.1; Analysis 11.1; Analysis 12.1).
2.

Figure 2. Risk of bias summary
1.1. Analysis.

Comparison 1: Diet quality, Outcome 1: Diet quality
2.1. Analysis.

Comparison 2: Fruit consumption, Outcome 1: Fruit consumption
3.1. Analysis.

Comparison 3: Vegetable consumption, Outcome 1: Vegetable consumption
4.1. Analysis.

Comparison 4: Fruit and vegetable consumption, Outcome 1: Fruit and vegetable consumption
5.1. Analysis.

Comparison 5: Non‐core foods consumption, Outcome 1: Non‐core foods (i.e. less healthy/discretionary) consumption
6.1. Analysis.

Comparison 6: Sugar‐sweetened beverage consumption, Outcome 1: Sugar‐sweetened beverage consumption
7.1. Analysis.

Comparison 7: BMI, Outcome 1: BMI
8.1. Analysis.

Comparison 8: BMI z‐score, Outcome 1: BMI z‐score
9.1. Analysis.

Comparison 9: Absolute weight (kg), Outcome 1: Absolute weight (kg)
10.1. Analysis.

Comparison 10: Overweight and obesity, Outcome 1: Overweight and obesity
11.1. Analysis.

Comparison 11: Waist circumference, Outcome 1: Waist circumference
12.1. Analysis.

Comparison 12: Quality of life, Outcome 1: Quality of life
Allocation
We assessed 29 studies as low risk of bias for random sequence generation as studies used methods such as computerised random number functions, randomisation tables, opaque envelopes, or drawing names from a hat to generate random sequences, and allocation was either completed by an independent entity (e.g. uninvolved party, independent statistician, coordinating centre) or after baseline data collection, thereby preventing allocation from being pre‐empted (Başkale 2011; Blomkvist 2021; Céspedes 2013; Davis 2016; Gans 2022; Hodgkinson 2019; Hu 2009; Iaia 2017; Jones 2015; Kipping 2019; Kornilaki 2021; Leis 2020; Lumeng 2017; Morris 2018; Namenek Brouwer 2013; Natale 2021; Nekitsing 2019a; Nemet 2011a; Nemet 2011b; Pearson 2022; Pinket 2016; Puder 2011; Ray 2020; Reyes‐Morales 2016; Seward 2018; Stookey 2017; Toussaint 2021; Vaughn 2021; Ward 2020a). We assessed 22 studies as unclear risk of bias for random sequence generation as they did not describe the random sequence generation procedure for the primary outcome (Alkon 2014; De Bock 2011; De Coen 2012; Eliakim 2007; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Grummon 2019; Kobel 2019; Kristiansen 2019; Lerner‐Geva 2014; Natale 2014a; Peñalvo 2015; Roberts‐Gray 2018; Vereecken 2009; Witt 2012; Yeh 2018; Yoong 2020a; Zask 2012; Zeinstra 2018). We assessed one study as high risk of bias for random sequence generation as services were added to the control arm following randomisation and these additional centres do not appear to have been randomly chosen or assigned (Natale 2014b).
We assessed 21 studies as low risk for allocation bias as an independent statistician conducted allocation after baseline data collection (Blomkvist 2021; Céspedes 2013; Davis 2016; Gans 2022; Hodgkinson 2019; Jones 2015; Kipping 2019; Kristiansen 2019; Morris 2018; Namenek Brouwer 2013; Nekitsing 2019a; Pearson 2022; Pinket 2016; Puder 2011; Ray 2020; Seward 2018; Stookey 2017; Vaughn 2021; Vereecken 2009; Ward 2020a; Yoong 2020a). We assessed 30 studies as unclear risk as the method of allocation concealment was either not reported or it was unclear whether participants were aware of their allocation prior to recruitment (Alkon 2014; Başkale 2011; De Bock 2011; Eliakim 2007; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Grummon 2019; Hu 2009; Iaia 2017; Kobel 2019; Kornilaki 2021; Leis 2020; Lerner‐Geva 2014; Lumeng 2017; Natale 2014a; Natale 2014b; Natale 2021; Nemet 2011a; Nemet 2011b; Peñalvo 2015; Reyes‐Morales 2016; Roberts‐Gray 2018; Toussaint 2021; Witt 2012; Yeh 2018; Zask 2012; Zeinstra 2018). We assessed one study as high risk of selection bias as ECEC services were aware of their treatment allocation prior to recruitment (De Coen 2012).
Blinding
Thirty‐eight studies measured dietary outcomes. We assessed most of them as high risk of performance bias due to participants and ECEC service staff not being blind to group allocation (27 studies; Blomkvist 2021; De Bock 2011; De Coen 2012; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Grummon 2019; Hu 2009; Iaia 2017; Jones 2015; Kipping 2019; Kobel 2019; Kornilaki 2021; Kristiansen 2019; Lerner‐Geva 2014; Morris 2018; Namenek Brouwer 2013; Natale 2014b; Natale 2021; Nekitsing 2019a; Pinket 2016; Ray 2020; Reyes‐Morales 2016; Seward 2018; Vereecken 2009). For the remaining 11 studies with dietary outcomes, we assessed the risk of performance bias as unclear due to insufficient information on whether the lack of blinding would affect the outcome (Başkale 2011; Leis 2020; Lumeng 2017; Pearson 2022; Puder 2011; Roberts‐Gray 2018; Vaughn 2021; Ward 2020a; Witt 2012; Yoong 2020a; Zeinstra 2018).
For 12 studies that measured dietary outcomes, we assessed the risk of detection bias as low because children’s intake was either measured, observed or obtained from the parent or ECEC staff by a blinded outcome assessor (Fitzgibbon 2005; Gans 2022; Jones 2015; Leis 2020; Namenek Brouwer 2013; Nekitsing 2019a; Pearson 2022; Roberts‐Gray 2018; Ward 2020a; Witt 2012; Yoong 2020a; Zeinstra 2018). We assessed 21 studies that measured dietary outcomes as high risk of detection bias because parents reported children’s dietary intake, yet blinding of parents was either not reported, not possible, or likely broken (Blomkvist 2021; De Bock 2011; De Coen 2012; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Grummon 2019; Hu 2009; Iaia 2017; Kipping 2019; Kobel 2019; Kornilaki 2021; Lerner‐Geva 2014; Morris 2018; Natale 2014b; Natale 2021; Pinket 2016; Ray 2020; Reyes‐Morales 2016; Seward 2018; Vereecken 2009). For the remaining five studies with dietary outcomes, we assessed the risk of detection bias as unclear due to multiple measurement methods used or unclear blinding (Başkale 2011; Kristiansen 2019; Lumeng 2017; Puder 2011; Vaughn 2021).
Incomplete outcome data
We assessed the risk of attrition bias as low for dietary outcomes for 10 studies as either data were available for all or most participants (with similar loss and reasons for loss between treatment groups) or we conducted sensitivity analysis to assess the impact of missing data (Başkale 2011; Fitzgibbon 2011; Grummon 2019; Hu 2009; Iaia 2017; Lumeng 2017; Pearson 2022; Puder 2011; Roberts‐Gray 2018; Ward 2020a). We assessed the risk of bias as high for dietary outcomes for 14 studies due to the magnitude of missing data, large difference in proportions of participants followed up between treatment groups or use of complete‐case analyses instead of the intention‐to‐treat principle (Blomkvist 2021; De Bock 2011; De Coen 2012; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2013; Kipping 2019; Kobel 2019; Kristiansen 2019; Leis 2020; Nekitsing 2019a; Vereecken 2009; Witt 2012; Yoong 2020a). We assessed risk of attrition bias for dietary outcomes as unclear for 14 studies, as they provided insufficient information regarding loss to follow‐up or due to the treatment of missing data (Gans 2022; Jones 2015; Kornilaki 2021; Lerner‐Geva 2014; Morris 2018; Namenek Brouwer 2013; Natale 2014b; Natale 2021; Pinket 2016; Ray 2020; Reyes‐Morales 2016; Seward 2018; Vaughn 2021; Zeinstra 2018).
Selective reporting
We assessed the risk of reporting bias as low for 13 studies, as the reported outcomes aligned with those outlined in a published protocol paper or trial registration (Blomkvist 2021; Fernandez‐Jimenez 2019; Gans 2022; Grummon 2019; Hodgkinson 2019; Kipping 2019; Kornilaki 2021; Peñalvo 2015; Puder 2011; Roberts‐Gray 2018; Seward 2018; Yoong 2020a; Zask 2012). For five studies, we assessed the risk of reporting bias as high, either because findings of prespecified outcomes were incompletely reported in the study or the study included outcomes that were not prespecified in the published protocol paper (De Bock 2011; Jones 2015; Leis 2020; Pearson 2022; Toussaint 2021). We assessed risk of reporting bias as unclear for the remaining 34 studies either because a published protocol paper or trial registration record was not identified, outcomes were vaguely or incompletely described in the protocol or trial registration or not all prespecified outcomes were reported in the study (Alkon 2014; Başkale 2011; Céspedes 2013; Davis 2016; De Coen 2012; Eliakim 2007; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Hu 2009; Iaia 2017; Kobel 2019; Kristiansen 2019; Lerner‐Geva 2014; Lumeng 2017; Morris 2018; Namenek Brouwer 2013; Natale 2014a; Natale 2014b; Natale 2021; Nekitsing 2019a; Nemet 2011a; Nemet 2011b; Pinket 2016; Ray 2020; Reyes‐Morales 2016; Stookey 2017; Vaughn 2021; Vereecken 2009; Ward 2020a; Witt 2012; Yeh 2018; Zeinstra 2018).
Other potential sources of bias
All included studies were cluster‐RCTs. As such, we assessed the potential risk of additional cluster‐related biases.
Recruitment
We assessed the risk of recruitment to cluster bias as low for 16 studies as recruitment occurred prior to cluster randomisation (Blomkvist 2021; Céspedes 2013; Davis 2016; Gans 2022; Jones 2015; Kristiansen 2019; Lerner‐Geva 2014; Lumeng 2017; Morris 2018; Namenek Brouwer 2013; Nekitsing 2019a; Pearson 2022; Pinket 2016; Puder 2011; Ray 2020; Vaughn 2021). Eight studies recruited following cluster randomisation, so we deemed them to have high risk of bias as (De Coen 2012; Fernandez‐Jimenez 2019; Grummon 2019; Hodgkinson 2019; Kipping 2019; Natale 2014b; Reyes‐Morales 2016; Yoong 2020a). For the remaining 28 studies, we assessed recruitment bias as unclear due to insufficient information regarding participant recruitment (Alkon 2014; Başkale 2011; De Bock 2011; Eliakim 2007; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Hu 2009; Iaia 2017; Kobel 2019; Kornilaki 2021; Leis 2020; Natale 2014a; Natale 2021; Nemet 2011a; Nemet 2011b; Peñalvo 2015; Roberts‐Gray 2018; Seward 2018; Stookey 2017; Toussaint 2021; Vereecken 2009; Ward 2020a; Witt 2012; Yeh 2018; Zask 2012; Zeinstra 2018).
Baseline imbalance
We assessed 27 studies as low risk of bias for baseline imbalance because either there were no baseline imbalances that were likely to influence the outcomes or adjusted analytic models controlled for any imbalances (Başkale 2011; Blomkvist 2021; Céspedes 2013; Davis 2016; De Coen 2012; Eliakim 2007; Fernandez‐Jimenez 2019; Gans 2022; Hodgkinson 2019; Hu 2009; Iaia 2017; Kobel 2019; Kristiansen 2019; Leis 2020; Lerner‐Geva 2014; Lumeng 2017; Morris 2018; Nekitsing 2019a; Nemet 2011a; Nemet 2011b; Pearson 2022; Pinket 2016; Puder 2011; Reyes‐Morales 2016; Roberts‐Gray 2018; Vaughn 2021; Zeinstra 2018). We assessed three studies as high risk of bias due to baseline imbalances that were likely to influence the outcomes, but were not accounted for in the analysis (Fitzgibbon 2006; Fitzgibbon 2011; Natale 2021). For the remaining 22 studies, we assessed the risk of baseline imbalance bias as unclear due to insufficient information reported regarding baseline data (Alkon 2014; De Bock 2011; Fitzgibbon 2005; Fitzgibbon 2013; Grummon 2019; Jones 2015; Kipping 2019; Kornilaki 2021; Namenek Brouwer 2013; Natale 2014a; Natale 2014b; Peñalvo 2015; Ray 2020; Seward 2018; Stookey 2017; Toussaint 2021; Vereecken 2009; Ward 2020a; Witt 2012; Yeh 2018; Yoong 2020a; Zask 2012).
Loss of clusters
Regarding risk of bias due to loss of clusters, we assessed 20 studies as low risk of bias as either there was no loss of clusters, lost clusters were replaced prior to intervention or loss of clusters comprised a small percentage (< 20%; Higgins 2011), of the overall sample (Alkon 2014; Blomkvist 2021; Céspedes 2013; Davis 2016; De Coen 2012; Eliakim 2007; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2013; Grummon 2019; Iaia 2017; Jones 2015; Leis 2020; Lumeng 2017; Namenek Brouwer 2013; Nekitsing 2019a; Nemet 2011b; Puder 2011; Roberts‐Gray 2018). We assessed the risk of bias for loss of clusters as high for 10 studies as the loss of clusters could have impacted the results (De Bock 2011; Hodgkinson 2019; Kipping 2019; Kobel 2019; Natale 2014a; Pearson 2022; Peñalvo 2015; Seward 2018; Stookey 2017; Yoong 2020a). For the remaining 22 studies, risk of bias was unclear due to insufficient reporting regarding loss of clusters or the impact of lost clusters on the outcomes was unclear (Başkale 2011; Fitzgibbon 2011; Gans 2022; Hu 2009; Kornilaki 2021; Kristiansen 2019; Lerner‐Geva 2014; Morris 2018; Natale 2014b; Natale 2021; Nemet 2011a; Pinket 2016; Ray 2020; Reyes‐Morales 2016; Toussaint 2021; Vaughn 2021; Vereecken 2009; Ward 2020a; Witt 2012; Yeh 2018; Zask 2012; Zeinstra 2018).
Incorrect analysis
For risk of bias due to incorrect analysis, we assessed most studies as low risk of bias because clustering was taken into account in the analysis (38 studies; Alkon 2014; Céspedes 2013; Davis 2016; De Bock 2011; De Coen 2012; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Grummon 2019; Hodgkinson 2019; Iaia 2017; Jones 2015; Kristiansen 2019; Leis 2020; Lerner‐Geva 2014; Lumeng 2017; Natale 2014b; Natale 2021; Nekitsing 2019a; Nemet 2011a; Nemet 2011b; Pearson 2022; Peñalvo 2015; Pinket 2016; Puder 2011; Ray 2020; Roberts‐Gray 2018; Seward 2018; Stookey 2017; Toussaint 2021; Vaughn 2021; Ward 2020a; Witt 2012; Yoong 2020a; Zask 2012). We assessed 10 studies as high risk of bias as there was no accounting for clustering (Eliakim 2007; Hu 2009; Kipping 2019; Kobel 2019; Kornilaki 2021; Morris 2018; Namenek Brouwer 2013; Natale 2014a; Reyes‐Morales 2016; Yeh 2018). For the remaining four studies, we assessed the risk of bias due to incorrect analysis as unclear due to insufficient information reported (Başkale 2011; Blomkvist 2021; Vereecken 2009; Zeinstra 2018).
Contamination
We assessed the risk of contamination bias as low for five studies (Leis 2020; Lumeng 2017; Pearson 2022; Pinket 2016; Toussaint 2021). We assessed the remaining 47 studies as unclear risk of bias due to insufficient information provided (Alkon 2014; Başkale 2011; Blomkvist 2021; Céspedes 2013; Davis 2016; De Bock 2011; De Coen 2012; Eliakim 2007; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Grummon 2019; Hodgkinson 2019; Hu 2009; Iaia 2017; Jones 2015; Kipping 2019; Kobel 2019; Kornilaki 2021; Kristiansen 2019; Lerner‐Geva 2014; Morris 2018; Namenek Brouwer 2013; Natale 2014a; Natale 2014b; Natale 2021; Nekitsing 2019a; Nemet 2011a; Nemet 2011b; Peñalvo 2015; Puder 2011; Ray 2020; Reyes‐Morales 2016; Roberts‐Gray 2018; Seward 2018; Stookey 2017; Vaughn 2021; Vereecken 2009; Ward 2020a; Witt 2012; Yeh 2018; Yoong 2020a; Zask 2012; Zeinstra 2018).
Other bias
In terms of additional sources of bias, we assessed 22 studies as low risk of bias as there were no clear sources of other bias (Blomkvist 2021; Céspedes 2013; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Gans 2022; Grummon 2019; Hodgkinson 2019; Hu 2009; Kipping 2019; Kristiansen 2019; Lerner‐Geva 2014; Lumeng 2017; Natale 2014b; Natale 2021; Nemet 2011a; Pearson 2022; Pinket 2016; Reyes‐Morales 2016; Vaughn 2021; Ward 2020a; Yoong 2020a). We assessed five studies as high risk of bias because no funding statement was provided or because of potentially confounding, effect‐modifying, and time‐varying factors (Kornilaki 2021; Morris 2018; Namenek Brouwer 2013; Stookey 2017; Witt 2012). For 25 studies, we assessed the risk of other sources of bias as unclear because no conflict of interest statement was reported or there was insufficient information to assess whether an important risk of bias exists, or both (Alkon 2014; Başkale 2011; Davis 2016; De Bock 2011; De Coen 2012; Eliakim 2007; Fernandez‐Jimenez 2019; Fitzgibbon 2005; Iaia 2017; Jones 2015; Kobel 2019; Leis 2020; Natale 2014a; Nekitsing 2019a; Nemet 2011b; Peñalvo 2015; Puder 2011; Ray 2020; Roberts‐Gray 2018; Seward 2018; Toussaint 2021; Vereecken 2009; Yeh 2018; Zask 2012; Zeinstra 2018).
Overall risk of bias for primary outcome (across domains)
For dietary outcomes, we judged 19 studies to be at overall high risk of bias (assessed as high risk of bias on three or more domains; Blomkvist 2021; De Bock 2011; De Coen 2012; Fitzgibbon 2006; Fitzgibbon 2011; Fitzgibbon 2013; Grummon 2019; Hu 2009; Kipping 2019; Kobel 2019; Kornilaki 2021; Morris 2018; Namenek Brouwer 2013; Natale 2014b; Natale 2021; Reyes‐Morales 2016; Seward 2018; Vereecken 2009; Yoong 2020a).
Assessment of reporting bias
Visual inspection of the funnel plots for the primary outcome found potential publication bias (as assessed via presence of outliers) for diet quality (in both directions from the pooled treatment effect) and vegetable consumption (in a positive direction from the treatment effect). Comparison of small and large studies for fruit, fruit and vegetable, non‐core foods and sugar‐sweetened beverage consumption found no subgroup differences in effects (see Figure 3; Figure 4; Figure 5Figure 6; Figure 7).
3.

Funnel plot: diet quality
4.

Funnel plot: fruit consumption
5.

Funnel plot: vegetable consumption
6.

Funnel plot: non‐core foods (i.e. less healthy/discretionary) consumption
7.

Funnel plot: sugar‐sweetened beverage consumption
Effects of interventions
See: Table 1
See Table 1 for the main comparison and Table 2 for studies not pooled in the meta‐analysis.
1. Study findings of primary and secondary outcomes not included in the meta‐analysis.
| Study ID | Outcome | Reason not‐meta‐analysed | Findings |
| Fruit consumption | |||
| De Bock 2011 | Daily consumption of fruit (g) | Missing data | Positive, participant numbers not available |
| Morris 2018 | Daily consumption of fruit (g) | Missing data | Positive, 201 children |
| Namenek Brouwer 2013 | Daily consumption of fruit (g) | Missing data | Negative, 6 children |
| Natale 2014b | Rate of fruit consumption (per week) | Different measure | SMD −0.06 (95% CI −0.22 to 0.10), 634 children |
| Natale 2021 | Rate of fruit consumption (per week) | Different measure | SMD 0.02 (95% CI −0.15 to 0.20), 493 children |
| Pinket 2016 | Daily consumption of fruit (g) | Missing data | Negative, 4970 children |
| Witt 2012 | % fruit snack consumed in care | Different measure | Positive, 153 |
| Vegetable consumption | |||
| Başkale 2011 | Weekly consumption of vegetables (scale) | Different measure | SMD 0.09 (95% CI −0.21 to 0.39), 172 children |
| De Bock 2011 | Daily consumption of vegetables (g) | Missing data | Positive, participant numbers not available |
| Morris 2018 | Daily consumption of vegetables (g) | Missing data | Positive, 203 children |
| Namenek Brouwer 2013 | Daily consumption of vegetables (g) | Missing data | Positive, 6 children |
| Natale 2014b | Rate of vegetable consumption (per week) | Different measure | SMD 0.25 (95% CI 0.09 to 0.41), 634 children |
| Natale 2021 | Rate of vegetable consumption (per week) | Different measure | SMD −0.23 (95% CI −0.41 to −0.05), 493 children |
| Pinket 2016 | Daily consumption of vegetables (g) | Missing data | Positive, 4970 children |
| Witt 2012 | % vegetable snack consumed in care | Different measure | Positive, 122 children |
| Fruit and vegetable consumption combined | |||
| Iaia 2017 | % children consuming ≥ 4 servings of fruit and vegetables | Different measure | RR 1.16 (95% CI 0.70 to 1.93), 234 children |
| Morris 2018 | Fruit and vegetables consumed daily (servings) | Missing data | Positive, 200 children |
| Non‐core foods (i.e. less healthy/discretionary) consumption | |||
| Morris 2018 | Unhealthy food consumed daily (servings) | Missing data | Positive, 200 children |
| Natale 2014b | Rate of snack consumption (per week) | Different measure | SMD −0.26 (95% CI −0.42 to −0.11), 634 children |
| Natale 2021 | Rate of snack consumption (per week) | Different measure | SMD 1.19 (95% CI 1.00 to 1.38), 493 children |
| Sugar‐sweetenedbeverage consumption | |||
| Iaia 2017 | % children not consuming sugar‐sweetened beverages daily | Different measure | RR 1.09 (95% CI 1.00 to 1.19), 234 children |
| Kobel 2019 | % children consuming sugar‐sweetened beverages daily | Different measure | RR 0.73 (95% CI 0.35 to 1.52), 474 children |
| Morris 2018 | Consumption of sugar‐sweetened beverages | Missing data | Negative, 170 children |
| BMI z‐score | |||
| Natale 2014a | BMI z‐score | Missing data | Positive, participant numbers not available |
| Peñalvo 2015 | BMI z‐score | Missing data | Positive, participant numbers not available |
| Stookey 2017 | Annual change in BMI z‐score | Different measure | Positive, 791 children |
| Waist circumference | |||
| Peñalvo 2015 | Waist circumference | No data | Positive, participant numbers not available |
| Language and cognitive performance | |||
| Puder 2011 | Konzentrations‐Handlungsverfahren für Vorschulkinder‐ KHV‐VK | Not pooled in meta‐analysis | Attention (minutes): SMD −0.06 (95% CI −0.29 to 0.16), 309 children Attention: number of correct cards: SMD 0.02 (95% CI −0.17 to 0.21), 434 children Spatial working memory: SMD 0.12 (95% CI −0.07 to 0.31), 434 children |
| Ray 2020 | Child Social Behaviour Questionnaire | Not pooled in meta‐analysis | SMD 0.05 (95% −0.14 to 0.31), 432 children |
| Social/emotional performance | |||
| Fernandez‐Jimenez 2019 | Test of Emotional Comprehension | Not pooled in meta‐analysis | SMD 0.15 (95% CI −0.09 to 0.40), 282 children |
| Ray 2020 | Child Social Behaviour Questionnaire | Not pooled in meta‐analysis | SMD 0.08 (95% CI −0.11 to 0.26), 432 children |
| BMI: body mass index; CI: confidence interval; RR: risk ratio; SMD: standardised mean difference | |||
Primary outcomes: dietary intake
Diet quality
Six studies reported on some measure of overall diet quality in studies when comparing an ECEC‐based healthy eating intervention with usual practice or no intervention. All measures were scale‐based using either educator or parent self‐reported measures (Seward 2018; Yoong 2020a), direct observations (Ward 2020a), or a combination of observations in care and parent self‐report at home (Fitzgibbon 2011; Gans 2022). All were reported as continuous data, with higher scores indicating better diet quality, and were assessed as differences between groups at follow‐up.
Pooled analysis including all six studies provided very low‐certainty evidence that ECEC‐based healthy eating interventions may improve child diet quality score relative to control (SMD 0.34, 95% CI 0.04 to 0.65; P = 0.03, I2 = 91%; 1973 children; Analysis 1.1). A SMD of 0.34 is equivalent to a score 3.68 points better in diet quality. We assessed the certainty of evidence as very low due to assessment of high overall risk of bias for three studies, high heterogeneity between studies (I2 = 91%) and strong detection of publication bias as assessed via visual inspection of funnel plots. When we carried out a sensitivity analysis excluding the three studies at high risk of bias, results were no longer statistically significant, and the effect size was smaller (SMD 0.21, 95% CI −0.03 to 0.45; P = 0.08, I2 = 70%; 957 children; Analysis 1.2). We did not conduct a sensitivity analysis excluding industry‐funded studies as there were none.
1.2. Analysis.

Comparison 1: Diet quality, Outcome 2: Diet quality (sensitivity: studies at low overall risk of bias)
Subgroup analyses
Health Promoting Schools Framework
Two studies with 639 participants included curriculum strategies as part of the healthy eating intervention and had a lower pooled effect (SMD 0.10, 95% CI −0.11 to 0.32) on diet quality, compared to four studies that did not target curriculum strategies (SMD 0.46, 95% CI 0.08 to 0.84; 1334 children). However, no subgroup effect was noted (P = 0.10, I2 = 62%; Analysis 1.3). All six studies targeted ethos and environment, and partnerships, and as such, we could not undertake any subgroup analysis by the components.
1.3. Analysis.

Comparison 1: Diet quality, Outcome 3: Diet quality (Health Promoting Schools: curriculum versus no curriculum)
Socioeconomic status
In the subgroup analysis by socioeconomic status, three studies were classed as specifically undertaken with low‐socioeconomic status groups and had a lower pooled effect (SMD 0.30, 95% CI 0.16 to 0.44; 834 children) compared to three that were undertaken with high/unclear socioeconomic status groups (SMD 0.40, 95% CI −0.22 to 1.01; 1139 children). However, no subgroup effect was noted (P = 0.76; I2 = 0%; Analysis 1.4).
1.4. Analysis.

Comparison 1: Diet quality, Outcome 4: Diet quality (SES: low versus high/unclear)
Other subgroup analyses
As the I2 statistic was higher than 75%, we undertook prespecified subgroup analysis to explore heterogeneity by intervention modality and delivery personnel (Analysis 1.5; Analysis 1.6). The subgroup analysis suggests that delivery modalities that included a combination of face‐to‐face, telephone and online interventions (I2 = 62%), and delivery personnel that included healthcare professionals (I² = 62.0%) may have contributed to the high heterogeneity of studies. We did not undertake subgroup analyses by setting, nor follow‐up period, given that only one study was included in the subgroups.
1.5. Analysis.

Comparison 1: Diet quality, Outcome 5: Diet quality (intervention modality: included face‐to‐face, telephone and online delivery versus did not include face‐to‐face, telephone and online delivery)
1.6. Analysis.

Comparison 1: Diet quality, Outcome 6: Diet quality (intervention delivery personnel: included healthcare professionals versus did not include healthcare professionals)
Fruit consumption
Eighteen studies reported on fruit consumption outcomes, 15 of which reported on servings or portions, times (e.g. per day) or weight (e.g. grams) of fruit consumption. We undertook a pooled analysis including 11 of the 15 studies that reported on servings or portions, times or weight of fruit consumption. All outcomes were continuous and were assessed as difference between groups at follow‐up. Pooled analysis provides moderate‐certainty evidence favouring those receiving the healthy eating intervention on servings of fruit consumed (SMD 0.11, 95% CI 0.04 to 0.18; P < 0.01; I2 = 0%; 2901 children; Analysis 2.1). A SMD of 0.11 is equivalent to an increase of 0.13 servings of fruit. We downgraded the certainty of evidence due to assessment of overall high risk of bias for seven studies. When we carried out a sensitivity analysis excluding the studies at high risk of bias, results were no longer statistically significant, with the effect size reduced (SMD 0.05, 95% CI −0.08 to 0.17; P = 0.44; I2 = 0%; 996 children; Analysis 2.2). We did not conduct a sensitivity analysis excluding industry‐funded studies as there were none.
2.2. Analysis.

Comparison 2: Fruit consumption, Outcome 2: Fruit consumption (sensitivity: studies at low overall risk of bias)
We were unable to include four of the 15 studies in the meta‐analysis due to insufficient data (e.g. missing SD, missing sample size). An additional three studies reported on outcomes that were inappropriate for pooling due to substantial differences in the way the outcomes were reported (Natale 2014b; Natale 2021; Witt 2012). Witt 2012 reported on the percentage of fruit snacks children consumed in care, as assessed using a weighed food record, and Natale 2014b and Natale 2021 reported on rate of fruit consumption (per week). Four of the seven studies showed positive effects in the intervention group (see Figure 8 for harvest plot).
8.

Harvest plot presenting direction of effect for studies not included in the meta‐analysis for fruit consumption, vegetable consumption, non‐core foods consumption and sugar‐sweetened beverage consumption
Subgroup analyses
Health Promoting Schools Framework
Seven studies with 2037 children targeted the curriculum and had a pooled effect of SMD 0.08 (95% CI −0.01 to 0.17), compared to four studies that did not target the curriculum (SMD 0.17, 95% CI 0.03 to 0.32; 864 children). No subgroup effect was noted (P = 0.31, I2 = 3.9%; Analysis 2.3). All studies targeted ethos and environment and only one did not target partnerships. As such, we did not undertake subgroup analysis by these components.
2.3. Analysis.

Comparison 2: Fruit consumption, Outcome 3: Fruit consumption (Health Promoting Schools: curriculum versus no curriculum)
Socioeconomic status
Four studies were classed as undertaken with a low‐socioeconomic status population. No subgroup effect was noted (P = 0.75, I2 = 0%; Analysis 2.4).
2.4. Analysis.

Comparison 2: Fruit consumption, Outcome 4: Fruit consumption (SES: low versus high/unclear)
Other subgroup analyses
As we did not identify high statistical heterogeneity in the primary analysis (I2 < 75%) we did not undertake further subgroup analyses.
Vegetable consumption
In total, 21 studies reported on vegetable consumption, with 17 of these studies reporting on servings or portions, times or weight of vegetable consumption. We undertook a pooled analysis with 13 of the 17 studies comparing an ECEC‐based healthy eating intervention with usual practice/no‐intervention control. Pooled analysis of vegetable servings consumed provides very low‐certainty evidence with an estimated pooled effect of SMD 0.12 (95% CI −0.01 to 0.25; P = 0.08, I2 = 70%; 3335 children; Analysis 3.1). A SMD of 0.12 is equivalent to an increase of 0.14 servings of vegetables. We downgraded the certainty of evidence because we assessed eight studies at high overall risk of bias, there was considerable heterogeneity (I2 = 70%), and strong detection of publication bias as assessed via visual inspection of funnel plots. The effect size was reduced in the sensitivity analysis excluding those at high risk of bias (SMD 0.06, 95% CI −0.05 to 0.17; P = 0.25, I2 = 0%; 1276 children; Analysis 3.2). We did not conduct a sensitivity analysis excluding industry‐funded studies as there were none.
3.2. Analysis.

Comparison 3: Vegetable consumption, Outcome 2: Vegetable consumption (sensitivity: studies at low overall risk of bias)
Of the 17 studies, we were unable to include four in the meta‐analysis due to insufficient data (e.g. missing SD, missing sample sizes; De Bock 2011; Morris 2018; Namenek Brouwer 2013; Pinket 2016). An additional four studies reported on outcomes deemed as not appropriate for pooling in the meta‐analysis due to differences in the way the outcomes were reported (Başkale 2011; Natale 2014b; Natale 2021; Witt 2012). Witt 2012 reported on the percentage of vegetable snacks children consumed in care, as assessed using a weighed food record, Başkale 2011 reported on weekly consumption of vegetables on a scale of 1 to 5, and both Natale 2014b and Natale 2021 measured rate of vegetable consumption (per week). Seven of the eight studies demonstrated improvements in the intervention group (see Figure 8 for harvest plot).
Subgroup analyses
Health Promoting Schools Framework
Nine studies with 2400 children targeted the curriculum in their healthy eating intervention and had a pooled effect of SMD 0.07 (95% CI −0.01 to 0.16), compared to four studies that did not target the curriculum (SMD 0.21, 95% CI −0.19 to 0.60; 935 children). No subgroup effect was noted (P = 0.52, I2 = 0%; Analysis 3.3). Eleven studies with 3042 children targeted partnerships in their healthy eating intervention and had a pooled effect of SMD 0.11 (95% CI −0.04 to 0.25) compared to two studies that did not target partnerships (SMD 0.19, 95% CI −0.19 to 0.57; 293 children). No subgroup effect was noted (P = 0.69; I2 = 0%; Analysis 3.4). All studies targeted ethos and environment, and as such, we could not undertake any subgroup analysis by these domains.
3.3. Analysis.

Comparison 3: Vegetable consumption, Outcome 3: Vegetable consumption (Health Promoting Schools: curriculum versus no curriculum)
3.4. Analysis.

Comparison 3: Vegetable consumption, Outcome 4: Vegetable consumption (Health Promoting Schools: partnerships versus no partnerships)
Socioeconomic status
Four studies were classed as specifically undertaken with low‐socioeconomic status populations, and had a pooled effect of SMD −0.04 (95% CI −0.19 to 0.11; 717 children), compared to nine that were undertaken with high socioeconomic status populations (SMD 0.19, 95% CI 0.03 to 0.35; 2618 children). We observed a subgroup effect favouring the studies undertaken with high socioeconomic status populations (P = 0.04, I2 = 75.8%; Analysis 3.5).
3.5. Analysis.

Comparison 3: Vegetable consumption, Outcome 5: Vegetable consumption (SES: low versus high/unclear)
Other subgroup analyses
As we did not identify high statistical heterogeneity in the primary analysis (I2 < 75%) we did not undertake any further subgroup analyses.
Fruit and vegetable consumption
Six studies measured the consumption of fruit and vegetables together. We undertook a pooled analysis including four of the five studies that reported on servings of fruit and vegetables combined, comparing an ECEC‐based healthy eating intervention with usual practice. Findings from the pooled analysis found no evidence of an effect on those receiving the intervention on servings of fruit and vegetable consumed (SMD 0.05, 95% CI −0.05 to 0.15; P = 0.36, I2 = 0%; 1547 children; see Analysis 4.1). The effect was increased in the sensitivity analysis excluding those at high risk of bias (SMD 0.08, 95% CI −0.05 to 0.21; P = 0.23, I2 = 0%; 919 children; Analysis 4.2). We did not conduct a sensitivity analysis excluding industry‐funded studies as there were none.
4.2. Analysis.

Comparison 4: Fruit and vegetable consumption, Outcome 2: Fruit and vegetable consumption (sensitivity: studies at low overall risk of bias)
We were unable to include one of the five studies in the meta‐analysis due to missing data (Morris 2018). An additional study reported on an outcome (i.e. proportion of children consuming four or more servings of fruit) not included in the meta‐analysis (Iaia 2017). Both studies demonstrated favourable effects in the intervention group.
Subgroup analyses
Due to the small number of studies included in the meta‐analysis (fewer than five), we did not undertake any subgroup analyses.
Non‐core foods (less healthy/discretionary foods) consumption
Eleven studies that compared an ECEC‐based healthy eating intervention with usual practice or no intervention reported on consumption of non‐core foods (i.e. less healthy/discretionary). We included seven of the eight studies that reported on servings or portions, times or weight of non‐core foods consumption in the meta‐analysis. Pooled analysis including seven studies provides moderate‐certainty evidence that healthy eating interventions likely result in little to no difference in number of times non‐core foods are consumed (SMD −0.05, 95% CI −0.17 to 0.08; P = 0.48, I2 = 16%; 1369 children; Analysis 5.1). A SMD of −0.05 is equivalent to consuming non‐core foods 0.04 times fewer per day. We assessed the certainty of evidence as moderate due to five studies assessed as overall high risk of bias. The pooled effect was higher (less favourable) when we excluded studies at high risk of bias, however, we included only two studies in this analysis (SMD 0.11, 95% CI −0.11 to 0.34; P = 0.31, I2 = 0%; 316 children; Analysis 5.2). We did not conduct a sensitivity analysis excluding industry‐funded studies as there were none.
5.2. Analysis.

Comparison 5: Non‐core foods consumption, Outcome 2: Non‐core foods (i.e. less healthy/discretionary) consumption (sensitivity: studies at low overall risk of bias)
Of the seven studies, we were unable to include one study in the meta‐analysis due to missing data (Morris 2018), and two further studies because they used measures we deemed not appropriate for pooling; Natale 2014b and Natale 2021 reported on the rate of snack consumption (per week). Two of the three studies favoured the intervention (see Figure 8 for harvest plot).
Subgroup analyses
Health Promoting Schools Framework
Three studies targeted the curriculum in their healthy eating intervention and had a smaller pooled effect (SMD −0.05, 95% CI −0.18 to 0.08; 982 children), compared to four studies that did not target the curriculum (SMD −0.13, 95% CI −0.48 to 0.22; 387 children). No subgroup effect was noted (P = 0.69, I2 = 0%; Analysis 5.3). All studies targeted ethos and environment, and only one study did not actively target partnerships and as such, we could not undertake any subgroup analysis by those components.
5.3. Analysis.

Comparison 5: Non‐core foods consumption, Outcome 3: Non‐core foods (i.e. less healthy/discretionary) consumption (Health Promoting Schools: curriculum versus no curriculum)
Socioeconomic status
We did not undertake a subgroup analysis by socioeconomic status as only one study was classed as taking place in a low‐socioeconomic status population.
Other subgroup analyses
As we did not identify any high statistical heterogeneity in the primary analysis (I2 < 75%) we did not undertake any further subgroup analyses.
Sugar‐sweetened beverage consumption
Seven studies comparing an ECEC‐based healthy eating intervention with usual practice or no intervention reported on portions or servings of sugar‐sweetened beverages consumed. Pooled analysis including three studies provides moderate‐certainty evidence that healthy eating interventions probably result in little to no difference in portions/servings of sugar‐sweetened beverages consumed for those receiving the healthy eating intervention (SMD −0.10, 95% CI −0.34 to 0.14; P = 0.41, I2 = 45%; 522 children; Analysis 6.1). A SMD of −0.10 is equivalent to 0.16 fewer portions or servings of sugar‐sweetened beverage. We downgraded the certainty of evidence as we assessed two studies at high overall risk of bias. We did not conduct a sensitivity analysis as only one study was classed as low risk of bias.
We were unable to include one of the five studies that reported on servings/ounces (1 ounce = approximately 28 g) due to missing data (Morris 2018 ). An additional two studies used different measures including proportion of children not consuming any sugar‐sweetened beverages daily (Iaia 2017), and proportion of children consuming sugar‐sweetened beverages daily (Kobel 2019). Two of the three studies favoured the intervention (see Figure 8 for harvest plot).
Subgroup analyses
Due to the small number of studies included in the meta‐analysis (fewer than five), we did not undertake any subgroup analyses.
Secondary outcomes
BMI
Seventeen studies measured BMI. Pooled analysis of 15 studies found that ECEC‐based healthy eating interventions may result in little to no difference in child BMI (MD −0.08, 95% CI −0.23 to 0.07; P = 0.30, I2 = 65%; 3932 children; Analysis 7.1). Excluding those studies that had some industry contribution did not change the effect size (MD −0.10, 95% CI −0.28 to 0.07; P = 0.26, I2 = 69%; 3319 children; Analysis 7.2). We assessed the certainty of evidence for BMI as low due to high heterogeneity and evidence of potential publication bias. We did not conduct a sensitivity analysis excluding by study quality as no studies were classified as high risk of bias. Two studies did not provide any data on BMI and were not included in the meta‐analysis (De Bock 2011; Kornilaki 2021). These studies reported that the intervention found no significant intervention effects on child BMI.
7.2. Analysis.

Comparison 7: BMI, Outcome 2: BMI (sensitivity: studies with no industry funding)
Subgroup analyses
Health Promoting Schools Framework
Thirteen studies targeted the curriculum in their healthy eating intervention and had a lower (more favourable) pooled effect (MD −0.13, 95% CI −0.29 to 0.03; 3506 children) compared to two studies that did not target the curriculum (MD 0.27, 95% CI −0.15 to 0.68; 426 children). No subgroup effect was noted (P = 0.08, I2 = 66.9%; Analysis 7.3). We did not undertake a subgroup analysis by ethos and environment as only one study did not actively target this as part of the intervention. All studies targeted partnership, and as such we could not undertake any subgroup analysis.
7.3. Analysis.

Comparison 7: BMI, Outcome 3: BMI (Health Promoting Schools: curriculum versus no curriculum)
Socioeconomic status
Eleven studies with 2804 children were categorised as specifically undertaken with a low‐socioeconomic status population and had a lower (more favourable) pooled effect (MD −0.10, 95% CI −0.29 to 0.08) compared to four studies undertaken with high/unclear socioeconomic status groups (MD 0.02, 95% CI −0.17 to 0.22; 1128 children). No subgroup effect was noted (P = 0.36, I2 = 0%; Analysis 7.4).
7.4. Analysis.

Comparison 7: BMI, Outcome 4: BMI (SES: low versus high/unclear)
Other subgroup analyses
As we did not identify high statistical heterogeneity in the primary analysis (I2 < 75%) we did not undertake any further subgroup analyses.
BMI z‐score
Twenty studies reported on BMI z‐score outcomes; 19 studies reported on BMI z‐score and one study reported on annual changes in BMI z‐score (Stookey 2017). We were able to pool data from 17 of the 19 studies that reported on BMI z‐scores, which found that healthy eating interventions may result in little to no difference in child BMI z‐scores (MD −0.03, 95% CI −0.09 to 0.03; P = 0.36, I2 = 0%; 4766 children; Analysis 8.1). We assessed the certainty of evidence for BMI z‐score as high. The effect was reduced in the sensitivity analysis excluding studies at high risk of bias (MD −0.01, 95% CI −0.08 to 0.06; I2 = 0%; P = 0.80, 14 studies, 3645 children; Analysis 8.2). We did not conduct a sensitivity analysis excluding industry‐funded studies as there were was only one study.
8.2. Analysis.

Comparison 8: BMI z‐score, Outcome 2: BMI z‐score (sensitivity: studies at low overall risk of bias)
One study reported on a different measure (i.e. annual changes in BMI z‐score) which we were unable to pool in the meta‐analysis (Stookey 2017). We were also unable to include two of the 19 studies that reported BMI z‐score in the meta‐analysis as they did not provide total sample data (Natale 2014a; Peñalvo 2015). All three studies found favourable effects of the intervention on child BMI z‐score.
Subgroup analyses
Health Promoting Schools Framework
Twelve studies targeted the curriculum in their healthy eating intervention and had a lower (more favourable) pooled effect (MD −0.03, 95% CI −0.09 to 0.04; 3867 children), compared to five studies that did not target the curriculum (MD 0.00, 95% CI −0.17 to 0.18; 899 children). No subgroup effect was noted (P = 0.75, I2 = 0%; Analysis 8.3). We did not undertake a subgroup analysis by ethos and environment, or partnerships, as only one study did not actively target these components in their intervention.
8.3. Analysis.

Comparison 8: BMI z‐score, Outcome 3: BMI z‐score (Health Promoting Schools: curriculum versus no curriculum)
Socioeconomic status
Ten studies with 2193 participants were categorised as specifically undertaken with low‐socioeconomic status children and had a similar pooled effect (MD −0.01, 95% CI −0.11 to 0.08), compared to seven studies undertaken with high/unclear socioeconomic status groups (MD −0.04, 95% CI −0.13 to 0.06; 2573 children). No subgroup effect was noted (P = 0.73, I2 = 0%; Analysis 8.4).
8.4. Analysis.

Comparison 8: BMI z‐score, Outcome 4: BMI z‐score (SES: low versus high/unclear)
Other subgroup analyses
As we did not identify high statistical heterogeneity in the primary analysis (I2 < 75%) we did not undertake any further subgroup analyses.
Absolute weight in kilograms (kg)
Nine studies measured weight and we included them all in the meta‐analysis. Pooled analysis on these nine studies found that children who received the healthy eating intervention on average had lower weight by 0.23 kg (95% CI −0.49 to 0.03; P = 0.09, I2 = 0%; 2071 children; Analysis 9.1). We assessed the certainty of evidence as high. We did not conduct a sensitivity analysis by study quality as only one study was classed as high risk and there were no industry‐funded studies.
Subgroup analyses
Health Promoting Schools Framework
We did not undertake any subgroup analysis by the Health Promoting Schools' components as all studies targeted ethos and environment, and partnership as part of their intervention. Only one study did not target the curriculum.
Socioeconomic status
Six studies with 1600 children were categorised as specifically undertaken with low‐socioeconomic status children and had a smaller (less favourable) pooled effect (MD −0.22, 95% CI −0.52 to 0.08) on weight compared to three studies undertaken with high/unclear socioeconomic status groups (MD −0.26, 95% CI −0.82 to 0.30; 471 children). No subgroup effect was noted (P = 0.90, I2 = 0%; Analysis 9.2).
9.2. Analysis.

Comparison 9: Absolute weight (kg), Outcome 2: Absolute weight (kg) (SES: low versus high/unclear)
Other subgroup analyses
As we did not identify high heterogeneity in the primary analysis (I2 < 75%) we did not undertake any further subgroup analyses.
Overweight and obesity
Five studies reported on number of children with overweight and obesity and we included them all in the meta‐analysis. Pooled analysis of these five studies found that those receiving the healthy eating intervention have a reduced risk ratio of 0.81 (95% CI 0.65 to 1.01; P = 0.07, I2 = 0%; 1070 children) for overweight and obesity (see Analysis 10.1). We assessed the certainty of evidence as high. This equates to an absolute risk reduction of 19%, however, the 95% CI indicates possible positive and negative effects.
Subgroup analyses
Health Promoting Schools Framework
We did not undertake any subgroup analysis by the Health Promoting Schools' components as all studies targeted partnerships and only one did not target ethos and environment, or the curriculum as part of their intervention.
Socioeconomic status
Two studies with 806 children were categorised as specifically undertaken with low‐socioeconomic status children and had a pooled effect of RR 0.86 (95% CI 0.67 to 1.11) on weight compared to three studies undertaken with high/unclear socioeconomic status groups (RR 0.69, 95% CI 0.43 to 1.09; 264 children). No subgroup effect was noted (P = 0.40, I2 = 0%; Analysis 10.4).
10.4. Analysis.

Comparison 10: Overweight and obesity, Outcome 4: Overweight and obesity (SES: low versus high/unclear)
Other subgroup analyses
As we did not identify high heterogeneity in the primary analysis (I2<75%) we did not undertake any further subgroup analyses.
Waist circumference
Three studies reported on the impact of the ECEC‐based healthy eating intervention on waist circumference. Pooled analysis on two studies estimated a reduction in waist circumference for those receiving the healthy eating intervention by MD 0.82 cm (95% CI −1.35 to −0.29; P = 0.002; I2 = 0%; 838 children; Analysis 11.1). Peñalvo 2015 did not provide a sample and as such could not be included in the meta‐analysis. The study authors reported a favourable effect of the intervention on waist circumference.
Subgroup analyses
Due to the small number of studies included in the meta‐analysis (fewer than five), we did not undertake any subgroup analyses.
Language and cognitive outcomes
Two studies reported on language and cognitive outcomes. Ray 2020 reported on the effect of vegetable tasting sessions and nutrition games on cognitive self‐regulation skills using five items derived from the Child Social Behaviour Questionnaire, rated on a scale of 1 to 3, previously used in the Millennium Cohort Study on three year olds. The study found evidence of a between‐group difference (SMD 0.05, 95% −0.14 to 0.24; 432 children).
Puder 2011 found varying evidence of an effect of the intervention on measures of concentration, assessed using a validated measure, Konzentrations‐Handlungsverfahren für Vorschulkinder. The study found a reduction in attention measured in minutes (SMD −0.06, 95% CI −0.29 to 0.16; 309 children) and an increase in attention measured by number of correct cards (SMD 0.02, 95% CI −0.17 to 0.21; 434 children), and in spatial working memory (SMD 0.12, 95% CI −0.07 to 0.31; 434 children).
Social/behavioural outcomes
Two studies reported on social and behavioural outcomes. Fernandez‐Jimenez 2019 reported on the impact of a multi‐component, ECEC‐based healthy eating intervention that included education meetings with children and family and 11 activities delivered by ECEC educators. The authors reported on child scores on the Test of Emotion Comprehension questionnaire that was used to assess emotional understanding, and found favourable effects (SMD 0.15, 95% CI −0.09 to 0.40; 282 children).
Ray 2020 reported on the effect of vegetable tasting sessions and nutrition games on emotional self‐regulation skills using five items derived from the Child Social Behaviour Questionnaire rated on a scale of 1 to 3, previously used in the Millennium Cohort Study on three year olds. The study found evidence of a between‐group difference (SMD 0.08; 95% −0.11 to 0.26; 432 children).
Child quality of life
Three studies comparing an ECEC‐based healthy eating intervention with usual practice or no intervention reported on a measure of quality of life. All measures were validated, score‐based and continuous, including the Paediatric Quality of Life Inventory (PedsQL) 4.0 (Kipping 2019; Puder 2011), and parent proxy version of KIDSCREEN‐10 (Yoong 2020a). Pooled analysis of all three studies found no evidence of effect of those receiving the ECEC‐based healthy eating intervention on child quality of life (SMD 0.07, 95% CI −0.09 to 0.23; P = 0.37, I2 = 0%; 644 children; Analysis 12.1).
Subgroup analyses
Due to the small number of studies included in the meta‐analysis (fewer than five), we did not undertake any subgroup analyses.
Cost assessments
Six studies presented cost assessments of ECEC‐based interventions with varying levels of detail. Only one study undertook a formal economic analysis examining the impact of a web‐based menu‐planning intervention to improve child dietary intake in ECEC (Yoong 2020a). This was conducted on the primary outcome of menu compliance with dietary guidelines rather than on child diet, and assessed the impact of an online menu planning program together with health promotion practitioner support relative to usual care. The prospective economic evaluation of the intervention versus usual practice was conducted from a modified societal perspective over 12 months. A modified societal perspective allows for the financial implications of various stakeholders to be taken into account. This economic analysis was constrained to those who would be impacted financially by the intervention, and as such included the health services (as the organisation providing implementation support) and ECEC services (as the ones enacting the changes).
At 12‐month follow‐up, these costs were calculated to be AUD 4634 per centre for intervention services and AUD 7640 per centre for usual practice services. The mean difference in total cost (intervention plus menu planning and review investment) was −AUD 482 (95% uncertainty interval (UI) −AUD 859 to −AUD 56). That is, the average cost per intervention service would be AUD 482 less per year than for usual practice services. The average cost‐effectiveness ratio for usual practice was ‐AUD 2897 and the Relative Vigour Index was calculated to be 1.11 and should be interpreted to mean that the intervention offers better outcomes at an acceptable cost.
Natale 2014b undertook a cost analysis of the Healthy Caregiver‐Healthy Children Program (HC2) that was targeted primarily towards low‐income, ethnically diverse children in the USA. The HC2 intervention consisted of: implementing daily nutrition‐ and physical activity‐focused curricula for teachers, parents, and separately, for children; providing technical assistance with menu modifications; and the creation of centre policies on dietary requirements for meals and snacks, time spent engaging in physical activity and limited television viewing. This was delivered over 12 months, with booster sessions in years 2 and 3. The total cost of HC2 was valued at USD 206,319 (estimated at a cost of USD 114 per child in year 1, and USD 29 per child in years 2 and 3), totalling USD 172 per child.
Leis 2020 undertook a study to describe the implementation costs of the Saskatchewan/New Brunswick Healthy Start‐Départ Santé (HS‐DS) intervention that was focused on supporting ECEC services to implement healthy eating and physical activity programmes. The implementation steps included engaging with ECEC directors and educators, training, booster training, provision of materials and ongoing support. All the inputs (including staff time, materials, development cost and support services) into the programme were characterised and then costed to provide an overall cost of implementing a programme. The total overall cost of implementing HS‐DS slightly decreased each year from USD 378,753 (year 1), USD 356,861 (year 2) and USD 312,179 (year 3), equating to approximately USD 258 per child.
Three studies captured intervention costs, however, did not do a formal cost analysis. Kipping 2019 captured all intervention costs associated with delivering the NAP SACC UK programme. The total cost of the workshop delivery in nurseries was GBP 4373 including trainers' time, refreshments, equipment, administration and travel (as a one‐off cost). The mean cost incurred by each nursery was GBP 717 (SD GPB 260). The mean cost of health visitor intervention delivery (including workshop delivery) per nursery was GBP 1092 (SD GBP 198). The NAP SACC UK at Home element cost GBP 11,947. Additionally, there was a small increase in self‐reported family food expenditure between baseline and follow‐up in both the intervention (GBP 17; SD GBP 52) and the control arms (GBP 3; SD GBP 46), and mean spend on physical activity (intervention: GBP 7; SD GBP 113; control: GBP 5; SD GBP 28).
Iaia 2017 captured the cost associated with intervention delivery (including educator training and parent motivational interviewing) should it be carried out again in the future, however, did not include one‐off costs (i.e. project planning, database management). The estimated cost was EUR 6500 for delivery of the training by a psychiatrist, two psychologists and two experts in early childhood physical activity. Additionally, it was estimated that the time for delivering the intervention by all participants and healthcare professionals was a total of 1094 hours, and an additional EUR 4000 was estimated for cost of printing the educational material.
Stookey 2017 estimated that the ECEC‐based intervention (including 16 hours of health professional one‐on‐one support provided to the ECEC educator) was low‐cost and required one full‐time staff person at the local ECEC agency to co‐ordinate processes. Additionally, all operation costs were covered through grant funds of less than USD 100,000 per year. The integration of the Healthy Apple programme with a child health programme required child health staff to spend approximately 16 hours more per ECEC centre than routine services.
All six studies estimated overall implementation cost including cost to both the health service (i.e. healthcare providers) and ECEC service and one included cost to the home (Kipping 2019). The only study that did a formal economic analysis found that the intervention offered a better outcome at an acceptable cost. Two studies reported cost per child and this was USD 172 and USD 258 per child. All other studies described total cost to deliver the intervention with varying detail. The few studies that described relevant economic evaluations indicate that economic evidence regarding ECEC‐based healthy eating interventions to improve child diet is currently lacking (Aluko 2022).
Adverse consequences
We undertook an exploratory approach to describe all or any potential adverse effects mentioned in the included studies. Three studies included an explicit measure to assess potential unintended adverse effects of the healthy eating intervention (Kipping 2019; Pearson 2022; Seward 2018).
In the evaluation of NAP SACC UK (Kipping 2019), centre managers and those delivering the intervention (health visitors and trainers) were asked to contact the study team within five working days if any untoward incident or adverse event occurred to a member of staff or child, as a direct result of participation in the study. Study‐specific adverse event/incident report forms were made available, and no events were reported.
Seward 2018 reported no evidence of a difference between intervention and control service cooks receiving negative feedback about the service menu in the past month from educators (intervention 32% (n 7/22 services) versus control 25% (n 4/16 services); P = 0.62), children (intervention 32% (n 7/22) versus control 6% (n 1/16); P = 0.07) or parents (intervention 9% (n 2/ 22) versus control 0% (n 0/16); P = 0.95). There were also no significant differences, after adjusting for baseline values, observed between groups for the estimated average % of food classified as waste for each meal: morning tea (adjusted difference −0.41, 95% CI −2.35 to 1.52; P = 0.66); lunch (adjusted difference 3.31, 95% CI −2.64 to 9.27; P = 0.26); and afternoon tea (adjusted difference −1.24, 95% CI −3.77 to 1.28; P = 0.31).
Pearson 2022 assessed whether there were increases in frequency of parent complaints or concerns regarding a m‐health intervention targeting packing of lunch boxes and introducing a lunchbox policy and found no evidence of differences between intervention and control groups.
None of the three studies reported a higher number of adverse effects from participation in the intervention. Overall, this review identified few studies specifically assessing and describing adverse events, indicating that the evidence surrounding adverse consequences of the delivery of ECEC‐based healthy eating interventions is currently lacking.
Studies not reporting on primary or secondary outcomes synthesised in our review
Four studies (Nekitsing 2019a; Reyes‐Morales 2016; Yeh 2018; Zeinstra 2018) met our eligibility criteria and were included in this review, however, did not report on any of the primary and secondary outcomes synthesised in our review. This primarily included studies that assessed child consumption of single foods including Nekitsing 2019a, which reported on child consumption of a test vegetable (mooli), Zeinstra 2018, which reported on child consumption of pumpkin, white radish and courgette and Reyes‐Morales 2016, which reported on the proportion of children consuming sugary water, plain water, fruit water, soft drink, processed juice, savoury milk, yoghurt, fritters, hamburgers, hotdogs, French fries and pizza separately. Yeh 2018 did not report on child diet and reported on child BMI percentile, which was not included in our synthesis.
Discussion
Summary of main results
Our review found that healthy eating interventions delivered in ECEC settings may improve child diet quality, but the evidence is very uncertain and likely increases fruit consumption (moderate‐certainty evidence). There is uncertainty about the effect of ECEC‐based healthy eating interventions on vegetable consumption (very low‐certainty evidence). The exploratory subgroup analysis found that the effect on vegetable consumption may be higher in high socioeconomic status populations compared to low‐socioeconomic status populations (P = 0.04). ECEC‐based healthy eating interventions likely result in little to no difference in consumption of non‐core foods (i.e. less healthy/discretionary) and sugar‐sweetened beverages, with moderate‐certainty evidence.
In terms of secondary outcomes, healthy eating interventions may have favourable effects on child weight (high‐certainty evidence) and risk of being overweight or obese (moderate‐certainty evidence), although they may result in little to no difference in mean BMI (low‐certainty evidence) and BMI z‐scores (high‐certainty evidence). The meta‐analyses of two studies suggest some favourable findings of ECEC‐based healthy eating interventions on child waist circumference, however, given the small number of studies, the evidence remains highly uncertain. For weight loss interventions, the US Preventive Services Task Force suggests that a BMI z‐score reduction of 0.20 to 0.25 may be clinically significant and equivalent to a 5% weight loss (US Preventive Services Task Force 2017). For prevention interventions, however, there is no clear consensus on what constitutes a clinically significant reduction in weight gain for this age group. Other studies have reported that a small energy deficit (~ 400 kJ/day) in children can meaningfully reduce the prevalence of overweight and obesity (Cochrane 2016; Wang 2012). As such, it is likely that an effect of this magnitude for both weight (approximately 230 g) and waist circumference (0.82 cm) if sustained, could be meaningful at a population level.
Three or fewer studies examined child social and emotional outcomes, language and cognitive outcomes and quality of life, suggesting that little is known about the impact of ECEC‐based healthy eating interventions on these outcomes. Less than 15% of the included studies assessed cost or cost‐effectiveness (providing very low‐certainty evidence about whether interventions are cost‐effective) and adverse consequences (providing low certainty evidence of little to no adverse consequences).
Overall, findings from our review support existing recommendations for the delivery of ECEC‐based healthy eating interventions by providing empirical evidence from RCTs that ECEC‐based healthy eating interventions may improve some measures of child diet and child physical outcomes, with little evidence of any adverse consequences. It should be noted, however, that the certainty of this evidence is moderate to very low.
Overall completeness and applicability of evidence
We undertook a comprehensive database search of RCTs using a validated search filter, supplemented by searches of grey literature, trials registries, and protocols, and author contact. As such, it is unlikely that many published studies were missed in this process. However, visual inspection of the forest plots indicated some asymmetry potentially due to publication bias (i.e. studies with null results may have not been published or are delayed in publication). The majority of the studies were conducted in the USA (20 studies), Australia (6 studies) and Israel (4 studies), and no studies were undertaken in low‐ and low‐ to middle‐income countries. Therefore, findings from studies included in this review are likely applicable to public health and education decision making in high‐income countries only and the effectiveness of these interventions in low‐ and lower‐middle‐income countries remains unknown. All but one study was undertaken in children aged between two and six years, therefore the impact of the interventions on children aged six months to two years also remains unknown.
The majority of the studies targeted multiple risk factors (primarily physical activity, 35 interventions, (60%)). Therefore, the effects of interventions that target healthy eating in isolation remains unknown. The majority of studies (in 37 interventions, 64%) also targeted all three Health Promoting Schools' components (health curriculum, ethos and environment, and partnership). Although we undertook a number of subgroup analyses to explore potential differences in effects on dietary outcomes by these components, there was no evidence to suggest any difference by subgroups. As such, we know very little about the specific components of ECEC‐based healthy eating interventions that may be associated with improved child dietary outcomes.
We included only RCTs in this review as they are considered the gold standard design for exploring intervention effects. It is possible that inclusion of non‐randomised studies may have captured different studies, including those from low‐income countries. However, given that the original aim of the review was to establish efficacy of ECEC‐based healthy eating interventions and the large number of included studies, it was not feasible for us to include non‐randomised evidence in the current review.
Quality of the evidence
Several factors may limit the certainty of the evidence outlined in this review. The most common reason for downgrading was due to studies assessed as high risk of bias overall, inconsistency (as assessed via I² statistic values from the meta‐analysis) and publication bias (as assessed through visual inspection of the forest plot). The number of studies classified as high risk of bias overall is unsurprising as this is primarily related to blinding of participants and personnel. For dietary outcomes, blinding of participants and personnel, and of outcome assessors, is highly challenging, introducing the potential for performance and detection bias in outcome assessments. Additionally, blinding of participants to intervention allocation is often not possible with the types of interventions assessed in this review. Future studies should better report on blinding of outcome assessors and statistical analyses, particularly for measures such as diet where objective measurement is challenging or high‐cost, or both. For diet quality and vegetable consumption, we noted high heterogeneity and publication bias via the visual inspection of forest plots. Some inconsistency in findings was also expected given the differences in target populations, characteristics of the intervention, the ways in which these outcomes were assessed and follow‐up periods. Additionally, our subgroup analysis did not find any evidence favouring small studies (< 400 children). It is possible that positive results bias may have been present, however, the included outcomes appear to be well distributed across both positive and negative findings, and there was little indication of selective publishing in our review of trial registry and protocol papers.
Attrition bias also appears prevalent across studies, particularly for measures of dietary intake. Attrition is challenging for interventions delivered in this setting due to families moving or changing services, or children in the older rooms transitioning to schools and leaving ECEC. Some studies have attempted to address this by utilising cross‐sectional study designs, where children are resampled at baseline and follow‐up. Further reporting of reasons for dropout and comparison of characteristics between those dropping out with those who were retained, will help with future assessments of attrition bias. Lastly, very few studies assessed adverse consequences and cost, and we downgraded evidence for indirectness as many RCTs were not designed to directly answer this question.
In the sensitivity analysis removing studies classed as high overall risk of bias, we noted a reduction in the estimated pooled effect, with evidence no longer supporting a positive effect for diet quality (SMD 0.34 vs 0.21) and fruit consumption (SMD 0.11 vs. 0.05) suggesting that these findings may need to be interpreted with caution. Baseline imbalance and loss of clusters were the main reasons for this, indicating that attrition bias (particularly at a cluster level) could have resulted in more positive results given the likelihood that those who were not responding to the intervention may be more likely to drop out. However, this could also be attributed to the smaller sample size and number of included studies.
Potential biases in the review process
We attempted to minimise positive results bias in interpreting study results by involving multiple authors in the review and interpretation process and by following publishing guidance when describing study findings (Santesso 2020). Authors did not screen, extract data, or undertake any risk of bias assessments for any studies that they were involved in for this review. As many of the review authors also undertake primary research related to the review topic, it is possible that we have interpreted the results to be more positive. While we attempted to adhere to the methods outlined in the review protocol as closely as possible (Yoong 2021), we included a posthoc decision rule for selecting from multiple dietary and anthropometric outcomes due to the large number of different outcomes measured in these studies. However, the selection of these outcomes was based on a core outcome set for early intervention studies to prevent obesity (Brown 2022), which were most commonly reported in studies, and allowed for comparison with population‐level guidelines.
Agreements and disagreements with other studies or reviews
Overall, although no other systematic reviews with a meta‐analysis directly addressing the same question exist, our findings are consistent with reviews addressing similar questions more broadly. This includes a living systematic review by Hodder 2020, which included all healthy eating interventions targeting children aged five years and under (ECEC‐ and non‐ECEC‐based) that found small effects of multicomponent interventions, child feeding interventions and parent nutrition education interventions on fruit and vegetable consumption. Our effect sizes for fruit and vegetable consumption are comparable to those described in Hodder 2020. A Cochrane Review examining obesity prevention interventions among children aged zero to five years also found a small pooled effect of physical activity and nutrition interventions on child BMI and BMI z‐scores (Brown 2019). Similarly, the effect sizes are comparable across our review and in Brown 2019.
Other non‐Cochrane reviews that have explored ECEC‐based interventions specifically have used narrative or vote‐counting approaches, have included non‐controlled studies and did not report on the impact of the interventions on specific dietary outcomes (Matwiejczyk 2018; Van de Kolk 2019; Ward 2015; Yoong 2020b; Yuan 2014). Despite these differences, findings from our review are broadly consistent with previous reviews that reported primarily positive effects on dietary outcomes and inconsistent effects on child weight outcomes. Further, previous reviews also described a small‐to‐moderate effect size, consistent with that identified in our review for a range of dietary outcomes. Our review significantly adds to the evidence base by describing the effects of only RCTs on specific dietary outcomes and examining impact on a broader range of child physical outcomes.
Authors' conclusions
Implications for practice.
Findings from our review support the likely positive impact of healthy eating interventions delivered in early childhood education and care settings (ECEC) on a number of dietary and anthropometric outcomes, although certainty of evidence was moderate to very low. It highlights the importance of this setting to support the development of healthy eating behaviours in the early years and as a key setting for population‐wide obesity prevention efforts.
Most of the interventions delivered in this setting targeted all components of the Health Promoting Schools Framework and also included efforts to promote physical activity. This review provides compelling evidence for ECEC educators and managers to prioritise the delivery of multi‐component healthy eating interventions, including those that target the curriculum, ethos and environment, and partnerships with community and parents. Despite the potential benefits, the challenges with implementing multi‐component and comprehensive healthy eating programmes in ECEC settings have been well described, with suboptimal implementation documented across many jurisdictions (Grady 2019; Yoong 2016). There is, therefore, a need for government action and investment to support co‐ordinated, population‐wide implementation on multiple levels, if the benefits of such programmes are to result in larger health gains.
The WHO have released Global Standards for Healthy Eating, Physical Activity and Sedentary Behaviour in the ECEC setting (World Health Organization 2021). This resource provides guidance regarding national and subnational actions that can be taken by policy and decision makers to provide supportive systems to implement these programmes in practice. The key strategies outlined include providing policy leadership, resourcing and financing, building workforce capability, generating evidence‐informed standards and establishing partnerships. A Cochrane Review by the authors of this review also describes a number of local‐level, evidence‐based implementation strategies that can be employed by local health promotion teams or other organisations responsible for supporting obesity prevention efforts in ECEC (Wolfenden 2020). This includes providing educational materials, educational meetings, audit and feedback, opinion leaders, small incentives or grants, educational outreach visits or academic detailing and reminders that can be provided to ECEC services.
Implications for research.
Findings from this review highlighted a number of areas where limited evidence exists and future research is likely warranted. Only one randomised controlled trial (RCT) targeted children aged between six months to two years, and found a positive improvement in child vegetable consumption (Blomkvist 2021). Given the increasing number of parents returning to work and accessing ECEC services for their young children, future studies targeting this age group are needed to support the development of healthy infant feeding behaviours. Additionally, we found only two RCTs undertaken in family day care settings, which were both conducted in the USA, consistent with our previous review of controlled trials in this setting (Yoong 2020b). Family day care services are structurally different from centre‐based services and provide care to a significant proportion of young children in high‐income countries. Additionally, a number of studies suggest that these services may be accessed by more disadvantaged groups (Benjamin‐Neelon 2018; Lindsay 2015; Lum 2021). Therefore, interventions in this setting provide an opportunity to influence the nutrition behaviour of these groups.
Critically, our review found that no studies have been undertaken in low‐ and lower‐middle‐income countries. This lack of research focusing on young children's activity and healthy eating in low‐ and middle‐income countries has been previously documented (Kariippanon 2022; Zhou 2014), with much of the existing ECEC‐based intervention research primarily focused on child cognitive, educational and developmental outcomes. Such outcomes may be more aligned to the immediate priorities and needs of low‐ and middle‐income countries. It is possible that the delivery and evaluation of ECEC‐based healthy eating interventions in these countries may need to be integrated within other programmes focused on child learning and development more broadly. As observational studies have documented associations between improved child nutrition and cognitive and behavioural outcomes (Khalid 2017; O'Neil 2014; Tandon 2016), we sought also to explore the impact of healthy eating interventions on these outcomes. However, we identified few studies that measured these outcomes and of those that did, findings indicate possible positive and negative effects. Lastly, few studies formally reported undertaking a cost evaluation and assessing adverse consequences. Future research should attempt to examine more directly any adverse consequences and undertake formal prespecified cost evaluations in order to provide essential data needed for decision making.
While findings from this review highlight the potential for this setting to deliver effective healthy eating programmes, little is known about the specific characteristics of the intervention that may have influenced child diet and physical outcomes. Given the challenges and additional resourcing needed to implement complex interventions, a better understanding of the discrete components that influence child health outcomes are needed to support prioritising of implementation efforts. We are aware of a number of multi‐arm (Grady 2020), or factorial trials (Zarnowiecki 2021), to allow for better understanding of the impact of discrete intervention components. For example, Zarnowiecki 2021 applied the multiphase optimisation strategy (MOST) which is a multiphase experimental design to support optimisation of an ECEC‐based healthy eating intervention. This study is currently in progress and utilises a factorial RCT design to describe the impact of different strategies targeting the curriculum, and ethos and environment components of ECEC‐based healthy eating interventions. Additionally, the inclusion of comparative effectiveness studies (those that compared two healthy eating interventions) are likely to help with better understanding the effects of different intervention components.
Finally, we identified a large number of dietary outcomes that have been assessed in studies of ECEC‐based healthy eating interventions. Despite the large number of studies included overall in the review, the variability in reported outcomes resulted in only small number of studies included for each dietary outcome synthesised in our review. A recent publication outlines the development of a recommended core outcome set, including key dietary and anthropometric measures for early obesity prevention studies (Brown 2022). The reporting of outcomes consistent with that outlined in the recommended core outcomes will reduce heterogeneity in outcomes and increase the likelihood of new studies being in future meta‐analyses.
History
Protocol first published: Issue 2, 2021
Acknowledgements
This review is funded by National Health and Medical Research Council Centre for Research Excellence grant (CIA: Luke Wolfenden, CIG Sze Lin Yoong, APP1153479). Sze Lin Yoong was a research fellow funded by an Australian Research Council Discovery Early Career Researcher Award while working on this review (DE170100382). Luke Wolfenden is a Hunter New England Clinical Research Fellow and is supported by a National Health and Medical Research Council (NHMRC) Career Development Fellowship (1128348) and Heart Foundation Future Leader Fellowship (101175). Alice Grady receives salary support from a Heart Foundation Postdoctoral Fellowship (102518). Therese McDonnell was part supported by the Health Research Board (Ireland) and the HSC Public Health Agency (Grant number CBES‐2018‐001) through Evidence Synthesis Ireland and Cochrane Ireland. Infrastructure support was provided by Hunter New England Population Health and Hunter Medical Research Institute. Salary support was provided by Deakin University, University of Newcastle, Montclair State University and Hunter New England Population Health.
Appendices
Appendix 1. Electronic databases search terms
| MEDLINE (OVID) search | |
| 1 | Exp Diet/ |
| 2 | Nutrition*.mp. |
| 3 | (health* adj2 eat*).mp. |
| 4 | Child Nutrition Sciences/ |
| 5 | Exp Fruit/ |
| 6 | Fruit*.mp. |
| 7 | Vegetable/ |
| 8 | Vegetable*.mp. |
| 9 | ((Fruit or vegetable) adj2 juice).mp. |
| 10 | Canteen.mp. |
| 11 | Food Services/ |
| 12 | Menu*.mp. |
| 13 | (Calories or kilocalories or kilojoules).mp. |
| 14 | Energy density.mp. |
| 15 | Eating/ |
| 16 | Feeding Behavio?r*.mp. |
| 17 | Dietary intake.mp. |
| 18 | Food habits/ |
| 19 | Food/ |
| 20 | Carbonated beverages/ |
| 21 | Soft drink*.mp. |
| 22 | Soda.mp. |
| 23 | Sugar‐Sweetened beverages/ |
| 24 | Dietary fats/ |
| 25 | Confectionary.mp. |
| 26 | (school adj2 (lunch* or meal*)).mp. |
| 27 | Menu planning.mp. |
| 28 | Feeding program*.mp. |
| 29 | Food program*.mp. |
| 30 | (nutrition* adj2 program*).mp. |
| 31 | Cafeteria*.mp. |
| 32 | Nutritional status/ |
| 33 | Dietary salt.mp. |
| 34 | Table salt.mp. |
| 35 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 |
| 36 | Child, Preschool/ |
| 37 | Child Day Care Centers/ |
| 38 | (childcare* or child care*).mp. |
| 39 | (daycare* or day care*).mp. |
| 40 | Early child*.mp. |
| 41 | (nursery or nurseries).mp. |
| 42 | Kinder*.mp. |
| 43 | (family or home base or homebased or in home).mp. |
| 44 | (pre‐school* or preschool*).mp |
| 45 | 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 |
| 46 | Randomized controlled trial.pt. |
| 47 | Controlled clinical trial.pt. |
| 48 | Randomized.ab. |
| 49 | Trial.ti. |
| 50 | Randomly.ab. |
| 51 | Clinical Trials as topic.sh. |
| 52 | 46 or 47 or 48 or 49 or 50 or 51 |
| 53 | 35 and 45 and 52 |
| 54 | Animals/ not humans/ |
| 55 | 53 not 54 |
| Embase (OVID) search | |
| 1 | Exp diet/ |
| 2 | Nutrition*.mp. |
| 3 | Nutrition/ |
| 4 | (health* adj2 eat*).mp. |
| 5 | Child nutrition sciences.mp. |
| 6 | Nutritional science/ |
| 7 | Fruit*.mp. |
| 8 | Fruit/ |
| 9 | ((fruit or vegetable) adj2 juice).mp. |
| 10 | Vegetable*.mp. |
| 11 | Vegetable/ |
| 12 | Canteen*.mp. |
| 13 | Food Services.mp. |
| 14 | Catering service/ |
| 15 | Menu*.mp. |
| 16 | (calories or kilocalories or kilojoules).mp. |
| 17 | Energy intake.mp. |
| 18 | Caloric intake/ |
| 19 | Energy density.mp. |
| 20 | Eating/ |
| 21 | Feeding behaviu?r*.mp. |
| 22 | Feeding behaviour/ |
| 23 | Dietary intake.mp. |
| 24 | Dietary intake/ |
| 25 | Food habit*.mp. |
| 26 | Food/ |
| 27 | Carbonated beverage/ |
| 28 | Soft drink*.mp. |
| 29 | Soft drink/ |
| 30 | Soda.mp. |
| 31 | Sugar‐sweetened beverage/ |
| 32 | Dietary fats.mp. |
| 33 | Fat intake/ |
| 34 | Confectionary.mp. |
| 35 | (school adj2(lunch* or meal*)).mp. |
| 36 | Menu Planning.mp. |
| 37 | Feeding program*.mp. |
| 38 | Food program*.mp. |
| 39 | (nutrition* adj2 program*).mp. |
| 40 | Cafeteria*.mp. |
| 41 | Nutritional status/ |
| 42 | Dietary salt.mp. |
| 43 | Table salt.mp. |
| 44 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 |
| 45 | Child, Preschool/ |
| 46 | (pre‐school* or preschool*).mp. |
| 47 | Day care/ |
| 48 | Child care/ |
| 49 | Childcare*.mp. |
| 50 | (daycare* or day care*).mp. |
| 51 | Early child*.mp. |
| 52 | (nursery or nurseries).tw. |
| 53 | Kinder*.mp. |
| 54 | (family or home based or homebased or “in home”).mp. |
| 55 | 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 |
| 56 | “randomized controlled trial”/ |
| 57 | “controlled clinical trial”/ |
| 58 | Randomized.ab. |
| 59 | Trial.ti. |
| 60 | Randomly.ab. |
| 61 | 56 or 57 or 58 or 59 or 60 |
| 62 | 44 and 55 and 61 |
| 63 | Animal experiment/ |
| 64 | “human experiment”/ |
| 65 | Human/ |
| 66 | 64 or 65 |
| 67 | 63 not 66 |
| 68 | 62 not 67 |
| PsycINFO (OVID) search | |
| 1 | Diets/ |
| 2 | Exp Nutrition/ or Nutrition*.mp. |
| 3 | (health* adj2 eat*).mp. |
| 4 | Child Nutrition Sciences.mp. |
| 5 | Fruit*.mp. |
| 6 | ((fruit or vegetable) adj2 juice).mp. |
| 7 | Vegetable*.mp. |
| 8 | Canteen*.mp. |
| 9 | Food Services.mp. |
| 10 | Menu*.mp. |
| 11 | (calories or kilocalories or kilojoules).mp. |
| 12 | Food Intake/ or Energy Intake.mp. |
| 13 | Energy density.mp. |
| 14 | Eating.mp. |
| 15 | Eating behaviour/ |
| 16 | Feeding behavio?r*.mp. |
| 17 | Dietary intake.mp. |
| 18 | Food/ |
| 19 | ((carbonated or sweetened or soft) adj (drink* or beverage*)).mp. |
| 20 | Soda.mp. |
| 21 | Dietary fat*.mp. |
| 22 | Confectionary.mp. |
| 23 | (school adj2 (lunch* or meal*)).mp. |
| 24 | Feeding program*.mp. |
| 25 | Food program*.mp. |
| 26 | (nutrition* adj2 program*).mp. |
| 27 | Cafeteria*.mp. |
| 28 | Dietary salt.mp. |
| 29 | Table salt.mp. |
| 30 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 |
| 31 | Preschool students/ or nursery school students/ |
| 32 | (pre‐school* or preschool*).mp. |
| 33 | Day Care Centers/ or Child Day Care/ |
| 34 | (childcare* or child care*).mp. |
| 35 | (daycare* or day care*).mp. |
| 36 | Early child*.mp. |
| 37 | (nurseries or nursery).mp. |
| 38 | Kindergarten Students/ or Kinder*.mp. |
| 39 | (family or home based or homebased).mp. |
| 40 | 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 |
| 41 | Randomi?ed controlled trial*.mp. |
| 42 | Clinical Trials/ |
| 43 | Trial.ti. |
| 44 | Randomized.ab. |
| 45 | Randomly.ab. |
| 46 | 41 or 42 or 43 or 44 or 45 |
| 43 | 30 and 40 and 46 |
| CINAHL (EBSCO) searcha | |
| S1 | (MH “Diet+”) |
| S2 | “nutrition*” |
| S3 | (MH “Nutrition”) |
| S4 | Health* n2 eat* |
| S5 | (MH “Child Nutrition”) |
| S6 | (MH “Vegetables”) OR “vegetable*” |
| S7 | Fruit* or ((fruit or vegetable) n2 juice) |
| S8 | “canteen*” |
| S9 | (MH “Food Services”) |
| S10 | (MH “Menu Planning”) OR “menu*” |
| S11 | Calories or kilocalories or kilojoules |
| S12 | (MH “Energy Intake”) OR (MH “Food Intake”) |
| S13 | (MH “Energy Density”) OR “Energy Density” |
| S14 | “feeding behavio?r*” |
| S15 | (MH “Eating”) OR (MH “Eating Behavior”) |
| S16 | “dietary intake” |
| S17 | (MH “Food Habits”) |
| S18 | (MH “Food”) |
| S19 | (MH "Carbonated Beverages”) OR “soft drink*” |
| S20 | Soda |
| S21 | “Sweetened drink*” |
| S22 | (MH “Dietary Fats”) |
| S23 | “confectionary” OR (MH “candy”) |
| S24 | School n2 (lunch* or meal*) |
| S25 | “feeding program*” |
| S26 | “food program*” |
| S27 | (nutrition* n2 program*) |
| S28 | Cafeteria* |
| S29 | (MH “Nutritional Status”) or "dietary salt" or "table salt" |
| S30 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 |
| S31 | (MH “Child, Preschool”) |
| S32 | “pre‐school*” or preschool* |
| S33 | (MH "Child Day Care") OR (MH "Child Care Providers") OR (MH "Child Care (Saba CCC)") OR (MH "Child Care") |
| S34 | Childcare* or "child care*" |
| S35 | Daycare* or "day care*" |
| S36 | "early child*" |
| S37 | (MH "Schools, Nursery") |
| S38 | Nursery or nurseries |
| S39 | Kinder* |
| S40 | Family or "home based" or homebased or "in home" |
| S41 | S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 |
| S42 | (MH "Randomized Controlled Trials") |
| S43 | (MH "Clinical Trials") |
| S44 | TI trial |
| S45 | AB random* |
| S46 | S42 OR S43 OR S44 OR S45 |
| S47 | S30 AND S41 AND S46 |
| CENTRAL search | |
| #1 | MeSH descriptor: [Diet] explode all trees |
| #2 | (nutrition*): ti,ab,kw |
| #3 | ((health*near/2 eat*)):ti,ab,kw |
| #4 | MeSH descriptor: [child nutrition sciences] explode all trees |
| #5 | (fruit*):ti,ab,kw |
| #6 | MeSH descriptor: [Fruit] this term only |
| #7 | (vegetable*):ti,ab,kw |
| #8 | MeSH descriptor: [vegetables] this term only |
| #9 | (canteen*):ti,ab,kw |
| #10 | MeSH descriptor: [Fruit and vegetable juices] this term only |
| #11 | ((fruit or vegetable) near/2 juice):ti,ab,kw |
| #12 | MeSH descriptor: [Food Services] this term only |
| #13 | (menu*):ti,ab,kw |
| #14 | (calories or kilocalories or kilojoules):ti,ab,kw |
| #15 | (“energy density”): ti,ab,kw |
| #16 | MeSH descriptor: [Eating] this term only |
| #17 | MeSh descriptor: [Feeding Behavior] this term only |
| #18 | (“feeding behavio*”):ti,ab,kw |
| #19 | (“dietary intake”):ti,ab,kw |
| #20 | MeSH descriptor: [Food] this term only |
| #21 | MeSH descriptor: [Carbonated Beverages] this term only |
| #22 | (“soft drink”): ti,ab,kw |
| #23 | (soda):ti,ab,kw |
| #24 | (“sweetened drink*”):ti,ab,kw |
| #25 | MeSH descriptor: [Dietary Fats] this term only |
| #26 | (confectionary):ti,ab,kw |
| #27 | (school near/2 (lunch* or meal*)):ti,ab,kw |
| #28 | MeSH descriptor: [Menu Planning] this term only |
| #29 | (“feeding program*”):ti,ab,kw |
| #30 | (“food program*”):ti,ab,kw |
| #31 | (nutrition* near/2 program*):ti,ab,kw |
| #32 | (cafeteria*):ti,ab,kw |
| #33 | MeSH descriptor: [Nutritional Status] this term only |
| #34 | {or #1‐#33} |
| #35 | MeSH descriptor: [child, preschool] this term only |
| #36 | (“pre‐school*” or preschool*):ti,ab,kw |
| #37 | MeSH descriptor: [Child Day Care Centers] this term only |
| #38 | (childcare* or “child care*”):ti,ab,kw |
| #39 | (daycare* or “day care*”):ti,ab,kw |
| #40 | (“early child*”):ti,ab,kw |
| #41 | (nursery or nurseries):ti,ab,kw |
| #42 | (Kinder):ti,ab,kw |
| #43 | Family or homebased or “home based” or “in home” |
| #44 | or #35‐#43 |
| #45 | and #34, #44 |
| SPORTDiscus (EBSCO) searchb | |
| S46 | S30 AND S40 AND S45 |
| S45 | S41 OR S42 OR S43 OR S44 |
| S44 | AB trial* or random* |
| S43 | TI trial* |
| S42 | “clinical trials” |
| S41 | Randomised controlled trial or randomized controlled trial |
| S40 | S31 or S32 or S33 or S34 or S35 or S36 or S38 or S39 |
| S39 | Family or “home based” or homebased or “in home” |
| S38 | Kinder* or preschool or early childhood education |
| S37 | Nursery or nurseries |
| S36 | “early child*” |
| S35 | Daycare* or “day care” |
| S34 | Childcare* |
| S33 | “child day care” or “child care providers” or “child care (saba CCC)” or “child care” |
| S32 | “pre‐school*” or preschool* |
| S31 | AB child, preschool |
| S30 | S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 |
| S29 | (AB “Nutritional Status”) OR “dietary salt” OR “table salt” |
| S28 | Cafeteria* |
| S27 | (nutrition* n2 program*) |
| S26 | ”food program*” |
| S25 | “feeding program*” |
| S24 | School n2 (lunch* or meal*) |
| S23 | “confectionary” OR (AB “candy”) |
| S22 | (AB “Dietary Fats”) |
| S21 | “Sweetened drink*” |
| S20 | Soda |
| S19 | (AB “Carbonated beverages” OR “Soft drink*” |
| S18 | (AB “Food”) |
| S17 | (AB “food habits”) |
| S16 | “dietary intake” |
| S15 | (AB “Eating”) OR (AB “Eating Behaviour”) |
| S14 | “feeding behavio?r*” |
| S13 | (AB “Energy density”) OR “Energy density” |
| S12 | (AB “Energy Intake”) OR (AB “Food Intake”) |
| S11 | Calories or kilocalories or kilojoules |
| S10 | (AB “Menu Planning”) OR “menu*” |
| S9 | (AB “Food Services”) |
| S8 | “canteen*” |
| S7 | Fruit* OR ((fruit OR vegetable) n2 juice) |
| S6 | (AB “vegetables” OR “vegetable*” |
| S5 | (AB “Child nutrition”) |
| S4 | Health* n2 eat* |
| S3 | (AB “Nutrition”) |
| S2 | “nutrition*” |
| S1 | “Diet” |
| ERIC (Proquest) search | |
| (Diet OR nutrition* OR (health* AND eat*) OR ("child nutrition") OR fruit* OR vegetable* OR ((fruit or vegetable) n/2 juice) OR canteen* OR menu* OR calories OR kilocalories OR kilojoules OR "energy intake" OR "energy density" OR eating OR ("feeding behavior" OR "feeding behaviors" OR "feeding behaviour") OR "dietary intake" OR food OR ((carbonated OR sweetened OR soft) n/2 (drink* or beverage*)) OR soda OR ("dietary fat" OR "dietary fats") OR confectionary OR (school n/2 (lunch* OR meal*)) OR ("feeding program" OR "feeding programme" OR "feeding programmes" OR "feeding programs") OR cafeteria* OR “dietary salt” OR “table salt”) AND ("pre‐school*" OR preschool* OR childcare* OR "child care" OR daycare* OR ("day care" OR "day career" OR "day cares") OR ("early child" OR "early childcare" OR "early childhood" OR "early children") OR nursery OR nurseries OR kinder* OR family OR homebased OR "home based" OR "in home") AND (Random* OR trial*) | |
| SCOPUS (Scopus) search | |
| TITLE‐ABS ( diet OR nutrition* OR ( health* W/2 eat* ) OR "Child Nutrition*" OR fruit* OR vegetable* OR ( ( fruit OR vegetable ) W/2 juice ) OR canteen* OR menu* OR calories OR kilocalories OR kilojoules OR "Energy Intake" OR "energy density" OR eating OR "Feeding Behavio*" OR "dietary intake" OR food OR ( ( carbonated OR sweetened OR soft ) AND ( drink* OR beverage* ) ) OR soda OR "Dietary Fat*" OR confectionary OR ( school AND ( lunch* OR meal* ) ) OR "feeding program*" OR cafeteria* OR "dietary salt" OR "table salt" ) AND TITLE‐ABS ( "pre‐school*" OR preschool* OR childcare* OR "child care*" OR daycare* OR "day care*" OR "early child*" OR nursery OR nurseries OR kinder* ) AND TITLE‐ABS ( random* OR trial* ) AND ( LIMIT‐TO ( EXACTKEYWORD , "Human" ) OR LIMIT‐TO ( EXACTKEYWORD, "Humans" ) ) | |
aUnless otherwise specified, the default search was used. This searches across the following fields.
Title
Abstract
Subject headings
PubMed ID
DOI
Author
bUnless otherwise specified, the default search was used. This searches across the following fields.
Authors
Subjects
Keywords
Title
Abstracts
Data and analyses
Comparison 1. Diet quality.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Diet quality | 6 | 1973 | Std. Mean Difference (IV, Random, 95% CI) | 0.34 [0.04, 0.65] |
| 1.2 Diet quality (sensitivity: studies at low overall risk of bias) | 3 | 957 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.03, 0.45] |
| 1.3 Diet quality (Health Promoting Schools: curriculum versus no curriculum) | 6 | 1973 | Std. Mean Difference (IV, Random, 95% CI) | 0.34 [0.04, 0.65] |
| 1.3.1 Curriculum | 2 | 639 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.11, 0.32] |
| 1.3.2 No curriculum | 4 | 1334 | Std. Mean Difference (IV, Random, 95% CI) | 0.46 [0.08, 0.84] |
| 1.4 Diet quality (SES: low versus high/unclear) | 6 | 1973 | Std. Mean Difference (IV, Random, 95% CI) | 0.34 [0.04, 0.65] |
| 1.4.1 Low | 3 | 834 | Std. Mean Difference (IV, Random, 95% CI) | 0.30 [0.16, 0.44] |
| 1.4.2 High/unclear | 3 | 1139 | Std. Mean Difference (IV, Random, 95% CI) | 0.40 [‐0.22, 1.01] |
| 1.5 Diet quality (intervention modality: included face‐to‐face, telephone and online delivery versus did not include face‐to‐face, telephone and online delivery) | 6 | 1973 | Std. Mean Difference (IV, Random, 95% CI) | 0.34 [0.04, 0.65] |
| 1.5.1 Included face‐to‐face, telephone and online delivery | 4 | 1334 | Std. Mean Difference (IV, Random, 95% CI) | 0.46 [0.08, 0.84] |
| 1.5.2 Did not include face‐to‐face, telephone and online delivery | 2 | 639 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.11, 0.32] |
| 1.6 Diet quality (intervention delivery personnel: included healthcare professionals versus did not include healthcare professionals) | 6 | 1973 | Std. Mean Difference (IV, Random, 95% CI) | 0.34 [0.04, 0.65] |
| 1.6.1 Included healthcare professionals | 4 | 1334 | Std. Mean Difference (IV, Random, 95% CI) | 0.46 [0.08, 0.84] |
| 1.6.2 Did not include healthcare professionals | 2 | 639 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.11, 0.32] |
Comparison 2. Fruit consumption.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Fruit consumption | 11 | 2901 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [0.04, 0.18] |
| 2.2 Fruit consumption (sensitivity: studies at low overall risk of bias) | 4 | 996 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.08, 0.17] |
| 2.3 Fruit consumption (Health Promoting Schools: curriculum versus no curriculum) | 11 | 2901 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [0.04, 0.18] |
| 2.3.1 Curriculum | 7 | 2037 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.01, 0.17] |
| 2.3.2 No curriculum | 4 | 864 | Std. Mean Difference (IV, Random, 95% CI) | 0.17 [0.03, 0.32] |
| 2.4 Fruit consumption (SES: low versus high/unclear) | 11 | 2901 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [0.04, 0.18] |
| 2.4.1 Low | 4 | 717 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.06, 0.23] |
| 2.4.2 High/unclear | 7 | 2184 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [0.03, 0.20] |
| 2.5 Fruit consumption (study size: small (< 400 participants) versus large (≥ 400 participants)) | 11 | 2901 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [0.04, 0.18] |
| 2.5.1 Small (< 400 participants) | 8 | 1518 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.01, 0.20] |
| 2.5.2 Large (≥ 400 participants) | 3 | 1383 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [0.02, 0.23] |
2.5. Analysis.

