Abstract
Although social support is commonly investigated in the context of substance recovery, researchers have widely neglected its multilevel nature, thus limiting what we know about its measurement across levels of observation. The current study used multilevel confirmatory factor analyses (MCFA) on 229 individuals living in 42 recovery homes to investigate the structure of single factor of social support at the individual and house-levels. Multilevel structural equation model (MSEM) was then conducted to examine whether the social support factor was associated with stress at the individual and house-levels. MCFA results showed that within individuals, all social support measures were significant and positive while at the house-level, there were a few discrepancies (e.g., IP was negative). Stress was significantly negatively related to the social support factor at the individual-level, but this association was positive at the house-level. These findings suggest that on an individual-level, a person’s perception and source of social support is particularly important —even if the source of support comes from someone who is not abstinent. On a house-level, social support is more sensitive to outside influences than within individuals. Implications for future research and substance use interventions targeting social support are discussed.
Keywords: substance abuse, recovery, social support, multi-level confirmatory factor analysis
Social support is frequently noted as an important factor in recovery from alcohol and drug use (Beattie & Longabaugh, 1997; Havassy et al., 1991). Indeed, greater social support has predicted lower substance use rates after treatment (Broome et al., 2002; Humphreys & Noke, 1997; Humphreys et al., 1995), treatment retention (Dobkin et al., 2002; Lang & Belenko, 2000), days abstinent (Longabaugh et al., 2010), and abstinence self-efficacy (Stevens et al., 2015). Additionally, past research has suggested that social support is linked to positive health outcomes for individuals in recovery, such as greater quality of life and subjective well-being (Beattie et al., 1993). Higher levels of social support have also been associated with less stress (Hyman et al., 2009). Conversely, individuals in recovery with low social support have been found to have higher severity of drug and alcohol use alongside greater psychological distress six months after entering treatment (Dobkin et al., 2002).
Perceived social support embodies resources obtained from interpersonal relationships and can consist of the provision of information, emotional guidance, and positive appraisal, and tangible resources (Cohen & McKay, 1984). The quality of social support has been found to impact substance use and/or abstinence as well as treatment compliance (Spohra et al., 2019). Conversely, those who feel socially isolated may be at a greater risk of exiting treatment prematurely and relapsing (Muller et al., 2017). Researchers have suggested that social support may buttress recovery outcomes through multiple mechanisms such as social control (e.g., bonding, cohesion, and monitoring), behavioral choice theory (i.e., protective activities within the social context which provide rewards other than substance use), social learning (e.g., observation and imitation of social behavior), and stress and coping (e.g., stressful life circumstances either caused by social relationships or buffered by social relationships and the coping skills individuals possess; Moos, 2007). As recovering individuals develop new relationships, social standards can discourage disruptive behavior such as substance abuse and encourage the utilization of healthy coping skills in its stead.
Researchers have utilized social networks to gain insight into how social support influences recovery. Participating in a social network supportive of recovery is also associated with completing treatment, greater abstinence, and greater quality of life (Muller et al., 2017). Additionally, the size and composition (e.g., having more individuals who are abstinent) of the network is positively correlated with abstinence rates (Best et al., 2008, Best, et al., 2012; Wasserman et al., 2001, Zywiak et al., 2002) and quality of life (Muller et al., 2017; Best, et al., 2012). More support for abstinence in one’s social network has predicted higher abstinence rates (Havassy et al., 1991; Hser, 2007; Stone et al., 2016). Conversely, relapse is predicted by support for substance use (Stone et al., 2016), and social networks where members abuse substances (Best et al., 2008; Hser, 2007).
Many individuals who enter recovery participate in mutual help organizations (MHO) which utilize peer-to-peer support. Twelve-step groups, such as Alcoholics Anonymous (AA), are one example of MHO that serve as a vital resource of social support for many recovering individuals. Participation in AA has been shown to predict positive recovery outcomes, such as higher abstinence rates and higher quality relationships (Humphreys et al., 1997; Kaskutas et al., 2002). Greater 12-step involvement is associated with larger social networks, networks with higher quality friendships, as well as greater general social support over time (Groh et al., 2005). Moreover, Individuals who participate in AA are more motivated to stay involved due to the amount of social support they receive to remain sober (Nealon-Woods et al., 1995). Residents of recovery home who have high AA participation are more likely to have long-term sobriety compared to those with low AA involvement and those in usual aftercare conditions (Groh et al., 2009).
Another type of MHO are recovery homes, such as Oxford Houses (OH), which embed their members in a network of recovery resources that fosters social support and retention in the homes (Brereton et al., 2014). Specifically, OHs are comprehensive, self-governing social environments, which provide residents with a daily social environment (Doogan et al., 2019). A greater presence of other OH members in one’s social network has predicted abstinence (Jason et al., 2012), revealing that these networks are a major protective factor against relapse. Jason et al. (2014) found that OH may be an important source of support and mentorship for recovering individuals to obtain.
Although social support is extensively researched in the context of recovery from substance use disorders, the multilevel nature of the construct remains largely unexplored. Obtaining social support data from multiple levels can help yield rich conceptual information that would otherwise not be possible when data are limited to a single level of analysis. Previous studies using multilevel analyses have found that the measurement structure of social support varies across levels of measurement (Aldrup et al., 2018; Downer et al., 2014). However, these studies were conducted in school settings and examined classroom level effects of social support on student educational outcomes. Such investigation needs to be replicated with individuals in recovery. A study by Jason et al. (2021) demonstrates how examining individuals and their shared social environments can further what we know about recovery processes. The study found that peers highly influence individuals’ recovery, with the house environment having a more substantial impact on residents’ recovery over time rather than their individual level scores on latent recovery measures.
The current study used multilevel confirmatory factor analysis (MCFA) to examine a single factor of social support using data from 229 individuals residing in 42 recovery homes. Five measures of social support were used in the construction of the factor: general support, network size, network quality, satisfaction with social relationships, and AA affiliation. The latent factor was examined at the individual and house-level which allowed us to determine the extent that specific types of social support converged or diverged across levels. Since social support is known to function as a buffer against stress, we then investigated whether the social support factor was negatively associated to stress at the individual and house-level.
