Abstract
Objective:
The Composite Index of Anthropometric Failure (CIAF) can only be applied to children under 5 years of age and does not contemplate obesity. The aim of this study was to propose an Extended CIAF (ECIAF) that combines the characterization of malnutrition due to undernutrition and excess weight, and apply it in six Argentine provinces.
Design:
ECIAF excludes children not in anthropometric failure (group A) and was calculated from a percentage of children included in malnutrition categories B: wasting only; C: wasting and underweight; D: wasting, stunting and underweight; E: stunting and underweight; F: stunting only; Y: underweight only; G: only weight excess; and H: stunting and weight excess.
Setting:
Cross-sectional study conducted in Buenos Aires, Catamarca, Chubut, Jujuy, Mendoza and Misiones (Argentina).
Participants:
10 879 children of both sexes aged between 3 and 13·99.
Results:
ECIAF in preschool children (3 to 4·99 years) was 15·1 %. The highest prevalence was registered in Mendoza (16·7 %) and the lowest in Misiones (12·0 %). In school children (5 to 13·99 years) ECIAF was 28·6 %. Mendoza also recorded the highest rate (30·7 %), while Catamarca and Chubut had the lowest values (27·0 %). In the whole sample, about 25 % of the malnutrition was caused by undernutrition and 75 % by excess weight.
Conclusions:
The ECIAF summarizes anthropometric failure by both deficiency and excess weight and it highlights that a quarter of the malnutrition in the Argentine population was caused by undernutrition, although there are differences between Provinces (P < 0·05). ECIAF estimates are higher than those of CIAF or under-nutrition.
Keywords: Anthropometric failure Malnutrition, Children, Argentina
One of the main aims of the Millennium Development Goals was to reduce hunger to half of its prevalence, which only 79 of 129 countries managed to achieve. Currently, the second of the new Sustainable Development Goals (SDGs) for 2030 is to end hunger definitively and all kinds of malnutrition( 1 ). Specifically, the goal for 2025 is to reduce stunting by 40 % and acute malnutrition should not exceed 5 % among children younger than 5 years of age( 2 ). However, it is also necessary to improve the nutrition conditions in all population groups, especially in adolescents.
Undernutrition in children under 5 years old is one of the indicators used by the Food and Agriculture Organization of the United Nations and other international organizations to evaluate food security and its progress in the target population( 3 , 4 ). In particular, it is recommended that the proportion of children under 5 years old with stunting (low height for age), wasting (low weight for height) and underweight (low weight for age) be determined. Low height for age (H/A) allows a diagnosis to be made for retarded growth due to an insufficient diet over a long period of time (evidence of chronic malnutrition). Low weight for height (W/H) is an indicator of acute undernutrition (independently of age), which reflects an important food deprivation in a recent period causing a significant loss of lean and fatty tissue. Finally, low weight for age (W/A), is an index of global undernutrition, and it does not discriminate between chronic and acute states of undernutrition.
However, the same child could show signs of being in two or more of these malnutrition categories simultaneously. Additionally, even though chronic, acute or global malnutrition are very informative indexes when looked at separately, they do not offer a broader view of child malnutrition in the whole population. In order to solve this issue, Svedberg( 5 ) conceived an index that synthesized the proportion of malnourished children under 5 years of age based on the combination of several indicators. Svedberg proposed the Composite Index of Anthropometric Failure (CIAF), which has been successfully applied in different Asian countries such as India, Bangladesh or Nepal( 6 – 9 ), and African countries such as Nigeria, Liberia, Ghana and Ethiopia( 10 , 11 ). In Latin American countries, this indicator has been evaluated in Peruvian, Bolivian, Dominic Republic, Guatemala and Argentinian populations( 12 – 14 ) Recently, the CIAF has been also applied in an extended review, including 49 countries in which Colombian data were also involved( 15 ).
As indicated above, the SDGs for 2030 point both to the need to improve the nutritional status of children over 5 years of age and adolescents as well as to eliminate all types of malnutrition. More and more countries with economies in transition are facing a double burden of malnutrition. Childhood obesity and being overweight are emerging problems in Africa and Asia and childhood obesity rates in Latin America are among the highest in the world( 16 – 18 ). This situation calls for prevention and monitoring and for this purpose tools are needed to jointly assess malnutrition by deficiency and by excess. In this regard, we present a new methodological proposal that also includes excess weight and its eventual combination with retarded growth as other forms of anthropometric failure. In fact, in Latin American countries, the coexistence of stunting and excess weight is a topic that was addressed at the beginning of this century( 19 , 20 ). This issue, known as obesity in poverty, is emerging in nutritional transition and developed countries( 21 – 23 ), such as Argentina, where this process has been studied( 24 – 27 ). In addition, it is relevant to point out that Svedberg( 28 ), like Nandy and Svedberg( 10 ), emphasized the relevance of including overweight and obesity to complete the information provided by the CIAF. However, these authors have not published any paper in this regard. Sibrián and Palma de Fulladolsa( 29 ), however, have calculated the Malnutrition Anthropometric Index (MAI), which takes into account the double burden of malnutrition for children under five years of age.
Our proposal intends to extend the anthropometric failure evaluation to children over 5 years old, applying a new index called the extended CIAF (ECIAF). In this paper, this new and broader indicator will be implemented to evaluate the prevalence of malnutrition in the child and youth population in six Argentinian provinces.
