Abstract
Objective:
The majority of groceries purchased by US households are industrially processed, yet it is unclear how processing level influences diet quality. We sought to determine if processing level is associated with diet quality of grocery purchases.
Design:
We analysed grocery purchasing data from the National Household Food Acquisition and Purchase Survey 2012–2013. Household grocery purchases were categorized by the NOVA framework as minimally processed, processed culinary ingredients, processed foods or ultra-processed foods. The energy share of each processing level (percentage of energy; %E) and Healthy Eating Index-2015 (HEI-2015) component and total scores were calculated for each household’s purchases. The association between %E from processed foods and ultra-processed foods, respectively, and HEI-2015 total score was determined by multivariable linear regression. Foods purchased by households with the highest v. lowest ultra-processed food purchases and HEI-2015 total score <40 v. ≥60 were compared using linear regression.
Setting:
USA.
Participants:
Nationally representative sample of 3961 households.
Results:
Processed foods and ultra-processed foods provided 9·2 (se 0·3) % and 55·8 (se 0·6) % of purchased energy, respectively. Mean HEI-2015 score was 54·7 (se 0·4). Substituting 10 %E from minimally processed foods and processed culinary ingredients for ultra-processed foods decreased total HEI-2015 score by 1·8 points (β = −1·8; 95 % CI −2·0, −1·5). Processed food purchases were not associated with diet quality. Among households with high ultra-processed food purchases, those with HEI-2015 score <40 purchased less minimally processed plant-foods than households with HEI-2015 score ≥60.
Conclusions:
Increasing purchases of minimally processed foods, decreasing purchases of ultra-processed foods and selecting healthier foods at each processing level may improve diet quality.
Keywords: NOVA, FoodAPS, Diet quality, Healthy Eating Index-2015, Ultra-processed food
It is well documented that the US food supply and the dietary intakes of the US population do not adhere to the federal government’s dietary recommendations for a healthy diet( 1,2). Compared with the Dietary Guidelines for Americans 2010, the average intakes of fruits, vegetables, whole grains, dairy and legumes are 20–80 % below the recommended levels while the amounts of sodium, added sugar, solid fats and refined grains in the diet are excessive(1). Given that the majority of food dollars in the USA are spent on groceries (57·3 %), household food purchases may significantly influence diet quality(3).
The types of foods available in the home are strongly correlated with individual dietary intake and diet quality among adults and youth(4–12). Household grocery purchases may therefore serve as a proxy to study the home food environment and household members’ food consumption and diet quality. As food purchasing behaviours are modifiable by interventions(13,14), grocery purchases may be an opportune target for public health efforts to enhance home food environments and improve the diet quality of all household members. In particular, some research groups have hypothesized that reducing the proportion of ultra-processed foods in the diet may be a simple and effective strategy to improve diet quality(15–17).
Industrially processed foods and beverages constituted over 75 % of energy purchased by US households in 2012(18). The role of industrially processed foods in a healthy diet is controversial(15–17,19,20). Researchers have argued that so-called ‘ultra-processed foods’, defined as industrial formulations made with no or minimal whole foods, are inherently nutritionally unbalanced as these are generally high in total energy, sugar, sodium and/or saturated fat, while low in fibre, essential micronutrients and phytochemicals(15–17). Conversely, others disagree that food processing level is useful predictor of nutritional quality and maintain that ultra-processed and processed foods are nutritionally important in the USA(19,20).
National and international studies support that diets higher in ultra-processed foods are of poorer nutritional quality, lower in fibre, protein and several essential micronutrients, and higher in saturated fat, carbohydrates and added sugars(21–27). Nevertheless, industrially processed foods provide a significant proportion of several essential micronutrients in the US diet(28). Foods of all processing levels have also been found to contribute to both ‘nutrients to increase’ and ‘food components to limit/reduce’ according to the Dietary Guidelines for Americans 2010(28).
To date, the contribution of ultra-processed foods to US household grocery purchases and its association with diet quality has not been empirically determined. It is unclear if interventions aimed at improving the healthfulness of food purchases should emphasize processing level or other metrics of diet quality, such as the Healthy Eating Index-2015 (HEI-2015). The current study therefore aims to: (i) describe the processing level defined by the NOVA framework and diet quality of US households’ grocery purchases for home consumption, as measured by NOVA and the HEI-2015, respectively; and (ii) examine the associations between food processing level and the diet quality of household grocery purchases.
Methods
Data source
The present study uses data from the US Department of Agriculture’s National Household Food Acquisition and Purchase Survey (FoodAPS) collected between April 2012 and January 2013. FoodAPS is a cross-sectional survey designed to collect comprehensive data regarding household food purchases and factors that may impact food purchase decisions from a nationally representative sample of US households(29). A multistage sample design was used to obtain the FoodAPS sample of households(29).
A total of 14 317 individuals from 4826 households participated in FoodAPS(29). The main food shopper or meal planner of each household was selected as the primary respondent for the survey and provided information regarding household demographic characteristics, income, employment status and food security status(29). All household members were asked to document detailed information regarding all food acquisitions over a 7 d period, regardless if foods were consumed or not(29). Each purchasing event was classified into two mutually exclusive groups, as: (i) grocery purchases, i.e. all foods acquired for at-home consumption; and (ii) away-from-home purchases, i.e. all foods acquired and consumed while outside the home(29). In cases where information on the quantities of foods acquired were missing, the Economic Research Service (ERS) imputed estimated quantities based on information about food items, the stores from which they were acquired and household characteristics(30). The methodology for imputing missing quantities is described in detail elsewhere(30).