Comparison 2: Fruit consumption, Outcome 5: Fruit consumption (study size: small (< 400 participants) versus large (≥ 400 participants))
Comparison 3. Vegetable consumption.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Vegetable consumption | 13 | 3335 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.01, 0.25] |
| 3.2 Vegetable consumption (sensitivity: studies at low overall risk of bias) | 5 | 1276 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.05, 0.17] |
| 3.3 Vegetable consumption (Health Promoting Schools: curriculum versus no curriculum) | 13 | 3335 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.01, 0.25] |
| 3.3.1 Curriculum | 9 | 2400 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.01, 0.16] |
| 3.3.2 No curriculum | 4 | 935 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.19, 0.60] |
| 3.4 Vegetable consumption (Health Promoting Schools: partnerships versus no partnerships) | 13 | 3335 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.01, 0.25] |
| 3.4.1 Partnerships | 11 | 3042 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.04, 0.25] |
| 3.4.2 No partnerships | 2 | 293 | Std. Mean Difference (IV, Random, 95% CI) | 0.19 [‐0.19, 0.57] |
| 3.5 Vegetable consumption (SES: low versus high/unclear) | 13 | 3335 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.01, 0.25] |
| 3.5.1 Low | 4 | 717 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.19, 0.11] |
| 3.5.2 High/unclear | 9 | 2618 | Std. Mean Difference (IV, Random, 95% CI) | 0.19 [0.03, 0.35] |
| 3.6 Vegetable consumption (study size: small (< 400 participants) versus large (≥ 400 participants)) | 13 | 3335 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.01, 0.25] |
| 3.6.1 Small (< 400 participants) | 10 | 1952 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.06, 0.13] |
| 3.6.2 Large (≥ 400 participants) | 3 | 1383 | Std. Mean Difference (IV, Random, 95% CI) | 0.31 [‐0.02, 0.64] |
3.6. Analysis.

Comparison 3: Vegetable consumption, Outcome 6: Vegetable consumption (study size: small (< 400 participants) versus large (≥ 400 participants))
Comparison 4. Fruit and vegetable consumption.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Fruit and vegetable consumption | 4 | 1547 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.05, 0.15] |
| 4.2 Fruit and vegetable consumption (sensitivity: studies at low overall risk of bias) | 2 | 919 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.05, 0.21] |
Comparison 5. Non‐core foods consumption.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Non‐core foods (i.e. less healthy/discretionary) consumption | 7 | 1369 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.17, 0.08] |
| 5.2 Non‐core foods (i.e. less healthy/discretionary) consumption (sensitivity: studies at low overall risk of bias) | 2 | 316 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.11, 0.34] |
| 5.3 Non‐core foods (i.e. less healthy/discretionary) consumption (Health Promoting Schools: curriculum versus no curriculum) | 7 | 1369 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.17, 0.08] |
| 5.3.1 Curriculum | 3 | 982 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.18, 0.08] |
| 5.3.2 No curriculum | 4 | 387 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.48, 0.22] |
Comparison 6. Sugar‐sweetened beverage consumption.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Sugar‐sweetened beverage consumption | 3 | 522 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.34, 0.14] |
Comparison 7. BMI.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 BMI | 15 | 3932 | Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.23, 0.07] |
| 7.2 BMI (sensitivity: studies with no industry funding) | 13 | 3319 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.28, 0.07] |
| 7.3 BMI (Health Promoting Schools: curriculum versus no curriculum) | 15 | 3932 | Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.23, 0.07] |
| 7.3.1 Curriculum | 13 | 3506 | Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.29, 0.03] |
| 7.3.2 No curriculum | 2 | 426 | Mean Difference (IV, Random, 95% CI) | 0.27 [‐0.15, 0.68] |
| 7.4 BMI (SES: low versus high/unclear) | 15 | 3932 | Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.23, 0.07] |
| 7.4.1 Low | 11 | 2804 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.29, 0.08] |
| 7.4.2 High/unclear | 4 | 1128 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.17, 0.22] |
| 7.5 BMI (study size: small (< 400 participants) versus large (≥ 400 participants)) | 15 | 3932 | Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.23, 0.07] |
| 7.5.1 Small (< 400 participants) | 13 | 2705 | Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.31, 0.09] |
| 7.5.2 Large (≥ 400 participants) | 2 | 1227 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.17, 0.08] |
7.5. Analysis.

Comparison 7: BMI, Outcome 5: BMI (study size: small (< 400 participants) versus large (≥ 400 participants))
Comparison 8. BMI z‐score.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 BMI z‐score | 17 | 4766 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.09, 0.03] |
| 8.2 BMI z‐score (sensitivity: studies at low overall risk of bias) | 14 | 3645 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.08, 0.06] |
| 8.3 BMI z‐score (Health Promoting Schools: curriculum versus no curriculum) | 17 | 4766 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.09, 0.03] |
| 8.3.1 Curriculum | 12 | 3867 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.09, 0.04] |
| 8.3.2 No curriculum | 5 | 899 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.17, 0.18] |
| 8.4 BMI z‐score (SES: low versus high/unclear) | 17 | 4766 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.09, 0.03] |
| 8.4.1 Low | 10 | 2193 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.11, 0.08] |
| 8.4.2 High/unclear | 7 | 2573 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.13, 0.06] |
| 8.5 BMI z‐score (study size: small (< 400 participants) versus large (≥ 400 participants)) | 17 | 4766 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.09, 0.03] |
| 8.5.1 Small (< 400 participants) | 14 | 2935 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.12, 0.04] |
| 8.5.2 Large (≥ 400 participants) | 3 | 1831 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.10, 0.09] |
8.5. Analysis.

Comparison 8: BMI z‐score, Outcome 5: BMI z‐score (study size: small (< 400 participants) versus large (≥ 400 participants))
Comparison 9. Absolute weight (kg).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 9.1 Absolute weight (kg) | 9 | 2071 | Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.49, 0.03] |
| 9.2 Absolute weight (kg) (SES: low versus high/unclear) | 9 | 2071 | Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.49, 0.03] |
| 9.2.1 Low | 6 | 1600 | Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.52, 0.08] |
| 9.2.2 High/unclear | 3 | 471 | Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.82, 0.30] |
Comparison 10. Overweight and obesity.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 10.1 Overweight and obesity | 5 | 1070 | Risk Ratio (IV, Random, 95% CI) | 0.81 [0.65, 1.01] |
| 10.2 Overweight and obesity (sensitivity: studies at low overall risk of bias) | 4 | 1022 | Risk Ratio (IV, Random, 95% CI) | 0.86 [0.69, 1.09] |
| 10.3 Overweight and obesity (sensitivity: studies with no industry funding) | 4 | 418 | Risk Ratio (IV, Random, 95% CI) | 0.81 [0.59, 1.12] |
| 10.4 Overweight and obesity (SES: low versus high/unclear) | 5 | 1070 | Risk Ratio (IV, Random, 95% CI) | 0.81 [0.65, 1.01] |
| 10.4.1 Low | 2 | 806 | Risk Ratio (IV, Random, 95% CI) | 0.86 [0.67, 1.11] |
| 10.4.2 High/unclear | 3 | 264 | Risk Ratio (IV, Random, 95% CI) | 0.69 [0.43, 1.09] |
10.2. Analysis.

Comparison 10: Overweight and obesity, Outcome 2: Overweight and obesity (sensitivity: studies at low overall risk of bias)
10.3. Analysis.

