Abstract
Objective
Rates of migration have increased substantially in recent years and so has the number of left-behind children (LBC). We investigated the impact of parental migration on nutritional disorders of LBC in Bangladesh.
Design
We analysed data from the nationally representative cross-sectional Multiple Indicator Cluster Survey 2012–2013. Child stunting, wasting and underweight were used as measures of nutritional disorders. Descriptive statistics were used to describe characteristics of the respondents and to compare nutritional outcomes based on status of parental migration. Multivariate logistic regression models were used to examine the associations between parental migration and child nutritional disorders.
Setting
Bangladesh.
Participants
Data of 23 402 children (aged <5 years), their parents and households.
Results
In the unadjusted models, parental migration was found significantly protective for stunting, wasting and underweight – both separately and jointly. After potential confounders were controlled for, no difference was found between LBC and non-LBC in any of these three nutritional outcome measures. Household wealth status and maternal educational status were found to significantly influence the nutritional development of the children.
Conclusions
At the population level there is no negative impact of parental migration on stunting, wasting and underweight of LBC in Bangladesh. Remittance from parental migration might enhance affordability of better foods, health care and supplies for a cleaner environment. This affordability is crucial for the poorest section of the society.
Keywords: Parental migration, Left-behind children, Child nutritional disorder, Bangladesh
Migration is often considered an important way of improving livelihood conditions( 1 ). Usually migration occurs from one country to another or from rural to urban areas within a country, often on a temporary basis. In most cases children of these migrants do not move with their parents due to financial constraints and/or the transient nature of the work at the destination. These children who are left-behind (termed LBC hereafter) are usually taken care of by members of the extended family such as grandparents, uncles and aunts. On the one hand, earnings through migration can ease budget constraints of the left-behind household and thereby may increase household spending on children’s nutrition and education. On the other hand, parental migration inherently can lead to parental absence from the home and prolonged separation of children from one or both parents( 2 – 4 ). This separation and parental absence might be harmful for the children’s physical and mental health, having a negative impact on their development.
Bangladesh is one of the major labour-exporting countries in the world. Labour migration – both internal and international – has been an integral part of the economic development of Bangladesh. Much of the credit behind Bangladesh’s progress to a developing nation goes to migrant workers. Against this backdrop, migration in Bangladesh is always assessed from the standpoint of its positive impact on the economy through the remittances sent to improve the family life of the dependants left behind( 5 , 6 ). One estimate shows that about 14 to 40 % of rural households in Bangladesh have at least one migrated person and most of them have LBC( 7 ).
Research around health and well-being of LBC is scarce and concentrated in a few countries. Moreover, the findings are inconsistent. For instance, three studies conducted in China found negative impacts of parental migration on LBC’s health and nutritional development( 8 – 10 ), while another study found no significant impact( 11 ). Similarly, Mansuri found a significant positive effect of migration on LBC’s height-for-age in Pakistan( 12 ), while Nobles found that migration to other countries has negative effect on LBC’s height-for-age in Mexico( 13 ). These variations are likely to result from a range of factors including broader sociocultural elements such as ethnicity, sociocultural diversity, local v. international migration, food culture and the relatives with whom the children are left behind( 14 , 15 ). Also, the pattern of parental migration (e.g. father only, mother only, or both) may have an impact on study findings( 16 ). Compared with other Asian countries such as the Philippines and China( 11 , 17 ), migrants from Bangladesh are mostly men workers( 18 ).
Although Bangladesh is one of the countries with highest child malnutrition rate in the world( 19 ) and a leading country of high-level migration, almost nothing is known about the impact of migration on LBC’s nutritional development. Recently the International Organization for Migration assessed the social cost of migration on LBC and found mixed results( 20 ). For instance, children of migrants were in a better situation than children of non-migrants in terms of having three or more meals per day and improved access to more expensive health-care facilities. However, there seemed to be a negative effect on the psychological development of LBC and parental absence contributed to a sense of insecurity for them. Siddiqui( 21 ) reported that in some instances, migration afforded children better educational opportunities, and in others, children’s education suffered because of the absence of their mothers. Also, the uncertainty of the timing and magnitude of remittances can force LBC from poor labouring households to participate in the labour market under adverse conditions.
Recent data from Bangladesh suggest that about one-third of children <5 years of age are underweight, 42 % are stunted and about 10 % are wasted. Almost 9 % of children are severely underweight and 16 % are severely stunted, and about 1·6 % children in that age group are overweight( 18 ). The Bangladesh Demographic and Health Survey 2014 found similar results and noted that the prevalence of stunting and underweight is lowest among children aged 0–6 months and highest at the age of 18–23 months (stunted 48 % and underweight 37 %)( 19 ). There is a great deal of geographical variation in the prevalence of nutritional disorders across districts and divisions (Fig. 1). A recent national-level estimate found child malnutrition is prevalent in locations( 19 ) from where substantial national and international migration takes place( 22 ). Therefore, it would be interesting to see if LBC’s nutritional status is related to migration of their parent(s). The aim of the present study was to assess the impact of parental migration on nutritional disorders among LBC in Bangladesh.