Methods
Participants and Procedure
The data were taken from the first wave of data collection from a larger, longitudinal study on social networks in the OH (Jason et al., 2021). The longitudinal study examined how residents’ recovery-related attitudes, behaviors, and social relationships co-evolve, and how individual and house level factors are related to recovery outcomes. OHs are the largest network of democratic, self-run recovery homes in the United States (Jason, Olson et al., 2008).
Two-hundred and twenty-nine participants were recruited from 42 OHs across Oregon, Texas, and North Carolina. These three states were chosen for their geographical diversity and for their well-developed and well-established OH organizations. One field research staff member was assigned to each state. The field member reached out to individual houses and individual participants for study recruitment. The first 13 houses in each state that consented with all or all-but-one household member were recruited to the study. Three more houses were later added to make the total number of participating houses 42. The field staff member conducted and debriefed the nature of the study to all individual house members and house presidents in a one-on-one interview.
The final sample included 229 OHs residents residing in 42 different OHs with a mean of 5.45 members per house. The sample of the current study included 88.8% of the current members residing in the 42 different OHs (actual mean number of members per house was 6.14 and the current sample has a mean of 5.45 members per house). The sample for the current study included 126 (55%) males, 102 (44.5%) females, and 1 (.4%) participant who did not identify as male or female. The average age was 38 years (standard deviation [SD] = 10.82). Most participants 214 (93.4%) identified as non-Hispanic/Latinx and 15 (6.5%) identified as Hispanic/Latinx. Most of the participants 188 (82.1%) identified as White, 21 (9.2%) identified as Black/African American, four (1.7%) as American Indian or Alaskan Native, and one (0.4%) participant identified as Pacific Islander. The average length of stay in their OHs was 10.3 months (SD=12.55). Participants were compensated $20 for participation. Approval from the was obtained from the last author’s Institutional Review Board.
Measures
To examine which social support measurement instruments add unique variance or which ones may be repetitive, Interpersonal Support Evaluation List (ISEL), The Important People Inventory (IP), Alcoholics Anonymous Affiliation Scale (AAAS), The Quality of Life- Social Instrument (QOLS), and Social Network Instrument (SNI) were examined. ISEL inquired from the respondent their perceived levels of social supports. IP asked respondents to list the total number of people they deemed as their important people. AAAS assessed the respondents’ AA involvement, including relational involvement with other AA members. SNI measures the relationships by observing loaning, friendship, frequency of contact, help, and strength of the relationships and was used as a measure of network quality The Perceived Stress Scale—Brief Version was used a measure of psychological stress.
The ISEL (Cohen et al., 1985) is a 12-item multidimensional inventory that measures an individual’s general perceived social support. Responses are rated on a 4-point Likert-type scale ranging from 0 (“definitely false”) to 3 (“definitely true”), with statements describing the presence of social support in diverse situations. The internal reliability for the sample of the ISEL scale was α =.88.
The IP (Groh et al., 2007) is an adapted version of the Important People and Activities Inventory (Clifford & Longabaugh, 1991), used to measure the important members of an individual’s social network. Respondents named up to eight important individuals with whom they frequently contacted in the last six months. The IP was scored by looking at the total number of important individuals the respondent listed. The internal reliability of the IP in the present study was good (Cronbach’s α = 79).
The AAAS (Humphreys et al., 1998) is a 9-item measure assessing AA involvement through questions about AA meeting attendance, reading AA literature, and involvement with other members. All items were coded dichotomously (0 = No, 1 = Yes) except for two items reflecting AA meeting attendance in the past year and in one’s lifetime (coded as 0 for no meetings, 0.25 for 1–30 meetings, 0.5 for 30–90 meetings, 0.75 for 90–500 meetings, and 1 for more than 500 meetings). Item scores were summed to produce the total scale score. The internal reliability for the AAAS in this study was very good (Cronbach's α = .84).
The SNI (Jason & Stevens, 2017) measures six aspects of a social network: loaning, advice seeking, friendship, frequency of contact, help, and strength of friendship. Participants rated all other house residents on each of the six items. The measures are scored on a 5-point Likert score scale (0 = high to 4 = low). All components except loaning were reverse scored such that 0 = low to 4 = high). Advice seeking, friendship, frequency, help, and strength of friendship were reversed coded to obtain a mean score in which higher scores indicated a stronger social network. The SNI used with our sample had a Cronbach’s α of 0.85 and all items contributed positively. A multilevel confirmatory factor analysis of the SNI found an excellent fit and per-item contribution, and neither age nor sex significantly correlated with this instrument (Jason & Stevens, 2017).
The (QOLS) is a 3-item subscale of the World Health Organization Quality of Life Assessment Brief Version (The WHOQOL Group, 1998). It is a measure of satisfaction with social relationships. It is scored using a 5-point Likert scale and measures an individual’s satisfaction with their social relationships. The internal reliability was very good (αs = .89).
The Perceived Stress Scale—Brief Version (PSS; Cohen, Kamarck, & Mermelstein, 1983) is 4-item measure asking participants to rate statements about their feelings of control and stress. Responses were rated on a 5-point Likert-type scale from “never” to “very often”, with items asking how often participants felt stressed and/ or able to control their circumstances. Internal reliability was good (α = .77).
Statistical analyses
A multilevel confirmatory factor analysis (MCFA) was conducted to examine a single latent factor of social support at the individual and house-level using Mplus (Version 7.31, Muthén & Muthén, 2019). Internal validity of the social support latent factor was assessed using the Maximum Likelihood Estimation method (Hu & Bentler, 1998). The following variables were used as indicators: general support (ISEL), AA affiliation (AAAS), important people (IP), quality of life social (QOLS), and in-house social network (SNI). All variables entered in the models were group mean centered. Intraclass correlations (ICCs), or the amount of variability between houses and the degree of clustering within houses, were examined using a random effects model before conducting the MCFA. ICCs range from 0 to 1, with values less than .05 indicating MCFA is not appropriate for the data (Dyer et al., 2005). All measure ICCs indicated appropriate use in a MCFA: ISEL (0.15), QOLS (0.11), AAAS (0.20), IP (0.50), and SNI (0.29). A Multilevel structural equation model (MSEM) was then used to determine whether the social support factor was related to stress at the individual and house-level.