Methods
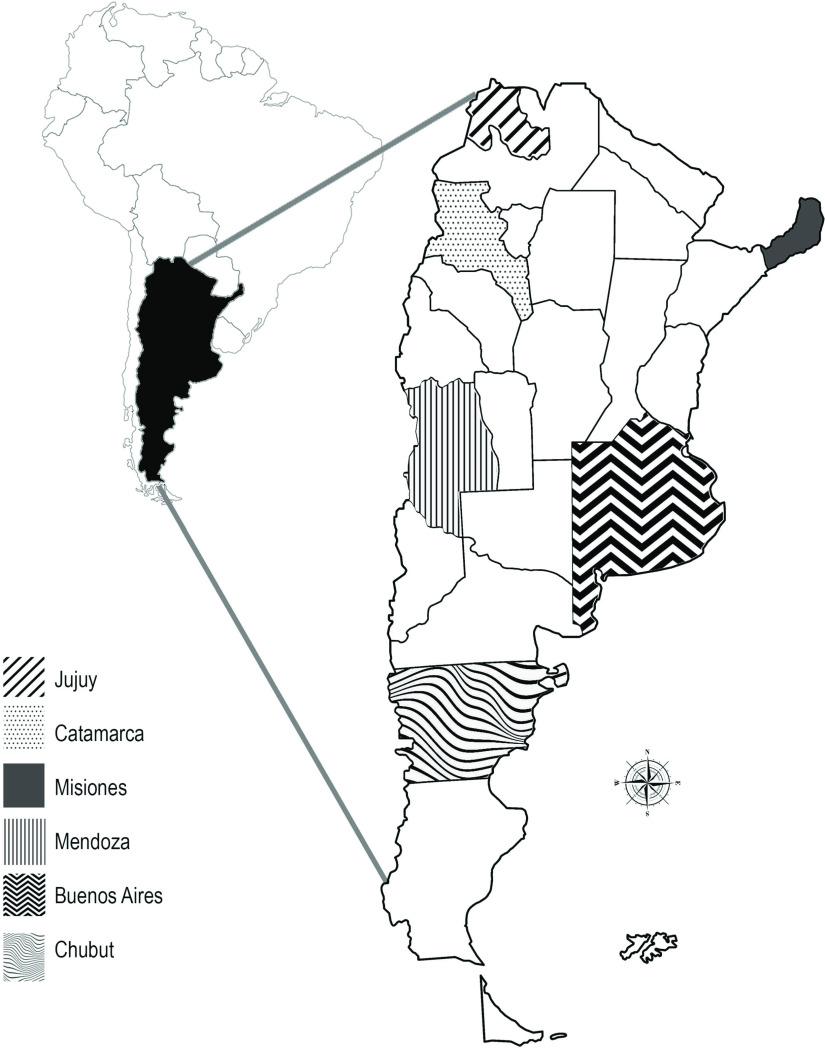
This is a cross-sectional study using a convenience sample and it was conducted according to the guidelines laid down in the Helsinki Declaration( 30 ) and approved by the ethics committees of the universities involved. After obtaining the written informed consent of the parents or guardians and excluding the subjects who had known pathological antecedents, a total of 10 879 school children were recruited from the provinces of Buenos Aires, Catamarca, Chubut, Jujuy, Mendoza and Misiones (Fig. 1). The sample was divided into two series of children depending on their age. The first series included 1952 preschool children (992 boys; 960 girls) between 3 and 4.99 years old. The second was formed by 8927 school children (5199 boys; 3728 girls) with ages from 5 to 13·99 years. The sample was collected between 2003 and 2010 in public schools. In the province of Buenos Aires, data were obtained in the villages of La Plata and Coronel Brandsen (urban and peri-urban area); in Catamarca, in the city of San Fernando del Valle (urban area) and in the municipalities of Antofasga de la Sierra and Ambato (rural area). In Chubut, data were collected in the city of Puerto Madryn (urban area). In Jujuy, the city of San Salvador de Jujuy, capital of the province and the rural villages of Susques, Abra Pampa, La Quiaca and Fraile Pintado were sampled. In Mendoza, data were collected in urban and rural areas of the Department of General Alvear and in Misiones in the town of Aristóbulo del Valle (urban and rural area). Table 1 shows in detail the distribution of the sample by province according to sex and age and Table 2 contains some sociodemographic indicators for the time interval in which the data collection was carried out.
Fig. 1.
Geographical location of the Argentine provinces analysed
Table 1.
Distribution of the sample by province of origin, sex and age
| Age | Buenos Aires (N) | Catamarca (N) | Chubut (N) | Jujuy (N) | Mendoza (N) | Misiones (N) | Total (N) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | M | F | M | F | M | F | M | F | M | F | M | F | |
| 3·00–4·99 | 312 | 351 | 44 | 43 | 123 | 133 | 167 | 148 | 209 | 165 | 137 | 120 | 992 | 960 |
| 5·00–6·99 | 273 | 257 | 49 | 40 | 119 | 83 | 139 | 113 | 165 | 127 | 100 | 110 | 845 | 730 |
| 7·00–8·99 | 547 | 508 | 105 | 84 | 233 | 233 | 256 | 256 | 346 | 342 | 262 | 239 | 1722 | 1662 |
| 9·00–10·99 | 499 | 343 | 96 | 52 | 207 | 125 | 235 | 181 | 302 | 158 | 245 | 176 | 1584 | 1035 |
| 11·00–13·99 | 293 | 62 | 66 | 35 | 108 | 32 | 163 | 58 | 252 | 65 | 166 | 49 | 1048 | 304 |
| Total (N) | 1924 | 1521 | 360 | 254 | 790 | 606 | 960 | 756 | 1274 | 857 | 910 | 694 | 6191 | 4688 |
Table 2.
Sociodemographic indicators in the Argentine provinces analysed
| Infant mortality per 1000 live births (2010) | Children aged 0–14 without health coverage (%) (2010) | % Households with UBN (urban–rural) (2010) | % Households with UBN (2001–2010) | % Adult illiteracy (2010) | HDI (2009) | |
|---|---|---|---|---|---|---|
| Buenos Aires | 11·8 | 45·58 | 6·4–7·1 | 10·5–6·4 | 1·3 | 0·869 |
| Catamarca | 14·0 | 45·59 | 9·2–18·6 | 18·4–11·3 | 2·0 | 0·808 |
| Chubut | 10·2 | 39·19 | 8·1–12·1 | 13·4–8·4 | 1·2 | 0·812 |
| Jujuy | 12·9 | 52·47 | 13·4–29·4 | 26·1–15·5 | 3·1 | 0·797 |
| Mendoza | 11·7 | 64·30 | 5·7 –16·5 | 13·1–7·6 | 2·1 | 0·826 |
| Misiones | 13·7 | 60·30 | 13·4–22·1 | 23·5–15·6 | 4·1 | 0·786 |
UBN: Unmet Basic Needs (Inability to provide for one’s own and one’s dependants food, clothing, housing and health care because of insufficient income and/or resources). HDI: Human Development Index. Source: National Institute of Statistics and Censuses. National Ministry of Economy( 37 ) and National Ministry of Health of the Republic of Argentina( 45 ).