Analytical sample
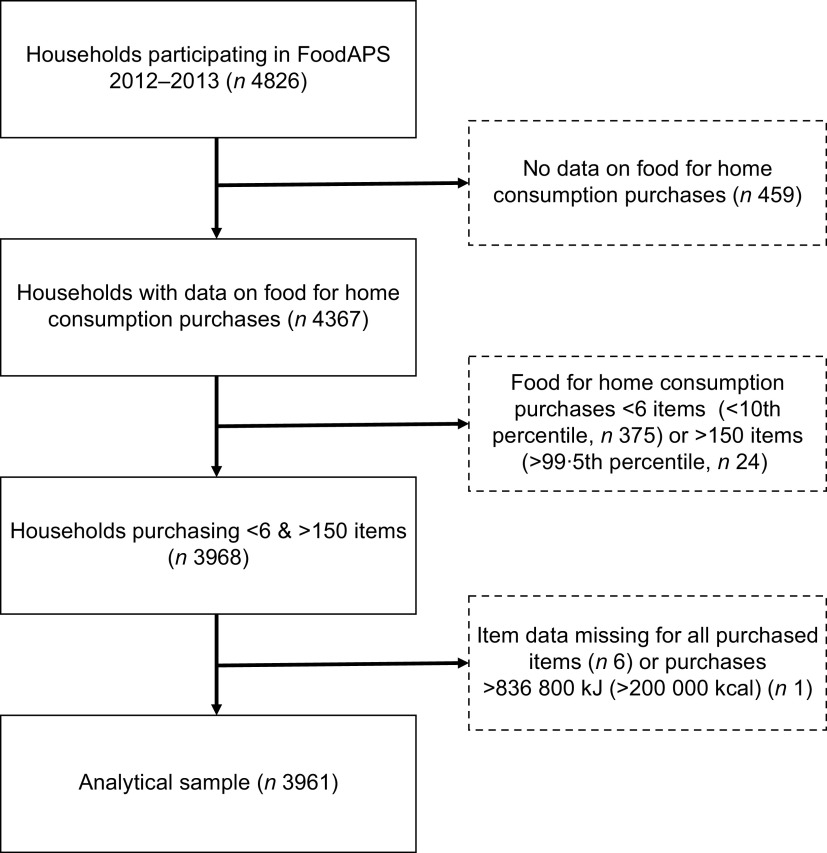
All households with data regarding grocery purchases were eligible to be included in the current study (n 4367). Households reporting grocery purchases <6 items (<10th percentile, n 375) or >150 items (>99·5th percentile, n 24) were excluded as purchases were considered unlikely to be representative of usual grocery purchases. Additionally, we excluded six households purchasing only unidentified items and one household identified as an outlier, as total energy purchased was >15 times greater compared with the household purchasing the second greatest amount of energy (11 367 204 v. 743 279 kJ (2 716 827 v. 177 648 kcal)). A total of 3961 households were included in the final analytical sample. A flowchart of the creation of the analytical sample is presented in Fig. 1.
Fig. 1.
Creation of the analytical sample for the current study from the National Household Food Acquisition and Purchase Survey 2012–2013 (FoodAPS)
Determination of level of processing of purchased items
All recorded food items were classified based on the extent and purpose of the industrial food processing applied, in accordance with the NOVA food classification(31). NOVA distinguishes four mutually exclusive levels of processing: (i) ‘unprocessed or minimally processed foods’ including fresh, dry or frozen plant and animal foods; (ii) ‘processed culinary ingredients’ including table sugar, oils, fats, salt and other constituents used in kitchens to make culinary preparations; (iii) ‘processed foods’ including foods such as canned fish and vegetables, simple breads and artisanal cheeses which are manufactured by adding processed culinary ingredients to unprocessed or minimally processed foods; and (iv) ‘ultra-processed food and drink products’, which are industrial formulations made with no or minimal whole foods and produced with substances extracted from foods or synthesized in laboratories such as dyes, flavourings and preservatives, often using processing techniques with no domestic equivalent(31). All items were further classified into thirty-four mutually exclusive subgroups. The online supplementary material, Supplemental Table S1, describes each NOVA processing level and lists the subgroups included in each level.
We classified foods by considering: (i) the US Department of Agriculture main food description and additional food description of food codes; and (ii) the ERS food group. The ERS food group classification captures level of processing and convenience of foods and provides information regarding the exact form in which each item was acquired (e.g. fresh, frozen, canned or further processed into a prepared dish)(32). ERS food group assignation is based on both the item description provided by the participant and the item information in the Information Resources, Inc. database(32). We used the ERS food groups to identify processing level of food items that could be bought in multiple forms and processed to various degrees. The ERS food groups were primarily used to distinguish between 100 % fruit and vegetable juices and juices with added sugar; to differentiate fresh/frozen from canned vegetables, fruits, legumes, meat and fish; and to discriminate between store-prepared ready-to-eat meals and industrially manufactured frozen, canned and packaged meals. In cases of conflicting information regarding processing level, we gave priority to the ERS food group over food code information, as food codes that accurately reflect all properties of the food item were not available for all reported items. Two authors independently reviewed the classification of each item. Utilizing data regarding all household grocery purchases, we calculated the relative contribution of each NOVA category to the total energy acquired by each household (percentage of energy; %E).
Healthy Eating Index-2015
Diet quality of grocery purchases was evaluated using the HEI-2015. The HEI was developed in 1995 by the US Department of Agriculture and is updated every five years to reflect current national dietary recommendations(33,34). The HEI-2015 is comprised of nine adequacy and four moderation component scores, the latter being reverse coded(35). The component scores are summed to determine the total HEI-2015 score, which has a maximum score of 100. Higher values indicate better diet quality.
Publicly available SAS code from the Division of Cancer Control and Population Sciences of the National Cancer Institute was used to calculate the HEI-2015 total score and its component scores for the grocery purchases of each household(36). Participating households were categorized into three groups of HEI-2015 total score: <40, 40–59 and ≥60. The cut-offs were established based on the sample distribution in order to ensure a sufficient number of households in each score group. The grading system for the HEI-2015 recommended in the literature categorizes scores from A (>90) to F (<60)(37). As only 26·8 % of households in the analytical sample had a HEI-2015 total score >60, this grading system would not allow us to differentiate between varying diet quality in the majority of the sample. We therefore chose to use the data-driven approach outlined above.
Covariates
Potential covariates were selected based on the literature to be tested in univariate models. Covariates of interest included age of the primary respondent, race of primary respondent (categorized as White, Black, Hispanic and Other race), highest education level in household (categorized as less than high school, high-school degree or some college, bachelor’s degree and above), any smoker in the household (yes or no), participation in the Supplemental Nutrition Assistance Program (SNAP; yes or no), benefits from the Special Supplemental Nutrition Program for Woman, Infants, and Children (WIC; yes or no) and family income-to-poverty ratio (continuous)(38,39). The number of people in the household (continuous), number of children under 18 years in the household (continuous), census region (categorized as Northeast, Midwest, South, West) and household location (categorized as rural or urban) were also considered potentially relevant covariates.