The overall goodness of fit for the models were evaluated using the X2 likelihood ratio statistic, the comparative fit index (CFI), the Tucker-Lewis fit index (TLI), root mean square error of approximation (RMSEA), and the standardized root mean square residual (SRMR). CFI and TLI fit indices are sensitive to model misspecification and are recommended for sample sizes smaller than 250 (Hu & Bentler, 1998). Model was based on recommended cutoff values frequently cited in the literature (i.e., TLI ≥ 0.95; CFI ≥ 0.90; RMSEA < 0.08; SRMR < 0.08) (Cummings & Brown, 2019; Kline, 2000). However, there is considerable disagreement about strictly adhering to cutoffs as there is a paucity of evidence of their use within the context of multilevel models (Dyer et al., 2005). Designating cutoff values for good and acceptable fit is difficult due to factors such as sample size dependency and sensitivity that can vary across models (Hu & Bentler, 1998). Strict adherence to cutoffs should be avoided unless further multilevel model simulations can be conducted as supportive evidence (Dyer et al., 2005). Multiple fit statistics were utilized to evaluate the fit of the model since each statistic has its limitations and there are no standard cutoffs for fit indices for multilevel models (Shen & Ma, 2016).
Results
Preliminary Analyses
Data for 229 OH residents were analyzed. There were no missing data for any of the variables analyzed in this study. Descriptive statistics for all measures are reported in Table 1. Correlations amongst the measures are reported in Table 2. Participants responses on the AAAS ranged from 0.25 and 9.00, with means of 7.00 and 7.09 at the individual-level and house-level, respectively, indicating that AA affiliation was high. On average, participants reported having 3 important people in their network (individual-level M = 3.32; house-level M = 3.17). The ISEL means were close to the scale’s midpoint (individual-level M = 2.41; house-level M = 2.43), indicating that participants perceived having moderate levels of general social support. The SNI means (individual-level M = 2.48; house-level M = 2.47), and QOLS means (individual-level M = 3.76; house-level M = 3.75), were above the scale mid-points indicating that in-house networks were strong and that participants on average were satisfied with their social relationships. The PSS means were at the scale’s midpoint (individual-level M = 2.49; house-level M = 2.52), indicating moderate levels of perceived stress. The intraclass correlations indicated between 11% to 50% variance in participants ratings across all measures can be attributed to differences between houses.
Table 1.
Descriptive statistics for the various inventories at the individual-level and house-level
| Measures | M w | M b | Var w | Var b | ICC |
|---|---|---|---|---|---|
| AAAS | 7.00 | 7.09 | 1.89 | 1.10 | 0.20 |
| IP | 3.32 | 3.17 | 2.02 | 1.61 | 0.50 |
| ISEL | 2.41 | 2.43 | 0.57 | 0.50 | 0.15 |
| QOLS | 3.76 | 3.75 | 0.74 | 0.41 | 0.11 |
| SNI | 2.48 | 2.47 | 0.54 | 0.36 | 0.29 |
| PSS | 2.49 | 2.52 | 0.77 | 0.50 | 0.22 |
Note: AAAS = Alcoholics Anonymous Affiliation Scale; IP = The Important People Inventory; ISEL = Interpersonal Support Evaluation List; QOLS = The Quality of Life- Social Instrument; SNI = Social Network Instrument; PSS = Perceived Stress Scale. Varw and Varb refers to variance within residents and between houses. ICC refers to intraclass correlations.
Table 2.
Correlations among study measures at the individual and house-level
| Measures | ||||||
|---|---|---|---|---|---|---|
| Measures | AAAS | IP | ISEL | QOLS | SNI | PSS |
| WITHIN-LEVELS | ||||||
| AAAS | --- | |||||
| IP | 0.28** | --- | ||||
| ISEL | 0.27** | 0.26** | --- | |||
| QOLS | 0.13* | 0.10* | 0.41*** | --- | ||
| SNI | 0.10* | 0.15* | 0.27** | 0.23** | --- | |
| PSS | −0.23** | −0.11* | −0.29** | −0.41*** | −0.07 | --- |
| BETWEEN-LEVELS | ||||||
| AAAS | --- | |||||
| IP | −0.36*** | --- | ||||
| ISEL | 0.25** | 0.15* | --- | |||
| QOLS | 0.54*** | −0.01 | 0.81*** | --- | ||
| SNI | 0.68*** | −0.37*** | 0.35** | 0.39*** | --- | |
| PSS | 0.15* | −0.49*** | −0.58*** | −0.65*** | 0.16* | --- |
Note:
p < 0.05
p < 0.01
<0.001; AAAS = Alcoholics Anonymous Affiliation Scale; IP = The Important People Inventory; ISEL = Interpersonal Support Evaluation List; QOLS = The Quality of Life- Social Instrument; SNI = Social Network Instrument; PSS = Perceived Stress Scale.
Pearson’s correlations (Table 2) showed statistically significant associations between most study variables at both the individual and house-levels. At the individual-level, PSS and SNI were not significantly correlated. All other measures at individual-level were significantly related, with small to moderate associations. PSS and SNI were significantly positively correlated at the house level (r = 0.16, p < 0.05), and this association was small. This indicated that houses reporting stronger in-house networks also reported higher stress scores. QOLS and IP were not significantly related at the house-level. All other house-level associations ranged from small to large. PSS was very strongly associated with QOLS (r = −0.65, p < 0.001), and therefore were allowed to correlate in the MSEM model. There were also a few differences in the directionality of relationships across levels. At the individual-level, there was a positive relationship between IP and AAAS (r = 0.28, p < 0.01), while at the house-level, this relationship was negative (r = −0.36, p< 0.01). Similarly, there was a positive relationship between IP and SNI (r = 0.15, p<0.05), while at the house-level, this relationship was negative (r = −0.37, p<0.01). Additionally, AAAS was negatively related to stress at the individual-level (r = −0.23, p< 0.01), but positively related at the house-level (r = 0.15, p< 0.05).
