Abstract
Objective
People who eat alone, which is becoming a new trend owing to the increasing proportion of one-person households in Korea, are more likely to become overweight and obese. Therefore, we investigated the association between having a dinner companion and BMI.
Design
A linear regression model adjusted for covariates was utilized to examine the association between having a dinner companion and BMI. Subgroup analyses were performed, stratified by age group, gender, household income, educational level and occupation.
Setting
We used the data from the Korean Health and Nutrition Examination Survey VI. Our primary independent variable was having a dinner companion while the dependent variable was BMI.
Subjects
In total, 13303 individuals, aged 20 years or over, were analysed.
Results
Compared with the solo eating group, BMI was lower in the family dinner group (β=−0·39, P<0·01) but not in the non-family dinner group (β=−0·06, P=0·67). The subgroup analysis revealed that the difference in BMI was most significant in young generations, such as those aged 20–29 years (β=−1·15, P<0·01) and 30–39 years (β=−0·78, P=0·01).
Conclusions
We found that people who eat dinner alone are more likely to become overweight and obese than those who eat with their family. This association was stronger in males and young adults than their counterparts. Considering the increasing trends in the proportion of single-person households and solo eating, appropriate intervention is needed.
Keywords: Obesity, Overweight, Eating alone, Family dinner, Commensality
Koreans used to live by a typical traditional concept of family; however, rapid industrialization and modernization have caused family disorganization over the last several decades. This phenomenon has resulted in a shift in Korea’s family structure to not only nuclear families, but also single-person households. In particular, the proportion of single-person households has been increasing over recent decades. Single-person households accounted for 15·5 % of the total Korean population in 2000, 23·9 % in 2010 and 27·2 % in 2015, and it is expected to increase to 33·3 % in 2030( 1 ). In accordance with social atmosphere changes, people’s eating patterns have also been changing.
One example of this change is the fewer number of people having family dinner. In the past, family meals were considered important( 2 ). However, the percentage of people having family dinner has decreased continuously, from 76·1 % in 2005 to 64·9 % in 2014( 3 ). As a result, a novel dining trend has emerged, with a substantial increase in people who eat alone rather than with others. Over 75 % of those who live alone reported eating dinner alone; approximately 52 % ate all three meals alone( 4 ). Furthermore, a survey reported that even 20·9 % of non-single-member households ate meals alone. Considering the health benefits of commensality, this trend may present some worrisome risks of damaging people’s health.
Commensality can influence not only mental health( 5 ) but also diet and eating patterns. In fact, several studies have reported that sharing meals can positively affect weight or BMI( 6 ). In practice, a study has shown that eating patterns differ among groups with different BMI( 7 ). Specifically, having meals as a family increases the individual’s intake of fruits and vegetables and reduces the consumption of sugar-sweetened beverages, as well as boosts the individual’s intake of a variety of vitamins/minerals and reduces the consumption of nutrient-poor foods( 8 – 11 ). On the contrary, eating alone has been reported to have negative effects on health, such as low food diversity or higher energy intake that could lead to obesity (BMI≥30·0 kg/m2) or overweight (BMI≥25·0 kg/m2)( 10 , 12 ).
The global incidence of obesity and overweight has been increasing over the past few decades and these remain the ever-rising global health concerns. A previous study reported that approximately 2 billion adults are overweight worldwide, among which 650 million are obese( 13 ). In South Korea, the incidence of overweight and obesity in adults has increased steadily from 26·0 % in 1998 to 33·2 % in 2016( 14 ). Naturally, overweight and obesity have become major health burdens in many countries, leading to about 3 million deaths worldwide every year and loss of 35 million disability-adjusted life years( 15 ). Research on factors related to obesity is crucial for its prevention. Since obesity is caused by various factors and eating patterns, it is important to investigate the possible consequences of eating alone to prevent overweight and obesity.
In the current study, we investigated the association between having a dinner companion and BMI. Of the three meals, we found that dinner would be the most suitable for our study for the following reasons: (i) a greater number of people skipped breakfast; and (ii) the percentage of people who ate lunch with family was lower than those who consumed the other two meals with family. Therefore, we decided to examine the benefits of having dinner companions for further research.