Statistical analysis
Descriptive statistics (means and frequencies) for household characteristics and food purchases were calculated for the full sample and according to HEI-2015 score group. Differences between household characteristics and food acquisitions according to HEI-2015 score group were determined by Pearson’s χ2 test for categorical variables, and by unadjusted linear regression, treating HEI-2015 score group as an ordinal variable, for continuous variables.
Mean total and component HEI-2015 scores and associated standard errors were computed for tertiles of ultra-processed food purchases (%E) by unadjusted linear regression, treating tertile of ultra-processed food purchases as an ordinal variable. Unadjusted and multivariable linear regression analysis was used to determine the association between household purchases of ultra-processed foods and processed foods (%E; continuous), respectively, and HEI-2015 total score (continuous). Potential confounders were included separately in the unadjusted model and were retained in the final model if they changed the coefficients of the main exposures by >10 %, as previously published(40) or if theoretically important based on the previous literature. The final multivariable model was adjusted for race of the primary respondent, number of people in the household, family income-to-poverty ratio, highest education level in household, SNAP participation and any smoker in the household. The exposure variables (ultra-processed foods and processed foods) were included in the same model in order to determine the effect of each exposure independent of the other. Unadjusted linear regression was used to determine mean differences in the most commonly purchased foods (%E) within each NOVA processing level: (i) between households in the top tertile of ultra-processed food purchases (≥67·9 %E) with HEI-2015 total score <40 and ≥60, respectively; and (ii) between households in the bottom tertile of ultra-processed food purchases (<48·4 %E) with HEI-2015 total score <40 and ≥60, respectively.
All analyses were performed using the statistical software package Stata/SE version 14.0 and used the FoodAPS sample weights to account for oversampling of certain populations, non-response and population coverage. The Taylor series linearization variance approximation procedure was used to account for the complex sample design of FoodAPS in the variance estimation. Statistical significance was set to α < 0·05.
Results
Sample characteristics
Household characteristics of the analytical sample, overall and according to HEI-2015 total score groups, are presented in Table 1. Primary respondents were primarily non-Hispanic White (70·3 %) and had attended some college or obtained an associate’s degree (53·4 %). Mean HEI-2015 score was 54·7 (se 0·4). Households with HEI-2015 total score ≥60 were less likely to participate in SNAP (6·3 v. 21·0 %, P < 0·001) and WIC (19·4 v. 33·3 % of WIC-eligible households, P = 0·038), less likely to be located in a rural census tract (28·3 v. 40·8 %, P = 0·004), and the primary respondent was more likely to have a bachelor’s or higher degree (55·3 v. 23·0 %, P < 0·001), compared with households with HEI-2015 score <40.
Table 1.
Characteristics of households participating in the National Household Food Acquisition and Purchase Survey 2012–2013 (n 3961), according to Healthy Eating Index-2015 (HEI-2015) total score
| Characteristic | All (n 3961) |
HEI-2015 < 40 (n 702) |
HEI-2015 = 40–59 (n 2195) |
HEI-2015 ≥ 60 (n 1064) |
P | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean or % | se | Mean or % | se | Mean or % | se | Mean or % | se | ||
| Number of people in HH | 2·5 | 0·0 | 2·6 | 0·1 | 2·6 | 0·1 | 2·3 | 0·0 | 0·043 |
| Number of children (<18 years) in HH | 0·7 | 0·0 | 0·7 | 1·1 | 0·7 | 1·2 | 0·5 | 0·9 | 0·002 |
| Age of primary respondent (years) | 50·6 | 0·5 | 48·4 | 1·4 | 50·4 | 0·7 | 51·8 | 0·6 | <0·001 |
| Race of primary respondent (%) | 0·003 | ||||||||
| Non-Hispanic White | 70·3 | – | 69·5 | – | 69·7 | – | 71·6 | – | |
| Non-Hispanic Black | 9·9 | – | 11·7 | – | 12·0 | – | 5·9 | – | |
| Hispanic/Other race | 19·8 | – | 18·8 | – | 18·4 | – | 22·5 | – | |
| Highest education level in HH (%) | <0·001 | ||||||||
| Less than high school | 6·0 | – | 7·8 | – | 6·8 | – | 4·0 | – | |
| High-school degree or some college | 53·4 | – | 69·3 | – | 57·3 | – | 40·7 | – | |
| Bachelor’s degree and above | 40·5 | – | 23·0 | – | 35·8 | – | 55·3 | – | |
| Any smoker in the HH (%) | 29·5 | – | 46·8 | – | 33·2 | – | 16·4 | – | <0·001 |
| SNAP participation (%) | 12·7 | – | 21·0 | – | 14·7 | – | 6·3 | – | <0·001 |
| WIC participation* (%) | 27·0 | – | 33·3 | – | 29·8 | – | 19·4 | – | 0·038 |
| Family income-to-poverty ratio (%) | <0·001 | ||||||||
| <130 % | 17·0 | – | 27·2 | – | 18·1 | – | 10·9 | – | |
| 130–349 % | 41·1 | – | 46·8 | – | 42·6 | – | 36·4 | – | |
| ≥350 % | 42·0 | – | 26·0 | – | 39·4 | – | 52·7 | – | |
| Census region (%) | 0·001 | ||||||||
| Northeast | 15·8 | – | 15·0 | – | 14·6 | – | 18·0 | – | |
| Midwest | 31·4 | – | 27·3 | – | 33·6 | – | 29·4 | – | |
| South | 34·7 | – | 44·1 | – | 35·6 | – | 29·4 | – | |
| West | 18·2 | – | 13·6 | – | 16·3 | – | 23·3 | – | |
| HH located in rural census tract (%) | 34·6 | – | 40·8 | – | 37·0 | – | 28·3 | – | 0·004 |
HH, household; SNAP, Supplemental Nutrition Assistance Program; WIC, Special Supplemental Nutrition Program for Woman, Infants, and Children.
All values are means with their se unless otherwise noted. P values were estimated by unadjusted linear regression, treating HEI-2015 group as an ordinal variable, for continuous variables, and by Pearson’s χ2 for categorical variables. Missing values: SNAP participation (n 1), anyone in HH receives benefits from WIC (n 3100), race of primary respondent (n 4).
Of WIC-eligible households (n 861).
Household grocery purchases according to Healthy Eating Index-2015 score group
As shown in Table 2, ultra-processed foods provided 55·8 %E of grocery purchases, while minimally processed foods provided 28·4 %E. The energy share of ultra-processed foods was greater among households with a HEI-2015 total score <40 compared with ≥60 (67·3 v. 47·4 %E, P < 0·001).
