Abstract
Objective
To summarise findings of systematic reviews that distinctively report dietary intervention components and their effects on diet-, health- and economic-related outcomes in the workplace setting.
Design
MEDLINE, Embase, CINAHL, Web of Science, Cochrane Library and Google Scholar were searched in December 2014 and the search was updated in August 2017.
Results
The search identified 1137 titles, of which nineteen systematic reviews from the initial search and two systematic reviews from the updated search met the inclusion criteria (twenty-one systematic reviews, published in twenty-two papers). Most systematic reviews were of moderate quality and focused on dietary behaviour change outcomes and some health-related biomarkers. Evidence was strongest for interventions to increase fruit and vegetable intake, reduce fat intake, aid weight loss and reduce cholesterol. Few reported workplace-related and evaluation outcomes.
Conclusions
These findings suggest that workplace dietary interventions can positively influence diet and health outcomes. Suggestions for effective interventions components have been made.
Keywords: Dietary intervention, Workplace, Health outcomes, Literature review
In accordance with a growing interest in workplace well-being, the number of interventions in this field has increased over recent years. Researchers aim to identify the most effective strategies for workplaces to encourage staff to live healthier lifestyles (e.g. facilitate healthy eating at work, provide facilities to exercise more frequently and/or offer services to quit smoking). Numerous studies of diet, physical activity, weight loss and/or smoking behaviour change interventions in the workplace setting are published annually, to assess the impact of such interventions on health-, diet- and ultimately economic-related (i.e. work-related) outcomes. Simultaneously, the number of reviews, systematic reviews (SR) and meta-analyses (MA) summarising these interventions is increasing, attempting to synthesise the wealth of published evidence and to inform future intervention designs as well as guide policy makers.
Few SR highlight findings from solely dietary interventions( 1 – 5 ). Therefore, it proves challenging to filter out intervention components successful in changing dietary behaviour as part of a workplace well-being project. To learn from previous research and implement diet behaviour change interventions likely to be most effective, relevant literature on dietary workplace interventions needs to be reviewed. When turning to SR, it needs to be considered that new guidelines on how to conduct and report SR have been introduced since the first SR were conducted( 6 , 7 ). Hence, SR are likely to differ in their reporting structure and quality. Therefore, the aims of the current SR of SR was to: (i) summarise the findings of published SR reviewing either dietary interventions or multicomponent lifestyle interventions that distinctively report dietary intervention components and their effects on diet, health- and economic-related outcomes in the workplace setting; (ii) assess the most effective intervention components; and (iii) assess the quality of the SR.
Methods
A systematic search was carried out following a predefined search protocol in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines( 6 ).
Inclusion criteria
SR and MA had to meet the following criteria: (i) be published in a peer-reviewed journal before August 2017; (ii) review interventions based in the workplace setting; (iii) be published in the English language; (iv) include adults aged ≥18 years; (v) clearly describe dietary intervention components or clearly describe the impact of a multicomponent intervention on diet-related outcomes; (vi) describe the effect of dietary intervention components on dietary behaviour-related outcomes (i.e. intake, knowledge, attitude, skills), health-related outcomes (i.e. weight, BMI, waist circumference, blood pressure, blood lipids, fasting blood glucose) or economic-related outcomes (i.e. absenteeism, sick leave, productivity, return on investment); and (vii) include the general population and/or ‘at risk’ groups. Narrative reviews, reports and position statement were excluded from the analysis.
Search strategy
The search strategy was developed in Embase and was then adapted for the following databases: MEDLINE, CINAHL, Web of Science, Cochrane Library and Google Scholar (see online supplementary material, Supplemental Fig. 1). In addition, relevant studies were identified in Zetoc and NHS Evidence, and reference lists were hand-searched to identify studies that were not detected through the database search. The search was conducted in December 2014 and was updated in August 2017. Abstracts and full texts were reviewed independently, by two reviewers (D.S. and J.V.W.), for inclusion in the current SR of SR. Any disagreement between reviewers was solved by discussion until an agreement was reached.
Data extraction
The first reviewer (D.S.) extracted all outcomes under review into a structured template which was then reviewed by the second reviewer (J.V.W.) for completeness. Any discrepancies between reviewers were discussed and resolved. All results were condensed and reported as extracted from the original research paper. Where information from the primary studies was not summarised in the SR, the researchers reported the findings as stated in the SR and did not refer back to the primary studies.
Quality assessment
The AMSTAR (‘assessment of multiple systematic reviews’) quality criteria tool has been recommended as the only validated tool for quality assessment of reviews( 7 ) and was used to assess the quality of identified SR. The AMSTAR criteria tool ranks SR on eleven quality items. The SR quality rating was conducted by the two reviewers independently and any disagreements were discussed until consensus was reached.