Fig. 1.
(colour online) Prevalence of stunting among children <5 years of age in different districts in Bangladesh, 2012–2013
Data and methods
Data
We extracted nationally representative data from the Multiple Indicator Cluster Survey (MICS) conducted by UNICEF in 2012–2013. The survey protocol was reviewed and approved by the National Research Ethics Committee in Bangladesh. The detailed sampling design and other related issues of MICS data are available elsewhere( 18 ). Briefly, districts (n 64) were identified as the main sampling strata and the sample was selected in two stages. Within each district, a specified number of census enumeration areas was selected systematically with probability proportional to size. After a household listing was carried out within the selected enumeration areas, a systematic sample of twenty households was drawn in each sample enumeration area. Using this approach, a total of 55 120 households were selected, of which 52 771 households were occupied. Data were collected for 23 402 children aged <5 years.
Exposure variables
The analysis was carried out for three exposure variables: paternal migration (yes v. no), maternal migration (yes v. no) and migration of both parents (yes v. no). Parental information on each selected child was collected by asking the question, ‘Where does his/her natural father and mother live?’ Responses were recorded as one of the following options: (i) in another household in the country; (ii) abroad; (iii) in an institution; and (iv) at home. We then classified these responses as an occurrence of parental migration if a child’s parent(s) lived in another household of the country, abroad or in an institution.
Outcome variables
Child nutritional disorders, namely stunting, wasting and underweight, were the outcome variables. Children whose height-for-age was more than 2 sd below the median height-for-age of the reference population were considered short for their age and classified as stunted. Similarly, children whose weight-for-height and weight-for-age were more than 2 sd below the median weight-for-height and weight-for-age of the reference population were considered wasted and underweight, respectively( 23 ). Two other outcome variables were developed: (i) children with any of the three nutritional disorders (yes v. no); and (ii) children with all three nutritional disorders (yes v. no). Height and weight were measured using a weighing board and scale, respectively.
Covariate adjustment
Covariates that were found important in the literature for child nutrition were included in the present study( 24 – 26 ). The covariates were: migration destination (abroad or within the country); educational attainment (no formal education, primary, secondary, higher); region of residence (seven divisions); place of residence (rural, urban); child’s sex (male, female); and wealth status of child’s household. The data custodians (MICS) constructed a wealth index for each household using the statistical method of principal component analysis. A wealth score was assigned using information on the ownership of consumer goods (e.g. radio, television, refrigerator, landline telephone, watch, mobile phone, bicycle, motorcycle, boat with motor, car), dwelling characteristics (e.g. housing, fuel type for cooking, electricity), water and sanitation, and other characteristics that are related to household wealth (e.g. bank account, ownership of buffalo, cattle, horse, donkey, goat, sheep, chicken, pig)( 18 ). The survey population was then ranked according to the wealth score of the household they were living in and finally divided into five equal parts (quintiles): poorest, poorer, middle, richer and richest. We also adjusted for common illnesses such as diarrhoea and cold/cough, as these may have an impact on the outcome measures and can potentially skew the relationship with parental migration. A categorical variable named ‘illness’ was created, distinguishing those who did and those who did not have any of these two illnesses during the two weeks preceding the survey.
Statistical analysis
Descriptive statistics (n, mean, se, etc.) were used to describe the main features of the participants. We also estimated the prevalence and 95 % CI of each exposure and outcome variable. Prevalence of the three nutritional disorders was calculated separately for all children, and for malnourished children who lived with and without parents. We performed multivariate logistic regression analysis. The initial models included only one specific outcome and exposure variable, and the final models were adjusted for all potential confounding factors. The statistical software package Stata version 15 was used for all statistical analyses.
Results
The mean age of mothers and children was 29·7 and 2·0 years, respectively. Table 1 summarizes some basic information about children and exposure and outcome variables. Paternal migration was reported for almost 7 % and maternal migration for 0·2 % of children. Overall, 62 % of migrated parents went abroad and the rest (38 %) migrated within Bangladesh. The rates of stunting, wasting and underweight over the survey years were 42·2, 9·9 and 32·4 %, respectively. There was a higher proportion of male children (51·3 %) than female children (48·7 %). A little less than half (46·3 %) of the mothers completed either secondary or higher levels of education. As per the wealth index, more than half of the children were living in households of the lowest two quintiles.
Table 1.