Table 2.
Characteristics of household grocery purchases in the National Household Food Acquisition and Purchase Survey 2012–2013 (n 3961), according to Healthy Eating Index-2015 (HEI-2015) total score
| Dietary factor | All (n 3961) |
HEI-2015 < 40 (n 702) |
HEI-2015 = 40–59 (n 2195) |
HEI-2015 ≥ 60 (n 1064) |
P | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | se | Mean | se | Mean | se | Mean | se | ||
| Total energy purchased (kJ) | 149 016·9 | 3056·4 | 135 021·9 | 7105·7 | 156 357·8 | 4470·2 | 143 133·0 | 5034·6 | 0·985 |
| Total energy purchased (kcal) | 35 615·9 | 730·5 | 32 271·0 | 1698·3 | 37 370·4 | 1068·4 | 34 209·6 | 1203·3 | 0·985 |
| Relative energy (%E) purchased as | |||||||||
| Unprocessed/minimally processed foods | 28·4 | 0·4 | 19·1 | 1·2 | 25·7 | 0·6 | 36·6 | 0·8 | <0·001 |
| Processed culinary ingredients | 6·6 | 0·3 | 6·7 | 0·6 | 7·4 | 0·4 | 5·3 | 0·5 | <0·001 |
| Processed foods | 9·2 | 0·3 | 6·9 | 0·8 | 8·9 | 0·4 | 10·8 | 0·6 | <0·001 |
| Ultra-processed foods and drinks | 55·8 | 0·6 | 67·3 | 1·2 | 58·0 | 0·7 | 47·4 | 1·1 | <0·001 |
| HEI-2015 scores (maximum score)* | |||||||||
| Total score (100) | 54·7 | 0·4 | 34·5 | 0·3 | 50·5 | 0·2 | 69·6 | 0·4 | <0·001 |
| Total fruit (5) | 2·5 | 0·1 | 1·1 | 0·1 | 2·1 | 0·1 | 3·8 | 0·1 | <0·001 |
| Whole fruit (5) | 2·8 | 0·1 | 1·1 | 0·1 | 2·4 | 0·1 | 4·2 | 0·1 | <0·001 |
| Total vegetables (5) | 2·9 | 0·0 | 1·6 | 0·1 | 2·8 | 0·0 | 3·8 | 0·1 | <0·001 |
| Greens and beans (5) | 1·9 | 0·1 | 0·5 | 0·1 | 1·5 | 0·1 | 3·1 | 0·1 | <0·001 |
| Whole grains (10) | 2·8 | 0·1 | 1·0 | 0·2 | 2·3 | 0·1 | 4·4 | 0·2 | <0·001 |
| Dairy (10) | 5·3 | 0·1 | 4·7 | 0·1 | 5·3 | 0·1 | 5·6 | 0·1 | <0·001 |
| Total protein foods (5) | 3·6 | 0·0 | 3·1 | 0·1 | 3·5 | 0·1 | 3·9 | 0·1 | <0·001 |
| Seafood and plant protein (5) | 2·4 | 0·1 | 1·0 | 0·1 | 2·1 | 0·1 | 3·4 | 0·1 | <0·001 |
| Fatty acid ratio (10) | 5·0 | 0·1 | 2·7 | 0·2 | 4·5 | 0·2 | 6·7 | 0·1 | <0·001 |
| Refined grains (10) | 6·8 | 0·1 | 4·8 | 0·3 | 6·5 | 0·2 | 8·2 | 0·1 | <0·001 |
| Sodium (10) | 6·7 | 0·1 | 4·6 | 0·3 | 6·5 | 0·1 | 7·9 | 0·1 | <0·001 |
| Added sugars (10) | 6·2 | 0·1 | 4·4 | 0·3 | 5·8 | 0·1 | 7·6 | 0·1 | <0·001 |
| Saturated fats (10) | 5·7 | 0·1 | 3·9 | 0·2 | 5·4 | 0·1 | 7·0 | 0·2 | <0·001 |
%E, percentage of energy.
Higher scores of the HEI-2015 total and component scores indicate higher diet quality.
Healthy Eating Index-2015 total and component scores according to ultra-processed food purchases
HEI-2015 total and component scores according household grocery purchases of ultra-processed foods (%E; tertiles) are presented in Table 3. On average, households purchasing the least ultra-processed foods had 10·7 points higher HEI-2015 total scores than those purchasing the most ultra-processed foods (HEI-2015 total score of 59·6 v. 48·9, P < 0·001). Households purchasing the highest proportion of ultra-processed foods were furthest from meeting the recommendations of the Dietary Guidelines for Americans 2015–2020 for all food groups and nutrients except whole grains, dairy, fatty acid ratio and saturated fats. HEI-2015 component scores for dairy, fatty acid ratio and saturated fat did not differ according to tertile of ultra-processed food purchases.
Table 3.