Data synthesis
The heterogeneity in reporting among studies under review did not allow for a statistical analysis in form of a MA to be conducted. Instead, the reviewers conducted a narrative synthesis and systematically extracted the results for each outcome under review addressed in the SR and MA.
Results
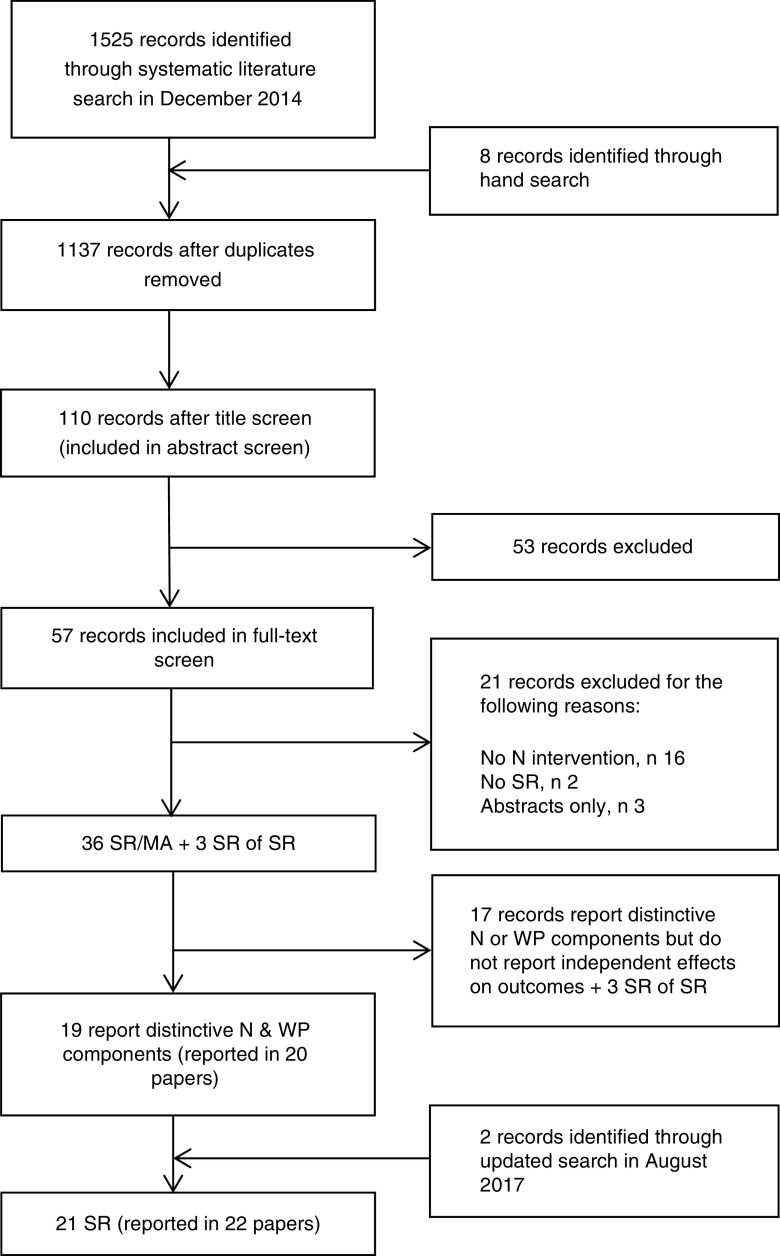
The search generated 1137 potential articles after duplicates were removed (Fig. 1), of which thirty-nine SR and SR of SR were identified that reported workplace interventions including dietary components (see online supplementary material, Supplemental Table 1). Out of these SR, nineteen SR (published in twenty papers) were identified as distinctly reporting the effect of either dietary interventions or dietary intervention components on dietary behaviour and/or other outcomes. Two additional SR were identified in the updated search, so that the final analysis included twenty-one SR (published in twenty-two papers).
Fig. 1.