Methods
Study population
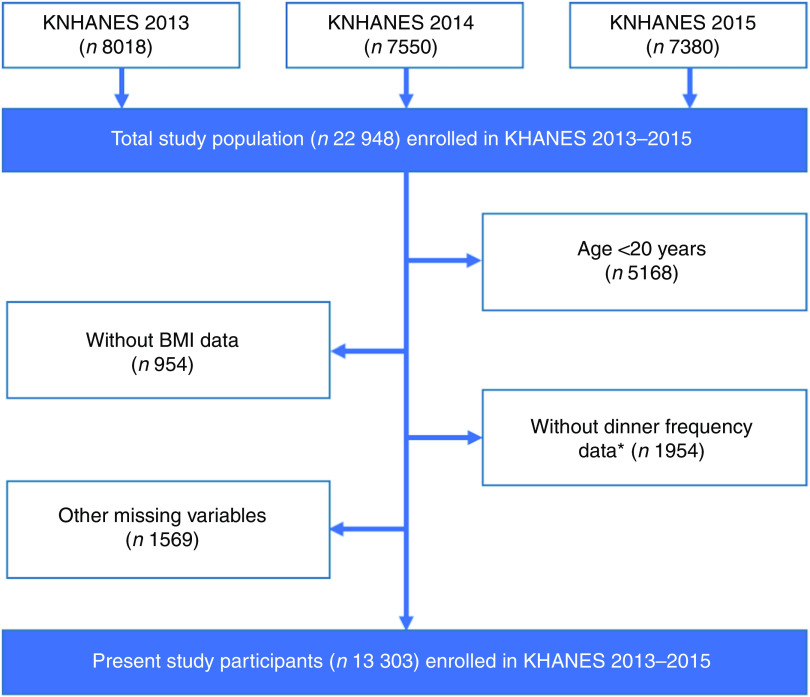
We used data from the Korean National Health and Nutrition Examination Survey VI (KNHANES VI). KNHANES is a nationwide cross-sectional study that has been performed in Korea since 1998. KNHANES VI is a rolling sample survey that was executed by the Korea Centers for Disease Control and Prevention from 2013 to 2015. KNHANES uses a complex study design, with multistage probability samples. To obtain data, physical examinations and household interviews were conducted. A written informed consent was obtained from all survey participants. The survey was approved by the Institutional Review Board of the Korea Centers for Disease Control and Prevention (2013-07CON-03-4C, 2013-12EXP-03-5C). A total of 22984 individuals participated in the survey. We excluded those who had fewer than two dinners per week on average, since the data on whether they usually dined alone or with others were unavailable. Individuals aged below 20 years were excluded. Additionally, we excluded individuals with missing data. Finally, a total of 13303 individuals were included in the present study (Fig. 1).
Fig. 1.
(colour online) Flowchart showing selection of the present study participants from those enrolled in the Korean Health and Nutrition Examination Survey (KHANES VI, 2013–2015). *Dinner frequency data are essential to move to the question about dinner companion
Variables
The dependent variable in the present study was BMI, which was used to diagnose overweight and obesity. BMI was computed as weight/height2 (kg/m2). In KNHANES VI, the height and weight of the participants were measured by professional investigators using mobile examination vehicles.
Our primary independent variable was dinner companion. Data were collected through individual interviews conducted by nutrition investigators who visited the participants’ households. The interviewers asked the following question: ‘Over the past year, how many times a week did you eat dinner?’ Possible choices were as follows: ‘5–7 times a week’, ‘3–4 times a week’, ‘1–2 times a week’ and ‘almost none (0 time)’. Respondents who ate dinner at least three times per week were asked: ‘When eating dinner over the past year, did you generally eat with others?’ We coded those who replied ‘No’ as eating alone. For those who replied ‘Yes’, we asked another question: ‘In general, who did you eat dinner with?’ We labelled those who answered ‘Family’ as family and those who answered ‘People other than family’ as non-family.
We controlled for several covariates in accordance with previous studies. Our covariates comprised age, household income, marital status, living alone, education level, occupation, average sleep time, average sedentary time, frequency of eating out, smoking and alcohol consumption frequency. Household income was measured in quartiles. Marital status was divided into married, widowed, divorced and unmarried. We separated people who live alone based on the number of household members. Education level was classified as follows: middle school or less; high school; and college or a higher degree. Occupation was recategorized into the following four groups according to the International Standard Classification of Occupations codes: white collar (managers, office clerks and related professionals); pink collar (service and sales workers); blue collar (skilled agricultural, forestry and fishery workers, crafts and related workers, equipment/machine operating and assembling workers, and elementary workers); and unemployed. Military personnel were excluded from the study. Average daily sleep time was split into four levels: <6 h, 6–7 h, 7–8 h and >8 h. Average sedentary time was defined as time spent sitting or lying except when sleeping and was divided into three groups: <5 h, 5–9 h and >9 h. Frequency of eating out was categorized into four groups: ‘once a day or more’, ‘3–6 times a week’, ‘1–2 times a week’ and ‘less than once a week’. Smoking was coded into current smoker, past smoker and never smoker. Alcohol consumption frequency over the past year was divided into four groups: never, once/month or less, 2–4 times/month and twice/week or more.