Comparison 10: Overweight and obesity, Outcome 3: Overweight and obesity (sensitivity: studies with no industry funding)
Comparison 11. Waist circumference.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 11.1 Waist circumference | 2 | 838 | Mean Difference (IV, Random, 95% CI) | ‐0.82 [‐1.35, ‐0.29] |
Comparison 12. Quality of life.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 12.1 Quality of life | 3 | 644 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.09, 0.23] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alkon 2014.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 7 months Unit of allocation: centre Unit of analysis: child |
|
| Participants |
Service type: centre‐based Operation: not reported Country (region): USA (California, Connecticut, North Carolina) Country income classification: high Low‐SES sample: yes Population description: racial/ethnic diversity among the children Inclusion criteria: included English‐speaking director, on‐site kitchen, racial/ethnic diversity among the children, participation by at least 60% of families and a population of children in care primarily comprised of low‐income children between the ages of 3‐5 years Exclusion criteria: chronic illnesses or conditions that affected nutritional status, severe food allergies, gastrointestinal disorders or mobility impairment Number of services randomised: 18 (9 intervention, 9 control) Number of children randomised: 552 (260 intervention, 292 control) Characteristics Children Age: Intervention: 3 years: 31%; 4 years: 50%; 5 years: 19% Control: 3 years: 29%; 4 years; 54%; 5 years: 17% Gender (% female): Intervention: 44% Control: 48% Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: Intervention: white: 55%; African American: 17%; Hispanic, Latino: 15%; Asian: 8%; other: 5% Control: white: 37%; African American: 16%; Hispanic, Latino: 19%; Asian: 19%; other: 9% Parent/family SES: Employment status (primary caregiver): Intervention: working full time: 74%; working part time: 14%; unemployed: 2%; student: 5%; not working: 5% Control: working full time: 74%; working part time: 17%; unemployed: 5%; student: 2%; not working: 2% Parent education (primary caregiver): Intervention: < high school: 23%; high school and higher: 77% Control: < high school: 44%; high school and higher: 56% Method of recruitment: not reported Missing data/dropout: 1 control centre withdrew and was replaced with a matched centre prior to intervention Reasons for dropout: the centre was unable to complete the required number of study questionnaires. Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: NAP SACC (The Nutrition And Physical Activity Self‐Assessment for Child Care) Number of conditions: 1 intervention, 1 control Intervention duration: 7 months Intervention setting: ECEC Intervention strategies: Ethos and environment ECEC staff Workshops: NAP SACC workshops for ECEC providers and staff included education on childhood obesity, healthy eating for young children, physical activity for young children, personal health and wellness and working with families to promote healthy behaviours. Support: on‐site consultations and additional telephone and email consultations Resources: written materials around nutrition and physical activity were provided to staff. Service Materials: posters displayed in centres and information sheets on nutrition and physical activity Policy: child‐care health consultants worked with centre directors to write and update the centre's nutrition and physical activity policies. Partnerships Families Workshop: services were provided the parent workshop 'raising healthy kids'. Resources: written materials around nutrition and physical activity were provided to parents. Healthcare Delivery: nurse child healthcare consultants delivered the intervention to staff and parents. Intensity of intervention: 5 x 1‐h NAPSACC workshops to ECEC providers and staff (e.g. cooks, administration); 1 x at least monthly consultations; additional phone and email consultations and posters and information sheets distributed (and displayed in the centre and provided to parents) Intervention delivered by: healthcare staff Modality: face‐to‐face, telephone, online, written Theoretical basis: not reported Description of control: delayed intervention control |
|
| Outcomes |
Outcomes relating to child dietary intake: not reported Outcomes relating to child physical measures: BMI z‐score, % underweight, % healthy weight, % overweight, % obese Number of participants analysed: Intervention baseline: 99 Intervention follow‐up: 99 Control baseline: 110 Control follow‐up: 110 Data collection measure: objectively measured (CDC) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: grant funded by the US Department of Health and Human Services, health resources and services administration, maternal and child health research program | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Children's height and weight were measured by a research assistant blinded to group assignment. |
| Incomplete outcome data (attrition bias) Physical outcomes | High risk | One cluster withdrew prior to the intervention but after randomisation and was replaced. Study authors stated that "There were 211 children (63% of 336) with measurements at both the pre‐ and post‐intervention periods." Due to the magnitude of missing data, we assessed the risk of bias as high. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol, and trial registration is vague so it was unclear whether there was selective outcome reporting |
| Recruitment bias | Unclear risk | It is unclear whether allocation occurred before or after baseline data collection. One control cluster was lost and replaced with a matched centre prior to intervention but after randomisation. |
| Baseline imbalance | Unclear risk | Although centres were matched on size and proportion of children eligible for income subsidies, groups significantly differed in parent ethnicity, parent education, employment status, and household density. Only state, parent education, and family poverty were included in regression analysis. Some known confounders of children's BMI, such as parent BMI and child‐level accelerometer and sleep data, were not collected. |
| Loss of clusters | Low risk | One control cluster lost and replaced with a matched centre prior to intervention |
| Incorrect analysis | Low risk | Hierarchical linear models were conducted to assess child‐level BMI z‐score outcomes while accounting for clustering within centres. |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Unclear risk | Study authors stated that "Third, some centres had more child‐level data and some states had more centres contributing to the final analyses. Fourth, some known confounders of children's BMI, such as parent BMI and child‐level accelerometer and sleep data were not collected... Lastly, there was a historical cohort effect on both the intervention and control centres given obesity prevention campaigns at the national level (i.e., Let's Move Child Care) and legislation (i.e., Healthy Hunger‐Free Kids Act) in the U.S. that promoted healthy nutrition and physical activity in child care during the study period." There is insufficient information to assess whether an important risk of bias exists. |
Başkale 2011.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 4 months (varies with outcomes) Unit of allocation: nursery schools Unit of analysis: child |
|
| Participants |
Service type: centre‐based (nurseries) Operation: nursery schools connected to the Izmir Provincial Directorate of National Education Country (region): Turkey (Izmir) Country income classification: upper‐middle Low‐SES sample: no Population description: nursery schools connected to the Izmir Provincial Directorate of National Education. These schools were layered into the 3 socioeconomic levels they represent: low‐, middle‐, and upper‐income brackets. 2 schools from each bracket were included. Inclusion criteria: 12 nursery schools are connected to the Izmir Provincial Directorate of National Education. Children included in the study were 5 years of age. The children in the control group had not received nutrition education but they had received a general programme of education (the nutrition education prescribed by the Ministry of National Education preschool). Exclusion criteria: not reported Number of services randomised: 12 (6 intervention, 6 control) Number of children randomised: 238 (141 intervention, 97 control) Characteristics Children Age: not reported Gender (% female): not reported Ethnicity: not reported Parents Age (years): Intervention: mother: 33.45; father: 36.96 Control: mother 33.42; father: 36.84 Gender (% female): both mother and father reported Ethnicity: not reported Parent/family SES: low: 16%; medium: 73.1%; upper: 10.9 % Method of recruitment: not reported Missing data/dropout: 11 children (4.6%) were lost to follow‐up. Reasons for dropout: some sample losses were experienced, often due to illness, moving, and registering for the primary schools’ preclasses children would attend the next year. Characteristics of dropouts: there were no differences between the dropped‐out children/parents and the children/parents who remained in the study. |
|
| Interventions |
Programme name: not reported Number of conditions: 1 intervention, 1 control Intervention duration: 6 weeks Intervention setting: ECEC Intervention strategies: Health curriculum Children Education: game‐based nutrition education was delivered to children, guided by a nurse educator, including activities such as playing, painting, colouring and interactive stories. Partnerships Healthcare Delivery: a nurse educator guided the nutrition education. Intensity of intervention: 20‐30‐min sessions once a week for 6 weeks (classes were divided into groups and held with 8‐15 children). Parent nutrition education sessions were given to both intervention and control (1.5‐2 h). Intervention delivered by: research team, healthcare staff Modality: face‐to‐face Theoretical basis: Piaget’s Cognitive Development Theory Description of control: usual care, plus parents in both groups were provided with the same nutrition education (1.5‐2 h) to present them with information on children’s nutritional needs and educational booklet |
|
| Outcomes |
Outcomes relating to child dietary intake: Weekly frequency of vegetable consumption, weekly frequency of green leafy vegetables, weekly frequency of root vegetables, weekly frequency of cabbage, weekly frequency of citrus, weekly frequency of other fruits Number of participants analysed Intervention baseline: 141 Intervention follow‐up: 141 Control baseline: 97 Control follow‐up: 97 Data collection measure: FFQ Data collector: parents Validity of measures used: not reported Outcomes relating to child physical measures: BMI, mid‐upper arm circumference, underweight, healthy weight, overweight or obese, underweight, healthy weight, mid‐upper arm circumference ≤ 10, mid‐upper arm circumference > 10 to < 85, mid‐upper arm circumference ≥ 85 Number of participants analysed: Intervention baseline: 37 Intervention follow‐up: 37 Control baseline: 48 Control follow‐up: 48 Data collection measure: objectively measured (CDC) Data collector: not reported Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: no external or intramural funding was received. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 2 schools from each income bracket (low, middle, and upper) were drawn from a bag, then randomised to intervention and control. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Diet outcomes | Unclear risk | Blinding not reported, and it is not clear whether parents were aware of allocation as parents in both experimental and control groups were provided the same nutrition education. Parents completed the food frequency form prior to the intervention, following the intervention, and 1 year after the intervention. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | Unclear risk | Blinding not reported, and it is not clear whether parents were aware of allocation as parents in both experimental and control groups were provided the same nutrition education. Parents completed the food frequency form prior to the intervention, following the intervention and 1 year after the intervention. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's weight, height, and mid‐upper arm circumference were measured and are not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Low risk | Data were available for 139 (99%) students in the intervention group and 88 (91%) students in the control group at post‐test 1, and 67 (48%) students in the intervention group and 48 (49%) students in the control group at post‐test 2. Post‐tests occurred a year apart, and an ITT analysis was conducted. Reasons provided for attrition (i.e. illness, moving, and registering for primary schools) appear reasonable. Therefore, risk of attrition bias was considered to be low. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Data were available for 67 (48%) students in the intervention group and 48 (49%) students in the control group at post‐test 2. An ITT analysis was conducted. Reasons provided for attrition (i.e. illness, moving, and registering for primary schools) appear reasonable. Therefore, risk of attrition bias was considered to be low. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting. |
| Recruitment bias | Unclear risk | There is no information regarding whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Low risk | The analysis showed that the groups were not statistically different (P > 0.05). |
| Loss of clusters | Unclear risk | Not reported |
| Incorrect analysis | Unclear risk | Adjusting for clusters was not reported, though some of the sociodemographic characteristics of the families and children in the experimental and control groups were tested for homogeneity to confirm that there were no differences. There is not enough information to assess whether an important risk of bias exists. |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Unclear risk | The control group appears ambiguous and it is unclear if nutrition education, which was the intervention, was also delivered at the control schools. There is insufficient information to assess whether an important risk of bias exists. |
Blomkvist 2021.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 3 months Unit of allocation: kindergartens Unit of analysis: child |
|
| Participants |
Service type: kindergarten Operation: public and private Country (region): Norway ((Telemark, Oppland, Sør‐Trøndelag and Møre og Romsdal) Country income classification: high Low‐SES sample: unclear Population description: the 4 counties covered 2 different geographical areas of Norway and included public and private kindergartens located in both rural and urban settings. Inclusion criteria: having children of the appropriate age (i.e. born in 2016) Exclusion criteria: kindergartens registered as ‘open kindergartens’ in which children and their parents attend together (n = 18), kindergartens registered with < 4 children (n = 7) and kindergartens with children from 3‐5 years only (n = 12) were not invited. Number of services randomised: 46 kindergartens (16 intervention 1, 15 intervention 2, 15 control) Number of children randomised: 267 children (111 intervention 1, 85 intervention 2, 71 control) Characteristics Children Age: 16.7 months (SD 3.0) Gender (% female): 47.60% Ethnicity: all children were born in Norway Parents Age (years): 30.9 (SD 5.4) Gender (% female): 88.70% Ethnicity: Mother born in Norway: 91.5% Father born in Norway: 89.5% Parent/family SES: Mothers' education, high: 64% Fathers' education, high: 42.1% Method of recruitment: the invitations were sent to the kindergarten managers by email and included detailed information about the study and a link to the study registration web page. The kindergarten managers received 1 reminder email after a couple of weeks. As few kindergartens (n = 32) registered for the study initially, a random selection of kindergarten managers (n = 321) was additionally contacted by telephone and asked if they had received the email and further asked if they could be interested in participating in the study. The phone call recruitment lasted until the number of kindergartens registered was assumed to yield the planned study sample size. Missing data/dropout: total loss to follow‐up: 102/246 = 41% Reasons for dropout: 21 parents registered for the trial but did not complete the baseline questionnaire, leaving 246 children. 3 of the kindergartens (n = 29 children) withdrew consent shortly after randomisation (2 of them due to sick leaves and pregnancies amongst the staff and 1 kindergarten withdrew due to economic issues). 73 parents (34%) did not complete the post‐intervention questionnaire, leaving 144 children for the main analysis. Characteristics of dropouts: mothers without a higher education were more likely to drop out of the study. Amongst the complete cases, there were slightly fewer fathers with a higher education in Intervention 1, and a slightly higher baseline intake of intervention vegetables amongst children in Intervention 2. |
|
| Interventions |
Programme name: Barns matmot 2.0 Number of conditions: 2 interventions, 1 control Intervention duration: 12 weeks Intervention setting: ECEC Intervention strategies: Intervention 1 (Menu moderation and sensory lessons) Health curriculum Children Education: kindergarten staff were instructed to implement pedagogical tools including weekly sensory lessons for the participating children. Ethos and environment Children Exposure: during the sensory lessons, children were introduced to the intervention vegetable of the month, presented in 3 different ways; in the first week, it was presented raw, in the second week, raw with a dip and in the third week, it was presented differently (e.g. baked or otherwise prepared) (3 additional exposures of each food compared to Intervention 2). Children were served a warm lunch meal with alternating vegetables for 3 d/week during the 3‐month intervention period. Role modelling/healthy eating practices: kindergarten staff were given advice on meal practice and feeding practices during mealtime and encouraged to sit down with the children and eat the same food during lunchtime. Service Resources: the kindergartens had access to the 3 menus with 9 different recipes in a password‐protected website designed specifically for each intervention group. Each of the 3 menus had 1 vegetable in focus: spinach, celeriac and fennel. Recommendations for meal and feeding practices were also presented in short informational videos on the study website. Kindergartens were offered compensation to buy necessary kitchenware, such as a good knife, saucepans or a hand blender. Support: if the kindergarten personnel had questions during the intervention, they could email or telephone a contact person using information on the website. Families Resources: the parents of the registered children were also given access to the website with the 9 recipes; however, the parents had no commitments or tasks regarding introducing the menus at home. Recommendations for meal and feeding practices were also presented in short informational videos on the study website. Intervention 2 (Menu moderation) Ethos and environment Children Exposure: children were served a warm lunch meal with alternating vegetables for 3 d/week during the 3‐month intervention period. Service Resources: the kindergartens had access to the 3 menus with 9 different recipes in a password‐protected website designed specifically for each intervention group. Each of the 3 menus had one vegetable in focus: spinach, celeriac and fennel. Kindergartens were offered a compensation to buy necessary kitchenware, such as a good knife, saucepans or a hand blender. Support: if the kindergarten personnel had questions during the intervention, they could email or telephone a contact person using information on the website. Families Resources: the parents of the registered children were also given access to the website with the 9 recipes; however, the parents had no commitments or tasks regarding introducing the menus at home. Intensity of intervention: Intervention 1: children were exposed to 3 d/week for 3 months; staff implemented weekly sensory lessons in the classroom. Intervention 2: children were exposed to alternating vegetables for 3 d/week for 3 months. Intervention delivered by: Intervention 1: ECEC staff Intervention 2: ECEC staff Modality: Intervention 1: face‐to‐face, online, written Intervention 2: online, written Theoretical basis: not reported Description of control: Usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: Vegetable intake, intervention vegetables intake Number of participants analysed: Intervention 1 baseline: 103 Intervention 1 follow‐up: 63 Intervention 2 baseline: 78 Intervention 2 follow‐up: 42 Control baseline: 65 Control follow‐up: 39 Data collection measure: selected items from FFQ Data collector: parent Validity of measures used: not reported Outcomes relating to child physical measures: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: this research project was funded by the Norwegian Women’s Public Health Association, and some projects costs were funded by the University of Agder and the Teacher’s Education Unit at the University of Agder. Approximately one‐fifth of the wages cost for the corresponding author was funded by the Hospital of Southern Norway. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Study authors stated that "The random allocation sequence was generated in SPSS by the last author, who had neither contact with the kindergartens nor access to or information from the completed questionnaires." |
| Allocation concealment (selection bias) | Low risk | Study authors stated that "The 46 kindergartens included were randomised into one of three groups after the parents had completed the baseline questionnaire, approximately 2 weeks before the start of the intervention." |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | Study authors stated that "The first author contacted the kindergarten managers to inform them about which group they were randomised to." Blinding of staff not reported, though staff in the intervention groups had access to resources indicating blinding may have been broken and the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Study authors stated that "The first author contacted the kindergarten managers to inform them about which group they were randomised to." Parents completed the food frequency questionnaire. Blinding of parents not reported, though parents in the intervention groups had access to resources indicating blinding may have been broken. The outcome measurement is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | High risk | Study authors stated that "In total, 267 children were registered for the study. Twenty‐one parents registered for the trial but did not complete the baseline questionnaire, leaving 246 children. Three of the kindergartens (n = 29 children) withdrew consent shortly after randomisation (two of them due to sick leaves and pregnancies amongst the staff and one kindergarten withdrew due to economic issues). Seventy‐three parents (34%) did not complete the post‐intervention questionnaire, leaving 144 children for the main analysis (total loss to follow‐up: 102/246 = 41%)." A full intention‐to‐treat analysis could not be performed. Due to the magnitude of missing data, the risk of bias was assessed as high. |
| Selective reporting (reporting bias) | Low risk | Additional measures, including anthropometric data of children, were also collected according to the protocol, however the authors stated that "Only primary outcomes of the intervention are included in the present paper." |
| Recruitment bias | Low risk | All participants and kindergartens were recruited prior to randomisation. |
| Baseline imbalance | Low risk | Study authors stated that "The cluster randomisation produced groups that were broadly comparable at baseline." It is reported that there were slightly fewer fathers with a higher education in intervention 1, and a slightly higher baseline intake of intervention vegetables amongst children in intervention 2, based on case completers. The authors used adjusted models to control for these variables. |
| Loss of clusters | Low risk | Loss of 3 clusters, however reasons were unrelated to the intervention and comprised a small percentage of all clusters. Study authors stated that "Three of the kindergartens (n = 29 children) withdrew consent shortly after randomisation (two of them due to sick leaves and pregnancies amongst the staff and one kindergarten withdrew due to economic issues)." |
| Incorrect analysis | Unclear risk | Adjusting for clusters was not reported, however the authors stated that "To address any imbalances that may have resulted from the cluster design and losses to follow‐up, we also present a set of adjusted effect estimates, controlling for the baseline values of each outcome, and maternal and paternal education." There is not enough information to assess whether an important risk of bias exists. |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Céspedes 2013.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 6 months Unit of allocation: preschool Unit of analysis: child |
|
| Participants |
Sevice type: centre‐based Operation: not reported Country (region): Colombia (Usaquén, Bogota) Country income classification: upper‐middle Low‐SES sample: yes Population description: Usaquén represents the different SES levels seen in Colombia and includes an underprivileged community with a high migration rate. Inclusion criteria: all children 3–5 years of age at baseline and their parents and teachers were eligible. Exclusion criteria: children, parents or teachers who had received formal training in healthy habits, nutrition or physical activity in the 6 months before the study and children whose parents did not consent Number of services randomised: 14 (7 intervention, 7 control) Number of children randomised: 1216 children (622 intervention, 594 control) Characteristics Children Age: Intervention: 3 years: 55%; 4 years: 43.4%; 5 years: 1.6% Control: 3 years: 52%; 4 years: 44.8%; 5 years: 3.2% Gender (% female): Intervention: 47.6% Control: 46.3% Ethnicity: not reported Parents Age (years): Intervention: 31.25 (SD 8.1) Control: 29.94 (SD 6.8) Gender (% female): Intervention: 83.6% Control: 85.8% Ethnicity: not reported Parent/family SES: not reported ECEC staff Age (years): Intervention: 39.04 (SD 10.6) Control: 35.05 (SD 8.9) Gender (% female): Intervention: 100% Control: 98.5% Ethnicity: not reported Service/ECEC staff SES: SES of the neighbourhood where the preschool facility is located: Intervention: low: 57.1%; high: 42.9% Control: low: 71.4%; high: 28.6% Method of recruitment: not reported Missing data/dropout: all ECEC services were retained. 91.8% of children retained; 93.7% of parents retained; 88.9% of teachers retained Reasons for dropout: attrition was mainly due to school change or migration associated with factors such as local violence or changing jobs. Characteristics of dropouts: there were no significant differences associated with sex or weighted score change observed after the initial 5‐month period between those lost to follow‐up and those remaining in the study. In both cohorts, children lost to follow‐up were older (3.7 and 3.3 years, P < 0.01; and 3.8 and 3.1 years, P < 0.01, respectively). |
|
| Interventions |
Programme name: not reported Number of conditions: 1 intervention, 1 control Intervention duration: 5 months Intervention setting: ECEC Intervention strategies: Health curriculum Children Education: educational and playful activities including Sesame Workshop Healthy Habits story books, posters, videos, games and songs. Workshops: a "healthy family day" workshop with families Ethos and environment Children Resources: weekly health notes ECEC staff Training: 3 x centralised training sessions, plus personalised sessions with a research supervisor Resources: teachers' guide Partnerships Families Meeting: 1 x 1‐h presentation of the intervention Workshops: 3 x workshops Resources: weekly notes containing positive health messages about nutrition and active lifestyles to share with children Intensity of intervention: 1 h/d of Sesame Workshop Healthy Habits story‐books, posters, videos, games and songs for children; 1 x 1‐h "healthy family day" workshop; weekly health notes for children; 3 x parent workshops and weekly health notes; 3 x centralised teacher training sessions, plus personalised working sessions with research supervisor (2 h every 15 d) Intervention delivered by: research team Modality: face‐to‐face, written Theoretical basis: Social Cognitive Theory and the Transtheoretical Model Description of control: wait‐list control |
|
| Outcomes |
Outcomes relating to child dietary intake: not reported Outcomes relating to child physical measures: BMI, eutrophic, risk of undernourished, undernourished, overweight, obese Number of participants analysed: Intervention baseline: 488 Intervention follow‐up: 433 Control baseline: 476 Control follow‐up: 425 Data collection measure: objectively measured (CDC) Data collector: nutritionist Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: The Santo Domingo Foundation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A blinded randomisation assignment schedule was used to allocate to treatment groups. The sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Low risk | The blinded randomisation assignment schedule was concealed until treatments had been allocated. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured by nutritionists using standard techniques and were not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | 100 (8.2%) children were lost to follow‐up, with similar numbers of attrition in both groups (51/622 = 8.2% intervention, 49/594 = 8.2% control). Therefore, risk of attrition bias was considered to be low. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting |
| Recruitment bias | Low risk | Per the PRISMA diagram, full recruitment occurred before randomisation |
| Baseline imbalance | Low risk | There were no significant differences between groups with respect to baseline characteristics except for modest differences in teachers’ educational level, age of parents and teachers, and children's weight. The researchers ran additional models simultaneously, adjusting by the effect of parents’ and teachers’ age, and children’s weight. |
| Loss of clusters | Low risk | No loss of clusters |
| Incorrect analysis | Low risk | Study authors stated that “Changes between baseline and end‐of study scores were modelled as the outcome, randomisation assignment as the independent predictor variable of interest, and subject’s preschool facilities as the clustering variable.” |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Davis 2016.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 7 months Unit of allocation: Head Start centres Unit of analysis: child |
|
| Participants |
Service type: centre‐based (Head Start) Operation: Head Start centres Country (region): USA (New Mexico) Country income classification: high Low‐SES sample: yes Population description: a primarily Hispanic or American Indian student population and a location in a nonmetropolitan community within 150 miles (240 km) of the research centre. Inclusion criteria: Head Start centres were eligible for the study if they had at least 2 classrooms, ≥ 15 3‐year‐old children enrolled, a retention rate of at least 80% over 2 school years, a primarily Hispanic or American Indian student population and a location in a nonmetropolitan community within 150 miles (240 km) of the research centre. Exclusion criteria: Head Start centres housing other prekindergarten programs were excluded. Number of services randomised: 16 centres (8 intervention, 8 control) Number of children randomised: 1898 (945 intervention, 871 control) Characteristics Children Age: 2 years: 1.6%; 3 years: 41.1%; 4 years: 55.4%; 5 years: 1.8% Gender (% female): 47.4% Ethnicity: Hispanic: 57.2%; non‐Hispanic: 42.8% Parents Age (years): not reported Gender (% female): not reported Ethnicity: centre race/ethnicity: American Indian: 40.6%; Hispanic: 59.4% Parent/family SES: not reported Method of recruitment: Head Start centres were recruited by a community engagement specialist on the research team. Missing data/dropout: all ECEC services were retained. 74% of eligible population consented to participate. 99% of consenting participants provided data. Reasons for dropout: graduation or transfer to prekindergarten classes, the difficulty in instituting environmental and policy changes and the large effect size required by the small number of study sites. Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: CHILE: Child Health Initiatative for Lifelong Eating and Exercise Number of conditions: 1 intervention, 1 control Intervention duration: 2 years Intervention setting: ECEC, home and local community Intervention strategies: Health curriculum Children Education: a nutrition and physical activity curriculum for the Head Start centres provided to children. Each lesson incorporates child's development Head Start domains such as emotional/social, literacy and mathematics. Ethos and environment Children Exposure: children were provided opportunities to try new fruits and vegetables and to participate in physical activity during daily class activities. Menu modification: as new fruits and vegetables were introduced to children, they were incorporated in the school menu. ECEC staff Training: quarterly professional development for Head Start teachers and food service staff. Hands‐on sessions provide staff with information about physical activity and nutrition and technical assistance for implementing the intervention. Service Policy: policy changes were made for the food service to switch to healthier food products. Partnerships Families Resources: take‐home materials about nutrition and physical activity were provided to families. Events: 2 family events reinforcing these messages during the school year. Community Access: increasing availability and visibility of healthier food options in local grocery stores and providing recipes and nutrition‐related information to families while shopping. Healthcare Engagement: local healthcare providers were asked to emphasise healthy eating and physical activity during routine patient visits and health professionals were invited to attend family events to show support for the intervention. Intensity of intervention: nutrition curriculum to be incorporated into Head Start learning domains including literacy, maths or science; addition of 30 min of physical activity to daily class activities; quarterly professional development (8 sessions) for ECEC staff; in‐class nutrition lessons provide children multiple exposures to each novel fruit or vegetable; take home materials for families 2 times/year Intervention delivered by: research team, ECEC staff, healthcare staff Modality: face‐to‐face, written Theoretical basis: Socioecological approach Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: not reported Outcomes relating to child physical measures: Underweight, healthy weight, overweight, obese, adjusted BMI z‐score Number of participants analysed Intervention baseline: 210 Intervention follow‐up: 157 Control baseline: 226 Control follow‐up: 174 Data collection measure: objectively measured (CDC) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: The National Institute of Diabetes and Digestive and Kidney Diseases (Grant R01 DK72958) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Head Start centres were stratified by race/ethnicity and average BMI. A random uniform variable was generated for each centre. Centres with smaller values within each stratum were assigned to the intervention group until desired sample sizes were achieved. |
| Allocation concealment (selection bias) | Low risk | Before allocation, centres were stratified according to the race/ethnicity and average BMI of the centres' population. Randomisation occurred after all centres were recruited. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were assessed at the centres and were not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Physical outcomes | High risk | Data were available for 157 (75%) participants in the intervention group and 174 (77%) participants in the control group. Study authors stated that "Limitations of the CHILE study included the drop out of students due to graduation or transfer to prekindergarten classes." Due to the magnitude of missing data over the short‐term and long‐term follow‐up, the risk of bias was assessed as high. |
| Selective reporting (reporting bias) | Unclear risk | Outcomes are not clearly reported in the trial registration or trial protocol, so it was unclear whether there was selective outcome reporting. |
| Recruitment bias | Low risk | Individual recruitment occurred prior to cluster randomisation. |
| Baseline imbalance | Low risk | The intervention and comparison groups did not differ significantly at baseline. |
| Loss of clusters | Low risk | No loss of clusters |
| Incorrect analysis | Low risk | Study authors stated that "Analyses accounted for repeated measurements for Head Start centers and children by including random effects for each center and child." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Unclear risk | Study authors stated that "The large effect size required by the small number of study sites, which may have resulted in the study being underpowered." There is insufficient information to assess whether an important risk of bias exists. |
De Bock 2011.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 6 months Unit of allocation: preschool Unit of analysis: child |
|
| Participants |
Service type: centre‐based (preschools) Operation: not reported Country (region): Germany (Baden‐Württemberg) Country income classification: high Low‐SES sample: unclear Population description: the study was set in Baden‐Württemberg, a federal state (population nearly 11 million) in south‐west Germany with an extensive network of urban and rural preschools Inclusion criteria: preschools were eligible to participate in the study if they were located in 1 of 3 predefined regions and had applied to participate in the nutritional intervention module of a state‐sponsored health promotion programme ‘Komm mit in das gesunde Boot’ (‘Come aboard the healthy boat’) with at least 15 children participating. Exclusion criteria: sites were excluded if they had < 15 children participating in the state‐sponsored programme or if there was no external physical activity teacher available in the area. Number of services randomised: 18 preschools (10 intervention, 8 control) Number of children randomised: 377 (194 intervention, 183 control) Characteristics Children Age: 3 years: 16%; 4 years: 45.6%; 5 years: 33.6%; 6 years: 4.6% Gender (% female): 46.8% Ethnicity: without migrant background: 65.5%; with migrant background: 32.4%; missing: 2% Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: Maternal education level: low: 16.3%; middle: 55.7%; high: 21.2%; missing: 6.6% Method of recruitment: a 2‐level sampling strategy involving both preschools from 3 geographic regions that had formally applied for participation in the state‐sponsored programme and the parents of children enrolled at these sites Missing data/dropout: of the 348 preschool children providing data, 29.6% (n = 103) participated in measurements at all 3 time points, 51.4% (n = 179) children participated twice and 19.0% (n = 66) at 1measurement point, with 58.0 % of the children (n = 202) providing both pre and post‐intervention measurements. Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: ‘Komm mit in das gesunde Boot’ (‘Come aboard the healthy boat’) (nutrition module) Number of conditions: 1 intervention, 1 control Intervention duration: 6 months Intervention setting: ECEC and home Intervention strategies: Health curriculum Children Education: external nutrition experts delivered 15 x standardised 2‐h nutrition sessions, mostly during preschool hours, conducted once weekly over a 6‐month period. Ethos and environment Children Exposure: children were offered weekly healthy snacks like fruit and vegetables and water. Intervention activities included familiarising children with different food types and preparation methods and cooking and eating meals in groups of children, teachers and parents. ECEC staff Training: preschool group teachers assisted the nutrition expert during sessions, to enable them to sustain intervention‐related activities after the study. Partnerships Families Education: 5 of the 15 sessions actively involved parents by targeting them alone (discussions on parents’ modelling role and nutritional needs of children) or together with their children. Healthcare Delivery: external experts delivered nutrition sessions. Intensity of intervention: external nutrition experts were trained to deliver the intervention in intensive 4‐d training sessions. The experts delivered 15 standardised 2‐h nutrition sessions (during preschool hours), conducted once weekly over a 6‐month period, with 5 of these sessions actively involving parents (alone and with their children). Intervention delivered by: research team, healthcare staff Modality: face‐to‐face Theoretical basis: The Theory of Social Learning and Zajonc’s Exposure Effect Description of control: wait‐list control |
|
| Outcomes |
Outcomes relating to child dietary intake: Fruit intake, vegetable intake, water intake, sugared drink intake Number of participants analysed: not reported Data collection measure: parent survey Data collector: parent Validity of measures used: not reported Outcomes relating to child physical measures: BMI, waist circumference, skinfold sum Number of participants analysed: not reported Data collection measure: objectively measured Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: the study was funded by a grant from the Baden‐Württemberg Stiftung. Authors were funded by European Social Fund and by the Ministry of Science, Research and the Arts Baden‐Württemberg. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | Assignment of preschools was blinded through the use of sequentially numbered, sealed envelopes. However, there is no mention as to whether envelopes were opaque. |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | Teachers and children were not blind to study allocation, and the outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | Teachers and children were not blind to study allocation, however the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Parents completed the eating behaviour questionnaire. Blinding of parents not reported, and the outcome measurement is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Children's height, weight, waist circumference, and skinfold thickness were measured by study personnel who were blinded to group assignment. |
| Incomplete outcome data (attrition bias) Diet outcomes | High risk | There was substantial dropout, whereby only 58% of the children provided both pre‐ and post‐intervention measurements. It is unclear if the dropout is evenly distributed across arms, and no information is provided as to reasons for missing data/dropout. Due to the magnitude of missing data, the risk of bias was assessed as high. |
| Incomplete outcome data (attrition bias) Physical outcomes | High risk | There was substantial dropout, whereby only 58% of the children provided both pre‐ and post‐intervention measurements. It is unclear if the dropout is evenly distributed across arms, and no information is provided as to reasons for missing data/dropout. Due to the magnitude of missing data, the risk of bias was assessed as high. |
| Selective reporting (reporting bias) | High risk | Anthropometric outcomes of BMI, weight‐to‐height ratio, and skinfold sum are specified in the protocol and study methods, however are reported incompletely. Study authors stated that "We also found no significant intervention effect on BMI, waist‐to‐height ratio, or skinfold sum," though no data are provided. Further, secondary dietary outcomes of water intake and consumption of high‐energy drinks are specified in the protocol and study methods, however are reported incompletely. Study authors stated that "The intervention did not have significant effects on daily water intake or the consumption of high‐energy drinks (data not presented)." |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of centres. |
| Baseline imbalance | Unclear risk | Study authors state that "We stratified the recruited pre‐schools before randomisation to balance aggregate pre‐school social background and immigrant proportion." Analysis adjusted for confounding factors, including child's age, gender, SES, and immigrant background. However, no baseline data are provided to compare randomised groups. |
| Loss of clusters | High risk | One cluster lost |
| Incorrect analysis | Low risk | Study authors stated that “As our data stemmed from natural pre‐school‐bound clusters of children, we first determined the extent of clustering. Intraclass correlation coefficients (ICC) on the level of pre‐schools were 0.016 and 0.014 for the primary outcomes of fruit intake and vegetable intake, respectively. With an average cluster size of 19.5 children per pre‐school, the design effect (d = 1 + (average cluster size‐1) x ICC) did not exceed 2, allowing us to ignore the issue of clustering in our analyses." |
| Contamination | Unclear risk | No evidence to make assessment. |
| Other bias | Unclear risk | Study authors stated that "First, children were sampled from pre‐schools that applied for a nutritional intervention, possibly resulting in limited generalizability" and "Third, despite the calculation of a minimal sample size of 332, we only had 202 children providing both pre‐ and post‐intervention measurements. Our analysis thus may have been underpowered for detecting changes in anthropometric outcomes or water and sugar‐sweetened drinks consumption." There is insufficient information to assess whether an important risk of bias exists. |
De Coen 2012.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 2 years Unit of allocation: communities (a local authority ‐ town or municipality) Unit of analysis: child |
|
| Participants |
Service type: centre‐based (pre‐primary school) Operation: not reported Country (region): Belgium (Flanders) Country income classification: high Low‐SES sample: no Population description: the 6 communities were selected from the research regions in Flanders, Belgium disposed by the Flemish Policy Research Centre for Welfare, Health and Family, which commissioned the research project. The selection of these 6 communities out of the research regions was based on 5 socioeconomic characteristics: (i) the number of births in underprivileged families; (ii) the proportion of pupils in primary school with a school delay; (iii) the rate of unemployment; (iv) the number of people on welfare support; and (v) the number of underprivileged foreigners. High scores on these parameters are indicators of a lower socioeconomic profile. Inclusion criteria: the selection of these 6 communities out of the research regions was based on 5 socioeconomic characteristics: (i) the number of births in underprivileged families; (ii) the proportion of pupils in primary school with a school delay; (iii) the rate of unemployment; (iv) the number of people on welfare support; and (v) the number of underprivileged foreigners. High scores on these parameters are indicators of a lower SES profile. If a community scored higher than the Flemish mean on 3‐5 of the abovementioned characteristics, it was labelled as ‘low SES’; communities with 1 or 2 scores higher than the Flemish mean were labelled as ‘medium SES’; and communities with no scores higher than the mean were labelled as ‘high SES’. 2 communities had a high, 2 had a medium and 2 had a low‐SES profile. Exclusion criteria: not reported Number of services randomised: 6 communities (18/32 schools participated in intervention, 13/17 schools participated in control) Number of children randomised: 1589 participated Characteristics Children Age: 4.95 years (SD 1.31) Gender (% female): 50% Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported Method of recruitment: recruitment of the participants took place in pre‐primary and primary schools. Missing data/dropout: 46% dropout: 586 children dropped out for the questionnaire; 178 BMI values could not be attained at follow‐up Reasons for dropout: for BMI only: due to absence on the day of the measurement or change of school Characteristics of dropouts: the baseline BMI z‐scores were not significantly different between the communities. There were no other significant differences between intervention and control regions. Over the conditions, participants with a low SES dropped out significantly more at the follow‐up measurement (Chi2 = 10.03, P = 0.001). |
|
| Interventions |
Programme name: the POP (Prevention of Overweight among Pre‐school and school children) Number of conditions: 1 intervention, 1 control Intervention duration: 2 school years Intervention setting: ECEC and wider community Intervention strategies: Health curriculum Children Education: schools were requested to implement 5 x Healthy Weeks per intervention year (1 for each cluster of topics) with a minimum 1 h of classroom time dedicated to the topic together with extracurricular activities. Ethos and environment ECEC staff Resources: schools received guidelines and a manual describing the modules/objectives, tasks and responsibilities, including theory‐based methods and practical strategies. These 7 modules were: the organisation of the POP project at school level; the organisation of classroom activities (Healthy Weeks), including suggested dose and content; development of an active playground; implementation of health‐related physical education; environmental and policy changes to increase the availability of water at school (e.g. water fountains); environmental and policy changes to increase to availability of vegetables and fruits at school; and, educational strategies for parents on all topics. Meetings: 4 x meetings with the teachers. An implementation plan and problem solving was discussed. Financial support: teachers received EUR 250 to buy materials or finance environmental changes. Service Policy: schools were requested to evaluate and improve their playground and snack and beverage policy. Partnerships Families Resources: parents received a poster, 5 letters and a website link to resources, distributed by the school. Communication: schools were requested to communicate with the parents on the programme and distribute materials to the parents. Community Meetings: 2 x meetings were held in each intervention community with the researchers, community organisations and stakeholders regarding local social and health problems. Engagement: community organisations, members of the city council, aldermen and local non‐profit organisations working with children or health topics were approached to support the intervention at community level, to raise awareness and give greater publicity to the project. Resources: each intervention year, information brochures and posters regarding the 5 topics of the project were distributed through general practitioners, pharmacists, social services and at relevant community events by the regional health boards and the research team. Healthcare Support: regional health boards supported schools and communities to implement the project (making contact with services at least twice/year). Regional health boards received EUR 500. Intensity of intervention: 2 x community meetings to support the development of the intervention; yearly dissemination of information brochures and posters regarding the 5 intervention topics; 5 x Healthy Weeks per intervention year with a minimum of 1 h classroom time dedicated to the topic with extracurricular activities; 4 x teacher meetings; regional health boards contacted services at least twice yearly; parents received a poster, 5 letters and a website link. Intervention delivered by: research team, ECEC staff, healthcare staff Modality: face‐to‐face, telephone, online, written Theoretical basis: Socio‐Ecological Model in health promotion programmes Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: Fruit intake, vegetable intake, milk intake, water intake, soft drink intake, sweet or savoury snack intake Number of participants analysed: Intervention baseline: 1032 Intervention follow‐up: 396 Control baseline: 557 Control follow‐up: 398 Data collection measure: 24‐item semi‐quantitative FFQ Data collector: parent Validity of measures used: validated Outcomes relating to child physical measures: BMI z‐score Number of participants analysed Intervention baseline: 1032 Intervention follow‐up: 670 Control baseline: 557 Control follow‐up: 442 Data collection measure: objectively measured (Flemish reference data using the LMS (curve‐L, mean‐M and coefficient of variation‐S) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: commissioned, financed and steered by the Ministry of the Flemish Community (Department of Economics, science and Innovation; Department of Welfare, Public Health and Family). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure was not described. |
| Allocation concealment (selection bias) | High risk | Study authors stated that “Schools were aware of the fact that they were in an intervention community or in a control community.” |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. The outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Parents completed the semi‐quantitative FFQ. Blinding of parents not reported, and the outcome measurement is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured by the research team and are not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | High risk | Data were available for 694 (54%) of sample at follow‐up. Study authors stated that "selective drop‐out may have influenced the outcomes. Although this was not particular for one condition, the low‐SES participants dropped out significantly more." Due to the magnitude of missing data, the risk of bias was assessed as high. |
| Incomplete outcome data (attrition bias) Physical outcomes | High risk | Data were available for 1112 (70%) of sample at follow‐up, and a higher percentage of the intervention group was lost to follow‐up compared to the control group (35% vs 21%). Of the 477 dropouts, 178 (37%) were due to absence on the day of the measurement or change of school. Study authors stated that "selective drop‐out may have influenced the outcomes. Although this was not particular for one condition, the low‐SES participants dropped out significantly more." Due to the magnitude of missing data and difference in the proportions of participants followed up between groups, the risk of bias was assessed as high. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting. |
| Recruitment bias | High risk | Individuals and schools were recruited after randomisation of clusters. |
| Baseline imbalance | Low risk | The baseline BMI z‐scores were not significantly different between the communities. There were no other significant differences between intervention and control regions. |
| Loss of clusters | Low risk | No apparent loss of clusters |
| Incorrect analysis | Low risk | Study authors stated that “Children were clustered in thirty‐one schools (nesting variable).” and "the community was entered as a possible moderating factor by investigating the interaction between condition and community." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Unclear risk | Study authors stated that "In some schools, parents experiencing language or other problems filling in the questionnaire were assisted by an intercultural worker or interpreter." However, it is not mentioned that the parental intervention itself was offered in multiple languages, introducing possible bias, especially if language barriers were higher in one group versus another. There is insufficient information to assess whether an important risk of bias exists. |
Eliakim 2007.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 14 weeks Unit of allocation: preschool class Unit of analysis: child |
|
| Participants |
Service type: centre‐based (preschool) Operation: not reported Country (region): Israel (Oranit) Country income classification: high Low‐SES sample: no Population description: an upper‐middle SES community Inclusion criteria: the study included all 4 preschool classes in the community of Oranit, Israel. Children were included after their parents signed an informed consent form. Exclusion criteria: not reported Number of services randomised: 4 (2 interventions, 2 control) Number of children randomised: 118 Characteristics Children Age: Intervention: 66 months (SD 0.6) Control: 67 months (SD 0.7) Gender (% female): Intervention: 39% Control: 47% Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported Method of recruitment: not reported Missing data/dropout: no dropout during the intervention period Reasons for dropout: not applicable Characteristics of dropouts: not applicable |
|
| Interventions |
Programme name: not reported Number of conditions: 1 intervention, 1 control Intervention duration: 14 weeks (4 months) Intervention setting: ECEC Intervention strategies: Health curriculum Children Education: integrating nutritional topics, such as basic knowledge about major food groups and the food pyramid, vitamins, food choices, food preparation and cooking methods, fast food vs home cooking, and drinking and eating habits into the current curriculum. Topics were taught through short lectures/talks, games and book reading. Children were encouraged to reduce sedentary activities and increase after‐school activity. Ethos and environment Children Exposure: children participated in 45 min/d exercise training (6 d/week), primarily in the form of games. Resources: children received dietary information using work sheets/flyers. ECEC staff Training: the intervention group preschool teachers were instructed so that all the nutritional aspects of the intervention and the majority of exercise classes were performed by the preschool staff. Partnerships Healthcare Delivery: twice a week, physical activity training was directed by a professional youth coach. Intensity of intervention: preschool teachers instructed so they could deliver the intervention; 2 x parent orientation lectures; nutrition education (intensity not reported); exercise training 45 min/d, 6 d/week Intervention delivered by: research team, ECEC staff, healthcare Modality: face‐to‐face, written Theoretical basis: not reported Description of control: usual care, plus parents were invited for 2 orientation lectures (childhood obesity and beneficial effects of exercise in children) during the first 2 months of the programme |
|
| Outcomes |
Outcomes relating to child dietary intake: not reported Outcomes relating to child physical measures: Weight, BMI, BMI percentile, body fat percentage, obese, overweight, overweight or obese Number of participants analysed: Intervention baseline: 54 Intervention follow‐up: 54 Control baseline: 47 Control follow‐up: 47 Data collection measure: objectively measured (CDC) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive: not reported Outcome relating to child social/emotional measures performance: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: Study authors state only, "No adverse events were reported" Number of participants analysed: not reported Data collection measure: not reported Data collector: not reported Validity of measures used: not reported |
|
| Notes | Funding source: grant from the Israel Heart Fund, and the Carlos Lindenfeld Memorial Fund of the Jewish Community of San Diego, USA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | Teachers appear to have been involved in intervention design and delivery so we assumed they were not blind to the study allocation. However the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height, weight, and skinfold thickness were measured by the same trained individual and were not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Study authors stated that “54 children from the intervention group and 47 children from the control group started the program. No dropouts occurred during the intervention period.” Therefore, risk of attrition bias was considered to be low. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting. |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Low risk | No significant differences in age, gender, body weight and height, BMI, BMI percentiles, body fat, and fitness were found between groups prior to intervention |
| Loss of clusters | Low risk | No loss of clusters |
| Incorrect analysis | High risk | Classes were randomised, however there was no accounting for clustering of children within classes. |
| Contamination | Unclear risk | All 4 preschool classes were from the same community, however there is not enough information provided to assess whether contamination exists. |
| Other bias | Unclear risk | No conflict of interest statement was reported. |
Fernandez‐Jimenez 2019.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 5 months Unit of allocation: school Unit of analysis: child |
|
| Participants |
Service type: centre‐based (Head Start) Operation: public Country (region): USA (Harlem, New York City) Country income classification: high Low‐SES sample: yes Population description: minority community (underserved, urban, multi‐ethnic). Harlem is predominantly a mix of immigrant Hispanic and African‐American populations. Inclusion criteria: the preschools must be located in Harlem, New York; public; have children between ages 3 and 5 years of age; provide meals for the children; and, must make available use of their applicable programme operation space. Preschools were also asked to commit to not to participate in any other major structured health intervention programme aside from the usual curriculum during the study. Exclusion criteria: not reported Number of services randomised: Number of children randomised: 585 (413 intervention, 172 control) Characteristics Children Age: 4.1 years (SD 0.6) Gender (% female): 51.10% Ethnicity: non‐Hispanic black: 37.4%; Hispanic/Latino: 53.9%; other/multiracial: 8.7% Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported Method of recruitment: not reported Missing data/dropout: approximately 20% of children were lost to follow‐up or had incomplete data. No school withdrew from the study. Reasons for dropout: mainly because preschoolers aged out and moved to other schools and/or residencies Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: the FAMILIA (Family‐Based Approach in a Minority Community Integrating Systems‐Biology for Promotion of Health) trial Number of conditions: 1 intervention, 1 control Intervention duration: 4 months Intervention setting: ECEC Intervention strategies: Health curriculum Children Education: 37 h of educational programme over 4 months Partnerships Families Education: invitations to informational and educational meetings, called FAMILIA days, and a minimum of 11 family health activities (12 h) that the teacher regularly provided to parents during the duration of the child educational intervention Resources: teachers regularly sent educational material with the students to work on with their families at home. Intensity of intervention: 37‐h educational programme for children over 4 months; 12 h of educational meetings for parents/caregivers Intervention delivered by: research team, ECEC staff Modality: face‐to‐face Theoretical basis: not reported Description of control: wait‐list control |
|
| Outcomes |
Outcomes relating to child dietary intake: not reported Outcomes relating to child physical measures: BMI z‐score Number of participants analysed: Intervention baseline: 304 Intervention follow‐up: 304 Control baseline: 144 Control follow‐up: 144 Data collection measure: objectively measured (CDC) Data collector: not reported Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: emotional comprehension score Number of participants analysed: Intervention baseline: 304 Intervention follow‐up: 304 Control baseline: 144 Control follow‐up: 144 Data collection measure: Test of Emotion Comprehension (TEC) questionnaire Data collector: not reported Validity of measures used: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: Study authors state only, "No adverse events were reported" Number of participants analysed: not reported Data collection measure: not reported Data collector: not reported Validity of measures used: not reported |
|
| Notes | Funding source: American Heart Association under grant No. 14SFRN20490315 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Social/emotional outcomes | Low risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured and were not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Social/emotional outcomes | Unclear risk | No information provided on whether the individuals conducting the Test of Emotion Comprehension were blind to group allocation. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Study authors stated that "After a median follow‐up of 5.4 months, ~20% of children were lost to follow‐up or had incomplete data; therefore, 448 children (304 in the intervention group and 144 in the control group) were included in the main analysis (complete‐case intention‐to‐treat analysis) of the primary outcome of the study." Similar reasons for loss to follow‐up were noted between groups (i.e. unable to contact, unable to schedule, moved, withdrew consent). Study authors stated that "The primary analysis was supplemented by sensitivity analyses conducted using multiple imputation procedures, which explored different assumptions for the distribution of the missing data. Similar results were obtained across these sensitivity analyses. Therefore, we might reasonably assume that the missing data did not significantly affect the validity of our findings." Therefore, risk of attrition bias was considered to be low. |
| Incomplete outcome data (attrition bias) Social/emotional outcomes | Low risk | Study authors stated that "After a median follow‐up of 5.4 months, ~20% of children were lost to follow‐up or had incomplete data; therefore, 448 children (304 in the intervention group and 144 in the control group) were included in the main analysis (complete‐case intention‐to‐treat analysis) of the primary outcome of the study." Similar reasons for loss to follow‐up were noted between groups (i.e. unable to contact, unable to schedule, moved, withdrew consent). Study authors stated that "The primary analysis was supplemented by sensitivity analyses conducted using multiple imputation procedures, which explored different assumptions for the distribution of the missing data. Similar results were obtained across these sensitivity analyses. Therefore, we might reasonably assume that the missing data did not significantly affect the validity of our findings." Therefore, risk of attrition bias was considered to be low. |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the paper were pre‐specified in the protocol paper. |
| Recruitment bias | High risk | Individual recruitment occurred after randomisation of clusters. |
| Baseline imbalance | Low risk | No significant differences were found between groups at baseline, except that there was a greater proportion of Hispanic/Latino compared with non‐Hispanic Black children in the intervention group as compared with the control group. Study authors state that "Interaction models were also fitted to identify possible baseline score‐, age‐, sex‐, race/ ethnicity‐, and socioeconomic‐by‐treatment effects for the main outcome variable." |
| Loss of clusters | Low risk | No loss of clusters |
| Incorrect analysis | Low risk | Study authors stated that “Multilevel linear mixed‐effects models that account for the hierarchical cluster randomized design were used to test for the adjusted intervention effect.” |
| Contamination | Unclear risk | All schools were from the same community, however there is not enough information provided to assess whether contamination exists. |
| Other bias | Unclear risk | Protocol states that school recruitment would occur in a 2:1 ratio (intervention: control), however the study states that recruitment occurred in a 3:2 ratio. No explanation provided for deviation from protocol. There is insufficient information to assess whether an important risk of bias exists. |
Fitzgibbon 2005.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 14 weeks Unit of allocation: school Unit of analysis: child |
|
| Participants |
Service type: centre‐based (Head Start) Operation: not reported Country (region): USA (Chicago) Country income classification: high Low‐SES sample: yes Population description: primarily black Inclusion criteria: all children at the sites were eligible to participate. Exclusion criteria: not reported Number of services randomised: 12 (6 intervention, 6 control) Number of children randomised: 409 (197 intervention, 212 control) Characteristics Children Age: Intervention: 48.6 months (SD 7.6) Control: 50.8 months (SD 6.4) Gender (% female): Intervention: 49.7% Control: 50.5% Ethnicity: Intervention: black: 99%; Latino: 0%; multiracial/other: 1% Control: black: 80.7%; Latino: 12.7%; multiracial/other: 6.6% Parents Parent/caregiver age (years): Intervention: 30.0 (SD 9.7) Control: 30.8 (SD 9.5) Parents gender (% female): 100% Parent/Caregiver Ethnicity: not reported Parent/family SES: Female parent years of education Intervention: 12.4 (SD 1.8) Control: 12.7 (SD 1.7) Method of recruitment: not reported Missing data/dropout: 89% retention for BMI and 78% for dietary outcomes Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Hip‐Hop to Health Jr Number of conditions: 1 intervention, 1 control Intervention duration: 14 weeks Intervention setting: ECEC and home Intervention strategies: Health curriculum Children Education: healthy eating and exercise intervention covered health topics. Sessions included a 20‐min lesson that introduced a healthy eating or exercise concept with an activity. The lessons and activities often involved colourful, friendly, handheld puppets that represent the 7 foods of the food pyramid. Ethos and environment Children Exposure: sessions also incorporated 20 min of teacher‐led, ongoing physical activity with a 5‐min warm‐up, 10 min of aerobic activity, and a 5‐min cool‐down. Partnerships Families Resources: parents received weekly newsletters with information that mirrored the children's curriculum and included a homework assignment to reinforce concepts. Incentive: parents received USD 5 grocery store coupon for each homework assignment completed. Intensity of intervention: 40‐min lessons, 3 times a week for children for 14 weeks; weekly newsletters and weekly homework assignment (approximately 15 min activity) for parents Intervention delivered by: ECEC staff Modality: face‐to‐face, written Theoretical basis: Social Learning theory, Self‐Determination Theory and the Transtheoretical Model that incorporates stages of change Description of control: alternative intervention control (covered general health concepts such as dental health, immunization, seat belt safety, and 911 procedures). |
|
| Outcomes |
Outcomes relating to child dietary intake: Total fat intake, saturated fatty acids, dietary fibre Number of participants analysed: Intervention baseline: 175 Intervention follow‐up: 133 Control baseline: 183 Control follow‐up: 147 Data collection measure: partial or full recall by parent Data collector: researcher (parents provided information to researcher) Validity of measures used: not reported Outcomes relating to child physical measures: BMI, BMI z‐score, weight Number of participants analysed: Intervention baseline: 197 Intervention follow‐up: 179 Control baseline: 212 Control follow‐up: 183 Data collection measure: objectively measured (CDC) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: Study authors state only, "No adverse events were reported for any participants" Number of participants analysed: not reported Data collection measure: not reported Data collector: not reported Validity of measures used: not reported |
|
| Notes | Funding source: supported by a grant from the National Heart, Lung, and Blood Institute (Grant HL58871). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported. |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. The outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | Low risk | Dietary intake data were obtained from the parent by a trained and certified registered dietitian who was blinded to treatment group. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured and were not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | High risk | Data were available for 133 (68%) participants in the intervention group and 147 (69%) students in the control group at post‐intervention. Due to the magnitude of missing data at follow‐up, the risk of bias was assessed as high. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Data were available for 179 (96%) participants in the intervention group and 183 (86%) students in the control group at post‐intervention. Due to the relatively small (< 20%) proportion of missing data across both groups, risk of attrition bias was considered to be low. |
| Selective reporting (reporting bias) | Unclear risk | Only 24‐h recall results were published in study, yet prior publication mentions diet observation and FFQ, as well. |
| Recruitment bias | Unclear risk | It is unclear whether allocation occurred before or after baseline data collection. |
| Baseline imbalance | Unclear risk | Groups were comparable at baseline for all but age, race, exercise frequency, height, and weight, though height and weight differences were no longer significant when adjusted for age. |
| Loss of clusters | Low risk | No apparent loss of clusters |
| Incorrect analysis | Low risk | Dietary measures, BMI and BMI z‐score are adjusted for Head Start site |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Unclear risk | No conflict of interest statement was reported. |
Fitzgibbon 2006.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 14 weeks Unit of allocation: school Unit of analysis: child |
|
| Participants |
Service type: centre‐based (Head Start) Operation: not reported Country (region): USA (Chicago) Country income classification: high Low‐SES sample: yes Population description: predominantly Latino centres Inclusion criteria: all children were eligible to participate in the intervention. Exclusion criteria: not reported Number of services randomised: 12 (6 intervention, 6 control) Number of children randomised: 401 (202 intervention, 199 control) Characteristics Children Age: Intervention: 50.8 months (SD 7.3) Control: 51.0 months (SD 7.0) Gender (% female): Intervention: 47.5% Control: 51.3% Ethnicity: Intervention: black: 15.8%; Latino: 73.3%; multiracial/other: 10.9% Control: black: 6.5%; Latino: 89.4%; multiracial/other: 4% Parents Age (years): Intervention: 31.5 (SD 8.6) Control: 30.7 (SD 7.2) Gender (% female): 100% Ethnicity: not reported Parent/family SES: Female parent years of education Intervention: 11.3 (SD 3.6) Control: 10.6 (SD 3.7) Method of recruitment: not reported Missing data/dropout: retention rate at post‐intervention was 97% Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Hip‐Hop to Health Jr Number of conditions: 1 intervention, 1 control Intervention duration: 14 weeks Intervention setting: ECEC and home Intervention strategies: Health curriculum Children Education: a diet/physical activity curriculum delivered by trained ECEC educators 3 x/week. Each session included 20 min of nutrition activity based on hand puppets that reflected the food pyramid. Ethos and environment Children Exposure: 20 min of aerobic activity led by trained ECEC educators 3 x/week All participants Cultural: the programme was culturally proficient, tailored to a Latinx population and delivered in both Spanish and English. Partnerships Families Resources: parents received weekly newsletters and accompanying homework assignments designed to be an interactive activity between parents and children. Incentive: a small monetary incentive was provided for completed homework. Intensity of intervention: 40‐min lessons, 3 times/week for children for 14 weeks; 12 x weekly newsletters, weekly homework assignments for parents Intervention delivered by: ECEC staff Modality: face‐to‐face, written Theoretical basis: Social Cognitive Theory and Self‐Determination Theory Description of control: alternative intervention control (covered general health concepts such as seat belt safety, immunisation, and dental health) |
|
| Outcomes |
Outcomes relating to child dietary intake: Total fat, saturated fatty acids, fibre Number of participants analysed: Intervention baseline: 188 Intervention follow‐up: 178 Control baseline: 174 Control follow‐up: 156 Data collection measure: partial or full recall by parent Data collector: researcher (parent provided information to researcher) Validity of measures used: not reported Outcomes relating to child physical measures: Weight, BMI, BMI z‐score Number of participants analysed: Intervention baseline: 202 Intervention follow‐up: 196 Control baseline: 199 Control follow‐up: 187 Data collection measure: objectively measured (CDC) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: Study authors state only, "No adverse events reported during the trial for any participants" Number of participants analysed: not reported Data collection measure: not reported Data collector: not reported Validity of measures used: not reported |
|
| Notes | Funding source: National Heart, Lung, and Blood Institute (Grant HL 58871) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. The outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Parents reported children's dietary intake. Blinding of parents not reported, and the outcome measurement is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured and were not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | High risk | Data were available for 178 (88%) participants in the intervention group and 156 (78%) students in the control group at post‐intervention. Due to the magnitude of missing data and difference in the proportions of participants followed up between groups, the risk of bias was assessed as high. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Data were available for 196 (97%) participants in the intervention group and 187 (94%) students in the control group at post‐intervention. There were no significant differences in retention rates between intervention and control groups. Study authors stated that “The primary analytic approach was ITT, with all participants completing follow‐ups included in the condition to which they were assigned.” Therefore, risk of attrition bias was considered to be low. |
| Selective reporting (reporting bias) | Unclear risk | Only 24‐h recall results were published in the study, yet prior publication mentions diet observation and FFQ |
| Recruitment bias | Unclear risk | Baseline data collection occurred after randomisation of schools, however it is unclear whether individual recruitment occurred before or after randomisation. |
| Baseline imbalance | High risk | Study authors report baseline imbalance that is not accounted for in the analysis |
| Loss of clusters | Low risk | No apparent loss of clusters |
| Incorrect analysis | Low risk | Study authors stated that "Proc Mixed was used, with the individual school as the unit of randomization, yielding a test statistic with 10 df for 12 schools." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Fitzgibbon 2011.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 14 weeks (varies with outcomes) Unit of allocation: school Unit of analysis: child |
|
| Participants |
Service type: centre‐based (Head Start) Operation: public Country (region): USA (Chicago) Country income classification: high Low‐SES sample: yes Population description: not reported Inclusion criteria: up to 2 children/family were eligible to participate. Exclusion criteria: not reported (exclusions appear to occur after baseline) Number of services randomised: 18 (9 intervention, 9 control) Number of children randomised: 729 (376 intervention, 353 control) Characteristics Children Age: 51.3 months (SD 6.6) Gender (% female): 53% Ethnicity: black: 94%; Latino: 3%; multiracial/other: 3% Parents Age (years): 30.9 (SD 8.6) Gender (% female): 90% Ethnicity: not reported Parent/family SES: Income, USD, median: 15,000 Education, years: 12.3 (SD 1.7) Method of recruitment: not reported Missing data/dropout: baseline data were collected for the 669 children (92%) however, 50 of these children were excluded. Reasons for dropout: transferred out of the participating schools before the intervention began, and 1 child was excluded because he was the 3rd child in a participating family. Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: teacher‐delivered Hip‐Hop to Health Jr Number of conditions: 1 intervention, 1 control Intervention duration: 14 weeks Intervention setting: ECEC and home Intervention strategies: Health curriculum Children Education: teachers taught 2 sessions/week, with the option of including a 3rd session. Each week focused on a theme with a specific objective. Each session included a 20‐min lesson related to healthy eating and exercise. Lessons featured colourful "pyramid puppets" to represent the 7 food groups of the food pyramid. Intervention incorporated songs and raps on a CD. Ethos and environment Children Exposure: each session also incorporated 20 min of physical activity. Intervention CD included 2 fully scripted exercise routines. ECEC staff Training: teachers attended training sessions. Following the first formal session, the intervention co‐ordinator conducted 3 in‐school training sessions and met with teachers on an individual basis weekly. All participants Cultural: cultural considerations for black children were incorporated in the intervention. Partnerships Families Resources: parents received weekly newsletters that paralleled the children's curriculum in content and included a homework assignment. Parents also received the CD to reinforce nutrition and physical activity concepts at home. Incentive: parent received USD 5 for each homework assignment completed and returned. Intensity of intervention: 1 x 3 h initial staff training, plus 3 x in‐school staff training sessions; intervention co‐ordinator met with teachers weekly to support intervention delivery; 40‐min lessons, 2 sessions/week (teacher could opt for 3rd); weekly parent newsletters that included homework Intervention delivered by: research team, ECEC staff Modality: face‐to‐face, written Theoretical basis: Social Cognitive Theory and Self Determination Theory Description of control: alternative intervention control (covered health concepts including care seats, seat belt safety, immunisation, dental health and calling 911) |
|
| Outcomes |
Outcomes relating to child dietary intake: Energy, total fat, fibre, fruit, 100% fruit juice, vegetables, diet quality (total, total fruit, whole fruit, saturated fat, whole grains, total vegetables, solid fats and added sugars) Number of participants analysed: Intervention baseline: 278 Intervention follow‐up: 196‐238 Control baseline: 230 Control follow‐up: 160‐202 Data collection measure: 24‐h diet record (combination of in‐school observations and food records or recalls completed by parent) Data collector: parent and researcher Validity of measures used: not reported Outcomes relating to child physical measures: BMI, BMI z‐score, weight Number of participants analysed: Intervention baseline: 325 Intervention follow‐up: 309 Control baseline: 293 Control follow‐up: 280 Data collection measure: objectively measured (CDC) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: supported by the National Heart, Lung and Blood Institute (HL081645) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure was unclear. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported. |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | Due to the nature of the study design, both parents and interviewers were aware of group assignments. The outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | Due to the nature of the study design, both parents and interviewers were aware of group assignments. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Dietary intake was reported by parents and observed by research staff. There was no blinding of outcome assessors, and the outcome measurement is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Children's height and weight were measured by interviewers aware of group assignments, however the outcome measurements are not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Low risk | Only 86% of intervention and 79% of control had baseline diet data, and follow‐up loss was 14% of intervention children with baseline diet data (27% loss from all children in intervention group) and 12% of control children with baseline diet data (31% loss from all children in control group). Study authors stated that "The proportion of children with valid records differed by school (highest = 94%, lowest = 55%, p< 0.001) but not by intervention group (P = 0.24). The 440 children who had valid diet records at both visits did not differ significantly from the other 178 children in gender, race, age, BMI, BMI z‐score, weight or height. There was also no significant difference in parents' gender, age, education, median income, marital status, full‐time employment, BMI, height, or weight." Study authors stated that "Only children with valid data for the relevant variables at baseline and postintervention were included in analyses (BMI change, physical activity, screen time, and diet)." Therefore, risk of attrition bias was considered low. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | All children enrolled in the study (minus those who were excluded prior to intervention) were measured at baseline. Follow‐up data were available for 309 (95%) children in the intervention group and 280 (96%) children in the control group. No information regarding missing data provided. Study authors stated that "Only children with valid data for the relevant variables at baseline and postintervention were included in analyses (BMI change, physical activity, screen time, and diet)." Therefore, risk of attrition bias was considered low. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting. |
| Recruitment bias | Unclear risk | Recruitment of preschools occurred before randomisation, however it is not clear whether recruitment of children came before or after randomisation of preschools. |
| Baseline imbalance | High risk | Groups differed at baseline by total screen time/d, energy intake, and fibre intake, however the model only adjusted for baseline BMI and BMI z‐score, age, preschool, and classroom. |
| Loss of clusters | Unclear risk | One cluster did not have diet observation data because school personnel felt the in‐school diet observations would be disruptive. It is unclear whether other clusters were lost due to insufficient reporting. |
| Incorrect analysis | Low risk | Study authors stated that "To test for differences between groups in BMI and BMI Z score change at postintervention, we used both mixed‐model analysis of variance, controlling for school and classroom nested within school, and mixed model analysis of covariance, controlling for school, classroom nested within school, the baseline value, and baseline age." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Fitzgibbon 2013.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 14 weeks Unit of allocation: preschool Unit of analysis: child |
|
| Participants |
Service type: centre‐based (Head Start) Operation: public Country (region): USA (Chicago) Country income classification: high Low‐SES sample: yes Population description: Hispanic children and their parents Inclusion criteria: a parent‐child dyad was eligible if the parent gave informed consent for herself and the child, the child's height and weight were measured at baseline, and the child was still enrolled in a participating classroom when the intervention began. Up to 2 children per family were eligible to participate. Exclusion criteria: not reported Number of services randomised: 4 (2 interventions, 2 control) Number of children randomised: 157 (78 intervention, 79 control) Characteristics Children Age: 54.2 months (SD 5.0) Gender (% female): 50% Ethnicity: Latino: 94%; black: 2%; multiracial/other: 4% Parents Age (years): 32.8 (SD 6.0) Gender (% female): 89% Ethnicity: unclear Parent/family SES: Income (USD median: 15,000 Parent education (years): 11.2 (SD 2.2) Method of recruitment: not reported Missing data/dropout: all clusters retained, however 1 intervention and 2 control participants were missing from follow‐up. Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Family‐Based Hip‐Hop to Health Number of conditions: 1 intervention, 1 control Intervention duration: 14 weeks Intervention setting: ECEC and home Intervention strategies: Health curriculum Children Education: a nutrition and physical activity curriculum (3 x/week) was provided to children, led by bilingual/bicultural educator and supplemented by a Spanish language CD. The nutrition instructions included activities led by puppets representing food groups. The nutrition and physical activity components designed to target specific child behaviours (e.g. increase consumption of fruits and vegetables, reduce television viewing, and increase duration of daily physical activity). Ethos and Environment Children Exposure: each session also included 20 min of aerobic activity. All participants Cultural: the intervention was tailored to cultural and developmental needs of the population (lower‐income, Hispanic populations). Partnerships Parents Education: parents encouraged to attend 6 weekly 90‐min classes that included 60 min of interactive curriculum (healthy eating and exercise for weight management), supplemented with the Spanish language CD. Exposure: the remaining 30 min involved moderate physical activity (e.g. salsa aerobics, walking group). Resources: parents received weekly newsletters with programme information. Each family received a copy of the Spanish language CD to reinforce the classroom material at home. Intensity of intervention: 40‐min nutrition education sessions/week for children; 6 x 90‐min education sessions for parents; weekly newsletters for parents Intervention delivered by: ECEC staff Modality: face‐to‐face, written Theoretical basis: Social Cognitive Theory, the Health Belief Model and Self‐Determination Theory Description of control: alternative intervention control (covered health concepts including seat belt safety, immunisation, dental health and calling 911) |
|
| Outcomes |
Outcomes relating to child dietary intake: Energy, total fat, fibre, fruit, 100% fruit juice, vegetables Number of participants analysed: Intervention baseline: 55 Intervention follow‐up: 50 Control baseline: 58 Control follow‐up: 56 Data collection measure: 24‐h diet record (combination of in‐care observations and parent records for all foods consumed outside of care) Data collector: parent‐reported and researcher observations Validity of measures used: not reported Outcomes relating to child physical measures: BMI, BMI z‐score, weight Number of participants analysed: Intervention baseline: 72 Intervention follow‐up: 71 Control baseline: 74 Control follow‐up: 72 Data collection measure: objectively measured (CDC) Data collector: not reported Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: National Cancer Institute (CA121423), R25CA057699, and the Consortium to Lower Obesity in Chicago Children (CLOCC) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. The outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Dietary intake was reported by parents and observed by research staff. There was no blinding of outcome assessors, and the outcome measurement is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Children's height and weight were measured by interviewers aware of group assignments, however the outcome measurements are not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | High risk | Only 76% of intervention and 78% of control had baseline diet data, and follow‐up loss was 9% of intervention children with baseline diet data (31% loss from all children in intervention group) and 3% of control children with baseline diet data (24% loss from all children in control group). Study authors stated that "Only participants with height and weight measurements, valid accelerometer records, complete screen time data, or valid diet data at baseline and follow‐up were included in the relevant follow‐up analyses." No information provided regarding reasons for missing data at follow‐up. Due to the magnitude of missing data, the risk of bias was assessed as high. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Data were available for 71 (99%) participants in the intervention group and 72 (97%) students in the control group at post‐intervention. Study authors stated that "Only participants with height and weight measurements, valid accelerometer records, complete screen time data, or valid diet data at baseline and follow‐up were included in the relevant follow‐up analyses." Reason for missing data was similar across groups (i.e. missed visit). Therefore, risk of attrition bias was considered to be low. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting |
| Recruitment bias | Unclear risk | Per the PRISMA diagram, individual recruitment occurred after randomisation of preschools. However, it is unclear if parents were aware of allocation at recruitment. |
| Baseline imbalance | Unclear risk | Baseline analysis was conducted but results were not provided. |
| Loss of clusters | Low risk | No loss of clusters |
| Incorrect analysis | Low risk | Study authors stated that "We used a mixed model analysis of covariance to test for differences between groups in physical activity at post‐intervention and in screen time and diet at post‐intervention and follow‐up, controlling for school, classroom nested within school, and the baseline value." and "To test for differences between groups in BMI and BMI z‐score change at post‐intervention and 1‐year follow‐up, we used a mixed model ANOVA, controlling for school and classroom nested within school, as well as a mixed model analysis of covariance, controlling for school, classroom nested within school, the BMI percentile at baseline (< 85th or > 85th), baseline age, and time between visits." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Gans 2022.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 8 months Unit of allocation: family child‐care homes (i.e. family day care) Unit of analysis: child |
|
| Participants |