Health Eating Index-2015 (HEI-2015) total and component scores according to relative energy contribution of ultra-processed food energy to household grocery purchases (percentage of energy; %E) in the National Household Food Acquisition and Purchase Survey 2012–2013, n 3961
| Tertile of ultra-processed food purchases (%E) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| All (n 3961) |
1 (≤48·4 %) (n 1321) |
2 (48·4–67·9 %) (n 1320) |
3 (≥67·9 %) (n 1320) |
||||||
| HEI-2015 scores (maximum score) | Mean | se | Mean | se | Mean | se | Mean | se | P |
| Total fruit (5) | 2·5 | 0·1 | 2·7 | 0·1 | 2·7 | 0·1 | 2·1 | 0·1 | <0·001 |
| Whole fruit (5) | 2·8 | 0·1 | 3·1 | 0·1 | 2·9 | 0·1 | 2·4 | 0·1 | <0·001 |
| Total vegetables (5) | 3·0 | 0·0 | 3·3 | 0·1 | 3·1 | 0·1 | 2·4 | 0·1 | <0·001 |
| Greens and beans (5) | 1·9 | 0·1 | 2·4 | 0·1 | 1·9 | 0·1 | 1·3 | 0·1 | <0·001 |
| Whole grains (10) | 2·8 | 0·1 | 2·5 | 0·2 | 2·8 | 0·2 | 3·2 | 0·2 | 0·002 |
| Dairy (10) | 5·3 | 0·1 | 5·1 | 0·1 | 5·7 | 0·1 | 5·1 | 0·1 | 0·836 |
| Total protein foods (5) | 3·6 | 0·0 | 3·8 | 0·1 | 3·8 | 0·1 | 3·2 | 0·1 | <0·001 |
| Seafood and plant protein (5) | 2·4 | 0·1 | 2·7 | 0·1 | 2·4 | 0·1 | 2·0 | 0·0 | <0·001 |
| Fatty acid ratio (10) | 5·0 | 0·1 | 5·2 | 0·2 | 4·6 | 0·1 | 5·1 | 0·2 | 0·616 |
| Refined grains (10) | 6·8 | 0·1 | 7·8 | 0·1 | 6·8 | 0·2 | 5·8 | 0·2 | <0·001 |
| Sodium (10) | 6·7 | 0·1 | 7·7 | 0·2 | 6·6 | 0·1 | 5·6 | 0·2 | <0·001 |
| Added sugars (10) | 6·2 | 0·1 | 7·5 | 0·1 | 6·1 | 0·1 | 4·7 | 0·2 | <0·001 |
| Saturated fats (10) | 5·7 | 0·1 | 5·6 | 0·2 | 5·5 | 0·1 | 6·1 | 0·1 | 0·066 |
| Total score (maximum score 100) | 54·7 | 0·4 | 59·6 | 0·6 | 54·9 | 0·8 | 48·9 | 0·2 | <0·001 |
P values were calculated by unadjusted linear regression using tertile of ultra-processed food purchases as the independent variable (ordinal) and HEI-2015 score as the dependent variable.
Association between food processing level and Healthy Eating Index-2015 total score
A 10 % increase of purchased energy from ultra-processed foods was associated with a 1·8-point reduction in HEI-2015 total score, controlling for purchases of processed foods (%E), race of the primary respondent, number of people in the household, family income-to-poverty ratio, highest education level in household, SNAP participation and any smoker in the household (β = −1·8, 95 % CI −2·0, −1·5, data not shown). Purchases of processed foods were not associated with HEI-2015 total score in unadjusted (β = −0·3, 95 % CI −0·3, 1·0) and multivariable linear regression analyses (β = −0·1, 95 % CI −0·4, 0·7).
Commonly purchased foods within each NOVA processing level
Households with HEI-2015 total score ≥60 (n 1064) included households both in the lowest (<48·4 %E; n 515) and the highest tertile (≥67·9 %E; n 163) of ultra-processed food purchases, yet the average HEI-2015 total score was significantly higher among those in the lowest tertile of ultra-processed food purchases (71·3 v. 67·0, P < 0·001, data not shown). The energy contribution of the foods most commonly purchased by households in the top tertile of ultra-processed food purchases (≥67·9 %E) with HEI-2015 total score <40 and ≥60, respectively, and households in the bottom tertile of ultra-processed food purchases (<48·4 %E) with HEI-2015 total score <40 and ≥60, respectively, is presented in Fig. 2.
Fig. 2.
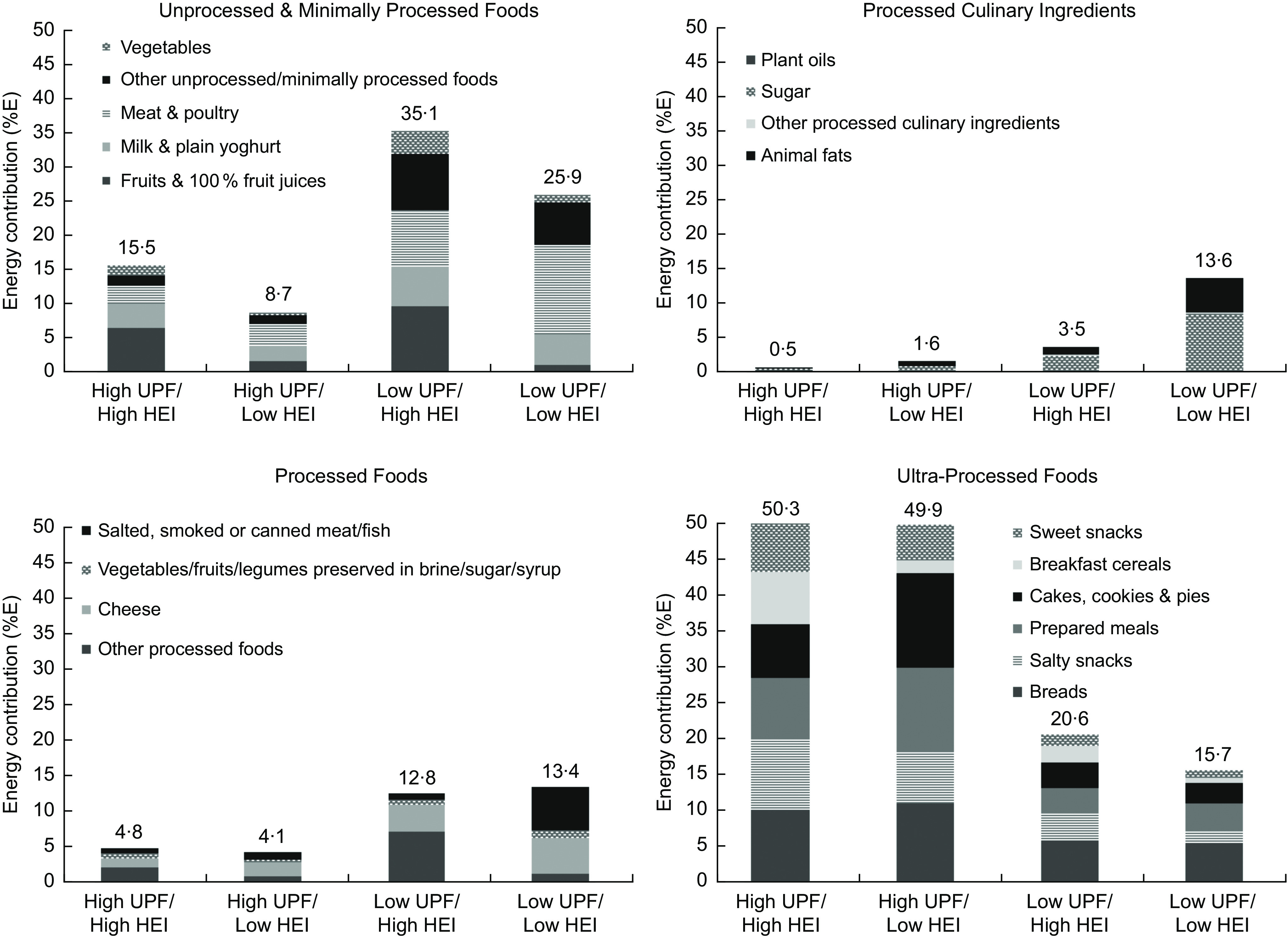
Relative energy contribution (percentage of energy; %E) of the six most commonly purchased foods, within each NOVA processing level, among households with high ultra-processed food (UPF) purchases/high Healthy Eating Index-2015 (HEI-2015; n 163, 4·1 %), high UPF purchases/low HEI-2015 (n 385, 9·7 %), low UPF purchases/high HEI-2015 (n 515, 13·0 %), and low UPF purchases/low HEI-2015 (n 135, 3·4 %), respectively, in the National Household Food Acquisition and Purchase Survey 2012–2013. High and low UPF purchases defined as ≥67·9 and <48·4 %E from UPF, respectively; high and low HEI-2015 defined as total score ≥60 and <40, respectively. Other minimally processed foods include nuts and seeds (unsalted); yeast; dried fruits (without added sugars) and vegetables; non-presweetened, non-whitened, non-flavoured coffee and tea; coconut water and meat; flours; tapioca. Other processed foods include salted or sugared nuts and seeds; peanut, sesame, cashew and almond butter or spread; beer and wine. Prepared meals include frozen, canned and shelf-stable meals
Households in the top tertile of ultra-processed food purchases with a HEI-2015 total score ≥60 purchased significantly more minimally processed fruits and vegetables, milk, plain yoghurt and ultra-processed breakfast cereals than households with equally high ultra-processed food purchases yet HEI-2015 total score <40 (n 385, P < 0·05). Households with high ultra-processed food purchases and a HEI-2015 total score ≥60 also acquired less animal fats; cheese; ultra-processed cakes, cookies and pies; prepared meals; as well as less ice cream (not shown) and carbonated soft drinks (not shown; P < 0·02). Conversely, households in the bottom tertile of ultra-processed food purchases with a HEI-2015 total score <40 (n 135) acquired significantly less minimally processed fruits and vegetables, ultra-processed breakfast cereals and salty snacks but more animal fats, sugar, ultra-processed desserts (not shown) and carbonated soft drinks (not shown) than households with equally low ultra-processed food purchases and HEI-2015 total score ≥60 (P < 0·05).