Statistical analyses
We investigated the general characteristics of our study population. Means and sd of BMI were compared using Student’s t test and ANOVA. Stepwise regression was conducted to select covariates. For conducting stepwise regression, we selected dinner companion, age, gender, household income, marital status, living arrangement, educational level, occupation, working hours per week, average sleep hours per day, average sedentary hours per day, eating out frequency, smoking status, total energy intake, alcohol consumption frequency and survey year. Based on stepwise regression, dinner companion, age, gender, household income, marital status, education, sleep hours, sedentary hours, total energy intake and survey year were selected; living arrangement, occupation, working hours per week, eating out frequency, smoking status and alcohol consumption frequency were excluded. Even though living arrangement, occupation, smoking status and alcohol consumption frequency were not selected based on stepwise regression, we additionally included those variables in the model because they could be associated with BMI as reported in previous studies( 16 , 17 ). A multiple linear regression model was used to evaluate the effects of dinner companion on BMI, adjusted for covariates. Lastly, a set of subgroup analyses was conducted by socio-economic variables: age, gender, household income, educational level and occupation. Differences in socio-economic status and lifestyle patterns have been associated with changes in BMI( 18 ). Thus, we conducted subgroup analyses by socio-economic variables to observe any independent association between having a dinner companion and BMI after controlling for covariates. The survey samples’ weights and complex survey design were accounted for in all statistical analyses( 19 ). All statistical tests were two-sided and calculated P values of <0·05 were considered significant. All statistical analyses were performed using the statistical software package SAS version 9.4.
Results
The general characteristics of our study population are shown in Table 1. The mean BMI was 23·75 (sd 0·04) kg/m2 for 13303 participants. Of those participants, 62·26 % (n 8553) usually ate dinner with family, 14·43 % (n 1501) ate dinner with non-family members and 23·30 % (n 3249) usually ate dinner alone. The family dinner group had the lowest BMI (23·62 (sd 0·05) kg/m2), whereas the solo eating group had the highest BMI (24·05 (sd 0·08) kg/m2).
Table 1.
General characteristics of the study population of Korean adults, aged 20 years or over, from the Korean Health and Nutrition Examination Survey VI (2013–2015)*
| BMI (kg/m2) | |||||
|---|---|---|---|---|---|
| Variable | n | % | Mean | sd | P value |
| Dinner companion | <0·001 | ||||
| With family | 8553 | 62·26 | 23·62 | 0·05 | |
| With others | 1501 | 14·43 | 23·87 | 0·11 | |
| Alone | 3249 | 23·30 | 24·05 | 0·08 | |
| Age (years) | <0·001 | ||||
| 20–29 | 1413 | 16·97 | 22·76 | 0·12 | |
| 30–39 | 2176 | 19·45 | 23·58 | 0·09 | |
| 40–49 | 2413 | 20·98 | 23·93 | 0·08 | |
| 50–59 | 2617 | 19·63 | 24·18 | 0·07 | |
| 60–69 | 2403 | 12·16 | 24·34 | 0·08 | |
| 70+ | 2281 | 10·81 | 23·85 | 0·09 | |
| Gender | <0·001 | ||||
| Male | 5381 | 46·65 | 24·32 | 0·06 | |
| Female | 7922 | 53·35 | 23·26 | 0·05 | |
| Household income | 0·162 | ||||
| Q1 (low) | 2628 | 15·48 | 24·11 | 0·10 | |
| Q2 | 3370 | 24·83 | 23·77 | 0·08 | |
| Q3 | 3610 | 29·45 | 23·76 | 0·07 | |
| Q4 (high) | 3695 | 30·23 | 23·55 | 0·07 | |
| Marital status | <0·001 | ||||
| Married | 9639 | 68·99 | 23·89 | 0·04 | |
| Widowed | 1327 | 6·87 | 24·25 | 0·12 | |
| Divorced | 534 | 3·83 | 23·76 | 0·18 | |
| Unmarried | 1803 | 20·31 | 23·10 | 0·11 | |
| Living alone | 0·758 | ||||
| Yes | 1360 | 8·33 | 24·08 | 0·12 | |
| No | 11 943 | 91·67 | 23·72 | 0·04 | |
| Educational level | <0·001 | ||||
| Middle school or less | 4713 | 26·72 | 24·33 | 0·06 | |
| High school | 4350 | 36·75 | 23·69 | 0·07 | |
| College or over | 4240 | 36·53 | 23·39 | 0·07 | |
| Occupation | 0·347 | ||||
| White collar | 2862 | 25·13 | 23·52 | 0·08 | |
| Pink collar | 1643 | 13·33 | 23·85 | 0·10 | |
| Blue collar | 3136 | 23·24 | 24·29 | 0·07 | |