Descriptive characteristics and exposure and outcome variables among Bangladeshi children (n 23 402) aged <5 years, Multiple Indicator Cluster Survey 2012–2013
| Characteristic | % | 95 % CI |
|---|---|---|
| Child’s age (months) | ||
| 0–11 | 18·7 | 18·1, 19·2 |
| 12–23 | 19·3 | 18·7, 19·8 |
| 24–35 | 20·0 | 19·4, 20·5 |
| 36–47 | 21·0 | 20·5, 21·6 |
| 48–59 | 21·1 | 20·6, 21·6 |
| Child’s sex | ||
| Male | 51·3 | 50·6, 51·9 |
| Female | 48·7 | 48·1, 49·4 |
| Migration | ||
| None of the parents migrated | 91·9 | 90·9, 92·1 |
| Only father migrated | 6·9 | 6·6, 7·3 |
| Only mother migrated | 0·2 | 0·1, 0·2 |
| Both parents migrated | 1·0 | 0·1, 1·1 |
| Child’s nutritional status | ||
| Stunting | 42·2 | 41·5, 42·9 |
| Wasting | 9·9 | 9·5, 10·3 |
| Underweight | 32·4 | 31·8, 33·1 |
| Any of the three nutritional disorders | 49·5 | 48·8, 50·2 |
| All three nutritional disorders | 4·7 | 4·4, 5·0 |
n, number of observations.
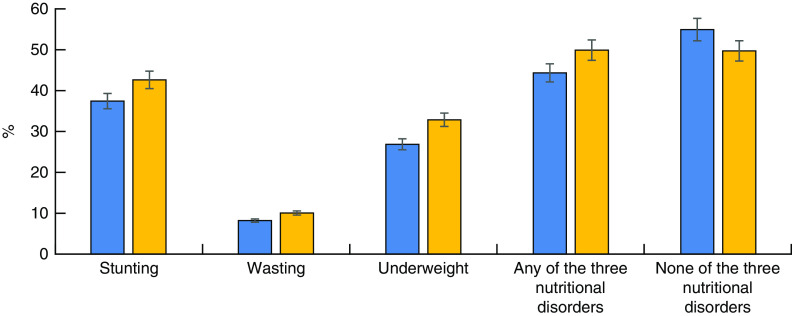
The rate of any of the three nutritional disorders was lower among LBC than the children who lived with both parents (χ 2=18·1; P<0·01). The mean of stunting (height-for-age Z-score), wasting (weight-for-height Z-score) and underweight (weight-for-age Z-score) for the malnourished children were −3·0, −2·6 and −2·8 respectively. These scores for LBC were −2·9, −2·6 and −2·7, respectively. The rates of child nutritional disorders by parental migration status are presented in Fig. 2.
Fig. 2.
(colour online) Estimates of child nutritional disorders (vertical bars represent percentages and error bars represent 5% errors in both directions) by parent’s migration status ( , child left behind by at least one of the parents;
, child left behind by at least one of the parents;  , child not left behind) among Bangladeshi children (n 23 402) aged <5 years, Multiple Indicator Cluster Survey 2012–2013
, child not left behind) among Bangladeshi children (n 23 402) aged <5 years, Multiple Indicator Cluster Survey 2012–2013
The children whose mothers completed secondary or higher education or who were from households of the richer wealth quintile were least likely to be underweight and stunted compared with the children of mothers with little or no education or children from the poor wealth quintile, respectively. The age pattern showed that a higher percentage of children aged 24–47 months were stunted or underweight in comparison to children who were younger or older. Children’s sex, rural/urban location or illnesses (i.e. diarrhoea or cold/cough) in the two weeks preceding the survey had no significant association with the outcome variables.
The results of the unadjusted and adjusted analyses for each of the nutritional outcomes are presented in Tables 2 and 3. In the unadjusted models, father only migration (compared with migration by none of the parents) was found to be significantly protective for all five outcomes: stunting, wasting, underweight, any of the three nutritional disorders and all three nutritional disorders. None of these five outcome variables showed any significant association with the other two exposure variables, namely maternal migration and both parents’ migration. In the adjusted models, none of the univariate associations were found to be statistically significant (Table 2).
Table 2.