Anthropometric measurements were taken according to international and national recommendations( 31 , 32 ). Body weight was measured using a digital scale (100 g precision) and the subjects wore light clothing, which was weighed and discounted from the total weight. The height (cm) was measured with an anthropometer (1 mm accuracy). The equipment was calibrated at the beginning of each anthropometric session.
The nutritional status of the preschool children (under 5 years old) was evaluated. All subjects with H/A, W/H or W/A <–2 standard deviation (sd), with respect to the standards of the World Health Organization( 33 ) were considered malnourished. In children between 5 and 13 years of age, H/A and W/A were assessed according to WHO references( 34 ). In this case, the W/H indicator (which measured acute undernutrition) was replaced by the Body Mass Index (BMI) for age (BMI-for-age), considering again <–2 sd to diagnose undernutrition. In both child groups, the excess weight was evaluated by W/H (under 5) and BMI-for-age (5–13 years of age), with a cutoff of ≥1 sd.
Svedberg’s index( 5 ) identified six groups in which A was comprised of the children without anthropometric failure. The other five are: B: wasting only; C: wasting and underweight; D: wasting, stunting and underweight; E: stunting and underweight; and F: stunting only. Afterwards, Nandy et al.( 6 ) added the Y group for underweight only. In this study we include two more categories; G: only excess weight and H: stunting and excess weight (Table 3). The ECIAF is calculated by subtracting the group A children from the total number. Therefore, ECIAF is the sum of the percentages from the rest of the categories (B + C + D + E + F + Y + G + H).
Table 3.
Categories that make up the new proposal of the extended composite index of anthropometric failure (ECIAF)
| Categories | Description | W/H or BMI/A < –2DE | W/H or BMI/A > 2DE | H/A < –2DE | W/A < –2DE |
|---|---|---|---|---|---|
| A | Without anthropometric failure | No | No | No | No |
| B | Wasting only | Yes | No | No | No |
| C | Wasting and underweight | Yes | No | No | Yes |
| D | Wasting, stunting and underweight | Yes | No | Yes | Yes |
| E | Stunting and underweight | No | No | Yes | Yes |
| F | Stunting only | No | No | Yes | No |
| Y | Underweight only | No | No | No | Yes |
| G | Weight excess (being overweight or obese) only | No | Yes | No | No |
| H | Stunting and weight excess | No | Yes | Yes | No |
| ECIAF = % (B+C+D+E+F+Y+G+H) | |||||
This paper examines both parameters, CIAF and ECIAF, to allow a comparison to be made with other populations analysed previously with CIAF only. Chi-square and Bonferroni (significant level P < 0·05) test were used to analyse the contrast of prevalence between sexes, age groups or provinces.
Results
The prevalence of ECIAF in preschool children aged under 5 was 15·1 %. The rate was higher (P < 0·05) in females (17·4 %) than in males (12·9 %). The highest incidence took place in Mendoza province and the lowest in Misiones. Nonetheless, when the CIAF index (which only takes into account undernutrition states) was applied, sexual differences were not statistically significant and the highest prevalence for this parameter was found in Jujuy while the lowest was in Chubut province (Table 4).
Table 4.
Prevalence of anthropometric failure in preschool children (under 5 years) by Argentine provinces, by sex and for the whole sample.
| A | B | C | D | E | F | Y | G | H | ECIAF | CIAF | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | |
| Buenos Aires | 84·0 | 557 | 0·7 | 5 | – | – | 0·82 | 4 | 2·1 | 14 | 0·6 | 4 | 11·8 | 78 | 0·1 | 1 | 16·0 | 106 | 4·1 | 27 | ||
| Catamarca | 84·3 | 73 | – | – | – | 1·1 | 1 | 2·2 | 2 | – | 12·4 | 11 | – | 15·7 | 14 | 3·3 | 3 | |||||
| Chubut | 86·7 | 222 | – | – | – | – | 0·8 | 2 | 0·4 | 1 | 12·0 | 31 | – | 13·2 | 34 | 1·2 | 3 | |||||
| Jujuy | 84·5 | 266 | 0·3 | 1 | – | – | 1·3 | 4 | 3·2 | 10 | 0·3 | 1 | 10·4 | 33 | – | 15·5 | 49 | 5·1 | 16 | |||
| Mendoza | 83·1 | 311 | – | – | – | 1·3 | 5 | 2·7 | 10 | – | 12·5 | 47 | 0·3 | 1 | 16·7 | 62 | 3·9 | 14 | ||||
| Misiones | 88·0 | 226 | – | – | – | 0·4 | 2 | 2·7 | 7 | 0·8 | 3 | 6·9 | 17 | 0·4 | 2 | 12·0 | 31 | 4· | 12 | |||
| Total simple | 84·9 | 1659 | 0·3 | 6 | – | – | 0·8 | 16 | 2·5 | 49 | 0·4 | 8 | 10·9 | 209 | 0·2 | 5 | 15·1 | 295 | 3·9 | 78 | ||
| Total males | 87·1 | 865 | 0·4 | 4 | – | – | 0·7 | 7 | 2·2 | 20 | 0·5 | 5 | 9·0 | 9 | 0·1 | 1 | 12·9 | 128 | 3·8 | 38 | ||
| Total females | 82·6 | 793 | 0·2 | 2 | – | – | 0·8 | 8 | 2·6 | 27 | 0·3 | 3 | 13·0 | 125 | 0·2 | 2 | 17·4 | 167 | 4·2 | 40 | ||
A: Without anthropometric failure; B: Wasting only; C: Wasting and underweight; D: Wasting, stunting and underweight; E: Stunting and underweight; F: Stunting only; Y: Underweight only; G: Weight excess (being overweight or obese) only; H: Stunting and weight excess
In addition, Table 4 shows that no children were included in the C (wasting and underweight) and D (wasting, stunting and underweight) groups. The B category (wasting only) was only present in Buenos Aires and Jujuy but in rates below 1 %. The E group prevalence (stunting and underweight) was significantly higher in Jujuy and Mendoza than in the other provinces (P < 0·05). Additionally, Jujuy had the maximum prevalence in group F (stunting only). This province, together with Mendoza and Misiones, reached rates between 3·2 % and 2·7 %, which were significantly higher than in Buenos Aires, Catamarca and Chubut (P < 0·05). The Y group (Underweight only) reaches 0·8 % in Misiones and it was significantly higher (P < 0·05) than in Buenos Aires, Chubut and Jujuy, ranging within 0·3–0·6 %. This category was absent in Catamarca and Mendoza. The G category (only overweight) registered the lowest prevalence in Misiones and the highest in Mendoza, with interprovincial differences (P < 0·05). The H category (stunting and overweight) had no prevalence in Catamarca, Chubut and Jujuy and was very low in the rest of the provinces, reaching values ranging from 0·1 to 0·4.