Multilevel Confirmatory Factor Analysis Results
MCFA was used to provide support for a single factor model of social support using six social support measures. The single factor model demonstrated good model fit (X2(5, N = 299) = 9.91, p = 0.11; CFI = 0.97; TLI = 0.91; RMSEA = 0.06; SRMR within = 0.04; SRMR between 0.02) (see Table 3). Table 4 displays the standardized factor loadings and residual variances for the two-level model. All level-1 factor loadings were significant (p < 0.001) and positive. At the individual-level, ISEL and QOLS had the strongest factor loadings with standardized loadings of .80 and .57, respectively. AAAS, IP, and SNR had weaker standardized loadings of 0.38, 0.37, and 0.40, respectively.
Table 3.
Summary of fit indices of MCFA and MSEM models
| Measures | X2(df) | CFI | TLI | RMSEA | SRMRw | SRMRb |
|---|---|---|---|---|---|---|
| MCFA | ||||||
| Model 1 | 8.91(5) | 0.97 | 0.91 | 0.06 | 0.04 | 0.02 |
| MSEM | ||||||
| Model 2 | 18.24 (13) | 0.97 | 0.94 | 0.04 | 0.05 | 0.16 |
Note: Model 1 = MCFA of a single factor of social support; Model 2 = MSEM examining the relationship of the social support factor and stress. X2 = chi-square; df = degrees of freedom; CFI = comparative fit index; TLI = Tucker-Lewis index; RMSEA = root mean square error of approximation; SRMR = standardized root mean square residual; w = within individuals; b = between houses.
Table 4.
MCFA standardized social support factor loadings
| Measures | βa | SE b | p |
|---|---|---|---|
| WITHIN-LEVEL | |||
| F1 by | |||
| AAAS | 0.38 | 0.08 | < .001 |
| IP | 0.37 | 0.08 | < .001 |
| ISEL | 0.80 | 0.07 | < .001 |
| QOLS | 0.57 | 0.07 | < .001 |
| SNI | 0.40 | 0.08 | < .001 |
| BETWEEN-LEVEL | |||
| DF1 by | |||
| AAAS | 0.73 | 0.26 | 0.005 |
| IP | −0.49 | 0.20 | 0.016 |
| SNI | 0.86 | 0.27 | 0.002 |
Note:
Standardized estimate
Standard Error; AAAS = Alcoholics Anonymous Affiliation Scale; IP = The Important People Inventory; ISEL = Interpersonal Support Evaluation List; QOLS = The Quality of Life- Social Instrument; SNI = Social Network Instrument.
At the house level, AAAS and SNI had the strongest factor loadings, with standardized loadings of 0.73 and 0.86, respectively. IP had a negative and weaker standardized loading of −0.49. Due to between-level multicollinearity, QOLS and ISEL were not entered into the model at the house-level.
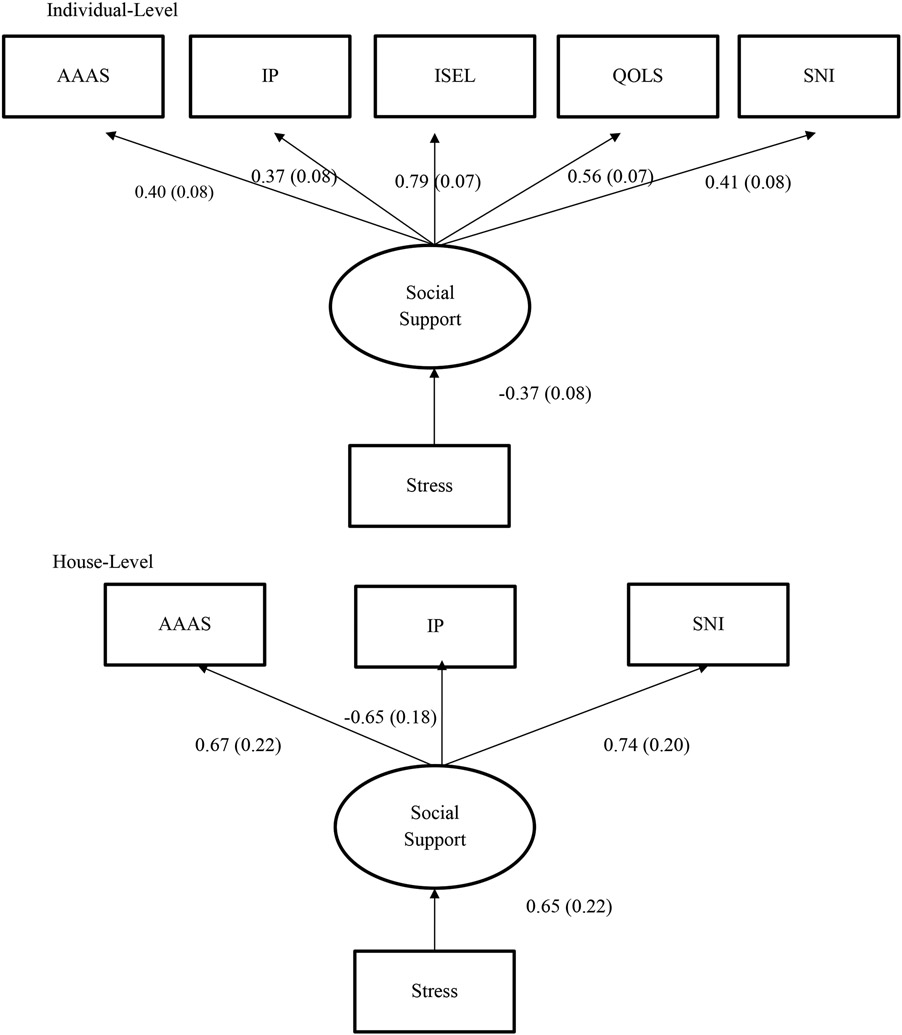
Multilevel Structural Equation Modeling Results
MSEM was used to investigate the associations between the social support factor and stress at the individual and house-level. The MSEM model demonstrated good model fit good model fit (X2(13, N = 299) = 18.24, p = 0.15; CFI = 0.97; TLI = 0.94; RMSEA = 0.04) (Table 3). The SRMR fit indices indicated the fit of the model for Level-1 (within) was better fitting than Level-2 (between) (SRMR within = 0.05; SRMR between 0.16). The results of the MSEM model are displayed in Figure 1, At the individual-level, stress was significantly negatively related to the social support factor (β = −0.37, SE = 0.081, p <0.001). This indicated that individuals higher in perceived stress had lower social support. Conversely, the relationship between social support and stress was significant, but positive (β = 0.65, SE = 0.18, p <0.001).