Service type: family child‐care homes Operation: not reported Country (region): USA (Rhode Island and Massachusetts) Country income classification: high Low‐SES sample: yes Population description: Rhode Island (RI) is a state where approximately 16% of the population identifies as Hispanic or Latinx, at least 40% of family child‐care providers are Spanish speaking. Inclusion criteria: family child‐care providers had to meet the following criteria: have a family day care within 60 miles of Providence, Rhode Island in operation for at least 6 months; be able to read and speak Spanish or English; have a working phone; care for at least 1 unrelated 2–5 year‐old child for 10 h or more/week who ate at least 1 meal and snack/d at the family child‐care home and, family child‐care providers could not plan to close their service for > 3 consecutive weeks during the year following their enrolment in the study. Exclusion criteria: not reported Number of services randomised: unclear Number of children randomised: 119 (60 intervention, 59 control) Characteristics Children Age: 41.7 months (SD 12.0) Gender (% female): 50% Ethnicity: Ethnicity: Latinx: 55%, non‐Latinx: 43, missing: 2% Race: white: 46%, black: 10%, Asian: 1%, American Indian: 1%, Native Hawaiian: 1%, other/> 1 race: 39%, missing: 3% Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported ECEC staff Age (years): 48.86 (SD 8.96) Gender (% female): 100% Ethnicity: Ethnicity: Hispanic: 67.2%; non‐Hispanic: 32.8% Race: white: 2.6%; NA/NA/NP/PI (not defined): 19%; mixed race: 24.1%; declined or missing: 54.3% Service/ECEC staff SES: household income < USD 25,000: 12.6%; USD 25,001‐USD 50,000: 47.9%, USD 50,001‐USD 75,000: 20.2%; USD 75,001‐USD 100,000: 10.1%; ≥ USD 100,001: 5.9%; missing: 3.4% Method of recruitment: recruitment, enrolment and baseline assessment was conducted on a rolling basis from 2015‐2018. A variety of recruitment strategies were used including: (1) information sessions at community organisations that provide training and support for family child‐care providers. These organisations also offered recruitment flyers and brochures to family child‐care providers; (2) meetings with the co‐ordinators of family child‐care provider systems who then emailed study information to family child‐care providers in their systems; (3) presentations at local family child‐care providers' conferences; (4) direct mailings followed by staff phone calls to licensed family child‐care providers whose contact information was publicly available through state databases in Rhode Island, and Massachusetts; and (5) word of mouth referrals from family child‐care providers already participating in the study. Missing data/dropout: 168 family child‐care providers completed the baseline survey, 126 completed the in‐person survey/baseline visit and consented to enrol, and 120 completed the 2‐d baseline observations. Of those, 1 family child‐care provider withdrew after baseline measurement but before randomisation. A total of 423 parents of eligible children consented for their children to be observed and/or measured; 377 of those children had at least 1 measurement; 370 children had their meals observed; 349 had accelerometer measurement, and 327 had anthropometric measurements. Reasons for dropout: reasons for dropout included: did not have kids 2‐5 in home to observe at follow‐up, did not want home observation, withdrew from study and loss of contact. Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Healthy Start‑Comienzos Sanos Number of conditions: 1 intervention, 1 control Intervention duration: 8 months Intervention setting: family child‐care home Intervention strategies: Ethos and environment ECEC staff Resources: monthly materials (a report, newsletters and videos (via DVD or emailed video link) in English or Spanish) tailored to the topic chosen by the family child‐care provider Feedback and support: monthly support from a support coach trained in brief motivational interviewing. First, the coach reviewed with the family child‐care provider in person, an individually tailored written feedback report that indicated whether the provider met or did not meet best practices for nutrition, physical activity and screen‐time topics (based on baseline data). Motivational interviewing: the coach then conducted brief motivational interview with the family child‐care provider. At the end of the session, the family child‐care provider selected 1 topic to work on. Monthly calls using motivational interviewing were completed following this. Meetings: in‐person group meetings led by the support coach were also held every 6 weeks in a central public location (e.g. library or church). All participating family child‐care providers were invited to attend these meetings to support one another, discuss challenges and successes, learn a new activity, and share a meal. Service Resources: a set of active toys (e.g. hula hoops, tunnel, bean bags, soft balls) with accompanying activity cards and video clips with ideas for using the toys. Partnerships External provider Delivery: a support coach delivered the intervention. Intensity of intervention: 8 x monthly staff meetings; 8 x monthly staff resources; staff group meetings every 6 weeks Intervention delivered by: healthcare staff Modality: face‐to‐face, telephone, online, written Theoretical basis: Social ecological framework, Social Cognitive Theory, Self Determination Theory Description of control: alternative intervention (covered reading readiness and early literacy skills) |
|
| Outcomes |
Outcomes relating to child dietary intake: Diet quality (total fruit, whole fruit, total vegetable, greens and beans, whole grains, total dairy, total protein, seafood and plant protein, fatty acids, refined grains, sodium, added sugar, saturated fats) Number of participants analysed: Intervention baseline: 187 Intervention follow‐up: 187 Control baseline: 190 Control follow‐up: 190 Data collection measure: Dietary Observation in Child Care Data collector: researchers Validity of measures used: validated Outcomes relating to child physical measures: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: this project was funded by the National Heart Lung and Blood Institute, Grant # NIH ‐ R01HL123016. The funding body had no role in the design of the study and collection, analysis, and interpretation of data nor in writing the manuscript. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Study authors state that services were "randomized into either the intervention or comparison group in matched pairs based on primary language spoken and number of age eligible children in their family childcare homes using a Microsoft Excel randomization function." |
| Allocation concealment (selection bias) | Low risk | Study authors state "Once family childcare home providers completed all baseline measures, they were randomized into either the intervention or comparison group in matched pairs". |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | Study authors state that "Because the days of observation were announced, it is possible that family child care providers changed their behavior on the occasions of having observers in their home, although this would likely have affected both experimental groups." However, providers were informed of their study allocation by the project co‐ordinator. The outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | Low risk | Evaluation staff were not informed of the intervention group assignment. Study authors state that "we did not measure whether blinding of observers was successfully achieved. However, the field staff were not told the experimental group of family child care provider they observed. Toys that were provided did not have any project identifying information on them, so should not have unblinded experimental group status. In addition, the observers were trained not to have conversations with providers except to clarify information about recipes or ingredients." |
| Incomplete outcome data (attrition bias) Diet outcomes | Unclear risk | Data were available for 370/423 (87%) of children overall, 42/60 (70%) services in the intervention group, and 47/59 (80%) services in the control group. Study authors state that "Family child care providers and children who completed follow‐up were similar to those who were lost to follow‐up, suggesting that attrition did not overly bias the sample." Reasons for service dropout were provided, however it is unclear whether missing outcome data were related to the true outcome. |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the paper were prespecified in the protocol paper. |
| Recruitment bias | Low risk | Individual recruitment occurred prior to service randomisation |
| Baseline imbalance | Low risk | Baseline analysis was conducted and there were no significant differences between groups for age, sex, race, ethnicity, or other demographic variables for children or family child‐care provider. |
| Loss of clusters | Unclear risk | 30% of clusters were lost in the intervention group and 20% of clusters lost in the control group. Study authors state that "there was no differential dropout between experimental groups, therefore we did not include imputation of missing values in the analyses." It is unclear whether this loss of clusters introduced bias. |
| Incorrect analysis | Low risk | Study authors state that "Generalized Estimating Equations (GEE) with robust standard errors were used to model HEI [Healthy Eating Index] scores and physical activity over time. A working independence correlation structure was used to correct for dependency of observations within family child care providers." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Grummon 2019.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 12 weeks Unit of allocation: centre Unit of analysis: child |
|
| Participants |
Service type: centre‐based Operation: public (combination of full‐time and part‐time programmes) Country (region): USA (San Mateo County, California) Country income classification: high Low‐SES sample: yes Population description: primarily English‐ or Spanish‐speaking families and low income Inclusion criteria: centres were eligible if they were in San Mateo County, California; were licensed; had enrolled at least 10 children aged 2–5 years; had English‐ or Spanish‐speaking staff; served primarily English‐ or Spanish‐speaking families; and participated in the Child and Adult Care Food Program (a federal nutrition assistance programme providing funding for meals and snacks, and a marker for centres that serve lower‐income children). At each centre, all eligible children and their parents were invited to participate. Children were eligible if they were 2–5 years old. Their parents were eligible if they spoke English or Spanish. Exclusion criteria: not reported Number of services randomised: 4 (2 intervention, 2 control) Number of children randomised: 164 (87 intervention, 77 control) Characteristics Children Age: Intervention: 4.1 years (SD 0.59) Control: 4.32 years (SD 0.44) Gender (% female): 56% Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: Intervention: Hispanic ethnicity: 98% Control: Hispanic ethnicity: 82% Parent/family SES: Annual household income ≤ USD 30,000: Intervention: 67% Control: 67% Education of high school degree or less: Intervention: 66% Control: 54% Method of recruitment: not reported Missing data/dropout: of the 161 children measured at baseline, 7 (4%) were lost to follow‐up. Reasons for dropout: child no longer enrolled at child care Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: not reported Number of conditions: 1 intervention, 1 control Intervention duration: 12 weeks Intervention setting: ECEC and home Intervention strategies: Health curriculum Children Education: children participated in activities while at child care, including singing along to the ‘Drink More Water’ children’s song, and reading the children’s book Potter the Otter: A Tale About Water (facilitated by child‐care teachers or research assistants). Ethos and environment Children Exposure: providers served children water at meals and snacks. Children sampled water infused with fruit or herbs. Materials: children received a CD with the ‘Drink More Water’ song, a copy of the Potter the Otter book and stickers promoting water consumption. Service Environment: classrooms provided with child‐sized pitchers, cups and water bottles Policy: implementation of rules and policies. The study principal investigator met with centre directors and head teachers to explain the Healthy Beverages policy and asked that centres comply with standards. Centre directors incorporated rules about beverages into staff handbooks or policies using language provided by the research team. Partnerships Families Workshop: parents invited to attend in‐person training (study staff described how to determine the amount of added sugar in beverages) Resources: parents received written ‘behavioural contracts’ listing rules about beverages they might consider adopting. Educational activities: parents received personalised report cards with their child’s weight and beverage consumption, handouts (e.g. recipes for spa water) and interactive family activities (e.g. a worksheet for finding free water sources at the park). Community Engagement: community advisory board (representatives from county public health, local child‐care organisations, child‐care providers and parents) provided regular feedback. Intensity of intervention: frequency and duration of strategies were not reported Intervention delivered by: research team, ECEC staff Modality: face‐to‐face, written Theoretical basis: The Social Ecological Framework Description of control: wait‐list control |
|
| Outcomes |
Outcomes relating to child dietary intake: All less healthy beverage intake, all healthier beverage intake, 100% juice intake, total sugar‐sweetened beverage intake (excluding sweetened milk), unsweetened high‐fat milk (2% or whole) intake, sweetened milk intake, total water intake, tap water intake, bottled water intake, unsweetened low‐fat or non‐fat milk intake Number of participants analysed: Intervention baseline: 80 Intervention follow‐up: 80 Control baseline: 74 Control follow‐up: 74 Data collection measure: parent‐reported questionnaire Data collector: parent Validity of measures used: not reported Outcomes relating to child physical measures: BMI percentile, BMI, overweight or obese Number of participants analysed: Intervention baseline: 80 Intervention follow‐up: 80 Control baseline: 74 Control follow‐up: 74 Data collection measure: objectively measured (CDC) Data collector: trained research assistants Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: National Institutes of Health (grant number K23 HD067305 to A.I.P.). Carolina Population Center (grant numbers P2C HD050924 and T32 HD007168). Johns Hopkins Center for a Livable Future – Lerner Fellowship. Maternal and Child Health Bureau, Health Resources and Services Administration, US Department of Health and Human Services (grant numbers U45MC27709 and UA6MC27378) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. The outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Parents reported children's at‐home beverage consumption. Blinding of parents not reported, and the outcome measurement is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured by a trained research assistant and the outcome measurements are not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Low risk | Data were available for 80 (94%) children in the intervention group and 74 (97%) children in the control group. Reasons for loss to follow‐up similar between groups (i.e. child no longer enrolled at child‐care facility). Therefore, risk of attrition bias was considered to be low. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Data were available for 80 (94%) children in the intervention group and 74 (97%) children in the control group. Reasons for loss to follow‐up similar between groups (i.e. child no longer enrolled at child‐care facility). Therefore, risk of attrition bias was considered to be low. |
| Selective reporting (reporting bias) | Low risk | The reported outcomes aligned with those outlined in the trial registration. |
| Recruitment bias | High risk | Individual recruitment occurred after randomisation of clusters. |
| Baseline imbalance | Unclear risk | Study authors state that “Analytic models controlled for child’s age and sex and parent/household demographic characteristics," though differences in these variables were not reported. |
| Loss of clusters | Low risk | No apparent loss of clusters |
| Incorrect analysis | Low risk | Study authors stated that "To account for clustering, models clustered SE within children and included a set of indicator variables (i.e. fixed effects) for child‐care classrooms. Inclusion of classroom fixed effects also accommodated and corrected for any potential pair effects resulting from having conducted randomization within cities." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Hodgkinson 2019.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 6 months Unit of allocation: centre Unit of analysis: centre |
|
| Participants |
Service type: centre‐based (Sure Start Early Years) Operation: not reported Country (region): UK (Lancashire) Country income classification: high Low‐SES sample: yes Population description: Sure Start Early Years’ Centres focus on the 20% most disadvantaged families. Inclusion criteria: inclusion criteria were (1) located in one of the 12 district authorities of Lancashire, UK, (2) located in an area of deprivation, (3) high levels of overweight/obese reception class children (4‐5 years) in the neighbouring primary school, (4) not previously taken part in the intervention and (5) has a matched Centre in the geographical locality. Exclusion criteria: centres were excluded if they had previously accessed any part of the intervention being evaluated. Number of services randomised: 10 (5 intervention, 5 control) Number of children randomised: 87 (48 intervention, 39 control) Characteristics Children Age: Intervention: 51% 24‐25 months; 51%; 26‐27 months: 15%; 28‐29 months: 11%; 30+ months: 23% Control: 24‐25 months: 44%; 26‐27 months: 9%; 28‐29 months: 12%; 30+ months: 35% Gender (% female): 49% Ethnicity: not reported Parents Age (years): Intervention: 19‐29 years: 40%; 30‐34 years 36%; 235‐41 years: 3% Control: 19‐29 years: 47%; 30‐34 years: 27%; 35‐41 years: 27% Gender (% female): 99% Ethnicity: Intervention: Asian: 13% ; white: 87%; black: 0%; other: 0% Control: Asian: 12%; black: 6%; white: 76%; other: 6% Parent/family SES: Paid employment: Intervention: none: 51%; part time: 40%; full time: 9%; Control: none: 47%; part time: 44%; full time: 9% Socioeconomic group Intervention: professional/managerial/technical: 13%; skilled/partially skilled/unskilled: 87% Control: professional/managerial/technical: 18%; skilled/partially skilled/unskilled: 82% Method of recruitment: Early Years’ Centres sent out recruitment letters to 160 (10%) parents with a 2‐year old child on their registers. Only 1 parent responded. Therefore, with the assistance of the centre staff, 1 of the authors spent time at each centre, recruiting parents with a 2‐year‐old child into the study. Missing data/dropout: 1 control centre withdrew, so the matched intervention centre needed to withdraw (6 families lost to follow‐up). Reasons for dropout: 1 pair of centres was withdrawn because the control centre refused to allow families to be recruited to the study Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: not reported Number of conditions: 1 intervention, 1 control Intervention duration: 6 months Intervention setting: ECEC and home Intervention strategies: Ethos and environment Children Exposure: trained ECEC centre staff delivered healthy cooking courses and active play sessions to children families, in groups or one‐to‐one. ECEC staff Training: educators were trained to educate families about healthy eating and being active (2‐3 staff from each intervention centre were trained for 2 h). 1‐2 were educators trained to deliver group or one‐on one sessions with parent‐child dyads. Training covered centre policies for food, drink and physical activity, provision of snack/meals service, cooking, good growing and active play, practice breastfeeding; and health promotion in the form of leaflets, displays, advice on nutrition and physical activity. Service Resources: centre received curriculum pack called Healthy Heroes – 4 bright coloured characters who lead healthy lifestyles. Partnerships Families Resources: families received the Healthy Heroes Activity Pack including activity cards (e.g. eating at the table), stickers, songs, puppets, national campaign materials (Change4Life), and activity cards for families to use at home Exposure: trained ECEC centre staff delivered healthy cooking courses and active play sessions to families, in groups or one‐to‐one. Healthcare Engagement: Lancashire County Council’s Children and Young People’s Team, National Health Service (NHS) Public Health personnel and NHS Early Years Health Practitioners trained the educators. Intensity of intervention: 2‐3 staff from each service provided training for 2 h; 1‐2 staff from each service trained to provide parent‐child dyad sessions over 2 d; parent child‐dyads attended sessions over 6 months (duration and frequency not reported) Intervention delivered by: ECEC staff, healthcare Modality: face‐to‐face, written Theoretical basis: Social Learning Theory Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: not reported Outcomes relating to child physical measures: BMI z‐score Number of participants analysed: Intervention baseline: 46 Intervention follow‐up: 46 Control baseline: 34 Control follow‐up: 34 Data collection measure: objectively measured (WHO) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: Alison Hodgkinson was sponsored by her employer NHS North Lancashire and Lancashire County Council. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Centres were matched in pairs by disadvantaged geographical area. Matched centres were randomly allocated to intervention or control by picking their name from a hat. |
| Allocation concealment (selection bias) | Low risk | Study authors stated that "Ten centres were recruited in five matched pairs and all centres had agreed to be allocated to either the intervention or control arm of the study." |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, child‐care service staff and study personnel delivering the intervention were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | No blinding of outcome assessors, however children's height and weight were measured and are unlikely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Physical outcomes | Unclear risk | Attrition was not reported for the time point extracted (6 months), so risk of attrition bias is unclear. |
| Selective reporting (reporting bias) | Low risk | The reported outcomes aligned with those outlined in the trial registration. |
| Recruitment bias | High risk | Individual recruitment occurred after randomisation of clusters. Study authors state that "This lack of balance is common in cluster trials where randomisation is not at the individual level but at the cluster level and is likely a result of recruitment bias by children centre staff, subconsciously selecting those they thought could benefit most." |
| Baseline imbalance | Low risk | Baseline imbalance was reported for the number of Centre visits per week, children > 98th percentile BMI‐for‐age, and mother's smoking. Only imbalance of BMI was accounted for in analysis, though BMI is the only one likely to impact the outcome. |
| Loss of clusters | High risk | One control cluster lost, and the matched intervention cluster was removed from analysis |
| Incorrect analysis | Low risk | Study authors stated that "Finally, two multilevel models were fitted, allowing the variance between centres and between children within centres to be jointly estimated together with the effect of the intervention versus control, and thus allowed for non‐ignorable intraclass correlation." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Hu 2009.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 1 year Unit of allocation: kindergartens Unit of analysis: child |
|
| Participants |
Service type: centre‐based (kindergartens) Operation: not reported Country (region): China (Anhui Province) Country income classification: upper‐middle Low‐SES sample: unclear Population description: this study was performed in Hefei, the capital city of Anhui Province, eastern China. The city is divided into 3 administrative districts: east urban, central urban and west urban, which have been built around 17 kindergartens (totaling 8752 children). Inclusion criteria: not reported Exclusion criteria: not reported Number of services randomised: 7 (4 intervention, 3 control) Number of children randomised: 2102 (1252 intervention, 850 control) Characteristics Children Age: 4.6 years (SD 0.6) Gender (% female): Intervention: 47.7% Control: 44.04% Ethnicity: not reported Parents Age (years): Intervention: mother: 31.5 (SD 2.6); father: 33.6 (SD 2.9) Control group: mother: 31.4 (SD 2.1); father: 33.3 (SD 2.3). Gender (% female): not reported Ethnicity: not reported Parent/family SES: Family income per capita (RMB/month): Intervention < 400: 13.99%; 400‐800: 57.48%; > 800: 28.54% Control: < 400: 14.56%; 400‐800: 61.13%; > 800: 24.31% Mothers' education: Intervention: elementary: 1.21%; junior middle: 22.23%; senior middle: 38.80%; college: 27.41%; graduate: 10.35% Control: elementary: 1.56%; junior middle: 19.98%; senior middle: 38.03%; college: 29.96%; graduate: 10.47% Fathers' education: Intervention: elementary school: 0.49%; junior middle: 14.31%; senior middle: 32.34%; college: 31.93%; graduate: 20.94 Control: elementary school: 0.84%: junior middle: 15.40%; senior middle: 34.66%; college: 29.72%; graduate: 19.37% Method of recruitment: not reported Missing data/dropout: 87.95% retained at mid‐term follow‐up and 84.86% retained at post‐intervention follow‐up Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: not reported Number of conditions: 1 intervention, 1 control Intervention duration: 12 months (including 2 months of summer and winter vacation) Intervention setting: ECEC Intervention strategies: Health curriculum Children Education: monthly nutrition education sessions with a flexible curriculum delivered by trained graduate students and research assistants. The programme was developed by nutrition professionals and included basic nutrition information, skills for food preparation and cooking and benefits of physical activity. Ethos and environment Children Resources: teachers distributed an illustrated book to children about nutritional themes. Service Resources: 2 promotional pictures depicting common unhealthy dietary behaviours and good lifestyle behaviours were displayed in the kindergartens. Partnerships Families Education: a flexible curriculum for in‐kindergarten education delivered monthly to children and parents by trained nutrition graduate students and research assistants. Parents were informed of the events by their children's teachers and training took place within the kindergartens. At least 8 lectures or activities were implemented in each kindergarten during the 1‐year intervention period. Resources: pamphlets, which included nutritional information and described healthy lifestyle behaviours were distributed to parents. Activities: parents were instructed to read the pamphlet and were periodically checked by research assistants. The nutritional prejudices of the parents were addressed directly in a series of activities. Intensity of intervention: at least 8 lectures or activities were implemented in each intervention kindergarten; 1 x illustrated book was distributed to children; pamphlets delivered to parents; 2 series of promotion pictures displayed in intervention kindergartens Intervention delivered by: research team Modality: face‐to‐face, written Theoretical basis: not reported Description of control: usual care, plus children in the control group received a book with general picture stories |
|
| Outcomes |
Outcomes relating to child dietary intake: Unhealthy snacks intake, Western‐style high‐energy foods intake, preference for salty foods, monophagia, eating candy before meal, eating candy before going to bed, eating breakfast, eating a fixed quantity at a particular time Number of participants analysed: Intervention baseline: 1237 Intervention follow‐up: 1042 Control baseline: 831 Control follow‐up: 713 Data collection measure: parent questionnaire Data collector: parent Validity of measures used: not reported Outcomes relating to child physical measures: Weight, weight‐for‐age z‐score Number of participants analysed: Intervention baseline: 1237 Intervention follow‐up: 1042 Control baseline: 831 Control follow‐up: 713 Data collection measure: objectively measured (WHO) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: Nutrition Educational Project of the Chinese Academy of Preventive Medicine (No. 200106) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was stratified by administrative district in order to achieve heterogeneity in location. Kindergartens were then randomised to either an intervention or control group using computer‐generated numbers within each district. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported. |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | No clear blinding of participants and personnel to study allocation, and the outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | No clear blinding of participants and personnel to study allocation, however the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Parents reported children's dietary behaviours. Blinding of parents not reported, and the outcome measurement is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured by trained graduate student research assistants using a standard technique and the outcome measurements are not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Low risk | Data were available for 1092 (88%) pairs in the intervention group and 727 (87%) pairs in the control group at follow‐up. Loss to follow‐up is reasonable and similar across both groups, though no reasons are given for missing data. Therefore, risk of attrition bias was considered to be low. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Data were available for 1092 (88%) pairs in the intervention group and 727 (87%) pairs in the control group at midterm, and 1042 (84%) pairs in the intervention group and 713 (86%) pairs in the control group at post‐test. Loss to follow‐up is reasonable and similar across both groups, though no reasons are given for missing data. Therefore, risk of attrition bias was considered to be low. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting. |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Low risk | There were no significant differences in age, gender, parents' education, or family income between groups. Randomisation was stratified by administrative district. |
| Loss of clusters | Unclear risk | Not sufficiently reported |
| Incorrect analysis | High risk | Kindergartens were randomised, however there was no accounting for clustering of children within kindergartens. |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Iaia 2017.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 1 year Unit of allocation: child‐care centre Unit of analysis: child |
|
| Participants |
Service type: centre‐based Operation: public Country (region): Italy (Cesena, Forlì‐Cesena) Country income classification: high Low‐SES sample: unclear Population description: not reported Inclusion criteria: each cluster aimed to include at least 15 3‐year‐old children to be eligible for the trial. Eligibility criteria for participants were: no chronic medical condition precluding them from study participation; being Italian or Italian‐speaking non‐Italian families. Exclusion criteria: not reported Number of services randomised: 16 (8 intervention, 8 control) Number of children randomised: 425 children (199 intervention, 226 control) Characteristics Children Age: 3.41 (SE 0.09) Gender (% female): 48% Ethnicity: Italian: 91.2%; non‐Italian: 8.8% Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: Mothers' employment status: working full time: 44.9%; working part time: 31.7%; unemployed: 23.3% Fathers' employment status: working full time: 92.1%; working part time: 5.1%; unemployed: 2.8% Mothers' level of education: none: 1.3%; primary school: 0.8%; secondary school: 17.6%; high school: 51.1%; graduation: 29.2%; Fathers' level of education: none: 1.4%; primary school: 0.9%; secondary school: 33.1%; high school: 43.7%; graduation: 21% Method of recruitment: "we informed all childcare centre directors about our study procedures. They all agreed to take part in it without knowing the random allocation of their centres." Missing data/dropout: intervention: 23/199 (11.6%); control: 16/226 (7.1%) Reasons for dropout: intervention: 8 children changing ECEC centre; data collection problems (15 incomplete diaries and 8 diaries missing; 8 children without weight/height measurements). Control: 6 children changing ECEC centre; data collection problems (10 incomplete diaries and 6 diaries missing; 6 children without weight/height measurements) Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: not reported Number of conditions: 1 intervention, 1 control Intervention duration: 6 months Intervention setting: ECEC and local health centres Intervention strategies: Health curriculum Children Education: children and teachers engaged in learning experiences (~1 h/d) to achieve 3 behaviour goals: increasing fruit and vegetable intake (e.g. via encouragement to eat vegetables first at lunch, tending vegetable gardens, inventing and playing stories with fruit and vegetable characters, making creative experiences with fruit and vegetables and peer‐to‐peer role modelling); reducing time spent watching television; and, limiting sugar‐sweetened beverage intake. Ethos and environment Children Exposure: children were exposed to new fruit and vegetables. Peer modelling: teachers repeatedly allocated ‘good fruit and vegetable eaters’ to different tables so as to raise the fruit and vegetable intake among ‘bad' fruit and vegetable eaters. ECEC staff Training: teachers received 10 h of training to promote more active play at ECEC centres and inserted this subject into their annual educational timetables. Resources: information manual Service Environment: water is the only beverage at special events, such as birthdays or parties Partnerships Families Education: parents received 2 x face‐to‐face motivational interviews to help families to increasingly adopt healthy lifestyles, the first was conducted by trained paediatric nurses, the second by trained primary care paediatricians. Resources: an information leaflet and manual Activities: teachers launched a book‐lending initiative among parents. Community Environment: a poster highlighting 4 key behaviours was displayed in waiting rooms of paediatric clinics and in child‐care centre halls. Healthcare Delivery: trained primary care paediatricians delivered education. Intensity of intervention: 2 x 20‐min face‐to‐face parent motivational interviews; information tools; 10 h‐long teacher training; teachers engaged children in learning experiences for 1 h/d Intervention delivered by: research team, ECEC staff, healthcare Modality: face‐to‐face, written Theoretical basis: not reported Description of control: usual care and parents were offered routine healthcare advice during child health visits. |
|
| Outcomes |
Outcomes relating to child dietary intake: Fruit and vegetable intake, sugar‐sweetened beverages intake Number of participants analysed: Intervention baseline: 185 Intervention follow‐up: 162 Control baseline: 178 Control follow‐up: 162 Data collection measure: parent diary Data collector: parent Validity of measures used: not reported Outcomes relating to child physical measures: BMI, BMI z‐score Number of participants analysed: Intervention baseline: 184 Intervention follow‐up: 176 Control baseline: 191 Control follow‐up: 185 Data collection measure: objectively measured (CDC) Data collector: researchers Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: Training, time for carrying out the intervention study, cost of materials Number of participants analysed (intervention group only): Services: 8 Children: 199 Data collection measure: not reported Data collector: not reported Validity of measures used: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: in September 2012, OROGEL S.p.A., a company based in via Dismano 2600, I‐47522, Cesena, Forlì Cesena, Italy, granted EUR 10 000 in support of the educational intervention. "This sponsor had no role in designing and conducting our study; collecting, managing, analysing and interpreting its data; and preparing, reviewing and approving the paper." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Study authors stated that "A person not involved in the study used a computer to create an allocation table to randomly allocate 8 clusters to the intervention group and 8 clusters to the control group." |
| Allocation concealment (selection bias) | Unclear risk | Study authors stated that "We informed all childcare centre directors about our study procedures. They all agreed to take part in it without knowing the random allocation of their centres. We did not provide parents with any information about their children's allocation before we achieved their parental consent." However, it is possible that centres shared allocation with parents due to randomisation occurring prior to recruitment. |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | We assumed that due to the nature of the intervention, childcare service staff and parents were not blind to the study allocation. The outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, childcare service staff and parents were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Cost | Unclear risk | We assumed that due to the nature of the intervention, child‐care service staff and parents were not blind to the study allocation. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Parents reported children's dietary intake. Blinding of parents not reported, and the outcome measurement is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured by trained nurses and were not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Cost | Unclear risk | Blinding not reported. It is unclear if this outcome is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Low risk | Data were available for 162 (88%) participants in the intervention group and 162 (91%) participants in the control group at follow‐up. Further, ITT analyses were used. Study authors stated that "We suffered a significant loss of the data at follow‐up. Nevertheless, the ITT approach is likely to have successfully accounted for potential attrition bias." Reasons for missing data were similar across groups (i.e. changing child‐care centre, data collection problems). Therefore, risk of attrition bias was considered to be low. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Data were available for 176 (96%) participants in the intervention group and 185 (97%) participants in the control group at follow‐up. Further, ITT analyses were used. Study authors stated that "We suffered a significant loss of the data at follow‐up. Nevertheless, the ITT approach is likely to have successfully accounted for potential attrition bias." Reasons for missing data were similar across groups (i.e. changing child‐care centre, data collection problems). Therefore, risk of attrition bias was considered to be low. |
| Incomplete outcome data (attrition bias) Cost | Low risk | Data was available for all participants in the intervention arm (no data was collected for the control arm given the outcome). |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting. |
| Recruitment bias | Unclear risk | Individual recruitment occurred after randomisation of clusters. Study authors stated that "We did not provide parents with any information about their children's allocation before we achieved their parental consent." It is unclear whether this blinding could have been broken. |
| Baseline imbalance | Low risk | Study authors states that there were "no differences between the groups in the children's baseline characteristics. There was a higher percentage of overweight and obese fathers (IOTF cutoffs) in the intervention group compared with the control group: 55 vs 36.4% overweight and 7.7 vs 4.1% obese (χ2 = 7.34; P = 0.025)." Analyses did not account for this difference, however this is unlikely to influence the outcome. |
| Loss of clusters | Low risk | No clusters were lost at follow‐up. Study authors stated that "All the randomized childcare centres completed our study protocol." |
| Incorrect analysis | Low risk | Study authors stated that "To examine the hierarchical data structure (children's measurements, child, childcare centres), we applied a three‐level linear model, though preferring a two‐level model that used children as random effect because of a school random effect near to 0. We provided both multilevel models: a random intercept model and a random intercept and slope model. We chose the first model in order to apply a principle of parsimony." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Unclear risk | The intervention received financial support from a commercial organisation. Study authors state that this company had no operational role. |
Jones 2015.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 12 months Unit of allocation: centre Unit of analysis: child |
|
| Participants |
Service type: centre‐based (preschools and long‐day care) Operation: were not 100% government‐funded services. 90%‐98% of services operated 5 d/week Country (region): Australia (Hunter region, New South Wales) Country income classification: high Low‐SES sample: yes Population description: the study took place in the Hunter region of New South Wales, Australia. The region encompasses non‐metropolitan ‘major cities’ and ‘inner regional’ areas as described by the Australian Statistical Geography Standard. There are 586,000 people residing in the area, of whom 23,000 are children aged 3–5 years. Approximately 3% of residents are of Aboriginal or Torres Strait Islander origin and 4% speak languages other than English. The Hunter region has lower indices of SES than the New South Wales state average. Inclusion criteria: not reported Exclusion criteria: services in the region were ineligible if they: catered exclusively for children requiring specialist care (< 1 % of services), provided all on‐site meals to children (approximately 30% of services) or were fully government‐funded (approximately 3 % of services), as the ethical clearance and intervention design were not appropriate for such services. Number of services randomised: 128 (64 intervention, 64 control) Number of children randomised: not reported (3 children from each service randomly selected for dietary outcome assessment) Characteristics Children Age: not reported Gender (% female): not reported Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported Service Ethnicity: Children of Aboriginal or Torres Strait Islander background enrolled: Intervention: 68% Control: 78% Service socioeconomic area: Top 50% of New South Wales: Intervention: 30% Control: 27% Method of recruitment: Phone and mail Missing data/dropout: 6 child‐care services with baseline data declined to participate in the trial. 62 services were retained in the intervention group, and 60 in the control. But observational data were collected from 17 intervention centres and 19 control centres. Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: not reported Number of conditions: 1 intervention, 1 control Intervention duration: 12 months Intervention setting: ECEC Intervention strategies: Ethos and environment Children Exposure: provision of adult‐guided fundamental movement skills for at least 75% of children daily. Restriction of sedentary screen time to less than weekly. Role modelling: staff role modelling of physical activity and healthy eating to children Prompts and feedback: staff provision of prompts and positive feedback to encourage child healthy eating ECEC staff Training: a series of 3 x 1‐h training workshops which focused on policy and practice implementation. Support: following each staff training workshop, implementation support staff facilitated a discussion with nominated supervisors and ECEC service staff to reach group agreement regarding an implementation strategy for the targeted policies and practices. Engagement: nominated supervisors were asked to lead the development and implementation of nutrition and physical activity policies, co‐facilitate training workshops with implementation support staff and communicate expectations regarding the implementation of policies and practices to ECEC service staff during staff meetings. Service Policy: development and implementation of written nutrition and physical activity policies Monitoring: daily staff monitoring of children's lunch boxes against written nutritional guidelines and provision of feedback to parents when a non‐compliant food was packed. Provision of water or reduced‐fat milk only. Resources: all services received an electronic and hardcopy package of tools and resources to support ECEC service staff to implement the healthy eating and physical activity policies and practices. Services received hard copy and electronic bimonthly newsletters, which communicated key messages relating to the healthy eating and physical activity policies and practices. Services that implemented all policies and practices received a certificate of recognition, were acknowledged in newsletters and were used as case‐study examples. Feedback: verbal and written feedback describing service progress toward implementation of the targeted policies and practices was delivered at 6 intervals throughout the 12‐month intervention. Partnerships Healthcare Support: health promotion officers provided each service with a support staff member who provided ongoing implementation support and positive reinforcement via in‐person visits, telephone and email contact. Intensity of intervention: 3 x 1‐h staff training workshops; bimonthly newsletters. The frequency and duration of the following strategies were not reported: ongoing implementation support; face‐to‐face meetings; telephone and email contact; executive support; consensus process with staff; academic detailing visits; provision of tools and resources; performance monitoring and feedback. Intervention delivered by: research team, ECEC staff, healthcare staff Modality: face‐to‐face, telephone, online, written Theoretical basis: Damschroder’s Consolidated Framework for Implementation Research Description of control: usual care, plus services received 3 newsletters at the commencement, mid‐point and conclusion of the 12‐month intervention. The newsletters were provided in hard copy and electronic formats and contained information on healthy eating and physical activity unrelated to the specific policies and practices targeted by the intervention. |
|
| Outcomes |
Outcomes relating to child dietary intake: Fruit intake, vegetable intake, grains (breads and cereals) intake, meat and meat alternatives intake, milk/yoghurt/cheese intake, discretionary food intake Number of participants analysed: Intervention baseline: not reported Intervention follow‐up: 41 Control baseline: not reported Control follow‐up: 49 Data collection measure: in‐care observations Data collector: trained research observers Validity of measures used: validated Outcomes relating to child physical measures: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: Increased occurrence of injury among staff or children Number of participants analysed: not reported Data collection measure: nominated supervisors were asked to report on the number of staff and children involved in adverse events in their service Data collector: nominated supervisors Validity of measures used: not reported |
|
| Notes | Funding source: Australian National Preventive Health Agency (reference 95WOL2011), Hunter New England Population Health and Hunter Medical Research Institute. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | After the completion of baseline data collection, ECEC services were randomly allocated to either the intervention or control condition by a research assistant using a random number function in a 1:1 (intervention:control) ratio. |
| Allocation concealment (selection bias) | Low risk | After baseline data were collected, a statistician not involved in the trial allocated the services to groups using a random number function. |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | Services were not blind to study allocation, and the outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Adverse consequences | Unclear risk | Services were not blind to study allocation. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | Low risk | Children's dietary intake was observed by a trained observer who did not participate in the intervention delivery and who was blind to service group allocation. |
| Blinding of outcome assessment (detection bias) Adverse consequences | Unclear risk | Services were not blind to study allocation. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Unclear risk | Data analysed for 17/62 (27%) of intervention services and 19/60 (32%) of control services. Dietary observations were conducted in a random subsample of intervention and control services at follow‐up, however there is no information on how the random sample was determined or if there was loss to follow‐up in the random subsample. Risk of attrition bias is unclear. |
| Incomplete outcome data (attrition bias) Adverse consequences | Unclear risk | The number of services that reported on this outcome at follow‐up is unclear. |
| Selective reporting (reporting bias) | High risk | Observation data and adverse events, the data of interest for the review, are not mentioned in the available protocol. These outcomes appear to have been added in post‐hoc with no reasoning provided. |
| Recruitment bias | Low risk | ECEC services were recruited prior to randomisation, and no ECEC services were recruited after randomisation. |
| Baseline imbalance | Unclear risk | No information provided on individual participants. Data only provided at the service level |
| Loss of clusters | Low risk | 2 of the 64 intervention clusters and 4 of the 64 control clusters were lost. However, this is a small percentage (< 5%) of the overall sample. Study authors stated that "There were no differences between the characteristics of services that provided follow‐up data and those that did not (p = 0.22‐1.00)." |
| Incorrect analysis | Low risk | Study authors stated that "The model was adjusted for potential clustering effect." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Unclear risk | Intervention and control groups showed baseline imbalance in terms of extraneous training. Study authors stated that "Project records show that 80% of intervention group services and 12% of control group services attended training in healthy eating and physical activity provided by the 'Munch & Move' program during the study period." and "Project records provided by the program show 45% of intervention group services and 52% of control group services attended training in healthy eating and physical activity provided by the 'Good for Kids. Good for Life' program during the period from 2006 to 2011." There were also baseline differences in the implementation of policies and practices between groups. Study authors stated that "However, five of the seven policies and practices were being implemented by 80% or more of intervention group services at baseline, limiting scope for further improvements. Second, the trial did not exclude services who were already implementing all policies and practices at baseline (24% of intervention services)." Children who were randomly selected for observation were chosen based on their birth date. There is insufficient information to assess whether an important risk of bias exists. |
Kipping 2019.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 8‐10 months Unit of allocation: nurseries Unit of analysis: child |
|
| Participants |
Service type: centre‐based (preschools, day nurseries and centre nurseries) Operation: combination of community and private Country (region): UK (North Somerset and Gloucestershire ) Country income classification: high Low‐SES sample: no Population description: the study took place in nurseries in 2 areas of England (North Somerset and Gloucestershire) and in the homes of children recruited to the study. North Somerset is a rural area adjacent to Bristol, with 14.1% of children living in poverty (percent of children aged < 16 years in families receiving means‐tested benefits and low income in 2012). Gloucestershire is a large rural county to the north of Bristol. The health of people in Gloucestershire is generally better than the England average; however, 13.8% of children live in poverty. Inclusion criteria: child‐care providers must be a day nursery, private nursery school, maintained nursery school, children’s centre with nursery, or preschool, in North Somerset or Gloucestershire. Settings were eligible if they had a minimum of 20 children aged 2–4 years who attend the child‐care providers for at least 12 h/week over 50 weeks of the year, or 15 h/week in term time. Exclusion criteria: excluded child‐care settings were child minders, crèches, playgroups, primary school reception classes (where schools operate an early‐admission policy to admit children aged 4 years) and au pairs. Number of services randomised: 12 (6 intervention, 6 control) Number of children randomised: 476 (86 participated intervention, 91 participated control) Characteristics Children Age: 2‐4 year olds Gender (% female): not reported Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported Method of recruitment: ECEC providers were sent a letter from the Council, project information sheet, reply envelope and form indicating if they wished to participate and reason for their response. Non‐responders were followed up with a reminder and then a telephone call. All interested ECEC providers were contacted by telephone to discuss the study following which, if the provider was still interested, they were offered a visit to discuss the intervention and study in more detail. A GBP 200 incentive was provided to all participating nurseries at the end of the study. Missing data/dropout: at the follow‐up data collection, 147 (87.5%) out of 168 children at baseline participated in data collection. Out of the 476 potentially eligible children at baseline, 147 (30.9%) children provided data at baseline and follow‐up. Reasons for dropout: 2 (1.2%) children had consent withdrawn, 2 (1.2%) refused to participate in measurements and their parents did not return follow‐up questionnaires, 8 (4.8%) moved nursery and 9 (5.4%) moved to primary school and did not take up the offer to continue participation. Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: NAP SACC UK ((The Nutrition And Physical Activity Self‐Assessment for Child Care UK) Number of conditions: 1 intervention, 1 control Intervention duration: 5 months Intervention setting: ECEC and home Intervention strategies: Ethos and environment ECEC staff Workshop: specialised staff delivered 2 workshops to the nursery staff on nutrition, oral health and physical activity. Action planning: the NAP SACC UK partners worked with the nursery manager to set out an action plan, listing 8 goals for improvement. These were 3 nutrition goals, 3 physical activity goals and 2 further goals of their choice. The NAP SACC partner helped the nursery manager agree how and when these goals will be reached. Support: intervention partners continued regular contact with nursery (via telephone, email or in person), providing support and advice to help the nursery meet their goals. Self‐monitoring: 'Review and reflect' process of self‐assessment to see where improvements were made. Where improvements were not made, reasons why were discussed to help overcome barriers. Action plans were revised to set new goals. Service Policy: nursery staff were supported to review the nutrition, oral health, physical activity and screen time environment, policies and practices against best practice and national guidelines. Partnerships Families Resources: parents were given access to the NAP SACC at home website to complete healthy habits forms and set goals. As an incentive, the first 50 parents to register received a swimming voucher to the local pool. Support: parents received tailored texts/emails giving them suggestions or areas to set goals. Partners Workshop: a 2‐2.5 h training session was delivered to partners. Support: intervention partners provided support and advice to help the nursery meet their goals. Intensity of intervention: initial staff meetings lasted for > 2 h (between the health visitor and nursery manager); average number of advice/support opportunities was 2.2 face‐to‐face meetings, 1.8 telephone calls and 2.8 emails. 2 x workshops delivered to nursery staff by local experts in nutrition (3 h) and physical activity (2.5 h); a home component (website, short message service and emails) was developed to support parents in setting goal, they could assess this as often as they liked (tailored text messages or emails were sent to parents on a fortnightly basis). Intervention delivered by: research team Modality: face‐to‐face, telephone, online, written Theoretical basis: Social Cognitive Theory and the Socioeconomic Framework Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: Types of fruit and vegetable intake; meat, fish, eggs, beans and other non‐dairy sources of protein intake; desserts, puddings and cakes intake; beverages intake; starchy food intake Number of participants analysed: Intervention baseline: 13‐30 Intervention follow‐up: 13‐30 Control baseline: 12‐27 Control follow‐up: 12‐27 Data collection measure: child and Diet Evaluation Tool (CADET) Data collector: trained observer Validity of measures used: validated Outcomes relating to child physical measures: BMI z‐score, weight, overweight or obese, obese Number of participants analysed: Intervention baseline: 30‐58 Intervention follow‐up: 30‐58 Control baseline: 18‐76 Control follow‐up: 18‐76 Data collection measure: objectively measured (UK, 1990 age and gender growth reference charts and International Obesity Task Force (IOTF) reference points) Data collector: trained field workers Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: Quality of life (total, physical function, emotional function, social function, nursery function) Number of participants analysed: Intervention baseline: 32 Intervention follow‐up: 32 Control baseline: 45 Control follow‐up: 45 Data collection measure: Paediatric Quality of Life Inventory (PedsQL) 4.0 Data collector: parent Validity of measures used: validated Outcome relating to cost: Average cost of health visitor intervention delivery per nursery (including workshop), average cost of intervention to nursery, parental weekly food spend Number of participants analysed: not reported Data collection measure: nursery logs and parent‐completed questionnaire Data collector: unclear and parent Validity of measures used: not reported Outcome relating to adverse consequences: Incident or adverse event Number of participants analysed: not reported Data collection measure: nursery managers and those delivering the intervention were asked to contact the study team within 5 working days if any untoward incident or adverse event occurred to a member of staff or child as a result of the intervention Data collector: nursery managers and those delivering the intervention Validity of measures used: not reported |
|
| Notes | Funding source: North Somerset Council and Gloucestershire Council. Development and Evaluation of Complex Interventions for Public Health Improvement (DECIPHer). Elizabeth Blackwell Institute (University of Bristol) and the Wellcome Trust. Medical Research Council (MRC) and from the Scottish Government Chief Scientist Office | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ECEC providers were stratified by geographic area, deprivation of location, and size of provider and randomised to the control or intervention groups. Allocation was conducted by an independent statistician at the Bristol Randomised Trials Collaboration, blind to the identity of the ECEC providers. |
| Allocation concealment (selection bias) | Low risk | Allocation was conducted by an independent statistician who was blind to the identity of the ECEC providers. |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | No clear blinding of participants and personnel to study allocation, and the outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | No clear blinding of participants and personnel to study allocation, however the outcome is not likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Quality of life outcomes | High risk | No clear blinding of participants and personnel to study allocation, and the outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Cost | Unclear risk | No clear blinding of participants and personnel to study allocation. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Adverse consequences | Unclear risk | No clear blinding of participants and personnel to study allocation. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Dietary intake data were reported by researcher observers and parents using the Child and Diet Evaluation Tool (CADET). Blinding of parents and researchers not reported, and the outcome measurement is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured by trained field workers with a member of nursery staff present and the outcome measurements are not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Quality of life outcomes | High risk | Parents reported children's functioning using the Paediatric Quality of Life Inventory 4.0. Blinding of parents not reported, and the outcome measurement is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Cost | Unclear risk | No clear blinding of participants and personnel to study allocation. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Adverse consequences | Unclear risk | No clear blinding of participants and personnel to study allocation. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | High risk | CADET nursery data are available for 130 (85%) children at follow‐up, while CADET home data are available for 79 (57%) children at follow‐up. Due to the magnitude of missing data and difference in the proportions of participants followed up between groups, the risk of bias was assessed as high. |
| Incomplete outcome data (attrition bias) Physical outcomes | High risk | In the intervention group, 81 children were analysed at baseline, however only 41 (51%) had BMI z‐score data at follow‐up. In the control group, 86 children were analysed at baseline, however only 56 (65%) had BMI z‐score data at follow‐up. Due to the magnitude of missing data, the risk of bias was assessed as high. |
| Incomplete outcome data (attrition bias) Quality of life outcomes | High risk | Study authors stated that "A total of 124 parents (72.1%) completed the questionnaire about the child's quality of life, expenditure on food and physical activity and child health‐care use at baseline. A total of 86 parents (50%) completed the questionnaire at follow‐up. The complete case for HRQoL [health‐related quality of life] analysis was 77 (44.8%)." Due to the magnitude of missing data, the risk of bias was assessed as high. |
| Incomplete outcome data (attrition bias) Cost | High risk | Data were available for 86 (51.8%) of parents at follow‐up and 12 services did not take part in the whole intervention, indicating high attrition. |
| Incomplete outcome data (attrition bias) Adverse consequences | Unclear risk | The number of services and participants that reported on this outcome at follow‐up is unclear. |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the paper were prespecified in the protocol paper. |
| Recruitment bias | High risk | Centres were allocated prior to individual recruitment, and thus an individual knew if the school was receiving the intervention or control prior to signing up. |
| Baseline imbalance | Unclear risk | Baseline differences are noted, although it is unclear if these differences are statistically significant. Study authors state that "Stratified randomisation was used to ensure balance for (1) deprivation... (2) size of child‐care provider...and (3) location." |
| Loss of clusters | High risk | One cluster did not fully implement the intervention, and it is unclear what happened with these data and the children from this centre. All analyses are descriptive. |
| Incorrect analysis | High risk | There was no accounting for clustering of children within nurseries. |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Kobel 2019.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 1 year Unit of allocation: kindergartens Unit of analysis: child |
|
| Participants |
Service type: centre‐based (kindergartens) Operation: not reported Country (region): Germany (South‐West Germany) Country income classification: high Low‐SES sample: unclear Population description: not reported Inclusion criteria: only kindergartens that had not previously taken part in the programme were included in the study. Children within the recruited kindergartens were eligible if they were between 3 and 5 years old at the time of baseline measurements and their parents provided a signed consent form. Exclusion criteria: not reported Number of services randomised: 57 (30 intervention, 27 control) Number of children randomised: 973 (318 participated intervention, 240 participated control) Characteristics Children Age: 3.6 years (SD 0.6) Gender (% female): 47.7% Ethnicity: migration background: 33.4% Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported Method of recruitment: participating kindergartens were recruited from all kindergartens in southwest Germany, which had received written information about programme and study, asking interested kindergarten teachers to participate. Missing data/dropout: 57% dropout Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Join the Healthy Boat Number of conditions: 1 intervention, 1 control Intervention duration: 12 months Intervention setting: ECEC and home Intervention strategies: Health curriculum Children Education: the intervention materials consisted of 20 exercise and games lessons and 30 ready‐to‐use ideas, action alternatives and lessons promoting increased physical activity, reduced screen media consumption, and a more healthy diet, including the reduction of sweetened drinks and an increased fruit and vegetable intake. Ethos and environment Children Exposure: short activity games (exercises of 5–7 min each, which also promote children's motor skills) were used twice daily. ECEC staff Training: kindergarten teachers were trained twice in 16 h of peer‐to‐peer training courses. Resources: kindergarten teachers received instructional and behavioural educational resources. Partnerships Families Resources: family homework, materials for parents' nights and parental letters were provided in 3 languages. Intensity of intervention: 2 x 16 h of peer‐to‐peer training (by teachers); all intervention materials are integrated into the everyday life of kindergartens so no external staff or extra time was required; 20 exercise and games lessons and 30 ready to use ideas, action alternatives and lessons for children Intervention delivered by: ECEC staff Modality: face‐to‐face, written Theoretical basis: Bandura's Socio‐Cognitive Theory and Socio‐Ecological approach Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: Fruit and vegetable intake, sugar sweetened beverage intake Number of participants analysed: Intervention baseline: 318 Intervention follow‐up: 318 Control baseline: 240 Control follow‐up: 240 Data collection measure: parent questionnaire Data collector: parent Validity of measures used: not reported Outcomes relating to child physical measures: BMI percentile Number of participants analysed: Intervention baseline: 538 Intervention follow‐up: 318 Control baseline: 435 Control follow‐up: 240 Data collection measure: objectively measured (German reference data) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: the kindergarten‐based health promotion programme “Join the Healthy Boat” and its evaluation study was financed by the BadenWürttemberg Foundation (grant number BWS_1.479.00_2009). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | No clear blinding of participants and personnel to study allocation, and the outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | No clear blinding of participants and personnel to study allocation, however the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Parents reported dietary patterns via questionnaire. Blinding of parents not reported, and the outcome measurement is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured by trained technicians and were not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | High risk | Follow‐up data are available for 558 (57%) of the children who were assessed at baseline. At baseline, 18% of dietary data were missing, while 30% of dietary data were missing at follow‐up. Reasons for missing data are unclear, and the distribution of loss between groups is not noted. Due to the magnitude of missing data, the risk of bias was assessed as high. |
| Incomplete outcome data (attrition bias) Physical outcomes | Unclear risk | Follow‐up data are available for 558 (57%) of the children who were assessed at baseline. At baseline, 14% of BMI percentile data were missing, while 14% of BMI percentile data were missing at follow‐up. Reasons for missing data are unclear, and the distribution of loss between groups is not noted. Risk of attrition bias is unclear. |
| Selective reporting (reporting bias) | Unclear risk | Protocol states variables for nutrition include consumption of sugar‐sweetened beverages, fruit, vegetables, and high‐calorie foods. Data on consumption of high‐calorie foods are not reported in the study. Further, the protocol states variables for anthropometric parameters include waist circumference, waist‐to‐height ratio, BMI, and subcutaneous fat. Only BMI percentile outcomes are reported in the study. |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Low risk | No baseline differences were noted between groups for any relevant variables except for gender. The researchers controlled for gender in the analysis. |
| Loss of clusters | High risk | After randomisation, 4 kindergartens with 22 kindergarten teachers dropped out, mainly due to personnel and organisation issues, resulting in 376 partaking kindergarten teachers and 62 heads of kindergartens. It is not stated which group these clusters were randomised to. |
| Incorrect analysis | High risk | There was no accounting for clustering of children within kindergartens. |
| Contamination | Unclear risk | Study authors state that "Even though, a major strength of this study is its randomised controlled design with a control group, the kindergarten teachers in that group were also very health conscious and have not been “inactive”, which might have led to a strong contamination with other efforts to promote children's health in the control group." There is not enough information provided to assess whether contamination exists. |
| Other bias | Unclear risk | Study authors stated that "The minimum assumed number was therefore 880 children, the maximum 1120 children. The overall significance level is set to 0.05 (2‐sided). Depending on the number of kindergartens, a small effect size of 0.288 to 0.325 could be achieved for a power of 0.80 for the metric targets." With 558 children at baseline, this study does not appear to be adequately powered. There is insufficient information to assess whether an important risk of bias exists. No conflict of interest statement was reported. |
Kornilaki 2021.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 3 months Unit of allocation: nursery schools Unit of analysis: child |
|
| Participants |
Service type: centre‐based (nursery schools) Operation: not reported Country (region): Greece (Heraklion region of Crete) Country income classification: high Low‐SES sample: unclear Population description: not reported Inclusion criteria: parents were eligible if they were Greek speakers (for questionnaire purposes only). Exclusion criteria: not reported Number of services randomised: 15 (groups not reported) Number of children randomised: 329 (184 intervention, 145 control) Characteristics Children Age: Intervention: 5.03 years (SD 0.54) Control: 5.05 years (SD 0.54) Gender (% female): Intervention: 50% Control: 54.5% Ethnicity: not reported Parents Age (years): Intervention: mother: 37.69 (SD 6.2); father: 40.83 (SD 5.4) Control: mother 37.28 (SD 4.96); father: 40.66 (SD 6.08) Gender (% female): not reported Ethnicity: not reported Parent/family SES: Family income Intervention: up to EUR 14,999, 37.61%; EUR 15,000‐29,999, 47.86%; EUR 30,000‐49,999, 10.26%; > 50,000 euros, 4.27% Control: up to EUR 14,999, 46.66%; EUR 15,000‐29,999, 48%; EUR 30,000‐49,999, 2.67%; > EUR 50,000, 2.67% Mothers' education Intervention: compulsory: 4.24%; high school: 27.12%; technical/vocational: 33.05%; university: 35.59% Control: compulsory: 7.79%; high school: 28.57%; technical/vocational: 28.87%; university: 33.77% Fathers' education Intervention: compulsory: 11.86%; high school: 34.74%; technical/vocational: 23.74%; university: 29.66% Control: compulsory: 16.88%; high school: 32.87%; technical/vocational: 28.18%; university: 22.07% Method of recruitment: all nursery schools in the Heraklion area were invited to participate in the study through phone and email. After organisational approval was given, all educators in each nursery school were verbally invited to the research project and informed consent was obtained. All eligible parents of children in the nursery school were invited to participate through information provided by the educators received directly from the researcher. Missing data/dropout: 26 of 329 did not return the eating and physical activity questionnaire at any time point and were withdrawn from the sample. All 3 time points were returned by 137 parents, 113 parents returned 2 questionnaires and 53 parents returned only 1. Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: not reported Number of conditions: 1 intervention, 1 control Intervention duration: 4‐6 weeks Intervention setting: ECEC Intervention strategies: Health curriculum Children Education: educators delivered the curriculum they had developed (tailored to each class) following training. Ethos and environment ECEC staff Training: 2 x 2‐h professional learning sessions were delivered by trained researchers to the nursery school educators to build the educator’s capacity to develop age‐appropriate educational curriculum activities that increased young children’s healthy eating habits, raised children’s environmental consciousness and provided physical activity opportunities, while engaging their popular culture interests. Educators were encouraged to follow 4 best practice principles when delivering the curriculum: implementing the curriculum experiences in the morning when most cognitively alert; using a combination of 3 identified play types; conducting the curriculum activities 2–3 times/week for between 4 and 6 weeks; and, using a range of real‐life props as resources. Support: researcher support via telephone and email was provided. Intensity of intervention: 2 x 2‐h professional learning sessions were delivered to staff; delivery of curriculum activities 2‐3 times/week by educators Intervention delivered by: research team, ECEC staff Modality: face‐to‐face, telephone, online, written Theoretical basis: Funds of Knowledge Description of control: wait‐list control |
|
| Outcomes |
Outcomes relating to child dietary intake: Fruit and vegetables intake, unhealthy food (packaged snacks, chocolates and confectionary, flavoured milk, cakes and sweet biscuits) intake, sugar sweetened beverages intake, unsweetened beverages (unflavoured milk and water) intake, fruit intake, vegetable intake Number of participants analysed: Intervention baseline: 107‐150 Intervention follow‐up: 115‐119 Control baseline: 86‐114 Control follow‐up: 70‐77 Data collection measure: eating and physical activity questionnaire (EPAQ) Data collector: parents Validity of measures used: validated Outcomes relating to child physical measures: BMI Number of participants analysed: not reported Data collection measure: objectively measured (IOTF) Data collector: not reported Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Nursery schools were randomly allocated to the intervention and control groups through a computer‐generated random number allocation. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. The outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Parents completed the Eating and Physical Activity Questionnaire to report children's dietary intake. Blinding of parents not reported, and the outcome measurement is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured and were not likely to be influenced by lack of blinding |
| Incomplete outcome data (attrition bias) Diet outcomes | Unclear risk | Data from the Eating and Physical Activity Questionnaire for at least 2 time points are available for 142 (77%) children in the intervention group and 108 (74%) of the control group. However, it is not known whether those who only submitted 2 questionnaires had completed the baseline questionnaire. Reasons for missing data not provided. Risk of attrition bias is unclear. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Data were available for 177 (96%) participants in the intervention group and 138 (95%) students in the control group at immediate post‐intervention, and 167 (91%) students in the intervention group and 133 (92%) students in the control group at 3‐month follow‐up. Loss to follow‐up is similar across both groups and within reason (< 10%). Therefore, risk of attrition bias was considered to be low. |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the paper were prespecified in the protocol paper. |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Unclear risk | No significant differences in demographic characteristics were noted between trial groups, except for father's height. However, demographic data weren't obtained until 3 months post‐intervention. Study authors also state that "Finally, no data were collected about the demographics of each classroom (for example, educator/child ratios) or their educators (years of experience)." |
| Loss of clusters | Unclear risk | Not reported |
| Incorrect analysis | High risk | There was no accounting for clustering of children within schools. |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | High risk | No funding statement was provided. |
Kristiansen 2019.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 1 year (varies with outcomes) Unit of allocation: kindergartens Unit of analysis: child |
|
| Participants |
Service type: centre‐based (kindergarten) Operation: public (control 42.5% vs intervention 57.5%) or private (control 57.5% vs intervention 42.5%) Country (region): Norway (Vestfold and Buskerud) Country income classification: high Low‐SES sample: unclear Population description: not reported Inclusion criteria: the target group for the current study was preschool children with year of birth 2010 and 2011, attending public or private kindergartens in the counties of Vestfold and Buskerud, Norway. Exclusion criteria: not reported Number of services randomised: 73 (37 intervention, 36 control) Number of children randomised: 633 (313 intervention, 320 control) Characteristics Children Age: 3‐5 year‐olds Gender (% female): Intervention: 51.1% Control: 51.9% Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: Maternal education: Intervention: low (≤ upper secondary: 32.9%; high (college/university): 67.1% Control: low: 29.9%; high (college/university): 70.1% Method of recruitment: all regular kindergartens (n = 479) in the 2 counties were invited by letter followed‐up by a phone call to inform about the study and to motivate for participation Missing data/dropout: from baseline to follow‐up 1, 16 children (5%) were lost to follow‐up in the control group and 20 children (6%) were lost to follow‐up in the intervention group. Reasons for dropout: the main reason for this loss was children moving to other kindergartens. Characteristics of dropouts: dropout analysis showed no differences in background characteristics between participating children (n = 633) and those lost to follow‐up (n = 66), except that significantly more children were lost in the intervention group compared to the control group (P = 0.02) |
|
| Interventions |
Programme name: BRA‐study (an acronym for the Norwegian words “Barnehage” (kindergarten), “gRønnsaker” (vegetables) and “fAmilie” (family)) Number of conditions: 1 intervention, 1 control Intervention duration: 5 months Intervention setting: ECEC and home Intervention strategies: Ethos and environment ECEC staff Training: kindergarten staff received a 1‐d inspirational course (cooking, taste testing, theoretical sessions, action plans). Attendees were instructed to train/inform the relevant staff in their kindergarten. The theoretical sessions covered availability, accessibility, encouragement and role modelling. Service Resources: each kindergarten received 4 aprons, a vegetable memory game, booklets, 1 hand blender, 6 posters and brochures. They were also given access to a website with all materials and additional information about vegetables and 4 determinants and invited to a closed Facebook group. Booster: booster activities were provided at 3 months and 6 months and included booklets with recipes; a vegetable card/poster to register when and which vegetables were served for 3 d with potential for winning a gift card; and suggestions of tasting games to play with the children. Partnerships Families Resources: kindergarten staff provided families with a 'welcome package' including a cover letter explaining the rationale and the purpose of the intervention, a brochure with vegetable recipe ideas, a stack of post‐its with prompts to buy fruit and vegetables and a booklet to read to children. They were also given access to a website with all materials and additional information about vegetables and 4 determinants and invited to a closed Facebook group. Booster: booster activities were provided at 3 months and 6 months and included booklets with recipes; a vegetable card/poster to register when and which vegetables were served for 3 d with potential for winning a gift card; and suggestions of tasting games to play with the children. Intensity of intervention: 1 x inspirational training day; 1 x resource pack to staff; 1 x resource pack to parents, 1 x website materials to parents and staff (each), 1 x Facebook page for parents and staff (each), 2 x staff booster training; 2 x parent booster training/activity Intervention delivered by: research team, ECEC staff Modality: face‐to‐face, online, written Theoretical basis: not reported Description of control: wait‐list control |
|
| Outcomes |
Outcomes relating to child dietary intake: Vegetable intake, variety in vegetable intake Number of participants analysed: Intervention baseline: 129‐222 Intervention follow‐up: 137‐218 Control baseline: 142‐206 Control follow‐up: 160‐229 Data collection measure: parent questionnaire, direct observation and combination of parent questionnaire and direct observation Data collector: parents and researchers Validity of measures used: not reported Outcomes relating to child physical measures: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: The Research Council of Norway (project number 228452) with supplementary funds from the Throne Holst Nutrition Research Foundation, University of Oslo | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | An external statistician conducted a stratified block randomisation. The randomisation ensured an equal distribution of kindergartens within ownership (public and private) in the 2 groups and total number of participating children in each group. However, the study authors state that the subsample of children who were observed for diet outcomes were "preferably, children of mothers with a low educational level...and otherwise children were chosen for observation at random." The random sequence generation procedure for this subsample was not described. |
| Allocation concealment (selection bias) | Low risk | Allocation was conducted after baseline data collection, however this was done by an independent statistician to ensure even groups. |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | Kindergarten employees were not blind to study allocation as they received kitchen education. Families were not blind as they received take‐home packages and website log‐ons. The outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Diet outcomes | Unclear risk | Study authors state that "Researchers were not blinded to intervention group during data collection at follow‐up 1. However, as there occasionally were options for the researchers to observe the same child/children during the direct observation of vegetable intake, intraclass correlation (ICC) as an estimate of inter‐rater reliability between pairs of observers was calculated. The level of agreement between pairs of observers at follow‐up 1 was 0.99 for the 37 children that were observed by two researchers. This agreement did not change when split into intervention (n 24, ICC = 0.99) and control groups (n 13, ICC = 0.98). This corresponds to the ICC found in the baseline data collection. Hence, this might indicate an unbiased observed vegetable intake." Study authors also state "Parents reported children's dietary intake and knew the aims of the intervention." As dietary outcomes were assessed by 2 methods (observation and parent‐reported data), risk of bias is unclear. |
| Incomplete outcome data (attrition bias) Diet outcomes | High risk | Follow‐up data from observation are available for 311 (76%) of the 411 children who were observed at baseline. Follow‐up data from the questionnaire were available for 311 (71%) of the 439 children with baseline data, and follow‐up data from the 24‐h recall are available from 295 (63%) of the 470 children with baseline data. Reasons for missing data not provided. Due to the magnitude of missing data, the risk of bias was assessed as high. |
| Selective reporting (reporting bias) | Unclear risk | Trial registration states the following primary outcome measures: "Frequency and variation of vegetable intake in children is measured by internet‐based questionnaires completed by parents at baseline (Spring 2015), year 1 (Spring 2016), and year 2 (Spring 2017)," and "Amount of vegetables consumed by children is measured using an internet‐based 24 hour recall where parents report the amounts of vegetables that the child ate the day before at baseline (Spring 2015), year 1 (Spring 2016), and year 2 (Spring 2017)." However, the study combines the internet‐based 24‐h recall with the direct observation to determine baseline total vegetable amount rather than reporting the outcomes of the internet‐based 24‐h recall alone. |
| Recruitment bias | Low risk | Individual recruitment occurred before randomisation of clusters. |
| Baseline imbalance | Low risk | At baseline, groups differed by percent of children attending a public kindergarten, and in children's frequency and variety of vegetable intake. Statistical models adjusted for baseline intake and kindergarten ownership (private or public). |
| Loss of clusters | Unclear risk | No loss of cluster reported, however some kindergartens had 0‐22 students. |
| Incorrect analysis | Low risk | Study authors stated that "Kindergarten was used as a random effect to account for random inhomogeneity between kindergartens." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Leis 2020.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 9 months Unit of allocation: centre Unit of analysis: child |
|
| Participants |
Service type: centre‐based (licensed child‐care centres or preschools) Operation: not reported Country (region): Canada (Saskatchewan and New Brunswick) Country income classification: high Low‐SES sample: unclear Population description: given the large area Saskatchewan represents (652 000 km2), it was decided to carry the study with selected early child‐care centres in the central region in year 1, and in the South and central‐North in years 2 and 3. Inclusion criteria: to be included in the study, an ECEC centre had to prepare and provide meals for lunch. This is required for assessing the quality of foods being served and for measuring nutritional intake. Exclusion criteria: centres with < 20 children between the ages of 3 and 5 were excluded. Number of services randomised: 61 (31 intervention, 30 control) Number of children randomised: 897 (464 intervention, 433 control) Characteristics Children Age: 4.1 years (SD 0.8) Gender (% female): Intervention: 49% Control: 46% Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: Median household income: Intervention: CAD 54,769 (SD 11,067) Control: CAD 54,773 (SD 10,790) Method of recruitment: selected ECEC centres were contacted, provided with information, and invited to participate in the project. Subsequently, ECEC centre directors were telephoned to answer their questions and to confirm their participation while securing the parents’ board support. Missing data/dropout: 1/61 centres dropped out (intervention); participants lost to follow‐up: 117 Reasons for dropout: change in centre management Characteristics of dropouts: no differences in baseline outcome food intake |
|
| Interventions |
Programme name: Healthy Start‐Départ Santé (HSDS) Number of conditions: 1 intervention, 1 control Intervention duration: 6‐8 months Intervention setting: ECEC Intervention strategies: Ethos and environment ECEC staff Training: staff received 1 x 3‐h on‐site training sessions and were also offered a tailored 90‐min booster session at the midway point of the intervention period. The training session covered best practices in physical activity and healthy eating in early childhood, including topics such as the importance of physical activity and healthy eating for preschoolers, how to easily integrate physical activity and healthy eating in the ECEC’s daily routine, how to introduce and encourage children to try new and healthy foods, and how to help children develop their fundamental movement skills. Service Resources: services received an implementation manual, physical activity and healthy eating manuals, an active play equipment kit and other complementary resources for child‐care staff and families. Monthly newsletters were also sent to services, which included tips on how to get children moving or on how to improve healthy eating. Services were encouraged to share these newsletters with parents. Champion: services encouraged to identify a 'Healthy Star' – a staff member who was a champion for physical activity and healthy eating, and the point of contact for the programme co‐ordinators. Support: ongoing online and telephone support and monitoring. Partnerships Healthcare Delivery: training was delivered by specialists (dietitians, kinesiologists or other experts in the fields of nutrition and physical activity. Intensity of intervention: 3‐h training, ongoing online and telephone support and monitoring and 9‐ min booster session. Intervention delivered by: research team, ECEC staff, healthcare staff Modality: face‐to‐face, telephone, online, written Theoretical basis: not reported Description of control: wait‐list control |
|
| Outcomes |
Outcomes relating to child dietary intake: Fibre intake, fruit and vegetable intake, sodium intake Number of participants analysed: Intervention baseline: 356 Intervention follow‐up: 356 Control baseline: 314 Control follow‐up: 314 Data collection measure: weighed plate waste enhanced with digital photography Data collector: not reported Validity of measures used: validated Outcomes relating to child physical measures: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: Average cost of training, total intervention implementation cost Number of participants analysed: ECEC staff: 893 Trainers: 92 Data collection measure: intervention database and semi‐structured interviews with intervention staff Data collector: researchers Validity of measures used: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: a grant from the Public Health Agency of Canada (# 6282‐15‐2010/3381056‐RSFS), a research grant from the Consortium National de Formation en Santé (# 2014‐CFMF‐01), and a grant from the Heart and Stroke Foundation of Canada (# 2015‐PLNI). AFC was funded through a postdoctoral fellowship from the Saskatchewan Health Research Foundation and SW was funded through a Canadian Institutes of Health Research Charles Best Canada Graduate Scholarships Doctoral Award and a Gérard‐Eugène‐Plante Doctoral Scholarship from the Faculty of Medicine and Health Sciences at the Université de Sherbrooke. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple randomisation was used to allocate ECEC centres to either the intervention or control group with a 1:1 ratio. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Diet outcomes | Unclear risk | While blinding was not possible for the ECEC centres, parents and children were not informed about group assignment. Research assistants responsible for collecting data were not told about the ECEC centre’s group allocation. It is unclear whether lack of blinding would affect the outcome. For example, teachers could have encouraged children to eat more healthy foods on the days of observation, though this is unknown. |
| Blinding of participants and personnel (performance bias) Cost | Unclear risk | Blinding was not possible for the ECEC centres. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | Low risk | Children's dietary intake was measured using weighed plate waste enhanced with digital photography. Research assistants responsible for collecting data were not told of the centre's group allocation. |
| Blinding of outcome assessment (detection bias) Cost | Unclear risk | Blinding was not possible for the ECEC centres. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | High risk | Data were available for 356 (85%) children in the intervention group and 314 (85%) children in the control group at follow‐up. Study authors stated that "We used complete case analysis, such that only participants with complete outcome data were included. This represents a deviation from our original protocol, which planned for analyses to be pursued according to the intention‐to‐treat principle. This modification was necessary as the issue of missing data largely affected outcome variables, and it is generally the norm not to use imputation for missing data among outcome variables, especially when the proportion of missing data is large." Authors also stated that "Although not as susceptible to bias as a per‐protocol analysis, the complete case analyses used are associated with a higher risk that the study groups being compared differ in terms of potentially confounding variables that if the intention‐to‐treat principle were used." As a result, the risk of attrition bias is considered high. |
| Incomplete outcome data (attrition bias) Cost | Unclear risk | The number of participants or services which did not complete outcome follow‐up data for this outcome is unclear. |
| Selective reporting (reporting bias) | High risk | Dietary outcomes were reported for fibre (g), fruit and vegetable servings, and sodium (mg). Registration notes calories, macronutrients, and micronutrients. Anthropometric data not reported here |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Low risk | Children in both groups were similar on all baseline characteristics. |
| Loss of clusters | Low risk | One cluster lost 9 children, but loss was a small percentage (< 5%) of the overall sample. |