Flowchart of the systematic review selection process (N, nutrition; SR, systematic review; WP, workplace)
Systematic review characteristics
Among the identified SR, three carried out a MA which all assessed different outcomes: weight( 8 ), dietary behaviour( 9 ) and theoretical framework( 10 ), and could therefore not be directly compared. To be included in the current SR of SR, the effect of the dietary part of the intervention had to be apparent. Only four of the SR evaluated solely dietary interventions( 1 , 2 , 5 , 11 ), compared with other SR that evaluated general workplace wellness programmes including multiple behaviours such as physical activity, smoking and alcohol consumption. Interventions reviewed were conducted mainly in the USA or Western Europe. One SR explicitly reviewed interventions carried out in Europe( 12 ). All SR included interventions carried out in both male and female adults. None of the SR included focused on groups at high risk of disease and two SR focused on health-care professionals( 9 , 13 ). Therefore, no conclusions could be drawn with regard to nationality, work type, high-risk populations or other sociodemographic characteristics of the target population, as this was not examined in most SR. Three SR focused on weight-loss interventions( 8 , 9 , 14 ) and four SR examined interventions focusing on environmental aspects( 15 – 18 ). One SR looked at interventions to reduce major cancer risk factors( 19 ) and Steyn et al. ( 11 ) focused on interventions published by the World Health Organization. The aims and objectives, as well as the focus of the interventions and outcomes of each SR, are reported in the online supplementary material, Supplemental Table 1. Outcomes that could most commonly be linked to the dietary intervention component were diet-related outcomes, such as fruit and vegetable (FV) intake (rather than health- or economic-related outcomes).
Study quality
Table 1 provides an overview of the quality of the SR according to AMSTAR criteria( 7 ): five SR were of high quality (8–11 points)( 1 , 8 , 9 , 18 , 20 ); fifteen were of medium quality (4–7 points)( 2 – 5 , 10 – 17 , 19 , 21 , 22 ); and one was rated low quality (0–3 points)( 23 ).
Table 1.
Quality of systematic reviews and meta-analysis under review rated according to the AMSTAR (‘assessment of multiple systematic reviews’) quality criteria
| Study | Priori design | Two independent extractors | Comprehensive search | Publication status | List of studies | Study characteristics | Quality assessment | Quality in conclusion | Combine findings | Publication bias | Conflict of interest | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| High quality | ||||||||||||
| Allan et al. (2017)( 18 ) | + | + | + | o | o | + | + | + | + | o | + | 8 |
| Anderson et al. (2009)( 8 ) | + | + | + | + | + | + | + | + | + | + | + | 11 |
| Geaney et al. (2013)( 1 ) | + | + | + | o | + | + | + | + | o | + | + | 9 |
| Osilla et al. (2012)( 20 ) | + | + | + | o | o | + | + | + | o | + | + | 8 |
| Power et al. (2014)( 9 ) | + | + | + | + | + | + | + | + | + | + | + | 11 |
| Medium quality | ||||||||||||
| Aneni et al. (2014)( 21 ) | + | o | + | o | o | + | + | + | o | + | + | 7 |
| Benedict and Arterburn (2008)( 14 ) | + | + | + | o | o | + | + | + | o | + | o | 7 |
| Engbers et al. (2005)( 17 ) | + | o | + | o | o | + | + | + | o | + | o | 6 |
| Glanz et al. (1996)( 4 ) | + | o | + | o | o | + | + | + | o | o | + | 6 |
| Hutchinson and Wilson (2011)( 10 ) | + | o | o | o | o | o | + | + | + | + | o | 5 |
| Janer et al. (2002)( 19 ) | + | o | o | o | o | + | + | + | o | o | o | 4 |
| Jensen (2011)( 2 ) | o | o | + | o | o | + | + | + | o | o | o | 4 |
| Kahn-Marshall and Gallant (2012)( 16 ) | + | o | + | o | o | + | + | + | o | + | + | 7 |
| Maes et al. (2012)( 12 ) | + | o | + | o | o | + | + | + | o | + | + | 7 |
| Matson-Koffmann et al. (2004)( 15 ) | o | o | + | + | o | + | + | + | o | + | + | 7 |
| Ni Mhurchu et al. (2010)( 3 ) | o | o | + | o | o | + | + | + | o | + | + | 6 |
| Pomerlau et al. (2005)( 5 ) | + | o | + | o | o | + | + | + | o | + | + | 7 |
| Steyn et al. (2009)( 11 ) | + | o | + | o | o | + | + | + | o | o | + | 6 |
| Torquati et al. (2016)( 13 ) | o | + | + | o | o | + | + | + | + | o | + | 7 |
| Wilson (1996)( 22 ) | o | o | + | + | o | o | + | + | o | o | + | 5 |
| Low quality | ||||||||||||
| Riedel et al. (2001)( 23 ) | o | o | + | + | o | o | o | o | o | o | o | 2 |
+, criteria met; o, criteria not met.