Regarding the school children aged five and over, it is important to highlight that anthropometric failure (in all its categories) reached higher values than in children under five years of age. Contrary to the group with the lowest age, the ECIAF was significantly more prevalent (P < 0·05) in males (30·9 %) than females (25·5 %). When the analysis was made by provinces, Mendoza also registered the highest rate, while Catamarca and Chubut had the lowest values. When CIAF was applied (replacing W/H by BMI-for-age in order to identify wasting children), Chubut was also the province with less prevalence, however, in this case Jujuy showed the maximum rate.
Unlike what is observed in children under five years of age, among children between 5 and 13 years of age (Table 5) there were cases in group C (wasting and underweight) and D (wasting, stunting and underweight). Significant differences between provinces (P < 0·05) were found, even though the prevalence was low, and Jujuy showed the highest rate (0·5%) for C and D categories. In the same way, Jujuy had the highest rate in groups E (stunting and underweight) (2 %) and F (stunting only) (6 %), while the lowest values were registered in Chubut (E: 0·3 % and F: 1·8 %). Group Y (underweight only) had minimum rates in all the provinces, except Catamarca and Chubut where they have not been observed. Conversely, the children’s prevalence classified in group G (only weight excess) was highest in Chubut and the lowest rate was found in Catamarca. The differences between provinces were significant (P < 0·05). Lastly, the highest rate for group H was observed in Jujuy (1·3 %) (stunting and weight excess) compared with the other provinces studied. Chubut registered the minimum prevalence for this group (H: 0·4 %).
Table 5.
Prevalence of anthropometric failure in school children (from 5 to 13·99 years) by Argentine provinces, by sex and for the whole sample
| A | B | C | D | E | F | Y | G | H | ECIAF | CIAF | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | |
| Buenos Aires | 72·1 | 2011 | 0·3 | 10 | 0·3 | 10 | 0·1 | 3 | 0·7 | 20 | 3·6 | 101 | 0·1 | 3 | 22·4 | 626 | 0·5 | 5 | 27·9 | 78 | 5·2 | 147 |
| Catamarca | 73·0 | 385 | 0·5 | 3 | 0·3 | 2 | 0·3 | 2 | 1·4 | 7 | 5·0 | 25 | – | 18·8 | 99 | 0·8 | 4 | 26·9 | 142 | 7·4 | 39 | |
| Chubut | 72·9 | 831 | 0·7 | 8 | 0·3 | 3 | 0·2 | 2 | 0·3 | 3 | 1·8 | 21 | – | 268 | 23·5 | 0·4 | 5 | 27·1 | 309 | 3·2 | 37 | |
| Jujuy | 70·2 | 984 | 0·2 | 3 | 0·5 | 7 | 0·5 | 7 | 2·0 | 28 | 6·0 | 84 | 0·3 | 4 | 19·0 | 266 | 1·3 | 18 | 29·8 | 417 | 9·5 | 133 |
| Mendoza | 69·3 | 1218 | 0·6 | 11 | 0·4 | 7 | 0·4 | 7 | 1·5 | 26 | 5·6 | 98 | 0·4 | 7 | 21·3 | 374 | 0·5 | 9 | 30·7 | 539 | 8·9 | 156 |
| Misiones | 72·2 | 973 | 0·4 | 5 | 0·3 | 4 | 0·3 | 4 | 1·1 | 15 | 5·0 | 67 | 0·2 | 3 | 19·8 | 267 | 0·8 | 11 | 27·8 | 375 | 7·2 | 97 |
| Total sample | 71·4 | 6377 | 0·4 | 36 | 0·3 | 27 | 0·3 | 27 | 1·1 | 98 | 4·4 | 393 | 0·2 | 18 | 21·2 | 1893 | 0·7 | 62 | 28·6 | 2554 | 6·7 | 598 |
| Total males | 69·1 | 3593 | 0·4 | 21 | 0·4 | 21 | 0·2 | 10 | 0·9 | 47 | 4·5 | 234 | 0·2 | 10 | 23·6 | 1227 | 0·7 | 36 | 30·9 | 1606 | 6·6 | 344 |
| Total females | 74·5 | 2776 | 0·5 | 19 | 0·2 | 9 | 0·3 | 12 | 1·5 | 56 | 4·4 | 164 | 0·2 | 9 | 17·8 | 663 | 0·6 | 23 | 25·5 | 955 | 7·1 | 265 |
A: Without anthropometric failure; B: Wasting only; C: Wasting and underweight; D: Wasting, stunting and underweight; E: Stunting and underweight; F: Stunting only; Y: Underweight only; G: Weight excess (overweight or obesity) only; H: Stunting and weight excess.
The joint analysis of both anthropometric failure (Fig. 2) rates in the Argentinian population considered in this study highlights that about a quarter of the malnutrition observed in the sample is caused by undernutrition, although there are differences between provinces (P < 0·05). Undernutrition with respect to total malnutrition registers a maximum in Misiones (among children under 5 years of age) and Jujuy (from 5 years onwards) and minimum in Chubut. Furthermore, all prevalence associated with indicators of underweight, stunting and wasting presented values below the significant cut-off levels established by WHO( 35 ), revealing a state of health due to undernutrition of small magnitude.
Fig. 2.