| Incorrect analysis | Low risk | Study authors stated that "To account for clustering related to repeated measures and due to the sampling of participants in early childcare centres, variables representing participants and early childcare centres were included as random effects in all models." |
| Contamination | Low risk | Contamination unlikely. Study authors stated that "Following recruitment of one of the childcare centres in the usual practice arm, it was found that it had the same director and shared staff with a nearby early childcare centre which had been recruited in the intervention arm. Given the risk of contamination quasi certain it was decided to amalgamate the 2 centres as one intervention centre." |
| Other bias | Unclear risk | Deviations from protocol noted. Study authors stated that "The study protocol was implemented as planned; however, as detailed in the analysis section, the amount of missing data for the outcomes forced us to modify the analysis plan from an intention‐to‐treat to a complete‐cases analysis approach." There is insufficient information to assess whether an important risk of bias exists. |
Lerner‐Geva 2014.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 4 months Unit of allocation: kindergartens Unit of analysis: child |
|
| Participants |
Service type: centre‐based (kindergartens) Operation: not reported Country (region): Israel (Ra'anaana) Country income classification: high Low‐SES sample: no Population description: Ra’anaana is placed in the second highest rank of socioeconomic clusters of the population. Inclusion criteria: the study population comprised children aged 4–6 years attending full‐day kindergartens in the city of Ra’anaana. Kindergartens considered for inclusion were those that ran a full‐day programme until 16:00 h, which all received lunch from the same catering service and had the same standard of physical exercise of 1 h/week. Exclusion criteria: not reported Number of services randomised: 6 (2 Intervention 1; 2 Intervention 2; 2 control) Number of children randomised: 204 (69 Intervention 1; 67 Intervention 2; 68 control) Characteristics Children Age: Intervention 1: ≤ 4 years, 31.9%; 5‐6 years, 43.5%; ≥ 6 years, 24.6% Intervention 2: ≤ 4 years, 23.9%; 5‐6 years, 43.3%; ≥ 6 years, 32.8% Control: ≤ 4 years, 10.3%; 5‐6 years, 61.8%; ≥ 6 years, 27.9% Gender (% female): Intervention 1: 46.4% Intervention 2: 55.2% Control: 45.5% Ethnicity: Intervention 1: birthplace ‐ Israel: 91.3%; other: 8.7% Intervention 2: birthplace ‐ Israel: 98.5%; other: 1.5% Control: birthplace ‐ Israel: 95.4%; other: 4.6% Parents Age (years): not reported Gender (% female): not reported Ethnicity: Intervention 1: both parents born in Israel, 60.3%; 1 parent born in Israel, 26.5%; both parents born overseas, 13.2% Intervention 2: both parents born in Israel, 73.4%; 1 parent born in Israel, 17.2%; both parents born overseas, 9.4% Control: both parents born in Israel, 64.2%; 1 parent born in Israel, 23.9%; both parents born overseas, 11.0% Parent/family SES: Parent education: intervention 1: both ≥ 13 years, 74.6%; 1 ≥ 13 years, 12.7%; both < 13 years, 12.7% Intervention 2: both ≥ 13 years, 62.7%; 1 ≥ 13 years, 20.3%; both < 13 years, 17.0% Control: both ≥ 13 years, 89.1%; 1 ≥ 13 years,, 24.7%; both < 13 years, 6.2% Method of recruitment: 6 kindergartens were randomly approached to participate in the programme. Missing data/dropout: not reported Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: It Fits Me: adapted for kindergarten children Number of conditions: 2 interventions, 1 control Intervention duration: intervention 1: 4 months; Intervention 2: 10 weeks Intervention setting: ECEC Intervention strategies: Intervention 1: full intervention Health curriculum Children Education: 10 lessons on healthy eating delivered by teachers Ethos and environment Children Exposure: a daily exercise programme (5 d/week) for 30 min in the morning, delivered by a teacher of physical education who had undergone training. ECEC staff Training: teachers were given training by attending lectures where they were familiarised with the materials, in order to facilitate their ability to perform the lessons in their classes. Resources: supporting materials included posters, worksheets, games, colouring‐in sheets and instruction materials for teachers. Families Resources: a summary for parents about each nutrition lesson was provided to reinforce messages. Intervention 2: partial intervention Health curriculum Children Education: 10 lessons on healthy eating delivered by teachers Ethos and environment ECEC staff Training: teachers were given training by attending lectures where they were familiarised with the materials, in order to facilitate their ability to perform the lessons in their classes. Resources: supporting materials included posters, worksheets, games, colouring‐in sheets and instruction materials for teachers. Families Resources: a summary for parents about each nutrition lesson was provided to reinforce messages. Intensity of intervention: Intervention 1: 1 x healthy eating lesson/week for 10 weeks; 30‐min physical activity class daily from March‐June; teachers attended training lecture (frequency and duration not reported) Intervention 2: 1 x healthy eating lesson/week for 10 weeks; teachers attended training lecture (frequency and duration not reported) Intervention delivered by: Intervention 1: research team, ECEC staff Intervention 2: research team, ECEC staff Modality: Intervention 1: face‐to‐face, written Intervention 2: face‐to‐face, written Theoretical basis: not reported Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: Daily energy intake Number of participants analysed: Intervention 1 baseline: 69 Intervention 1 follow‐up: 69 Intervention 2 baseline: 67 Intervention 2 follow‐up: 67 Control baseline: 68 Control follow‐up: 68 Data collection measure: FFQ and 24‐h recall questionnaire Data collector: parents Validity of measures used: validated Outcomes relating to child physical measures: BMI z‐score Number of participants analysed: Intervention 1 baseline: 69 Intervention 1 follow‐up: 69 Intervention 2 baseline: 67 Intervention 2 follow‐up: 67 Control baseline: 68 Control follow‐up: 68 Data collection measure: objectively measured (CDC) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: this research received no specific grant from any funding agency in the public, commercial or not‐for‐profit sector. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported. |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | No clear blinding of participants and personnel to study allocation, and the outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | No clear blinding of participants and personnel to study allocation, however the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Parents reported children's dietary intake via a quantified FFQ outside of school, and a helper completed a structured form to document children's intake during school. Blinding of parents and helpers not reported, and the outcome measurement is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured by a single investigator and the outcome measurements were not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Unclear risk | The number of students available at follow‐up is not reported, so risk of attrition bias is unclear. |
| Incomplete outcome data (attrition bias) Physical outcomes | Unclear risk | The number of students available at follow‐up is not reported, so risk of attrition bias is unclear. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting |
| Recruitment bias | Low risk | Parental consent was obtained at the beginning of the programme. All parents were invited to an information evening at the beginning of the programme, where they received an explanation of the research without knowing to which group their child would be allocated. |
| Baseline imbalance | Low risk | Baseline differences between groups were found for age of children, parents' education, and religious level. Analysis accounted for these differences |
| Loss of clusters | Unclear risk | Not reported |
| Incorrect analysis | Low risk | Study authors stated that "Each model included fixed effects: baseline measures, age, parents' education, religious status, study group and random effect of kindergarten and child." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Lumeng 2017.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 6 months Unit of allocation: classrooms Unit of analysis: child |
|
| Participants |
Service type: centre‐based (Head Start) Operation: federally‐funded Country (region): USA (Michigan) Country income classification: high Low‐SES sample: yes Population description: urban and rural Inclusion criteria: inclusion criteria are that the child is aged 3 or 4 years at study enrolment. Exclusion criteria: exclusions were significant developmental disabilities that would preclude participation, child is a foster child, or parent is non‐English speaking. Number of services randomised: 3 Head Start agencies, 18 classrooms (6 Intervention 1; 6 Intervention 2; 6 control) Number of children randomised: 697 (224 Intervention 1; 255 Intervention 2; 218 control) Characteristics Children Age: Intervention 1: 4.10 years (SD 0.52) Intervention 2: 4.12 years (SD 0.52) Control: 4.12 (SD 0.53) Gender (% female): Intervention 1: 49.1% Intervention 2: 51.4% Control: 53.7%; Ethnicity: Intervention 1: white, non‐Hispanic: 35.9%; African American, non‐Hispanic: 39%; Hispanic/other: 25.1% Intervention 2: white, non‐Hispanic: 56.4%; African American, non‐Hispanic: 27%; Hispanic/other: 16.7% Control: white, non‐Hispanic: 52.1%; Hispanic/other: 24.9% Parents Age (years): Intervention 1: 29.8 (SD 6.8) Intervention 2: 29.6 (SD 6.7) Control: 29.2 (SD 12.2) Gender (% female): not reported Ethnicity: Intervention 1: white: 46%; African American, non‐Hispanic: 38.7%; Hispanic or other: 15.3% Intervention 2: white: 63.1%; African American, non‐Hispanic: 26.7%; Hispanic or other: 10.2% Control: white: 63.6%; African American, non‐Hispanic: 23%; Hispanic or other: 13.4% Parent/family SES: Family income‐to‐needs ratio Intervention 1: 0.84 (SD 0.53) Intervention 2: 0.84 (SD 0.56) Control: 0.88 (SD 0.53) Caregiver education Intervention 1: < high school: 17.1%; high school diploma or GED: 32.4%; some college courses but no degree: 40.1%; 2‐year college degree: 6.3%; ≥ 4‐year college degree: 4.1% Intervention 2: < high school: 14.7%; high school diploma or GED: 31%; some college courses but no degree: 39.3%; 2‐year college degree: 11.1%; ≥ 4‐year college degree: 4% Control: < high school: 14.3%; high school diploma or GED: 35.5%; some college courses but no degree: 33.6%; 2‐year college degree: 12.9%; ≥ 4‐year college degree: 3.7% Method of recruitment: families were told about the study during classroom open houses and through flyers in children’s backpacks, and compensated for returning an initial enrolment packet, including a signed written informed consent form. They were then contacted by telephone to review eligibility criteria that they reported in the enrolment packet and to confirm complete understanding of the study and validate informed consent. Missing data/dropout: Intervention 1: 21 lost to follow‐up, 2 discontinued intervention; Intervention 2: 18 lost to follow‐up, 2 discontinued intervention, 1 no longer eligible; Control: 11 lost to follow‐up, 3 discontinued intervention, 1 was no longer eligible Reasons for dropout: Intervention 1: 21 lost to follow‐up, 2 discontinued intervention; Intervention 2: 18 lost to follow‐up, 2 discontinued intervention, 1 no longer eligible; Control: 11 lost to follow‐up, 3 discontinued intervention, 1 was no longer eligible Characteristics of dropouts: not reported |
|
| Interventions |
1Programme name: The Growing Healthy Study Number of conditions: 2 interventions, 1 control Intervention duration: 4 x 1 school year Intervention setting: ECEC and home Intervention strategies: Intervention 1: Preschool Obesity Prevention Series (POPS) Health curriculum Children Education: 6 lessons delivered over 12 weeks by the Head Start teacher and Extension Educators (trained master's level nutrition educator), using children's stories with embedded obesity prevention themes related to behavioural goals (e.g. more fruit and vegetable consumption; less screen time) Ethos and environment Children Exposure: activities include classroom cooking experiences, games/activities associated with story themes, and goal setting. ECEC staff Training: training for Head Start. Training covers curriculum specifics as well as strategies for promoting parent self‐efficacy for behaviour change and importance of fidelity. Booster: booster training was provided each year. Support: phone support from trainers was available as needed. Partnerships Families Education: 8 x 75‐min lessons to develop and practice skills and a discussion of strategies to overcome challenges and problem‐solving techniques, with an emphasis on building knowledge and self‐efficacy about preventing childhood obesity. Recipes are included in each lesson. Exposure: hands‐on activities are included in each lesson. Support: reinforcing telephone contacts after every other lesson. 'Family Links' and 'Parent Pages' are sent home to reinforce content from school to home. Transportation and child care provided for parents to attend activities, as needed. Healthcare Delivery: a trained Master's‐level nutrition educator delivered parent education. Training: nutrition educators received 2‐d training (with booster sessions each year). Support: phone support from trainers was also available as needed. Intervention 2: POPS + Incredible Years Series (IYS) Health curriculum Children Education: 6 lessons delivered over 12 weeks by the Head Start teacher and Extension Educators, using children's stories with embedded obesity prevention themes related to behavioural goals (e.g. more fruit and vegetable consumption; less screen time). 60 x 15–20 min lessons delivered throughout the year during "Circle Time" in Head Start classrooms, followed by small group activities. Lessons address self‐regulation skills, problem solving strategies, and prosocial behaviour, and use child‐size puppets to teach skills and engage children. IYS child lessons were delivered by Master’s‐level mental health specialists, and Head Start teachers direct small group activities after each lesson. Ethos and environment Children Exposure: activities include classroom cooking experiences, games/activities associated with story themes, and goal setting. ECEC staff Training: training for Head Start. Training covers curriculum specifics as well as strategies for promoting parent self‐efficacy for behaviour change and importance of fidelity. Teachers also received training in classroom management strategies (e.g. handling transitions effectively) and were mentored by Master’s‐level mental health specialists in delivering IYS‐Child, so that delivery can slowly progress from delivery by mental health specialist, to co‐delivery by mental health specialist and teacher, to sole delivery by the teacher over time. Booster: booster training was provided each year. Support: phone support from trainers was also available as needed. Partnerships Families Education: 8 x 75‐min lessons to develop and practice skills and a discussion of strategies to overcome challenges and problem‐solving techniques, with an emphasis on building knowledge and self‐efficacy about preventing childhood obesity. Recipes are included in each lesson. 12–14 x 2‐h lessons focusing on parenting skills such as using effective praise, incentives, limit‐setting, and handling misbehaviour. Concepts are discussed using video vignettes about parenting challenges. Exposure: hands‐on activities are included in each lesson. Materials: homework Support: follow‐up phone calls. "Family Links" and "Parent Pages" are sent home to reinforce content from school to home. Transportation and child care provided for parents to attend activities, as needed. Healthcare Delivery: a trained Master's‐level nutrition educator delivered parent education. Training: nutrition educators received 2‐d training. The Master's‐level trained mental health specialists received training in classroom management strategies (e.g. handling transitions effectively). Booster: booster training was provided each year. Support: phone support from trainers was also available as needed. Master's level trained mental health specialists communicated extensively to share ideas and co‐ordinate efforts across sites, and received monthly supervision from IYS trainers about their delivery of IYS components, and consultation as needed. Master's‐trained mental health specialists also worked with teachers within their own site to develop lesson plans and small group activities. Intensity of intervention: Intervention 1: 8 x 75‐min weekly parent lessons with telephone follow‐ups every other lesson; 6 lessons for children over 12 weeks; 2 h of training for Head Start teachers; phone support as needed; 2 d of training for Extension educator Intervention 2: 8 x 75‐min weekly parents lessons with telephone follow‐ups every other lesson; 6 x 15‐20‐min lessons for children followed by small group activities; 2 h of training for Head Start teachers and phone support as needed; 2 h/week parent lessons with homework and follow‐up calls; 2 d of training for Extension educator Intervention delivered by: Intervention 1: research team, ECEC staff, healthcare staff Intervention 2: research team, ECEC staff, healthcare staff Modality: Intervention 1: face‐to‐face, telephone, written Intervention 2: face‐to‐face, telephone, written Theoretical basis: POPS is based on social cognitive theory Description of control: usual Head Start curriculum and support |
|
| Outcomes |
Outcomes relating to child dietary intake: Vegetable intake, 100% fruit juice intake, sugar‐sweetened beverages intake, whole fruit intake Number of participants analysed: Intervention 1 baseline: 224 Intervention 1 follow‐up: 224 Intervention 2 baseline: 255 Intervention 2 follow‐up: 255 Control baseline: 218 Control follow‐up: 218 Data collection measure: 24 h diet recalls and observation Data collector: parent and researcher Validity of measures used: not reported Outcomes relating to child physical measures: Overweight, obese, normal weight, underweight, BMI z‐score Number of participants analysed: Intervention 1 baseline: 84‐220 Intervention 1 follow‐up: 82‐195 Intervention 2 baseline: 82‐250 Intervention 2 follow‐up: 82‐230 Control baseline: 68‐213 Control follow‐up: 68‐200 Data collection measure: objectively measured (CDC) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: USDA/National Institute of Food and Agriculture/Agriculture and Food Research Initiative grant 2011‐68001‐30089 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Study authors stated that "The 6 teaching teams (hereafter referred to as “classrooms”) within each agency were randomly assigned by using an automated system overseen by the study statistician to 1 of 3 study arms, with the limitation that each agency have 2 classrooms allocated per study arm and that the classrooms were located in different communities to prevent cross contamination." |
| Allocation concealment (selection bias) | Unclear risk | Centres appear to be randomised prior to data collection, however it is unclear if families could potentially know allocation prior to recruitment. Study authors stated that "Families were assigned to a study arm as a function of their classroom assignment, which was based on the location geographically closest to their home address." |
| Blinding of participants and personnel (performance bias) Diet outcomes | Unclear risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were aware of their study allocation (intervention or control). However, the protocol states that "Only one classroom participates per physical school site to prevent cross‐contamination across study arms and ensure that participants are blind to group assignments." It is unclear whether the blinding of participants could have been broken or whether the lack of blinding would affect the outcome. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | Although protocol states that "Only one classroom participates per physical school site to prevent cross‐contamination across study arms and ensure that participants are blind to group assignments," we assumed that due to the nature of the intervention, ECEC service staff, study personnel delivering the intervention, and parents were aware of their study allocation (intervention or control). However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | Unclear risk | Parents reported children's dietary intake via multiple 24‐h recalls conducted by trained dietitians who were blinded to study arm. Although protocol states that "Only one classroom participates per physical school site to prevent cross‐contamination across study arms and ensure that participants are blind to group assignments," due to the nature of the intervention, parents may have been aware that they were assigned to an intervention. The outcome measurement is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Study authors stated that "Data collectors and interventionists did not interact, and data collectors were blinded to study arm." |
| Incomplete outcome data (attrition bias) Diet outcomes | Low risk | Follow‐up data were available for 201 (90%) children in the Head Start (HS) + POPS group, 234 (92%) children in the HS + POPS + IYS group, and 203 (93%) children in the HS only (control) group. < 20% of participants dropped out with similar numbers across groups. ITT analyses were also used also. Therefore, risk of attrition bias was considered to be low. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Follow‐up data were available for 201 (90%) children in the HS + POPS group, 234 (92%) children in the HS + POPS + IYS group, and 203 (93%) children in the HS only (control) group. < 20% of participants dropped out with similar numbers across groups. ITT analyses were also used also. Therefore, risk of attrition bias was considered to be low. |
| Selective reporting (reporting bias) | Unclear risk | Study authors stated that "research staff trained in dietary recall methods observed each meal and snack at school and recorded each child's intake; these data were incorporated into the recall." However, this procedure was not specified in the protocol. |
| Recruitment bias | Low risk | Individuals were recruited and enrolled prior to cluster randomisation. |
| Baseline imbalance | Low risk | Participant characteristics at the time of allocation were similar except for child race/ethnicity. This was accounted for in the analyses. |
| Loss of clusters | Low risk | No reported loss of clusters, with small numbers of children lost to follow‐up. |
| Incorrect analysis | Low risk | Study authors stated that "Mixed models were used to account for having repeated measures (pre and post) as well as for clustering of children within a classroom." |
| Contamination | Low risk | Study authors stated that "The 6 teaching teams (hereafter referred to as “classrooms”) within each agency were randomly assigned by using an automated system overseen by the study statistician to 1 of 3 study arms, with the limitation that each agency have 2 classrooms allocated per study arm and that the classrooms were located in different communities to prevent cross‐contamination." |
| Other bias | Low risk | No clear other source of bias |
Morris 2018.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 3 months Unit of allocation: kindergartens Unit of analysis: child |
|
| Participants |
Service type: centre‐based (Early Childhood Management Services‐run kindergartens) Operation: not reported Country (region): Australia (Melbourne) Country income classification: high Low‐SES sample: no Population description: not reported Inclusion criteria: sessional kindergartens Exclusion criteria: not reported Number of services randomised: 25 teachers (14 intervention, 11 control) Number of children randomised: 300 (168 intervention, 132 control) Characteristics Children Age: Intervention: 4.76 years (SD: 0.36) Control: 4.68 years (SD: 0.37) Gender (% female): not reported Ethnicity: Intervention: born in Australia: 90.6%; not born in Australia: 9.4% Control: born in Australia: 94.6%; not born in Australia: 5.4% Parents Age (years): Intervention: mother: 35.15 (SD 4.92); father: 38.32 (SD 5.69) Control: 35.32 (SD 4.93); fathers: 37.29 (5.31) Gender (% female): not reported Ethnicity: Mothers: Intervention: born in Australia: 72.4% (intervention); not born in Australia: 27.6% Control: born in Australia: 70.3%; not born in Australia: 29.7% Fathers: Intervention: born in Australia: 74.8%; not born in Australia: 24.4% Control: born in Australia: 61.8%; not born in Australia: 36.4% Parent/family SES: Combined family income Intervention: low < AUD 25,000‐65,000: 28.1%; medium AUD 65,001‐105,000: 31.4%; ; high AUD 105,001‐145,000: 40.5% Control: low < AUD 25,000‐65,000: 27.4%; medium AUD 65,001‐105,000: 29.2%; high AUD 105,001‐145,000: 43.4% Mothers' education Intervention: high school only: intervention 29.5%; vocation/technical: intervention 13.1%; all university: 49.2% Control: high school only: 33.7%; vocation/technical: 5.8%; all university: 51.9% Fathers' education Intervention: high school only: 35.5%; vocation/technical: 21.5%; all university: 37.2% Control: high school only: 40.6%; vocation/technical: 20.8%; all university: 34.6% Method of recruitment: all eligible parents of children were personally invited to participate by the researchers at the kindergarten service. Parents initiated their child’s participation. Missing data/dropout: not reported Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: not reported Number of conditions: 1 intervention, 1 control Intervention duration: 8 weeks Intervention setting: ECEC Intervention strategies: Health curriculum Children Education: teachers implemented their planned play‐based learning experiences over a period of 8 weeks. Ethos and environment ECEC staff Training: session 1 ‐ All teachers (intervention and control) attended a professional learning session (delivered by research group) to explain the project. They also considered a case study detailing a preschool‐aged child’s interest in digital media and popular culture characters. Waitlist control teachers then departed the session. The remaining intervention group teachers brainstormed a series of play‐based learning experiences, connecting well‐being and sustainability knowledge to the case study‐child’s interests. Session 2 ‐ Intervention teachers only attended a second professional learning session. The session started with a seminar detailing content knowledge about well‐being and sustainability appropriate for young children (topics were physical activity, healthy eating, healthy lifestyles, and natural environments). This was followed by a discussion and workshop of teacher's play‐based learning experience. Resources: teachers were provided with: professional learning materials, namely a Pedagogical Communication Strategy and details of different play types (e.g. open‐ended, modelled and purposefully framed play) used to build children’s knowledge about well‐being and sustainability; a visual‐arts diary to record their planned play‐based learning experiences and observation/assessment of the implemented experiences using their normal methods; and, a book detailing the use of the 3 play‐types in the provision of early childhood environmental education. Teachers had access to a purpose‐designed website containing copies of all project materials. Support: teachers were provided with an implementation protocol and the phone and email contact details of researchers. Intensity of intervention: 2 x professional learning sessions; at least 2 x play based learning experiences implemented each week for children Intervention delivered by: research team, ECEC staff Modality: face‐to‐face, online, written Theoretical basis: Funds of Knowledge Description of control: wait‐list control, plus teachers attended 1 professional learning session |
|
| Outcomes |
Outcomes relating to child dietary intake: Total unhealthy food (e.g. packaged snack foods, confectionary and cakes) intake, fruit and vegetable intake, unsweetened drinks intake, sweetened drink intake, vegetable intake, usual vegetables intake, fruit intake, packaged snacks intake Number of participants analysed: Intervention baseline: 89‐102 Intervention follow‐up: 89‐102 Control baseline: 81‐101 Control follow‐up: 81‐101 Data collection measure: Eating and Physical Activity questionnaire (EPAQ) Data collector: parent Validity of measures used: validated Outcomes relating to child physical measures: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An uninvolved researcher used a computer algorithm to complete random permutations of 1 for intervention and 2 for waitlist control |
| Allocation concealment (selection bias) | Low risk | While the group allocation could not be concealed from the ECEC teachers, it was concealed from the parents and data collection researchers. |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | No blinding of teachers, and although allocation was concealed from the parents, it is likely that the blinding could have been broken. The outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Parents reported children's dietary intake. Although the group allocation was concealed from parents, it is likely that the blinding could have been broken and the outcome measurement is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Unclear risk | Study authors stated that "Almost three quarters of the parents (n = 187; 72.2 per cent) returned EPAQ surveys at all three timepoints, and 14 per cent did not return any EPAQ surveys." No information is provided as to whether missing data and reasons for missing data were similar across groups. Study authors stated that "Multiple imputation of the EPAQ data was used to address missing values." Risk of attrition bias is unclear. |
| Selective reporting (reporting bias) | Unclear risk | The protocol states that the Eating and Physical Activity Questionnaire will be used to measure dietary outcomes, however the outcomes of interest are not specifically reported. |
| Recruitment bias | Low risk | Group allocation was concealed from parents so it is likely that individuals consented to the study without knowing allocation. |
| Baseline imbalance | Low risk | Study authors state that "No significant differences were seen between age, gender, country of birth or BMI in the intervention group and waitlist control group." ANOVA calculations found only one significant demographic characteristic difference between the means of fathers' height in each group. |
| Loss of clusters | Unclear risk | Not reported |
| Incorrect analysis | High risk | There was no accounting for clustering of children within kindergartens. |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | High risk | No funding statement was provided. No conflict of interest statement was reported. |
Namenek Brouwer 2013.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 4 months Unit of allocation: centre Unit of analysis: centre |
|
| Participants |
Service type: centre‐based (licensed) Operation: not reported Country (region): USA (North Carolina) Country income classification: high Low‐SES sample: unclear Population description: not reported Inclusion criteria: to participate in the study, centres had to provide all foods and beverages to children in care (i.e. parents could not send food from home), not have an open case of abuse or neglect with the state licensing agency, and have at least 3 children between the ages of 3 and 5 years in care on a regular basis. Exclusion criteria: not reported Number of services randomised: 4 (2 interventions, 2 control) Number of children randomised: not reported (3 children from each classroom randomly selected for dietary outcome assessment) Characteristics Children Age: 3‐5 years Gender (% female): not reported Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported ECEC staff Age (years): not reported Gender (% female): 100% Ethnicity: African American: 75% Service/ECEC staff SES: not reported Method of recruitment: a letter of invitation was mailed to every licensed centre (n = 6) in the city limits of a small community near the researchers' offices. The letter was followed by a telephone call from the study team. The first 4 centres that agreed to participate were enrolled. Centre directors provided written informed consent to participate in the study; parents were provided a fact sheet describing the study and were asked to contact the project director if they did not want their children observed during the dietary assessment. Missing data/dropout: not reported Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Watch Me Grow Number of conditions: 1 intervention, 1 control Intervention duration: 4 months Intervention setting: ECEC Intervention strategies: Health curriculum Children Education: the programme included a "crop‐a‐month" structured curriculum highlighting the garden's targeted crop each month (lettuce, strawberries, spinach and broccoli). Ethos and environment Children Menu modification: garden produce was integrated onto service menu and children were provided taste testing activities. Centres were supported to increase the number and nutritional quality of vegetables and fruits provided to children in care, beyond what the garden would produce. Activities: providers and children grew: lettuce, strawberries, spinach and broccoli. Activities included reading, gardening, taste testing and songs. ECEC staff Education: the curriculum included an overview module, followed by monthly modules designed around a specific crop. Each month, the health educator described 4 discrete activities included in each module so that centre staff could deliver the activities to the children approximately weekly. Staff were encouraged to act as positive role models. Support: monthly technical assistance from a health educator to teachers. Email support for garden maintenance. Monthly visits to the provider at the centre who was directly responsible for food purchasing and menu planning. These visits were to help centres explore low‐cost, sustainable ways to increase the number and nutritional quality of vegetables and fruits provided to children in care. Service Environment: an 8′ × 4′ (approximately 2.5 m x 1.2 m) raised bed outdoor garden was installed at all intervention services. Resources: intervention classrooms received corresponding curriculum materials (including an existing published children’s book) highlighting the target fruit or vegetable of the month. The study provided all garden supplies, including plants, watering cans, brackets, and materials for the raised garden bed. Support: monthly consultation by a gardener Partnerships Families Event: 1‐h early spring kick‐off event at each intervention service. Parents and other family members, providers, and children were invited to help plant the gardens. Healthcare Support: a health educator met monthly with the provider at the centre who was directly responsible for food purchasing and menu planning. The intent was to help centres explore low‐cost, sustainable ways to increase the number and nutritional quality of vegetables and fruits provided to children in care, beyond what the garden would produce. Intensity of intervention: 1 x crop/month (with related class materials); 1 x installed garden in an appropriate location (plus gardening supplies, plus gardening expertise); 1‐h early spring kick‐off event; curriculum included overview modules, monthly module, 4 x activities provided to children weekly Intervention delivered by: research team, ECEC staff, healthcare staff Modality: face‐to‐face, written Theoretical basis: not reported Description of control: wait‐list control |
|
| Outcomes |
Outcomes relating to child dietary intake: Fruit intake, vegetable intake, dark vegetable intake, white potato intake Number of participants analysed: Intervention baseline: 6 Intervention follow‐up: 6 Control baseline: 6 Control follow‐up: 6 Data collection measure: in‐care observation Data collector: trained registered dietitian Validity of measures used: validated Outcomes relating to child physical measures: not reported Outcome relating to child cognitive performance: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Following baseline data collection, centres were randomised via a simple randomisation scheme (randomisation without restriction) to either the intervention or control condition in a 1:1 ratio, using the Research Randomizer (http://www.randomizer.org/form.htm). |
| Allocation concealment (selection bias) | Low risk | Baseline data collected before centres were allocated to groups |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | Teachers were aware of allocation and may have encouraged children to eat more fruits and vegetables on the days of diet observation. |
| Blinding of outcome assessment (detection bias) Diet outcomes | Low risk | Children's dietary intake was observed by a trained Registered Dietitian who was blinded to treatment group. |
| Incomplete outcome data (attrition bias) Diet outcomes | Unclear risk | There is no information regarding the number of participants at baseline or follow‐up. It is also unknown if the children observed at baseline were the same as those observed at follow‐up. Risk of attrition bias is unclear. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting |
| Recruitment bias | Low risk | Individual recruitment and child consent (opt‐out) to participate occurred before randomisation of clusters. |
| Baseline imbalance | Unclear risk | No baseline details on children provided; only details on the ECEC included |
| Loss of clusters | Low risk | Only 3 students were observed pre‐ and post‐interventions. Appears no ECEC was lost to follow‐up |
| Incorrect analysis | High risk | There was no accounting for clustering of children within centres. |
| Contamination | Unclear risk | All 4 centres were located within the city limits of a small community near the researchers' offices. Only 2 other centres existed in that community that were not chosen to participate. It is possible that ECEC staff from an intervention centre started working at a control centre, or for a child attending an intervention centre to switch to a control centre. However, there is not enough information provided to assess whether contamination exists. |
| Other bias | High risk | Study authors stated that “we randomly selected a classroom and then three children within that classroom for dietary observation at intervention and control centres before and after the intervention.” No further information is provided as to how classrooms and children were chosen. It is possible that choices were made in a biased way. No funding statement was provided. |
Natale 2014a.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 3 months Unit of allocation: centre Unit of analysis: child |
|
| Participants |
Service type: centre‐based Operation: subsidised Country (region): USA (Miami‐Dade County, Florida) Country income classification: high Low‐SES sample: yes Population description: Miami‐Dade County, Florida, is one of the only counties in the USA that is 'minority majority': 64% of its residents identify as Hispanic, and 20% as African American. Over 51% of its 2.3 million residents were born outside the USA (138 countries identified). Nearly a quarter of the population is younger than 18 years, > 15% of the school‐aged population has limited English proficiency (Spanish and Haitian Creole as their primary languages), the graduation rate is only 45%, and 22% of young adults have limited literacy skills. Rates of obesity are higher among ethnic‐minority children in Miami‐Dade County, compared with ethnic‐minority children nationally (31% vs 26%, respectively). In addition, there are more than 1400 child‐care centres in the county serving over 20,000 children; 18% live below the poverty line. Inclusion criteria: centres' study inclusion criteria consisted of (a) serve > 30 children, (b) serve low‐income children, and (c) ethnic make‐up had to be reflective of the county as a whole (minority majority). Low income was determined based on whether or not the child received subsidised child care. Exclusion criteria: not reported Number of services randomised: 8 (6 intervention, 2 control) Number of children randomised: 307 (238 intervention, 69 control) Characteristics Children Age: Intervention: 2 years: 14.3%; 3 years: 35.7%; 4 years: 36.6%; 5 years: 13.5% Control: 2 years: 29%; 3 years: 33.3%; 4 years: 31.9%; 5 years: 5.8% Gender (% female): Intervention: 49.2% Control: 47.8% Ethnicity: Intervention: Hispanic/other: 35.7%; Hispanic/Cuban: 24%; African American: 19.3%; Hispanic/Puerto Rican: 3.8%; Haitian: 1.3%; Hispanic/Mexican: 2.1%; other Caribbean black: 2.5%; white: 0.8%; other: 4.2%; unknown: 6.3% Control: Hispanic/other: 20.3%; Hispanic/Cuban: 27.5%; African American: 30.4%; Hispanic/Puerto Rican: 1.5%; Haitian: 7.5%; Hispanic/Mexican: 1.4%; other Caribbean black: 0%; white: 4.4%; other: 1.5%; unknown: 5.8% Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported Method of recruitment: all participants were recruited at the child‐care centre. Parents were approached during drop‐off or pick‐up times. Missing data/dropout: attrition rates were calculated based on available data for child BMI as well as parent measures for each of the time points. At baseline, there were 318 child and parent dyads; at 6 months, there were 239 child and parent dyads; and at 1 year, there were 185 parent and child dyads Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Healthy Inside ‐ Healthy Outside (HI‐HO) program Number of conditions: 1 intervention, 1 control Intervention duration: 6 months Intervention setting: ECEC and home Intervention strategies: Health curriculum Children Education: the 6‐month intervention presented a developmentally, culturally, and linguistically appropriate curriculum that targets preschoolers. Ethos and environment ECEC staff Training: 2 x training sessions. Teachers and staff were trained on the role and rationale of the Hip Hop to Health Jr. programme, taught implementation strategies, and provided lessons to use with the children. Support: weekly technical assistance visits with the teachers and a Hip Hop to Health specialist to ensure the implementation of a low‐fat, high‐fibre diet that included more fruits and vegetables with an emphasis on cultural barriers. Service Policy: the development of policies to increase physical activity and healthy eating Menu modification: a nutritionist worked with each ECEC centre to modify menus to improve the health profile, make them compliant with the policies, and also to ensure that the USDA nutritional requirements were met. All participants Cultural: the programme was designed to be culturally sensitive, given the ethnic diversity of the families, teachers, and administrators and staff at participating schools. Partnerships Families Education: the parent curriculum was modelled after a modified version of the Eating Right Is Basic and Hip‐Hop to Health Jr. programmes. Monthly educational dinner in which nutrition and physical activity were discussed. Sessions were provided by registered dietitians who were of the same cultural background as the parents. Resources: monthly newsletters, and at‐home activities. For each of the 6 x at‐home activities that each family completed, they received a healthy snack bag. At the end of the programme, parents who attended ≥ 3 dinners received a certificate of completion. Healthcare Delivery: a nutritionist assisted centres in menu modification. Intensity of intervention: Teacher component: 2 x training sessions/centre; monthly educational parent dinner; monthly parent newsletters; monthly at‐home activities; each centre agreed on a drink policy; a snack policy and physical activity policy. Intervention delivered by: research team, ECEC staff, healthcare staff Modality: face‐to‐face, written Theoretical basis: Socio‐Ecological Model Framework Description of control: alternative intervention control (safety education) |
|
| Outcomes |
Outcomes relating to child dietary intake: not reported Outcomes relating to child anthropometric measures: Weight z‐score, BMI z‐score Number of participants analysed: not reported Data collection measure: objectively measured (CDC) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: Miami‐Dade County Children’s Trust (grant number 764‐287) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | No clear blinding of participants and personnel to study allocation, however the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured by the research assistants and are not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Physical outcomes | High risk | Data were available for 239 (75%) of child‐parent dyads at 6‐month follow‐up and 185 (58%) dyads at 1‐year follow‐up. Distribution of loss not provided, and reasons for loss not reported. Due to the magnitude of missing data over the short‐term and long‐term follow‐up, the risk of bias was assessed as high. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Unclear risk | Differences noted, however there is no report on whether these were statistically significant. Models included age in months, race, and gender as potential confounders. Ethnicity was not controlled for in the models yet there appears to be baseline differences between groups. |
| Loss of clusters | High risk | Study authors stated that there was an "unexpected closure of a control centre." There were only 2 control centres, so this may be a large proportion of controls. |
| Incorrect analysis | High risk | There was no accounting for clustering of children within centres. |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Unclear risk | No conflict of interest statement was reported. |
Natale 2014b.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 1 school year (varies with outcomes) Unit of allocation: centre Unit of analysis: child |
|
| Participants |
Service type: centre‐based Operation: part of the USDA food program and SNAP‐eligible Country (region): USA (Miami‐Dade County, Florida) Country income classification: high Low‐SES sample: yes Population description: low income, ethnically diverse Inclusion criteria: to be included in the randomisation process, centres met the following inclusion criteria: (1) have 30 children ages 2‐5 years enrolled, (2) serve low‐income families, (3) be part of the USDA food program and SNAP (Supplemental Nutrition Assistance Program)‐eligible, (4) reflect the ethnic distribution of the Miami‐Dade County Public School System (63% Hispanic, 19% African‐American, and 18% white), and (5) centre directors agree to participate and sign a letter of commitment as evidence of such. Exclusion criteria: not reported Number of services randomised: 28 (12 intervention, 16 control) Number of children randomised: 1224 (767 intervention, 457 control) Characteristics Children Age: 46.72 months (SD 11.18) Gender (% female): 50.12% Ethnicity: Hispanic (Cuban): 15.35%; other Hispanic: 40.96%; non‐Hispanic black (Haitian): 14.12%; other non‐Hispanic Black: 19.02%; non‐Hispanic white: 6.69%; other: 3.86% Parents Age (years): 18‐24: 15.05%; 25‐30: 37.19%; 31‐40: 37.99%; 41‐50: 8.57%; 51+: 1.2% Gender (% female): 90% Ethnicity: Hispanic (Cuban): 15.35%; other Hispanic: 40.96%; non‐Hispanic black (Haitian): 14.12%; other non‐Hispanic black: 19.02%; non‐Hispanic white: 6.69%; other: 3.86% Parent/family SES: Level of education: < 12th grade: 35.19%; completed high school or equivalency: 52.02%; completed education beyond high school: 12.79% Method of recruitment: not reported Missing data/dropout: not reported Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Healthy Caregivers‐Healthy Children Number of conditions: 1 intervention, 1 control Intervention duration: 6‐10 months Intervention setting: ECEC Intervention strategies: Health curriculum Children Education: weekly lesson plans were designed to incorporate and reinforce the policy standards (drink policy, snack policy, physical activity policy and screen‐time policy) Ethos and environment Children Role modelling: by means of role modelling, parents and teachers were encouraged to implement change at the family/home and ECEC centre level. Cultural: curriculum is available in both English and Spanish, with culturally sensitive language and activities. ECEC staff Education: 6 x monthly nutritional gatekeeper training (along with parents) using evidence‐based nutrition and physical activity curriculum Meetings: parent‐teacher meetings conducted by research staff that focused on an evidence‐based nutrition and physical activity curriculum. Support: teachers were provided with lesson plans and received weekly technical assistance instruction by curriculum specialists on how to promote wellness within a group’s child‐care setting. Role modelling: nutrition professionals served as role models for the teachers and parents. Service Policy: development of a centre policy for dietary requirements for meals and snacks, drinks, physical activity and screen time. Partnerships Families Education: 6 x monthly nutritional gatekeeper training (along with teachers) using evidence‐based nutrition and physical activity curriculum. Healthcare Support: nutrition professionals served as role models for the teachers and parents. Intensity of intervention: 29 weeks of teacher curriculum technical sessions; 6 x monthly teacher‐parent role‐modelling training; parent‐teacher meetings (frequency and duration not reported) Intervention delivered by: research team, ECEC staff, healthcare staff Modality: face‐to‐face, written Theoretical basis: Reach Effective Adoption Implementation and Maintenance Framework Description of control: alternative intervention control (safety education) |
|
| Outcomes |
Outcomes relating to child dietary intake: Vegetable intake, fruit intake, fried intake, fast food intake, snack food intake, soda intake, fruits and vegetables intake, junk food intake Number of participants analysed: Intervention baseline: 767 Intervention follow‐up: 767 Control baseline: 457 Control follow‐up: 767 Data collection measure: Healthy Kids Checklist Data collector: parent/caregiver Validity of measures used: validated Outcomes relating to child physical measures: BMI percentile, healthy BMI percentile, unhealthy BMI percentile Number of participants analysed: Intervention baseline: 767 Intervention follow‐up: 767 Control baseline: 457 Control follow‐up: 457 Data collection measure: objectively measured (CDC) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: Total costs, resource costs, projected lifetime savings Number of participants analysed (intervention group only): Services: 12 Children: approximately 1200 Data collection measure: detailed staffing and financial records Data collector: researcher Validity of measures used: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: The USDA (Grant number: AFRI/NRI‐2009–0506, RCT, registration number: NCT017220321) and USDA NRI/AFRI Grant # 2009‐05065 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | A random number table was used to randomly assign 28 centres to intervention or control. However, an additional 4 centres were added to the control arm due to low enrolment at the centres. These additional centres do not appear to have been randomly chosen or assigned. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported. |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. The outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | No clear blinding of participants and personnel to study allocation, however the outcome is not likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Cost | Low risk | No clear blinding of participants and personnel to study allocation, however due to measures used for data collection, the outcome is unlikely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Parents reported children's dietary intake via questionnaire. Blinding of parents was not possible and the outcome measurement is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured by trained staff and were not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Cost | Low risk | No clear blinding of participants and personnel to study allocation, however due to measures used for data collection, the outcome is unlikely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Unclear risk | The number of children available at follow‐up is not reported. Risk of attrition bias is unclear. |
| Incomplete outcome data (attrition bias) Physical outcomes | Unclear risk | The number of children available at follow‐up is not reported. Risk of attrition bias is unclear. |
| Incomplete outcome data (attrition bias) Cost | Low risk | Data were calculated based on all participating services. |
| Selective reporting (reporting bias) | Unclear risk | Reporting of dietary components in the protocol is unclear. Protocol also includes waist circumference, which is not reported. |
| Recruitment bias | High risk | Sample sizes differ between protocol and manuscript, suggesting individual recruitment after randomisation. |
| Baseline imbalance | Unclear risk | There were significant baseline differences between the treatment and control groups, where the treatment group started at a higher consumption of fruits and vegetables, making interpretation of these changes difficult. Therefore, models with the child Consumption of Fruit/Vegetables used the change of child Consumption of Fruit/Vegetables from Time 1 to Time 2 as the outcome measure, and baseline Consumption of Fruit/Vegetables was included as a covariate. There were several caregiver demographic differences by group that were not accounted for in analysis (e.g. caregiver languages spoken at home, caregiver level of education, birthplace of caregiver, etc.), though there is no statistical analysis to determine if differences are significant. |
| Loss of clusters | Unclear risk | Not reported |
| Incorrect analysis | Low risk | Study authors stated that "A random effect was included to measure the variation of schools nested in treatment groups. In the models including teacher factor scores, another random term was included for the clustering effect of teachers (classrooms) nested within schools." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Natale 2021.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT (this study reported on a comparison of 2 RCTs that included different samples. As Phase 1 (RCT 1) is reported in Natale 2014b, only Phase 2 (RCT 2) is reported for Natale 2021 (i.e. treated as a singular RCT) Length of follow‐up from baseline: 10 months Unit of allocation: centre Unit of analysis: centre |
|
| Participants |
Service type: centre‐based Operation: not reported Country (region): USA (Miami‐Dade County) Country income classification: high Low‐SES sample: yes Population description: low resource, predominantly ethnic minority families Inclusion criteria: ECEC centres must have met the following criteria to be included in the study: (1) have > 50 children enrolled who are 18‐66 months in age, (2) serve low‐income families (i.e. the child meets state eligibility as receiving school readiness funds), (3) reflect the ethnic diversity of the MDC Public School System (63% Hispanic, 19% non‐Hispanic black, and 18% non‐Hispanic white), and (4) obtain agreement from child‐care centre directors and teachers to participate. Exclusion criteria: ECEC centres were excluded if they did not meet the inclusion criteria and if they had a high prevalence of special needs children (i.e. a child with a diagnosed disability with an Individual Education Plan). Special needs did not include children with food allergies and sensitivities; these children were included if their parent consented to study participation. Children who brought their own meals because of diet restrictions and those who were identified by parents on the demographic form as failure to thrive were also excluded. Number of services randomised: 24 (12 intervention, 12 control) Number of children randomised: 825 (465 intervention, 360 control) Characteristics Children Age: 43.4 months (SD 13.3) Gender (% female): 52.5% Ethnicity: Hispanic Cuban: 20.5%; other Hispanic: 43.5%; non‐Hispanic black: 25.2%; non‐Hispanic white: 4.9%; other: 5.8% Parents Age (years): 18‐24: 6.9%; 25‐30: 21.1%; 31‐40: 30.1%; 41‐50: 6.7%; 51+: 1.5%; missing: 33.8% Gender (% female): unclear Ethnicity: not reported Parent/family SES: < 12th grade or GED: 5.3%; completed high school: 7.1%; completed education > high school: 66.6%; missing: 31.4% Method of recruitment: centre directors and teachers were invited to attend a project orientation describing the activities at their centres. Parents/guardians were recruited for participation in the study via verbal announcements, flyers, and letters sent home. Family members who returned a signed interest form were contacted by telephone. Missing data/dropout: not reported Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Healthy Caregivers‐Healthy Children Phase 2 Number of conditions: 1 intervention, 1 controls Intervention duration: 2 school years (approximately 10 months ) Intervention setting: ECEC Intervention strategies: Health curriculum Children Education: the child curriculum had lesson plans for instructional needs that were consistent with the policies outlined in the toolkit (3 plans focus on beverage/snack policies and 3 plans focus on physical activity/screen‐time policies). Consisted of physical activities and health‐orientated messages incorporated into everyday activities. Ethos and environment ECEC staff Support: monthly technical assistance Curriculum: role modelling curriculum delivered via train‐the trainer model Service Materials/Policy: The Health Caregivers Healthy Children toolkit consists of material designed to incorporate all current nutrition and physical activity policy requirements for preschool children in Florida and embrace best‐practice guidelines (snack policy, beverage policy, physical activity policy, and screen‐time policy). Partnerships Parents Workshops: 6 monthly role modelling workshops the University of Florida Institute of Food and Agricultural Sciences Extension Family Nutrition Program staff Intensity of intervention: 6 x 3‐h monthly workshops for teachers; 6 monthly role‐modelling workshops for parents; child lesson plans (frequency and duration not reported) Intervention delivered by: research team, ECEC staff, healthcare staff Modality: face‐to‐face, written Theoretical basis: Reach Effective Adoption Implementation and Maintenance Framework, Social Cognitive Theory and Adult Learning Theory Description of control: alternative intervention control (safety education) |
|
| Outcomes |
Outcomes relating to child dietary intake: Vegetable intake, fruit intake, fried intake, fast food intake, snack food intake, soda intake Number of participants analysed: Intervention baseline: 465 Intervention follow‐up: 465 Control baseline: 360 Control follow‐up: 360 Data collection measure: Healthy Kids Checklist Data collector: parent/caregiver Validity of measures used: validated Outcomes relating to child physical measures: BMI percentile, healthy BMI percentile, unhealthy BMI percentile Number of participants analysed: Intervention baseline: 465 Intervention follow‐up: 465 Control baseline: 360 Control follow‐up: 360 Data collection measure: objectively measured (US Health and Human Services (HHS) guidelines) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: The USDA NRI/AFRI (grant numbers #2009‐05065 and #2014‐08403) and National Institutes of Health (F31DK116533) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A total of 24 ECEC centres were randomly assigned (via a random number table) to 1 of 2 study arms. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. The outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, child‐care service staff and study personnel delivering the intervention were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Parents reported children's dietary intake via questionnaire. Blinding of parents was not possible and the outcome measurement is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured and were not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Unclear risk | The number of children available at follow‐up is not reported. Risk of attrition bias is unclear. |
| Incomplete outcome data (attrition bias) Physical outcomes | Unclear risk | The number of children available at follow‐up is not reported. Risk of attrition bias is unclear. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | High risk | There was a statistically significant difference between the intervention group and the control group for child race/ethnicity, child age, caregiver age, caregiver relationship to child, caregiver language spoken in home, caregiver level of education, and birthplace of caregiver. |
| Loss of clusters | Unclear risk | Not reported |
| Incorrect analysis | Low risk | Study authors stated that "All models also accounted for clustering of students within centers." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Nekitsing 2019a.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT (2 x 2 factorial design) Length of follow‐up from baseline: 12 weeks Unit of allocation: preschools Unit of analysis: child |
|
| Participants |
Service type: centre‐based (preschools) Operation: not reported Country (region): UK (Leeds, Brighouse, and Halifax) Country income classification: high Low‐SES sample: unclear Population description: not reported Inclusion criteria: preschools were eligible to take part in the case that they were not participating in other nutrition health programmes and were able to commit to the time frame of the study (9 months). All children aged 2‐5 years attending their preschool class on the agreed test day were included. Exclusion criteria: children were excluded from the study in the case that they had any relevant food allergies, a medical condition that would prevent them from eating the test vegetable, or if their parents opted out of the study. Number of services randomised: 11 (2 Intervention 1; 3 Intervention 2; 3 Intervention 3; 3 control) Number of children randomised: 219 (62 Intervention 1; 68 Intervention 2; 55 Intervention 3; 34 control) Characteristics Children Age: Intervention 1: 38.11 months (SD 0.83) Intervention 2: 43.42 months (SD: 0.54) Intervention 3: 40.54 months (SD 0.65) Control: 41.75 months (SD 0.87) Gender (% female): Intervention 1: 51.1% Intervention 2: 52.1% Intervention 3: 64.1% Control: 37.5% Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported Method of recruitment: 55 preschools from Leeds, Brighouse, and Halifax (West Yorkshire, UK) were sent a recruitment e‐mail in July 2016, followed by a telephone call. Missing data/dropout: lost at baseline: intervention 1: 0/62; Intervention 2: 11/68; Intervention 3: 0/55; Control: 2/34 Lost at follow‐up: intervention 1: 2/62; Intervention 2: 4/68; Intervention 3: 2/55; Control: 3/34 Reasons for dropout: children missed intake assessment days Characteristics of dropouts: no differences were found in baseline characteristics or intake of the children who were lost to follow‐up compared with those who completed the study. |
|
| Interventions |
Programme name: not reported Number of conditions: 3 interventions, 1 control Intervention duration: 10 weeks Intervention setting: ECEC Intervention strategies: Intervention 1: Taste exposure Ethos and environment Children Exposure: ECEC staff offered children mooli (40‐g portions) during usual snack time once/week, for 10 weeks. Intervention 2: Nutrition education Health curriculum Children Education: staff members were instructed to teach 2 specific components of the PhunkyFood Program as often as possible during the 10‐week period. Ethos and environment ECEC staff Training: staff members were trained to deliver the existing PhunkyFoods program. Resources: ideas and inspiration for classroom carousel play activities (e.g. stories, role‐play, and games), practical food handling/preparation activities, educational displays for the classroom and parental involvement opportunities. Resources were available in both online and offline formats. Staff members were given materials to support their teaching (e.g. photo cards, posters, a floor mat, game ideas, interactive video stories, music, food preparation, tasting ideas, and drawing and colouring activities). Partnerships External provider Delivery: The PhunkyFoods team trained educators. Intervention 3: Taste Exposure + Nutrition Education Health curriculum Children Education: staff members were instructed to teach 2 specific components of the PhunkyFood Program as often as possible during the 10‐week period. Ethos and environment Children Exposure: ECEC staff offered children mooli (40‐g portions) during usual snack time once/week, for 10 weeks. ECEC staff Training: staff members were trained by the PhunkyFoods team to deliver the existing PhunkyFoods program. Resources: ideas and inspiration for classroom carousel play activities (e.g. stories, role‐play, and games), practical food handling/preparation activities, educational displays for the classroom and parental involvement opportunities. Resources were available in both online and offline formats. Staff members were given materials to support their teaching (e.g. photo cards, posters, a floor mat, game ideas, interactive video stories, music, food preparation, tasting ideas, and drawing and colouring activities). Partnerships External provider Delivery: The PhunkyFoods team trained educators. Intensity of intervention: Intervention 1: children were offered 40‐g portions of the vegetable snack once/week for 10 weeks. Invervention 2: staff trained in PhunkyFoods; 2 specific components of the PhunkyFood Program delivered to children as often as possible during the 10‐week period Intervention 3: children were offered 40‐g portions of the vegetable snack once a week for 10 weeks; staff trained in PhunkyFoods; 2 specific components of the PhunkyFood Program delivered to children as often as possible during the 10‐week period. Intervention delivered by: Intervention 1: research team, ECEC staff Intervention 2: ECEC staff, healthcare staff Intervention 3: research team, ECEC staff, healthcare staff Modality: Intervention 1: face‐to‐face Intervention 2: face‐to‐face, online, written Intervention 3: face‐to‐face, online, written Theoretical basis: not reported Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: Intake of test vegetable (mooli) Number of participants analysed: Intervention 1 baseline: 32‐47 Intervention 1 follow‐up: 44‐47 Intervention 2 baseline: 31‐38 Intervention 2 follow‐up: 38 Intervention 3 baseline: 25‐29 Intervention 3 follow‐up: 25‐39 Control baseline: 12‐16 Control follow‐up: 12‐16 Data collection measure: each vegetable portion was weighed before and after each snack time using a digital scale Data collector: researcher Validity of measures used: not reported Outcomes relating to child physical measures: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: White Rose Doctoral Training Centre (WRDTC) Economic and Social Research Council (ESRC) Collaborative Award. The collaborative partner is Purely Nutrition Ltd. Contribution in kind, which includes storybooks and photo cards, were received from Purely Nutrition Ltd. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Preschools were stratified by size and randomly assigned to one of 4 intervention conditions using an online list generator (https://www.random.org/lists). |
| Allocation concealment (selection bias) | Low risk | Preschool managers were not informed of their condition allocation until all preschools were recruited (after consent) and randomised. It was possible to conceal condition allocation between clusters but not within a cluster. |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | Teachers were aware of allocation and could have encouraged students to eat or try more of the vegetable on testing days. |
| Blinding of outcome assessment (detection bias) Diet outcomes | Low risk | Blinding not reported, however vegetable portions were measured before and after intake to the nearest 0.01 g to determine consumption. The outcome measurement is not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | High risk | Data were available for 140 (64%) children allocated to a treatment group at follow‐up, with follow‐up rates between 47%‐76% across the 4 groups. Study authors stated that "due to the nature of the study design there was a high rate of missing data over time for the complete set of intake data, including follow‐ups (36%). As a result of this, there was a substantially smaller sample size in the control condition" Due to the magnitude of missing data and difference in the proportions of participants followed up between groups, the risk of bias was assessed as high. |
| Selective reporting (reporting bias) | Unclear risk | Trial registered with primary outcome reported as described. Secondary outcome measure of intake of usual vegetables, however this outcome was not reported in the study. |
| Recruitment bias | Low risk | Individuals and schools were recruited before randomisation of clusters. Study authors state that "Preschool managers were not informed of their condition allocation until all preschools were recruited (after consent) and randomized. It was possible to conceal condition allocation between clusters but not within a cluster." |
| Baseline imbalance | Low risk | No baseline differences noted between groups with regards to sex distribution or mean BMI z‐score, but there were differences in mean age. Age was controlled for in analyses. |
| Loss of clusters | Low risk | No loss of clusters |
| Incorrect analysis | Low risk | Study authors stated that "Because children were recruited using a cluster design, it was important to account for the influence of cluster assignment. In addition, for repeated measures, each data point was clustered within child. Therefore all the models described below corrected for this using the complex samples procedure within SPSS version 24 to incorporate the contribution of these variance components to the data." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Unclear risk | Deviation from methods noted. Study authors stated that "However, given that many children did not eat mooli at baseline, the data were significantly skewed and not suited to simple parametric analysis. Therefore, children were categorized according to their eating pattern at postintervention, Follow‐up 1 and Follow‐up 2 (noneater, eater) and these are shown in Table 2." There is insufficient information to assess whether an important risk of bias exists. A commercial organisation provided in‐kind support. |
Nemet 2011a.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 12 months Unit of allocation: kindergarten class Unit of analysis: child |
|
| Participants |
Service type: kindergartens (within schools) Operation: not reported Country (region): Israel (Sharon) Country income classification: high Low‐SES sample: yes Population description: low‐SES communities in the Sharon area, Israel. SES was determined with criteria set by the Israeli Central Bureau of Statistics. A scale of 1‐10 refers to the SES, whereas low SES was defined by a score of 1‐4. The score is comprised of the level of education, employment/unemployment status, income level, number of children per family, number of people per household, and additional standard of living characteristics (e.g. brand and model of cars) Inclusion criteria: kindergartens from low‐SES communities in the Sharon area, Israel. Low‐SES classification refers to 1‐4 on 10‐point scale with criteria set by the Israeli Central Bureau of Statistics. Exclusion criteria: not reported Number of services randomised: 30 classes (15 intervention, 15 control) Number of children randomised: 725 (376 intervention, 349 control) Characteristics Children Age: Intervention: 5.2 years (SD 0.02) Control: 5.24 years (SD 0.03) Gender (% female): Intervention: 46% Control: 44% Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported Method of recruitment: not reported Missing data/dropout: 70 children did not complete the study (8.8%) (29/378 control, 41/417 intervention) Reasons for dropout: children absent on the days of follow‐up measurements Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: not reported Number of conditions: 1 intervention, 1 control Intervention duration: 1 year Intervention setting: ECEC and home Intervention strategies: Health curriculum Children Education: topics such as food groups, vitamins, healthy food choices, food preparation and cooking methods, and information on fast‐food versus home cooking were taught by preschool teachers through short lectures/talks, games, and story reading. Children were encouraged to increase their habitual afterschool physical activity and to reduce sedentary activities. Ethos and environment Children Exposure: children participated in 45‐min/d (divided to 3 x 15‐min sessions/d) of exercise training (6 d/week). Once a week, the training was directed by a professional youth coach. During the rest of the week similar physical activity sessions were co‐ordinated by the preschool teacher or assistant. Training took place indoors or outdoors, varied in intensity and duration, was designed primarily as games, and consisted primarily of endurance type activities (e.g. team sports and running). ECEC staff Training: teachers attended an all‐day seminar (lectures and hands‐on sessions) in which they were acquainted with the programme and were trained by the study team so that preschool staff (i.e. teacher and assistant teacher) could perform all the nutritional aspects of the intervention and most exercise classes. 2 additional training days were offered to collect feedback on the programme and to introduce new materials to the teachers. Meeting: summary meeting for teachers at the end the year. Resources: written materials around programme. Preschool teachers were given a CD collection of children’s songs related to nutrition and exercise. Partnerships Families Events: parents and children were invited to 2 x "Healthy Day Festivals" that focused on healthy nutrition, prevention of child obesity, and beneficial effects of exercise in children. The festivals included lectures given by the study team and games for both children and parents. Resources: monthly flyers detailing nutritional information were sent home via children. Activities: children were asked to present the flyer on nutritional information to their parents, and parents were asked to discuss the information with their children. Healthcare Delivery: once a week, the exercise training was directed by a professional youth coach to children. Intensity of intervention: 2 x staff training days; 2 x healthy day festivals with parents; nutrition activities delivered to children (frequency and duration not reported); monthly nutrition flyers sent home for children and parents to discuss; 3 x 15‐min physical activity sessions/week for children; 1 x CD with song on nutrition and physical activity Intervention delivered by: research team, ECEC staff, healthcare staff Modality: face‐to‐face, written Theoretical basis: not reported Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: not reported Outcomes relating to child physical measures: Weight, BMI, BMI percentile Number of participants analysed: Intervention baseline: 376 Intervention follow‐up: 376 Control baseline: 349 Control follow‐up: 349 Data collection measure: objectively measured (CDC) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: The Rosalinde and Arthur Gilbert Foundation, and the Israel Heart Fund | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Kindergarten classes were randomly assigned by computerised program to intervention or control group |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Children's height and weight were measured by an experienced technician who was blinded to group assignment. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Study authors stated that "Seventy children did not complete the study (8.8%), because they were absent on the days of follow‐up measurements (29/378 control, 41/417 intervention) and therefore were excluded from the study. Seven hundred twenty‐five participants completed the study (349 control subjects, 376 subjects treated with intervention)." Missing data were similar between groups and for similar reasons. Therefore, risk of attrition bias was considered to be low. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Low risk | Baseline characteristics of age, sex, and weight status were reported, although no statistical test of difference is reported. |
| Loss of clusters | Unclear risk | Not reported |
| Incorrect analysis | Low risk | Study authors stated that "A two‐way repeated measures analysis of variance was used to compare effects of the intervention on body weight, height, BMI, BMI percentiles, nutrition and physical activity knowledge and preferences and fitness between the intervention participants and the control participants with time serving as the within group, and intervention as the between group factor. When differences between the 2 groups were identified, a mixed model analysis was performed, to ensure no class effect." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Nemet 2011b.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 1 school year Unit of allocation: kindergarten classes Unit of analysis: child |
|
| Participants |
Service type: centre‐based (kindergartens) Operation: not reported Country (region): Israel (Central Israel) Country income classification: high Low‐SES sample: yes Population description: low‐SES communities Inclusion criteria: not reported Exclusion criteria: not reported Number of services randomised: 11 (5 intervention, 6 control) Number of children randomised: 342 (154 intervention, 188 control) Characteristics Children Age: Intervention: 5.36 years (SD 0.03) Control: 5.4 years (SD 0.02) Gender (% female): Intervention: 45% Control: 45% Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported Method of recruitment: not reported Missing data/dropout: 45 children did not complete the study (13.0 %) Reasons for dropout: mainly due to absence in the final data collection day Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: not reported Number of conditions: 1 intervention, 1 control Intervention duration: 1 school year Intervention setting: ECEC and home Intervention strategies: Health curriculum Children Education: topics such as food groups, vitamins, healthy food choices, food preparation and cooking methods, and information on fast‐food versus home cooking were taught by preschool teachers through short lectures/talks, games, and story reading. Children were encouraged to increase their habitual afterschool physical activity and to reduce sedentary activities. Ethos and environment Children Exposure: children participated in 45‐min/d (3 x 15‐min/d) sessions of exercise training (6 d/week). Once a week, the training was directed by a professional youth coach. During the rest of the week similar physical activity sessions were co‐ordinated by the preschool teacher or assistant. Training took place indoors or outdoors, varied in intensity and duration, was designed primarily as games, and consisted primarily of endurance type activities (e.g. team sports and running). ECEC staff Training: teachers attended an all‐day seminar (lectures and hands‐on sessions) in which they were acquainted with the programme and were trained by the study team so that preschool staff (i.e. teacher and assistant teacher) could perform all the nutritional aspects of the intervention and most exercise classes. 2 additional training days were offered to collect feedback on the programme and to introduce new materials to the teachers. Meeting: summary meeting for teachers at the end the year. Resources: written materials around programme. Preschool teachers also were given a CD collection of children’s songs related to nutrition and exercise. Partnerships Families Events: parents and children were invited to 2 x "Healthy Day Festivals" that focused on healthy nutrition, prevention of child obesity, and beneficial effects of exercise in children. The festivals included lectures given by the study team and games for both children and parents. Resources: monthly flyers detailing nutritional information were sent home via children. Children were asked to present the nutritional information to their parents, and parents were asked to discuss the information with their children. Healthcare Delivery: once a week, the exercise training was directed by a professional youth coach to children. Intensity of intervention: Teachers: 1 x all‐day staff seminar; 2 additional staff training days; 2 x "Health Festival" days (lectures) with parents Intervention delivered by: research team, ECEC staff, healthcare staff Modality: face‐to‐face, written Theoretical basis: not reported Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: not reported Outcomes relating to child physical measures: Weight, BMI, BMI percentile Number of participants analysed: Intervention baseline: 134 Intervention follow‐up: 134 Control baseline: 163 Control follow‐up: 163 Data collection measure: objectively measured (CDC) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: a grant from the Rosalinde and Arthur Gilbert Foundation and the Israel Heart Fund | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Study authors stated that "Kindergarten classes were randomly assigned by computerized program to participate in a year‐round, in‐school, combined, nutritional and physical activity intervention or to serve as controls (six kindergarten classes in the control group and five the intervention group)." |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Study authors stated that "Measurements were performed by an experienced technician who was blinded to the group assignment." |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Study authors stated that "Forty‐five children did not complete the study (13.0%) because they were absent at the days of follow‐up measurements (25/188 control and 20/154 intervention) and were therefore excluded from the study." As this is < 20% and numbers are similar across groups and unlikely due to the true outcome, this is unlikely to affect outcomes. Missing data were similar between groups and for similar reasons. Therefore, risk of attrition bias was considered to be low. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting |
| Recruitment bias | Unclear risk | Study authors stated that "Children were included after parental consent" though it is unclear if individual recruitment occurred before or after randomisation of clusters. |
| Baseline imbalance | Low risk | Study authors stated that "No significant differences in age, gender, body weight, height, BMI, or BMI percentile were found between groups before the intervention." |
| Loss of clusters | Low risk | No clusters appear to have been lost, based on attrition and reasons. |
| Incorrect analysis | Low risk | Study authors stated that "When differences between the two groups were identified, a mixed model analysis was performed to ensure no class effect." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Unclear risk | No conflict of interest statement was reported |
Pearson 2022.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 4 months Unit of allocation: centre Unit of analysis: child |
|
| Participants |
Service type: centre‐based Operation: Lunchbox services Country (region): Australia (Hunter New England) Country income classification: high Low‐SES sample: no Population description: the sample area includes major metropolitan centres and inner regional communities, with a small proportion (14%) of people in remote communities. Inclusion criteria: ECEC services from the region that required parents to provide food for consumption at the service (i.e. lunch box services). Recruitment for the trial occurred in 2 phases. Initially, ECEC services were eligible to participate in the trial if they enrolled children aged 3‐6 years and were existing users of the designated parent communication app. As this eligibility criterion did not result in adequate ECEC services being recruited, phase 2 recruitment extended the eligibility criteria to include ECEC services not yet using the app but willing to commence using the app for the trial. Parents or carers of children aged 3‐6 years were eligible to participate if their child attended during the designated days of data collection and if they used or indicated a willingness to download the intervention app on the consent form. Exclusion criteria: services were excluded if they were participating in any other trial related to improving child nutrition, catered exclusively for children with special needs or are a Department of Education community‐run service (as they are not covered within the ethics arrangement). Children were excluded if they had special dietary requirements or allergies that would necessitate specialised tailoring of their diet. Number of services randomised: 18 (9 intervention, 9 control) Number of children randomised: 400 children (191 intervention, 209 control) Characteristics Children Age: Intervention: 3.9 years (SD 0.68); control: 3.9 years (SD 0.67) Gender (% female): Intervention: 52.1% Control: 51.6% Ethnicity: not reported Parents Parent/caregiver age (years): not reported Parents gender (% female): not reported Parent/Caregiver Ethnicity: not reported Parent/family SES: Low SES: intervention: 62.8% Control: 55.7%; High SES: intervention: 37.2% Control: 44.3% Parent education: Attended or completed high school: Intervention: 23.4% Control: 22.2%; Technical or further education (TAFE) certificate or diploma: intervention: 31.6% Control: 32.8% Completed university or college degree or higher Intervention: 44.9% Control: 45% Method of recruitment: for both phases, recruitment involved research assistants posting and emailing information statements and consent forms to ECEC services outlining the study, data collection procedures, and requesting participation. To obtain parental consent for participation in the study, ECEC service staff distributed hard copies of parent information statements and consent forms. Parents could also consent on the day of the data collection. Missing data/dropout: a service in the intervention arm ceased using the required app and withdrew from the study (before baseline data but after random allocation). Consumption data were collected for 88% (352/400) of children at baseline and for 84.3% (337/400) after the intervention. Reasons for dropout: a service in the intervention arm ceased using the required app and withdrew from the study. Child attrition reasons were not reported. Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: SWAP IT for Childcare Number of conditions: 1 intervention, 1 control Intervention duration: 10 weeks Intervention setting: ECEC and home Intervention strategies Ethos and environment Service Endorsement: the service managers were asked to communicate their endorsement of the intervention and guidelines to educators via a staff meeting or individual briefings and provide hard copies of the SWAP IT messages and the SWAP IT Lunchbox guidelines. Support: a health promotion officer conducted a brief onsite visit with the service manager to familiarise them with the guidelines and provide support to integrate these with existing service lunchbox policies (if required). Monitoring: a record of implementation was given to service managers to enable them to record their delivery of the agreed tasks during the intervention period. Parents Communication: service managers were asked to send 2 communications to parents via the app or other preferred communication methods (e.g. hard copy newsletters). Partnerships Parents Resource: parents were given access to the Skoolbag app which encourages the use of service‐endorsed ‘SWAP IT Options’ lunchbox guidelines recommending which foods and drinks to ‘swap from’ and which to ‘swap to’ when packing a healthy lunchbox. The guidelines were developed by dietitians and provide specific guidance in line with the Australian Guide to Healthy Eating, recommendations outlined in the NSW Ministry of Health nutrition sector‐specific resource and health and well‐being requirements outlined in national accreditation standards. Parents were also able to access messages and images, and through attachments and links to the ‘SWAP IT Childcare’ webpages, videos, fact sheets and other websites. Communication: push notifications alerted parents to messages sent via the service’s app for 10 weeks (1/week). Intensity of intervention: Parents: 1 x push notification for 10 weeks, plus an additional notification in the first week. 2 x communication by service (via app, email or preferred communication methods) Service: 1 on‐site visit (if required), implementation record Intervention delivered by: ECEC staff, healthcare staff Modality: face‐to‐face, online, written Theoretical basis: Behaviour Change Wheel Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: Vegetable intake, fruit intake, discretionary foods intake, breads and cereals intake, dairy intake, meat and alternatives intake, mean energy from discretionary foods, mean energy, saturated fat, total and added sugars, sodium consumed from all foods and calorific drinks packed in children’s lunch boxes Number of participants analysed Intervention baseline: 138 Intervention follow‐up: 137 Control baseline: 165 Control follow‐up: 164 Data collection method: weighed plate waste enhanced with digital photography and written records Data collector: researchers Validity of measures used: validated Outcomes relating to child physical measures: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: owing to the null findings, a cost‐effectiveness analysis, as specified in the study protocol, was not conducted. Outcome relating to adverse consequences: Changes in the frequency of parent complaints or concerns regarding healthy lunch box policy Number of participants analysed: not reported Data collection method: service manager pen and paper survey Data collector: service manager Validity of measures used: not reported |
|
| Notes | Funding source: this research received no specific grant from any funding agency in the public, commercial or not‐for‐profit sectors. Infrastructure funding was provided in kind by Hunter New England Population Health. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Study authors stated that "ECEC services were randomly allocated to the intervention group or no intervention control group in a 1:1 ratio by a statistician independent of the trial using a computerized random number generator." |
| Allocation concealment (selection bias) | Low risk | Centres were allocated to groups following recruitment. |
| Blinding of participants and personnel (performance bias) Diet outcomes | Unclear risk | Study authors state "Owing to the nature of the intervention, ECEC services and parents were not blinded to the intervention; however, outcome assessors were blinded to the service allocation." It is unclear whether lack of blinding would affect the outcome. For example, teachers could have encouraged their students to eat more of certain foods from their lunches on the days of observation, though this is unknown. |
| Blinding of participants and personnel (performance bias) Adverse consequences | Unclear risk | Services were not blind to study allocation. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | Low risk | Study authors state "outcome assessors were blinded to the service allocation." |
| Blinding of outcome assessment (detection bias) Adverse consequences | Unclear risk | Services were not blind to study allocation. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Low risk | Study authors stated that "Consumption data were collected for 88% (352/400) of children at baseline and for 84.3% (337/400) after the intervention." |
| Incomplete outcome data (attrition bias) Adverse consequences | Unclear risk | The number of services and participants that reported on this outcome at follow‐up is unclear. |
| Selective reporting (reporting bias) | High risk | Study authors stated that "Owing to the null findings, neither a cost‐effectiveness analysis, as specified in the study protocol, nor the planned analysis of data collected on the usual daily dietary intake of children (to be able to detect any compensatory dietary behaviors) was conducted." |
| Recruitment bias | Low risk | Allocation took place after recruitment and before baseline data collection. |
| Baseline imbalance | Low risk | Study authors stated that "Characteristics were similar across groups; however, the intervention group had a higher proportion of parents located in the outer regional areas than the control group. As the intervention was delivered at the cluster level rather than at the individual level, geographical remoteness was accounted for by stratifying services by this factor during randomisation and not controlled for as part of the analysis." |
| Loss of clusters | High risk | Study authors stated that "A service in the intervention arm ceased using the required app and withdrew from the study (before baseline data but after random allocation)." |
| Incorrect analysis | Low risk | Study authors stated that "Models were adjusted for potential ECEC service level clustering through a service random effect and controlled for baseline service Environment and Policy Assessment and Observation score and if ECEC services were existing app users before the trial." |
| Contamination | Low risk | Study authors stated that "No contamination was reported; that is, the app was not used to send any other health or nutrition information. No ECEC services in the intervention or control groups reported exposure to additional nutrition interventions throughout the duration of the trial." |
| Other bias | Low risk | No other clear source of bias |
Peñalvo 2015.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 3 years Unit of allocation: schools Unit of analysis: school and child |
|
| Participants |