Diet-related outcomes
Dietary behaviour change outcomes most under review were FV consumption, overall diet, and fat and fibre intake (descending in order of frequency; Table 2). Strongest evidence was reported for improving fruit and/or vegetable intake. Four( 1 , 9 , 18 , 20 ) high-quality SR and all eight( 2 , 3 , 5 , 13 , 16 , 17 , 19 , 21 ) medium-quality SR that reported FV intake as an outcome found that the number of studies reporting an increase in FV consumption outweighed the number of studies reporting no effect. Individual studies reviewed in the SR reported improvements in various ways, e.g. percentage of FV, grams of FV, portions or overall increase. The few SR that reported an increase in portions found an improvement of between 0·2 and 0·7 portions( 1 , 3 , 5 , 13 , 15 ). ‘Overall diet’ was reported in twelve SR( 2 , 4 , 9 , 12 , 13 , 15 , 16 , 18 – 22 , 24 ), with evidence being suggestive of a positive effect. Improvements in overall diet were defined as ‘significant improvements in any of the dietary factors’( 19 ) or ‘increased consumption of healthier foods’ (e.g. FV, fibre, low-fat products)( 9 , 18 ) and two SR( 9 , 13 ) reported diet scores as well as other diet-related factors; however, no explanation was given on how individual studies calculated diet scores. Findings on change in total fat consumption were reported in eight( 1 – 3 , 9 , 10 , 17 , 19 , 20 ), and on change in saturated fat consumption in two SR( 9 , 13 ), with mixed to positive results. Results on fat intake were generally reported as a reduction in fat consumption( 9 , 17 ) and a few studies reported a percentage reduction in total fat, e.g. a change of between −9·1 and +1·3 % in energy from total fat( 1 , 3 , 19 ). The evidence for change in fibre consumption was reported in four SR( 2 , 9 , 17 , 19 ) and was conflicting. The four SR that looked at total energy intake all demonstrated positive effects( 1 , 9 , 18 , 20 ); however, the number of individual studies included in these SR was very limited.
Table 2.
Summary of dietary, health and economic-related outcomes extracted from each systematic review/meta-analysis
| Outcomes | |||||
|---|---|---|---|---|---|
| Study, review type | Time range of studies included | Number of studies included (n) | Diet-related (intake, knowledge, attitude, skills) | Health-related (weight, BMI, WC, BP, blood lipids, fasting blood glucose) | Economic-related (absenteeism, sick leave, productivity, ROI, health-care costs) |
| High quality | |||||
| Allan et al. (2017)( 18 ) SR | Up to Nov 2014 | n 22 | D outcomes (FV consumption, increased sales of healthy options, reduction in total energy consumption) (n 13/22) + ‘Evidence from environmental interventions does not enable clear recommendations to be made’ | Weight and BMI (n 1/2) + after 1 and 2 years, NC ‘Further evidence required to understand impact on weight’ | n/a |
| Anderson et al. (2009)( 8 ) SR & MA | Up to 2005 | n 47 (total) (n 10, D; n 27, D and PA) | n/a | Weight modest + (at 6–12 months), NC ‘Consistent albeit modest effect on weight-related outcomes’, NC | Economic evaluation (n 8): more studies needed for definite conclusions, NC |
| Geaney et al. (2013)( 1 ) SR | Up to Nov 2011 | n 6 (12 articles) | FV (n 4/5) +; fat (n 1/3) +; energy (n 1/1) +; self-efficacy (n 1/1) +; dietary knowledge (n 1/1) +; food purchasing patterns (n 1/2)+‘Limited evidence suggests that workplace dietary modification interventions alone and in combination with dietary education increase FV intakes’ | BMI (n 1/1) −; HDL-C (n 1/1) + TC, WHR, perceived health: no change reported | ANR |
| Osilla et al. (2012)( 20 ) SR | 2000 to Jun 2011 | n 33 (n 12 with D component) | Diet (n 6/12) + including: FV, fat, total energy ‘Small effects and mixed results, lack of rigorous evaluation’ | Effects on endpoints such as BMI, BP reported, NC | (n 4) Absenteeism, health-care cost + , NC |
| Power et al. (2014)( 9 ) SR and MA | Up to Jul 2012 | n 13 (RCT) (n 2, D; n 6, D and PA) | Overall diet (n 1/4) +; total energy (n 2/2) +; fat (n 2/2) +; SFA (n 3/4) +; % energy from fat (n 2/4) +; F (n 3/3) +; V (n 2/2) +; fibre (n 2/2) +; diet score NS ‘Differences reported at different time points – generally significant outcomes after 6/12 months’ | Weight (n 1, D only): NS after 3 months, + after 6 months ‘Greater weight loss when allocated to D and PA intervention’ | n/a |
| Medium quality | |||||