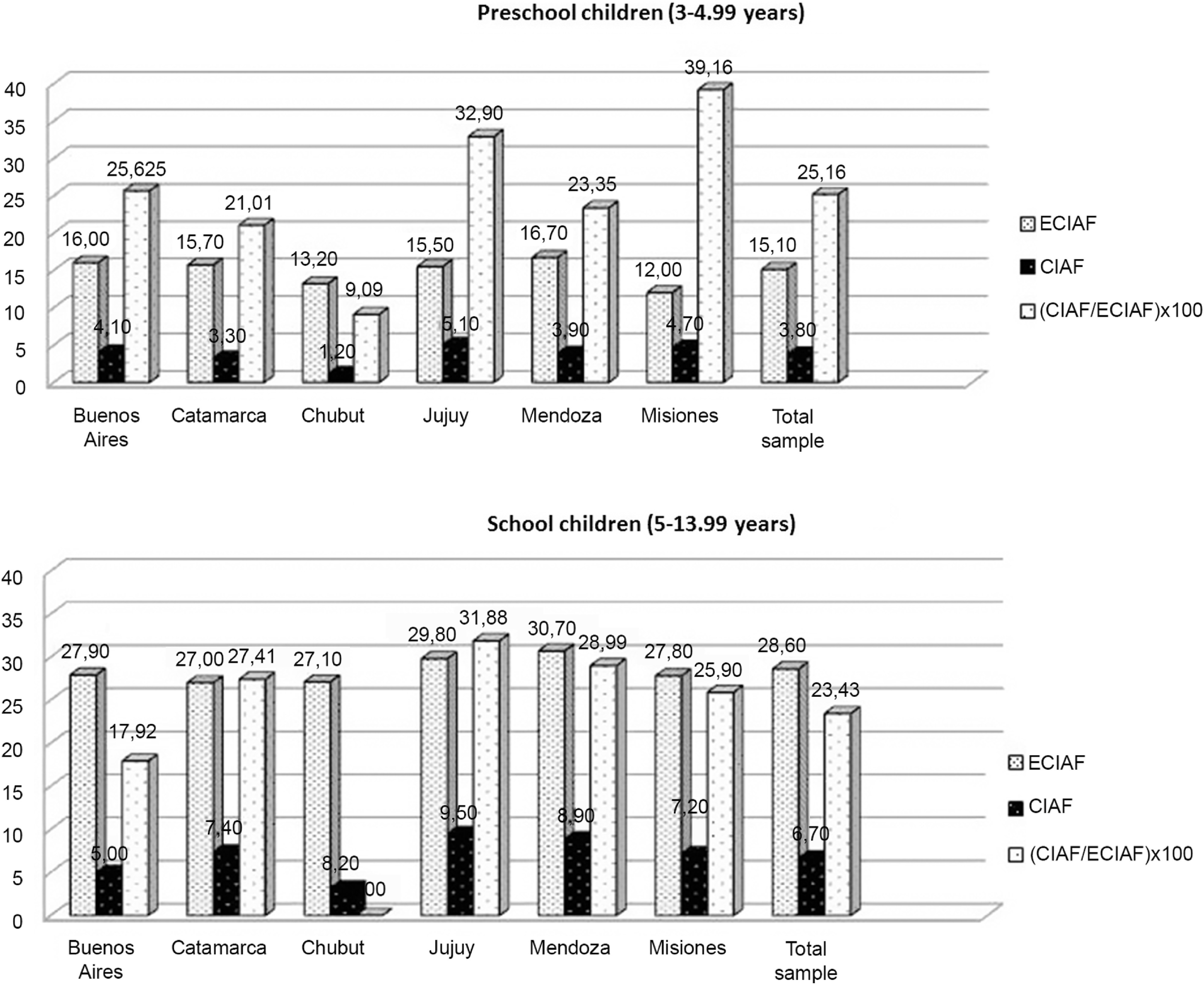
Prevalence of malnutrition evaluated through indicators of anthropometric failure (CIAF, ECIAF) and their relationship to each other (CIAF/ECIAF) × 100
Discussion
This paper has shown that both the CIAF and the ECIAF provide broad information about the nutritional status of the communities. The prevalence of malnutrition increases with age, for the whole sample. In children under 5 (males: 3·8 %; females: 4·2 %), the CIAF parameter is lower than in children over this age (males: 6·6 %; females: 7·1 %). Also, the malnutrition evaluated by ECIAF increases with age, revealing a rate of 12·9 % in preschool males under 5 years of age and 17·4 % in females. However, in school children between 5 and 13 years of age, this rate rises to 30·9 % and 25·5 %, respectively. The differences among the provinces observed here are in accordance with the results obtained in Argentina one decade ago( 36 ). In this past study, a north–south gradient was established, revealing a higher proportion of undernutrition in the northeast (Jujuy) and more obesity in the south (Chubut). This variation was directly related with other socio-environmental indicators such as economic activity, unmet basic needs, maternal and infant mortality rates and sanitary conditions. However, in the current study, Mendoza (located in the central region of Argentina) is the province with the highest ECIAF, to which overweight and stunting contribute significantly. It should be noted that quality of life indicators such as the HDI (0·826) or households with unsatisfied basic needs (7·6 % in 2010) place Mendoza in an intermediate position with respect to the country as a whole but it is the province with the lowest health coverage. Specifically, 64·30 % of children under the age of 14 did not have health insurance in 2010( 37 ). On the other hand, in the PROSANE Study (Programa Sanitario Escolar, School Health Program) conducted in 2012 on 9740 schoolchildren in the province, it was highlighted that Mendoza was one of the regions most affected by double malnutrition, since 31 % of the children were overweight and 13 % were at risk due to low weight( 38 ).
The CIAF prevalence in children under 5 years of age is considerably lower than the rates observed in other Latin American countries such as Peru (28·3 %), Bolivia (26·6) and the Dominican Republic (12·5 %)( 10 ). In addition, CIAF was lower than the figures reported in Guatemala by Sibrián and Palma de Fulladolsa( 29 ) or by Díez Navarro( 14 ): 43·7 % and 75·2 %, respectively. In this last study, it is important to mention that the high rate found was due to the high proportion of children who are classified exclusively as suffering from chronic malnutrition or, concomitantly, having low weight. The results recorded in the current study are also lower than the rates shown in recent studies( 39 ) in Nigeria (51 %) and Ethiopia (52 %). Similar outcomes are obtained in different Asian countries such as China (21·7 %)( 40 ), India (47·8 % - 51 %)( 41 , 42 ) or Pakistan (52·4 %)( 43 ).