The relative energy contribution of all foods purchased by households in the top tertile of ultra-processed food purchases (≥67·9 %E) with HEI-2015 total score <40 and ≥60, respectively, and households in the bottom tertile of ultra-processed food purchases (<48·4 %E) with HEI-2015 total score <40 and ≥60, respectively, is presented in the online supplementary material, Supplemental Table S2.
Discussion
In 2012–2013, ultra-processed foods provided the majority of energy in the average US grocery cart (55·8 %E). Higher purchases of ultra-processed foods were associated with lower overall diet quality, defined by the HEI-2015. At similar levels of ultra-processed food purchases, households purchasing more minimally processed fruits, vegetables, roots and legumes had higher diet quality than households purchasing less of these foods.
To our knowledge, previous studies have not assessed the association between NOVA processing levels and diet quality of household purchases, defined by the HEI-2015. Poti et al. compared the content of saturated fat, sugar and sodium of consumer packaged goods across processing levels using data from the 2000–2012 Nielsen Homescan Panel(18). It was observed that 94·7 % of ‘highly processed foods’ (defined as multi-ingredient formulated mixtures processed to the extent that they are no longer recognizable as their original plant or animal source) exceeded the recommendation for saturated fat (>10 %E) of the Dietary Guidelines for Americans 2010, while 94·5 % exceeded the recommendation for sugar (>15 %E) and 96·3 % exceeded the recommendation for sodium (>2400 mg/8368 kJ (2000 kcal)). A significantly higher proportion of highly processed foods (60 %) and ready-to-eat foods (27·1 %) exceeded the Dietary Guidelines for Americans 2010 limits for saturated fat, sugar and sodium, simultaneously, compared with less processed foods (5·6 %) and foods requiring cooking/preparation (4·9 %)(18). These findings are in line with our results for the HEI-2015 added sugar and sodium component scores. It is noteworthy, however, that saturated fat component scores did not differ according to processing level of food purchases in the current study. This may be because we assessed the average saturated fat content of all foods purchased by households, i.e. the whole grocery basket, rather than individual products. In our sample, households in the top tertile of ultra-processed foods purchased the least animal fats, such as butter, lard and cream, which are high in saturated fats.
Our results are consistent with previous international and national studies reporting that diets higher in ultra-processed foods tend to be less nutritious(21–27). Among participants in the National Health and Nutrition Examination Survey (NHANES) 2009–2010, a linear inverse association was found between consumption of ultra-processed foods (%E) and a principal component analysis-derived nutrient-balanced diet pattern high in fibre, potassium, magnesium and vitamin C, and low in saturated fat and added sugars(21). The average dietary content of protein, fibre, vitamins A, C, D and E, zinc, potassium, phosphorus, magnesium and calcium decreased significantly with greater intake of ultra-processed foods (%E), while carbohydrate, added sugar and saturated fat contents increased(21). Studies assessing diet quality in relation to dietary intake of ultra-processed foods in Canada, Brazil, Chile and France report similar findings(22–27). Of note, all of the studies examining saturated fat found that intake of saturated fat increased with greater intake of ultra-processed foods(22,23,25,26). The discrepancy between these results and the findings of the current study may be because we considered grocery purchases only and did not account for ultra-processed foods consumed away from home that may be high in saturated fat, such as fast foods.
It is noteworthy that households purchasing the most ultra-processed foods achieved the highest component scores for whole grains, which is a source of dietary fibre. Previous studies have observed an inverse association between ultra-processed food consumption and fibre intake(21–23,25,26). The greater dietary content of whole grains with higher purchases of ultra-processed foods in our sample may reflect greater acquisition of ultra-processed wholegrain products such as breakfast cereals, granola bars and popcorn. These products are often also high in sugar and/or sodium(18) for which the net effect on overall diet quality is uncertain. Conversely, the higher intake of fibre associated with diets lower in ultra-processed foods in previous studies may reflect greater intakes of other sources of dietary fibre, such as minimally processed legumes, fruits, vegetables, nuts and seeds.