| Aneni et al. (2014)( 21 ) SR | Up to Nov 2012 | n 29 (n 12 measured diet outcome) | High-quality RCT (n 4/9): + in a range of outcomes including improved dietary self-efficacy and attitude; greater intake of F, nuts, seeds; lower protein and Na intake (n 5/9), NS FV (n 3) + follow-up studies (low quality) ‘Internet-based interventions are more likely to be successful if physical components included’ | NC | n/a |
| Benedict and Arterburn (2008)( 14 ) SR | 1995–2006 | n 11 (total) (n 2, D; n 9, PA or multicomponent) | n/a | Weight: + , NC; lipids, BP: modest + , NC ‘Worksite-based weight loss programs can result in modest short improvements in weight; long-term data on health lacking’ | ANR ‘Long-term data on economic outcomes lacking’ |
| Engbers et al. (2005)( 17 ) SR | 1985–Jan 2004 | n 13 | FV (n 6/6) +; fat (n 5/6) +; fibre (n 1/3)+ ‘Strong evidence of the effectiveness of interventions with environmental modifications on FV, fat intake’ | Cholesterol (n 4) NS; BMI (n 1/3) −; BP (n 1) NS, NC ‘No evidence on the effectiveness of worksite health promotion programs on health risk indicators’ | n/a |
| Glanz et al. (1996)( 4 ) SR | 1980–1995 | n 26 (n 10, D; n 16, cholesterol) | Quality of evidence between suggestive and indicative; limitations in research methodology noted | Quality of evidence between suggestive and indicative; limitations in research methodology noted | n/a |
| Hutchinson and Wilson (2012)( 10 ) SR & MA | 1999–Mar 2009 | n 29 (n 7 reported solely D-related outcomes post-intervention; n 2 reported D outcomes change over time) | (i) Theoretical approaches (education, social influence and cognitive behavioural) associated with small effects on diet (FV, fat) (ii) Motivational enhancement associated with larger effects and, perhaps, maintenance over time. Considerable variation between studies (iii) Studies targeting multiple health behaviours were associated with smaller effect sizes than those that focused on one health behaviour ‘Workplace suitable environment for making modest changes in diet’ | Cholesterol, weight: results mixed, NC | n/a |
| Janer et al. (2002)( 19 ) SR | Not stated | n 45 (n 16, D only or with D component) | Overall diet (n 11/14) +; fat (n 6/10) +; fibre (n 3/5) +; V (n 6/7) +; F (n 4/5)+ ‘Positive but modest intervention effects’ | NC | n/a |
| Jensen (2011)( 2 ) SR | n/a | n 30 (n 13 addressing direct economic consequences; n 17 addressing health factors expected to generate economic effects) | Healthier diet (n 10/13) +; Dietary knowledge (n 4/4) + ‘Interventions capable of FV +; fibre +; fat + : small effect sizes’ | BMI and cholesterol (n 3/4) moderate + effects fairly well documented | Absenteeism +; cost of productivity loss in terms of presenteeism and high labour turnover+ ‘Well-targeted and efficiently implemented diet-related worksite health promotion interventions may improve labour productivity by 1–2 %’ |
| Kahn-Marshall & Gallant (2012)( 16 ) SR | 1995–2010 | n 27 (n 3, D environment/policy only; n 5, D environmental/individual-level interventions) | (i) Environment/policy: dietary behaviours (n 2/2) +; methodological concerns ‘Inconclusive evidence for the effectiveness of environmental and policy changes alone to change employee dietary behaviours’ (ii) Environmental/individual level: diet behaviours, modest +; FV (n 3/4)+ ‘Moderate evidence for effectiveness of environmental/policy and individual-level strategies’ (iii) (N and PA) dietary outcomes mostly +; FV (n 4/5) + ‘Evidence greatest for multicomponent interventions and with both environmental and individual-level strategies’ | NC | n/a |
| Matson-Koffmann et al. (2004)( 15 ) SR | 1970–Oct 2003 | n 129 (before 1990: n 18, WP & restaurants; after 1990: n 13, WP) | Overall diet (≥n 10 quasi- or experimental studies): strong + for environmental interventions (all settings) Strongest evidence for influencing dietary behaviour in the workplace: availability of healthier foods/choices, POP strategies, dietary education and employer support ‘Policy and environmental interventions may promote good diet; research needed to determine long-term effectiveness’ | n/a | n/a |
| Maes et al. (2012)( 12 ) SR | 1990–1 Oct 2010 | n 30 (n 17, D; n 13, D and PA) | ‘Moderate evidence of the effect of educational and multicomponent dietary interventions on dietary behaviours. Combined D and PA interventions showed less positive results’ | ‘Inconclusive evidence’ | n/a |
| Ni Mhurchu et al. (2010)( 3 ) SR | 1995–Apr 2009 | n 16 | FV (n 12) +; fat (n 9) + ‘In general, interventions led to positive changes in fruit, vegetable and total fat intake’ | Body weight: (n 2/3) +; (n 1/3) − | ANR |