Figure 1.
Standardized multilevel structural equation model results
Discussion
This study assessed how factors such as the structure of a social network, generalized social support, and the number of important people contributed to one’s overall social support system. Within individuals, we found that all factors significantly and positively contributed to social support. Loadings of ISEL suggest that individual’s perception of social support contributes to their overall social support. Moreover, this is reflected in an individual’s measure of QOLS, which serves as the wellbeing of a person’s social quality of life. Loadings of SNI onto social support suggest that the structure of a network is important. The structure of participants’ social network comprised their ties with individuals within their most immediate social environment, i.e., fellow recovery home residents, and their ratings of those relationships along dimensions such as loaning, advice seeking, and friendship. Moreover, this social network is comprised of other housemates who are also practicing abstinence, creating a source of social support from within the house. Similarly, AA affiliation also contributes to ones’ social support. Like within house social networks, AA groups are comprised of others who are abstaining from alcohol and drugs, creating another source of social support. However, unlike house social networks, AA groups produce a source of recovery-specific social support from outside the house. Nonetheless, persons in recovery do not have to be the only source of social support for individuals in recovery. The IP measure indicated that the more important people have, the greater their social support system was. This is critical as IP is not limited to someone abstaining; it can consist of friends and family members who may not be in recovery.
Between houses, the structure of a house’s social network contributes to the houses’ within-house social support, while AA affiliation contributes to a house’s social support system from outside the house. Interestingly, IP negatively loaded onto the latent social support factor. This may be because an IP does not have to be abstinent or anyone in recovery. This would suggest that the overall social support of a house is more sensitive to outside influences than individuals. Another possibility is that those the respondents indicated in the IP may be people that are not in recovery or are codependents in the relationship. It could be possible that what constitutes an important person, changes throughout an individual’s recovery trajectory, thus negatively influencing the IP score. For example, perhaps early in recovery, an individual, who is also codependent, considers an active user an important individual. At the same time, those further along in their recovery have managed or dissolved unhealthy relationships. And people in the early stages of change, such as pre-contemplation and contemplation, may have many that they indicate as important people, while those that are further along in their recovery replaced their important people with others that are also further along in their recovery, thus the ones in the middle, just starting or in the eve of their recovery journey, have a wide vacillating mix of new and old friends or only have decreased their pool of relationships, thus feeding into a cycle of isolation and fewer distractions from their usual habits of substance use and fewer reminders of coping skills and recovery and the support and comradery that accompanies support groups and recovery homes.
Social Support has been used as a measure for recovery in general and can be exhibited in many forms. Not only has past research noted a positive correlation between social support and recovery, but also a higher QOL (Beattie et al., 1993), subjective well-being, days of abstinence (Longabaugh et al., 2010), less stress (Hyman et al., 2009), treatment retention (Dobkin et al., 2002; Lang & Belenko, 2000, Sphora et al., 2019), and treatment self-efficacy (Stevens et al., 2015). Social support can be reflected in many forms and even more so for those in recovery. Research indicates that social support assists by providing support, discouraging previous habits, rewarding new habits, and emphasizing coping skills (Moos, 2007) other than substance use from adolescents (Hellandsjø et al., 2002; Jones, & Heaven, 1998) and adults (Skaff et al., 1999) alike. Conversely, social isolation and low social support have been indicative of increased psychological stress (Dobkin et al., 2002), more severe substance use, early termination of treatment (Muller et al., 2017), or shorter length of stay at recovery homes (Groh et al., 2007), and relapse (Stone et al., 2016).
Recovery homes and other sober living environments, in theory, assist their members in fostering relationships with others in recovery, and thus, in their recovery from substance use disorder. The current study consisted of a sample of residents from OH. OH is a network of independently run houses that aim to provide members affordable housing in a communal-living environment. There is no maximum length of stay, given that members avoid substance use and disruptive behavior (Jason & Ferrari, 2010). Unlike traditional recovery homes, OH is an environment in which everyone in the house has the same goal as there are no administrators, nurses, or outside individuals. This may assist in positively influencing and fostering stronger bonds and relationships and bring a sense of responsibility to the OH members. Research has indicated members of OH, a self-governed social sobriety environment embedded with resources, and their social networks are predictive of abstinence (Jason et al., 2012). Prior research has revealed that length of stay in OH is related to positive recovery outcomes, including higher abstinence rates and greater social support (Groh et al., 2009; Jason et al., 2012; Majer et al., 2002). Within the literature on OH recovery communities, social support is associated with less substance use and more days abstinent (Stone et al., 2016), and greater levels of social support have predicted fewer drinking behaviors (Groh et al., 2007) and more self-regulation (Ferrari et al., 2010) over time. Living in OH for at least six months has been shown to increase one’s abstinence self-efficacy, the number of sober people in one’s social network, and the likelihood of employment. Furthermore, the formation of just one relationship has been found to reduce the probability of relapse by nearly a factor of five (Jason et al., 2012). These findings highlight the importance of recovery homes for those with substance use disorders, and the ways that social support might be a critical variable facilitating positive changes in residents.
There are hundreds of thousands who leave jail/prison each year, and others who finish substance use rehab programs. One of their greatest needs is for housing, as often it is not easily available. Recovery homes for those who wish to live with other abstinent individuals could be a place for many and currently over 250,000 individuals live in them annually. Better understanding the types of support that is available in these settings is crucial for helping with the housing problems of these high-risk groups.