Results of multivariate logistic regression analyses assessing the associations between parental migration and the risk of adverse nutritional outcomes among Bangladeshi children (n 23 402) aged <5 years, Multiple Indicator Cluster Survey 2012–2013
| Nutritional status | Unadjusted OR | 95 % CI | Adjusted OR | 95 % CI |
|---|---|---|---|---|
| Stunting | ||||
| None of the parents migrated (ref.) | 1·00 | – | 1·00 | – |
| Only father migrated | 0·74 | 0·66, 0·84 | 1·61 | 0·93, 1·46 |
| Only mother migrated | 1·18 | 0·58, 2·42 | 0·93 | 0·45, 1·94 |
| Both parents migrated | 1·21 | 0·92, 1·60 | 0·90 | 0·68, 1·20 |
| Wasting | ||||
| None of the parents migrated (ref.) | 1·00 | – | 1·00 | – |
| Only father migrated | 0·83 | 0·67, 1·00 | 0·93 | 0·65, 1·34 |
| Only mother migrated | 0·30 | 0·04, 2·19 | 0·31 | 0·04, 2·27 |
| Both parents migrated | 0·75 | 0·45, 1·26 | 0·81 | 0·48, 1·35 |
| Underweight | ||||
| None of the parents migrated (ref.) | 1·00 | – | 1·00 | – |
| Only father migrated | 0·71 | 0·62, 0·80 | 1·00 | 0·80, 1·26 |
| Only mother migrated | 0·74 | 0·33, 1·68 | 0·62 | 0·27, 1·40 |
| Both parents migrated | 1·01 | 0·75, 1·35 | 0·77 | 0·57, 1·03 |
| Any of the three nutritional disorders | ||||
| None of the parents migrated (ref.) | 1·00 | – | 1·00 | – |
| Only father migrated | 0·74 | 0·66, 0·83 | 1·08 | 0·87, 1·33 |
| Only mother migrated | 0·94 | 0·47, 1·91 | 0·77 | 0·38, 1·58 |
| Both parents migrated | 1·21 | 0·92, 1·58 | 0·95 | 0·72, 1·25 |
| All three nutritional disorders | ||||
| None of the parents migrated (ref.) | 1·00 | – | 1·00 | – |
| Only father migrated | 0·73 | 0·54, 0·99 | 1·08 | 0·66, 1·77 |
| Only mother migrated | 0·69 | 0·09, 5·05 | 0·66 | 0·09, 4·93 |
| Both parents migrated | 0·41 | 0·15, 1·10 | 0·38 | 0·14, 1·04 |
n, number of observations; ref., reference group.
Significant associations are shown in bold font.
Table 3.
Adjusted odds ratio (95 % CI) of the associations between study outcomes and major demographic variables among Bangladeshi children (n 23 402) aged <5 years, Multiple Indicator Cluster Survey 2012–2013
| Stunting (n 19 130) | Wasting (n 19 327) | Underweight (n 19 654) | Any of the three nutritional disorders (n 19 841) | All three nutritional disorders (n 19 032) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95 % CI | OR | 95 % CI | OR | 95 % CI | OR | 95 % CI | OR | 95 % CI | |
| Child’s age | ||||||||||
| 0–1 year (ref.) | 1·00 | – | 1·00 | – | 1·00 | – | 1·00 | – | 1·00 | – |
| 1–2 years | 2·33 | 2·11, 2·58 | 1·37 | 1·18, 1·58 | 1·65 | 1·49, 1·84 | 1·87 | 1·70, 2·05 | 2·97 | 2·33, 3·79 |
| 2–3 years | 3·27 | 2·96, 3·62 | 0·95 | 0·82, 1·11 | 2·11 | 1·90, 2·34 | 2·40 | 2·18, 2·63 | 2·17 | 1·68, 2·80 |
| 3–4 years | 3·02 | 2·73, 3·34 | 0·77 | 0·66, 0·90 | 2·01 | 1·81, 2·23 | 2·19 | 2·00, 2·40 | 1·62 | 1·24, 2·11 |
| 4–5 years | 2·21 | 2·00, 2·45 | 0·96 | 0·82, 1·12 | 1·96 | 1·77, 2·18 | 1·79 | 1·63, 1·97 | 1·66 | 1·27, 2·15 |
| Maternal education | ||||||||||
| No formal education (ref.) | 1·00 | – | 1·00 | – | 1·00 | – | 1·00 | – | 1·00 | – |
| Primary incomplete | 1·03 | 0·94, 1·14 | 0·95 | 0·81, 1·10 | 0·98 | 0·89, 1·08 | 1·03 | 0·94, 1·13 | 1·01 | 0·83, 1·24 |
| Primary complete | 0·99 | 0·90, 1·09 | 0·91 | 0·78, 1·06 | 0·92 | 0·83, 1·02 | 1·01 | 0·93, 1·12 | 0·81 | 0·65, 1·00 |