| Pomerlau et al. (2005)( 5 ) SR | Up to Apr 2004 | n 44 (n 11, WP) | FV (n 8/11) +; larger effects in studies: (i) utilising social support activities; (ii) offering larger numbers of activities; or (iii) with higher greater participation ‘Larger effects for individuals at higher risk of disease’ | n/a | n/a |
| Steyn et al. (2009)( 11 ) SR | 1995–2006 | n 30 | Studies regarded as best practice studies (n 5) in terms of diet behaviour change: various intervention strategies successful including behavioural, educational and environmental Best practice studies in terms of psychosocial outcomes produced changes in dietary knowledge | Studies regarded as best practice in terms of clinical outcome: lipids (n 2) + | Cost-effectiveness (n 4/5) + (these were organised by employees, not health-care professionals) |
| Torquati et al. (2016)( 13 ) SR | Up to Oct 2014 | n 9 (n 6, D; but only n 4 measured D outcomes) | Overall diet (n 2/2) +; FV (n 1/1) +; SFA (n 1/1) +; diet knowledge, ANR ‘Inconsistent evidence to support workplace interventions improve diet in nurses’ | NC | n/a |
| Wilson et al. (1996; 2×)( 22 , 24 ) SR | 1968 to 1994 | n 316 | Dietary change and change in dietary attitude: suggestive/indicative for both | Cholesterol: suggestive/indicative Weight control: indicative | n/a |
| Low quality | |||||
| Riedel et al. (2001)( 23 ) SR | 1993–1998 | n 146 (total) | n/a | Long-term healthy improvements + | Performance loss, NC; medical cost + (in the long term); ROI data lacking |
WC, waist circumference; BP, blood pressure; ROI, return on investment; SR, systematic review; MA, meta-analysis; n/a, not assessed; D, diet; PA, physical activity; RCT, randomised controlled trial; WP, workplace; FV, fruit and vegetables; + , positive effect; F, fruit; V, vegetables; N, nutrition; POP, point-of-purchase labelling; ANR, outcomes were assessed but not reported; NC, data (as presented in SR) did not allow clear distinction between diet-related components; −, negative effect; HDL-C, HDL-cholesterol; TC, total cholesterol; WHR, waist-to-hip ratio.
The findings on diet-related behaviour change outcomes, such as diet knowledge, purchasing behaviour and attitudes towards healthy options, were also very limited. Three SR reported favourable findings on the effectiveness of dietary interventions to improve diet-related knowledge( 1 , 2 , 11 ). One of those SR( 1 ) described one study that reported a score improvement of 1·34 (out of 10), whereas other SR reported a general knowledge improvement, without reporting scores( 2 , 11 ). The association between dietary intervention and attitude towards diet was reported in only one medium-quality SR which concluded that results were not very strong; however, small positive results were reported( 22 ). Self-efficacy was reported in one SR( 1 ) and food purchasing patterns were reported in five SR( 1 , 4 , 15 , 16 , 18 ). However, the number of studies that reported on these outcomes was relatively small so that no conclusion could be made and further evidence was needed. Overall, changes, although positive, were small and the potential impact as well as the long-term effectiveness on diet and health are unknown.
Health-related outcomes
In total, nineteen SR(1–5,8–14,16–20,22–24) included health outcomes, five( 1 , 8 , 9 , 18 , 20 ) of which were from high-quality SR. However, only nine SR( 1 – 4 , 9 , 11 , 17 , 22 , 23 , 24 ) clearly drew conclusions with regards to the effectiveness of dietary interventions alone (Table 1), and results included mainly weight-related outcomes( 1 – 3 , 9 , 17 ) and cholesterol( 1 , 2 , 17 , 24 ). Results from high-quality SR were not conclusive for dietary interventions alone, except for two SR( 1 , 9 ) that reported positive outcomes regarding reductions in weight and HDL-cholesterol and were based on a very limited number of studies. Overall results for weight-related outcomes ranged from a weight reduction of between −4·4 and −1·0 kg( 2 , 3 , 9 ), which was in line with a reduction in energy intake, to a statistically significant BMI (kg/m2) increase( 1 , 3 , 17 ). Cholesterol reductions were generalised in most studies as a ‘significant decrease in cholesterol’ and Geaney et al. ( 1 ) reported an increase in HDL-cholesterol by 0·06 mmol/l. One SR reported overall positive long-term health improvements as a result of dietary interventions( 23 ). Blood pressure was another commonly reported measure; however, it was unclear whether change in blood pressure was due to a change in dietary behaviour. That applies also to other health-related outcomes, such as blood glucose levels and overall morbidity and mortality, which were reported less often.