Additionally, 12-step groups and other support groups such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) are other sources of social support for individuals in recovery. Like Recovery Homes, involvement in AA showed a link to positive recovery outcomes (Humphreys et al., 1997; Kaskutas et al., 2002). OH members that attend support groups such as AA in conjunction with being a part of OH may experience more benefits such as larger social networks, higher quality relationships, and general social support (Groh et al., 2005) and may be more inclined to remain sober due to the amount of social support they receive (Nealon-Woods et al., 1995).
The relationship between social support and stress differed at the individual and house-levels. At the individual-level, stress was negatively related to social support, indicating that participants who reported higher social support also reported less stress. The inverse of this relationship was found at the house-level, with houses reporting higher social support also reporting greater stress levels. This finding suggests that certain social contexts may be better at attenuating stress than others. It is also possible that settings with higher stress would elicit more support from available network. Given the cross-sectional nature of our study, causal inferences cannot be made, but our study can serve as the foundation for future longitudinal investigations.
There were several limitations in the current study. For example, the results are specific to self-run OHs in three states and might not generalize to other sober living homes. In addition, there was no direct measure of friends and family support. Also, this study only assessed one wave of data, and it would be of importance to assess how support might change or mediate change in other variables over time. Other limitations include that there were no direct measure of friends and family support, and a lack of further assessment of each relationship indicated in IP. An individual may define important people differently from other members across houses. Furthermore, perhaps different cultural lenses vary in what is deemed as an important person and what cultures and stigmas surrounding substance use and support for recovery, and further research might investigate different impacts of people based on varying demographics (e.g., female/male/non-binary, minority in-groups, age cohorts, different stage of change, etc.). Another cultural influence may be that there are different types of stigmas in terms of mental health and substance use amongst the respondents’ important persons. Along the same vein, further research could control for what constitutes an “important person” so that the definition is similar across the board. Other research to be further examined is to assess stress alongside relationships and social support.
Many different measures of social support have been used in studies on recovery outcomes, and the literature is unclear as to which instruments best measure this construct within the context of substance abuse and alcohol recovery. Moreover, it is unclear which measures add unique variance or which ones may be duplicative. Additionally, research participation can be burdensome as there is evidence that excessive administration of measures can cause assessment reactivity, which impacts the evaluation of treatment outcomes, treatments, and thereby obscuring responses to treatment (Gastfriend et al., 2005). Thus, our study helps elucidate which measures capture the most variance, which measures are redundant, and which measures capture something unique with the overarching aim of parsimonious research batteries.
Conclusion
In summary, our findings support the notion that social support comprises several conceptually congruent measures, furthering current literature. Our study reinforces the idea that social support can occur in a variety of different ways. It is imperative to understand which tools of measurement and inventories capture the most variance, which measures are redundant, and which measures capture something unique. These inventories would assist in maximizing recovery or at least in understanding the recovery influencing factors upon individuals. It is of importance to find ways to enhance aspects of social support for those in recovery from substance use disorders.
Acknowledgements
The authors appreciate the financial support from the National Institute on Alcohol Abuse and Alcoholism (grant number AA022763). We also acknowledge the assistance from members of the Oxford House organization, and in particular Paul Molloy, Alex Snowden, Casey Longan, and Howard Wilkins. In addition, we appreciate the help of Nathan Doogan on the social network data.
Footnotes
Declaration of Conflict of Interests
No conflict declared.
References
- Alcoholics Anonymous. (2001). Alcoholics anonymous: The big book, (4th ed.). New York, NY: Alcoholics Anonymous World Services. [Google Scholar]
- Aldrup K, Klusmann U, Lüdtke O, Göllner R, & Trautwein U (2018). Social support and classroom management are related to secondary students’ general school adjustment: A multilevel structural equation model using student and teacher ratings. Journal of Educational Psychology, 110(8), 1066. [Google Scholar]
- Beasley CR, & Jason LA (2015). Engagement and disengagement in mutual-help addiction recovery housing: A test of affective events theory. American Journal of Community psychology, 55(3-4), 347–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beattie MC, & Longabaugh R (1997). Interpersonal factors and post-treatment drinking and subjective wellbeing. Addiction, 92(11), 1507–1521. [PubMed] [Google Scholar]
- Beattie MC, Longabaugh R, Elliott G, Stout RL, Fava J, & Noel NE (1993). Effect of the social environment on alcohol involvement and subjective well-being prior to alcoholism treatment. Journal of Studies on Alcohol, 54(3), 283–296. [DOI] [PubMed] [Google Scholar]
- Best D, Gow J, Knox T, Taylor A, Groshkova T, & White W (2012). Mapping the recovery stories of drinkers and drug users in Glasgow: Quality of life and its associations with measures of recovery capital. Drug & Alcohol Review, 31(3), 334–341. [DOI] [PubMed] [Google Scholar]
- Best DW, Ghufran S, Day E, Ray R, & Loaring J (2008). Breaking the habit: A retrospective analysis of desistance factors among formerly problematic heroin users. Drug and Alcohol Review, 27(6), 619–624. [DOI] [PubMed] [Google Scholar]
- Bishop PD, Chertok F, & Jason LA (1997). Measuring sense of community: Beyond local boundaries. Journal of Primary Prevention, 18(2), 193–212. [Google Scholar]