| Secondary incomplete | 0·73 | 0·67, 0·80 | 0·97 | 0·85, 1·11 | 0·76 | 0·70, 0·83 | 0·78 | 0·72, 0·85 | 0·87 | 0·72, 1·05 |
| Secondary complete or higher | 0·49 | 0·42, 0·56 | 0·82 | 0·66, 1·03 | 0·59 | 0·51, 0·67 | 0·55 | 0·48, 0·62 | 0·60 | 0·42, 0·85 |
| Child’s sex | ||||||||||
| Male (ref.) | 1·00 | – | 1·00 | – | 1·00 | – | 1·00 | – | 1·00 | – |
| Female | 0·97 | 0·91, 1·03 | 0·78 | 0·71, 0·86 | 0·98 | 0·92, 1·04 | 0·95 | 0·90, 1·00 | 0·72 | 0·63, 0·83 |
| Wealth quintile | ||||||||||
| Poorest (ref.) | 1·00 | – | 1·00 | – | 1·00 | – | 1·00 | – | 1·00 | – |
| Poorer | 0·88 | 0·81, 0·96 | 0·93 | 0·82, 1·06 | 0·92 | 0·85, 1·00 | 0·89 | 0·82, 0·97 | 0·91 | 0·76, 1·09 |
| Middle | 0·74 | 0·67, 0·81 | 0·83 | 0·72, 0·96 | 0·79 | 0·72, 0·87 | 0·75 | 0·68, 0·82 | 0·75 | 0·61, 0·92 |
| Richer | 0·65 | 0·58, 0·72 | 0·74 | 0·62, 0·87 | 0·64 | 0·58, 0·72 | 0·63 | 0·57, 0·69 | 0·66 | 0·52, 0·84 |
| Richest | 0·46 | 0·40, 0·52 | 0·53 | 0·43, 0·65 | 0·41 | 0·36, 0·47 | 0·45 | 0·40, 0·51 | 0·36 | 0·26, 0·51 |
| Place of residence | ||||||||||
| Rural (ref.) | 1·00 | – | 1·00 | – | 1·00 | – | 1·00 | – | 1·00 | – |
| Urban | 0·96 | 0·88, 1·05 | 1·06 | 0·92, 1·23 | 0·99 | 0·90, 1·09 | 0·97 | 0·89, 1·06 | 0·94 | 0·75, 1·16 |
| Region of residence | ||||||||||
| Barisal (ref.) | 1·00 | – | 1·00 | – | 1·00 | – | 1·00 | – | 1·00 | – |
| Chittagong | 1·21 | 1·07, 1·36 | 0·94 | 0·78, 1·13 | 1·02 | 0·90, 1·15 | 1·21 | 1·08, 1·36 | 0·94 | 0·72, 1·22 |
| Dhaka | 1·12 | 1·00, 1·26 | 0·81 | 0·68, 0·97 | 0·92 | 0·81, 1·03 | 1·11 | 1·00, 1·24 | 0·81 | 0·62, 1·05 |
| Khulna | 0·79 | 069, 0·89 | 0·87 | 0·71, 1·06 | 0·77 | 0·67, 0·88 | 0·84 | 0·74, 0·95 | 0·70 | 0·52, 0·94 |
| Rajshahi | 0·97 | 0·85, 1·12 | 0·80 | 0·64, 0·99 | 0·86 | 0·74, 0·99 | 0·98 | 0·86, 1·12 | 0·80 | 0·59, 1·09 |
| Rangpur | 1·08 | 0·95, 1·23 | 0·77 | 0·63, 0·94 | 0·88 | 0·77, 1·00 | 1·04 | 0·92, 1·18 | 0·88 | 0·67, 1·17 |
| Sylhet | 1·54 | 1·34, 1·78 | 1·25 | 1·02, 1·54 | 1·30 | 1·13, 1·49 | 1·46 | 1·28, 1·67 | 1·41 | 1·06, 1·88 |
| Migration* | ||||||||||
| Within country (ref.) | 1·00 | – | 1·00 | – | 1·00 | – | 1·00 | – | 1·00 | – |
| Abroad | 0·80 | 0·61, 1·04 | 1·02 | 0·66, 1·58 | 0·92 | 0·70, 1·21 | 0·87 | 0·68, 1·12 | 0·85 | 0·45, 1·59 |
| Illness in the two weeks preceding data collection | ||||||||||
| No (ref.) | 1·00 | – | 1·00 | – | 1·00 | – | 1·00 | – | 1·00 | – |
| Yes | 1·01 | 0·94, 1·08 | 1·04 | 0·93, 1·15 | 1·03 | 0·96, 1·10 | 1·00 | 0·93, 1·06 | 1·11 | 0·96, 1·28 |
n, number of observations; ref., reference group.
Not migrated group was omitted due to collinearity.
Discussion
In Bangladesh, previous studies around migration have mainly investigated the linkage of remittances with livelihoods and economic development but the health and well-being of children, particularly LBC, has attracted little attention. The current study was conducted to identify the impact of parental migration (father, mother, or both) on nutritional disorders of LBC. Study findings suggest that, in Bangladesh, LBC of migrant parent(s) are better off in terms of nutritional development than children who live with their parents. However, when other related factors such as wealth status of children’s households and maternal educational status are accounted for, the nutritional advantage of parental migration on the LBC over non-LBC disappears.