Economic-related outcomes
In eight SR (two of high quality( 8 , 20 ), three of medium quality( 2 , 11 , 14 ) and one of low quality( 23 )), work-related outcomes, i.e. productivity, return on investment, health-care costs and sickness/absenteeism, were assessed (Table 1). Three of these SR did not find information on economic outcomes in the individual intervention studies under review( 1 , 3 , 14 ). Furthermore, three SR reported findings but could not draw conclusions with regard to dietary interventions alone( 8 , 20 , 23 ). Only two medium-quality SR reported a positive change in work-related outcomes as a result of a dietary intervention, i.e. that interventions were cost-effective( 11 ) and reduced absenteeism as well as costs due to loss of productivity( 2 ). No specific values were provided, except for one study included in the SR by Jensen that reported a reduction in absenteeism by 20 % which was the equivalent of three days( 2 ). Kahn-Marshall and Gallant( 16 ) also noted that environmental and policy-based interventions were low-cost to implement.
Evaluation outcomes
Evaluation outcomes such as attrition( 14 ), staff participation and feasibility of the interventions were often not reported. No adverse intervention outcomes or financial losses were found. A criticism of individual studies included in the SR was that any problems in study implementation and study fidelity were frequently not reported( 12 , 18 ). Some SR did report information on the intervention workplaces but did not make comments on intervention effectiveness with regard to the kind of workplace or workplace size, except for some SR which highlighted that most interventions are carried out in medium- and large-sized businesses and interventions may not be suitable for smaller businesses( 2 , 8 , 16 , 19 , 20 ). Anderson et al. noted that one potential benefit of workplace well-being projects would be to improve the relationship between staff and management( 8 ). Interventions were criticised, however, for not including qualitative evaluation findings that would help explore that aspect( 3 ).
Findings for most effective intervention
Due to the high heterogeneity in the design of the interventions under review and in SR, there was a lack of consistency in findings of what interventions were most effective. Therefore, a summary of suggestions that were pointed out by at least some of the SR is presented in Table 3. Only findings from high- and medium-quality studies have been summarised.
Table 3.
Limitations from previous research and recommendations for the future (high- and medium-quality studies only)
| Limitations from previous interventions | ∙ Low participation rates( 11 , 12 ) and high attrition rates( 19 ) ∙ Lack of thorough description of intervention content and delivery( 9 , 15 , 18 ) ∙ Self-reported diet measures may have introduced bias and impact on validity of results( 5 , 13 , 20 ) ∙ Evidence supported that workplace interventions provided benefits in the short term( 4 , 16 , 20 ); however, information on long-term benefits was missing( 1 , 11 , 15 , 19 ) ∙ Selection bias in studies (i.e. self-selected volunteers rather than the whole workplace) that may have skewed results( 11 , 13 ) ∙ Lack of cost-saving evaluation reported in studies( 14 , 20 ) |
| Recommendations for future interventions | Designing interventions ∙ Obtain management support and commitment as this is key for intervention success( 8 , 16 , 19 ) ∙ Maximise participation rates and intervention adherence( 11 , 12 , 16 ) ∙ Involve employees in planning, implementation and management( 11 , 16 ) ∙ Plan for a longer study duration( 11 ); recommendations ranged from at least 6 months( 19 , 21 ) to 12 months( 1 , 9 ) ∙ Develop intervention based on an underlying behaviour change theory and explain reasoning( 9 – 11 ) ∙ Intervene at multiple levels (e.g. environment and individual), utilise the social and organizational environment in work for greater impact, and develop the study tailored to the workplace context and the population( 1 , 3 , 11 , 13 , 19 ) ∙ Increase the availability of healthy options at work( 11 , 15 , 16 ) ∙ Include multiple face-to-face contacts( 14 , 19 ) ∙ Address multiple behaviours( 16 ) v. diet-only interventions( 10 , 12 ) |
| Evaluating interventions ∙ Carry out detailed process evaluation, using a mixed-methods approach (i.e. qualitative and quantitative evaluation) to report outcomes( 1 , 3 , 9 ) | |
| Reporting interventions ∙ Report objective measures such as diet and health biomarkers (e.g. urine, blood)( 1 , 21 ) or actual purchasing of items when canteen changes took place( 5 ) and cost-effectiveness (e.g. absenteeism, productivity, presenteeism, health-care costs)( 1 , 3 ) ∙ Report adequately and in detail the content delivered( 9 , 15 , 18 ) |
Discussion
Overall findings
The current SR of SR synthesises best available evidence from SR and MA evaluating dietary workplace interventions. Individual workplace dietary interventions assessed a range of outcomes and the heterogeneity of reported findings made it challenging to summarise results. Overall, positive effects for increasing FV consumption and overall diet, increasing diet knowledge, aiding weight loss and reducing total cholesterol were reported. Improvements in health- and diet-related outcomes were often small but may potentially be clinically significant, i.e. a reduction in total fat intake has been linked to a reduction in body weight and improvement in LDL-cholesterol and total cholesterol, as well as the ratio between HDL- and LDL-cholesterol( 25 ). Furthermore, an improvement in FV intake by up to 0·7 portions is an important improvement, considering that FV intake has stagnated over recent years( 26 ). None of the SR distinguished between dietary behaviour at home in comparison to dietary behaviour at work. Change in diet throughout the week, however, is important, as it might indicate whether or not employees are likely to continue with the positive changes they have made at work( 1 , 3 ). Few studies examined the effect of dietary interventions alone on work-related outcomes. Overall, findings suggest that outcomes from dietary interventions may help to reduce employer’s expenses. Cancelliere et al. found that people who had a poor diet and were overweight were more likely to suffer from absenteeism( 27 ), which suggests that dietary interventions may result in cost savings due to preventing presenteeism as well as absenteeism. Further supportive evidence on cost savings is available for workplace well-being projects in general, rather than specifically dietary interventions, that were not included in the current SR of SR( 28 , 29 ).