Service type: preschool (within schools) Operation: public schools Country (region): Spain (Madrid) Country income classification: high Low‐SES sample: no Population description: not reported Inclusion criteria: participating schools were selected from among all public schools in the city of Madrid, Spain, on the basis of size (> 50 children/class) and availability of cafeteria service. The study focused only on schools located in the city of Madrid, having full canteen services, and with ≥ 2 classrooms per preschool level (needed to attain the 50 students per level used in sample size calculation). Exclusion criteria: schools on the extremes of the distribution for percentage of immigration and percentage scholarships were excluded. Number of services randomised: 24 (12 intervention, 12 control) Number of children randomised: 2062 (groups not reported) Characteristics Children Age: 3‐5 years Gender (% female): not reported Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported Method of recruitment: not reported Missing data/dropout: 20% of children 3 years of age (3‐year intervention), 13% of children 4 years of age (2‐year intervention), and 3.2% of children 5 years of age (1‐year intervention) were lost to follow‐up. Reasons for dropout: this was due to 1 intervention school discontinuing the study because the school’s principal was replaced after the first year. Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: The SI! Program for Cardiovascular Health Promotion in Early Childhood Number of conditions: 1 intervention, 1 control Intervention duration: 3 years Intervention setting: ECEC and home Intervention strategies: Health curriculum Children Education: didactic units, including 7 key activities/unit, relating to 4 lifestyle‐related components: diet, physical activity, knowledge of the human body and heart, and management of emotions. Teachers delivered the intervention through classroom materials for a minimum of 20 h for the diet, physical activity, and human body components and a minimum of 10 h for the emotion management component. The Program SI! is embedded in the school curriculum and implemented in the classroom on 4 complete weeks during every school year. Ethos and environment Children Resources: Sesame Street audio visuals, books and games, and cooking workshops, and tales of healthy living. ECEC staff Resources: all preschool teachers had access to an online repository of the intervention resources. Teachers also interacted via the intervention website on a blog where activities were shared between participating schools and in an open forum where they discussed any aspect of the intervention. Training: in each school, a teacher volunteered as the intervention co‐ordinator and received regional, government‐certified training in the SI! Program contents and strategies (an expert‐led 30‐h course). Support: continuing counselling from programme staff to liaisons. Service Event: parents, children and teachers were invited to an annual Health Fair. Resources: documentation of healthy recommendations in schools Support: periodical meetings between principal and programme liaisons Partnerships Families Resources: families were given access to the programme website and given informative letters and leaflets. Activities: families were provided activities to do over the weekend. Event: parents were invited to whole‐school events such as the annual health fair. Intensity of intervention: 70 h x health curriculum for children; 30 h x teacher training each year; 12 h x parent components (health fair; information; activities); 2 h x school component. Intervention delivered by: ECEC staff, healthcare staff Modality: face‐to‐face, online, written Theoretical basis: not reported Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: not reported Outcomes relating to child physical measures: BMI percentile, BMI z‐score, waist circumference, skinfold thickness tricep, skinfold thickness subscapular, obese, overweight Number of participants analysed: not reported Data collection measure: objectively measured (CDC) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: research grant FIS‐PI11/01885 (Fondo de Investigación Sanitaria del Instituto de Salud Carlos III), Fondo Europeo de Desarrollo Regional (FEDER 2007–2013), and the Daniel and Nina Carasso Foundation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | No clear blinding of participants and personnel to study allocation, however the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height, weight, waist circumference, and skinfold thickness were measured and not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Study authors stated that "During follow‐up, 20% of children 3 years of age (3‐year intervention), 13% of children 4 years of age (2‐year intervention), and 3.2% of children 5 years of age (1‐year intervention) were lost to follow‐up. This was due to 1 intervention school discontinuing the study because the school’s principal was replaced after the first year. No significant differences were found in baseline demographic or outcome‐related variables (KAH score and anthropometric measures) for those children lost to follow‐up compared to the rest of participants (intervention or control groups)." Therefore, risk of attrition bias was considered to be low. |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the paper were prespecified in the protocol paper. |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Unclear risk | Stratified randomisation was conducted to account for discrepancies in SES, however baseline demographic data are not reported for treatment groups. |
| Loss of clusters | High risk | One intervention cluster lost because the school’s principal was replaced after the first year. |
| Incorrect analysis | Low risk | Study authors stated that "Mixed‐linear models that account for the cluster randomized design were used to test for intervention effect. Fixed effects in each model were the corresponding baseline score, school year, and treatment group. Schools were handled as random effects. No correction for multiple comparisons was used." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Unclear risk | Study authors stated that "Despite finding strong statistical associations, the lack of adjustment for multiple comparisons could have affected the results." There is insufficient information to assess whether an important risk of bias exists. No conflict of interest statement was reported. |
Pinket 2016.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 12 months Unit of allocation: municipalities Unit of analysis: child |
|
| Participants |
Service type: centre‐based: (Germany: kindergartens; Bulgaria: kindergartens; Spain: kindergartens; Poland: kindergartens; Greece: kindergartens and day‐care centres; Belgium: preschool settings) Operation: not reported Country (region): 6 European countries (Belgium, Bulgaria, Germany, Greece, Poland and Spain) Country income classification: Belgium: high; Germany: high; Greece: high; Poland: high; Spain: high; Bulgaria: upper‐middle Low‐SES sample: unclear Population description: not reported Inclusion criteria: kindergartens were considered eligible for inclusion in the intervention if (i) they were located within a radius of 50 km around the local institutes; (ii) headmasters and teachers provided signed consent form and (iii) families’/children’s participation rate was at least 50%. Children within recruited kindergartens were eligible if (i) they were aged between 3.5 and 5.5 years at the time of recruitment (i.e. born between January 2007 and December 2008); (ii) their parents/caregivers provided a signed consent form and (iii) were not participating in any other clinical trial or other health‐oriented project during the academic years 2012–2013 and 2013–2014. Exclusion criteria: not reported Number of services randomised: 309 (groups not reported) Number of children randomised: 4964 (groups not reported) Characteristics Children Age: 4.7 years (SD 0.4) Gender (% female): 48.5% Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: SES (years of school education mother), % lower SES (= % ≤ 14 years of education): 38.5% Method of recruitment: not reported Missing data/dropout: not reported Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: The ToyBox‐intervention Number of conditions: 1 intervention, 1 control Intervention duration: 24 weeks in the school year Intervention setting: ECEC and home Intervention strategies: Health curriculum Children Education: teachers promoted the 4 targeted energy balance‐related behaviours (i.e. water consumption, snacking, physical activity and sedentary behaviour) on a regular basis and predefined time within each day, in the classroom/kindergarten. Teachers implemented interactive classroom activities, aiming at total class participation, minimum for 1 h/week. Ethos and environment Children Exposure: teachers remind children to drink water regularly and do short movement breaks twice in the morning and twice in the afternoon, arranging a daily break for the whole class to eat healthy snacks and performing 2 physical education sessions/week with a duration of 45 min each. Role modelling: teachers were also instructed to use the kangaroo hand puppet and perform these 4 topics, so as to enhance the effects of the intervention via role modelling ECEC staff Training: 2 x voluntary teacher training sessions to explain the programme and materials. An additional non‐compulsory training session was also offered. Teachers were not tested, but researchers provided certificates of attendance to the teachers as incentives. Resources: a box including the ToyBox‐intervention material (teacher's guide, classroom activity guide, kangaroo hand puppet) was provided to teachers. Service Environment: installation of water stations and the ‘magic snack plate’ to assist water and healthy snack consumption; rearrangements of the classroom/kindergarten to create some free space to assist children’s movement. Partnerships Families Resources: 9 x newsletters, 8 x tip cards and 4 x posters, coloured by their child, which aimed to encourage parents/caregivers to apply relevant environmental changes at home, act as role models and implement these lifestyle behaviours together with their children. Intensity of intervention: 3 x teacher training sessions; permanent environmental changes; teachers promote targeted behaviours every day; 2 x 45 min physical education lessons/week for children; 1 h/week interactive classroom activity; 9 x parent newsletters; 8 x parent tip cards; 4 x parent posters; 1 box of intervention materials provided to teachers. Intervention delivered by: research team, ECEC staff Modality: face‐to‐face, written Theoretical basis: PRECEDE‐PROCEED Model Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: Plain yoghurt intake, cheese intake, fresh fruit intake, raw vegetable intake, sugared or aromatised yoghurt intake, chocolate and candy bars intake, milk‐based desserts intake, cake intake, biscuit intake, sugar‐based dessert intake, salty snack intake, healthy snack intake, unhealthy snack intake, unhealthy snacks intake, plain water intake, tea intake, soft drink intake, light soft drink intake, pure fruit juice intake, pre‐packaged fruit juice intake, smoothie intake, plain milk intake, sugared and chocolate milk, total water, fruit juice intake, soft drink intake, water intake Number of participants analysed: Intervention baseline: 3255 Intervention follow‐up: 3255 Control baseline: 1715 Control follow‐up: 1715 Data collection measure: FFQ Data collector: parent/caregiver Validity of measures used: validated Outcomes relating to child physical measures: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: Seventh Framework Programme (CORDIS FP7) of the European Commission under grant agreement n° 245200 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation of the recruited municipalities to intervention and control group was conducted centrally using Excel by the co‐ordinating centre in a 2:1 ratio within each SES strata. |
| Allocation concealment (selection bias) | Low risk | Allocation to intervention and control group was conducted centrally by the co‐ordinating centre, after the completion of baseline measurements. |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. The outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Parents reported children's dietary intake via a FFQ. Blinding of parents not reported, and the outcome measurement is likely to be influenced by a lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Unclear risk | Study authors stated that "Completer analysis was carried out to handle missing data, which means that only preschoolers with valid data at both baseline and follow‐up were included in the analyses." Data were available for 4970 (70%) of children whose parents consented to the study. No information is provided as to reasons for missing data or whether the loss or reasons for loss differed by intervention group. Risk of attrition bias is unclear. |
| Selective reporting (reporting bias) | Unclear risk | Outcomes are not clearly reported in the trial registration or trial protocol, so it was unclear whether there was selective outcome reporting. |
| Recruitment bias | Low risk | Individuals and centres were recruited before randomisation of municipalities. Randomisation of the municipalities to treatment group was conducted centrally by the co‐ordinating centre, after the completion of baseline measurements. |
| Baseline imbalance | Low risk | Descriptive analyses showed that there was no significant difference between the intervention and control groups regarding sex, age, intake of healthy snacks, and intake of unhealthy snacks at baseline. Clusters were stratified by SES prior to random selection and all analyses were corrected for preschool children's sex and age. |
| Loss of clusters | Unclear risk | There is a large number of missing data, however it is unclear if there were losses of clusters. |
| Incorrect analysis | Low risk | Study authors stated that "To take clustering of baseline and follow‐up measurements of preschool children in kindergarten classes in kindergartens into account, multilevel modeling was used." |
| Contamination | Low risk | Study authors stated that "After the recruitment of kindergartens and to avoid contamination between kindergartens in the same municipality, kindergartens’ municipalities were randomly assigned to the intervention or control group (2:1)." Therefore, contamination is unlikely. |
| Other bias | Low risk | No clear other source of bias |
Puder 2011.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 11 months Unit of allocation: preschool class Unit of analysis: child |
|
| Participants |
Service type: centre‐based (preschools) Operation: public Country (region): Switzerland (St Gallen and Lausanne) Country income classification: high Low‐SES sample: yes Population description: public preschool classes in areas with a high migrant population from 2 different sociocultural and linguistic regions in Switzerland. The study was conducted in the German‐speaking (city of St Gallen; 70,000 inhabitants) and the French‐speaking (urban surroundings of Lausanne, canton Vaud; 50,000 inhabitants) regions of Switzerland during the school year 2008‐9. All children in Switzerland attend preschool. The city of St. Gallen and the Lausanne area were chosen due to a high prevalence (i.e. at least 40%) of children of migrant background. Migrant background was defined as at least one parent born out of Switzerland. Inclusion criteria: inclusion criteria were > 40% prevalence of migrant children and no participation in any other prevention project. Exclusion criteria: not reported Number of services randomised: 40 (20 intervention, 20 control) Number of children randomised: 727 (342 intervention, 310 control) Characteristics Children Age: 5.2 years (SD 0.6) Gender (% female): 50% Ethnicity: Mainly speak a foreign language at home (any language other than German or French): 40% Most common migrant regions (according to country of birth of father): Former Yugoslavia: 25% (91); Portugal: 17%; rest of Europe: 31%; Africa: 12%; rest of world: 15% Parents Age (years): not reported Gender (% female): not reported Ethnicity: 1 parent migrant: 24%; both parents migrant: 48% Migrant areas: Yugoslavia: 25%; Portugal: 17%; rest of Europe: 31%; Africa: 12%; rest of world: 15% Parent/family SES: Parental low education level (max 9 years education): neither parent: 62%; 1 parent: 21%; both parents 17% Method of recruitment: not reported Missing data/dropout: all ECEC classes retained. Of the 655 children with consent, 652 were present at baseline for BMI measures Reasons for dropout: 26 children dropped out of the intervention due to moving away. Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Ballabeina Number of conditions: 1 intervention, 1 control Intervention duration: 1 school year Intervention setting: ECEC and home Intervention strategies: Health curriculum Children Education: 22 sessions on healthy nutrition, media use, and sleep Ethos and environment Children Exposure: 45‐min physical activity sessions prepared by an exercise physiologist with the aim to improve aerobic fitness and co‐ordination skills. Taught weekly by a health promoter for the first 4 months and then reduced to twice a month and taught by preschool teachers. Children in preschool classes are exclusively offered water and healthy food. Resources: every other week children received a new fun physical activity or nutrition activity card to take home and a CD with music. ECEC staff Workshops: teachers participated in 2 x workshops before the intervention to learn about the content and the practical aspects of the intervention. Meeting: 1 formal meeting to exchange their experience and involved in evenings organised for the parents. Support: teachers were supported to deliver physical activity sessions through hands‐on training by health promotors during the initial visits. Health promoters also assisted in the choices regarding how to adapt the built environment in and around the preschool class. Service Environment: healthy snacks during recess and healthy treats for special occasions were promoted and water and healthy food was exclusively offered during class. Fixed and mobile equipment were installed or provided in and around classrooms, including a “movement corner.” Materials: coloured poster of the "Ballabeina track", was hung in classroom and stickers were pasted on the poster to show progress. Event: a Ballabeina event was organised with games implementing the main messages of the intervention. All participants Cultural: intervention culturally tailored based on evaluation of norms and needs. Partnerships Families Meetings: 3 x interactive information and discussion evenings. Organised by health promoters in collaboration with preschool teachers Resources: brochures, information leaflets, physical activity or nutrition activity cards and worksheets. The information leaflets for parents were provided in 10 different languages, and native speakers of the main foreign languages were available to answer questions. Healthcare Delivery: health promoters assisted in the delivery of the intervention. Intensity of intervention: 4 x 45‐min sessions of physical activity each week (trained staff delivered these once a week, which was reduced to twice a month after 4 months) for children; 22 sessions on healthy nutrition/media use and sleep for children; take home messages once/week for children; 1 x Ballabeina event (organised games, and materials provided); 2 x teacher workshops; 3 x interactive parent information evenings Intervention delivered by: research team, ECEC staff, healthcare staff Modality: face‐to‐face, written Theoretical basis: Social Ecological Model Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: Proportion healthy eaters Number of participants analysed: Intervention baseline: 342 Intervention follow‐up: 333 Control baseline: 310 Control follow‐up: 292 Data collection measure: semi‐qualitative FFQ Data collector: parent Validity of measures used: not reported Outcomes relating to child physical measures: BMI, percentage body fat, sum of 4 skin folds, waist circumference, overweight or obese Number of participants analysed: Intervention baseline: 342 Intervention follow‐up: 333 Control baseline: 310 Control follow‐up: 292 Data collection measure: objective measure (IOTF) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: Attention, spatial working memory Number of participants analysed: Intervention baseline: 342 Intervention follow‐up: 333 Control baseline: 310 Control follow‐up: 292 Data collection measure: Konzentrations‐Handlungsverfahren für Vorschulkinder and Intelligence and Development Scales Data collector: parent Validity of measures used: validated Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: Quality of life Number of participants analysed: Intervention baseline: 342 Intervention follow‐up: 333 Control baseline: 310 Control follow‐up: 292 Data collection measure: general health questionnaire (PedsQL 4.0) Data collector: parent Validity of measures used: validated Outcome relating to cost: not reported Outcome relating to adverse consequences: Study authors state only, "No injuries or other adverse events occurred during physical activity sessions in the intervention classes" Number of participants analysed: not reported Data collection measure: not reported Data collector: not reported Validity of measures used: not reported |
|
| Notes | Funding source: mainly supported by the Swiss National Science Foundation (grant No 3200B0‐116837) and Health Promotion Switzerland (project No 2104). Additional funding was obtained from a research award for interdisciplinary research from the University of Lausanne, a Takeda research award, the Wyeth Foundation for the Health of Children and Adolescents, the Freie Akademische Gesellschaft, and an unrestricted educational grant from Nestlé. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Classes were randomised (1:1) with the use of opaque envelopes. |
| Allocation concealment (selection bias) | Low risk | Allocation took place after all classes were recruited and selected by someone from the school health services who was not involved in the study. |
| Blinding of participants and personnel (performance bias) Diet outcomes | Unclear risk | Teachers, parents, and children were informed that the intervention aimed to promote children’s health but were unaware of the main objectives of the study. Specially trained researchers measured outcomes and were blinded to group allocation. Eating habits were assessed by the parents with a semi‐qualitative FFQ. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | Teachers, parents, and children were informed that the intervention aimed to promote children’s health but were unaware of the main objectives of the study. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Language and cognitive performance outcomes | Low risk | Teachers, parents, and children were informed that the intervention aimed to promote children’s health but were unaware of the main objectives of the study. Specially trained researchers measured outcomes and were blinded to group allocation. The outcome is not likely to be influenced by lack of blinding |
| Blinding of participants and personnel (performance bias) Quality of life outcomes | Unclear risk | Teachers, parents, and children were informed that the intervention aimed to promote children’s health but were unaware of the main objectives of the study. Specially trained researchers measured outcomes and were blinded to group allocation. It is unclear whether the outcome could be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Adverse consequences | Unclear risk | Teachers, parents, and children were informed that the intervention aimed to promote children’s health but were unaware of the main objectives of the study. It is unclear whether the outcome could be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | Unclear risk | Eating habits were assessed by the parents with a semi‐qualitative FFQ. Parents were informed that the intervention aimed to promote children’s health but were unaware of the main objectives of the study. It is unclear if blinding could have been broken. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Specially trained researchers measured children's height, weight, bioelectrical impedance analysis, skinfold thickness, and waist circumference and were blinded to group allocation. |
| Blinding of outcome assessment (detection bias) Language and cognitive performance outcomes | Low risk | Attention and spatial working memory were assessed by specially trained researchers who were blinded to group allocation. |
| Blinding of outcome assessment (detection bias) Quality of life outcomes | Unclear risk | Parents completed the health‐related quality of life questionnaire. Parents were informed that the intervention aimed to promote children’s health but were unaware of the main objectives of the study. It is unclear if blinding could have been broken. |
| Blinding of outcome assessment (detection bias) Adverse consequences | Unclear risk | Teachers, parents, and children were informed that the intervention aimed to promote children’s health but were unaware of the main objectives of the study. It is unclear whether the outcome could be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Low risk | Data were available for 333 (97%) children in the intervention group and 292 (94%) children in the control group. Amount of loss and reasons for loss to follow‐up similar between groups (i.e. child moved away after baseline testing). Therefore, risk of attrition bias was considered to be low. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Data were available for 333 (97%) children in the intervention group and 292 (94%) children in the control group. Amount of loss and reasons for loss to follow‐up similar between groups (i.e. child moved away after baseline testing). Therefore, risk of attrition bias was considered to be low. |
| Incomplete outcome data (attrition bias) Language and cognitive performance outcomes | Low risk | Data were available for 333 (97%) children in the intervention group and 292 (94%) children in the control group. Amount of loss and reasons for loss to follow‐up similar between groups (i.e. child moved away after baseline testing). Therefore, risk of attrition bias was considered to be low. |
| Incomplete outcome data (attrition bias) Quality of life outcomes | Low risk | Data were available for 333 (97%) children in the intervention group and 292 (94%) children in the control group. Amount of loss and reasons for loss to follow‐up similar between groups (i.e. child moved away after baseline testing). Therefore, risk of attrition bias was considered to be low. |
| Incomplete outcome data (attrition bias) Adverse consequences | Unclear risk | The number of services and participants that reported on this outcome at follow‐up is unclear. |
| Selective reporting (reporting bias) | Low risk | The study protocol and trial registration are available and all of the study's pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported in the pre‐specified way. |
| Recruitment bias | Low risk | Individuals and classes were recruited before randomisation. |
| Baseline imbalance | Low risk | There were no differences in baseline characteristics and outcome variables between the intervention and control groups (all P ≥ 0.2). |
| Loss of clusters | Low risk | No loss of clusters |
| Incorrect analysis | Low risk | Study authors stated that "Analyses were performed on an intention to treat basis, by using data from individual children but adjusting for clustering of outcomes within preschool classes." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Unclear risk | Grant money was received from a commercial organisation. |
Ray 2020.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 5 months Unit of allocation: preschool centre Unit of analysis: child |
|
| Participants |
Service type: centre‐based (preschools) Operation: not reported Country (region): Finland Country income classification: high Low‐SES sample: no Population description: municipalities that had a high number of preschools and had a large variety in educational and income levels among inhabitants were recruited. Inclusion criteria: municipalities that had a high number of preschools and had a large variety in educational and income levels among inhabitants as well as being located within a convenient distance from the Helsinki region were invited to participate. Exclusion criteria: municipalities that were already part of the comprehensive DAGIS survey in 2015–2016 were excluded. Number of services randomised: 32 (13 intervention, 19 control) Number of children randomised: 802 (361 intervention, 441 control) Characteristics Children Age: Intervention: 5.14 years (SD 1.04) Control: 5.24 years (1.06) Gender (% female): Intervention: 47.8% Control: 46% Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: Parental education Intervention: low: 35.4%; middle: 46.4%; high: 18.2% Control: low: 29.9%; middle: 43.6%; high: 26.5% Method of recruitment: altogether, 7 municipalities were invited to participate in the study, and an oral presentation on the study was offered. 5 municipalities had an oral presentation; 2 of these municipalities chose to participate. Researchers visited each preschool to inform early educator professionals about the project and their role in the project. The recruitment phase lasted 1–2 weeks, and families returned informed consents (or refusals to participate) to preschools in sealed envelopes. Missing data/dropout: between 10%‐18% of children were missing across diet outcomes. Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: The Increased Health and Wellbeing in Preschools (DAGIS) intervention Number of conditions: 1 intervention, 1 control Intervention duration: 23 weeks (5 months) Intervention setting: ECEC Intervention strategies: Health curriculum Children Education: educators delivered a programme around 5 healthy energy balance‐related behaviours (self‐regulation skills; physical activity; fruit and vegetables; screen time; and sugary foods and beverages). Ethos and environment Children Exposure: self‐regulation skills were promoted by brain breaks, which were a few minutes’ calming down and breathing sessions 3 times/d, led by early educators. ECEC staff Training: 2 x training (approximately 8 h total) Support: email support from researchers throughout the intervention. Service Environment: materials that were produced during the activity afternoons were expected to be displayed at the preschool, so that families could see each other’s work. Partnerships Families Workshops: children and families were invited to 5 activity afternoons delivered by preschools. The focus was set on the children’s energy balance‐related behaviours, and on how parents, by acting as role models and changing the availability and accessibility of the home environment can influence children's energy balance‐related behaviours. Resources: information letters, emails containing videos or articles, bingos related to energy balance‐related behaviour, and 2 fairy tales Intensity of intervention: 2 x training, totaling 8 h; 20‐25 weeks of child program; parent‐child workshops (frequency and duration not reported); parents received materials Intervention delivered by: research team, ECEC staff Modality: face‐to‐face, online, written Theoretical basis: Social Cognitive Theory, Theory of Planned Behaviour, and Self‐Determination Theory Description of control: wait‐list control |
|
| Outcomes |
Outcomes relating to child dietary intake: Sugary everyday food and beverages intake, sugary treats intake, fruit and vegetable intake Number of participants analysed: Intervention baseline: 293‐299 Intervention follow‐up: 192‐200 Control baseline: 307‐323 Control follow‐up: 236‐238 Data collection measure: 51‐item FFQ (expanded from the original 47‐item survey) Data collector: parent Validity of measures used: validated Outcomes relating to child physical measures: not reported Outcome relating to child language and cognitive performance: Cognitive self‐regulation skills Number of participants analysed: Intervention baseline: 313 Intervention follow‐up: 256 Control baseline: 383 Control follow‐up: 324 Data collection measure: 5 items derived from the Child Social Behavior Questionnaire Data collector: not reported Validity of measures used: not reported Outcome relating to child social/emotional measures: emotional self‐regulation skills Number of participants analysed: Intervention baseline: 313 Intervention follow‐up: 256 Control baseline: 383 Control follow‐up: 324 Data collection measure: 5 items derived from the Child Social Behavior Questionnaire Data collector: not reported Validity of measures used: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: financially supported by the Ministry of Education and Culture in Finland, The Ministry of Social Affairs and Health, The Academy of Finland (Grants: 285439, 287288, 288038, 315816), the Päivikki and Sakari Sohlberg Foundation, Signe and Ane Gyllenberg Foundation, and the Medicinska Föreningen Liv och Hälsa. Folkhälsan Research Center and University of Helsinki provided the infrastructure and the funding for PIs (N.S., M.E., E.R.) and key personnel (C.R., R.L.). Open access funding was provided by University of Helsinki. The funding bodies were not involved and did not interfere with the study at any stage. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was made at the preschool manager‐level, separately for the 2 municipalities by an online randomisation program (https://www.randomlists.com/team‐generator). |
| Allocation concealment (selection bias) | Low risk | Preschools were divided into small and large preschools before randomisation. After the baseline measurements, preschools were informed whether they had been randomised into the intervention or control group. |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | No blinding of participants and personnel to study allocation, and the outcome is likely to be influenced by lack of blinding |
| Blinding of participants and personnel (performance bias) Language and cognitive performance outcomes | Unclear risk | No blinding of participants and personnel to study allocation, and it is unclear whether lack of blinding would affect the outcome |
| Blinding of participants and personnel (performance bias) Social/emotional outcomes | Unclear risk | No blinding of participants and personnel to study allocation, and it is unclear whether lack of blinding would affect the outcome |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Parents completed the FFQ. Blinding of parents not reported, and the outcome measurement is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Language and cognitive performance outcomes | High risk | Parents completed a questionnaire regarding children's cognitive self‐regulation skills. Blinding of parents not reported, and the outcome measurement is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Social/emotional outcomes | High risk | Parents completed a questionnaire regarding children's emotional self‐regulation skills. Blinding of parents not reported, and the outcome measurement is likely to be influenced by lack of blinding |
| Incomplete outcome data (attrition bias) Diet outcomes | Unclear risk | Data were available for between 192‐200 (64%‐68%) children in the intervention group and between 236‐258 (74%‐80%) children in the control group. Reasons for loss to follow‐up are not provided. Study authors stated that "All analyses were based on the intention‐to‐treat principle so that all randomized participants were included in the analysis in their randomized intervention group." Risk of attrition bias is unclear. |
| Incomplete outcome data (attrition bias) Language and cognitive performance outcomes | Unclear risk | Data were available for 256 (82%) children in the intervention group and 324 (85%) children in the control group. Reasons for loss to follow‐up are not provided. Study authors stated that "All analyses were based on the intention‐to‐treat principle so that all randomized participants were included in the analysis in their randomized intervention group." Risk of attrition bias is unclear. |
| Incomplete outcome data (attrition bias) Social/emotional outcomes | Unclear risk | Data were available for 256 (82%) children in the intervention group and 324 (85%) children in the control group. Reasons for loss to follow‐up are not provided. Study authors stated that "All analyses were based on the intention‐to‐treat principle so that all randomized participants were included in the analysis in their randomized intervention group." Risk of attrition bias is unclear. |
| Selective reporting (reporting bias) | Unclear risk | The reported self‐regulation outcomes are not specified in either the trial registration or protocol paper. |
| Recruitment bias | Low risk | Full recruitment occurred before randomisation, according to the manuscript's PRISMA diagram. |
| Baseline imbalance | Unclear risk | Even though most characteristics were similar among groups, a higher percentage of children with high educational‐level parents were found in the control group (26%) compared to the intervention group (18%). Study authors report the comparison between the intervention and control groups at follow‐up adjusted for respective baseline outcome values. |
| Loss of clusters | Unclear risk | Not reported |
| Incorrect analysis | Low risk | Study authors stated that "The preschool unit was used as a random effect in order to adjust for variability between the preschools." |
| Contamination | Unclear risk | No evidence to make assessment. |
| Other bias | Unclear risk | Study authors stated that "Finally, the sample size might not have been sufficiently large to detect significant results. The power calculations were conducted based on means and standard deviations from the DAGIS cross‐sectional survey. Some dissimilarities exist between these 2 studies such as the number of preschools and municipalities and the proportion of low parental education level families participating, which might have led to an underpowered study." There is insufficient information to assess whether an important risk of bias exists. One study author is reported to be a board member of a relevant commercial organisation. |
Reyes‐Morales 2016.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 6 months Unit of allocation: centre Unit of analysis: child |
|
| Participants |
Service type: centre‐based Operation: public Country (region): Mexico (Mexico City) Country income classification: upper‐middle Low‐SES sample: unclear Population description: "in the Mexican Social Security Institute (IMSS), which is the largest public health institution in Mexico, the prevalence of overweight has increased dramatically in recent years, even among children; in 2012, 38.1% of overweight in insured school children has been reported. In 2009, approximately 30,000 children were enrolled in 142 child‐care centres of direct provision of IMSS (ECEC centres run by the IMSS owned and attended by institutional staff). Children of IMSS cardholder working mothers remain under the care of educators and ECEC officers during the working hours of their mothers, receive their food at the ECEC centre and carry out activities in accordance with institutional programmes." Inclusion criteria: ECEC centres that were selected had registered at least 40 children between the ages of 2 and 4 years and the respective directors agreed to participate in the study. All children of 2 and 3 years of age, regardless of their nutritional status, and attending the selected ECEC centres were deemed eligible. Children whose participation was accepted by their parents by way of written informed consent were included. Exclusion criteria: children with chronic conditions that interfere with their growth and which would prevent performing physical activity and consequently limit anthropometric measurements, or children with special food requirements, were excluded. Number of services randomised: 16 (8 intervention, 8 control) Number of children randomised: 674 (336 intervention, 338 control) Characteristics Children Age: Intervention: 32.9 months (SD 6.1) Control: 33.1 months (SD 6.1) Gender (% female): Intervention: 51.2% Control: 48.8% Ethnicity: not reported Parents Age (years): Intervention: 32.6 (SD 5.6) Control: 32.5 (SD 6.1) Gender (% female): 100% Ethnicity: not reported Parent/family SES: mother employment Intervention: full‐time (≥ 35 h/week): 73.7%; part‐time: 8.6%; full‐time rotary working day: 8.6%; full‐time double working day: 5.4%; non‐specified: 4.8% Control: full‐time (≥ 35 h/week): 73.7%; part‐time: 10.7%; full‐time rotary working day: 7.7%; full‐time double working day: 4.7%; non‐specified: 3.3% Home monthly income (MXN) Intervention: < MXN 5,000: 15.5%; MXN 5,000–MXN 15,000: 43.8%; MXN 15,001–MXN 25,000: 14.3%; > MXN 25,000: 5.4%; non‐specified: 21.1% Control: < MXN 5,000: 18.9%; MXN 5,000–MXN 15,000: 38.2%; MXN 15,001–MXN 25,000: 14.2%; > MXN 25,000: 6.2%; non‐specified: 22.5% Method of recruitment: not reported Missing data/dropout: not reported Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: not reported Number of conditions: 1 intervention, 1 control Intervention duration: 12 months Intervention setting: ECEC and home Intervention strategies: Health curriculum Children Education: ECEC officials, with support from educators, conducted 12 interactive educational sessions (1/week) with game dynamics for key eating behaviours and physical activity. Ethos and environment Children Exposure: children were introduced to a variety of healthy snacks and natural water and offered options of different foods and beverages. Children were also presented with purpose‐built games to encourage physical activity. ECEC staff Training: a 3‐d researcher‐led workshop was held (24 h in total) for the benefit of educators and ECEC officers, with the aim of facilitating the knowledge and skills required for the delivery of educational sessions for children and the promotion of their role in daily care. Service Resources: the material and equipment for each ECEC centre to perform the activities were provided. Partnerships Families Workshops: educators in ECEC centres, in collaboration with the ECEC officers and the research group, conducted an afternoon workshop every 2 months throughout the implementation period, with dynamics in which they communicated key messages to promote behaviour changes in accordance with whatever was touched on in the sessions with the children. Resources: during the workshop, parents developed posters with the monthly target of changes, included in meetings with the children as well as card games and short messages that were permanently available to the parents throughout the study. External provider Delivery: ECEC officials delivered the educational and training sessions. Intensity of intervention: 3 d (24 h) x teacher training; 12 x 1 h/week education sessions for children; 1 parent workshop every 2 months Intervention delivered by: research team, ECEC staff Modality: face‐to‐face, written Theoretical basis: not reported Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: Sugary water intake, plain water intake, fruit water intake, yogurt intake, fritters intake, hamburgers intake, hot dogs intake, processed juice intake, savoury milk intake, French fries intake, pizza intake, soft drink intake Number of participants analysed: Intervention baseline: 336 Intervention follow‐up: 366 Control baseline: 338 Control follow‐up: 287 Data collection measure: Frequency of food consumption (144 items), modified from the individual questionnaire of children aged 0‐9 years of the National Health and Nutrition Survey Data collector: parent Validity of measures used: not reported Outcomes relating to child physical measures: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: Consejo Nacional de Ciencia y Tecnología, No. S0008‐114027 (National Council for Science and Technology) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Each pair was randomised using a computerised procedure in order to assign a ECEC centre to intervention and non‐intervention groups. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | Child‐care staff and parents were not blinded to study allocation, and the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Parents reported children's dietary intake via questionnaire. Parents were not blinded to study allocation and the outcome measurement is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Unclear risk | Study authors stated that "It can be observed that there are differences in the number of children in each group stage because, throughout the study, there were admissions of children from other rooms that met two years of age and departures of others who completed 4 years old and who changed room or left the childcare center. Despite this replacement, the study sample was similar in number during the three stages." Risk of attrition bias is unclear. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting. |
| Recruitment bias | High risk | There are differences in the number of children participating in each of the 3 time points throughout the study, with numbers increasing among the intervention group between baseline and 6 months, and numbers increasing in the control group between 6 months and 12 months. Study authors state that "It can be observed that there are differences in the number of children in each group stage because, throughout the study, there were admissions of children from other rooms that met two years of age and departures of others who completed 4 years old and who changed room or left the childcare center." |
| Baseline imbalance | Low risk | No clear differences or imbalances between clusters noted |
| Loss of clusters | Unclear risk | Not sufficiently reported |
| Incorrect analysis | High risk | There was no accounting for clustering of children within centres. |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Roberts‐Gray 2018.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 22 weeks (varies with outcomes) Unit of allocation: centre Unit of analysis: child |
|
| Participants |
Service type: centre‐based Operation: not reported Country (region): USA (Texas) Country income classification: high Low‐SES sample: no Population description: metro areas Inclusion criteria: ECEC centres that required parents to supply bag lunches Exclusion criteria: not reported Number of services randomised: 30 (15 intervention, 15 control) Number of children randomised: 633 (351 intervention, 282 control) Characteristics Children Age: 3.51 years (SD 0.69) Gender (% female): 48.8% Ethnicity: white: 65.6%; Hispanic: 19.0%; other: 15.4% Parents Age (years): 36.44 (SD 5.48) Gender (% female): 90.1% Ethnicity: white: 71.5%; Hispanic: 18.0%; other: 10.5% Parent/family SES: Annual family income: < USD 19,999: 3.5%; USD 20,000‐USD 39,999: 7.6%; USD 40,000‐USD 59,999: 6%; USD 60,000‐USD 79,999: 10%; USD 80,000‐USD 99,999: 15.7%; > USD 100,000: 57.1% highest level of education: some high school: 1.6%; high school diploma/GED: 3%; some college: 13%; associate or Bachelors: 49.4%; Masters or Doctorate: 33% Method of recruitment: ECEC centres that required parents to supply bag lunches were recruited during 2010 and 2011 via telephone survey and snowball referral methods. Missing data/dropout: all 30 of the ECEC centres were retained in the study through the 28‐week follow‐up Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Lunch is in the bag (LunchBag) Number of conditions: 1 intervention, 1 control Intervention duration: 5‐week intervention, + one‐week booster (23 weeks later) Intervention setting: ECEC and home Intervention strategies: Health curriculum Children Education: teachers deliver activities to children during class including a project, a food‐related book to read at circle time, favourite food show‐and‐tell at 1 or 2 snack times, and daily using a “Lunch Colors” placemat to unpack the lunch bag and assess contents based on the My Plate groups. Ethos and environment Children Incentive: children received a 'Gold Medal Lunch' certificate to take home when their lunch bag contained food from all 5 of the My Plate groups. ECEC staff Training: the programme developers provided training to the teachers immediately prior to the intervention launch. Resources: classroom kit, which contains lesson plans and resources for teacher‐led activities to encourage and support the child's learning about the 5 MyPlate food groups. Notes provided for the teacher to send to the parents describing the plan for the week and requesting needed items. Newsletters and other materials provided to support the teachers. Service Resources: centre‐level kit includes newsletters (for distribution to parents), parent‐child activity stations (for centre director to install on‐site), calendar with intervention sequence within. Partnerships Families Resources: centres provided parents with newsletters, which present menu ideas, portion size information, goal setting and other home practice assignments, as well as suggestions for home‐based parent‐child fun‐focused nutrition learning activities. Intensity of intervention: implementation was estimated to demand approximately 3.25 h for the centre director and 3.5 h for the classroom teacher each week of intervention. Estimated engaged time when the intervention is implemented as designed is 16.5 h for the child accumulated at the rate of 2.75 h/week and 9 h for the parent accumulated at 1.5 h/week Intervention delivered by: research team, ECEC staff Modality: face‐to‐face, written Theoretical basis: Social Cognitive Theory, the Theory of Reasoned Action, and an ecological approach Description of control: wait‐list control |
|
| Outcomes |
Outcomes relating to child dietary intake: Vegetable intake, fruit intake, wholegrains intake, refined grains intake, meats/beans/eggs/nuts intake, dairy intake, chips intake, sweets intake Number of participants analysed: Intervention baseline: 325 Intervention follow‐up: 325 Control baseline: 253 Control follow‐up: 253 Data collection measure: observation Data collector: researcher Validity of measures used: validated Outcomes relating to child physical measures: BMI percentile Number of participants analysed: Intervention baseline: 325 Intervention follow‐up: 325 Control baseline: 253 Control follow‐up: 253 Data collection measure: objectively measured (CDC) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: funding for this study was made possible by the National Cancer Institute (National Cancer Institute/NIH Grant R01CA149643, Clinical Trial Number NCT01292434) and the Michael and Susan Dell Foundation through the Michael and Susan Dell Center for Healthy Living. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Centres were randomised to the intervention or to a wait‐list control condition. The sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Diet outcomes | Unclear risk | No blinding of participants and personnel to study allocation, and it is unclear whether lack of blinding would affect the outcome. For example, teachers could have encouraged their students to eat more of certain foods from their lunches on the days of observation, though this is unknown. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | No blinding of participants and personnel to study allocation, however the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | Low risk | Blinding not reported, however direct observation of the contents of the children's parent‐provided bagged lunches was conducted by trained observers using a structured food record. The outcome measurement is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured by the trained data collectors using standard protocols and the outcome measurements were not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Low risk | Study authors stated that "Nearly all (91%) [parent‐child dyads] were retained in the study through the 28‐week follow‐up." "Numbers of dyads with data at one or more of the lunch observations were 325 or 93% of those in the intervention condition and 253 or 90% of those in the control condition. Numbers of parents who answered the questionnaires at one or more of the measurement periods were 327 or 93% of those in the intervention and 250 or 89% of those in the control condition." Therefore, risk of attrition bias was considered to be low. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Study authors stated that "Nearly all (91%) [parent‐child dyads] were retained in the study through the 28‐week follow‐up." Therefore, risk of attrition bias was considered to be low. |
| Selective reporting (reporting bias) | Low risk | The reported outcomes aligned with those outlined in the trial registration. |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Low risk | The intervention condition had relatively larger proportion of Hispanic children and parents, fewer parents older than 34, fewer parents with overweight or obesity, more parents with college degree, fewer single parents, and higher annual family income. Statistical analyses of the outcomes data included adjustment for these demographic differences, with education preferred over income as a covariate because it had fewer missing values. |
| Loss of clusters | Low risk | No loss of clusters |
| Incorrect analysis | Low risk | Study authors stated that "Three‐level regression models were constructed to allow random effects at the centre level, as well as at the family level, within and across time periods." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Unclear risk | No conflict of interest statement was reported |
Seward 2018.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 6 months Unit of allocation: centre Unit of analysis: service |
|
| Participants |
Service type: centre‐based (long day care) Operation: not reported Country (region): Australia (New South Wales) Country income classification: high Low‐SES sample: no Population description: not reported Inclusion criteria: centres were eligible to participate in the trial if they had an onsite cook who prepared and provided at least 1 main meal and 2 mid‐meals to children attending the centre; were open ≥ 8 h each day; and the individual centre played a role in planning their own menu. Exclusion criteria: centres that did not prepare meals onsite or those catering exclusively for children requiring specialist care, mobile preschools, and family day care centres were excluded. Number of services randomised: 54 (26 intervention, 28 control) Number of children randomised: 395 (220 intervention, 175 control) Characteristics Children Age: Intervention: 3.5 years (SD 1.0) Control: 3.6 years (SD: 1.0) Gender (% female): Intervention: 47.7% Control: 47.6% Ethnicity: Children of Aboriginal or Torres Strait Islander background enrolled in service Intervention: 66.7% Control: 61.5% Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported ECEC staff (service cook) Age (years): Intervention: 43.0 (SD 10.2) Control: 45.2 (SD 11.7) Gender (% female): Intervention: 100% Control: 92.3% Ethnicity: not reported Service/ECEC staff SES: not reported Method of recruitment: mailed recruitment with follow‐up telephone invitation Missing data/dropout: of the 54 services in the study, 9 services (intervention, n = 1; control, n = 8) withdrew consent prior to baseline data collection and without knowledge of group allocation. Only 1 service did not complete follow‐up data collection. Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: not reported Number of conditions: 1 intervention, 1 control Intervention duration: 6 months Intervention setting: ECEC Intervention strategies: Ethos and environment ECEC staff Training: 1 d face‐to‐face menu planning workshop provided to service managers and cooks to improve staff knowledge and skills in the application of nutrition guidelines to child‐care food service. The workshop incorporated both didactic and interactive components, including small group discussions, case studies, review of existing menu items, facilitator feedback, and opportunities to practise new skills. Service Resources: services received a resource pack to support the implementation of nutrition guidelines, which includes the Caring for Children resource, menu planning checklists, recipe ideas and budgeting fact sheets. 2 x newsletters were also distributed. Support: services were allocated an implementation support officer to provide expert advice and assistance to facilitate guideline implementation. Each intervention service received 2 face‐to‐face contacts, following the menu planning workshop. Support contacts were provided to service managers and cooks. Audit and feedback: service menus were audited by a dietitian and feedback was provided at 2 time points (baseline and mid‐intervention). Intervention service cooks and service managers received written (email) and verbal (service visit) feedback following each menu assessment via their implementation support officer. Policy: the implementation support officer, the service manager and cook signed a memorandum of understanding outlining each party’s responsibilities in working to improve food service. Service managers were asked to communicate support and endorsement of adhering to nutrition guidelines to other staff and update the service nutrition policy accordingly. Partnerships Healthcare Delivery: experienced implementation support staff and dietitian facilitated staff training and policy support. Intensity of intervention: 1 x 6‐h training session; 1 x resource pack; 2 x newsletters; 2 x rounds of audit and feedback; 2 x face‐to‐face visits; 1 x written commitment for supervisors and cooks to implement the intervention. Intervention delivered by: research team, ECEC staff, healthcare staff Modality: face‐to‐face, telephone, online, written Theoretical basis: Theoretical Domains Framework Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: Vegetable intake, fruit intake, breads and cereals intake, meat, dairy intake, discretionary food intake, diet quality (total, vegetable intake, fruit intake, breads and cereals intake, meat, dairy intake, discretionary food intake, water intake, variety intake, healthy fats intake) Number of participants analysed: Intervention baseline: 15‐220 Intervention follow‐up: 13‐259 Control baseline: 13‐175 Control follow‐up: 12‐216 Data collection measure: plate waste and educator‐reported short‐food survey Data collector: researchers and educator Validity of measures used: not reported Outcomes relating to child physical measures: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: Negative feedbacks, % of meal waste Number of participants analysed: Intervention baseline: 22 services Intervention follow‐up: 22 services Control baseline: 16 services Control follow‐up: 16 services Data collection measure: cooks’ pen‐and‐paper questionnaire Data collector: service cook Validity of measures used: not reported |
|
| Notes | Funding source: priority Research Centre for Health Behaviour and received infrastructure funding from Hunter New England Population Health and the University of Newcastle. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation schedule for the main trial was prepared a priori by an independent statistician. Centres were randomised to the intervention or control group via block randomisation (block size ranged between 2 and 6), using a central conceal random allocation process. Of these, 25 centres were approached in random order using a random number list generated in Microsoft Excel and invited to participate in the nested study. |
| Allocation concealment (selection bias) | Low risk | Allocation was conducted by an independent statistician after recruitment. |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | The study was conducted as an open trial as it was not possible to blind the ECEC centre staff receiving the intervention. The outcome is likely to be influenced by the lack of blinding. |
| Blinding of participants and personnel (performance bias) Adverse consequences | Unclear risk | The study was conducted as an open trial as it was not possible to blind the ECEC centre staff receiving the intervention. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Children's dietary intake (outcomes which were included in meta‐analysis) was assessed via questionnaire by centre educators who were not blinded to group allocation. Study authors state that, "While educators were not specifically targeted by the intervention, this could have resulted in detection bias where centres were more likely to report favorable outcomes due to receipt of the intervention." |
| Blinding of outcome assessment (detection bias) Adverse consequences | Unclear risk | The study was conducted as an open trial as it was not possible to blind the ECEC centre staff receiving the intervention. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Unclear risk | Study authors stated that "there was a significant amount of missing data for the questionnaire with approximately 21% of children at baseline or follow‐up, missing at least one item on the record. However, no significant differences in child age or gender were found among children with and without missing data and multiple imputation and intention to treat analysis did not result in any changes to statistical significance of trial outcomes." Risk of attrition bias is unclear. |
| Incomplete outcome data (attrition bias) Cost | Low risk | Data were available for 38 of the 45 (84%) participating services. |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the paper were prespecified in the protocol paper. |
| Recruitment bias | Unclear risk | Baseline data collection occurred after randomisation of centres, however it is unclear whether individual recruitment occurred before or after randomisation. |
| Baseline imbalance | Unclear risk | There were no differences in age or sex between groups, but these are the only 2 individual‐level variables measured. |
| Loss of clusters | High risk | One intervention cluster lost to follow‐up, and 2 intervention clusters and 1‐2 control clusters did not provide questionnaire data at baseline and/or follow‐up |
| Incorrect analysis | Low risk | Study authors stated that "Group differences for all outcome data were assessed through a group by time interaction using generalized linear mixed models, adjusting for clustering within centres." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Unclear risk | Study authors stated that "Additionally, the self‐reported dietary measure required childcare educators to recall child diet over the past month and as such is subject to recall bias." There is insufficient information to assess whether an important risk of bias exists. |
Stookey 2017.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 1 year Unit of allocation: centre Unit of analysis: child |
|
| Participants |
Service type: centre‐based Operation: not reported Country (region): USA (San Francisco) Country income classification: high Low‐SES sample: yes Population description: ECEC centres that primarily serve low‐income children in San Francisco and do not have federal, state or school district funding. Inclusion criteria: all ECEC centres that participated in Child Care Health Program (CCHP) nutrition screenings in 2011–2012 were eligible. Exclusion criteria: ECEC centres that were closed in Autumn 2012 or declined Child Care Health Program (CCHP) services for 2012–2013 before the randomisation were ineligible for the Healthy Apple Program (HAP) pilot. Child‐care centres with funding from Head Start, the San Francisco Unified School District, or Community College District were ineligible to receive CCHP screenings, and excluded from the HAP pilot. ECEC centres that declined one or both BMI screenings in any given year were excluded from evaluation analyses for that year, because of missing data regarding the primary outcome of interest, annual change in BMI between the Autumn and Spring screenings. Children who declined 1 or both screenings or were absent on the date(s) of screening in any given year were excluded from evaluation analyses for that year. Number of services randomised: 43 (19 intervention, 24 control) Number of children randomised: 902 (522 intervention, 380 control) Characteristics Children Age: Intervention: 2 years: 5%; 3 years: 40%; 4 years: 54%; 5 years: 1% Control: 2 years: 14%; 3 years: 40%; 4 years: 45%; 5 years: 0% Gender (% female): not reported Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported Method of recruitment: the programme was offered to those centres that completed the Child Care Health Program. A USD 25 gift card was offered to 1 representative/child‐care centre for participation in the Healthy Apple Program pilot. Missing data/dropout: 6/43 centres had missing data at follow‐up (2 intervention, 4 control). Reasons for dropout: 3 ineligible for CCHP BMI screenings (1 intervention, 2 control) and 3 declined 1 or both CCHP BMI screenings for the year (1 intervention, 2 control) Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Healthy Apple Program (HAP) Number of conditions: 1 intervention, 1 control Intervention duration: 6 months Intervention setting: ECEC Intervention strategies: Health curriculum Children Education: children received nutrition education (circle time for children). Ethos and environment ECEC staff Training: public health nurses or health workers introduced the HAP resources and process, in‐person, to child‐care centre staff and spent up to 16 h per ECEC centre, providing one‐on‐one support to each ECEC provider about the programme. Workshops: 2 x optional, tailored workshops (1 on nutrition, 1 on physical activity) to address participant needs Service Resources: Healthy Apple Program (HAP) resources included an invitation packet, which included information about the HAP, a self‐assessment for ECEC providers, and information about the gift card incentive for completing the self‐assessment. The HAP resources also included a goal‐setting worksheet, hard copy Tip Sheets and online technical assistance materials. Incentive: a USD 25 gift card was offered to 1 representative/ECEC centre for participation in the study. Partnerships Healthcare Health checks: bi‐annual BMI screenings offered by public health nurses or health workers at ECEC centres. Community Co‐ordination: citywide co‐ordination of quality improvement processes for ECEC providers. Intensity of intervention: up to 16 h staff training; 2 x optional workshops Intervention delivered by: ECEC staff, healthcare staff Modality: face‐to‐face, online, written Theoretical basis: not reported Description of control: delayed intervention control, plus included bi‐annual BMI screening; health education; dental and nutrition screening |
|
| Outcomes |
Outcomes relating to child dietary intake: not reported Outcomes relating to child physical measures: Annual change in BMI percentile, annual change in BMI z‐score Number of participants analysed: unclear Data collection measure: objectively measured (CDC) Data collector: health workers Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: Total operation cost, time Number of participants analysed: not reported Data collection measure: not reported Data collector: not reported Validity of measures used: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: CDC Community Transformation Grant. Funding for the HAP pilot evaluation was provided by the Feeling Good Project, funded by USDA SNAP‐Ed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | For each health worker, eligible ECEC centres were listed in alphabetical order. A list of the same length, of random, unique, unsorted numbers was generated using randomizer.org. For each health worker, ECEC centres had an equal chance of being assigned to 1 of 2 intervention groups. |
| Allocation concealment (selection bias) | Low risk | Baseline data collected before cluster randomisation |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | The programme health workers and ECEC providers were not blinded to treatment allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Cost | Unclear risk | The programme health workers and ECEC providers were not blinded to treatment allocation. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | No blinding of outcome assessors, however children's height and weight were measured using a standardised protocol and calibrated instruments, and are unlikely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Cost | Unclear risk | No blinding of outcome assessors. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Physical outcomes | High risk | The number of ECEC centres and children included in the HAP evaluation analysis varied each year, depending on the availability of BMI change data (primary outcome). Study authors stated that "Due to lack of unique child identifiers across child care centres, the analysis did not track the BMI changes of the same children across years." As a result, the risk of bias was assessed as high. |
| Incomplete outcome data (attrition bias) Cost | Low risk | The outcome was collected as an average cost per service. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting. |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Unclear risk | Children's income, race, ethnicity, and social determinants of health were unknown and not controlled for in the research design or analysis. |
| Loss of clusters | High risk | 9 of the 19 centres in the intervention group did not receive the allocated intervention. 7 of the 24 centres in the control group did not receive the allocated intervention. Loss of 6 clusters in Year 1 and 9 clusters in Year 2 |
| Incorrect analysis | Low risk | Study authors stated that "The Child Care Health Program + HAP vs. Child Care Health Program + HAP Delayed groups were compared in intention‐to‐treat analyses, which accounted for clustered data. Year‐specific hierarchical linear models used child‐level data to test for a main effect of time between the Autumn to Spring screenings." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | High risk | Study authors stated that "Many potentially confounding and/or effect modifying factors, including local, statewide, and National initiatives, were operating in the background during the HAP pilot evaluation period." (Detailed explanation in study.) Authors also stated that "Randomization may not have eliminated bias related to treatment assignment, due to the relatively small number of child care centres and uneven demographic distribution across child care centres. Randomisation would not have controlled for time‐varying factors that happened to correlate with HAP exposure, and independently predict changes in child BMI." |
Toussaint 2021.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 9 months Unit of allocation: preschool Unit of analysis: child |
|
| Participants |
Service type: centre‐based (preschools) Operation: not reported Country (region): The Netherlands (Amsterdam Nieuw‐West) Country income classification: high Low‐SES sample: yes Population description: the sample comprised preschools of the largest ECEC organisation in the deprived area Amsterdam Nieuw‐West, the Netherlands. Nieuw‐West is characterised by inhabitants with a migration background and low SES. Inclusion criteria: toddlers and their parents were included if the toddler was 2.5‐3.5 years old. Exclusion criteria: ECEC teachers who worked at multiple preschool locations were excluded. Number of services randomised: 41 (21 intervention, 20 control) Number of children randomised: 249 (137 intervention, 112 control) Characteristics Children Age: 3.0 years (SD 0.2) Gender (% female): 49% Ethnicity: Dutch: 19%; Moroccan: 35%; Turkish: 18%; other Western: 9%; other non‐Western: 20% Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: lower education: 20%; intermediate education: 43%; higher education: 37% ECEC staff (teachers) Age (years): 42 (SD 9.0) Gender (% female): 100% Ethnicity: Dutch: 38%; Moroccan: 33%; Turkish: 7%; other Western: 11%; other non‐Western: 11% Service/ECEC staff SES: lower education: 0%; intermediate education: 73%; higher education: 28% Method of recruitment: all ECEC teachers (n = 162) at the 41 included preschools were approached via information meetings. Parents were individually approached (face‐to‐face) at preschools by the research staff in close co‐operation with the centre. Missing data/dropout: 7 teachers dropped out of the study: 6 teachers in the control group and 1 teacher in the intervention. Reasons for dropout: teachers in the control group indicated that the measurements were too time consuming/invasive, 2 teachers in the control group were no longer working at the participating child‐care organisation, and 1 teacher in both the intervention and control group withdrew their consent to participate in the study. Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: a Healthy Start and PLAYgrounds for TODdlers (2 separate programmes applied in succession) Number of conditions: 1 intervention, 1 control Intervention duration: 9 months Intervention setting: ECEC Intervention strategies: Ethos and environment ECEC staff Education: the first programme was A Healthy Start: 3 x 2‐h face‐to‐face meetings organised for 8 groups of ECEC teachers (led by 1 of the coaches and a member of the research staff) including theory and practical assignments from the basic national 'A Healthy Start' module about a healthy ECEC environment and in‐depth national A Healthy Start modules about nutrition, physical activity and body weight. First meeting focused on self‐reflection; second meeting focused on interaction with children; and the third meeting focused on interaction with parents. The second programme was PLAYgrounds for TODdlers (PLAYTOD): 2 x 2‐h face‐to‐face training sessions organised for 4 groups of ECEC teachers. Each meeting was led by 2 certified PLAYTOD trainers. The first training session included theory about the importance of (outdoor) physical activity and a basic inviting structure of the playground (with the use of different activity zones) for variation in fundamental movement skills was demonstrated and practiced. Coaching: after 2 weeks of the second program, ECEC teachers received a coaching on‐the‐ job session. In the second training session, the activating role of the teachers (prompts) on the playground was practiced and reviewed in more detail. Incentive: ECEC teachers who attended at least 2 meetings of A Healthy Start and 1 training session of PLAYTOD received certificates. Partnerships External provider Delivery: coaches and PLAYTOD trainers delivered the meetings. Intensity of intervention: 3 x 2 A Healthy Start meetings; 2 x 2 h training sessions; 1 x on‐the‐job session Intervention delivered by: research team, ECEC staff Modality: face‐to‐face Theoretical basis: not reported Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: not reported Outcomes relating to child physical measures: BMI z‐score, BMI, fat‐free index, fat‐free mass index Number of participants analysed: Intervention baseline: 64‐101 Intervention follow‐up: 64‐101 Control baseline: 62‐93 Control follow‐up: 62‐93 Data collection measure: objectively measured (WHO) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: the study was funded by ‘Nationaal Regieorgaan Praktijkgericht Onderzoek SIA’, grant no. 2015‐02‐07P (www.regieorgaan‐sia.nl) (PJMW). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Study authors stated that "The randomisation was performed by an independent researcher with the use of computer‐generated lists." |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, ECEC service staff delivering the intervention were not blind to the study allocation. The study team was co‐ordinated by 3 unblinded researchers and 1 blinded researcher. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Children's height and weight were measured by trained research staff and students, though blinding was not reported. The study team was co‐ordinated by 3 unblinded researchers and 1 blinded researcher, however the outcome is not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Physical outcomes | Unclear risk | At baseline, 137 students were allocated to intervention and 112 students to control. However, only 101 students (74%) were analysed from the intervention group and 93 students (83%) from the control group. Not all missing data accounted for, and it is unclear if the reasons for missing data are similar between groups. |
| Selective reporting (reporting bias) | High risk | Study authors states in the protocol that "Parents will be asked to fill in the 3‐day food record for their toddler on 2 week days and 1 weekend day... The intake of foods will be converted (by coding and converting household measures into grams) into energy and nutrient intake using the Dutch Food Composition Database 2016 and a database with portion sizes." These findings were not reported because the authors stated that "For children, the recorded intake of foods and physical activities were not included in further analysis, as most of the parents did not fill in the records (or, at least not adequately)." |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Unclear risk | Models were adjusted for sex, age, and ethnicity, however, it is unclear whether additional baseline differences between children in the intervention and control exist as statistical comparisons were not reported between groups. |
| Loss of clusters | Unclear risk | 2 clusters were lost from the intervention group due to discontinued intervention. However, this was a small proportion of clusters and ITT analyses were used. |
| Incorrect analysis | Low risk | Study authors stated that "preschool location was added as random intercept to take into account the clustered data structure." |
| Contamination | Low risk | Protocol states that "In total, 42 preschools of child care organization Impuls were available for allocation. One location was excluded because of practical reasons and 4 preschools were combined in the allocation as they shared a building or playground." Additionally, "ECEC teachers who worked at multiple preschool locations were excluded." |
| Other bias | Unclear risk | No conflict of interest statement was reported. |
Vaughn 2021.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 8‐10 months Unit of allocation: centre Unit of analysis: child |
|
| Participants |
Service type: centre‐based Operation: not reported Country (region): USA (North Carolina) Country income classification: high Low‐SES sample: unclear Population description: Central North Carolina, including a mix of rural and suburban counties Inclusion criteria: centres having a 3–4‐year‐old classroom, having a 3–5‐star quality rating or being exempt from rating, providing lunch, not exclusively serving children with special needs Exclusion criteria: at least 7 parents had to sign consent for the centre to remain eligible. Number of services randomised: 92 (48 intervention, 44 control) Number of children randomised: 853 (446 intervention, 407 control) Characteristics Children Age: 47.93 months (SD 6.96) Gender (% female): 49.20% Ethnicity: white: 46.4%; black or African American: 36.3%; other: 17.4%; Latino ethnicity: 8.6% Parents Age (years): 33.46 (SD 7.82) Gender (% female): 85.30% Ethnicity: white: 53.3%; black or African American: 36.9%; other: 9.8% Latino ethnicity: 6.2% Parent/family SES: family income: under USD 30,000: 28.1%; USD 30,000‐USD 59,999: 18.3%; USD 60,000: 37.9%; Prefer not to answer: 15.7% Method of recruitment: community organisations shared information about the study with local centre directors and endorsed participation. Research staff followed‐up by phone to gauge initial interest and eligibility, and then in person to verify interest and obtain a Memorandum of Understanding. Information packets were shared with eligible classroom teachers (i.e. teachers of 3–4 year‐olds, able to write/speak English). At least 1 teacher had to sign consent for the centre to remain eligible. Research staff worked with participating teachers to distribute similar packets to eligible parents (i.e. parent of a 3–4 year old, able to write/speak English) and conduct in‐person visits to answer questions and collect written consent. At least 7 parents had to sign consent for the centre to remain eligible. Missing data/dropout: not reported Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Healthy Me, Healthy We Number of conditions: 1 intervention, 1 control Intervention duration: 8 months Intervention setting: ECEC Intervention strategies: Health curriculum Children Education: as part of the kick‐off event, the classroom activity involved the Healthy Me, Healthy We theme song and dance. Plus, 4 x 6‐week units where teachers used activity cue cards to lead 8 classroom activities to build children’s knowledge and skills. Ethos and environment Children Resources: a welcome letter from Dr. Fitbodi (Healthy Me, Healthy We mascot) was added in wave 2 to help teachers introduce the campaign. ECEC staff Training: directors and teachers received 2 x training sessions (5 h total) to support centres’ ability to deliver the campaign. Support: 3 x informal check‐ins (< 1 h) by the study interventionist to deliver programme materials, offer technical assistance and inquire about event planning Resources: in wave 2, teachers received an outreach toolkit with resources to boost parent engagement (e.g. social media posts about classroom activities). Service Environment: hanging the Healthy Me, Healthy We centre banner and classroom posters (1 per classroom). Event: the campaign initiated with a kick‐off event and concluded with a celebration event (promoting the event to parents, displaying a certificate of completion, having teachers wear Healthy Me, Healthy We buttons, posting pictures of activities, having children perform the Healthy Me, Healthy We song, and awarding children Healthy Me, Healthy We ribbons). Partnerships Families Invitation: sending invitations to parents, signing the Fit Family Promise (at school and at home) Resources: teachers distributed Our Turn cards to prompt parents to do at‐home activities. Parents received a Family Guide magazine at the start of each unit that introduced unit goals, presented benefits of healthier behaviours, encouraged practices to support healthier behaviours, and offered at‐home activities. Parents received an activity tracker to log at‐home activities. Intensity of intervention: 4 x 6‐week units for children; 2 x teacher training sessions (3 h and 2 h); 3 x check‐ins (< 60 min); 1 conclusion event Intervention delivered by: research team, ECEC staff Modality: face‐to‐face, online, written Theoretical basis: development was guided by Social Marketing Approach and informed by the Social Ecological Framework, Exchange Theory, and Social Cognitive Theory Description of control: wait‐list control |
|
| Outcomes |
Outcomes relating to child dietary intake: Diet quality (total) Number of participants analysed: Intervention baseline: 446 Intervention follow‐up: 446 Control baseline: 407 Control follow‐up: 407 Data collection measure: combination of observation (using the Diet Observation in Child Care protocol) and parent‐completed food diary Data collector: researchers and parent Validity of measures used: not reported Outcomes relating to child physical measures: BMI, BMI z‐score Number of participants analysed: Intervention baseline: 446 Intervention follow‐up: 446 Control baseline: 407 Control follow‐up: 407 Data collection measure: objectively measured (CDC) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: funded by the National Heart, Lung and Blood Institute [R01HL120969]. Support was also received from the Center for Disease Control and Prevention [U48DP005017] and National Institute of Diabetes and Digestive and Kidney Diseases [P30DK056350]. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Centres were stratified by county, and the study statistician created randomisation tables using a permuted block approach (with blocks of 2 and 4). The project manager used these tables to assign centres to the intervention or control arm. |
| Allocation concealment (selection bias) | Low risk | Randomisation occurred on a rolling basis after baseline measures were collected and sufficient data had been confirmed (i.e. at least 7 children per centre with usable diet and physical activity data). |
| Blinding of participants and personnel (performance bias) Diet outcomes | Unclear risk | Only the study statistician, project manager, and those delivering the intervention knew allocation assignments. Investigators and data collectors remained blind to study allocation. Teachers were not blind to the treatment, and it is unclear whether the outcome could be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | Only the study statistician, project manager, and those delivering the intervention knew allocation assignments. Investigators and data collectors remained blind to study allocation. The outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | Unclear risk | Parents recorded children's dietary intake in food diaries, and intake at child care was assessed by research staff using the Diet Observation in Child Care protocol. Parent‐reported outcome may be influenced by lack of blinding. Even though research staff were blinded to assignment, intervention posters were hung in the intervention classrooms and could have led to broken blinding for observers. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Children's height, weight, and waist circumference were measured by research staff who were blinded to group assignment. |
| Incomplete outcome data (attrition bias) Diet outcomes | Unclear risk | Study authors stated that "Hypotheses were tested under the intent‐to‐treat (ITT) principle using Generalized Linear Mixed Models (GLMM)." However, information on missing data is not reported. Risk of attrition bias is unclear. |
| Incomplete outcome data (attrition bias) Physical outcomes | Unclear risk | Study authors stated that "Hypotheses were tested under the intent‐to‐treat (ITT) principle using Generalized Linear Mixed Models (GLMM)." However, information on missing data is not reported. Risk of attrition bias is unclear. |
| Selective reporting (reporting bias) | Unclear risk | Waist circumference mentioned in protocol and methods of study, but findings not reported |
| Recruitment bias | Low risk | Randomisation occurred on a rolling basis once baseline measures were collected and sufficient data had been confirmed (i.e. at least 7 children/centre with usable diet and physical activity data). |
| Baseline imbalance | Low risk | There were slight differences between arms in terms of children’s Latino ethnicity (P = 0.02), family income (P = 0.03), and parents’ marital status (P = 0.04). These variables were incorporated as covariates in fully adjusted models. |
| Loss of clusters | Unclear risk | Not sufficiently reported |
| Incorrect analysis | Low risk | Study authors stated that "Hypotheses were tested under the intent‐to‐treat (ITT) principle using Generalized Linear Mixed Models (GLMM) that accounted for the correlation induced by the clustering of children within the childcare centres. Models did not account for clustering of children within classrooms as it is common for children to move between classrooms; hence, this level of clustering was not tracked." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Vereecken 2009.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 6 months Unit of allocation: preschools Unit of analysis: child |
|
| Participants |
Service type: centre‐based (preschools) Operation: not reported Country (region): Belgium (Flanders) Country income classification: high Low‐SES sample: unclear Population description: not reported Inclusion criteria: not reported Exclusion criteria: not reported Number of services randomised: 16 (8 intervention, 8 control) Number of children randomised: 1432 (867 intervention, 565 control) at baseline Characteristics Children Age: Intervention year of birth: < 2002: 41%; 2002: 28%; ≥ 2003: 31% Control year of birth: < 2002: 51%; 2002: 24%; ≥ 2003: 26%. Gender (% female): Intervention: 53% Control girls: 44% Ethnicity: not reported Parents Age (years): not reported Gender (% female): Intervention: 94% Control: 95% Ethnicity: not reported Parent/family SES: Mothers' education Intervention: low (secondary school or less): 49%; medium (Bachelor): 34%; high (Bachelor with supplementary education or Masters): 16% Control: low (secondary school or less): 49%; medium (Bachelor): 35%; high: (Bachelor with supplementary education or Masters): 16% Fathers' education Intervention: low (secondary school or less): 60%; medium (Bachelor): 22%; high (Bachelor with supplementary education or Masters): 18% Control: low (secondary school or less): 57%; medium (Bachelor): 26%; high (Bachelor with supplementary education or Masters): 17% Method of recruitment: schools were asked by mail if they would be willing to participate in an intervention study to promote healthy eating. Missing data/dropout: 46% returned a completed questionnaire at follow‐up Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Beastly Healthy at School Number of conditions: 1 intervention, 1 control Intervention duration: 6 months Intervention setting: ECEC and home Intervention strategies: Health curriculum Children Education: developmental education (e.g. explanation of concepts of food triangle) Ethos and environment Children Exposure: guided and self‐guided activities based on experiential education (e.g. tasting). Healthy foods made available to children Support: role model, feedback and reinforcement by teachers Resources: cooking equipment made available to children (for use under supervision) ECEC staff Training: 2 x full‐day training sessions for principals and cafeteria staff Resources: an educational package, including an educational map for the teachers, an educative story and educational material (e.g. life‐size food education model based on the Flemish “Active Food Triangle”) was developed. Food messages and newsletters directed at the school staff were provided. A digital learning environment was provided. Support: group discussions with teachers; help on demand via email; examples of good practices. Audit and feedback: feedback provided to schools. Partnerships Families Resources: parents were provided with food messages and newsletters, and work sheets and creations by children. Activities/meetings: parent evenings and other school activities with parents Intensity of intervention: 2 d staff training; support on demand was offered via email; child curriculum (frequency and duration not reported) Intervention delivered by: research team, ECEC staff Modality: face‐to‐face, online, written Theoretical basis: The Intervention Mapping Protocol Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: Water intake, fruit juice intake, sugared soft drinks intake, sugared milks intake, milk intake, fresh fruit intake, snacks intake, vegetable intake Number of participants analysed: Intervention baseline: 308‐618 Intervention follow‐up: 308‐618 Control baseline: 168‐445 Control follow‐up: 168‐445 Data collection measure: FFQ and teachers' audit Data collector: parent and teacher Validity of measures used: validated (FFQ) and not reported (teachers audit) Outcomes relating to child physical measures: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: the development of the intervention was funded by the PWO (Project‐related Scientific Research)‐funding of University College Arteveldehogeschool. Funds for the evaluation were provided by the Provincial Government East‐Flanders. Carine Vereecken is a postdoctoral researcher funded by the Research Foundation–Flanders (FWO–Flanders). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 8 control and 8 intervention schools were randomly selected and stratified on school authority, location, and size of the school. For 1 school in the intervention group, 3 departments at different locations participated. The sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Low risk | Recruitment materials indicated there was a 50% chance that schools be randomised to the control group. |
| Blinding of participants and personnel (performance bias) Diet outcomes | High risk | We assumed that due to the nature of the intervention, ECEC service staff and study personnel delivering the intervention were not blind to the study allocation. The outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | High risk | Parents reported children's dietary intake, and data on available snacks and drinks were recorded by the teachers on a pre‐defined list. Parents and teachers were not blinded to treatment allocation and the outcome measurement is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | High risk | Study authors stated that "Of all children approached at baseline (n = 1432) and follow‐up (1637), respectively 884 (62%) and 761 (46%) returned a completed questionnaire; of whom 570 could be matched. Only those completed by the same respondent at both measurement occasions were kept for analyses: 308 intervention children and 168 control children." Due to the magnitude of missing data, the risk of bias was assessed as high. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting. |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Unclear risk | Study authors state that "The control group contained considerably (borderline significantly) more boys and children from the youngest age group." Analyses of the FFQs were controlled for gender of the child and year of birth, however no other baseline data were reported (only gender, year of birth, education of mother and father, and who completed the FFQ were reported). There may be unmeasured differences between groups. |
| Loss of clusters | Unclear risk | Not reported |
| Incorrect analysis | Unclear risk | Study authors stated that "Linear mixed models (SPSS 15.0) were used to investigate the effect of the condition on changes in consumption and food policy aspects." No further information is provided. There is not enough information to assess whether an important risk of bias exists. |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Unclear risk | No conflict of interest statement was reported. |
Ward 2020a.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 9 months Unit of allocation: family child‐care homes (i.e. family day care) Unit of analysis: child |
|
| Participants |
Service type: family child‐care homes Operation: not reported Country (region): USA (North Carolina) Country income classification: high Low‐SES sample: yes Population description: counties across central North Carolina; to help target family child‐care homes in high‐need areas, recruitment efforts focus primarily on counties with a higher‐than‐average prevalence of childhood overweight and obesity among children aged 2‐4 years and below average median household income. Inclusion criteria: eligible family child‐care homes must have had at least 2 children currently enrolled who are between the ages of 18 months and 4 years (but not entering kindergarten before follow‐up measures), serve at least 1 meal and 1 snack to children, and have been in business for 2 years (as a demonstration of business stability) with no plans to close in the coming year. Exclusion criteria: not reported Number of services randomised: 166 (83 intervention, 83 control) Number of children randomised: 496 (242 intervention, 254 control) Characteristics Children Age: 35.7 months (SD 11.4) Gender (% female): 50.4% Ethnicity: black or African American: 63.3%; white: 27.2%; other: 9.5%; Hispanic or Latino: 4.1% Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES not reported ECEC staff (family child‐care home provider) Age (years): 49.3 (SD 9.1) Gender (% female): Ethnicity: black or African American: 74.1%; white: 18.1%; other: 7.8%; Hispanic or Latino: 4.8% Service/ECEC staff SES: education high school diploma or GED: 24.7%; Associate's degree or 60 h college credit: 49.4%; Bachelor's degree or greater: 25.3% Method of recruitment: community partners shared information about the project with local family child‐care homes. Then, study staff followed up with family child‐care home providers via mail, email, and telephone to invite study participation. During telephone follow‐ups, family child‐care homes were screened for eligibility (i.e. enrolling at least 2 children aged 1.5–4 years, providing at least 1 meal and snack/day, being open year‐round, and having been in business for 2 years with no plans to close in the coming year). Study staff then visited eligible family child‐care home providers to explain study details and obtain written informed consent. Study staff worked through the family child‐care home provider to share study information with parents (including project contact information for questions) and collect informed consent. Missing data/dropout: at postintervention 38% were lost to follow‐up. Reasons for dropout: children no longer being enrolled in the family child‐care home, or family child‐care home providers refusing to participate in measures. Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Keys to Healthy Family Child Care Homes Number of conditions: 1 intervention, 1 control Intervention duration: 9 months Intervention setting: family child‐care home Intervention strategies: Ethos and environment ECEC staff Education: module 1 focuses on the provider's own health behaviours and encourages comparison against current recommendations; module 2 focuses on comparing current practices of family child‐care homes against recommendations and identifying areas of improvement; module 3 targets financial, record keeping for tax purposes, creating and enforcing policies and contracts, communicating with parents, professionalism, and marketing. Workshops: 3 x 3‐h face‐to‐face group workshops (1 on each module: Healthy You, Healthy Home, Healthy Business) delivered by health coaches. Resources: 3 x set of educational materials and toolkit resources (per module). Resources include pedometers, re‐useable water cups, child‐sized divided plates, poly spots, diet and physical activity‐related book. Support: 12 x one‐on‐one coaching contacts (lasting approximately 30‐45 min) via face‐to‐face and phone/email (4/module) employing motivational interviewing techniques. During each contact, the health behaviour coach works with the provider to review current goals, assess progress toward goals, problem‐solve around any barriers that might be encountered, and revise action plans as needed. Participants are provided with tracking sheets and encouraged to self‐monitor on a daily or weekly basis to help them stay on track. Partnerships Healthcare Delivery: health coaches delivered staff workshops and provided support. Intensity of intervention: 3 x workshops; 3 x home visits; 9 x phone calls Intervention delivered by: research team, ECEC staff, healthcare staff Modality: face‐to‐face, telephone, online, written Theoretical basis: the Socio‐ecologic Framework, Social Cognitive Theory and Self Determination Theory Description of control: alternative intervention control (a business‐focused intervention) |