The UNICEF conceptual framework identifies three layers of causal factors in child undernutrition: immediate, underlying and basic causes( 27 ). As per this framework, food, health care, stimulation and emotional support are necessary elements for healthy survival, growth and development of children. Remittances from parental migration to families left behind help to increase purchasing power for foods, better health care and supplies for a cleaner environment (soap, clean water, etc.), which may result in improvements in child nutritional development. This purchasing power is crucial for relatively poor households. Although this data set did not have specific information about remittances, previous studies reported high levels of remittance sent back by the migrants( 28 ). On the other hand, a negative aspect of migration is family dissolution, which may have adverse effects on the psychosocial development of LBC( 29 , 30 ). This adverse effect may vary based on factors such as which parent migrates and who are left behind( 16 ). Our findings indicate that the negative impact of lack of direct care caused by parental migration might be offset by the remittances sent back home. Remittances may particularly be crucial for the poor households that struggle ensuring even three meals a day. De Bruyn and Kuddus( 31 ) compiled remittance use data of twenty-one individual studies in Bangladesh and found that a considerable proportion of remittances was used on food and clothing, and it was the highest of all categories of spending.
Although much of the remittances accrued from parental migration is used for food and clothing of the children and other family members( 20 , 31 ), the nutritional status of LBC is likely to be influenced by a complex interplay of underlying social determinants of health that extend beyond the effects of absence or presence of parent(s). To get to the bottom of the problem a wide range of factors needs to be considered. For instance, access to safe drinking-water, food preparation and serving dynamics and sanitation at household level, and prevalence of soil-transmitted helminth infection in rural Bangladesh( 32 ) can all have substantial impacts on nutritional development of LBC. Further studies are needed to unpack the factors that have immediate and long-term impacts on the nutritional development of LBC. Research is also needed to assess how factors such as the duration and frequency of an often-cyclical pattern of migration affect nutritional development and health outcomes of LBC.
As mentioned earlier, internationally the results of parental migration on LBC’s nutritional development are diverse( 8 , 12 , 13 , 33 – 36 ). Some authors such as Mansuri found a positive impact of migration on nutritional development of children( 12 ), and some such as Mo et al. found a negative impact( 36 ). Nguyen found that the effect of parental migration varies across countries and types of migration. For instance, in Ethiopia, parental migration did not have a significant effect on children. However, parental migration was found to have a significant impact on health outcomes of children in India, Peru and Vietnam( 29 ). Our findings of a null effect of migration, after adjustment for confounders, offer another set of evidence. This huge variability of findings in the international literature is possibly due to a long list of factors that include, but are not limited to, variation in study design, study settings, complexity of capturing socio-economic factors affecting nutrition and migration, and basic public health measures. This observation suggests the necessity of rigorous research specific to locations of interest.
Our findings suggest mother’s educational status and household’s wealth condition are significant determinants for nutritional development of children. This observation is consistent with that in the literature( 37 , 38 ). In most developing countries usually the fathers migrate, leaving the mothers behind to take care of their children. Financial solvency from remittances could bring better nutritional benefits if mothers are educated. On the other hand, the explanation for protective effects in wealthy households is likely to be the purchasing power and affordability of foods and health care.
The findings of the present study have some policy implications. First, in a labour-surplus country like Bangladesh, migration for work is a driving force for its socio-economic development. Policy makers should pay attention as to how to maximize the benefits of this migration. This needs multifaceted endeavours from all fronts. From the policy perspective, prioritizing formal education for women is perhaps the most important and achievable way forward. Second, the current study examined only the nutritional development of LBC. Psychosocial well-being is another important aspect that needs attention. Further studies with longitudinal data are recommended to have a comprehensive picture of parental migration on LBC’s overall health and well-being. Third, to ensure better dissemination of relevant information about migrant-specific services and to keep track of LBC, the government should take necessary measures to effectively utilize the Migrant Resource Centres that are available in some parts of the country.
To our knowledge, the current study is the first in Bangladesh that used data from a unique representative survey and examined potential impacts of parental migration on child nutritional disorders. A relatively large sample size helped us to assess the actual effect and therefore draw useful conclusions. The study also has several limitations. First, as it is a cross-sectional study, the relationship between parent(s) migration status and child nutritional disorders is correlational only. Second, all sociodemographic data about parents and children needed to be collected from the parent left behind, or the extended relatives if both parents migrated. This may result in reporting bias. However, any such bias is likely to be random. Also, only a small percentage of mothers migrated, which caused the OR for the outcomes related to mother-only migration to be imprecise. Moreover, there may be a selection effect involved, as the families deciding to migrate and leave their children behind with other caregivers may be fundamentally different from families in which parents decide to stay at home.