- Brereton KL, Álvarez J, Jason LA, Stevens EB, Dyson VB, Mcneilly C, & Ferrari JR (2014). Reciprocal responsibility and social support among women in substance use recovery. International Journal of Self Help & Self Care, 8(2), 239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broome KM, Simpson DD, & Joe GW (2002). The role of social support following short-term inpatient treatment. The American Journal on Addictions, 11(1), 57–65. [DOI] [PubMed] [Google Scholar]
- Clifford PR, & Longabaugh R (1991). Manual for the administration of the Important People and Activities Instrument. Adapted for use by Project MATCH for NIAAA, 5, R01AA06698-05. [Google Scholar]
- Cohen S, Doyle WJ, Turner R, Alper CM, & Skoner DP (2003). Sociability and susceptibility to the common cold. Psychological science, 14(5), 389–395. [DOI] [PubMed] [Google Scholar]
- Cohen S, & McKay G (1984). Social support, stress and the buffering hypothesis: A theoretical analysis. In Baum A, Taylor SE, & Singer JE (Eds.), Handbook of psychology and health (pp. 253–267). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. [PubMed] [Google Scholar]
- Cohen S, Mermelstein R, Kamarck T, & Hoberman HM (1985). Measuring the functional components of social support. In Social support: Theory, research and applications (pp. 73–94). Springer, Dordrecht. [Google Scholar]
- Cummings C, & Brown M (2019). Psychometric properties of the self-sufficiency matrix among homeless and vulnerably housed individuals and families. Journal of Community Psychology, 47(4), 979–994. [DOI] [PubMed] [Google Scholar]
- Dobkin PL, Civita MD, Paraherakis A, & Gill K (2002). The role of functional social support in treatment retention and outcomes among outpatient adult substance abusers. Addiction, 97(3), 347–356. [DOI] [PubMed] [Google Scholar]
- Doogan NJ, Light JM, Stevens EB, & Jason LA (2019). Quality of life as a predictor of social relationships in Oxford House. Journal of Substance Abuse Treatment, 101, 79–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downer JT, Stuhlman M, Schweig J, Martínez JF, & Ruzek E (2015). Measuring effective teacher-student interactions from a student perspective: A multi-level analysis. The Journal of Early Adolescence, 35(5-6), 722–758. [Google Scholar]
- Dyer NG, Hanges PJ, & Hall RJ (2005). Applying multilevel confirmatory factor analysis techniques to the study of leadership. The Leadership Quarterly, 16(1), 149–167. [Google Scholar]
- Ferrari JR, Stevens EB, & Jason LA (2010). An exploratory analysis of changes in self-regulation and social support among men and women in recovery. Journal of Groups in Addiction & Recovery, 5(2), 145–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gastfriend DR, Donovan D, Lefebvre R, Murray KT. Developing a baseline assessment battery: Balancing patient time burden with essential clinical and research monitoring. Journal on Studies on Alcohol and Drugs 2005;(Supplement No. 15):94–103. [DOI] [PubMed] [Google Scholar]
- Groh DR, Jason LA, Davis MI, Olson BD, & Ferrari JR (2007). Friends, family, and alcohol abuse: An examination of general and alcohol-specific social support. American Journal on Addictions, 16(1), 49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groh DR, Jason LA, Ferrari JR, & Davis MI (2009). Oxford House and Alcoholics Anonymous: The impact of two mutual-help models on abstinence. Journal of Groups in Addiction & Recovery, 4(1-2), 23–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groh D, Jason L, Ferrari J, & Halpert J (2005). The effects of twelve-step participation on social support: A longitudinal investigation within a recovery home sample. International Journal of Self-Help & Self-Care, 4(3). [Google Scholar]
- Groh DR, Olson BD, Jason LA, Davis MI, & Ferrari JR (2007). A factor analysis of the Important People Inventory. Alcohol & Alcoholism, 42(4), 347–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havassy BE, Hall SM, & Wasserman DA (1991). Social support and relapse: Commonalities among alcoholics, opiate users, and cigarette smokers. Addictive Behaviors, 16(5), 235–246. [DOI] [PubMed] [Google Scholar]
- Hellandsjø Bu ET, Watten RG, Foxcroft DR, Ingebrigtsen JE, & Relling G (2002). Teenage alcohol and intoxication debut: the impact of family socialization factors, living area and participation in organized sports. Alcohol and Alcoholism, 37(1), 74–80. [DOI] [PubMed] [Google Scholar]
- Hser YI (2007). Predicting long-term stable recovery from heroin addiction: findings from a 33-year follow-up study. Journal of Addictive Diseases, 26(1), 51–60. [DOI] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1998). Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods, 3(4), 424–453. [Google Scholar]
- Humphreys K, Kaskutas LA, & Weisner C (1998). The Alcoholics Anonymous Affiliation Scale: development, reliability, and norms for diverse treated and untreated populations. Alcoholism: Clinical and Experimental Research, 22(5), 974–978. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Mankowski ES, Moos RH, & Finney JW (1999). Do enhanced friendship networks and active coping mediate the effect of self-help groups on substance abuse?. Annals of Behavioral Medicine, 21(1), 54. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Moos RH, & Cohen C (1997). Social and community resources and long-term recovery from treated and untreated alcoholism. Journal of Studies on Alcohol, 58, 231–238. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Moos RH, & Finney JW (1995). Two pathways out of drinking problems without professional treatment. Addictive Behaviors, 20(4), 427–441. [DOI] [PubMed] [Google Scholar]
- Humphreys K, & Noke JM (1997). The influence of post-treatment mutual help group participation on the friendship networks of substance abuse patients. American Journal of Community Psychology, 25, 1–6. [DOI] [PubMed] [Google Scholar]
- Hyman SM, Hong K-IA, Chaplin TM, Dabre Z, Comegys AD, Kimmerling A, & Sinha R (2009). A stress-coping profile of opioid dependent individuals entering naltrexone treatment: A comparison with healthy controls. Psychology of Addictive Behaviors, 23(4), 613–619. 10.1037/a0017324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA, Guerrero M, Salomon-Amend M, Stevens E, Light JN & Stoolmiller M (2021). Context matters: Home-level but not individual-level recovery social capital predict residents’ relapse. American Journal of Community Psychology, 67(3-4), 392–404. 10.1002/ajcp.12481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA, Light JM, Stevens EB, & Beers K (2014). Dynamic social networks in recovery homes. American Journal of Community Psychology, 53(3-4), 324–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA, & Ferrari JR (2010). Oxford house recovery homes: Characteristics and effectiveness. Psychological Services, 7(2), 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA, Olson BD, & Foli K (2008). Rescued lives: The Oxford House approach to substance abuse. New York: Routledge. [Google Scholar]