| Unemployed | 5662 | 38·30 | 23·55 | 0·07 | |
| Average sleep hours per day | <0·001 | ||||
| <6 | 2240 | 15·30 | 24·23 | 0·09 | |
| 6–7 | 3636 | 27·52 | 23·96 | 0·07 | |
| 7–8 | 3708 | 28·88 | 23·58 | 0·06 | |
| >8 | 3719 | 28·31 | 23·47 | 0·08 | |
| Average sedentary hours per day | 0·011 | ||||
| <5 | 3925 | 28·74 | 23·79 | 0·06 | |
| 5–9 | 5106 | 37·44 | 23·71 | 0·06 | |
| >9 | 4272 | 33·82 | 23·78 | 0·07 | |
| Smoker | |||||
| Current | 2322 | 21·18 | 24·21 | 0·08 | 0·458 |
| Past | 2677 | 20·23 | 24·16 | 0·08 | |
| Never | 8304 | 58·59 | 23·45 | 0·05 | |
| Alcohol consumption frequency | 0·487 | ||||
| Never | 4042 | 25·47 | 23·81 | 0·07 | |
| Once/month or less | 3769 | 28·70 | 23·47 | 0·07 | |
| 2–4 times/month | 2815 | 23·89 | 23·67 | 0·08 | |
| Twice/week or more | 2677 | 21·94 | 24·15 | 0·07 | |
| Total energy intake | |||||
| <7513 kJ (<1800 kcal) | 6405 | 44·08 | 23·67 | 0·06 | 0·074 |
| 7535–10 456 kJ (1801–2499 kcal) | 3980 | 30·37 | 23·65 | 0·07 | |
| ≥10 460 kJ (≥2500 kcal) | 2918 | 25·55 | 24·03 | 0·08 | |
| Year | 0·191 | ||||
| 2013 | 4593 | 33·68 | 23·71 | 0·07 | |
| 2014 | 4343 | 32·68 | 23·69 | 0·07 | |
| 2015 | 4367 | 33·64 | 23·85 | 0·07 | |
| TOTAL | 13 303 | 100·00 | 23·75 | 0·04 | |
Complex study design, including survey weights, was considered.
Table 2 shows the association between having a dinner companion and BMI, based on a multiple linear regression model that was adjusted for covariates. The family dinner group was more likely to have a lower BMI (β=−0·39, P<0·01) than the solo eating group (reference group), but the non-family dinner group did not show a significant association (β=−0·06, P=0·67). Additionally, the lowest income group was more likely to have a higher BMI than the highest income group (β=0·30, P=0·04). With regard to educational level, the group who finished middle school or attained a lower educational level showed higher BMI than those who attained college or achieved a higher educational level (β=0·86, P<0·01).
Table 2.
Linear regression results regarding the association between dinner companion and BMI among Korean adults, aged 20 years or over, from the Korean Health and Nutrition Examination Survey VI (2013–2015)*
| BMI (kg/m2) | |||
|---|---|---|---|
| Variable | β | se | P value |
| Dinner companion | |||
| With family | −0·39 | 0·11 | <0·01 |
| With others | −0·06 | 0·14 | 0·67 |
| Alone | Ref. | – | – |
| Age (years) | |||
| 20–29 | −0·07 | 0·24 | 0·76 |
| 30–39 | 0·79 | 0·17 | <0·01 |
| 40–49 | 1·00 | 0·16 | <0·01 |
| 50–59 | 0·93 | 0·14 | <0·01 |
| 60–69 | 0·82 | 0·13 | <0·01 |
| 70+ | Ref. | – | – |
| Gender | |||
| Male | 1·31 | 0·11 | <0·01 |
| Female | Ref. | – | – |
| Household income | |||
| Q1 (low) | 0·30 | 0·14 | 0·04 |
| Q2 | 0·11 | 0·11 | 0·29 |
| Q3 | 0·17 | 0·10 | 0·09 |
| Q4 (high) | Ref. | – | – |
| Marital status | |||
| Married | 0·33 | 0·18 | 0·07 |
| Widowed | 0·76 | 0·22 | <0·01 |
| Divorced | −0·22 | 0·24 | 0·37 |
| Unmarried | Ref. | – | – |
| Living alone | |||
| Yes | −0·05 | 0·16 | 0·76 |
| No | Ref. | – | – |
| Educational level | |||
| Middle school or less | 0·86 | 0·12 | <0·01 |
| High school | 0·29 | 0·10 | <0·01 |
| College or over | Ref. | – | – |
| Occupation | |||
| White collar | −0·09 | 0·10 | 0·38 |
| Pink collar | 0·14 | 0·12 | 0·27 |
| Blue collar | 0·01 | 0·11 | 0·89 |
| Unemployed | Ref. | – | – |
| Average sleep hours per day | |||
| <6 | 0·53 | 0·11 | <0·01 |
| 6–7 | 0·33 | 0·10 | <0·01 |
| 7–8 | 0·03 | 0·09 | 0·75 |
| >8 | Ref. | – | – |
| Average sedentary hours per day | |||
| <5 | −0·28 | 0·10 | <0·01 |
| 5–9 | −0·20 | 0·09 | 0·02 |
| >9 | Ref. | – | – |
| Smoker | |||
| Current | −0·09 | 0·12 | 0·44 |
| Past | −0·14 | 0·11 | 0·21 |
| Never | Ref. | – | – |
| Alcohol consumption frequency | |||
| Never | 0·04 | 0·11 | 0·69 |
| Once/month or less | −0·10 | 0·10 | 0·36 |
| 2–4 times/month | −0·06 | 0·11 | 0·57 |
| Twice/week or more | Ref. | – | – |
| Total energy intake | |||
| <7513 kJ (<1800 kcal) | −0·03 | 0·10 | 0·76 |
| 7535–10 456 kJ (1801–2499 kcal) | −0·19 | 0·10 | 0·05 |
| ≥10 460 kJ (≥2500 kcal) | Ref. | – | – |
| Year | |||
| 2013 | −0·13 | 0·10 | 0·19 |
| 2014 | −0·17 | 0·10 | 0·08 |
| 2015 | Ref. | – | – |
Ref., reference category.