Conclusions
At the population level, there is no negative impact of parental migration on stunting, wasting and underweight of LBC in Bangladesh. Rather, household economic condition and maternal educational status are significant factors determining the nutritional development of children <5 years of age. As remittance is known to offer better economic condition, parental migration could be helpful for children’s nutritional development, particularly for those who live in extremely poor households. Further studies with longitudinal data are needed in Bangladesh to further assess the impact of various aspects of migration on LBC’s overall health and well-being.
Acknowledgements
Acknowledgements: Data used in this study were collected from the UNICEF MICS Archive. The authors would like to thank UNICEF for granting permission to use the data. Financial support: This research received no specific grant from any funding agency in the public commercial or not-for-profit sectors. Conflict of interest: None to declare. Authorship: M.M.I. and M.N.K. conceived the study and conducted the analyses. All three authors critically reviewed all versions of the manuscript. Ethics of human subject participation: The survey was approved by the National Research Ethics Committee, Bangladesh. Informed consent was obtained from the parents, guardians and relatives of the children.
References
- 1. Bangladesh Bureau of Statistics (2015) International Migration from Bangladesh: Socio-Economic and Regional Characteristics. Dhaka: BBS, Statistics and Informatics Division, Ministry of Planning. [Google Scholar]
- 2. Gao Y, Li LP, Kim JH et al. (2010) The impact of parental migration on health status and health behaviours among left behind adolescent school children in China. BMC Public Health 10, 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Botezat A & Pfeiffer F (2014) The Impact of Parents Migration on the Well-Being of Children Left Behind – Initial Evidence from Romania. IZA Discussion Paper no. 8225. Bonn: Institute for the Study of Labor; [Google Scholar]
- 4. Zhao C, Wang F, Li L et al. (2017) Long-term impacts of parental migration on Chinese children’s psychosocial well-being: mitigating and exacerbating factors. Soc Psychiatry Psychiatr Epidemiol 52, 669–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hossain M, Onel G & Mullally C (2016) Migration and household decision on occupational choice and investment: evidence from Bangladesh. Selected paper prepared for presentation at the 2016 Agricultural & Applied Economics Association Annual Meeting, Boston, MA, USA, 31 July–2 August 2016. https://ideas.repec.org/p/ags/aaea16/236136.html (accessed October 2018). [Google Scholar]
- 6. Orozco M (2010) Migration, Remittances and Assets in Bangladesh: Considerations about Their Intersection and Development Policy Recommendations. Dhaka: International Organization for Migration, Regional Office for South Asia. [Google Scholar]
- 7. Cortes R (2008) Children and Women Left Behind in Labour Sending Countries: An Appraisal of Social Risks. New York: UNICEF, Policy, Advocacy and Knowledge Management Section, Division of Policy and Practice. [Google Scholar]
- 8. Luo J, Peng X, Zong R et al. (2008) The status of care and nutrition of 774 left-behind children in rural areas in China. Public Health Rep 123, 382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Song Y & Zhang Y (2009) Parental migration, child health and healthcare services utilization in rural China. Popul Res 33, 57–66. [Google Scholar]
- 10. Wen Y, Wang J, Liu R et al. (2008) Study on health status of left behind children in rural southern Anhui. Mod Prev Med 35, 690–692. [Google Scholar]
- 11. Zhou C, Sylvia S, Zhang L et al. (2015) China’s left-behind children: impact of parental migration on health, nutrition, and educational outcomes. Health Aff (Millwood) 34, 1964–1971. [DOI] [PubMed] [Google Scholar]
- 12. Mansuri G (2006) Migration, Sex Bias, and Child Growth in Rural Pakistan. World Bank Policy Research Working Paper no. 3946. Washington, DC: World Bank. [Google Scholar]
- 13. Nobles J (2007) Parental Migration and Child Health in Mexico. Los Angeles, CA: California Center for Population Research, University of California–Los Angeles. [Google Scholar]
- 14. Zhang N (2015) Parental migration, care-giving practices and left-behind children’s nutritional health in rural China: a mixed-methods approach. PhD Thesis, University of Manchester. [Google Scholar]
- 15. Zezza A, Carletto C, Davis B et al. (2011) Assessing the impact of migration on food and nutrition security. Food Policy 36, 1–6. [Google Scholar]
- 16. Ng J (2018) Labour Migration in Indonesia and the Health of Children Left Behind. WIDER Working Paper no. 2018/10. Helsinki: United Nations University World Institute for Development Economics Research. [Google Scholar]
- 17. Hugo G (2005) Migration in the Asia-Pacific Region. A paper prepared for the Policy Analysis and Research Programme of the Global Commission on International Migration. https://www.iom.int/jahia/webdav/site/myjahiasite/shared/shared/mainsite/policy_and_research/gcim/rs/RS2.pdf (accessed October 2018).