|
| Outcomes |
Outcomes relating to child dietary intake: Diet quality (total, total fruit intake, whole fruit intake, total vegetables intake, greens and beans intake, whole grains intake, dairy intake, total protein intake, seafood and plant protein intake, fatty acids intake, sodium intake, empty calories intake) Number of participants analysed: Intervention baseline: 242 Intervention follow‐up: 149 Control baseline: 253 Control follow‐up: 142 Data collection measure: diet observation in child‐care protocol Data collector: data collectors Validity of measures used: not reported Outcomes relating to child physical measures: BMI, BMI percentile Number of participants analysed: Intervention baseline: 242 Intervention follow‐up: 149 Control baseline: 253 Control follow‐up: 142 Data collection measure: objectively measured (CDC) Data collector: data collectors Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: National Heart, Lung, and Blood Institute (HL108390), the Centers for Disease Control and Prevention (U48‐DP005017), and the National Institute of Diabetes and Digestive and Kidney Diseases (DK056350) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The study statistician used computerised block randomisation to assign family child‐care homes into either the intervention or control arm (1:1) (SAS 9.3, Cary, NC). |
| Allocation concealment (selection bias) | Low risk | Baseline data collected before cluster randomisation |
| Blinding of participants and personnel (performance bias) Diet outcomes | Unclear risk | We assumed that due to the nature of the intervention, teachers were not blind to the study allocation. It is unclear whether the outcome could be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | We assumed that due to the nature of the intervention, teachers were not blind to the study allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | Low risk | Children's diet quality was estimated from observed intakes of food and beverages collected via the Diet Observation in Child Care protocol by data collectors who were blinded to arm assignment. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Children's height, weight, and waist circumference were measured by data collectors who were blinded to arm assignment. |
| Incomplete outcome data (attrition bias) Diet outcomes | Low risk | Data were available for 149 (62%) children in the intervention group and 142 (56%) children in the control group. Most (84%) of the missing data are due to children no longer being enrolled in the service. Study authors stated that "To address missing child‐level data, multiple imputation was used, models were re‐run, and results were compared against the original. One hundred samples were imputed and analyzed in SAS (Proc MI) using available physical activity, HEI [healthy eating index], and covariate data. Comparison of baseline data from completers and non‐completers suggests that data are missing at random." Therefore, risk of attrition bias was considered to be low. |
| Incomplete outcome data (attrition bias) Physical outcomes | Low risk | Data were available for 149 (62%) children in the intervention group and 142 (56%) children in the control group. Most (84%) of the missing data are due to children no longer being enrolled in the service. Study authors stated that "To address missing child‐level data, multiple imputation was used, models were re‐run, and results were compared against the original. One hundred samples were imputed and analyzed in SAS (Proc MI) using available physical activity, HEI [healthy eating index], and covariate data. Comparison of baseline data from completers and non‐completers suggests that data are missing at random." Therefore, risk of attrition bias was considered to be low. |
| Selective reporting (reporting bias) | Unclear risk | Waist circumference mentioned in protocol and methods of study, but findings not reported |
| Recruitment bias | Unclear risk | Study authors stated that "Participants included a convenience sample of family child care home providers in central North Carolina and children aged 1.5‐4 years enrolled in these family child care homes, recruited in five cohorts over 2 years." Although randomisation occurred after baseline data collection, it is unclear if additional children were recruited from the same cluster. |
| Baseline imbalance | Unclear risk | Baseline differences between groups were not reported. Models of child‐level outcomes included child age, sex, and BMI as covariates. |
| Loss of clusters | Unclear risk | Loss of 3 intervention clusters (8 children) and 4 control clusters (11 children). Loss was a small percentage (< 5%) of the overall sample |
| Incorrect analysis | Low risk | Study authors stated that "Models of child‐level outcomes accounted for clustering; included child age, sex, and BMI as covariates; and for primary outcomes (HEI [healthy eating index score], MVPA [moderate‐to‐vigorous physical activity/hour]) used p values < 0.025." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Witt 2012.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 3 months Unit of allocation: centre Unit of analysis: child |
|
| Participants |
Service type: centre‐based Operation: all classrooms offered half‐day or full‐day care. All classrooms participated in the child and adult care food program and provided meals and snacks to children. Country (region): USA (not reported) Country income classification: high Low‐SES sample: yes Population description: 15/17 of the classrooms were from the Boise School District’s ECEC programme. Inclusion criteria: not reported Exclusion criteria: not reported Number of services randomised: 17 (10 intervention, 7 control) Number of children randomised: 263 (165 intervention, 98 control) Characteristics Children Age: the majority of children were 4 or 5 years old. Gender (% female): 47% Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported ECEC staff (lead teachers) Age (years): not reported Gender (% female): 94% Ethnicity: not reported Service/ECEC staff SES: not reported Method of recruitment: not reported Missing data/dropout: unclear Reasons for dropout: either absent or unenrolled from the centre at follow‐up assessments Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Color Me Healthy Number of conditions: 1 intervention, 1 control Intervention duration: 6 weeks Intervention setting: ECEC Intervention strategies: Health curriculum Children Education: 12 circle‐time lessons and 6 imaginary trips, using colour, music and exploration of the senses to teach children about healthy eating and physical activity. The majority of the Color Me Healthy circle‐time lessons focus on fruits and vegetables of different colours. Ethos and environment Children Exposure: several of the lessons provide opportunities for children to try (taste) fruits and vegetables. The imaginary trips allowed children to be physically active and role‐play eating nutritious food. ECEC staff Training: lead teachers attended a training session that was held prior to programme implementation. The teachers learned about the curriculum and were instructed on how to teach each lesson and imaginary trip. Materials: a ‘‘toolkit’’ that includes a teacher’s guide, 4 sets of picture cards, classroom posters, a music CD that contains 7 original songs, a hand stamp, and reproducible parent newsletters. Most of the kit materials emphasise fruits and vegetables of different colours. Partnerships Families Resources: 6 interactive take‐home activities for parents and children to complete. Parent newsletters. Intensity of intervention: 2 circle‐time lessons and 1 imaginary trip were taught to the children each week for 15‐30 min; staff training (frequency and duration not reported) Intervention delivered by: ECEC staff Modality: face‐to‐face, written Theoretical basis: not reported Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: Fruit snack intake, pineapple intake, cantaloupe intake, strawberry intake, purple grapes intake, vegetable snack intake, carrot intake, cherry tomato intake, celery intake, broccoli intake, Ritz cracker intake, graham cracker intake Number of participants analysed: Intervention baseline: 70‐83 Intervention follow‐up: 70‐83 Control baseline: 52‐70 Control follow‐up: 52‐70 Data collection measure: plate weight before and after Data collector: not reported Validity of measures used: not reported Outcomes relating to child physical measures: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 17 preschool classrooms were randomly assigned to 1 of 2 groups. The sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Diet outcomes | Unclear risk | No clear blinding of participants and personnel to study allocation, however teachers were instructed to avoid commenting on the snack and avoid encouraging children to eat the snack during outcome assessment. |
| Blinding of outcome assessment (detection bias) Diet outcomes | Low risk | Blinding not reported, however children's consumption was measured by weighing the fruit and vegetable snacks before and after intake. The outcome measurement is not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | High risk | Data for fruit snacks were available for 83 (50%) children in the intervention group and 70 (71%) children in the control group, while data for vegetable snacks were available for 70 (42%) children in the intervention group and 52 (53%) children in the control group. Although some reasons for loss provided, it is not known whether those reasons are exhaustive or equally distributed between treatment groups. Due to the magnitude of missing data and difference in the proportions of participants followed up between groups, the risk of bias was assessed as high. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting. |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Unclear risk | Baseline differences between groups were not reported. |
| Loss of clusters | Unclear risk | Not reported |
| Incorrect analysis | Low risk | Study authors stated that "The study design was a 3‐level design: the first level was the repeated measures; the second level included child variables; and the third level included classroom and teacher variables." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | High risk | There is insufficient information to draw conclusions. Study authors stated that "Two hundred sixty‐three parents were invited to participate in the evaluation, and 38% (n=100) completed the initial surveys, which assessed changes in children’s fruit and vegetable consumption in the home environment and included a 3‐day food diary, food frequency questionnaire, and a general health survey. At follow‐up, 14% (n=38) of the parents had completed the surveys. Thus, there were not enough data to make substantive conclusions about changes in fruit and vegetable consumption in the home environment." No funding statement was provided. No conflict of interest statement was reported. |
Yeh 2018.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 7 months Unit of allocation: preschool (Head Start programmes) Unit of analysis: child |
|
| Participants |
Service type: centre‐based (Head Start) Operation: half day program Country (region): USA (Midwestern metropolitan area) Country income classification: high Low‐SES sample: yes Population description: this study took place at the United Children and Family Head Start programmes in a major Midwestern metropolitan area. African American preschool children comprised 95% of the population in the half‐day programme. 6 Head Start programmes, each with a morning and an afternoon session, participated in the study. Inclusion criteria: the participants were preschoolers with ages ranging between 3 and 5 years old. Exclusion criteria: not reported Number of services randomised: 6 (2 intervention 1, 2 intervention 2, 2 control) Number of children randomised: 160 (47 intervention 1, 54 intervention 2, 59 control) Characteristics Children Age: 3‐5 years Gender (% female): Intervention 1: 49% Intervention 2: 41% Control: 44% Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported Method of recruitment: not reported Missing data/dropout: not reported Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Healthy Kids Healthy Lives Number of conditions: 2 interventions, 1 control Intervention duration: 7 months Intervention setting: ECEC Intervention strategies: Intervention 1: Group A Health curriculum Children Education: children received 30‐min nutrition education sessions 2 x/week, for 7 months, provided by dietetic interns under the supervision of a registered dietitian. The content included the introduction of healthy "body building" foods and discussion of food groups. Hand puppets in the form of vegetables or fruits were used to introduce the content. Ethos and environment Children Exposure: fresh fruit and vegetable tastings included in the nutrition education session Service Menu modification: wholegrain products were substituted for products usually made with white flour. Support: researchers worked with the food provider from each centre and purchased the required amount of wholegrain products based on the service menu from local grocery stores. Meetings: before commencement of this study, the researchers met once with the food service provider centres and went over the food substitution plan and encouraged them to use all the wholegrain products provided and follow the recommended menu and recipes/cooking method. Monitoring: researchers emphasised the food substitutions and monitored use of the foods during weekly high‐fibre food delivery. Partnerships Healthcare Delivery: dietetic interns delivered nutrition education. Intervention 2: Group B Health curriculum Children Education: children received 30‐min nutrition education sessions 2 x/week, for 7 months, provided by dietetic interns under the supervision of a registered dietitian. The content included the introduction of healthy "body building" foods and discussion of food groups. Hand puppets in the form of vegetables or fruits were used to introduce the content. Ethos and environment Children Exposure: fresh fruit and vegetable tastings included in the nutrition education session. Service Menu modification: wholegrain products were substituted for products usually made with white flour. Support: researchers worked with the food provider from each centre and purchased the required amount of wholegrain products based on the service menu from local grocery stores. Meetings: before commencement of this study, the researchers met once with the food service provider centres and went over the food substitution plan and encouraged them to use all the wholegrain products provided and follow the recommended menu and recipes/cooking method. Monitoring: researchers emphasised the food substitutions and monitored use of the foods during weekly high‐fibre food delivery. All participants Cultural: the nutrition education was culturally‐appropriate (tailored to the African‐American, Midwest, Head Start‐eligible study population). Partnerships Families Lecture: caregivers received a 1‐h nutrition lecture every month. Classes were taught by dietetic interns and held in the 2 centres. The classes included 20‐min presentation followed by group discussion and interactive activities related to the topic. Healthcare Delivery: dietetic interns delivered family lectures and nutrition education. Intensity of intervention: Intervention 1: 2 x 30‐min child nutrition education/week, over the course of 2 semesters (7 months) Intervention 2: 2 x 30‐min child nutrition education/week, over the course of 2 semesters (7 months); 1‐h caregiver group nutrition classes every month. Intervention delivered by: Intervention 1: research team, ECEC staff, healthcare staff Intervention 2: research team, ECEC staff, healthcare staff Modality: Intervention 1: face‐to‐face, written Intervention 2: face‐to‐face, written Theoretical basis: not reported Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: not reported Outcomes relating to child physical measures: BMI percentile Number of participants analysed: Intervention 1 baseline: 47 Intervention 1 follow‐up: 47 Intervention 2 baseline: 54 Intervention 2 follow‐up: 54 Control baseline: 59 Control follow‐up: 59 Data collection measure: objectively measured (CDC) Data collector: not reported Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: a grant from the Office of the Vice President for Research, Wayne State University. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The 6 participating schools were randomly assigned to one of 3 groups with 2 schools per group. The sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | No blinding of participants and personnel to study allocation, however the outcome is not likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height and weight were measured by train graduate students and were not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Physical outcomes | Unclear risk | Study authors stated that "A convenience sample of 203 preschooleres was recruited at baseline. Post‐intervention data collection occurred 7 months later and included 164 preschoolers who completed the Head Start program during the academic year (80% retention)." Reasons for missing data and differences between treatment groups are not reported. Risk of attrition bias is unclear. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting. |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Unclear risk | Only BMI was considered so there is insufficient information to assess whether bias exists. At baseline, there was no difference in BMI among the 3 groups. The control group had a higher mean BMI percentile than the intervention groups but the difference was nonsignificant (P = 0.067). No significant differences were found when comparing mean BMI and BMI percentiles from baseline to postintervention among the 3 groups. |
| Loss of clusters | Unclear risk | Not reported |
| Incorrect analysis | High risk | There was no accounting for clustering of children within Head Start centres. |
| Contamination | Unclear risk | No evidence to make assessment. |
| Other bias | Unclear risk | The study may have been underpowered. Study authors stated that "It is speculated that if the sample size is increased, the significant reduction in BMI percentile in group A may become apparent." There is insufficient information to assess whether an important risk of bias exists. |
Yoong 2020a.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 12 months Unit of allocation: centre Unit of analysis: child |
|
| Participants |
Service type: centre‐based Operation: not reported Country (region): Australia (New South Wales (NSW) Country income classification: high Low‐SES sample: unclear Population description: NSW is a demographically and socioeconomically diverse state and contains approximately 387,245 children aged 3–6 years. Inclusion criteria: eligible centres were required to 1) be users of the partner provider’s ECEC online reporting software (HubWorks; HubCare ANZ) (∼15% of all ECEC services in NSW); 2) prepare and provide ≥ 1 main and ≥ 2 mid‐meals to children onsite; 3) make menu‐planning decisions onsite; and 4) have a menu planner (typically a cook) with sufficient English to engage with the intervention. Eligible children were required to 1) be aged 2–6 years; 2) be present at the centre on days of data collection; 3) have no dietary requirements preventing consumption of foods while in care; and 4) have parental consent. Exclusion criteria: centres were excluded if they outsourced menu‐planning decisions, catered exclusively for special needs children, or were run by the NSW Department of Education because such services had different operational and catering arrangements. Number of services randomised: 35 (groups not reported) Number of children randomised: 522 (288 intervention, 234 control) Characteristics Children Age: 4.6 years (SD 8.2 months) Gender (% female): 49.6% Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported Method of recruitment: all ECEC centres were posted an invitation letter and information statement about the study 2 weeks before receiving a call from a research assistant to assess eligibility and obtain consent. These centres were asked to distribute information and consent forms to parents of children in the room with the highest number of children aged 2–6 years before the scheduled site visit. Consistent with previous approaches by the research team and to maximise consent, research assistants also approached parents at drop off on the day of the visit. Missing data/dropout: 14% (n = 31) of children at baseline were retained at follow‐up. Reasons for dropout: changeover of rooms and transition to school Characteristics of dropouts: not reported |
|
| Interventions |
Programme name not reported Number of conditions: 1 intervention, 1 control Intervention duration: 12 months Intervention setting: ECEC Intervention strategies: Ethos and environment ECEC staff Training: a health promotion officer with experience using the program conducted a 3‐h training session with the supervisor and menu planner within each service. Training consisted of updating centres with sector‐specific nutrition guidelines, the main features of the online menu‐planning program and how to use them, and supporting the service to make changes to their menu. Action plan: to generate service‐level support for use of the program, the health promotion officer also undertook action planning to ensure that allocated time and resources were provided to the menu planner(s) to access the program. Support: ongoing support was provided via 2–4 phone calls to ECEC service cooks. The purpose of these calls was to provide technical support with using the program and overcome any reported barriers to using the program. The number of phone calls provided to each service was tailored depending on engagement with the program and menu compliance as assessed via analytics data collected via the program. Centres could also seek technical support via an online “help desk” feature available within the web‐based program. Service Audit and feedback: services were given access to a web‐based menu‐planning program, which undertook automated assessments on meals and snacks entered by menu planners and provided real‐time feedback on the number of servings of each of the core food groups and discretionary foods. The feedback also outlined whether the menu was compliant with that recommended by sector‐specific nutrition guidelines Resources: where menus were not compliant, the online program automatically provided ECEC centres with suggestions and recipes on how to modify the menus to meet guidelines. The online menu‐planning tool (“feedAustralia”) also included > 200 healthy recipes that met the guidelines for inclusion in ECEC menus as well as complete 1‐week sample menus that were compliant with guidelines. Centres were also provided with a portable tablet to facilitate access to the online program and recipes during food preparation processes. Reminders: ECEC centres were prompted fortnightly in the main software program to make changes to their menu to increase compliance if noncompliant, or if they had an incomplete menu entered in the online program. Partnerships Healthcare Delivery: health promotion officers conducted training and provided support. Intensity of intervention: 1 x 3‐h training; 2‐4 telephone calls Intervention delivered by: research team, healthcare staff Modality: face‐to‐face, telephone, online Theoretical basis: Technology Acceptance Model and Theoretical Domains Framework Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: Vegetables intake, fruit intake, cereals and breads intake, meat and alternatives intake, dairy and alternatives intake, discretionary foods intake, diet quality (total) Number of participants analysed: Intervention baseline: 105‐112 Intervention follow‐up: 150‐183 Control baseline: 101‐108 Control follow‐up: 147‐151 Data collection measure: direct observation and short food survey Data collector: researcher and educator Validity of measures used: not reported Outcomes relating to child physical measures: BMI z‐score Number of participants analysed: Intervention baseline: 288 Intervention follow‐up: 268 Control baseline: 234 Control follow‐up: 215 Data collection measure: objectively measured (WHO) Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: Health rated quality of life Number of participants analysed: Intervention baseline: 94 Intervention follow‐up: 68 Control baseline: 69 Control follow‐up: 27 Data collection measure: parent proxy version of KIDSCREEN‐10 Data collector: parent Validity of measures used: validated Outcome relating to cost: Intervention delivery costs, cost per service, average cost‐effectiveness ratio, relative value index Number of participants analysed: not reported Data collection measure: micro‐costing and service questionnaire Data collector: researcher and nominated supervisors and menu planners Validity of measures used: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: supported by National Health and Medical Research Council (NHMRC) project grant APP1102943 and Cancer Council NSW (CCNSW) program grant PG16‐05. Pilot funding was also provided from the Hunter Cancer Research Alliance and the Priority Research Centre for Health Behaviour, University of Newcastle. Hunter New England Population Health, Hunter Medical Research Institute, and the University of Newcastle provided infrastructure funding. Healthy Australia Ltd provided in‐kind support for programming of the web program (“feedAustralia”). Healthy Australia Ltd co‐developed the web program and were members of the advisory group which supported decisions related to the design and delivery of the web‐based program. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Centres were stratified by SES and randomly assigned after baseline data collection to the intervention or control group in a 1:1 ratio by an independent statistician using a random number function in Microsoft Excel 2010. However, for diet and quality‐of‐life outcomes, authors stated that "To minimize selection bias, research assistants blinded to center allocation sought consent for dietary observations from all parents. After obtaining consent, research assistants randomly selected 6–9 children per center for dietary observations because 1 individual could only observe ≤ 3 children each." However the random sequence generation is not detailed with regard to the 6‐9 children selected for dietary observation. As the random sequence generation for the primary outcome is not specified, the assessment is rated as unclear. |
| Allocation concealment (selection bias) | Low risk | Allocation was conducted by an independent statistician after baseline data collection. |
| Blinding of participants and personnel (performance bias) Diet outcomes | Unclear risk | ECEC staff and those delivering the intervention were aware of group allocation; however, parents were not explicitly informed of centre allocation. The outcome may have been influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | ECEC staff and those delivering the intervention were aware of group allocation, though parents were not explicitly informed of centre allocation. However, the outcome is not likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Quality of life outcomes | High risk | Parents were not explicitly informed of treatment allocation, but they were not blind to it, either. The outcome is likely to be influenced by lack of blinding. |
| Blinding of participants and personnel (performance bias) Cost | Unclear risk | ECEC staff and those delivering the intervention were aware of group allocation; however, parents were not explicitly informed of centre allocation. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Diet outcomes | Low risk | 2 methods were used to obtain child diet outcomes: (1) children's dietary intake was observed by trained research assistants who were blinded to group allocation and (2) children's dietary intake was reported via survey by parents who were not explicitly informed of centre allocation, but they were not blind to it either. The outcomes included in the meta‐analyses were by blinded research assistants, therefore, we have assessed as low risk of bias |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Children's height and weight were objectively measured by trained research assistants who were blinded to group allocation. |
| Blinding of outcome assessment (detection bias) Quality of life outcomes | High risk | Parents reported children's health‐related quality of life via interview using the KIDSCREEN‐10. Parents were not explicitly informed of centre allocation, but they were not blind to it either. The outcome measurement is likely to be influenced by lack of blinding. Study authors state that "First, the use of questionnaires completed by educators and parents to assess child diet quality and HRQoL [health‐related quality of life] is likely subject to recall and social desirability bias." |
| Blinding of outcome assessment (detection bias) Cost | Unclear risk | ECEC staff and those delivering the intervention were aware of group allocation. It is unclear whether the outcome is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | High risk | Study authors stated that "We attempted to undertake a cohort analysis; however, as expected there was high attrition of children, with only 14% (n=31) of children at baseline retained at follow‐up owing to changeover of rooms and transition to school." Due to the magnitude of missing data, the risk of bias was assessed as high. |
| Incomplete outcome data (attrition bias) Physical outcomes | High risk | Study authors stated that "We attempted to undertake a cohort analysis; however, as expected there was high attrition of children, with only 14% (n=31) of children at baseline retained at follow‐up owing to changeover of rooms and transition to school." Due to the magnitude of missing data, the risk of bias was assessed as high. |
| Incomplete outcome data (attrition bias) Quality of life outcomes | High risk | Study authors stated that "We attempted to undertake a cohort analysis; however, as expected there was high attrition of children, with only 14% (n=31) of children at baseline retained at follow‐up owing to changeover of rooms and transition to school." Due to the magnitude of missing data, the risk of bias was assessed as high. |
| Incomplete outcome data (attrition bias) Cost | Unclear risk | The number of services and participants that reported on this outcome is unclear. |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the paper were prespecified in the protocol paper. |
| Recruitment bias | High risk | Children were recruited over time. Study authors state that "We attempted to undertake a cohort analysis; however, as expected there was high attrition of children, with = only 14% (n 31) of children at baseline retained at follow‐up owing to changeover of rooms and transition to school." |
| Baseline imbalance | Unclear risk | Baseline differences between groups were not reported. |
| Loss of clusters | High risk | One cluster lost |
| Incorrect analysis | Low risk | Study authors stated that "For continuous outcomes, group differences were assessed through a group‐by‐time interaction in mixed‐effects linear regression models, which included a random effect to account for potential clustering. For dichotomous outcomes, a logistic regression adjusting for baseline scores and clustering was undertaken." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Low risk | No clear other source of bias |
Zask 2012.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 10 months Unit of allocation: preschool Unit of analysis: child |
|
| Participants |
Service type: centre‐based (preschools) Operation: not reported Country (region): Australia (North Coast of New South Wales (NSW)) Country income classification: high Low‐SES sample: unclear Population description: not reported Inclusion criteria: preschools that submitted an expression of interest to participate Exclusion criteria: not reported Number of services randomised: 31 (18 intervention, 13 control) Number of children randomised: unclear (560 children participated) Characteristics Children Age: Girls: 50.5 months (SD 6.7) Boys: 58.8 months (SD 6.8) Gender (% female): 48.30% Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: not reported Method of recruitment: preschools that submitted an expression of interest to participate Missing data/dropout: records from 560 children (yielding a total of 1005 records with 537 and 468 records at pre‐ and postintervention) in 18 intervention and 13 control preschools were used in the study. Data were collected from 80.7% and 67.2% of all children enrolled pre‐ and postintervention respectively. Only 6.9% and 5.7% of enrolled children’s parents did not consent to participate at pre‐ and postintervention. Reasons for dropout: most of the missing data were due to children being absent on the day of testing or having left the preschool between consent and testing. Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: Tooty Fruity Vegie Number of conditions 1 intervention, 1 control Intervention duration: 10 months Intervention setting: ECEC Intervention strategies: Health curriculum Children Education: children received simple consistent messages about ‘sometimes’ and ‘everyday’ foods ‐ puppets, staff in fruit and vegetable costumes, stories, and role‐play, were used to reinforce this message. Structured 2 x/week fundamental movement skill development through prescribed games suitable for a wide age range. Ethos and environment Children Exposure: taste testing fruit and vegetables, growing and cooking used to reinforce nutrition messages. Role‐modelling: staff acting as role models and giving positive reinforcement to children about eating healthy food and drinking water. Service Audit and feedback: Project Management Committees reviewed playground environment and alterations to encourage more active movement and better access to sports equipment and water during free play times. Resources: small grants for sports equipment ECEC staff Training: preschool staff received a 1‐d training in running the ‘FunMoves’ programme. Resources: staff were given a kit comprising program notes and 30 laminated cards for each of the games. The cards were designed so that untrained parents or casual staff could quickly read the card and run the activity for 'FunMoves'. Environment: colourful posters on “better foods” and “foods better left out” on display all year. Drinking water made more accessible to children (so children could drink water without having to ask an adult for assistance). Policy: Project Management Committees worked with the team to review and adjust food and nutrition policies to explicitly identify appropriate and inappropriate foods in lunch boxes. Partnerships Families Workshop: health professional (dietitians, health promotion officer or child and family health nurse) delivered interactive workshops for parents on limiting sedentary time, promoting physical activity, fundamental movement skills and positive parenting in relation to healthy eating and feeding ‘fussy’ eaters, delivered by healthcare professionals. Parents were given support and practical, achievable advice to modify risk behaviours. Resources: a monthly 4‐page newsletter containing tips of healthy eating and active playing ideas was provided to each parent. Family Feud/ Food DVD was provided to parents, which models practical ways to improve children's eating habits Communication: communication of new policy to parents along with lunchbox displays Healthcare Engagement: health professionals (dietitians, health promotion officers and child and family health nurses) included in Project Management Committee and delivered the parent workshops. Intensity of intervention: twice‐weekly fundamental movement skills education for children; monthly 4‐page newsletter for parents; 1‐d staff training; parent workshops Intervention delivered by: ECEC staff, healthcare staff Modality: face‐to‐face, written Theoretical basis: The Health Belief Model and the Competence Motivational Theory. Capacity building and community participation theories were applied to build community action and ensure sustainability of the project Description of control: wait‐list control |
|
| Outcomes |
Outcomes relating to child dietary intake: not reported Outcomes relating to child physical measures: BMI z‐score, waist circumference Number of participants analysed: Intervention baseline: 149‐335 Intervention follow‐up: 114‐286 Control baseline: 108‐163 Control follow‐up: 99‐152 Data collection measure: objectively measured Data collector: researcher Validity of measures used: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: The Australian Better Health Initiative, a joint Australian, State and Territory government initiative, and supported by NSW Heath and the North Coast Area Health Service | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Preschools were randomly allocated to intervention or control groups in a ratio of approximately 1.4:1. The sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | Study authors stated that "Preschools that acted as control schools in one year, were on a waiting list for an intervention and were offered the full program in subsequent years (the program continued beyond 2007). After random allocation to either intervention or control arms of the study, we compared preschool localities’ SES to ensure the groups were matched. No change in allocation was required. Six intervention and one control preschool participated in the pilot stage in 2006 to test the intervention’s feasibility. The 2006 control preschool became an intervention preschool in 2007 with additional 11 intervention and 12 control preschools." |
| Blinding of participants and personnel (performance bias) Physical outcomes | Low risk | No clear blinding of participants and personnel to study allocation, however the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Physical outcomes | Low risk | Blinding not reported, however children's height, weight, and waist circumference were measured and were not likely to be influenced by lack of blinding |
| Incomplete outcome data (attrition bias) Physical outcomes | Unclear risk | Study authors stated that “Data were collected from 80.7% and 67.2% of all children enrolled pre‐ and postintervention respectively. Most of the missing data were due to children being absent on the day of testing or having left the preschool between consent and testing.” Missing data is not reported by treatment group. Risk of attrition bias is unclear. |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the paper were prespecified in the protocol paper. |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Unclear risk | Baseline data were reported, however not compared statistically. Study authors state that "The student and preschool variances have been accounted for in all models." |
| Loss of clusters | Unclear risk | Not reported |
| Incorrect analysis | Low risk | Study authors stated that "Data were further analysed by fitting multi‐level regression models in MLwiN to account for the clustered nature of the data (pre/post within students within preschools)." |
| Contamination | Unclear risk | No evidence to make assessment |
| Other bias | Unclear risk | Study authors stated that "There were reliability issues with waist circumference measurement so only data in which the same tester measured waist circumference pre and post intervention were included." There is insufficient information to assess whether an important risk of bias exists. No conflict of interest statement was reported. |
Zeinstra 2018.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT Length of follow‐up from baseline: 5 months Unit of allocation: centre Unit of analysis: child |
|
| Participants |
Service type: centre‐based Operation: not reported Country (region): The Netherlands (Utrecht) Country income classification: high Low‐SES sample: unclear Population description: not reported Inclusion criteria: all 4 centres belonged to the same organisation. Healthy children without any allergies to the study products could participate. Exclusion criteria: not reported Number of services randomised: 4 (2 interventions, 2 control) Number of children randomised: 250 (125 intervention, 125 control) Characteristics Children Age: Intervention: 25.6 months (SD 9.6) Control: 25.0 (SD 10.2) Gender (% female): Intervention: 44% Control: 42% Ethnicity: not reported Parents Age (years): not reported Gender (% female): not reported Ethnicity: not reported Parent/family SES: Parent education level: Intervention: low: 0%; middle: 5%; high: 95% Control: low: 0%; middle: 10%; high: 90% Method of recruitment: information packs were distributed to 526 parents to inform them about the study aims and procedures. Missing data/dropout: not reported Reasons for dropout: not reported Characteristics of dropouts: not reported |
|
| Interventions |
Programme name: not reported Number of conditions: 1 intervention, 1 control Intervention duration: 5 months (21 weeks) Intervention setting: ECEC Intervention strategies: Ethos and environment Children Exposure: each vegetable was served in 2 different preparations. Children were offered 1 vegetable product each day, in accordance with a predefined schedule. A vegetable song was played to make the vegetable eating occasion recognisable and fun for the children. The blanched and raw vegetables were offered on a group plate (portion available ~50 g/child). The spreads (~30 g) were offered on 1 or 2 crackers, and the soup was offered in an individual cup (~80 g). The children could eat as much or as little as they wanted from the vegetable products; child‐care employees invited the children to taste but never forced them to eat. ECEC staff Workshop: all ECEC employees were involved in a 1‐h workshop to explain the study procedures and to discuss and resolve any perceived barriers. Intensity of intervention: 1‐h ECEC staff workshop; children were offered 1 vegetable product each day. Intervention delivered by: research team, ECEC staff Modality: face‐to‐face Theoretical basis: not reported Description of control: usual care |
|
| Outcomes |
Outcomes relating to child dietary intake: Pumpkin intake, white radish intake, courgette intake Number of participants analysed: not reported Data collection measure: research team weighed the vegetable cups before and after consumption; vegetable intake was calculated by subtracting the leftovers from the pre‐weight Data collector: researcher Validity of measures used: not reported Outcomes relating to child physical measures: not reported Outcome relating to child language and cognitive performance: not reported Outcome relating to child social/emotional measures: not reported Outcome relating to child quality of life: not reported Outcome relating to cost: not reported Outcome relating to adverse consequences: not reported |
|
| Notes | Funding source: The Fresh Produce Centre and the Ministry of Economic Affairs (grant number TU 1310‐086). Neither organization had any role in the design, analyses, or writing of this article. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 2 ECEC centres were randomly assigned to the intervention condition. The sequence generation procedure was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information on the method of allocation concealment reported |
| Blinding of participants and personnel (performance bias) Diet outcomes | Unclear risk | All 4 ECEC centres were part of the same organisation, though the parents and day care employees were not informed about the exact study design and conditions until after the study ended. Study authors stated that "Employees were asked to refrain from making negative faces or negative comments regarding the food's smell, taste, texture, or appearance." However, they were not asked to refrain from encouragement, which could have increased children's intake. Further, "the childcare employees were instructed to maintain a neutral attitude, which may have been somewhat artificial." |
| Blinding of outcome assessment (detection bias) Diet outcomes | Low risk | Blinding of outcome assessors not reported, however children's consumption was measured by weighing the vegetable cups before and after intake out of the children's view. The outcome measurement is not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Diet outcomes | Unclear risk | Study authors stated that "The final dataset contained 250 children." However, the number of children at baseline and follow‐up is not reported. Risk of attrition bias is unclear. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it was unclear whether there was selective outcome reporting |
| Recruitment bias | Unclear risk | It is unclear whether individuals were recruited to the study before or after randomisation of clusters. |
| Baseline imbalance | Low risk | There were no significant differences between the intervention and the control groups. |
| Loss of clusters | Unclear risk | Not reported |
| Incorrect analysis | Unclear risk | There was no accounting for clustering of children within centres, however all 4 centres were part of the same organisation. There is not enough information to assess whether an important risk of bias exists. |
| Contamination | Unclear risk | All 4 centres were from the same community and belonged to the same organisation. However, this is unlikely to have affected the intervention given the nature of the intervention (repeated exposure to unfamiliar vegetables in the child‐care centre). |
| Other bias | Unclear risk | Discrepancies are noted in the manuscript regarding what teachers were instructed to do (or not do) during pretest and post‐test. There is insufficient information to assess whether an important risk of bias exists. The intervention received financial support from a commercial organisation. Study authors state that this company had no operational role. |
CDC: Centres for Disease Control; ECEC: early childhood education and care; FFQ: Food Frequency Questionnaire; GED: General Educational Development (tests); IOTF: International Obesity Task Force; ITT: intention‐to‐treat; PedsQL: Pediatric Quality of Life Inventory; RCT: randomised controlled trial; SD: standard deviation; SE: standard error; SES: socioeconomic status; USDA: United States Department of Agriculture; WHO: World Health Organization
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aherna 2019 | Study design: not a RCT |
| Ariati 2019 | Intervention: targets malnutrition |
| Batra 2014 | Intervention: targets malnutrition |
| Bayer 2009 | Participants: aged > 6 years at baseline |
| Benjamin 2007 | Outcome: no child dietary or anthropometric outcomes |
| Benjamin 2008 | Outcome: no child dietary or anthropometric outcomes |
| Benjamin 2014 | Outcome: no child dietary or anthropometric outcomes |
| Braga‐Pontes 2021 | Study design: does not have a minimum of 2 intervention sites and 2 control sites |
| Brophy‐Herb 2017 | Intervention: not primarily conducted in ECEC setting |
| Bryant 2021 | Intervention: not primarily conducted in ECEC setting |
| Buscemi 2019 | Study design: not a RCT |
| Byrne 2002 | Outcome: no child dietary or anthropometric outcomes |
| Carstairs 2020 | Outcome: assessed prior to 3 months |
| Caton 2013 | Study design: not a RCT |
| Chuang 2020 | Outcome: no child dietary or anthropometric outcomes |
| Correia 2014 | Study design: does not have a minimum of 2 intervention sites and 2 control sites |
| Coulthard 2017 | Study design: not a RCT |
| Coulthard 2018 | Outcome: assessed prior to 3 months |
| Dazeley 2015 | Outcome: assessed prior to 3 months |
| De Droog 2014 | Outcome: assessed prior to 3 months |
| De Droog 2017 | Outcome: assessed prior to 3 months |
| De Wild 2013 | Study design: not a RCT |
| De Wild 2015 | Study design: not a RCT |
| De Wild 2017 | Study design: not a RCT |
| De Zwarte 2019 | Outcome: no child dietary or anthropometric outcomes |
| Diktas 2021 | Outcome: assessed prior to 3 months |
| Earnesty 2019 | Outcome: no child dietary or anthropometric outcomes |
| Eichholzer‐Helbling 1986 | Study design: not a RCT |
| Esquivel 2016 | Study design: not a RCT |
| Ferris 2012 | Study design: not a RCT |
| Finch 2019a | Outcome: no child dietary or anthropometric outcomes |
| Finch 2019b | Outcome: no child dietary or anthropometric outcomes |
| Grady 2020 | Outcome: no child dietary or anthropometric outcomes |
| Hardy 2010 | Outcome: no child dietary or anthropometric outcomes |
| Harnack 2012 | Outcome: assessed prior to 3 months |
| Hausner 2012 | Outcome: assessed prior to 3 months |
| Hughes 2020b | Intervention: not primarily conducted in ECEC setting |
| Jouret 2009 | Study design: not a RCT |
| Kashef 2021 | Study design: not a RCT |
| Kim 2019 | Outcome: assessed prior to 3 months |
| Kling 2016 | Outcome: assessed prior to 3 months |
| Kostecka 2022 | Study design: not a RCT |
| Lanigan 2019 | Outcome: assessed prior to 3 months |
| Lawatsch 1990 | Outcome: no child dietary or anthropometric outcomes |
| Leahy 2008a | Outcome: assessed prior to 3 months |
| Leahy 2008b | Outcome: assessed prior to 3 months |
| Leahy 2008c | Outcome: assessed prior to 3 months |
| Leung 2019 | Intervention: not primarily conducted in ECEC setting |
| Lin 2016 | Intervention: not primarily conducted in ECEC setting |
| Malden 2019 | Outcome: no child dietary or anthropometric outcomes |
| Mannino 2019 | Outcome: no child dietary or anthropometric outcomes |
| McSweeney 2017 | Intervention: not primarily conducted in ECEC setting |
| NCT03672227 | Outcome: assessed prior to 3 months |
| NCT03957148 | Study design: not a RCT |
| NCT04552678 | Study design: not a RCT |
| NCT05050539 | Study design: not a RCT |
| Neelon 2016 | Outcome: no child dietary or anthropometric outcomes |
| Nekitsing 2019b | Outcome: assessed prior to 3 months |
| Norman 2019 | Participants: aged > 6 years at baseline |
| O'Connell 2012 | Study design: does not have a minimum of 2 intervention sites and 2 control sites |
| Rhee 2019 | Outcome: assessed prior to 3 months |
| Ritchie 2019 | Outcome: no child dietary or anthropometric outcomes |
| Rollins 2021 | Outcome: assessed prior to 3 months |
| Schuler 2019 | Outcome: no child dietary or anthropometric outcomes |
| Sirasa 2021 | Outcome: assessed prior to 3 months |
| Slining 2021 | Study design: not a RCT |
| Smith 2019 | Outcome: assessed prior to 3 months |
| Sojkowski 2012 | Outcome: assessed prior to 3 months |
| Sweitzer 2010 | Study design: not a RCT |
| Swindle 2021 | Study design: not a RCT |
| Vaughn 2019b | Study design: not a RCT |
| Vepsäläinen 2022 | Outcome: no child dietary or anthropometric outcomes |
| Verbestel 2014 | Intervention: not primarily conducted in ECEC setting |
| Vitale 2020 | Outcome: assessed prior to 3 months |
| Ward 2008 | Outcome: no child dietary or anthropometric outcomes |
| Ward 2017 | Outcome: no child dietary or anthropometric outcomes |
| Ward 2020b | Outcome: no child dietary or anthropometric outcomes |
| Williams 1998 | Study design: not a RCT |
| Williams 2002 | Study design: not a RCT |
| Yeom 2019 | Study design: not a RCT |
| Yoong 2016 | Outcome: no child dietary or anthropometric outcomes |
ECEC: early childhood education and care; RCT: randomised controlled trial
Characteristics of studies awaiting classification [ordered by study ID]
ChiCTR2200060958.
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): China (Shenzhen City) Number of services participating: unclear (1400 children) |
| Interventions | Insufficient information available in trial registry to determine eligibility |
| Outcomes | Insufficient information available in trial registry to determine eligibility |
| Notes | ChiCTR1800017292 |
RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
Armstrong 2019.
| Study name | CHAMP: a cluster randomized‐control trial to prevent obesity in child care centers |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): USA (Maryland) Number of services participating: 54 |
| Interventions |
Number of conditions: 2 interventions, 1 control Intervention strategies: Intervention 1: CHAMP Health curriculum Children Curriculum: physical activity programme (Get Movin’ with Mighty Moves®) to increase gross motor skills and healthful eating programme (Fun with New Foods®), including nutrition activities and opportunities to try new foods Ethos and environment ECEC staff Workshops: ECEC staff will receive 2 training sessions during the year which last approximately 1–2 h each. During the training sessions, staff are provided with general psychoeducation regarding childhood obesity, food neophobia and gross motor development. Materials: detailed implementation manuals on lesson plans and classroom activities will be provided to ECEC staff. ECEC staff and directors will receive a printed manual and have access to a staff website where they can access weekly lesson plans, handouts, additional resources and programme content including music to accompany lessons. Each week, lesson plans are emailed or texted to ECEC staff. Intervention 2: CHAMP + Health curriculum Children Curriculum: physical activity programme (Get Movin’ with Mighty Moves®) to increase gross motor skills and healthful eating programme (Fun with New Foods®), including nutrition activities and opportunities to try new foods. Ethos and environment ECEC staff Workshops: ECEC staff will receive 2 training sessions during the year which last approximately 1–2 h each. During the training sessions, ECEc staff are provided with general psychoeducation regarding childhood obesity, food neophobia and gross motor development. Materials: detailed implementation manuals on lesson plans and classroom activities will be provided to ECEC staff. ECEC staff and directors will receive a printed manual and have access to a staff website where they can access weekly lesson plans, handouts, additional resources and programme content including music to accompany lessons. Each week, lesson plans are emailed or texted to ECEC staff. ECEC staff will also receive additional information about the caregiver website. Partnerships Families Education: caregivers were given access to a caregiver education website, hosted by the university. Each week, caregivers will be provided content on physical activity, nutrition, and wellness topics relevant to caregivers of preschoolers and co‐ordinated with the activities conducted in the classrooms. Quizzes and monthly challenges will be available to increase caregiver interaction with the online content. Caregivers will be notified weekly (by email or text message) when new content is available on the website. |
| Outcomes |
Outcomes relating to child dietary intake: Fruit intake, vegetable intake, beverage consumption, red meats intake, processed meats intake, take‐out food intake, snack food intake, dessert intake Outcomes relating to child anthropometric measures: Height, weight, waist circumference, BMI |
| Starting date | June 2016 |
| Contact information | Dr Maureen M Black, mblack@som.umaryland.edu |
| Notes | ClinicalTrials.gov: NCT03111264 |
Barnes 2020.
| Study name | A pilot randomised controlled trial of a web‐based implementation intervention to increase child intake of fruit and vegetables within childcare centres |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): Australia (Hunter New England) Number of services participating: 22 |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Ethos and environment ECEC staff Materials: services will have access to a web‐based program (Childcare Electronic Assessment Tool and Support (EATS)), which aims to promote: supporting families to provide healthier foods consistent with dietary guidelines, provision of intentional learning experiences about healthy eating to children, use of feeding practices that support children’s healthy eating, staff participation in professional development in healthy eating and having a comprehensive written nutrition policy that outlines key healthy eating practices. Feedback: Childcare EATS includes a self‐assessment of the implementation of targeted healthy eating practices. Following the completion of the self‐assessment, the web‐based program will immediately provide centres with feedback on practice performance. ECEC centres will be encouraged to complete the self‐assessment at least twice during the intervention period to self‐monitor improvements in practice. ECECcentres will be encouraged to use Childcare EATS to set goals and create an action plan to facilitate improvements in practice. Support: ECEC centres allocated to the intervention will receive support from health promotion officers within the local health district with experience working with ECEC centres. |
| Outcomes |
Outcomes relating to child dietary intake: Fruit intake, vegetable intake, sodium intake, saturated fat intake, added sugar intake Outcomes relating to child anthropometric measures: not reported |
| Starting date | September 2019 |
| Contact information | Dr Courtney Barnes, courtney.barnes@health.nsw.gov.au |
| Notes | Australian New Zealand Clinical Trial Registry: ACTRN12619001158156 |
Beckerman 2019.
| Study name | Communities for healthy living (CHL) ‐ A family‐centered childhood obesity prevention program integrated into Head Start services: study protocol for a pragmatic cluster randomized trial |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): USA (Massachusetts) Number of services participating: 16 |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Ethos and environment ECEC staff Training: staff training Resources: nutrition support resources Partnerships Parents Education: parenting programme Resources: written and media nutrition resources and child health screening reports |
| Outcomes |
Outcomes relating to child dietary intake: Fruit, vegetables, 100% juice, sugary beverages, water, snacks, fast food Outcomes relating to child anthropometric measures: BMI |
| Starting date | Fall 2017 |
| Contact information | Professor Kirsten K. Davison, kdavison@hsph.harvard.edu; chlheadstart@gmail.com |
| Notes | ClinicalTrials.gov: NCT03334669 |
Cosco 2021.
| Study name | Research design, protocol, and participant characteristics of COLEAFS: a cluster randomized controlled trial of a childcare garden intervention |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): USA (North Carolina) Number of services participating: 15 |
| Interventions |
Number of conditions: 1 intervention, 2 controls Intervention strategies: Ethos and environment Staff Workshop: teachers received a one‐on‐one orientation to the activity guide to ensure that they were prepared to lead 12 activities. Support: each week, a research assistant will visit the classroom to interview teachers, discuss challenges and successes of the prior week and provide technical assistance Service Resources: garden installations, resources, and gardening activities. A coffer storage unit and a garden kit (hand tools, hose, gardening gloves, watering wand, and child‐sized cans) will be provided. |
| Outcomes |
Outcomes relating to child dietary intake: Fruit and vegetable consumption Outcomes relating to child anthropometric measures: not reported |
| Starting date | June 2017 |
| Contact information | Nilda Graciela Cosco, nilda_cosco@ncsu.edu and Nancy M. Wells, nmw2@cornell.edu |
| Notes | ClinicalTrials.gov: NCT04864574 |
Helland 2016.
| Study name | Study protocol for a multi‐component kindergarten‐based intervention to promote healthy diets in toddlers: a cluster randomized trial |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): Norway (Vest‐Agder and Aust‐Agder) Number of services participating: 18 (including 2 dropouts) |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Health curriculum Children Curriculum: children will be delivered Sapere‐sensory education in the kindergartens’ pedagogical group sessions. Ethos and environment Children Menu modification: children will be offered a cooked, healthy lunch prepared at the kindergarten on the intervention days over the 9‐week period. ECEC staff Workshop: kindergarten staff will attend a class at the university to learn about the Sapere method and intervention elements. The pedagogical leaders will also attend a class to learn about food neophobia, development of healthy eating habits early in life, and how kindergartens can play a role in healthy eating in children. Materials: all staff will be given a handbook entitled “Overall plan for the intervention” to guide them in implementing the programme. Kindergartens will also be assigned equipment to make cooking easy and feasible. They will also receive 3 different handbooks developed for the project “Home cooked food guide,” and 3 food kit boxes (including spices, herbs, vinegar, mustard, and so forth); 1 for each time period. Financial compensation for food costs will be provided after the intervention period. The kindergartens will receive pre‐printed postcards and posters. Environment: kindergarten staff will integrate 10 meal principles about feeding practices. Families Materials: parents will be given short postcard messages corresponding to the 10 meal principles. |
| Outcomes |
Outcomes relating to child dietary intake: Fruits intake, berries intake, vegetable intake, potato intake, rice intake, pasta intake, bread intake, cereals intake, porridge intake, unprocessed meat and fish intake, processed foods intake, snacks intake, beverage intake Outcomes relating to child anthropometric measures: Height, weight, BMI |
| Starting date | 2014 |
| Contact information | Associate Professor Sissel Helland, sissel.h.hellandg@gmail.com |
| Notes | ISRCTN registry: ISRCTN74823448 |
ISRCTN33134697.
| Study name | NAP SACC (UK): nutrition and physical activity self‐assessment for childcare |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): UK (Somerset, Swindon, Sandwell and Ayrshire and Arran) Number of services participating: 56 |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Ethos and environment Staff Workshop: specialised staff will deliver workshops to all nursery staff on nutrition and physical activity. Service Self‐assessment: nursery managers will complete a self‐assessment. Goal setting and action planning: the NAP SACC UK Partner will work with the nursery manager to develop an action plan, listing 8 goals for improvement. Support: NAP SACC UK Partner will continue regular contact with nurseries to provide support and advice toward them meeting their goals Evaluation: the Review & Reflect self‐assessment is repeated by the nursery manager after 6 months and reviewed with the NAP SACC UK Partner to see where improvements have been made or not, and to explore ways to overcome barriers. Action plans will revised to set 8 new goals for the next 6 months. Partnerships Partners Delivery: specialised staff will deliver workshops to all nursery staff and partners will provide support. |
| Outcomes |
Outcomes relating to child dietary intake: Total energy per snack and lunch eating occasion, average size of lunch (per occasion) consumed by children, average size of snacks (per occasion) consumed by children, average percentage of total energy in lunch from non‐core food served consumed by children, average percentage of total energy in snacks from non‐core food served consumed by children Outcomes relating to child anthropometric measures: BMI z‐score, overweight and obesity |
| Starting date | March 2022 |
| Contact information | Dr Ruth Kipping, ruth.kipping@bristol.ac.uk |
| Notes | ISRCTN registry: ISRCTN33134697 |
Lee 2019.
| Study name | Design and methodology of a cluster‐randomized trial in early care and education centers to meet physical activity guidelines: Sustainability via Active Garden Education (SAGE) |
| Methods | Study design: cluster‐RCT (2 x 2 factorial design) |
| Participants |
Service type: centre‐based Country (region): USA (Phoenix) Number of services participating: 28 |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Health curriculum Children Curriculum: a garden‐based physical activity and nutrition educational programme will be delivered to children. Children learn actively how to plant, water, weed, harvest and do simple food preparation involving washing, cleaning, and sampling fruit and vegetables. SAGE demonstrates how engaging in daily physical activity by tending the garden can contribute to meeting physical activity guidelines. Additional activities in the curriculum include 3 science experiments, a mindful eating exercise in every session and 22 interactive discussions. Ethos and environment Service Materials: gardens (4′ X 6′(approx 1.2 m x 1.8 m)) will be installed in centres. Climate appropriate fruits, vegetables, and herbs will be planted in advance of the curriculum with the aid of teachers and ECEC staff so that plants will be available throughout the SAGE curriculum. ECEC personnel will take primary responsibility for watering the garden with additional help from the SAGE team. |
| Outcomes |
Outcomes relating to child dietary intake: Fruit intake, vegetable intake Outcomes relating to child anthropometric measures: not reported |
| Starting date | January 2017 |
| Contact information | Dr Rebecca Lee, releephd@yahoo.com |
| Notes | ClinicalTrials.gov: NCT03261492 |
Malden 2018.
| Study name | Adapting the ToyBox obesity prevention intervention for use in Scottish preschools: protocol for a feasibility cluster randomised controlled trial |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): Scotland (Glasgow) Number of services participating: 6 |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Health curriculum Children Curriculum: teacher‐led interactive activities Ethos and environment Children Exposure: teacher‐led physical activity sessions and movement breaks, as well as interactive stories ECEC staff Training: early years practitioners will receive a 2.5 h training session prior to intervention commencement. The session will cover guidelines for designing a movement‐friendly classroom environment, delivery of the physical activity and sedentary behaviour components, use of the practitioner logbook and a briefing on the content and timing of the parental component of the intervention. Support: the lead researcher and coproducing early years practitioner will visit the preschools to assist with any issues, and observe delivery of the programme to ensure it is being delivered as intended. Service Materials: preschools will be provided with a "ToyBox" containing equipment, puppets and classroom activity guides. Partnerships Families Materials: parents will be provided with an introductory pack at the start of the intervention detailing what ToyBox‐Scotland is and how it relates to them. They will be given instructions on how to use the wallchart and stickers to incentivise their child’s behaviour, and short instructions for each homework game will be provided to parents via the early years practitioners. |
| Outcomes |
Outcomes relating to child dietary intake: Home eating/snacking intake, water consumption Outcomes relating to child anthropometric measures: BMI |
| Starting date | December 2017 |
| Contact information | Dr Stephen Malden, stephen.malden@strath.ac.uk |
| Notes | ISRCTN registry: ISRCTN12831555 |
Mehdizadeh 2018.
| Study name | Customized intervention program aiming to improve healthy eating and physical activity among preschool children: protocol for a randomized controlled trial (Iran Healthy Start Study) |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): Iran (Mashhad) Number of services participating: 6 |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Health curriculum Children Curriculum: children are delivered physical activity and nutrition units Ethos and environment ECEC staff Workshop: a workshop at baseline and a booster session at the middle of the intervention period will be conducted. Details of "Literacy, Education, Activity, Play" activities, activity demonstrations, role of educators, collaboration with parents, and other related implementation hints are presented and discussed. Service Materials: comprises 2 illustrated handbooks. The physical activity book containing 20 activity units along with a complementary chapter containing information for educators. The nutrition book contains 20 activity units along with a complementary chapter containing information for educators. This handbook is accompanied with “Healthy‐kid Toolkit,” which contains utilities and materials for "Literacy, Education, Activity, Play" activity units. A handbook for managers and educators containing modified self‐assessment tool, as well as principles of the programme, action planning, policies and practices, details of implementation, log pages, and report pages for both educators and managers. It also contains a suggested healthy weekly menu for serving a snack or a hot meal for children at preschool. Access to a comprehensive website containing details of the programme. Support: an on‐site training workshop will be followed by a supplementary booster session during the implementation (3‐4 h), as well as ongoing support through mobile and internet‐based contacts (Telegram) and weekly visits. Educators and managers of are invited to become a member of the Telegram channel. Partnerships Families Materials: a scientific, user‐friendly, and simple book entitled, “Knowledgeable Parents, Healthier Children,” will be provided to parents, aiming at improving their knowledge and practice regarding healthy eating for the whole family, especially their preschool child. Access to a comprehensive website containing details of the programme. Support: routine monthly meetings between parents and team nutritionists. Community Broadcasting: a television show and radio talks related to childhood obesity, physical activity in children, healthy nutrition, parenting, and many other related topics were recorded to introduce the programme and report the future outcomes. |
| Outcomes |
Outcomes relating to child dietary intake: diet quality Outcomes relating to child anthropometric measures: Weight, height, mid‐arm circumference, waist circumference, BMI, BMI percentile, BMI z‐score |
| Starting date | Dr Hassan Vatanparast, vatan.h@usask.ca |
| Contact information | International Clinical Trials Registry Platform: IRCT2016041927475N1 |
| Notes |
NCT01890681.
| Study name | Baby nutrition and physical activity self‐assessment for child care (NAP SACC) intervention study |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): USA Number of services participating: unclear (960 children) |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Ethos and environment ECEC staff Workshop: training workshops ECEC providers. Service Support: centre self‐assessment and targeted technical assistance by Baby NAP SACC consultant for providers Partnerships Families Support: family self‐assessment and targeted technical assistance by Baby NAP SACC consultant parents. Parent outreach and support |
| Outcomes |
Outcomes relating to child dietary intake: Dietary intake Outcomes relating to child anthropometric measures: Weight‐for‐length z‐score, skinfold thickness |
| Starting date | August 2013 |
| Contact information | Professor Sara Benjamin Neelon, sara.neelon@jhu.edu |
| Notes | ClinicalTrials.gov: NCT01890681 |
NCT02580123.
| Study name | Smile‐Kids: study on complementary feeding transition |
| Methods | Study design: RCT |
| Participants |
Service type: centre‐based Country (region): Portugal Number of services participating: 25 (children aged 4‐12 months) |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Ethos and environment ECEC staff Training: educators' training with the researchers Partnerships Families Training: training with parents and infants developed by trained educators |
| Outcomes |
Outcomes relating to child dietary intake: Dietary intake Outcomes relating to child anthropometric measures: Weight, length, BMI |
| Starting date | May 2012 |
| Contact information | Dr Helena Rafaela Vieira do Rosario, rrosario@ese.uminho.pt |
| Notes | ClinicalTrials.gov: NCT02580123 |
NCT03575884.
| Study name | Fit 5 kids screen time reduction curriculum for Latino preschoolers (Fit5Kids) |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): USA (Seattle, Houston, and the Central Valley of Washington State) Number of services participating: unclear (280 children) |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Health curriculum Children Curriculum: Fit5Kids classroom curriculum Partnerships Families Resources: weekly parent newsletters Goal setting: in‐person (or by telephone) goal setting on child's screen time, a lending library of resources (e.g. books, games, arts/crafts), and text messages on screen time parenting practices offered over 7‐8 weeks in the Fall (Autumn) semester |
| Outcomes |
Outcomes relating to child dietary intake: Dietary intake Outcomes relating to child anthropometric measures: BMI z‐score |
| Starting date | September 2018 |
| Contact information | Dr Jason Mendoza, jason.mendoza@seattlechildrens.org |
| Notes | ClinicalTrials.gov: NCT03575884 |
NCT03601299.
| Study name | Back to basics: addressing childhood obesity through traditional foods in Alaska |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): USA Number of services participating: unclear (804 children) |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Health curriculum Children Curriculum: a physical activity curriculum in Head Start programmes in all communities Menu: a traditional food in Head Start menu programme in intervention communities Partnerships Families Programme: a home‐based nutrition programme in intervention communities Community Resources: a mechanism to document traditional foods important to each community |
| Outcomes |
Outcomes relating to child dietary intake: Traditional food intake Outcomes relating to child anthropometric measures: BMI |
| Starting date | 2018 |
| Contact information | Dr Timothy K Thomas, tkthomas@anthc.org |
| Notes | ClinicalTrials.gov: NCT03601299 |
NCT03668678.
| Study name | iGrow Readers nutrition and physical activity curriculum efficacy |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): USA Number of services participating: unclear (568 children) |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Health curriculum Children Curriculum: as part of the iGrow Readers curriculum, the primary teacher first reads a book as a group with a specific health behaviour theme. Then, children participate in nutrition and physical activities that relate and reinforce the lessons learned in the book. Ethos and environment Families Resources: informational newsletters highlighting healthy behaviours from the stories' themes are provided to parents. |
| Outcomes |
Outcomes relating to child dietary intake: Diet Outcomes relating to child anthropometric measures: Height, weight, body composition, BMI |
| Starting date | 14 August 2014 |
| Contact information | Associate Professer Jessica R Meendering, jessica.meendering@sdstate.edu |
| Notes | ClinicalTrials.gov: NCT03668678 |
NCT04082247.
| Study name | Healthy children 2021 study in childcare centers (HC2021) |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): Portugal Number of services participating: 16 |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Ethos and environment ECEC staff Training: educators will receive training around healthy eating, physical activity and sleep for children |
| Outcomes |
Outcomes relating to child dietary intake: Dietary intake Outcomes relating to child anthropometric measures: Length and waist, weight |
| Starting date | September 2019 |
| Contact information | Dr Rafaela Vieira do Rosario, rrosario@ese.uminho.pt |
| Notes | ClinicalTrials.gov: NCT04082247 |
NCT04140032.
| Study name | Addressing obesity in early care and education settings |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): USA (Los Angeles) Number of services participating: 60 |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Health curriculum Children Curriculum: integration of nutrition and physical activity content into curricula Ethos and environment Service Policy: establishment of organisational policies to support healthy nutrition and physical activity ECEC staff Support: supports for teachers and staff to model healthy behaviour Partnerships Families Materials: engagement of parents as partners in implementing healthy policies in preschool and at home |
| Outcomes |
Outcomes relating to child dietary intake: Dietary intake Outcomes relating to child anthropometric measures: BMI z‐score |
| Starting date | October 2019 |
| Contact information | Dr Burton Cowgill, bcowgill@ucla.edu |
| Notes | ClinicalTrials.gov: NCT04140032 |
NCT04164277.
| Study name | FirstStep2Health intervention |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): USA Number of services participating: 6 |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Health curriculum Children Curriculum: preschoolers will receive weekly, age‐appropriate, participatory learning co‐delivered by teachers and university student educators Partnerships Families Meetings: 3 face‐to‐face or virtual caregiver meetings where research staff will lead the meetings at Head Start centres (weeks 1, 8, and 16) to connect caregivers to each other, offer health information, and discuss behavioural change strategies Resources: Facebook‐based programme including 4 new habit‐formation tasks/week. Preschoolers, using stickers, will create 2 letters each week regarding a food or activity presented in the centre‐based programme that they liked or want to try at home. Letters will be sent privately to each caregiver, and caregivers will be asked to respond to the letters. |
| Outcomes |
Outcomes relating to child dietary intake: Diet quality Outcomes relating to child anthropometric measures: Overweight, obesity, BMI z‐score |
| Starting date | September 2021 |
| Contact information | Associate Professor Jiying Ling, lingjiyi@msu.edu |
| Notes | ClinicalTrials.gov: NCT04164277 |
NCT04711525.
| Study name | i‐MaCHeL Study is a two‐group, cluster‐RCT, involves 460 preschool's child‐parent dyads, to prevent childhood obesity (i‐MaCHeL) |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): Malaysia Number of services participating: 12 |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Health curriculum Children Curriculum: children will be exposed to the interactive activities and quizzes using Web 2.0 tools, educational videos of a healthy lifestyle, sensory‐based food education activities, cooking demonstrations, fun, and active games, and exercises delivered through interactive classroom instruction Partnerships Families Web‐based program: parents will have access to the i‐MaCHeL Web‐based program |
| Outcomes |
Outcomes relating to child dietary intake: Dietary intake Outcomes relating to child anthropometric measures: BMI |
| Starting date | March 2022 |
| Contact information | Ahmad Faezi Ab.Rashid, faezi.ar@umk.edu.my |
| Notes | ClinicalTrials.gov: NCT04711525 |
NCT05112185.
| Study name | Childcare healthy beverage access, food and beverage intake, and obesity |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): USA Number of services participating: 14 |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Health curriculum Children Curriculum: education directed to children to increase the intake of healthy beverages, including lessons for children in ECEC centres Ethos and environment Service Environment: the Healthy Drinks, Healthy Futures intervention consists of increased access to healthy beverages in ECEC centres Partnerships Families Education: education directed to families to increase the intake of healthy beverages, including motivational beverage counselling for families |
| Outcomes |
Outcomes relating to child dietary intake: Caloric intake from beverages, beverage intake frequency Outcomes relating to child anthropometric measures: BMI z‐score |
| Starting date | August 2022 |
| Contact information | Associate Professer Anisha Pate, anipatel@stanford.edu |
| Notes | ClinicalTrials.gov: NCT05112185 |
Reeves 2018.
| Study name | ToyBox study Malaysia: improving healthy energy balance and obesity‐related behaviours among pre‐schoolers in Malaysia |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): Malaysia Number of services participating: not reported |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Health curriculum Children Curriculum: teachers will be encouraged to teach and promote the 4 key energy balance‐related behaviours drinking water; eating healthy snacks and meals; reducing sedentary behaviour; and increasing physical activity. Ethos and environment ECEC staff Training: teachers and their assistants will be trained to conduct the ToyBox Study programme, with a 2 d Training of teachers session prior to the start of the programme, and 2 half‐day sessions at regular intervals to obtain feedback on the programme up to that point and to provide a refresher on the upcoming components. Service Environment: the intervention may require making changes to the classroom environment; for example establishing a drinking water station or clearing an area to make space for physical activities. Partnerships Families Resources: parents and caregivers will be encouraged to get involved and advised via newsletters and tip cards to apply relevant environmental changes at home, act as role models and implement the healthy lifestyle behaviours together with their children. |
| Outcomes |
Outcomes relating to child dietary intake: Dietary intake Outcomes relating to child anthropometric measures: Anthropometric data |
| Starting date | Not reported |
| Contact information | Dr Sue Reeves, s.reeves@roehampton.ac.uk |
| Notes | Not reported |
Sisson 2019.
| Study name | Interventions to promote healthy environments in family child care homes in Oklahoma ‐ Happy Healthy Homes: study protocol for a randomized controlled trial |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: family child‐care homes Country (region): USA (Oklahoma City) Number of services participating: 52 |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Ethos and environment ECEC staff Training: the 2 individual educational training sessions, approximately 90 min in length, will be delivered to educators by trained interventionists. At the end of each module, participants discuss and set specific, measurable, attainable, realistic, and time‐sensitive (SMART) goals. A 3‐h group nutrition class will be conducted on campus after baseline visits. The class will be a cooking class that repeats key project goals and material in addition to hands‐on experience with best practices, food preparation tips, sensory experience, and tasting. Recipe preparation and tasting specific to feeding young children will be provided. Support: check‐in telephone calls will be completed between the first and second training sessions to discuss progress on SMART goals set during the first session and to troubleshoot any challenges. |
| Outcomes |
Outcomes relating to child dietary intake: Diet intake Outcomes relating to child anthropometric measures: not reported |
| Starting date | October 2017 |
| Contact information | Associate Professor Susan Sisson, susan‐sisson@ouhsc.edu |
| Notes | Clinicaltrials.gov: NCT03560050 |
Watt 2014.
| Study name | Methodological development of an exploratory randomised controlled trial of an early years' nutrition intervention: the CHERRY programme (Choosing Healthy Eating when Really Young) |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): England (Cornwall and Islington) Number of services participating: 16 |
| Interventions |
Number of conditions: 1 intervention, 1 control Intervention strategies: Ethos and environment ECEC staff Training: a staff training session will be offered to all staff working in the centres. The training session covered various aspects of healthy eating and nutrition for early years and included an introduction and overview of the CHERRY programme. Each training session will be tailored to the needs of the staff, as identified by heads of each intervention centre. Support: intervention centres will be given support and advice to revise and develop their centre’s food policies in order to support healthy eating practices and procedures. Partnerships Families Education: 4 x 2‐h sessions (1 each week) will be delivered over 4 weeks. The first hour of each session will involve parents discussing and learning about a variety of aspects of healthy eating. The second hour will involve parents and children together for a more practical, ‘hands on’ cook and eat session involving basic food preparation and tasting. Each session will begin with a recap from the previous week and finish with parents being given a ‘CHERRY at home’ activity to complete before the following week’s session. The intervention group will receive SMS reminders via mobile phones between sessions. |
| Outcomes |
Outcomes relating to child dietary intake: Fruit intake, vegetable intake, soft drink intake, sugary foods intake Outcomes relating to child anthropometric measures: not reported |
| Starting date | October 2010 |
| Contact information | Professor Richard Geddie Watt, r.watt@ucl.ac.uk |
| Notes | Trial registration not reported. |
Yin 2019.
| Study name | Study protocol for a cluster randomized controlled trial to test "¡Míranos! Look at Us, We Are Healthy!" ‐ an early childhood obesity prevention program |
| Methods | Study design: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): USA (San Antonio) Number of services participating: 12 |
| Interventions |
Number of conditions: 1 relevant intervention, 1 non‐ECEC intervention 1 control Intervention strategies: Health curriculum Children Curriculum: 9 modules with short, age‐appropriate learning activities, hands‐on games, and interactive DVD activities (The Get Healthy Now Show) will be integrated into daily centre routines. Ethos and environment Children Exposure: children will participate in daily physical activity (30‐min structured and 60‐min non‐structured play) during outdoor/indoor play, learning centre time, and transitions. Teachers will use ¡Míranos! Activity Cards (at least one card/d) and equipment supplied by the study to meet the physical activity goals. ECEC staff Wellness program: a staff wellness programme, which consists of a staff wellness manual and challenges, to improve staff's own health and become healthy role models for the children at the centre Materials: teachers will have access to a wellness manual and the ¡Míranos! eBook that will provide weekly intervention schedules, electronic copies of intervention activities, access to online movement music and videos, and online audio/video versions of the children’s storybooks. Posters to track staff progress will be posted in a staff‐only area and centre directors will report the number of staff who participated in the challenge and who achieved their goal to receive cash incentives for their centre. Service Policy: nutrition policies will be modified to include best practices. Meal modifications: menus will be modified to meet best practices and will be covered by supplemental funding from the study. Materials: a training DVD will be provided to detail lesson implementation and demonstrate gross motor activities to help teachers develop confidence and overcome challenges in leading the activities and to reinforce key concepts from the staff training. |
| Outcomes |
Outcomes relating to child dietary intake: Fruit intake, vegetable intake, beverage consumption Outcomes relating to child anthropometric measures: Height, weight, BMI, BMI z‐score |
| Starting date | May 2018 |
| Contact information | Professor Zenong Yin, zenong.yin@utsa.edu |
| Notes | ClinicalTrials.Gov: NCT03590834 |
Zarnowiecki 2021.
| Study name | Application of the multiphase optimisation strategy to develop, optimise and evaluate the effectiveness of a multicomponent initiative package to increase 2‐to‐5‐year‐old children's vegetable intake in long day care centres: a study protocol |
| Methods |
Study design: Phase 1: full factorial design Phase 2: cluster‐RCT |
| Participants |
Service type: centre‐based Country (region): Australia (Adelaide) Number of services participating: Phase 1: 32 Phase 2: 20 |
| Interventions |
Number of conditions: Phase 1: 7 interventions, 1 control Phase 2: 1 intervention, 1 control Intervention strategies: Phase 1 Intervention 1 Health curriculum Children Curriculum: a series of 16 short (~10–20‐min) lessons and hands‐on activities delivered during intentional teaching time. Children Exposure: a series of 16 snack time occasions where vegetables will be tasted and critical strategies to reinforce children’s enjoyment of vegetables can be consolidated. Materials: supporting resources and activities to further familiarise children with vegetables and their senses and a group reward chart to track progress of vegetables tasted. Ethos and environment ECEC staff Education: a lesson package for educators that aims to provide opportunities for children to learn about, try and enjoy vegetables by increasing their exposure to a variety of familiar and unfamiliar vegetables. Educators will complete an interactive online training module (~45–55 min) which includes topics about the role of the educator in promoting healthy eating, creating supportive meal time environments, use of feeding practices, overcoming barriers related to food rejection and planning and implementing a strategy within their centre. Educators and teachers will then apply the knowledge and strategies learnt in training during mealtimes in the 8 weeks of the implementation period. Training: cooks will complete an online training module, use an online menu planning tool to review their menu and implement the revised menu. Feedback: cooks will use an automated online menu assessment tool to assess compliance of their menu with guidelines and will revise their menu based on this feedback. Intervention 2 Ethos and environment ECEC staff Education: a lesson package for educators that aims to provide opportunities for children to learn about, try and enjoy vegetables by increasing their exposure to a variety of familiar and unfamiliar vegetables. Educators will complete an interactive online training module (~45–55 min) which includes topics about the role of the educator in promoting healthy eating, creating supportive meal time environments, use of feeding practices, overcoming barriers related to food rejection and planning and implementing a strategy within their centre. Educators and teachers will then apply the knowledge and strategies learnt in training during mealtimes in the 8 weeks of the implementation period. Training: cooks will complete an online training module, use an online menu planning tool to review their menu and implement the revised menu. Feedback: cooks will use an automated online menu assessment tool to assess compliance of their menu with guidelines and will revise their menu based on this feedback. Intervention 3 Ethos and environment ECEC staff Training: cooks will complete an online training module, use an online menu planning tool to review their menu and implement the revised menu. Feedback: cooks will use an automated online menu assessment tool to assess compliance of their menu with guidelines and will revise their menu based on this feedback. Intervention 4 Health curriculum Children Curriculum: a series of 16 short (~10–20 min) lessons and hands‐on activities delivered during intentional teaching time. Materials: supporting resources and activities to further familiarise children with vegetables and their senses and a group reward chart to track progress of vegetables tasted. Ethos and environment Children Exposure: a series of 16 snack time occasions where vegetables will be tasted and critical strategies to reinforce children’s enjoyment of vegetables can be consolidated. ECEC staff Education: a lesson package for educators that aims to provide opportunities for children to learn about, try and enjoy vegetables by increasing their exposure to a variety of familiar and unfamiliar vegetables. Training: cooks will complete an online training module, use an online menu planning tool to review their menu and implement the revised menu. Feedback: cooks will use an automated online menu assessment tool to assess compliance of their menu with guidelines and will revise their menu based on this feedback. Intervention 5 Health curriculum Children Curriculum: a series of 16 short (~10–20 min) lessons and hands‐on activities delivered during intentional teaching time. Materials: supporting resources and activities to further familiarise children with vegetables and their senses and a group reward chart to track progress of vegetables tasted. Ethos and environment Children Exposure: a series of 16 snack time occasions where vegetables will be tasted and critical strategies to reinforce children’s enjoyment of vegetables can be consolidated. ECEC staff Education: a lesson package for educators that aims to provide opportunities for children to learn about, try and enjoy vegetables by increasing their exposure to a variety of familiar and unfamiliar vegetables. Educators will complete an interactive online training module (~45–55 min) which includes topics about the role of the educator in promoting healthy eating, creating supportive meal time environments, use of feeding practices, overcoming barriers related to food rejection and planning and implementing a strategy within their centre. Educators and teachers will then apply the knowledge and strategies learnt in training during mealtimes in the 8 weeks of the implementation period. Intervention 6 Health curriculum Children Curriculum: a series of 16 short (~10–20 min) lessons and hands‐on activities delivered during intentional teaching time. Materials: supporting resources and activities to further familiarise children with vegetables and their senses and a group reward chart to track progress of vegetables tasted. Ethos and environment Children Exposure: a series of 16 snack time occasions where vegetables will be tasted and critical strategies to reinforce children’s enjoyment of vegetables can be consolidated. ECEC staff Education: a lesson package for educators that aims to provide opportunities for children to learn about, try and enjoy vegetables by increasing their exposure to a variety of familiar and unfamiliar vegetables. Intervention 7 Ethos and environment ECEC staff Training: educators will complete an interactive online training module (~45–55 min) which includes topics about the role of the educator in promoting healthy eating, creating supportive meal time environments, use of feeding practices, overcoming barriers related to food rejection and planning and implementing a strategy within their centre. Educators and teachers will then apply the knowledge and strategies learnt in training during mealtimes in the 8 weeks of the implementation period. Phase 2 Authors hypothesise that the optimised initiative package will include all 3 initiatives. |