Taken together, our findings, along with previous research using purchasing and consumption data, suggest that the energy share of minimally processed and ultra-processed foods in the diet may influence diet quality. Specifically, increasing the proportion of minimally processed plant foods and reducing the share of ultra-processed foods in the diet seems to be associated with better diet quality. Our results also highlight the importance of healthful food choices within each processing level. In particular, increasing minimally processed fruits, vegetables and legumes and reducing animal fats (processed culinary ingredients) as well as sugary ultra-processed foods, such as cakes, cookies, ice cream and carbonated soft drinks, in the diet may improve diet quality, regardless of the total energy contribution of ultra-processed foods.
Some limitations should be noted. FoodAPS does not have data regarding household consumption and waste of the purchased foods, and hence we cannot not make inferences about individual dietary intake. However, our estimates of food purchases according to processing level are similar to previously published estimates in NHANES 2009–2010 of the mean dietary share from each processing level(21). For example, minimally processed foods provided 30·2 %E and ultra-processed foods provided 57·5 %E in NHANES 2009–2010 (v. 28·4 and 55·8 %E, respectively, in FoodAPS). Furthermore, a considerable proportion of purchased items lacked information on quantity, for which the ERS added imputed estimated quantities(30). Nevertheless, the imputed values have been validated by the ERS(30). Furthermore, we did not assess energy adequacy. The HEI-2015 uses a density approach and defines diet quality based on food groups and nutrients per 4184 kJ (1000 kcal). It is therefore unknown if participating households acquired an insufficient or excessive amount of energy in relation to their energy needs. Misclassification of foods may have occurred for items for which insufficient details were available to determine processing level with certainty. Nevertheless, the use of the ERS food groups enabled greater precision in the determination of processing level, minimizing the risk of misclassification. Finally, we only assessed household purchases for home consumption and do not know if households differed with regard to the amount and nutritional quality of foods consumed away from home.
Our study also has several strengths. We used comprehensive food purchasing data collected from a nationally representative sample of US households. As a result, the external validity of our findings is likely to be high. Processing level was determined by NOVA, a comprehensive, coherent and specific classification framework that has been recommended by the FAO(41). FoodAPS collects data regarding the exact form in which foods were purchased, thus reducing the risk of misclassification of processing level(32). Finally, the use of purchasing data constitutes another advantage of the current study, as it mitigates the reporting bias associated with assessment of food consumption. Yet, it is worth noting that our results are consistent with previously published NOVA contributions estimated using dietary intake data(21).
In summary, our results indicate that processing level defined by the NOVA framework is useful to predict diet quality, defined according to the Dietary Guidelines for Americans 2015–2020. However, healthful food choices within each processing level are also of relevance for diet quality, e.g. choosing vegetable oils over animal fats and unsweetened over sugary breakfast cereals. Recommendations to consume more healthful unprocessed/minimally foods and less ultra-processed foods may enhance the current food-based Dietary Guidelines for Americans. Future studies should assess if dietary guidelines that combine information on processing level and type of foods facilitate healthier food choices and improve diet quality.
Acknowledgements
Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. B.S.S. was a research fellow of Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES; grant number 88881.131991/2016-01), as a visiting scholar at New York University School of Medicine, USA. CAPES had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: F.J. and B.S.S. are joint first authors. N.P., F.J., B.S.S., M.V. and A.D. developed the overall research plan; F.J., E.M.-S. and J.L. provided essential materials; B.S.S. performed the statistical analysis; F.J. and B.S.S. wrote the paper; N.P., M.V., A.D., E.M.-S. and J.L. revised the manuscript for important intellectual content. All authors have read and approved the final manuscript and take full responsibility for the final content. Ethics of human subject participation: This study involved secondary data analysis and no personally identifiable information about individuals was available to the researchers. Ethical approval was therefore not required.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980019001344.
click here to view supplementary material
References
- 1.Wilson MM, Reedy J & Krebs-Smith SM (2016) American diet quality: where it is, where it is heading, and what it could be. J Acad Nutr Diet 116, 302–310.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miller PE, Reedy J, Kirkpatrick SI et al. (2015) The United States food supply is not consistent with dietary guidance: evidence from an evaluation using the Healthy Eating Index-2010. J Acad Nutr Diet 115, 95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bureau of Labor Statistics, US Department of Labor (2017) Consumer Price Index – December 2017 (press release). https://www.bls.gov/news.release/archives/cpi_01122018.pdf (accessed January 2018).