- Jason LA, Schober D, & Olson BD (2008). Community involvement among residents of second-order change recovery homes. Australian Community Psychologist (Online), 20(1), 73. [PMC free article] [PubMed] [Google Scholar]
- Jason L, Stevens JRF, Thompson E, & Legler R (2012). Social networks among residents in recovery homes. Advances in Psychology Study, 1(3), 4. [PMC free article] [PubMed] [Google Scholar]
- Jason LA, & Stevens E (2017). The reliability and reciprocity of a social network measure. Alcoholism Treatment Quarterly, 35(4), 317–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones SP, & Heaven PC (1998). Psychosocial correlates of adolescent drug-taking behaviour. Journal of Adolescence, 21(2), 127–134. [DOI] [PubMed] [Google Scholar]
- Kaskutas LA, Bond J, & Humphreys K (2002). Social networks as mediators of the effect of Alcoholics Anonymous. Addiction, 97(7), 891–900. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Fallah-Sohy N, Vilsaint C, Hoffman LA, Jason LA, Stout RL, Cristello JV, & Hoeppner BB (2020). New kid on the block: An investigation of the physical, operational, personnel, and service characteristics of recovery community centers in the United States. Substance Abuse Treatment, 111(2020), 1–10. 10.1016/j.jsat.2019.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Fallah-Sohy N, Cristello J, Stout RL, & Jason LA (2021). Recovery community centers: Characteristics of new attendees and longitudinal investigation of the predictors and effects of participation. Substance Abuse Treatment, 124(2021). 10.1016/j.jsat.2021.108287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline P (2000). Handbook of psychological testing. New York: Routledge. [Google Scholar]
- LaBelle OP, & Edelstein RS (2018). Gratitude, insecure attachment, and positive outcomes among 12-step recovery program participants. Addiction Research & Theory, 26(2), 123–132. [Google Scholar]
- Lang M & Belenko S (2000). Predicting Retention in a Residential Drug Treatment Alternative to Prison Program. Journal of Substance Abuse Treatment. 19. 145–60. 10.1016/S0740-5472(00)00097-0. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Wirtz PW, Zywiak WH, & O'malley SS (2010). Network support as a prognostic indicator of drinking outcomes: The COMBINE study. Journal of Studies on Alcohol and Drugs, 71(6), 837–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majer JM, Droege JR, & Jason LA (2010). A categorical assessment of 12-step involvement in relation to recovery resources. Journal of Groups in Addiction & Recovery, 5(2), 155–167. [Google Scholar]
- Majer JM, Jason LA, Aase DM, Droege JR, & Ferrari JR (2013). Categorical 12-step involvement and continuous abstinence at 2 years. Journal of Substance Abuse Treatment, 44(1), 46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majer JM, Jason LA, Ferrari JR, Venable LB, & Olson BD (2002). Social support and self-efficacy for abstinence: Is peer identification an issue?. Journal of Substance Abuse Treatment, 23(3), 209–215. [DOI] [PubMed] [Google Scholar]
- Majer JM, Jason LA, Ferrari JR, & Miller SA (2011). 12-Step involvement among a U.S. national sample of Oxford house residents. Journal of Substance Abuse Treatment, 41 (1) 37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moitra E, Anderson BJ, & Stein MD (2013). Perceived stress and substance use in methadone-maintained smokers. Drug and Alcohol Dependence, 133(2), 785–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH (2007). Theory-based processes that promote the remission of substance use disorders. Clinical psychology review, 27(5), 537–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney JL, Minor KI, Wells JB, Leukefeld C, Oser CB, & Staton Tindall M (2008). The relationship of stress, impulsivity, and beliefs to drug use severity in a sample of women prison inmates. International Journal of Offender Therapy and Comparative Criminology, 52(6), 686–697. [DOI] [PubMed] [Google Scholar]
- Muller AE, Skurtveit S, & Clausen T (2017). Building abstinent networks is an important resource in improving quality of life. Drug & Alcohol Dependence, 180, 431–438. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 2017. Los Angeles, CA: Author. [Google Scholar]
- Narcotics Anonymous. (2008). Narcotics Anonymous: Basic text, (6th ed.).Van Nuys: World Service Office. [Google Scholar]
- Nealon-Woods MA, Ferrari JR, & Jason LA (1995). Twelve-step program use among Oxford House residents: spirituality or social support in sobriety?. Journal of Substance Abuse, 7(3), 311–318. [DOI] [PubMed] [Google Scholar]
- Shen S & Ma WJ (2016). A detailed comparison of optimality and simplicity in perceptual decision making. Psychological Review, 123(4), 452–480. 10.1037/rev0000028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skaff MM, Finney JW, & Moos RH (1999). Gender differences in problem drinking and depression: Different “vulnerabilities?”. American Journal of Community Psychology, 27(1), 25–54. [DOI] [PubMed] [Google Scholar]
- Spohra S & Livingston MD, Taxman FS, Walters ST (2019). What’s the influence of social interactions on substance use and treatment initiation? A prospective analysis among substance-using probationers. Addictive Behaviors, 89, 143–150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens E, Jason LA, Ram D, & Light J (2015). Investigating social support and network relationships in substance use disorder recovery. Substance Abuse, 36(4), 396–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone A, Jason LA, Light JM, & Stevens EB (2016). The role of ego networks in studies of substance use disorder recovery. Alcoholism Treatment Quarterly, 34(3), 315–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracy EM, Laudet AB, Min MO, Kim H, Brown S, Jun MK, & Singer L (2012). Prospective patterns and correlates of quality of life among women in substance abuse treatment. Drug and Alcohol Dependence, 124(3), 242–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman DA, Stewart AL, & Delucchi KL (2001). Social support and abstinence from opiates and cocaine during opioid maintenance treatment. Drug and Alcohol Dependence, 65(1), 65–75. [DOI] [PubMed] [Google Scholar]
- The World Health Organization Quality of Life Assessment (WHOQOL): development and general psychometric properties. Social Science and Medicine. 1998. Jun; 46(12):1569–85. doi: 10.1016/s0277-9536(98)00009-4. [DOI] [PubMed] [Google Scholar]
- Zywiak WH, Longabaugh R, & Wirtz PW (2002). Decomposing the relationships between pretreatment social network characteristics and alcohol treatment outcome. Journal of Studies on Alcohol, 63(1), 114–121. [PubMed] [Google Scholar]