| Outcomes |
Outcomes relating to child dietary intake: Phase 1: vegetable intake Phase 2: vegetable intake Outcomes relating to child anthropometric measures: not reported |
| Starting date | Phase 1: January 2021 Phase 2: January 2022 |
| Contact information | Professor Rebecca K Golley, rebecca.golley@flinders.edu.au |
| Notes | Phase 1: ACTRN12620001301954 Phase 2: ACTRN12620001323910p |
ECEC: early childhood education and care; RCT: randomised controlled trial
Differences between protocol and review
We specified that we would include all dietary outcomes and anthropometric outcomes in the protocol (Yoong 2021). However, we obtained a large number of dietary and anthropometric outcomes that were highly heterogeneous, only reported by one study, and could not reasonably be synthesised with other outcomes. As such, we undertook a posthoc selection of dietary and anthropometric outcomes consistent with those outlined in a recently published core outcome set of obesity prevention interventions in the early years (Brown 2022). The dietary outcomes selected were also consistent with those specified a priori for the summary of finding tables.
High risk of bias was defined inconsistently in the protocol (defined as scoring high on one or more of any risk of bias domains and scoring high on three or more risk of bias domains). We have chosen to classify overall high risk of bias as scoring high on three or more of the risk of bias criteria, given the challenges with blinding associated with public health interventions and assessment of the primary outcomes (diet).
We specified in the protocol that we would prioritise unadjusted over adjusted estimates. However, given that all included studies were cluster‐randomised controlled trials (RCTs), we have prioritised cluster‐adjusted estimates.
For cluster‐RCTs that did not appropriately account for clustering, we specified that we would calculate a design effect and effective sample size using study data (number of clusters, number of participants analysed) and mean intracluster correlation coefficient (ICC) from the included studies. As the ICC values across studies were skewed, we used the median ICC instead of the mean.
For multi‐arm studies, we specified that we would split the control group into two or more groups to form independent comparisons. However, we have combined the separate interventions arms, given that the overall aim was to assess the effectiveness of early childhood education and care‐based healthy eating interventions.
We specified that we would undertake pooled analysis by the World Health Organization Health Promoting Schools components by health curriculum only versus usual care/no intervention, ethos and environment only versus usual care/no intervention, and partnerships component only versus usual care/no intervention. As the majority of interventions included two or more Health Promoting Schools' components, we could not undertake a subgroup comparison by discrete components only. Instead, we included multi‐component interventions as long as a particular component was addressed relative to control.
Contributions of authors
Sze Lin Yoong, Luke Wolfenden and Alice Grady conceived the idea for this review. Sze Lin Yoong, Jacklyn Jackson, Luke Wolfenden, Sam McCrabb, Alix Hall and Alice Grady contributed to the methods for the protocol. Sze Lin Yoong, Melanie Lum, Jacklyn Jackson and Debbie Booth developed the search strategy for the review. Melanie Lum and Jannah Z Jones provided support with manuscript drafting and referencing. All authors provided critical comments and final approval for the manuscript.
Sources of support
Internal sources
-
Deakin University, Australia
Salary support for review author
-
University of Newcastle, Australia
Salary support for review authors
-
Hunter New England Population Health, Australia
Salary support for review authors
-
University College Dublin, Ireland
Salary support for review author
-
National Centre of Implementation Science, Australia
Salary support for review authors
-
Montclair State University, USA
Salary support for review author
External sources
-
National Health and Medical Research Council (NHMRC), Australia
This research is supported by the NHMRC through a Centre for Research Excellence grant (grant number APP1153479).
-
Priority Research Centre for Health Behaviour (PRCHB), Australia
This research received small grant funding from the Priority Research Centre for Health Behaviour (PRCHB) in 2021.
Declarations of interest
Sze Lin Yoong: is currently undertaking primary research that may be relevant to the review. Where we included such a study, other authors who were not directly involved in the study completed screening, data extraction and 'risk of bias assessments. This author has not received any benefit, in cash or kind, any hospitality, or any subsidy derived from any source perceived to have an interest in the outcome of the review.
Melanie Lum: declares no conflict of interest.
Jacklyn Jackson: declares no conflict of interest.
Luke Wolfenden: is currently undertaking primary research that may be relevant to the review. Where we included such a study, other authors who were not directly involved in the study completed screening, data extraction and risk of bias assessments. This author has not received any benefit, in cash or kind, any hospitality, or any subsidy derived from any source perceived to have an interest in the outcome of the review. Luke Wolfenden is Co‐ordinating Editor of Cochrane Public Health and was not involved in any stage of the editorial management or assessment of this review.
Courtney Barnes: is currently undertaking primary research that may be relevant to the review. Where we included such a study, other authors who were not directly involved in the study completed screening, data extraction and risk of bias assessments. This author has not received any benefit, in cash or kind, any hospitality, or any subsidy derived from any source perceived to have an interest in the outcome of the review.
Alix E Hall: is a Methods Editor for Cochrane Public Health and was not involved in any stage of the editorial management or assessment of this review.
Sam McCrabb: is Assistant Managing Editor and Methods Editor and was not involved in any stage of the editorial management or assessment of this review.
Nicole Pearson: is currently undertaking primary research that may be relevant to the review. Where we included such a study, other authors who were not directly involved in the study completed screening, data extraction and risk of bias assessments. This author has not received any benefit, in cash or kind, any hospitality, or any subsidy derived from any source perceived to have an interest in the outcome of the review.
Cassandra Lane: declares no conflict of interest.
Jannah Z Jones: is currently undertaking primary research that may be relevant to the review. Where we included such a study, other authors who were not directly involved in the study completed screening, data extraction and risk of bias assessments. This author has not received any benefit, in cash or kind, any hospitality, or any subsidy derived from any source perceived to have an interest in the outcome of the review.
Lauren Dinour: declares no conflict of interest.
Therese McDonnell: declares no conflict of interest.
Debbie Booth: declares no conflict of interest.
Alice Grady: is currently undertaking primary research that may be relevant to the review. Where we included such a study, other authors who were not directly involved in the study completed screening, data extraction and risk of bias assessments. This author has not received any benefit, in cash or kind, any hospitality, or any subsidy derived from any source perceived to have an interest in the outcome of the review.
New
References
References to studies included in this review
Alkon 2014 {published data only}
- Alkon A, Crowley A, Neelon S, Hill S, Pan Y, Nguyen V, et al. Nutrition and physical activity randomized control trial in child care centers improves knowledge, policies, and children’s body mass index. BMC Public Health 2014;14(215):13. [DOI: 10.1186/1471-2458-14-215] [DOI] [PMC free article] [PubMed] [Google Scholar]
Başkale 2011 {published data only}
- Başkale H, Bahar Z. Outcomes of nutrition knowledge and healthy food choices in 5- to 6-year-old children who received a nutrition intervention based on Piaget’s theory. Journal for Specialists in Pediatric Nursing 2011;16:263-79. [DOI: 10.1111/j.1744-6155.2011.00300.x] [DOI] [PubMed] [Google Scholar]
Blomkvist 2021 {published data only}
- Blomkvist E, Wills A, Helland S, Hillesund E, Øverby N. A cluster randomized web-based intervention trial to reduce food neophobia and promote healthy diets among one-year-old children in kindergarten: study protocol. BMC Pediatrics 2018;18:232. [DOI: 10.1186/s12887-018-1206-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blomkvist E, Wills A, Helland S, Hillesund E, Øverby N. Effectiveness of a kindergarten-based intervention to increase vegetable intake and reduce food neophobia amongst 1-year-old children: a cluster randomised controlled trial. Food & Nutrition Research 2021;65:7679. [DOI: 10.29219/fnr.v65.7679] [DOI] [PMC free article] [PubMed] [Google Scholar]
Céspedes 2013 {published data only}
- Céspedes J, Briceño G, Farkouh M, Vedanthan R, Baxter J, Leal M, et al. Promotion of cardiovascular health in preschool children: 36-month cohort follow-up. American Journal of Medicine 2013;126(12):1122-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Céspedes J, Briceño G, Farkouh M, Vedanthan R, Baxter J, Leal M, et al. Targeting preschool children to promote cardiovascular health: cluster randomized trial. American Journal of Medicine 2013;126(1):27-35e.3. [DOI: 10.1016/j.amjmed.2012.04.045] [DOI] [PMC free article] [PubMed] [Google Scholar]
Davis 2016 {published data only}
- Davis S, Sanders S, FitzGerald C, Keane P, Canaca G, Volker-Rector R. CHILE: an evidence-based preschool intervention for obesity prevention in Head Start. Journal of School Health 2013;83(3):223-9. [DOI: 10.1111/josh.12018] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis SM, Myers OB, Cruz TH, Morshed AB, Canaca GF, Keane PC, O'Donald ER. CHILE: Outcomes of a group randomized controlled trial of an interventionto prevent obesity in preschool Hispanic and American Indian children. Preventive Medicine 2016;89:162-8. [DOI: 10.1016/j.ypmed.2016.05.018] [DOI] [PMC free article] [PubMed] [Google Scholar]
De Bock 2011 {published data only}
- De Bock F, Breitenstein L, Fischer J. Positive impact of a pre-school-based nutritional intervention on children’s fruit and vegetable intake: results of a cluster-randomized trial. Public Health Nutrition 2011;15(3):466-75. [DOI: 10.1017/S136898001100200X] [DOI] [PubMed] [Google Scholar]
- De Bock F, Fischer J, Hoffmann K, Renz-Polster H. A participatory parent-focused intervention promoting physical activity in preschools: design of a cluster-randomized trial. BMC Public Health 2010;10(49):13. [DOI: 10.1016/j.amepre.2013.01.032] [DOI] [PMC free article] [PubMed] [Google Scholar]
De Coen 2012 {published data only}
- De Coen V, De Bourdeaudhuij I, Vereecken C, Verbestel V, Haerens L, Huybrechts I, et al. Effects of a 2-year healthy eating and physical activity intervention for 3–6-year-olds in communities of high and low socio-economic status: the POP (Prevention of Overweight among Pre-school and school children) project. Public Health Nutrition 2012;15(9):1737-45. [DOI: 10.1017/S1368980012000687] [DOI] [PubMed] [Google Scholar]
Eliakim 2007 {published data only}
- Eliakim A, Nemet D, Balakirski Y, Epstein Y. The effects of nutritional-physical activity school-based Intervention on fatness and fitness in preschool children. Journal of Pediatric Endocrinology & Metabolism 2007;20(6):711-8. [DOI: 10.1515/jpem.2007.20.6.711] [DOI] [PubMed] [Google Scholar]
Fernandez‐Jimenez 2019 {published data only}
- Bansilal S, Vedanthan R, Kovacic J, Soto A, Latina J, Björkegren J, et al. Rationale and design of family-based approach in a minority community integrating systems-biology for promotion of health (FAMILIA). American Heart Journal 2017;187:170-81. [DOI: 10.1016/j.ahj.2017.02.020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez-Jimenez R, Jaslow R, Bansilal S, Santana M, Diaz-Munoz R, Latina J, et al. Child health promotion in underserved communities: the FAMILIA Trial. Journal of the American College of Cardiology 2019;73(16):2011-21. [DOI: 10.1016/j.jacc.2019.01.057] [DOI] [PubMed] [Google Scholar]
Fitzgibbon 2005 {published data only}
- Fitzgibbon M, Stolley M, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Two-year follow-up results for Hip-Hop to Health Jr.: a randomized controlled trial for overweight prevention in preschool minority children. Journal of Pediatrics 2005;146(5):618-25. [DOI: 10.1016/j.jpeds.2004.12.019] [DOI] [PubMed] [Google Scholar]
- Stolley M, Fitzgibbon M, Dyer A, Van Horn L, KauferChristoffel K, Schiffer L. Hip-Hop to Health Jr., an obesity prevention program for minority preschool children: baseline characteristics of participants. Preventive Medicine 2003;36(3):320-9. [PMID: 10.1016/s0091-7435(02)00068-3] [DOI] [PubMed] [Google Scholar]
Fitzgibbon 2006 {published data only}
- Fitzgibbon M, Stolley M, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Hip-Hop to Health Jr. for Latino preschool children. Obesity 2006;14(9):1616-25. [DOI: 10.1038/oby.2006.186] [DOI] [PubMed] [Google Scholar]
Fitzgibbon 2011 {published data only}
- Fitzgibbon M, Stolley M, Dyer A, Van Horn L, KauferChristoffel K. A community-based obesity prevention program for minority children: rationale and study design for Hip-Hop to Health Jr. Preventive Medicine 2002;34(2):289-97. [PMID: 10.1006/pmed.2001.0977] [DOI] [PubMed] [Google Scholar]
- Fitzgibbon M, Stolley M, Schiffer L, Braunschweig C, Gomez S, Van Horn L, et al. Hip-Hop to Health Jr. obesity prevention effectiveness trial: post intervention results. Obesity 2011;19(5):994-1003. [DOI: 10.1038/oby.2010.314] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong A, Buscemi J, Stolley M, Schiffer L, Kim Y, Braunschweig C, et al. Hip-Hop to Health Jr. randomized effectiveness trial 1-year follow-up results. American Journal of Preventive Medicine 2016;50(2):136-44. [DOI: 10.1016/j.amepre.2015.07.008] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fitzgibbon 2013 {published data only}
- Fitzgibbon M, Stolley M, Schiffer L, Kong A, Braunschweig C, Gomez-Perez S, et al. Family-based Hip-Hop to Health: outcome results. Obesity 2013;21(2):274-83. [DOI: 10.1038/oby.2012.136] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gans 2022 {published data only}
- Gans K, Tovar A, Kang A, Ward D, Stowers K, Ash T, et al. A multi‑component tailored intervention in family childcare homes improves diet quality and sedentary behavior of preschool children compared to an attention control: results from the Healthy Start‑Comienzos Sanos cluster randomized trial. International Journal of Behavioral Nutrition and Physical Activity 2022;19:45. [DOI: 10.1186/s12966-022-01272-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Risica P, Tovar A, Palomo V, Dionne L, Mena N, Magid K, et al. Improving nutrition and physical activity environments of family child care homes:the rationale, design and study protocol of the ‘Healthy Start/Comienzos Sanos’ cluster randomized trial. BMC Public Health 2019;19(1):419. [DOI: 10.1186/s12889-019-6704-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Grummon 2019 {published data only}
- Grummon A, Cabana M, Hecht A, Alkon A, McCulloch C, Brindis C, et al. Effects of a multipronged beverage intervention on young children’s beverage intake and weight: a cluster-randomized pilot study. Public Health Nutrition 2019;22(15):2856-67. [DOI: 10.1017/S1368980019001629] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hodgkinson 2019 {published data only}
- Hodgkinson A, Abbott J, Hurley M, Lowe N, Qualter P. An educational intervention to prevent overweight in pre-school years: a cluster randomised trial with a focus on disadvantaged families. BMC Public Health 2019;19(1):13. [DOI: 10.1186/s12889-019-7595-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hu 2009 {published data only}
- Hu C, Ye D, Li Y, Huang Y, Li L, Gao Y, et al. Evaluation of a kindergarten-based nutrition education intervention for pre-school children in China. Public Health Nutrition 2009;13(2):253-60. [DOI: 10.1017/S1368980009990814] [DOI] [PubMed] [Google Scholar]
Iaia 2017 {published data only}
- Iaia M, Pasini M, Burnazzi A, Vitali P, Allara E, Farneti M. An educational intervention to promote healthy lifestyles in preschool children: a cluster-RCT. International Journal of Obesity 2017;41:582–90. [DOI: 10.1038/ijo.2016.239] [DOI] [PubMed] [Google Scholar]
Jones 2015 {published data only}
- Jones J, Wolfenden L, Wyse R, Finch M, Yoong S, Dodds P, et al. A randomised controlled trial of an intervention to facilitate the implementation of healthy eating and physical activity policies and practices in childcare services. BMJ Open 2014;4:e005312. [DOI: 10.1136/bmjopen-2014-005312] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones J, Wyse R, Finch M, Lecathelinais C, Wiggers J, Marshall J, et al. Effectiveness of an intervention to facilitate the implementation of healthy eating and physical activity policies and practices in childcare services: a randomised controlled trial. Implementation Science 2015;10(1):15. [DOI: 10.1186/s13012-015-0340-z] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kipping 2019 {published data only}
- Kipping R, Jago R, Metcalfe C, White J, Papadaki A, Campbell R, et al. NAP SACC UK: protocol for a feasibility cluster randomised controlled trial in nurseries and at home to increase physical activity and healthy eating in children aged 2–4 years. BMJ Open 2016;6:e010622. [DOI: 10.1136/bmjopen-2015-010622] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kipping R, Langford R, Brockman R, Wells S, Metcalfe C, Papadaki A, et al. Child-care self-assessment to improve physical activity, oral health and nutrition for 2- to 4-year-olds: a feasibility cluster RCT. Public Health Research 2019;7(13):1. [DOI: 10.3310/phr07130] [DOI] [PubMed] [Google Scholar]
Kobel 2019 {published data only}
- Kobel S, Wartha O, Wirt T, Dreyhaupt J, Lämmle C, Friedemann E, et al. Design, implementation, and study protocol of a kindergarten-based health promotion intervention. BioMed Research International 2017;2017:e4347675. [DOI: 10.1155/2017/4347675] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobela S, Warthaa O, Lämmlea C, Dreyhauptb J, Steinacker J. Intervention effects of a kindergarten-based health promotion programme on obesity related behavioural outcomes and BMI percentiles. Preventive Medicine Reports 2019;15:e100931. [DOI: 10.1016/j.pmedr.2019.100931] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kornilaki 2021 {published data only}
- Kornilaki E, Skouteris H, Morris H. Developing connections between healthy living and environmental sustainability concepts in Cretan preschool children: a randomized trial. Early Childhood Development and Care 2021;1:1-14. [DOI: 10.1080/03004430.2021.1925664] [DOI] [Google Scholar]
Kristiansen 2019 {published data only}
- Himberg-Sundet A, Kristiansen A, Frost Andersen L, Bjelland M, Lien N. Effects of a kindergarten intervention on vegetables served and staff's food-related practices: results of a cluster randomised controlled trial - the BRA study. Public Health Nutrition 2020;23(6):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristiansen A, Bjelland M, Himberg-Sundet A, Lien N, Andersen L. Associations between physical home environmental factors and vegetable consumption among Norwegian 3-5-year-olds: the BRA-study. Public Health Nutrition 2017;20(7):1173-83. [DOI: 10.1017/S1368980016003396] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristiansen A, Bjelland M, Himberg-Sundet A, Lien N, Holst R, Andersen L. Effects of a cluster randomized controlled kindergarten-based intervention trial on vegetable consumption among Norwegian 3–5-year-olds: the BRA-study. BMC Public Health 2019;19(1):1098. [DOI: 10.1186/s12889-019-7436-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristiansen A, Medin A, Bjelland M, Himberg‑Sundet A, Lien N, Holst R, et al. Long-term effects of a cluster randomized controlled kindergarten-based intervention trial on vegetable intake among Norwegian 3–5-year-olds: the BRA-study. BMC Research 2020;13(30):5. [DOI: 10.1186/s13104-020-4892-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Leis 2020 {published data only}
- Bélanger M, Humbert L, Vatanparast H, Ward S, Muhajarine N, Chow A, et al. A multilevel intervention to increase physical activity and improve healthy eating and physical literacy among young children (ages 3-5) attending early childcare centres: the Healthy Start-Départ Santé cluster randomised controlled trial study protocol. BMC Public Health volume 2016;16:313. [DOI: 10.1186/s12889-016-2973-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leis A, Ward S, Vatanparast H, Humbert M, Chow A, Muhajarine N, et al. Effectiveness of the Healthy Start-Départ Santé approach on physical activity, healthy eating and fundamental movement skills of preschoolers attending childcare centres: a randomized controlled trial. BMC Public Health 2020;20:523. [DOI: 10.1186/s12889-020-08621-9] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sari N, Muhajarine N, Chow A. The Saskatchewan/New Brunswick Healthy Start-Départ Santé intervention: implementation cost estimates of a physical activity and healthy eating intervention in early learning centers. BMC Health Services Research 2017;17:57. [DOI: 10.1186/s12913-017-1978-9] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lerner‐Geva 2014 {published data only}
- Lerner-Geva L, Bar-Zvi E, Levitan G, Boyko V, Reichman B, Pinhas-Hamiel O. An intervention for improving the lifestyle habits of kindergarten children in Israel: a cluster-randomised controlled trial investigation. Public Health Nutrition 2015;18(9):1537-44. [DOI: 10.1017/S136898001400024X] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lumeng 2017 {published data only}
- Lumeng J, Miller A, Horodynski M, Brophy-Herb H, Contreras D, Lee H, et al. Improving self-regulation for obesity prevention in Head Start: a randomized controlled trial. Pediatrics 2017;139(5):e20162047. [DOI: 10.1542/peds.2016-2047] [DOI] [PubMed] [Google Scholar]
- Miller A, Horodynski M, Herb H, Peterson K, Contreras D, Kaciroti D, et al. Enhancing self-regulation as a strategy for obesity prevention in Head Start preschoolers: the growing healthy study. BMC Public Health 2012;12:1040. [DOI: 10.1186/1471-2458-12-1040] [DOI] [PMC free article] [PubMed] [Google Scholar]
Morris 2018 {published data only}
- Morris H, Edwards S, Cutter-Mackenzie A, Rutherford L, Williams-Smith J, Skouteris H. Evaluating the impact of teacher-designed, wellbeing and sustainability play-based learning experiences on young children's knowledge connections: a randomised trial. Australasian Journal of Early Childhood 2018;43(4):33-42. [DOI: 10.23965/AJEC.43.4.04] [DOI] [Google Scholar]
- Skouteris H, Edwards S, Rutherford L, Cutter-MacKenzie A, Huang T, O'Connor A. Promoting healthy eating, active play and sustainability consciousness in early childhood curricula, addressing the Ben10 problem: a randomised control trial. BMC Public Health 2014;14(1):548. [DOI] [PMC free article] [PubMed] [Google Scholar]
Namenek Brouwer 2013 {published data only}
- Namenek Brouwer R, Neelon S. Watch Me Grow: a garden-based pilot intervention to increase vegetable and fruit intake in preschoolers. BMC Public Health 2013;13:363. [DOI: 10.1186/1471-2458-13-363] [DOI] [PMC free article] [PubMed] [Google Scholar]
Natale 2014a {published data only}
- Natale R, Lopez-Mitnik G, Uhlhorn S, Asfour L, Messiah S. Effect of a child care center-based obesity prevention program on body mass index and nutrition practices among preschool-aged children. Health Promotion Practice 2014;15(5):695-705. [DOI: 10.1177/1524839914523429] [DOI] [PubMed] [Google Scholar]
Natale 2014b {published data only}
- McCollister K, Tolbert D, Mishra S, Natale R, Uhlhorn S, Messiah S. Cost analysis of a childcare center-based intervention to prevent obesity in the preschool years. Journal of Comprehensive Pediatrics 2015;6(2):e25845. [DOI: 10.17795/compreped-25845] [DOI] [Google Scholar]
- Natale R, Messiah S, Asfour L, Uhlhorn S, Delamater A, Arheart K. Role modeling as an early childhood obesity prevention strategy: effect of parents and teachers on preschool children's healthy lifestyle habits. Journal of Developmental & Behavioral Pediatrics 2014;35(6):378-87. [DOI: 10.1097/DBP.0000000000000074] [DOI] [PubMed] [Google Scholar]
- Natale R, Messiah S, Asfour L, Uhlhorn S, Englebert N, Arheart K. Obesity prevention program in childcare centers: two-year follow-up. American Journal of Health Promotion 2017;31(6):502-10. [DOI: 10.1177/0890117116661156] [DOI] [PubMed] [Google Scholar]
- Natale R, Scott S, Messiah S, Schrack M, Uhlhorn S, Delamater A. Design and methods for evaluating an early childhood obesity prevention program in the childcare center setting. BMC Public Health 2013;13:78. [DOI: 10.1186/1471-2458-13-78] [DOI] [PMC free article] [PubMed] [Google Scholar]
Natale 2021 {published data only}
- Messiah S, Lebron C, Moise R, Mathew R, Sardinas K, Chang C, et al. Healthy caregivers-healthy children (HC2) phase 2: integrating culturally sensitive childhood obesity prevention strategies into childcare center policies. Contemporary Clinical Trials 2016;53:60-7. [DOI: 10.1016/j.cct.2016.12.011] [DOI] [PubMed] [Google Scholar]
- Natale R, Atem F, Weerakoon S, Lebron C, Mathew M, Sardinas K, et al. An implementation approach comparison of a child care center-based obesity prevention program. Journal of Developmental & Behavioral Pediatrics 2021;42(2):135-45. [DOI: 10.1097/DBP.0000000000000861] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nekitsing 2019a {published data only}
- Nekitsing C, Blundell-Birtill P, Cockroft J, Hetherington M. Taste exposure increases intake and nutrition education increases willingness to try an unfamiliar vegetable in preschool children: a cluster randomized trial. Journal of the Academy of Nutrition and Dietetics 2019;119(12):2004-13. [DOI: 10.1016/j.jand.2019.05.012] [DOI] [PubMed] [Google Scholar]
Nemet 2011a {published data only}
- Nemet D, Geva D, Eliakim A. Health promotion intervention in low socioeconomic kindergarten children. Journal of Pediatrics 2011;158(5):796-801. [DOI: 10.1016/j.jpeds.2010.10.040] [DOI] [PubMed] [Google Scholar]
- Nemet D, Geva D, Pantanowitz M, Igbaria N, Meckel Y, Eliakim A. Long term effects of a health promotion intervention in low socioeconomic Arab-Israeli kindergartens. BMC Pediatrics 2013;13:45. [DOI: 10.1186/1471-2431-13-45] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nemet 2011b {published data only}
- Nemet D, Geva D, Pantanowitz M, Igbaria N, Meckel Y, Eliakim A. Health promotion intervention in Arab-Israeli kindergarten children. Journal of Pediatric Endocrinology & Metabolism 2011;24(11-12):1001-7. [DOI: 10.1515/JPEM.2011.387] [DOI] [PubMed] [Google Scholar]
Pearson 2022 {published data only}
- Pearson N, Finch, M, Sutherland R, Kingsland M, Wolfenden L, Wedesweiler T, et al. An mHealth intervention to reduce the packing of discretionary foods in children’s lunch boxes in early childhood education and care services: cluster randomized controlled trial. Journal of Medical Internet Research 2022;24(3):e27760. [DOI: 10.2196/27760] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pond N, Finch M, Sutherland R, Wolfenden L, Nathan N, Kingsland M, et al. Cluster randomised controlled trial of an m-health intervention in centre-based childcare services to reduce the packing of discretionary foods in children's lunchboxes: study protocol for the 'SWAP IT Childcare' trial. BMJ Open 2019;9(5):e026829. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peñalvo 2015 {published data only}
- Peñalvo J, Santos-Beneit G, Sotos-Prieto M, Bodega P, Oliva B, Orrit X, et al. The SI! Program for cardiovascular health promotion in early childhood: a cluster-randomized trial. Journal of the American College of Cardiology 2015;66(14):1525-34. [DOI: 10.1016/j.jacc.2015.08.014] [DOI] [PubMed] [Google Scholar]
- Peñalvo J, Santos-Beneit G, Sotos-Prieto M, Martínez R, Rodríguez C, Franco M, et al. A cluster randomized trial to evaluate the efficacy of a school-based behavioral intervention for health promotion among children aged 3 to 5. BMC Public Health 2013;13:656. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pinket 2016 {published data only}
- De Craemer M, Verbestel V, Verloigne M, Androutsos O, Moreno L, Iotova V, et al. Combining effect and process evaluation on European preschool children’s snacking behavior in a kindergarten-based, family-involved cluster randomized controlled trial: the ToyBox Study. International Journal of Environmental Research and Public Health 2020;17(19):7312. [DOI: 10.3390/ijerph17197312] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manios Y, Androutsos O, Katsarou C, Iotova V, Socha P, Geyer C, et al, on behalf of the ToyBox-study group. Designing and implementing a kindergarten-based, family-involved intervention to prevent obesity in early childhood: the ToyBox-study. Obesity Reviews 2014;15(3):5-13. [DOI: 10.1111/obr.12175] [DOI] [PubMed] [Google Scholar]
- Pinket A, Van Lippevelde W, De Bourdeaudhuij I, Deforche B, Cardon, Androutsos O, et al, ToyBox-Study Group. Effect and process evaluation of a cluster randomized control trial on water intake and beverage consumption in preschoolers from six European countries: the ToyBoxStudy. PLoS ONE 2016;11(4):e0152928. [DOI: 10.1371/journal.pone.0152928] [DOI] [PMC free article] [PubMed] [Google Scholar]
Puder 2011 {published data only}
- Burgi F, Niederer I, Schindler C, Bodenmann P, Marques-Vidal P, Kriemler S, et al. Effect of a lifestyle intervention on adiposity and fitness in socially disadvantaged subgroups of preschoolers: a cluster-randomized trial (Ballabeina). Preventive Medicine 2012;54(5):335-40. [DOI] [PubMed] [Google Scholar]
- Niederer I, Burgi F, Ebenegger V, Marques-Vidal P, Schindler C, Nydegger A, et al. Effects of a lifestyle intervention on adiposity and fitness in overweight or low fit preschoolers (Ballabeina). Obesity 2013;21(3):E287-93. [DOI] [PubMed] [Google Scholar]
- Niederer I, Kriemler S, Zahner L, Bürgi F, Ebenegger V, Hartmann T, et al. Influence of a lifestyle intervention in preschool children on physiological and psychological parameters (Ballabeina): study design of a cluster randomized controlled trial. BMC Public Health 2009;9:94. [DOI: 10.1186/1471-2458-9-94] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puder J, Marques-Vidal P, Schindler C, Zahner L, Niederer I, Bürgi F, et al. Effect of multidimensional lifestyle intervention on fitness and adiposity in predominantly migrant preschool children (Ballabeina): cluster randomised controlled trial. BMJ 2011;343:d6195. [DOI: 10.1136/bmj.d6195] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ray 2020 {published data only}
- Ray C, Figuereido R, Vepsäläinen H, Lehto R, Pajulahti R, Skaffari E, et al. Effects of the preschool-based family-involving DAGIS intervention program on children's energy balance-related behaviors and self-regulation skills: a clustered randomized controlled trial. Nutrients 2020;12(9):2599. [DOI: 10.3390/nu12092599] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray C, Kaukonen R, Lehto R, Vepsäläinen H, Sajaniemi N, Erkkola M, et al. Development of the DAGIS intervention study: a preschool-based family-involving study promoting preschoolers’ energy balance-related behaviours and self-regulation skills. BMC Public Health 2019;19:1670. [DOI: 10.1186/s12889-019-7864-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
Reyes‐Morales 2016 {published data only}
- Reyes-Morales H, González-Unzaga M, Jiménez-Aguilar A, Uribe-Carvajal R. Effect of an intervention based on child-care centers to reduce risk behaviors for obesity in preschool children. Boletín Médico del Hospital Infantil de México (English Edition) 2016;73(2):75-83. [DOI: 10.1016/j.bmhimx.2015.11.010] [DOI] [PubMed] [Google Scholar]
Roberts‐Gray 2018 {published data only}
- Roberts-Gray C, Ranjit N, Sweitzer S, Byrd-Williams C, Romo-Palafox M, Briley M, et al. Parent packs, child eats: surprising results of Lunch is in the Bag‘s efficacy trial. Appetite 2018;121:249-62. [DOI: 10.1016/j.appet.2017.10.033] [DOI] [PMC free article] [PubMed] [Google Scholar]
Seward 2018 {published data only}
- Seward K, Wolfenden L, Finch M, Wiggers J, Wyse R, Jones J, et al. Improving the implementation of nutrition guidelines in childcare centres improves child dietary intake: findings of a randomised trial of an implementation intervention. Public Health Nutrition 2018;21(3):607-17. [DOI: 10.1017/S1368980017003366] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seward K, Wolfenden L, Finch M, Wiggers J, Wyse R, Jones J, et al. Multistrategy childcare-based intervention to improve compliance with nutrition guidelines versus usual care in long day care services: a study protocol for a randomised controlled trial. BMJ Open 2016;6(6):e010786. [DOI: 10.1136/bmjopen-2015-010786] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoong S, Grady A, Seward K, Finch M, Wiggers J, Lecathelinais C, et al. The impact of a childcare food service intervention on child dietary intake in care: an exploratory cluster randomized controlled trial. Quantitative Research 2019;33(7):991-1001. [DOI: 10.1177/0890117119837461] [DOI] [PubMed] [Google Scholar]
Stookey 2017 {published data only}
- Stookey R, Evans J, Chan C, Tao-Lew L, Arana T, Arthur S. Healthy Apple program to support child care centers to alter nutrition and physical activity practices and improve child weight: a cluster randomized trial. BMC Public Health 2017;17(1):965. [DOI: 10.1186/s12889-017-4951-y] [DOI] [PMC free article] [PubMed] [Google Scholar]
Toussaint 2021 {published data only}
- Toussaint N, Streppel M, Mul S, Balledux M, Van Drongelen K, Janssen M, et al. The effects of a preschool-based intervention for early childhood education and care teachers in promoting healthy eating and physical activity in young children: a cluster randomised controlled trial. PloS One 2021;16(7):e0255023. [DOI: 10.1371/journal.pone.0255023] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toussaint N, Streppel M, Mul S, Schreurs A, Balledux M, Van Drongelen K, et al. A preschool-based intervention for early childhood education and care (ECEC) teachers in promoting healthy eating and physical activity in toddlers: study protocol of the cluster randomized controlled trial PreSchool@HealthyWeight. BMC Public Health 2019;19(1):278. [DOI: 10.1186/s12889-019-6611-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vaughn 2021 {published data only}
- Hennink-Kaminski H, Vaughn A, Hales D, Moore R, Luecking C, Ward D. Parent and child care provider partnerships: protocol for the Healthy Me, Healthy We (HMHW) cluster randomized control trial. Contemporary Clinical Trials 2018;64:49-57. [DOI: 10.1016/j.cct.2017.11.007] [DOI] [PubMed] [Google Scholar]
- Vaughn A, Hennink-Kaminski H, Moore R, Burney R, Chittams J, Parker P, et al. Evaluating a child care-based social marketing approach for improving children’s diet and physical activity: results from the Healthy Me, Healthy We cluster-randomized controlled trial. Translational Behavioral Medicine 2021;11(3):775-84. [DOI: 10.1093/tbm/ibaa113] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vereecken 2009 {published data only}
- Vereecken C, Huybrechts I, Van Houte H, Martens V, Wittebroodt I, Maes L. Results from a dietary intervention study in preschools “Beastly Healthy at School”. International Journal of Public Health 2009;54(3):142-9. [EMBASE: 10.1007/s00038-009-8028-2] [DOI] [PubMed] [Google Scholar]
Ward 2020a {published data only}
- Mann C, Ward D, Vaughn A, Benjamin-Neelon S, Long Vidal L, Omar S, et al. Application of the intervention mapping protocol to develop Keys, a family child care home intervention to prevent early childhood obesity. BMC Public Health 2015;15:1227. [DOI: 10.1186/s12889-015-2573-9] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward D, Vaughn A, Burney R, Hales D, Benjamin-Neelon S, Tovar A, et al. Keys to healthy family child care homes: results from a cluster randomized trial. Preventive Medicine 2020;132:105974. [DOI: 10.1016/j.ypmed.2019.105974] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Østbye T, Mann C, Vaughn A, Namenek Brouwer R, Neelon S, Hales D, et al. The keys to healthy family child care homes intervention: study design and rationale. Contemporary Clinical Trials 2015;40:81-9. [DOI: 10.1016/j.cct.2014.11.003] [DOI] [PMC free article] [PubMed] [Google Scholar]
Witt 2012 {published data only}
- Dunn C, Thomas C, Pegram L, Ward D, Schmal S. Color me healthy, preschoolers moving and eating healthfully. Journal of Nutrition Education and Behavior 2004;36(6):327-8. [DOI: 10.1016/s1499-4046(06)60403-x] [DOI] [PubMed] [Google Scholar]
- Witt K, Dunn C. Increasing fruit and vegetable consumption among preschoolers: evaluation of Color Me Healthy. Journal of Nutrition Education and Behavior 2012;44:107-13. [DOI: 10.1016/j.jneb.2011.01.002] [DOI] [PubMed] [Google Scholar]
Yeh 2018 {published data only}
- Yeh Y, Hartlieb K, Danford C, Jen K. Effectiveness of nutrition intervention in a selected group of overweight and obese African-American preschoolers. Journal of Racial and Ethnic Health Disparities 2017;5(3):553-61. [DOI: 10.1007/s40615-017-0399-0] [DOI] [PubMed] [Google Scholar]
Yoong 2020a {published data only}
- Reeves P, Edmunds K, Szewczyk Z, Grady A, Yoong S, Wolfenden L, et al. Economic evaluation of a web-based menu planning intervention to improve childcare service adherence with dietary guidelines. Implementation Science 2021;16(1):1. [DOI: 10.1186/s13012-020-01068-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoong S, Grady A, Wiggers J, Flood V, Rissel C, Finch M, et al. A randomised controlled trial of an online menu planning intervention to improve childcare service adherence to dietary guidelines: a study protocol. BMJ Open 2017;7(9):e017498. [DOI: 10.1136/bmjopen-2017-017498] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoong S, Grady A, Wiggers J, Stacey F, Rissel C, Flood V, et al. Child-level evaluation of a web-based intervention to improve dietary guideline implementation in childcare centers: a cluster-randomized controlled trial. American Journal of Clinical Nutrition 2020;111(4):854-63. [DOI: 10.1093/ajcn/nqaa025] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zask 2012 {published data only}
- Adams J, Zask A, Dietrich U. Tooty Fruity Vegie in Preschools: an obesity prevention intervention in preschools targeting children’s movement skills and eating behaviours. Health Promotion Journal of Australia 2009;20(2):112-9. [DOI: 10.1071/he09112] [DOI] [PubMed] [Google Scholar]
- Zask A, Adams J, Brooks L, Hughes D. Tooty Fruity Vegie: an obesity prevention intervention evaluation in Australian preschools. Health Promotion Journal of Australia 2012;23(1):10-5. [DOI: 10.1071/he12010] [DOI] [PubMed] [Google Scholar]
Zeinstra 2018 {published data only}
- Zeinstra G, Vrijhof M, Kremer S. Is repeated exposure the holy grail for increasing children's vegetable intake? Lessons learned from a Dutch childcare intervention using various vegetable preparations. Appetite 2018;121:316-25. [DOI: 10.1016/j.appet.2017.11.087] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Aherna 2019 {published data only}
- Aherna SM, Caton SJ, Blundell-Birtillc P, Hetherington MM. The effects of repeated exposure and variety on vegetable intake in pre-school children. Appetite 2019;132:37-43. [DOI] [PubMed] [Google Scholar]
Ariati 2019 {published data only}
- Ariati N, Suiraoka I, Fetria A, Padmiari I, Sugiani P, Purnamawati A, et al. Balanced nutrition services to early childhood improving children’s nutritional status. Indian Journal of Public Health Research and Development 2019;10(8):1332-7. [Google Scholar]
Batra 2014 {published data only}
- Batra P, Schlossman N, Balan E, Pruzensky W, Saltzman E, Roberts S. Effects of two micronutrient-fortified food aid products containing different levels of dairy protein on anthropometric variables in rural pre-school children in Guinea-Bissau. FASEB Journal. Conference: Experimental Biology 2014;28(S1):804.15. [Google Scholar]
Bayer 2009 {published data only}
- Bayer O, Kries R, Strauss A, Mitschek C, Toschke A, Hose A, et al. Short- and mid-term effects of a setting based prevention program to reduce obesity risk factors in children: a cluster-randomized trial. Clinical Nutrition 2009;28(2):122-8. [DOI] [PubMed] [Google Scholar]
Benjamin 2007 {published data only}
- Benjamin S, Ammerman A, Sommers J, Dodds J, Neelon B, Ward D. Nutrition and physical activity self-assessment for child care (NAP SACC): results from a pilot intervention. Journal of Nutrition Education & Behavior 2007;39(3):142-9. [DOI] [PubMed] [Google Scholar]
Benjamin 2008 {published data only}
- Benjamin S, Tate D, Bangdiwala S, Neelon B, Ammerman A, Dodds J, et al. Preparing child care health consultants to address childhood overweight: a randomized controlled trial comparing web to in-person training. Maternal & Child Health Journal 2008;12(5):662-9. [DOI] [PubMed] [Google Scholar]
Benjamin 2014 {published data only}
- Benjamin Neelon S, Taveras E, Ostbye T, Gillman M. Preventing obesity in infants and toddlers in child care: results from a pilot randomized controlled trial. Maternal & Child Health Journal 2014;18(5):1246-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Braga‐Pontes 2021 {published data only}
- Braga-Pontes C, Simoes-Dias S, Lages M, Guarino M, Graca P. Nutrition education strategies to promote vegetable consumption in preschool children: the Veggies4myHeart Project. Public Health Nutrition 2022;25(4):1061-70. [DOI: 10.1017/S1368980021004456] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brophy‐Herb 2017 {published data only}
- Brophy-Herb H, Horodynski M, Contreras D, Kerver J, Kaciroti N, Stein M, et al. Effectiveness of differing levels of support for family meals on obesity prevention among Head Start preschoolers: the Simply Dinner study. BMC Public Health 2017;17(1):184. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bryant 2021 {published data only}
- Bryant M, Collinson M, Burton W, Stamp E, Schofield H, Copsey B, et al. Cluster randomised controlled feasibility study of HENRY: a community-based intervention aimed at reducing obesity rates in preschool children. Pilot and Feasibility Studies 2021;7(1):59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Buscemi 2019 {published data only}
- Buscemi J, Odoms-Young A, Stolley M, Schiffer L, Blumstein L, Clark M, et al. Comparative effectiveness trial of an obesity prevention intervention in EFNEP and SNAP-ED: primary outcomes. Nutrients 2019;11(5):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Byrne 2002 {published data only}
- Byrne E, Nitzke S. Preschool children’s acceptance of a novel vegetable following exposure to messages in a storybook. Journal of Nutrition Education and Behavior 2002;34:211-4. [DOI] [PubMed] [Google Scholar]
Carstairs 2020 {published data only}
- Carstairs S, Caton S, Hetherington M, Rolls B, Cecil J. Colour as a cue to eat: effects of plate colour on snack intake in pre-school children. Food Quality and Preference 2020;83:103862. [Google Scholar]
Caton 2013 {published data only}
- Caton S, Ahern S, Remy E, Nicklaus S, Blundell P, Hetherington M. Repetition counts: repeated exposure increases intake of a novel vegetable in UK pre-school children compared to flavour-flavour and flavour-nutrient learning. British Journal of Nutrition 2013;109(11):2089-97. [DOI] [PubMed] [Google Scholar]
Chuang 2020 {published data only}
- Chuang R, Cox J, Mincemoyer C, Sharma S. A pilot randomized controlled trial of a nutrition and dietary intervention for early care and education providers. Journal of School Health 2020;90(11):859-68. [DOI] [PubMed] [Google Scholar]
Correia 2014 {published data only}
- Correia D, O'Connell M, Irwin M, Henderson K. Pairing vegetables with a liked food and visually appealing presentation: promising strategies for increasing vegetable consumption among preschoolers. Childhood Obesity 2014;10(1):72-6. [DOI] [PubMed] [Google Scholar]
Coulthard 2017 {published data only}
- Coulthard H, Sealy A. Play with your food! Sensory play is associated with tasting of fruits and vegetables in preschool children. Appetite 2017;113:84-90. [DOI] [PubMed] [Google Scholar]
Coulthard 2018 {published data only}
- Coulthard H, Williamson I, Palfreyman Z, Lyttle S. Evaluation of a pilot sensory play intervention to increase fruit acceptance in preschool children. Appetite 2018;120:609-15. [DOI] [PubMed] [Google Scholar]
Dazeley 2015 {published data only}
- Dazeley P, Houston-Price C. Exposure to foods' non-taste sensory properties. A nursery intervention to increase children's willingness to try fruit and vegetables. Appetite 2015;84:1-6. [DOI] [PubMed] [Google Scholar]
De Droog 2014 {published data only}
- De Droog S, Buijzen M, Valkenburg P. Enhancing children's vegetable consumption using vegetable-promoting picture books. The impact of interactive shared reading and character-product congruence. Appetite 2014;73:73-80. [DOI] [PubMed] [Google Scholar]
De Droog 2017 {published data only}
- De Droog S, Van Nee R, Govers M, Buijzen M. Promoting toddlers' vegetable consumption through interactive reading and puppetry. Appetite 2017;116:75-81. [DOI] [PubMed] [Google Scholar]
De Wild 2013 {published data only}
- De Wild V, De Graaf C, Jager G. Effectiveness of flavour nutrient learning and mere exposure as mechanisms to increase toddler's intake and preference for green vegetables. Appetite 2013;64:89-96. [DOI] [PubMed] [Google Scholar]
De Wild 2015 {published data only}
- De Wild V, De Graaf C, Jager G. Efficacy of repeated exposure and flavour-flavour learning as mechanisms to increase preschooler's vegetable intake and acceptance. Pediatr Obes 2015;10(3):205-12. [DOI] [PubMed] [Google Scholar]
De Wild 2017 {published data only}
- De Wild V, De Graaf C, Jager G. Use of different vegetable products to increase preschool-aged children's preference for and intake of a target vegetable: a randomized controlled trial. Journal of the Academy of Nutrition & Dietetics 2017;117(6):859-66. [DOI] [PubMed] [Google Scholar]
De Zwarte 2019 {published data only}
- De Zwarte D, Kearney J, Corish C, Glennon C, Maher L, Johnston Molloy C. Randomised study demonstrates sustained benefits of a pre-school intervention designed to improve nutrition and physical activity practices. Journal of Public Health (Oxford, England) 2019;41(4):798-806. [DOI] [PubMed] [Google Scholar]
Diktas 2021 {published data only}
- Diktas H, Roe L, Keller K, Sanchez C, Rolls B. Promoting vegetable intake in preschool children: independent and combined effects of portion size and flavor enhancement. Appetite 2021;164:105250. [DOI] [PMC free article] [PubMed] [Google Scholar]
Earnesty 2019 {published data only}
- Earnesty D, Alaimo K, Ha W, Creger A, Weatherspoon L. Generic nutrition education intervention does not increase dietary quality in childcare homes. Journal of the Academy of Nutrition & Dietetics 2019;119(9):A72. [Google Scholar]
Eichholzer‐Helbling 1986 {published data only}
- Eichholzer-Helbling M, Ritzel G, Ackermann-Liebrich U, Bächlin A, Mühlemann R. Nutrition education in the kindergarten: results of an intervention trial. Sozial- und Praventivmedizin 1986;31(4-5):233-5. [DOI] [PubMed] [Google Scholar]
Esquivel 2016 {published data only}
- Esquivel M, Nigg C, Fialkowski M, Braun K, Li F, Novotny R. Head Start wellness policy intervention in Hawaii: a project of the Children's Healthy Living program. Childhood Obesity 2016;12(1):26-32. [DOI] [PubMed] [Google Scholar]
Ferris 2012 {published data only}
- Ferris A, Lora K, Quesada C, Wakefied D. Effectiveness of an Information, Motivation, Behavior (IMB)-based theoretical model for reducing sugar-sweetened beverage (SSB) consumption in preschool children. Journal of Nutrition Education & Behavior 2012;44 Suppl 4:S83. [Google Scholar]
Finch 2019a {published data only}
- Finch M, Seward K, Wedesweiler T, Stacey F, Grady A, Jones J, et al. Challenges of increasing childcare center compliance with nutrition guidelines: a randomized controlled trial of an intervention providing training, written menu feedback, and printed resources. American Journal of Health Promotion 2019;33(3):399-411. [DOI] [PubMed] [Google Scholar]
Finch 2019b {published data only}
- Finch M, Stacey F, Jones J, Yoong S, Grady A, Wolfenden L. A randomised controlled trial of performance review and facilitated feedback to increase implementation of healthy eating and physical activity-promoting policies and practices in centre-based childcare. Implementation Science 2019;14(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Grady 2020 {published data only}
- Grady A, Seward K, Finch M, Wolfenden L, Wyse R, Wiggers J, et al. A three-arm randomised controlled trial of high- and low-intensity implementation strategies to support centre-based childcare service implementation of nutrition guidelines: 12-month follow-up. International Journal of Environmental Research & Public Health 2020;17(13):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hardy 2010 {published data only}
- Hardy L, King L, Kelly B, Farrell L, Howlett S. Munch and Move: evaluation of a preschool healthy eating and movement skill program. International Journal of Behavioral Nutrition & Physical Activity 2010;7:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harnack 2012 {published data only}
- Harnack LJ, Oakes J, French SA, Rydell SA, Farah FM, Taylor GL. Results from an experimental trial at a Head Start center to evaluate two meal service approaches to increase fruit and vegetable intake of preschool aged children. International Journal of Behavioral Nutrition and Physical Activity 2012;9:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hausner 2012 {published data only}
- Hausner H, Olsen A, Møller P. Mere exposure and flavour-flavour learning increase 2-3 year-old children's acceptance of a novel vegetable. Appetite 2012;58(3):1152-9. [DOI] [PubMed] [Google Scholar]
Hughes 2020b {published data only}
- Hughes S, Power T, Beck A, Betz D, Goodell L, Hopwood V, et al. Short-term effects of an obesity prevention program among low-income Hispanic families with preschoolers. Journal of Nutrition Education and Behavior 2020;52(3):224-39. [DOI] [PubMed] [Google Scholar]
Jouret 2009 {published data only}
- Jouret B, Ahluwalia N, Dupuy M, Cristini C, Nègre-Pages L, Grandjean H, et al. Prevention of overweight in preschool children: results of kindergarten-based interventions. International Journal of Obesity 2009;33(10):1075-83. [PMID: 10.1038/ijo.2009.166] [DOI] [PubMed] [Google Scholar]
Kashef 2021 {published data only}
- Kashef S, Zarnowiecki D, Brown V, Arguelles J, Cox D, Golley R. Cluster randomised controlled trial of a menu box delivery service for Australian long day care services to improve menu guideline compliance: a study protocol. BMJ Open 2021;11(4):e045136. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2019 {published data only}
- Kim J, Kim G, Park J, Wang Y, Lim H. Effectiveness of teacher-led nutritional lessons in altering dietary habits and nutritional status in preschool children: adoption of a NASA mission X-based program. Nutrients 2019;11(7):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kling 2016 {published data only}
- Kling S, Roe L, Sanchez C, Rolls B. Does milk matter: is children's intake affected by the type or amount of milk served at a meal? Appetite 2016;105:509-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kostecka 2022 {published data only}
- Kostecka M. The effect of the "Colorful Eating Is Healthy Eating" long-term nutrition education program for 3-to 6-year-olds on eating habits in the family and parental nutrition knowledge. International Journal of Environmental Research and Public Health 2022;19(4):1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lanigan 2019 {published data only}
- Lanigan J, Bailey R, Jackson A, Shea V. Child-centered nutrition phrases plus repeated exposure increase preschoolers' consumption of healthful foods, but not liking or willingness to try. Journal of Nutrition Education & Behavior 2019;51(5):519-27. [DOI] [PubMed] [Google Scholar]
Lawatsch 1990 {published data only}
- Lawatsch D. A comparison of two teaching strategies on nutrition knowledge, attitudes and food behavior of preschool children. Journal of Nutrition Education 1990;22(3):117-23. [Google Scholar]
Leahy 2008a {published data only}
- Leahy K, Birch L, Fisher J, Rolls B. Reductions in entrée energy density increase children's vegetable intake and reduce energy intake. Obesity (Silver Spring, Md.) 2008;16(7):1559-65. [DOI] [PubMed] [Google Scholar]
Leahy 2008b {published data only}
- Leahy K, Birch L, Rolls B. Reducing the energy density of multiple meals decreases the energy intake of preschool-age children. American Journal of Clinical Nutrition 2008;88(6):1459-68. [DOI] [PubMed] [Google Scholar]
Leahy 2008c {published data only}
- Leahy K, Birch L, Rolls B. Reducing the energy density of an entree decreases children's energy intake at lunch. Journal of the American Dietetic Association 2008;108(1):41-8. [DOI] [PubMed] [Google Scholar]
Leung 2019 {published data only}
- Leung C, Tsang S, Heung K, Tam M. Healthy start home visiting program-school-based model: cluster randomized controlled trial. Research on Social Work Practice 2019;29(6):628-43. [Google Scholar]
Lin 2016 {published data only}
- Lin M, Pan L, Han J, Li L, Jiang J, Jin R. Behavioral intervention reduces unhealthy eating behaviors in preschool children via a behavior card approach. Journal of Huazhong University of Science and Technology. Medical Sciences 2016;36(6):895-903. [DOI] [PubMed] [Google Scholar]
Malden 2019 {published data only}
- Malden S, Reilly J, Gibson A, Bardid F, Summerbell C, De Craemer M, et al. A feasibility cluster randomised controlled trial of a preschool obesity prevention intervention: ToyBox-Scotland. Pilot and Feasibility Studies 2019;5(1):128. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mannino 2019 {published data only}
- Mannino M, Rollins B, Francis L. Improving preschool children's food knowledge and food choice intentions: results from a childhood obesity preventive intervention. Journal of Nutrition Education & Behavior 2019;51:S11.
McSweeney 2017 {published data only}
- McSweeney L, Araújo-Soares V, Rapley T, Adamson A. A feasibility study with process evaluation of a preschool intervention to improve child and family lifestyle behaviours. BMC Public Health 2017;17:1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT03672227 {published data only}
- NCT03672227. Obesity prevention in Head Start. https://clinicaltrials.gov/show/NCT03672227 2018.
NCT03957148 {published data only}
- NCT03957148. Effectiveness of an IMB-based intervention for reducing sweetened beverages consumption in preschool children. https://clinicaltrials.gov/show/NCT03957148 2019.
NCT04552678 {published data only}
- NCT04552678. Healthy Bodies Project to prevent childhood obesity. https://clinicaltrials.gov/show/NCT04552678 2020.
NCT05050539 {published data only}
- NCT05050539. Adaptive implementation to optimize delivery of obesity prevention practices in early care and education settings. https://clinicaltrials.gov/show/NCT05050539 2021. [DOI] [PMC free article] [PubMed]
Neelon 2016 {published data only}
- Neelon S, Mayhew M, O'Neill J, Neelon B, Li F, Pate R. Comparative evaluation of a South Carolina policy to improve nutrition in child care. Journal of the Academy of Nutrition and Dietetics 2016;116(6):949-56. [DOI] [PubMed] [Google Scholar]
Nekitsing 2019b {published data only}
- Nekitsing C, Blundell-Birtill P, Cockroft J, Fildes A, Hetherington M. Increasing intake of an unfamiliar vegetable in preschool children through learning using storybooks and sensory play: a cluster randomized trial. Journal of the Academy of Nutrition & Dietetics 2019;1:1. [DOI] [PubMed] [Google Scholar]
Norman 2019 {published data only}
- Norman Å, Zeebari Z, Nyberg G, Elinder L. Parental support in promoting children's health behaviours and preventing overweight and obesity - a long-term follow-up of the cluster-randomised healthy school start study II trial. BMC Pediatrics 2019;19(1):104. [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Connell 2012 {published data only}
- O'Connell ML, Henderson K, Luedicke J, Schwartz M. Repeated exposure in a natural setting: a preschool intervention to increase vegetable consumption. Journal of the Academy of Nutrition and Dietetics 2012;112(2):230-4. [DOI] [PubMed] [Google Scholar]
Rhee 2019 {published data only}
- Rhee K, Kessl S, Manzano M, Strong D, Boutelle K. Cluster randomized control trial promoting child self-regulation around energy-dense food. Appetite 2019;133:156-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ritchie 2019 {published data only}
- Ritchie L, Lee D, Alkon A, Neelon M, Rios K, Soule K. Evaluation of an interactive, online training for child care providers on healthy beverages for young children. Current Developments in Nutrition 2019;3 Suppl 1:P16-039-19.
Rollins 2021 {published data only}
- Rollins B, Stein W, Keller K, Savage J. Preschoolers will drink their GREENS! Children accept, like, and drink novel smoothies containing dark green vegetables (DGVs). Appetite 2021;162:105148. [DOI] [PubMed] [Google Scholar]
Schuler 2019 {published data only}
- Schuler B, Fowler B, Rubio D, Kilby S, Wang Y, Hager E, et al. Building blocks for healthy children: evaluation of a child care center-based obesity prevention pilot among low-income children. Journal of Nutrition Education & Behavior 2019;51(8):958-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sirasa 2021 {published data only}
- Sirasa F, Mitchell L, Azhar A, Chandrasekara A, Harris N. A six-week healthy eating intervention with family engagement improves food knowledge and preferences but not dietary diversity among urban preschool children in Sri Lanka. Public Health Nutrition 2021;24(12):4328-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Slining 2021 {published data only}
- Slining M, Wills S, Fair M, Stephenson J, Knobel S, Pearson M, et al. LiveWell in early childhood: results from a two-year pilot intervention to improve nutrition and physical activity policies, systems and environments among early childhood education programs in South Carolina. BMC Public Health 2021;21(1):919. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2019 {published data only}
- Smith E, Sutarso T, Kaye G. Access with education improves fruit and vegetable intake in preschool children. Journal of Nutrition Education & Behavior 2019;5:5. [DOI] [PubMed] [Google Scholar]
Sojkowski 2012 {published data only}
- Sojkowski S, Severin S, Kannan S. Sensory exploration of seasonally and locally available vegetables and their effects on vegetable consumption of Western Massachusetts Head Start preschool children. FASEB Journal. Conference: Experimental Biology 2012;26:Meeting Abstracts. [Google Scholar]
Sweitzer 2010 {published data only}
- Sweitzer S, Briley M, Roberts-Gray C, Hoelscher D, Harrist R, Staskel D, et al. Lunch is in the bag: increasing fruits, vegetables, and whole grains in sack lunches of preschool-aged children. Journal of the American Dietetic Association 2010;110(7):1058-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Swindle 2021 {published data only}
- Swindle T, McBride N, Selig J, Johnson S, Whiteside-Mansell L, Martin J, et al. Stakeholder selected strategies for obesity prevention in childcare: results from a small-scale cluster randomized hybrid type III trial. Implementation Science 2021;16(1):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vaughn 2019b {published data only}
- NCT03938103. Evaluation of an enhanced delivery model for go NAPSACC. https://clinicaltrials.gov/show/NCT03938103 (first received 6 May 2019).
- Vaughn A, Studts C, Powell B, Ammerman A, Trogdon J, Curran G, et al. The impact of basic vs. enhanced Go NAPSACC on child care centers' healthy eating and physical activity practices: protocol for a type 3 hybrid effectiveness-implementation cluster-randomized trial. Implementation Science 2019;14(1):101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vepsäläinen 2022 {published data only}
- Vepsäläinen H, Skaffari E, Wojtkowska K, Barliska J, Kinnunen S, Makkonen R, et al. A mobile app to increase fruit and vegetable acceptance among Finnish and Polish preschoolers: randomized trial. JMIR mHealth and uHealth 2022;10(1):e30352. [DOI] [PMC free article] [PubMed] [Google Scholar]
Verbestel 2014 {published data only}
- Verbestel V, De Coen V, Van Winckel M, Huybrechts I, Maes L, De Bourdeaudhuij I. Prevention of overweight in children younger than 2 years old: a pilot cluster-randomized controlled trial. Public Health Nutrition 2014;17(6):1384-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vitale 2020 {published data only}
- Vitale N, Coccia C. Effects of a Montessori-based nutrition education program with fruit and vegetable taste testing on intake, preferences, and nutrition knowledge of preschool and kindergarten children. Journal of the Academy of Nutrition & Dietetics 2020;120:A50.
Ward 2008 {published data only}
- Ward D, Benjamin S, Ammerman A, Ball S, Neelon B, Bangdiwala S. Nutrition and physical activity in child care: results from an environmental intervention. American Journal of Preventive Medicine 2008;35(4):352-6. [DOI] [PubMed] [Google Scholar]
Ward 2017 {published data only}
- Ward D, Vaughn A, Mazzucca S, Burney R. Translating a child care based intervention for online delivery: development and randomized pilot study of Go NAPSACC. BMC Public Health 2017;17(1):891. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ward 2020b {published data only}
- Ward S, Belanger M, Leis A. Comparison between the Healthy Start-Depart Sante online and in-person training of childcare educators to improve healthy eating and physical activity practices and knowledge of physical activity and fundamental movement skills: a controlled trial. Preventive Medicine Reports 2020;20:101264. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 1998 {published data only}
- Williams C, Squillace M, Bollella M, Brotanek J, Campanaro L, D'Agostino C, et al. Healthy Start: a comprehensive health education program for preschool children. Preventive Medicine 1998;27(2):216-23. [DOI] [PubMed] [Google Scholar]
Williams 2002 {published data only}
- Williams C, Bollella M, Strobino B, Spark A, Nicklas T, Tolosi L, et al. "Healthy-start": outcome of an intervention to promote a heart healthy diet in preschool children. Journal of the American College of Nutrition 2002;21(1):62-71. [DOI] [PubMed] [Google Scholar]
Yeom 2019 {published data only}
- Yeom M, Cho Y. Nutrition education on discouraging sugar intake led to improve the moderation factor of nutrition quotient in pre-school children. Annals of Nutrition & Metabolism 2019;75(3):126. [Google Scholar]
Yoong 2016 {published data only}
- Yoong Y, Jones J, Marshall J, Wiggers J, Seward K, Finch M, et al. A theory-based evaluation of a dissemination intervention to improve childcare cooks' intentions to implement nutritional guidelines on their menus. Implementation Science 2016;11(1):105. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
ChiCTR2200060958 {published data only}
- ChiCTR1800017292. Childhood Healthy Activities Model Policies Study. http://www.chictr.org.cn/showprojen.aspx?proj=29374 (first received 23 July 2018).
References to ongoing studies
Armstrong 2019 {published data only}
- Armstrong B, Trude A, Johnson C, Castelo R, Zemanick A, Haber-Sage S, et al. CHAMP: a cluster randomized-control trial to prevent obesity in child care centers. Contemporary Clinical Trials 2019;86:105849. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barnes 2020 {published data only}
- Barnes C, Grady A, Nathan N, Wolfenden L, Pond N, McFayden T, et al. A pilot randomised controlled trial of a web-based implementation intervention to increase child intake of fruit and vegetables within childcare centres. Pilot and Feasibility Studies 2020;6(1):163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes C, Yoong S, Nathan N, Wolfenden L, Wedesweiler T, Kerr J, et al. Feasibility of a web-based implementation intervention to improve child dietary intake in early childhood education and care: pilot randomized controlled trial. Journal of Medical Internet Research 2021;23(12):e25902. [DOI] [PMC free article] [PubMed] [Google Scholar]
Beckerman 2019 {published data only}
- Beckerman J, Aftosmes-Tobio A, Kitos N, Jurkowski J, Lansburg K, Kazik C, et al. Communities for healthy living (CHL) - a family-centered childhood obesity prevention program integrated into Head Start services: study protocol for a pragmatic cluster randomized trial. Contemporary Clinical Trials 2019;78:34-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cosco 2021 {published data only}
- Cosco N, Wells N, Monsur M, Goodell L, Zhang D, Xu T, et al. Research design, protocol, and participant characteristics of COLEAFS: a cluster randomized controlled trial of a childcare garden intervention. Journal of Environmental Research and Public Health 2021;18:13066. [DOI: 10.3390/ijerph182413066] [DOI] [PMC free article] [PubMed] [Google Scholar]
Helland 2016 {published data only}
- Helland S, Bere E, Overby N. Study protocol for a multi-component kindergarten-based intervention to promote healthy diets in toddlers: a cluster randomized trial. BMC Public Health 2016;16:273. [DOI] [PMC free article] [PubMed] [Google Scholar]
ISRCTN33134697 {published data only}
- ISRCTN33134697. NAP SACC (UK): nutrition and physical activity self-assessment for childcare. https://doi.org/10.1186/ISRCTN33134697 (first received 24 October 2019).
Lee 2019 {published data only}
- Lee R, Lorenzo E, Szeszulski J, Arriola A, Bruening M, Estabrooks P, et al. Design and methodology of a cluster-randomized trial in early care and education centers to meet physical activity guidelines: sustainability via Active Garden Education (SAGE). Contemporary Clinical Trials 2019;77:8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Malden 2018 {published data only}
- Malden S, Hughes A, Gibson A, Bardid F, Androutsos O, De Craemer M, et al. Adapting the ToyBox obesity prevention intervention for use in Scottish preschools: protocol for a feasibility cluster randomised controlled trial. BMJ Open 2018;8(10):e023707. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mehdizadeh 2018 {published data only}
- Mehdizadeh A, Nematy M, Khadem-Rezaiyan M, Ghayour-Mobarhan M, Sardar MA, Leis A, et al. A customized intervention program aiming to improve healthy eating and physical activity among preschool children: protocol for a randomized controlled trial (Iran Healthy Start Study). JMIR Research Protocols 2018;7(12):e11329. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT01890681 {published data only}
- NCT01890681. Baby nutrition and physical activity self-assessment for child care (NAP SACC) intervention study. https://clinicaltrials.gov/ct2/show/NCT01890681 (first received 2 July 2013).
NCT02580123 {published data only}
- NCT02580123. Smile-Kids: study on complementary feeding transition. https://clinicaltrials.gov/ct2/show/NCT02580123 (first received 20 October 2015).
NCT03575884 {published data only}
- NCT03575884. Fit 5 Kids screen time reduction curriculum for Latino preschoolers (Fit5Kids). https://clinicaltrials.gov/ct2/show/NCT03575884 (first received 3 July 2018).
NCT03601299 {published data only}
- NCT03601299. Back to Basics: addressing childhood obesity through traditional foods in Alaska. https://clinicaltrials.gov/ct2/show/NCT03601299 (first received 26 July 2018).
NCT03668678 {published data only}
- NCT03668678. iGrow Readers nutrition and physical activity curriculum efficacy. https://clinicaltrials.gov/ct2/show/NCT03668678 (first received 12 September 2018).
NCT04082247 {published data only}
- NCT04082247. Healthy Children 2021 Study in childcare centers (HC2021). https://clinicaltrials.gov/ct2/show/NCT04082247 (first received 9 September 2019).
NCT04140032 {published data only}
- NCT04140032. Addressing obesity in early care and education settings. https://clinicaltrials.gov/ct2/show/NCT04140032 (first received 25 October 2019).
NCT04164277 {published data only}
- NCT04164277. FirstStep2Health Intervention. https://clinicaltrials.gov/ct2/show/NCT04164277 (first received 15 November 2019).
NCT04711525 {published data only}
- NCT04711525. i-MaCHeL Study is a two-group, cluster-RCT, involves 460 preschool's child-parent dyads, to prevent childhood obesity (i-MaCHeL). https://clinicaltrials.gov/ct2/show/NCT04711525 (first received 15 January 2021).
NCT05112185 {published data only}
- NCT05112185. Childcare healthy beverage access, food and beverage intake, and obesity. https://www.clinicaltrials.gov/ct2/show/NCT05112185 (first received 8 November 2021).
Reeves 2018 {published data only}
- Reeves S, Poh B, Essau C, Summerbell C, Cheah W, Koh D, et al. ToyBox Study Malaysia: improving healthy energy balance and obesity-related behaviours among pre-schoolers in Malaysia. Nutrition Bulletin 2018;43(3):290-5. [Google Scholar]
Sisson 2019 {published data only}
- Sisson S, Salvatore A, Hildebrand D, Poe T, Merchant C, Slawinski M, et al. Interventions to promote healthy environments in family child care homes in Oklahoma - Happy Healthy Homes: study protocol for a randomized controlled trial. Trials 2019;20(1):541. [DOI] [PMC free article] [PubMed] [Google Scholar]
Watt 2014 {published data only}
- Watt R, Draper A, Ohly H, Rees G, Pikhart H, Cooke L, et al. Methodological development of an exploratory randomised controlled trial of an early years’ nutrition intervention: the CHERRY programme (Choosing Healthy Eating when Really Young). Maternal and Child Nutrition April 2014;10(2):280-94. [DOI: 10.1111/mcn.12061] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yin 2019 {published data only}
- Yin Z, Ullevig S, Sosa E, Liang Y, Olmstead T, Howard J, et al. Study protocol for a cluster randomized controlled trial to test "¡Míranos! Look at Us, We Are Healthy!" - an early childhood obesity prevention program. BMC Pediatrics 2019;19(1):190. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zarnowiecki 2021 {published data only}
- Zarnowiecki D, Kashef S, Poelman A, Cochet-Broch M, Arguelles J, Cox D, et al. Application of the multiphase optimisation strategy to develop, optimise and evaluate the effectiveness of a multicomponent initiative package to increase 2-to-5-year-old children's vegetable intake in long day care centres: a study protocol. BMJ Open 2021;11(12):e047618. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Aluko 2022
- Aluko P, Graybill E, Craig D, Henderson C, Drummond M, Wilson EC, et al, on behalf of the Campbell and Cochrane Economics Methods Group. Chapter 20: Economic evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook.
Australian Government 2009
- Department of Health and Ageing. Get up & grow: healthy eating and physical activity for early childhood. https://www.health.gov.au/sites/default/files/documents/2021/04/family-book-get-up-and-grow-family-book.pdf (accessed prior to 2 February 2022).
Ball 2007
- Ball S, Benjamin S, Ward D. Development and reliability of an observation method to assess food intake of young children in child care. Journal of the American Dietetic Association 2007;107:656-61. [DOI] [PubMed] [Google Scholar]
Baxter 2015
- Baxter J. Child care and early childhood education in Australia (Fact Sheets 2015). Available at aifs.gov.au/publications/child-care-and-early-childhood-education-australia (accessed prior to 20 July 2020).
Benjamin‐Neelon 2011
- Benjamin-Neelon S, Briley M, American Dietetic Association. Position of the American Dietetic Association: benchmarks for nutrition in child care. Journal of the American Dietetic Association 2011;111(4):607-15. [DOI: 10.1016/j.jada.2011.02.016] [DOI] [PubMed] [Google Scholar]
Benjamin‐Neelon 2018
- Benjamin-Neelon SE, Vaughn AE, Tovar A, Østbye T, Mazzucca S, Ward DS. The family child care home environment and children's diet quality. Appetite 2018;126:108-13. [DOI: 10.1016/j.appet.2018.03.024] [DOI] [PMC free article] [PubMed] [Google Scholar]
Berenson 1998
- Berenson G, Srinivasan S, Bao W, Newman W, Tracy R, Wattigney W. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. New England Journal of Medicine 1998;338:1650-6. [DOI] [PubMed] [Google Scholar]
Brown 2019
- Brown T, Moore T, Hooper L, Gao Y, Zayegh A, Ijaz S, et al. Interventions for preventing obesity in children. Cochrane Database of Systematic Reviews 2019, Issue 7. Art. No: CD001871. [DOI: 10.1002/14651858.CD001871.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brown 2022
- Brown V, Moodie M, Sultana M, Hunter K, Byrne R, Seidler A, et al. Core outcome set for early intervention trials to prevent obesity in childhood (COS-EPOCH): Agreement on "what" to measure. International Journal of Obesity 2022 Aug 4 [Epub ahead of print]. [DOI: 10.1038/s41366-022-01198-w] [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2020
- Campbell M, McKenzie J, Sowden A, Katikireddi S, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ 2020;368:16890. [DOI] [PMC free article] [PubMed] [Google Scholar]
Castellano 2014
- Castellano J, Peñalvo J, Bansilal S, Fuster V. Promotion of cardiovascular health at three stages of life: never too soon, never too late [Promoción de la salud cardiovascular en tres etapas de la vida: nunca es demasiado pronto, nunca demasiado tarde]. Revista Española de Cardiología (English Edition) 2014;67:731-7. [DOI] [PubMed] [Google Scholar]
Chriqui 2020
- Chriqui JF, Leider J, Schermbeck RM, Sanghera A, Pugach O. Changes in Child and Adult Care Food Program (CACFP) practices at participating childcare and education centers in the United States following updated national standards, 2017–2019. Nutrients 2020;12(9):2818. [DOI: 10.3390/nu12092818] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cochrane 2016
- Cochrane T, Davey R, Castella FR. Estimates of the energy deficit required to reverse the trend in childhood obesity in Australian school children. Australian and New Zealand Journal of Public Health 2016;40(1):62-7. [DOI: 10.1111/1753-6405.12474] [DOI] [PMC free article] [PubMed] [Google Scholar]
Covidence [Computer program]
- Covidence. Version (accessed prior to 8 January 2021). Melbourne, Australia: Veritas Health Innovation, 2021. Available at covidence.org.
Deeks 2022
- Deeks JJ, Higgins JP, Altman DG editor(s). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook. [www.training.cochrane.org/handbook]
Development Initiatives 2018
- Development Initiatives. Development Initiatives, 2018. 2018 Global Nutrition Report: shining a light to spur action on nutrition. Bristol, UK: Development Initiatives. Available at who.int/nutrition/globalnutritionreport/2018_Global_Nutrition_Report.pdf?ua=1 (accessed prior to 20 December 2020).
EPOC 2021
- Cochrane Effective Practice and Organisation of Care (EPOC). EPOC Resources for review authors. epoc.cochrane.org/resources/epoc-resources-review-authors (accessed prior to 14 January 2021).
Ettrich 2006
- Ettrich K, Ettrich C. Testmanual zum Konzentrations-Handlungsverfahren für Vorschulkinder [Testing manual for concentration assessment in preschool children]. Hogrefe, 2006. [Google Scholar]
European Commission 2021
- European Commission. Early childhood education and care. ec.europa.eu/education/policies/early-childhood-education-and-care_en (accessed prior to 14 January 2021).
GBD 2017 Diet Collaborators
- GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019;393(10184):1958-72. [DOI: 10.1016/S0140-6736(19)30041-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
Glanville 2020
- Glanville J, Kotas E, Featherstone R, Dooley G. Which are the most sensitive search filters to identify randomized controlled trials in MEDLINE? Journal of the Medical Library Association 2020;108(4):556-63. [DOI: 10.5195/jmla.2020.912] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Version (accessed prior to 8 January 2021). Hamilton (ON): McMaster University (developed by Evidence Prime), 2022. Available at gradepro.org.
Grady 2019
- Grady A, Wolfenden L, Rissel C, Green S, Reilly K, Yoong S. Effectiveness of a dissemination strategy on the uptake of an online menu planning program: a controlled trial. Health Promotion Journal of Australia 2019;30 Suppl 1:20-5. [DOI] [PubMed] [Google Scholar]
Grob 2009
- Grob A, Meyer CS, Hagmann-von Arx P. Intelligence and Development Scales (IDS). Hans Huber, 2009. [DOI] [PubMed] [Google Scholar]
Guerrero 2016
- Guerrero A, Mao C, Fuller B, Bridges M, Franke T, Kuo A. Racial and ethnic disparities in early childhood obesity: growth trajectories in body mass index. Journal of Racial and Ethnic Health Disparities 2016;3:129-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2011
- Guyatt G, Oxman A, Akl E, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2011;64:383-94. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins J, Thompson S, Deeks J, Altman D. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins J, Altman D, Sterne J editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. https://training.cochrane.org/handbook/archive/v5.1/.
Higgins 2022
- Higgins JP, Eldridge S, Li T (editors). Chapter 23: Including variants on randomized trials. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Available from www.training.cochrane.org/handbook.
Hodder 2020
- Hodder R, O'Brien K, Tzelepis F, Wyse R, Wolfenden L. Interventions for increasing fruit and vegetable consumption in children aged five years and under. Cochrane Database of Systematic Reviews 2020, Issue 5. Art. No: CD008552. [DOI: 10.1002/14651858.CD008552.pub7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Howard 2017
- Howard S, Melhuish E. An early years toolbox for assessing early executive function, language, self-regulation, and social development: validity, reliability, and preliminary norms. Journal of Psychoeducational Assessment 2017;35(3):255-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jackson 2021
- Jackson J, Jones J, Nguyen H, Davies I, Lum M, Grady A, et al. Obesity prevention within the early childhood education and care setting: a systematic review of dietary behavior and physical activity policies and guidelines in high income countries. International Journal of Environmental Research and Public Health 2021;18(2):838. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kamerman 2007
- Kamerman S, Gatenio-Gabel S. Early childhood education and care in the United States: an overview of the current policy picture. International Journal of Child Care and Education Policy 2007;1:23-34. [Google Scholar]
Kariippanon 2022
- Kariippanon K, Chong K, Janssen X, Tomaz S, Ribeiro E, Munambah N, et al. Levels and correlates of objectively measured sedentary behavior in young children: SUNRISE study results from 19 countries. Medicine and Science in Sports and Exercise 2022;54(7):1123-30. [DOI: 10.1249/MSS.0000000000002886] [DOI] [PMC free article] [PubMed] [Google Scholar]
Khalid 2017
- Khalid S, Williams C, Reynolds S. Is there an association between diet and depression in children and adolescents? A systematic review. British Journal of Nutrition 2017;116:2097–108. [DOI: 10.1017/S0007114516004359] [DOI] [PubMed] [Google Scholar]
Koning 2016
- Koning M, Hoekstra T, De Jong E, Visscher T, Seidell J, Renders C. Identifying developmental trajectories of body mass index in childhood using latent class growth (mixture) modelling: associations with dietary, sedentary and physical activity behaviors: a longitudinal study. BMC Public Health 2016;16:1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
Korin 2016
- Korin MR. Theory and Fundamentals of Health Promotion for Children and Adolescents. In: Korin, M. (eds) Health Promotion for Children and Adolescents. Boston, MA: Springer, 2016. [DOI: 10.1007/978-1-4899-7711-3_2] [DOI] [Google Scholar]
Langford 2014
- Langford R, Bonell C, Jones H, Pouliou T, Murphy S, Waters E, et al. The WHO Health Promoting School framework for improving the health and well‐being of students and their academic achievement. Cochrane Database of Systematic Reviews 2014, Issue 4. Art. No: CD008958. [DOI: 10.1002/14651858.CD008958.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lichtenberger 2005
- Lichtenberger E. General measures of cognition for the preschool child. Mental Retardation and Developmental Disabilities Research Reviews 2005;11:197-208. [DOI] [PubMed] [Google Scholar]
Lichtenberger 2009
- Lichtenberger E, Sotelo-Dynega M, Kaufman A. The Kaufman Assessment Battery for Children-Second Edition. In: Practitioner's guide to assessing intelligence and achievement. Hoboken, NJ, US: John Wiley & Sons Inc, 2009:61-93. [Google Scholar]
Lindsay 2015
- Lindsay AC, Salkeld JA, Greaney ML, Sands FD. Latino family childcare providers' beliefs, attitudes, and practices related to promotion of healthy behaviors among preschool children: a qualitative study. Journal of Obesity 2015;2015:409742. [DOI: 10.1155/2015/409742] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lum 2021
- Lum M, Grady A, Falkiner M, Jones J, Finch M, Green S, et al. Assessing the implementation of healthy eating and physical activity policies and practices in the family day care setting: a cross-sectional study. Health Promotion Journal of Australia 2021;32 Suppl 2:116-25. [DOI: 10.1002/hpja.420] [DOI] [PubMed] [Google Scholar]
Matwiejczyk 2018
- Matwiejczyk L, Mehta K, Scott J, Tonkin E, Coveney J. Characteristics of effective interventions promoting healthy eating for pre-schoolers in childcare settings: an umbrella review. Nutrients 2018;10:293. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maynard 2003
- Maynard M, Gunnell D, Emmett P, Frankel S, Davey Smith G. Fruit, vegetables, and antioxidants in childhood and risk of adult cancer: the Boyd Orr cohort. Journal of Epidemiology and Community Health 2003;57(3):218-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
McKenzie 2022a
- McKenzie JE, Brennan SE. Chapter 12: Synthesizing and presenting findings using other methods. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook.
McKenzie 2022b
- McKenzie JE, Brennan SE, Ryan RE, Thomson HJ, Johnston RV, Thomas J. Chapter 3: Defining the criteria for including studies and how they will be grouped for the synthesis. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook.
Microsoft Excel [Computer program]
- Microsoft Excel. Microsoft Corporation, (accessed prior to 20 April 2022). office.microsoft.com/excel.
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, for the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morgan 2020
- Morgan E, Schoonees A, Sriram U, Faure M, Seguin-Fowler R. Caregiver involvement in interventions for improving children's dietary intake and physical activity behaviors. Cochrane Database of Systematic Reviews 2020, Issue 1. Art. No: CD012547. [DOI: 10.1002/14651858.CD012547.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Murad 2017
- Murad M, Mustafa R, Schünemann H, Sultan S, Santesso N. Rating the certainty in evidence in the absence of a single estimate of effect. BMJ Evidence-Based Medicine 2017;22:85-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nathan 2019
- Nathan N, Janssen L, Sutherland R, Hodder R, Evans C, Booth D, et al. The effectiveness of lunchbox interventions on improving the foods and beverages packed and consumed by children at centre-based care or school: a systematic review and meta-analysis. International Journal of Behavioural Nutrition and Physical Activity 2019;16(1):38. [DOI: 10.1186/s12966-019-0798-1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ness 2005
- Ness A, Maynard M, Frankel S, Smith G, Frobisher C, Leary SD, et al. Diet in childhood and adult cardiovascular and all cause mortality: the Boyd Orr cohort. Heart 2005;91(7):894. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nixon 2012
- Nixon CA, Moore HJ, Douthwaite W, Gibson EL, Vogele C, Kreichauf S, et al, on behalf of the ToyBox‐study group. Identifying effective behavioural models and behaviour change strategies underpinning preschool-and school-based obesity prevention interventions aimed at 4–6-year-olds: a systematic review. Obesity Reviews 2012;13 Suppl 1:106-17. [DOI: 10.1111/j.1467-789X.2011.00962.x] [DOI] [PubMed] [Google Scholar]
O'Neil 2014
- O'Neil A, Quirk S, Housden S, Brennan S, Williams L, Pasco J, et al. Relationship between diet and mental health in children and adolescents: a systematic review. American Journal of Public Health 2014;104(10):e31-42. [DOI: 10.2105/AJPH.2014.302110] [DOI] [PMC free article] [PubMed] [Google Scholar]
OECD 2014
- OECD. Enrolment in childcare and pre-schools. Available at oecd.org/els/soc/PF3_2_Enrolment_childcare_preschool.pdf (accessed prior to 1 February 2021).
OECD 2019
- OECD - Social Policy Division - Directorate of Employment Labour and Social Affairs. PF3.2: Enrolment in childcare and pre-school. Available at oecd.org/els/soc/PF3_2_Enrolment_childcare_preschool.pdf (accessed prior to 1 February 2021).
Pons 2004
- Pons F, Harris PL, Rosnay M. Emotion comprehension between 3 and 11 years: developmental periods and hierarchical organization. European Journal of Developmental Psychology 2004;1(2):127-52. [DOI: 10.1080/17405620344000022] [DOI] [Google Scholar]
Ravens‐Sieberer 2010
- Ravens-Sieberer U, Erhart M, Rajmil L, Herdman M, Auquier P, Bruil J, et al, European KIDSCREEN Group. Reliability, construct and criterion validity of the KIDSCREEN-10 score: a short measure for children and adolescents' well-being and health-related quality of life. Quality of Life Ressearch 2010;19(10):1487-500. [DOI: 10.1007/s11136-010-9706-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan Web 2023 [Computer program]
- Review Manager Web (RevMan Web). Version 5.1.0. The Cochrane Collaboration, 2023. Available at revman.cochrane.org.
Rodrigues 2013
- Rodrigues A, Abreu G, Resende R, Goncalves W, Gouvea S. Cardiovascular risk factor investigation: a pediatric issue. International Journal of General Medicine 2013;6:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Santesso 2020
- Santesso N, Glenton C, Dahm P, Garner P, Akl E, Alper B, et al. GRADE guidelines 26: informative statements to communicate the findings of systematic reviews of interventions. Journal of Clinical Epidemiology 2020;119:126-35. [DOI] [PubMed] [Google Scholar]
Schünemann 2022a
- Schünemann HJ, Vist GE, Higgins JP, Santesso N, Deeks JJ, Glasziou P, et al. Chapter 15: Interpreting results and drawing conclusions. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook. [DOI: 10.1002/9781119536604.ch15] [DOI]
Schünemann 2022b
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Chapter 14: Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Available from www.training.cochrane.org/handbook. [www.training.cochrane.org/handbook]
Shrestha 2015
- Shrestha R, Copenhaver M. Long-term effects of childhood risk factors on cardiovascular health during adulthood. Clinical Medicine Reviews in Vascular Health 2015;7:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sisson 2016
- Sisson S, Krampe M, Anundson K, Castle S. Obesity prevention and obesogenic behavior interventions in child care: a systematic review. Preventive Medicine 2016;87:57-69. [DOI: 10.1016/j.ypmed.2016.02.016] [DOI] [PubMed] [Google Scholar]
Soanes 2001
- Soanes R, Miller M, Begley A. Nutrient intakes of two-and three-year-old children: a comparison between those attending and not attending long day care centres. Australian Journal of Nutrition and Dietetics 2001;58:114-20. [Google Scholar]
Stacey 2017
- Stacey F, Finch M, Wolfenden L, Grady A, Jessop K, Wedesweiler T, et al. Evidence of the potential effectiveness of centre-based childcare policies and practices on child diet and physical activity: consolidating evidence from systematic reviews of intervention trials and observational studies. Current Nutrition Reports 2017;6:228–46. [DOI: 10.1007/s13668-017-0212-z] [DOI] [Google Scholar]
Tandon 2016
- Tandon P, Tovar A, Jayasuriya A, Welker E, Schober D, Copeland K, et al. The relationship between physical activity and diet and young children's cognitive development: a systematic review. Preventive Medicine Reports 2016;3:379-90. [DOI: 10.1016/j.pmedr.2016.04.003] [DOI] [PMC free article] [PubMed] [Google Scholar]
Turco 2018
- Turco J, Inal-Veith A, Fuster V. Cardiovascular Health Promotion. Journal of the American College of Cardiology 2018;72:908. [DOI] [PubMed] [Google Scholar]
US Preventive Services Task Force 2017
- US Preventive Services Task Force, Grossman DC, Bibbins-Domingo K, Curry SJ, Barry MJ, Davidson KW. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. JAMA 2017;317(23):2417-26. [DOI: 10.1001/jama.2017.6803] [DOI] [PubMed] [Google Scholar]
Van de Kolk 2019
- Van de Kolk I, Verjans-Jansse S, Gubbels J, Kremers S, Gerards S. Systematic review of interventions in the childcare setting with direct parental involvement: effectiveness on child weight status and energy balance-related behaviours. International Journal of Behavioral Nutrition and Physical Activity 2019;16(110):57-69. [DOI: 10.1186/s12966-019-0874-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Varni 2001
- Varni J, Seid M, Kurtin P. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory Version 4.0 Generic Core Scales in healthy and patient populations. Medical Care 2001;39:800-12. [DOI] [PubMed] [Google Scholar]
Wang 2012
- Wang YC, Orleans CT, Gortmaker SL. Reaching the healthy people goals for reducing childhood obesity: closing the energy gap. American Journal of Preventive Medicine 2012;42(5):437-44. [DOI: 10.1016/j.amepre.2012.01.018] [DOI] [PubMed] [Google Scholar]
Ward 2015
- Ward S, Belanger M, Donovan D, Carrier N. Systematic review of the relationship between childcare educators' practices and preschoolers' physical activity and eating behaviours. Obesity Reviews 2015;16(12):1055-70. [DOI: 10.1111/obr.12315] [DOI] [PubMed] [Google Scholar]
Warden 2003
- Warden D, Cheyne B, Christie D, Fitzpatrick H, Reid K. Assessing children's perceptions of prosocial and antisocial peer behaviour. Educational Psychology 2003;23(5):547-67. [Google Scholar]
Waxman 2003
- Waxman A. Prevention of chronic diseases: WHO global strategy on diet, physical activity and health. Food and Nutrition Bulletin 2003;24:281-4. [DOI] [PubMed] [Google Scholar]
Wechsler 1989
- Wechsler D. WPPSI-R, Manual: Wechsler Preschool and Primary Scale of Intelligence. Revised edition. San Antonio, Texas: Psychological Corporation, 1989. [Google Scholar]
WHO 2012
- World Health Organization. Population based approaches to childhood obesity prevention. Available at who.int/dietphysicalactivity/childhood/WHO_new_childhoodobesity_PREVENTION_27nov_HR_PRINT_OK.pdf (accessed prior to 25 November 2020).
WHO 2021
- World Health Organization. The WHO child growth standards: body mass index-for-age (BMI-for-age). www.who.int/toolkits/child-growth-standards/standards/body-mass-index-for-age-bmi-for-age (accessed prior to 14 January 2021).
Wolfenden 2009
- Wolfenden L, Wiggers J, d'Espaignet E, Bell A. How useful are systematic reviews of child obesity interventions? Obesity Reviews 2009;11(2):159-65. [DOI: 10.1111/j.1467-789X.2009.00637.x] [DOI] [PubMed] [Google Scholar]
Wolfenden 2020
- Wolfenden L, Barnes C, Jones J, Finch M, Wyse R, Kingsland M, et al. Strategies to improve the implementation of healthy eating, physical activity and obesity prevention policies, practices or programmes within childcare services. Cochrane Database of Systematic Reviews 2020, Issue 2. Art. No: CD011779. [DOI: 10.1002/14651858.CD011779.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
World Cancer Research Fund 2018
- World Cancer Research Fund/American Institute for Cancer Research. Diet, nutrition, physical activity and cancer: a global perspective. Available at wcrf.org/dietandcancer (accessed prior to 8 April 2022).
World Health Organization 2021
- World Health Organization. Standards for healthy eating, physical activity, sedentary behaviour and sleep in early childhood education and care settings: a toolkit. Geneva: World Health Organization, 2021. [Google Scholar]
Yoong 2016
- Yoong S, Finch M, Nathan N, Wiggers J, Lecathelinais C, Jones J, et al. A longitudinal study assessing childcare services' adoption of obesity prevention policies and practices. Journal of Paediatrics and Child Health 2016;52(7):765-70. [DOI] [PubMed] [Google Scholar]
Yoong 2020b
- Yoong S, Lum M, Jones J, Kerr E, Falkiner M, Delaney T, et al. A systematic review of interventions to improve the dietary intake, physical activity and weight status of children attending family day care services. Public Health Nutrition 2020;23(12):2211-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yuan 2014
- Zhou YE, Emerson JS, Levine RS, Kihlberg CJ, Hull PC. Childhood obesity prevention interventions in childcare settings: systematic review of randomized and nonrandomized controlled trials. American Journal of Health Promotion 2014;28(4):e92-103. [DOI: 10.4278/ajhp.121129-LIT-579] [DOI] [PubMed] [Google Scholar]
Zhou 2014
- Zhou YE, Emerson JS, Levine RS, Kihlberg CJ, Hull PC. Childhood obesity prevention interventions in childcare settings: systematic review of randomized and nonrandomized controlled trials. American Journal of Health Promotion 2014;28(4):e92-103. [DOI: 10.4278/ajhp.121129-LIT-579] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Yoong 2021
- Yoong SL, Lum M, Jackson J, Wolfenden L, Barnes C, Jones J, et al. Healthy eating interventions delivered in early childhood education and care settings for improving the diet of children aged six years and below. Cochrane Database of Systematic Reviews 2021, Issue 2. Art. No: CD013862. [DOI: 10.1002/14651858.CD013862] [DOI] [Google Scholar]