- 4.Appelhans BM, French SA, Tangney CC et al. (2017) To what extent do food purchases reflect shoppers’ diet quality and nutrient intake? Int J Behav Nutr Phys Act 14, 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grant E, Gearry RB, Wilson R et al. (2017) Home availability of fruit and vegetables and obesogenic foods as an indicator of nutrient intake in 50 year olds from Canterbury, New Zealand. Asia Pac J Clin Nutr 26, 524–530. [DOI] [PubMed] [Google Scholar]
- 6.Couch SC, Glanz K, Zhou C et al. (2014) Home food environment in relation to children’s diet quality and weight status. J Acad Nutr Diet 114, 1569–1579.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alber JM, Green SH & Glanz K (2018) Perceived and observed food environments, eating behaviors, and BMI. Am J Prev Med 54, 423–429. [DOI] [PubMed] [Google Scholar]
- 8.Cullen KW, Baranowski T, Owens E et al. (2003) Availability, accessibility, and preferences for fruit, 100% fruit juice, and vegetables influence children’s dietary behavior. Health Educ Behav 30, 615–626. [DOI] [PubMed] [Google Scholar]
- 9.Ding D, Sallis JF, Norman GJ et al. (2012) Community food environment, home food environment, and fruit and vegetable intake of children and adolescents. J Nutr Educ Behav 44, 634–638. [DOI] [PubMed] [Google Scholar]
- 10.Granner ML & Evans AE (2011) Variables associated with fruit and vegetable intake in adolescents. Am J Health Behav 35, 591–602. [DOI] [PubMed] [Google Scholar]
- 11.Hanson NI, Neumark-Sztainer D, Eisenberg ME et al. (2005) Associations between parental report of the home food environment and adolescent intakes of fruits, vegetables and dairy foods. Public Health Nutr 8, 77–85. [DOI] [PubMed] [Google Scholar]
- 12.Neumark-Sztainer D, Wall M, Perry C et al. (2003) Correlates of fruit and vegetable intake among adolescents. Findings from Project EAT. Prev Med 37, 198–208. [DOI] [PubMed] [Google Scholar]
- 13.Liberato SC, Bailie R & Brimblecombe J (2014) Nutrition interventions at point-of-sale to encourage healthier food purchasing: a systematic review. BMC Public Health 14, 919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adam A & Jensen JD (2016) What is the effectiveness of obesity related interventions at retail grocery stores and supermarkets? A systematic review. BMC Public Health 16, 1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ludwig DS (2011) Technology, diet, and the burden of chronic disease. JAMA 305, 1352–1353. [DOI] [PubMed] [Google Scholar]
- 16.Lustig RH (2017) Processed food – an experiment that failed. JAMA Pediatr 171, 212–214. [DOI] [PubMed] [Google Scholar]
- 17.Monteiro CA, Moubarac JC, Cannon G et al. (2013) Ultra-processed products are becoming dominant in the global food system. Obes Rev 14, Suppl. 2, 21–28. [DOI] [PubMed] [Google Scholar]
- 18.Poti JM, Mendez MA, Ng SW et al. (2015) Is the degree of food processing and convenience linked with the nutritional quality of foods purchased by US households? Am J Clin Nutr 101, 1251–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weaver CM, Dwyer J, Fulgoni VL 3rd et al. (2014) Processed foods: contributions to nutrition. Am J Clin Nutr 99, 1525–1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dwyer JT, Fulgoni VL, Clemens RA et al. (2012) Is ‘processed’ a four-letter word? The role of processed foods in achieving dietary guidelines and nutrient recommendations. Adv Nutr 3, 536–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martinez Steele E, Popkin BM, Swinburn B et al. (2017) The share of ultra-processed foods and the overall nutritional quality of diets in the US: evidence from a nationally representative cross-sectional study. Popul Health Metr 15, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moubarac JC, Batal M, Louzada ML et al. (2017) Consumption of ultra-processed foods predicts diet quality in Canada. Appetite 108, 512–520. [DOI] [PubMed] [Google Scholar]
- 23.Adams J & White M (2015) Characterisation of UK diets according to degree of food processing and associations with socio-demographics and obesity: cross-sectional analysis of UK National Diet and Nutrition Survey (2008–12). Int J Behav Nutr Phys Act 12, 160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Louzada ML, Martins AP, Canella DS et al. (2015) Impact of ultra-processed foods on micronutrient content in the Brazilian diet. Rev Saude Publica 49, 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Julia C, Martinez L, Alles B et al. (2018) Contribution of ultra-processed foods in the diet of adults from the French NutriNet-Sante study. Public Health Nutr 21, 27–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Batal M, Johnson-Down L, Moubarac JC et al. (2018) Quantifying associations of the dietary share of ultra-processed foods with overall diet quality in First Nations peoples in the Canadian provinces of British Columbia, Alberta, Manitoba and Ontario. Public Health Nutr 21, 103–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cediel G, Reyes M, da Costa Louzada ML et al. (2018) Ultra-processed foods and added sugars in the Chilean diet (2010). Public Health Nutr 21, 125–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eicher-Miller HA, Fulgoni VL 3rd, Keast DR (2012) Contributions of processed foods to dietary intake in the US from 2003–2008: a report of the Food and Nutrition Science Solutions Joint Task Force of the Academy of Nutrition and Dietetics, American Society for Nutrition, Institute of Food Technologists, and International Food Information Council. J Nutr 142, issue 11, 2065S–2072S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.US Department of Agriculture, Economic Research Service (2019) FoodAPS National Household Food Acquisition and Purchase Survey. https://www.ers.usda.gov/foodaps (accessed March 2019).
- 30.Mancino L, Todd JE & Scharadin B (2018) USDA’s National Household Food Acquisition and Purchase Survey: Methodology for Imputing Missing Quantities to Calculate Healthy Eating Index-2010 Scores and Sort Foods into ERS Food Groups. Technical Bulletin no. TB-1947. Washington, DC: U.S. Department of Agriculture, Economic Research Service. [Google Scholar]
- 31.Moubarac JC, Parra DC, Cannon G et al. (2014) Food classification systems based on food processing: significance and implications for policies and actions: a systematic literature review and assessment. Curr Obes Rep 3, 256–272. [DOI] [PubMed] [Google Scholar]
- 32.US Department of Agriculture, Economic Research Service (2016) National Household Food Acquisition and Purchase Survey (FoodAPS): Nutrient Coding Overview. Washington, DC: US Department of Agriculture, Economic Research Service. [Google Scholar]
- 33.Guenther PM, Reedy J & Krebs-Smith SM (2008) Development of the Healthy Eating Index-2005. J Am Diet Assoc 108, 1896–1901. [DOI] [PubMed] [Google Scholar]
- 34.Kennedy ET, Ohls J, Carlson S & Fleming K (1995) The Healthy Eating Index: design and applications. J Am Diet Assoc 95, 1103–1108. [DOI] [PubMed] [Google Scholar]
- 35.National Cancer Institute (2018) Comparing the HEI-2015, HEI-2010 & HEI-2005. https://epi.grants.cancer.gov/hei/comparing.html (accessed September 2018).
- 36.National Cancer Institute (2018) SAS Code: National Cancer Institute. https://epi.grants.cancer.gov/hei/sas-code.html (accessed September 2018).
- 37.Krebs-Smith SM, Pannucci TE, Subar AF et al. (2018) Update of the Healthy Eating Index: HEI-2015. J Acad Nutr Diet 118, 1591–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hiza HA, Casavale KO, Guenther PM et al. (2013) Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J Acad Nutr Diet 113, 297–306. [DOI] [PubMed] [Google Scholar]
- 39.Andreyeva T, Tripp AS & Schwartz MB (2015) Dietary quality of Americans by Supplemental Nutrition Assistance Program participation status: a systematic review. Am J Prev Med 49, 594–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Makarem N, Bandera EV, Lin Y et al. (2018) Consumption of sugars, sugary foods, and sugary beverages in relation to adiposity-related cancer risk in the Framingham Offspring cohort (1991–2013). Cancer Prev Res (Phila) 11, 347–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Food and Agriculture Organization of the United Nations (2015) Guidelines on the Collection of Information on Food Processing through Food Consumption Surveys. Rome: FAO. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980019001344.
click here to view supplementary material