- 18. Bangladesh Bureau of Statistics & UNICEF Bangladesh (2014) Bangladesh Multiple Indicator Cluster Survey 2012–2013: Final Report. Dhaka: BBS and UNICEF Bangladesh. [Google Scholar]
- 19. National Institute of Population Research and Training, Mitra and Associates/Bangladesh & ICF International (2016) Bangladesh Demographic and Health Survey 2014. Dhaka and Rockville, MD: NIPORT, Mitra and Associates, and ICF International. [Google Scholar]
- 20. International Organization for Migration Bangladesh (2017) Social Cost of Migration on Children Left Behind due to Labour Migration. Dhaka: IOM. [Google Scholar]
- 21. Siddiqui T (2003) Migration as a Livelihood Strategy of the Poor: The Bangladesh Case. London: Department for International Development. [Google Scholar]
- 22. Civil Registration and Vital Statistics (2018) Migration Statistics in Bangladesh. http://crvs.gov.bd/statistics/bangladesh/migration (accessed February 2018).
- 23. UNICEF (2012) A Life Free from Hunger: Tackling Child Malnutrition. London: Save the Children. [Google Scholar]
- 24. Ahmed AS, Ahmed T, Roy S et al. (2012) Determinants of undernutrition in children under 2 years of age from rural Bangladesh. Indian Pediatr 49, 821–824. [DOI] [PubMed] [Google Scholar]
- 25. Aheto JMK, Keegan TJ, Taylor BM et al. (2015) Childhood malnutrition and its determinants among under‐five children in Ghana. Paediatr Perinat Epidemiol 29, 552–561. [DOI] [PubMed] [Google Scholar]
- 26. Chowdhury MRK, Rahman MS, Khan MMH et al. (2016) Risk factors for child malnutrition in Bangladesh: a multilevel analysis of a nationwide population-based survey. J Pediatr 172, 194–201.e191. [DOI] [PubMed] [Google Scholar]
- 27. UNICEF (1990) Conceptual framework of the determinants of child undernutrition. http://www.unicef.org/nutrition/training/2.5/4.html (accessed April 2018).
- 28. Yeoh BSA & Lam T (2006) The costs of (im)mobility: children left behind and children who migrate with a parent. In Perspectives on Gender and Migration: From the Regional Seminar on Strengthening the Capacity of National Machineries for Gender Equality to Shape Migration Policies and Protect Migrant Women, Bangkok, 22–24 November 2006, pp. 120–149. New York: United Nations Economic and Social Commission for Asia and the Pacific. [Google Scholar]
- 29. Nguyen CV (2016) Does parental migration really benefit left-behind children? Comparative evidence from Ethiopia, India, Peru and Vietnam. Soc Sci Med 153, 230–239. [DOI] [PubMed] [Google Scholar]
- 30. Wickramage K, Siriwardhana C, Vidanapathirana P et al. (2015) Risk of mental health and nutritional problems for left-behind children of international labor migrants. BMC Psychiatry 15, 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. De Bruyn T & Kuddus U (2005) Dynamics of Remittance Utilization in Bangladesh. IOM Migration Research Series no. 18. Geneva: International Organization for Migration. [Google Scholar]
- 32. Banul SS, Ahmed B-N, Jubayer S et al. (2011) Prevalence of soil transmitted helminthes (STH) infection among children aged 2–17 years in urban and rural areas of Dhaka district in Bangladesh. Bangladesh J Med Microbiol 5, 16–22. [Google Scholar]
- 33. Jayatissa R & Wickramage K (2016) What effect does international migration have on the nutritional status and child care practices of children left behind? Int J Environ Res Public Health 13, 218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. De Brauw A & Mu R (2012) Unattended but not Undernourished: Young Children Left Behind in Rural China. IFPRI Discussion Paper no. 01191. Washington, DC: International Food Policy Research Institute. [Google Scholar]
- 35. Lu Y (2015) Internal migration, international migration, and physical growth of left-behind children: a study of two settings. Health Place 36, 118–126. [DOI] [PubMed] [Google Scholar]
- 36. Mo X, Xu L, Luo H et al. (2016) Do different parenting patterns impact the health and physical growth of ‘left-behind’ preschool-aged children? A cross-sectional study in rural China. Eur J Public Health 26, 18–23. [DOI] [PubMed] [Google Scholar]
- 37. Miller JE & Rodgers Y (2009) Mother’s education and children’s nutritional status: new evidence for Cambodia. Asian Dev Rev 26, 131–165. [Google Scholar]
- 38. Semba RD, de Pee S, Sun K et al. (2008) Effect of parental formal education on risk of child stunting in Indonesia and Bangladesh: a cross-sectional study. Lancet 371, 322–328. [DOI] [PubMed] [Google Scholar]