Complex study design, including survey weights, was considered.
We performed subgroup analyses stratified by age, gender, household income, educational level and occupation (Table 3). With regard to gender, male participants who had dinner with family (β=−0·56, P<0·01) or with others (β=−0·41, P=0·04) showed a lower BMI compared with the solo eating group, whereas female participants showed a significant association only among the family dinner group (β=−0·31, P=0·01). For those aged 20–29 years, the family dinner group showed significantly lower BMI compared with the solo eating group (β=−1·15, P<0·01). For those aged 30–39 years, the family dinner group had lower BMI than the solo eating group (β=−0·78, P=0·01). Likewise, for those aged 70 years or over, the family dinner group showed a lower BMI than the solo eating group (β=−0·74, P=0·01). There was no significant difference in BMI between the family dinner group and the solo eating group in any of the other age groups. The non-family dinner group showed significantly different BMI compared with the solo eating group, but this difference was observed only in the group of participants aged 20–29 years (β=−1·03, P=0·01). Non-family dinner had no effect on BMI in any other subgroups.
Table 3.
Subgroup analyses for the effect of having dinner companions on BMI, stratified by age, gender, household income, educational level and occupation, according to multiple linear regression model, among Korean adults, aged 20 years or over, from the Korean Health and Nutrition Examination Survey VI (2013–2015)*
| With family | With others | Alone | |||||
|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | BMI (kg/m2) | BMI (kg/m2) | |||||
| Variable | β | se | P value | β | se | P value | β |
| Age (years) | |||||||
| 20–29 | −1·15 | 0·31 | <0·01 | −1·03 | 0·30 | <0·01 | Ref. |
| 30–39 | −0·78 | 0·31 | 0·01 | −0·18 | 0·33 | 0·58 | Ref. |
| 40–49 | 0·08 | 0·19 | 0·68 | 0·55 | 0·29 | 0·06 | Ref. |
| 50–59 | −0·16 | 0·17 | 0·33 | 0·01 | 0·26 | 0·97 | Ref. |
| 60–69 | 0·19 | 0·20 | 0·34 | 0·26 | 0·34 | 0·44 | Ref. |
| 70+ | −0·74 | 0·22 | <0·01 | −0·16 | 0·45 | 0·73 | Ref. |
| Gender | |||||||
| Boys | −0·56 | 0·17 | <0·01 | −0·41 | 0·20 | 0·04 | Ref. |
| Girls | −0·31 | 0·12 | 0·01 | 0·11 | 0·22 | 0·61 | Ref. |
| Household income | |||||||
| Q1 (low) | −0·70 | 0·22 | <0·01 | −0·04 | 0·35 | 0·90 | Ref. |
| Q2 | −0·13 | 0·17 | 0·46 | 0·04 | 0·24 | 0·88 | Ref. |
| Q3 | −0·41 | 0·16 | 0·01 | −0·01 | 0·21 | 0·96 | Ref. |
| Q4 (high) | −0·08 | 0·15 | 0·60 | 0·13 | 0·19 | 0·48 | Ref. |
| Educational level | |||||||
| Middle school or less | −0·20 | 0·13 | 0·14 | −0·13 | 0·24 | 0·60 | Ref. |
| High school | −0·28 | 0·15 | 0·06 | −0·04 | 0·19 | 0·85 | Ref. |
| College or over | −0·40 | 0·16 | 0·01 | 0·01 | 0·19 | 0·96 | Ref. |
| Occupation | |||||||
| White collar | −0·21 | 0·18 | 0·24 | 0·13 | 0·21 | 0·54 | Ref. |
| Pink collar | −0·31 | 0·22 | 0·16 | 0·19 | 0·27 | 0·49 | Ref. |
| Blue collar | −0·11 | 0·17 | 0·51 | 0·17 | 0·23 | 0·46 | Ref. |
| Unemployed | −0·37 | 0·13 | 0·01 | −0·44 | 0·25 | 0·08 | Ref. |
Ref., reference category.