According to a meta-analysis conducted in 10 developing countries( 44 ), the risk of mortality is 3·4 times higher in children who present as stunted and underweight (group E) with regard to children who do not have any anthropometric failure. This risk is 4·7 points greater in children who suffered from wasting and underweight (group C) and 12·3 points higher in those who are affected with wasting, stunting and being underweight simultaneously (group D). The results of this study( 44 ) suggest that ICFA is useful because the risk of death associated with multiple anthropometric deficits is higher than that associated with a single failure.
In the Argentinian population, the greatest contribution to the CIAF index is from group F (chronic undernutrition). This and group E (stunting and underweight) showed slightly higher percentages in Mendoza (1·3 %) and in the northeast provinces (Jujuy 1·3 %; Catamarca 1·1 %), which were also those with higher rates of infant mortality (Jujuy: 12·9/1000 and Catamarca: 14/1000), and unsatisfied basic needs (Jujuy: 15·5 %; Catamarca: 11·3 %) in the period analysed( 37 , 45 ).
The current paper shows that the proportion of children under 5 years old with retarded growth (3·3 % group F and E) and presenting low weight (1·3 % those included in categories E and Y) yield values below those published for South America( 46 ) in 2005 (11·3 % and 3·1 %, respectively). In contrast, the overweight and obesity rates reported here are more than double those in the aforementioned study. This supports the Durán et al.( 46 ) hypothesis, which predicts in Latin American populations a positive secular trend in height with an increase in excess weight. However, in societies undergoing a transition phase, overweight is increasing faster than chronic undernutrition is decreasing( 20 ). This fact allows a dangerous association between retarded growth and overweight and obesity, as pointed out in a study conducted with South African, Russian, Chinese and Brazilian populations( 47 ).
The malnutrition evaluation made by the ECIAF encompasses a higher prevalence of children in group G (excess weight), while the rates of those showing stunting and excess weight (group H) did not reach 0·5 %. These data highlight that malnutrition by excess weight is not as relevant as in other countries such as South Africa or Mexico. For example, in Limpopo (South Africa) it was observed that the 1·9 % of preschool children had retarded growth and obesity( 48 ). In addition, it has been verified in seven Mexican states (Guerrero, Hidalgo, Michoacán, Puebla, Querétaro, San Luis Potosí and Veracruz) that 10 % of children between 2 and 6 years old had stunting and were overweight or obese at the same time( 49 ).
When we applied the CIAF parameter to evaluate the conditions of children between 5 and 13 years of age, we observed that there was higher prevalence of undernutrition (in all its forms) than in the younger group. Although in a very low proportion, we found subjects classified in all categories, with both, simple and multiple anthropometric failures. As in children under 5 years of age, chronic undernutrition is the type that contributes more to the CIAF. However, it is important to underline that the retarded growth rate has doubled. A proper comparison with other populations is hard to make because the bibliography using the CIAF parameter in children over 5 years of age is very scarce. Mondal and Sen( 50 ) assessed underweight, stunting, low BMI for age and its combinations in Indian schoolchildren between 5 and 12 years old, based on references from the patterns of the National Center of Health Statistics( 51 ). Following the same methodology, Thakur and Gautam( 52 ) also analysed Indian school children between 5 and 18 years of age. The results obtained showed a great variability because of religious factors, ethnicity, geoclimatology and urban development. In addition, the authors observed that the low weight for age and also the low height for age progressively differed from the reference obtained from between 5 and 18-year-olds. This observation is in line with our results, specifically with the retarded growth increasing from 5 years old and upwards compared with children under 5 years of age. ECIAF proves that both the G (weight excess) and H (stunting and weight excess) groups doubled their prevalence in comparison with the younger children. A greater association between retarded growth and excess weight in adolescence compared with childhood was also found in the THUSA BANA study( 53 ) in South Africa.
In another important publication, Lobstein et al.( 54 ) suggested that short stature is an important cause of the obesity epidemic in children and adults. They compiled data from low and middle-income countries such as Mexico, Brazil, South Africa, India or Vietnam and also analysed economically depressed social groups from the United Kingdom and the United States. All their observations agree with our outcomes, since they observed that children with retarded growth and excess weight increased in prevalence with age, between 5 and 18 years.
CIAF is closely related to morbidity and mortality( 12 ) and it has been highlighted that despite having declined since 2000, the morbidity and mortality associated with childhood malnutrition is currently a public health problem in Argentina( 55 ). ECIAF is a more complete index that shows the overall magnitude of child and youth malnutrition and allows an analysis to be conducted on the direction and degree of population changes over time. For this reason, ECIAF can provide valuable epidemiological information for monitoring the progress of public health policies aimed at improving the nutritional condition of children and adolescents.
Conclusion
This paper proposes a new synthetic index to anthropometrically evaluate malnutrition by both deficiency and excess (ECIAF) which, unlike CIAF, can also be applied to children over 5 years old. The strength of this indicator is its capacity to summarize child malnutrition in a single value, facilitating comparison between populations or over time. The application of ECIAF to six Argentine provinces showed that malnutrition due to excess weight almost tripled undernutrition. In addition, ECIAF in school children aged five and over was double that reported for children under that age.
Acknowledgements
Acknowledgments: the authors thank the participating schools, teachers, parents and children. Financial support: The study was supported by Argentinean National Council of Scientific and Technical Research (Project PIP 0106). Secretariat of Science and Technology, National University of Catamarca (Project 02/L449) and Secretariat of Science and Technology, University of Santiago del Estero (Project CS No. 1033/2016). Conflict of interest: The authors declare that they have no conflict of interest. Authorship: All authors were involved in study design, anthropometric measurements, statistical analysis, interpretation, and preparation of the paper. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Ethics Committee of the Universidad de la Plata.
References
- 1. United Nations (2015) Full report of the open working group of the general assembly on sustainable development goals is issued as document A/68/970. http://undocs.org/A/68/970 (accessed November 2017).
- 2. de Onis M, Dewey KG, Borghi E et al. (2013) The World Health Organization’s global target for reducing childhood stunting by 2025: rationale and proposed actions. Matern Child Nutr 9, 6–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Food and Agriculture Organization of the United Nations. Agriculture and Economic Development Analysis Division (2015) The State of Food Insecurity in the World (SOFI) State of Food Insecurity in the World (FAO) Series. 61 pages. http://www.fao.org/publications/sofi/2015/en/ (accessed September 2017).
- 4. Misselhorn A & Hendriks SL (2017) A systematic review of sub-national food insecurity research in South Africa: Missed opportunities for policy insights. PLoS One 12, e0182399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Svedberg P (2000) Poverty and Undernutrition: Theory, Measurement and Policy. Oxford, UK: Oxford University Press. [Google Scholar]
- 6. Nandy S, Irving M, Gordon D et al. (2005) Poverty, child undernutrition and morbidity: new evidence from India. Bull World Health Organ 83, 210–216. [PMC free article] [PubMed] [Google Scholar]
- 7. Boregowda GS, Soni GP, Jain K & Agrawal S (2015) Assessment of under nutrition using Composite Index of Anthropometric Failure (CIAF) among toddlers residing in urban slums of Raipur City, Chattisgarh, India. J Clin Diagn Res 9, 4–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Manda G & Bose K (2009) Assessment of overall prevalence of undernutrition using Composite Index of Anthropometric Failure (CIAF) among preschool children of West Bengal, India and Iran. J Pediatr 19, 237–243. [Google Scholar]
- 9. Biswas S, Bose K, Mukhopadhyay A & Bhadra M (2009) Prevalence of undernutrition among pre-school children of Chapra, Nadia District, West Bengal, India, measured by Composite Index of Anthropometric Failure (CIAF). Anthropol Anz 67, 269–279. [DOI] [PubMed] [Google Scholar]
- 10. Nandy S. & Svedberg P (2012) The Composite Index of Anthropometric Failure (CIAF): an alternative indicator for malnutrition in young children 2012. In: Handbook of Anthropometry: Physical Measures of Human Form in Health and Disease, pp. 127–137 [Preedy V.R., editor]. London, UK: Springer, Chapter 6. [Google Scholar]
- 11. Endris N, Asefa H & Dube L (2017) Prevalence of malnutrition and associated factors among children in rural Ethiopia. Hindawi Biomed Res Int. 6 pages. Article ID: 6587853. doi: 10.1155/2017/6587853. [DOI] [PMC free article] [PubMed]
- 12. Nandy S & Miranda JJ (2008) Overlooking undernutrition? Using a composite index of anthropometric failure to assess how underweight misses and misleads the assessment of undernutrition in young children. Soc Sci Med 66, 1963–1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bejarano IF, Carrillo AR, Dipierri JE et al. (2014) Composite index of anthropometric failure and geographic altitude in children from Jujuy (1 to 5 years old). Arch Argent Pediatr 112, 526–531. [DOI] [PubMed] [Google Scholar]
- 14. Diez-Navarro A (2018) Comparative analysis of anthropometric indicators for the diagnosis of child malnutrition. Doctoral Thesis, Faculty of Nursing. Complutense University of Madrid.
- 15. Vollmer S, Harttgen K, Kupka R & Subramanian SV (2017) Levels and trends of childhood undernutrition by wealth and education according to a Composite Index of Anthropometric Failure: evidence from 146 Demographic and Health Surveys from 39 countries. BMJ Global Health 2, e000206. doi: 10.1136/bmjgh-2016-000206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Adom T, Puoane T, de Villiers A et al. (2017) Prevalence of obesity and overweight in African learners: a protocol for systematic review and meta-analysis. BMJ Open 7, e013538. doi: 10.1136/bmjopen-2016-013538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mazidi M, Banach M, Kengne AP & Lipid and Blood Pressure Meta-analysis Collaboration Group (2018) Prevalence of childhood and adolescent overweight and obesity in Asian countries: a systematic review and meta-analysis. Arch Med Sci 14, 1185–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Caballero B, Vorkoper S, Anand N & Rivera JA (2017) Preventing childhood obesity in Latin America: an agenda for regional research and strategic partnerships. Obes Rev 18, 3–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Peña M & Bacallao J (2000) Obesity in Poverty: A New Public Health Challenge. Pan American Health Organization PAHO. Scientific Publication 576. Geneva, Switzerland: WHO. [Google Scholar]
- 20. Uauy R, Albala C & Kain J (2001) Obesity trends in Latin America: transiting from under- to overweight. J Nutr 131, 893S–899S. [DOI] [PubMed] [Google Scholar]
- 21. Timaeus IM (2012) Stunting and obesity in childhood: a reassessment using longitudinal data from South Africa. Int J Epidemiol 41, 764–772. [DOI] [PubMed] [Google Scholar]
- 22. Vásquez-Garibay EM, Miranda-Ríos L, Romero-Velarde E et al. (2018) Stunting, overweight and obesity during the nutrition transition in schoolchildren of Arandas, Jalisco, Mexico. Rev Med Inst Mex Seguro Soc 56, 6–11. [PubMed] [Google Scholar]
- 23. Zukiewicz-Sobczak W, Wróblewska P, Zwoliński J et al. (2014) Obesity and poverty paradox in developed countries. Ann Agric Environ Med 21, 590–594. [DOI] [PubMed] [Google Scholar]
- 24. Bejarano I, Dipierri J, Alfaro E et al. (2005) Evolution of the prevalence of overweight, obesity and malnutrition in schoolchildren in San Salvador de Jujuy. Arch Arg Pediatr 103, 101–109. [Google Scholar]
- 25. Oyhenart EE, Orden AB, Forte LM et al. (2005) Nutritional transition in three cities with different environmental urban complexity. Rev Arg Antrop Biol 7, 35–46. [Google Scholar]
- 26. Lomaglio DB (2012) Nutrition transition and the impact on growth and body composition in northwestern Argentina (NOA). Nutr Clín Diet Hosp 32, 30–35. [Google Scholar]
- 27. Bergel Sanchıs ML, Cesani MF & Oyhenart EE (2017) Contexts of occurrence of child malnutrition in the district of Villaguay, Entre Rios, Argentina. A multivariate analysis. PLoS ONE 12, e0176346. doi: 10.1371/journal.pone.0176346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Svedberg P (2007) Can indicators of child malnutrition be improved – and for what purposes? Speaker summary note. Taking action for the world’s poor and hungry people. Beijing, China: International Food Policy Research Institute. [Google Scholar]
- 29. Sibrián R & Palma de Fulladolsa P (2016) Classification of dual burden of malnutrition in young children. J Nutr Food Sci 6, 4. [Google Scholar]
- 30. Wordl Medical Association (2008) Helsinki Declaration-Ethical principles for medical research involving human subjects. 59th WMA General Assembly. Seul, Republic of Korea.