Complex study design, including survey weights, was considered. The results were adjusted for covariates used in Table 2.
Discussion
In the present study we examined the association between commensal dinner and BMI among Korean adults. The results showed that those who usually have dinner with family were more likely to have a lower BMI compared with those who eat alone. Our subgroup analyses showed that the association was greater in males than in females, and in the younger age groups (people in their 20s and 30s).
Our main finding was that the family dinner group had significantly lower BMI compared with the solo eating group. Several factors could have contributed to these results. First, people who eat with family are more likely to eat dinner on a regular basis( 20 ), which may reduce their BMI. Studies have shown that regular meals could contribute to lower weight with increased metabolism and energy expenditure( 21 ). Second, family meals are more likely to consist of healthy foods. Studies have reported that people tend to eat more fruits and vegetables when they eat with family, in addition to having increased food diversity( 22 , 23 ). In practice, a study has shown that eating dinner with family is linked to higher nutritional scores( 24 ). Additionally, people are more likely to eat processed foods when eating alone, which may cause excessive intakes of saturated fat, sugar and sodium( 25 ). Third, different eating habits of eating alone and eating with others may have contributed to our results. People tend to eat faster when they eat alone, which results in higher energy intake and increased risk of obesity( 26 ). Moreover, people may use media devices more when eating alone, which is known to have negative dietary consequences( 27 ). Due to these reasons, people who eat alone would more likely have a higher BMI than those who have family dinners.
Besides dinner companion, age, household income, marital status, educational level, sleep hours and sedentary hours showed a significant association with BMI. Our study showed that people in the lower income groups will more likely show a higher BMI than those in the higher income groups. These results are in line with those reported in a previous study which showed that low socio-economic status can be a barrier to physical activity and healthy eating( 28 ). With regard to sleeping hours, people who have fewer sleeping hours are more likely to show a higher BMI. Several studies have suggested that people with insufficient sleep had higher appetite for foods with higher levels of carbohydrates and fat( 29 , 30 ), which could be related to overweight or obesity. Concerning sedentary hours, increasing sedentary behaviour could be associated with obesity by lowering physical activity energy expenditure( 31 , 32 ).
Our subgroup analysis showed that the association between having a dinner companion and BMI varied significantly among different age groups and gender. With regard to age group, family dinner and non-family dinner were associated with BMI in individuals aged 20–29 years, 30–39 years and 70 years or older, while non-family dinner was non-significant in all age groups except those aged 20–29 years. This may be closely related to prior reports on the negative association between family meals and BMI in children and adolescents. When eating alone, young people generally buy more home meal replacements( 33 ) and eat out more( 34 ). As these foods contain inadequate nutrients and a high amount of energy, young generations are more susceptible to unhealthy diet, resulting in a higher BMI. Moreover, older adults aged 70 years or more showed higher BMI when they ate dinner alone. According to a study conducted in Japan, eating alone was associated with unhealthy dietary behaviours in older adults, and such behaviours could lead to overweight or obesity( 35 ).
Interestingly, our study revealed a stronger association between family dinner and BMI in males, which contradicts the findings of previous studies showing that such association was significant only in females( 36 , 37 ). This result could be supported by different attitudes towards eating patterns or behaviours according to gender. Since men who have dinner alone need to prepare the food themselves, it leads to poor dietary habits including low intake of fruits or vegetables and meal skipping( 38 ). Furthermore, men tend to consume unhealthy foods, including fast foods, when they eat alone. Therefore, such food choices could be related to obesity( 38 ).
The present study had several limitations. First, we had to exclude people who had fewer than two dinners per week on average from our study, due to the unavailability of data regarding their dinner companions. Second, we could not obtain the exact number of times each of the participants dined with family, with non-family or alone. We used the data on who they usually dined with, which may have been insufficient to characterize their eating patterns. Therefore, individuals within the same group may depict far different eating patterns. Third, not all covariates may have been included in our study. Furthermore, since we used cross-sectional data for our study, it was difficult to establish a cause-and-effect relationship between dinner companion and BMI.