- 31. Lohman TG, Roche AF & Martorell R (1988) Anthropometric Standardization Reference Manual. Champaign, Illinois: Human Kinetics Books; [Google Scholar]
- 32. Argentine Pediatrics Society (2013) National Committee for Growth and Development. Guidelines for the Evaluation of physical growth. 3rd ed. Buenos Aires, Argentina: Publicaciones de la Sociedad Argentina de Pediatría. [Google Scholar]
- 33. World Health Organization (2006) WHO Multicentre Growth Reference Study Group: WHO Child Growth Standards: Length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: Methods and development. http://www.who.int/childgrowth/standards/en/ (accessed January 2018).
- 34. World Health Organization (2007) WHO Reference 2007 - Growth references 5–19 years. http://www.who.int/growthref/en/ (accessed January 2018).
- 35. de Onis M & Blössner M (1997) WHO Global Database on Child Growth and Malnutrition. Programme on Nutrition. Geneva: World Health Organization. [DOI] [PubMed] [Google Scholar]
- 36. Oyhenart E, Dahinten S, Alba JA et al. (2008) Nutritional status of children and young people in six provinces of Argentina: regional variation. Rev Arg Antrop Biol 10, 1–62. [Google Scholar]
- 37. INDEC. National Institute of Statistics and Censuses (2010) National Census of Population, Households and Housing. National Ministry of Economy. http://www.indec.gov (accessed November 2017).
- 38. Ministry of Health of the Argentine Republic (2014) PROSANE Survey. National School Health Program. https://www.argentina.gob.ar/salud/sanidadescolar (accessed November 2017).
- 39. Nandy S, Daoud A & Gordon D (2016) Examining the changing profile of undernutrition in the context of food price rises and greater inequality. Soc Sci Medicine 149, 153e163. [DOI] [PubMed] [Google Scholar]
- 40. Pei L, Ren L & Yan H (2014) A survey of undernutrition in children under three years of age in rural Western China BMC Public Health 14, 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Savanur MS & Ghugre PS (2015) Magnitude of undernutrition in children aged 2 to 4 years using CIAF and conventional indices in the slums of Mumbai city. J Health Popul Nutr 33, 3 doi: 10.1186/s41043-015-0017-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kramsapi R, Singh Kn N & Mondal N (2018) Composite Index of Anthropometric Failure (CIAF) among preschool (2–5 years) tribal children of Assam (India). Human Biology Review 7, 1–18. [Google Scholar]
- 43. Avan BI, Razab SA & Kirkwoodc BR (2015) An epidemiological study of urban and rural children in Pakistan: examining the relationship between delayed psychomotor development, low birth weight and postnatal growth failure. Trans R Soc Trop Med Hyg 109, 189–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. McDonald CM, Olofin I, Flaxman S et al. (2013) Nutrition impact model study. The effect of multiple anthropometric deficits on child mortality: meta-analysis of individual data in 10 prospective studies from developing countries. Am J Clin Nutr 97, 896–901. [DOI] [PubMed] [Google Scholar]
- 45. National Ministry of Health (2016) Secretariat of Policies, Regulation and Institutes. Directorate of Health Statistics and Information. Vital statistics. Basic information. Series 5 Number 59. Buenos Aires, Argentina: Argentinian National Ministry of Health. [Google Scholar]
- 46. Durán O, Caballero B & de Onís M (2006) The association between stunting and overweight in Latin American and Caribbean preschool children. Food Nutr Bull 27, 4, The United Nations University. [DOI] [PubMed] [Google Scholar]
- 47. Popkin BM, Richards MK & Monteiro CA (1996) Stunting is associated with overweight in children of four nations that are undergoing the nutrition transition. J Nutr 126, 3009–3016. [DOI] [PubMed] [Google Scholar]
- 48. Mamabolo RL, Alberts M, Steyn NP et al. (2005) Prevalence and determinants of stunting and overweight in 3-year-old black South African children residing in the Central Region of Limpopo Province, South Africa. Public Health Nutr 8, 501–508. [DOI] [PubMed] [Google Scholar]
- 49. Fernald LC & Neufeld LM (2007) Overweight with concurrent stunting in very young children from rural Mexico. Europ J Clin Nut 61, 623–632. [DOI] [PubMed] [Google Scholar]
- 50. Mondal N & Sen J (2010) Prevalence of undernutrition among children (5–12 years) belonging to three communities residing in a similar habitat in North Bengal, India. Ann Hum Biol 37, 198–216. [DOI] [PubMed] [Google Scholar]
- 51.National Center for Health Statistics (1977) Growth curves for children birth to 18 years: United States Department of Health Education and Welfare, Vital and Health Statistics; 1977 Series 11. Nb.165. https://www.cdc.gov/nchs/data/hus/hus7677.pdf (accessed September 2017). [PubMed]
- 52. Thakur R & Gautam RK (2015) Nutritional status among boys and girls of a central Indian Town (Sagar) Anthropological Review 78, 197–212. [Google Scholar]
- 53. Mukuddem-Petersen J & Kruger HS (2004) Association between stunting and overweight among 10–15-y-old children in the North West Province of South Africa: the THUSA BANA Study. Int J Obes Relat Metab Disord 28, 842–851. [DOI] [PubMed] [Google Scholar]
- 54. Lobstein T, Jackson-Leach R, Moodie ML et al. (2015) Child and adolescent obesity: part of a bigger picture. Lancet 385, 2510–2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Longhi F, Gómez A, Zapata ME, Paolasso P, Olmos F & Ramos Margarido S (2018) Malnutrition in Argentinean children in the early years of the 21st century: a quantitative approach. Salud Colectiva 14, 33–50. [DOI] [PubMed] [Google Scholar]