Conclusion
Our study indicates that people who eat dinner alone or with non-family members are more susceptible to weight gain than those who usually have dinner with family, especially in younger generations. This is a worrying trend, considering the prevalence of single-person households and solo eating in young generations. Thus, appropriate health interventions are required as overweight and obesity during adolescence often persist throughout life, leading to massive costs for both the individual and society. Therefore, careful health management for people who eat alone, as well as those living alone, is needed.
Acknowledgements
Acknowledgements: The authors thank colleagues from the Department of Public Health at Yonsei University Graduate School who provided advice for this manuscript. Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: The authors declare no conflict of interest. Authorship: W.R. and J.S. contributed equally to this work. W.R. designed the study and performed statistical analyses. J.S. helped with the literature review. E.-C.P. took part in designing study. S.A.L. and S.-I.J. helped supervise the entire process. All authors read and approved the final manuscript. Ethics of human subject participation: The KNHANES VI was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Korea Centers for Disease Control and Prevention (2013-07CON-03-4C, 2013-12EXP-03-5C). Written informed consent was obtained from all subjects.
Woongchan Rah and Jaewon So contributed equally to this work.
References
- 1. Statistics Korea (2017) Household projections. http://kosis.kr/statisticsList/statisticsListIndex.do?menuId=M_01_01vwcd=MT_ZTITLE&parmTabId=M_01_01#SelectStatsBoxDiv (accessed October 2018).
- 2. Wang X, Shen W, Wang C et al. (2016) Association between eating alone and depressive symptom in elders: a cross-sectional study. BMC Geriatr 16, 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ministry of Health and Welfare & Korea Centers for Disease Control and Prevention (2014) Korea Health Statistics 2014: Korea National Health and Nutrition Examination Survey (KNHANES VI-1). https://knhanes.cdc.go.kr/knhanes/sub04/sub04_03.do?classType=7 (accessed October 2018).
- 4. Lee H (2017) Current status of solo dining in our society. Ministry of Food and Drug Safety. https://www.mdon.co.kr/news/download.html?no=13716&atno=39457 (accessed October 2018).
- 5. Lee SA, Park EC, Ju YJ et al. (2016) Is one’s usual dinner companion associated with greater odds of depression? Using data from the 2014 Korean National Health and Nutrition Examination Survey. Int J Soc Psychiatry 62, 560–568. [DOI] [PubMed] [Google Scholar]
- 6. Fulkerson JA, Larson N, Horning M et al. (2014) A review of associations between family or shared meal frequency and dietary and weight status outcomes across the lifespan. J Nutr Educ Behav 46, 2–19. [DOI] [PubMed] [Google Scholar]
- 7. Lee Y, Cho W & Oh Y (2012) Comparison of eating behavior between commensality and solo-eating of university students by BMI. Korean J Community Nutr 17, 280–289. [Google Scholar]
- 8. Martin-Biggers J, Spaccarotella K, Berhaupt-Glickstein A et al. (2014) Come and get it! A discussion of family mealtime literature and factors affecting obesity risk. Adv Nutr 5, 235–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Neumark‐Sztainer D (2006) Eating among teens: do family mealtimes make a difference for adolescents’ nutrition? New Dir Child Adolesc Dev 2006, 91–105. [DOI] [PubMed] [Google Scholar]
- 10. Hammons AJ & Fiese BH (2011) Is frequency of shared family meals related to the nutritional health of children and adolescents? Pediatrics 127, e1565–e1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fulkerson JA, Larson N, Horning M et al. (2014) A review of associations between family or shared meal frequency and dietary and weight status outcomes across the lifespan. J Nutr Educ Behav 46, 2–19. [DOI] [PubMed] [Google Scholar]
- 12. Chekroun P & Brauer M (2002) The bystander effect and social control behavior: the effect of the presence of others on people’s reactions to norm violations. Eur J Soc Psychol 32, 853–867. [Google Scholar]
- 13. World Health Organization (2018) Fact sheet: Obesity and overweight. http://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed October 2018).
- 14. Ministry of Health and Welfare & Korea Centers for Disease (2016) Korea Health Statistics 2016: Korea National Health and Nutrition Examination Survey (KNHANES VI-1). https://knhanes.cdc.go.kr/knhanes/sub04/sub04_03.do?classType=7 (accessed October 2018).
- 15. World Health Organization (2017) Obesity: Situation and trends. http://www.who.int/gho/ncd/risk_factors/obesity_text/en/ (accessed September 2018).
- 16. Drewnowski A, Moudon AV, Jiao J et al. (2014) Food environment and socioeconomic status influence obesity rates in Seattle and in Paris. Int J Obes (Lond) 38, 306–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sayon-Orea C, Martinez-Gonzalez MA & Bes-Rastrollo M (2011) Alcohol consumption and body weight: a systematic review. Nutr Rev 69, 419–431. [DOI] [PubMed] [Google Scholar]
- 18. Sánchez-Vaznaugh EV, Kawachi I, Subramanian S et al. (2009) Do socioeconomic gradients in body mass index vary by race/ethnicity, gender, and birthplace? Am J Epidemiol 169, 1102–1112. [DOI] [PubMed] [Google Scholar]
- 19. Lee WJ, Kim HC, Oh SM et al. (2013) Factors associated with a low-sodium diet: the fourth Korean National Health and Nutrition Examination Survey. Epidemiol Health 35, e2013005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Neumark-Sztainer D, Story M, Ackard D et al. (2000) The ‘family meal’: views of adolescents. J Nutr Educ 32, 329–334. [Google Scholar]
- 21. Farshchi HR, Taylor MA & Macdonald IA (2005) Beneficial metabolic effects of regular meal frequency on dietary thermogenesis, insulin sensitivity, and fasting lipid profiles in healthy obese women. Am J Clin Nutr 81, 16–24. [DOI] [PubMed] [Google Scholar]
- 22. Welsh EM, French SA & Wall M (2011) Examining the relationship between family meal frequency and individual dietary intake: does family cohesion play a role? J Nutr Educ Behav 43, 229–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Berge JM, MacLehose RF, Loth KA et al. (2012) Family meals. Associations with weight and eating behaviors among mothers and fathers. Appetite 58, 1128–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. van Lee L, Geelen A, Hooft van Huysduynen EJ et al. (2016) Associations between company at dinner and daily diet quality in Dutch men and women from the NQplus study. Eur J Clin Nutr 70, 1368–1373. [DOI] [PubMed] [Google Scholar]
- 25. Poti JM, Mendez MA, Ng SW et al. (2015) Is the degree of food processing and convenience linked with the nutritional quality of foods purchased by US households? Am J Clin Nutr 101, 1251–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zhu B, Haruyama Y, Muto T et al. (2015) Association between eating speed and metabolic syndrome in a three-year population-based cohort study. J Epidemiol 25, 332–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Moray J, Fu A, Brill K et al. (2007) Viewing television while eating impairs the ability to accurately estimate total amount of food consumed. Bariatr Nurs Surg Patient Care 2, 71–76. [Google Scholar]
- 28. Janssen I, Boyce WF, Simpson K et al. (2006) Influence of individual-and area-level measures of socioeconomic status on obesity, unhealthy eating, and physical inactivity in Canadian adolescents. Am J Clin Nutr 83, 139–145. [DOI] [PubMed] [Google Scholar]
- 29. Spiegel K, Tasali E, Penev P et al. (2004) Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med 141, 846–850. [DOI] [PubMed] [Google Scholar]
- 30. Taheri S, Lin L, Austin D et al. (2004) Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med 1, e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Levine JA, Lanningham-Foster LM, McCrady SK et al. (2005) Interindividual variation in posture allocation: possible role in human obesity. Science 307, 584–586. [DOI] [PubMed] [Google Scholar]
- 32. Pate RR, O’Neill JR & Lobelo F (2008) The evolving definition of ‘sedentary’. Exerc Sport Sci Rev 36, 173–178. [DOI] [PubMed] [Google Scholar]
- 33. Ministry of Agriculture, Food and Rural Affairs (2017) 2017. Current State of Processed Food Market Segment Home Meal Replacement Market. http://www.mafra.go.kr/bbs/mafra/131/189565/download.do (accessed October 2018).
- 34. Kim B (2017) Looking ahead eating out trend in 2018. http://www.rating.co.kr/download//x8CXlZBDUD7IaDYgUPZhAg==/...==/research.do (accessed October 2018).
- 35. Tani Y, Kondo N, Takagi D et al. (2015) Combined effects of eating alone and living alone on unhealthy dietary behaviors, obesity and underweight in older Japanese adults: results of the JAGES. Appetite 95, 1–8. [DOI] [PubMed] [Google Scholar]
- 36. Neumark-Sztainer D, Larson NI, Fulkerson JA et al. (2010) Family meals and adolescents: what have we learned from Project EAT (Eating Among Teens)? Public Health Nutr 13, 1113–1121. [DOI] [PubMed] [Google Scholar]
- 37. Goldfield GS, Murray MA, Buchholz A et al. (2011) Family meals and body mass index among adolescents: effects of gender. Appl Physiol Nutr Metab 36, 539–546. [DOI] [PubMed] [Google Scholar]
- 38. Conklin AI, Forouhi NG, Surtees P et al. (2014) Social relationships and healthful dietary behaviour: evidence from over-50s in the EPIC cohort, UK. Soc Sci Med 100, 167–175. [DOI] [PMC free article] [PubMed] [Google Scholar]