Type of intervention
The majority of SR looked at interventions targeting multiple health behaviours. The evidence on whether dietary interventions alone or in combination with other health behaviours are more effective in improving health is mixed. A number of SR suggested that intensive interventions (i.e. interventions with numerous intervention components) are most effective( 8 , 17 ) and that environmental changes (e.g. improving food choices in canteens and vending machines and labelling healthy options) should be included( 1 , 11 , 21 ), although not all authors were able to draw that conclusion( 3 , 18 ). One large multicomponent randomised controlled trial (twenty-four worksites) that included environmental aspects was conducted by Sorensen et al. ( 30 ) in the USA. The intervention comprised education, food tastings, family training, increased availability of FV and food labelling. The study reported that the most intensive intervention arm (including the family component) was most successful and reported a significant increase in FV consumption. The Seattle 5 a Day Worksite Program by Beresford et al. ( 31 ) (twenty-eight worksites) also delivered multiple intervention components such as changes to the work environment (catering policies, healthier options in vending machines, etc.) and individual education components (e.g. cooking classes and posters), and reported an increase in FV consumption in the intervention sites compared with control sites.
This is in agreement with the Overcoming Obesity report by the McKinsey Global Institute, which outlines that healthy choices should be made easily accessible and less healthy choices should be made less easily accessible, to nudge healthier diet behaviour( 32 ). In a recent commentary, public health experts highlighted the need to reduce unhealthy nudges that can be detrimental to efforts made in public health and to increase positive nudges( 33 ). One limitation of interventions that have reported changes of the environment is that these are often carried out in workplace canteens. Therefore, the evidence for workplaces without canteen facilities on-site is limited and, in future, it should also be explored what works in smaller workplaces that often do not provide canteen facilities.
Systematic review quality
The SR were generally of medium quality, with few SR of high quality. It has to be taken into account that AMSTAR criteria were published in 2007, after some of the earlier SR were carried out, and therefore less guidance was available for researchers at the time. Furthermore, some of the criteria were not applicable and therefore the score may not accurately present the quality of each SR, namely: (i) ‘combining findings’, which indicates pooling of results and was not applicable for most SR due to the heterogeneity and may be more applicable for MA; (ii) ‘conflict of interest’ has only recently been introduced; (iii) ‘publication bias’, which is generally assessed through funnel plots, was also not applicable for most studies (the score for publication bias was given for SR that did not carry out a MA when publication bias was discussed); and (iv) depth of information on ‘study characteristics’ varied widely between studies. The quality scoring criteria used also varied in most SR, and few SR performed a formal quality assessment. A point was given for this criterion for a less formal consideration of study designs. Under ‘quality in conclusions’, only SR that clearly discussed their findings together with the quality of SR were scored a point.
Strengths and limitations
The current SR has extracted the results from the best knowledge sources available on dietary interventions or dietary intervention components, so that researchers, policy makers and employers have a reliable source of information when implementing dietary interventions in the workplace. However, by including SR only, important findings from other reviews may have been overlooked. Although we aimed to review only dietary interventions in the workplace, because most SR targeted multiple health behaviours, some of the conclusions made with regards to intervention delivery may overlap with recommendations for workplace interventions in general.
Publication bias (i.e. only successful interventions are published) and selection bias (i.e. participants who volunteered to take part in studies are more likely to want to change) in individual studies are a possible explanation for the positive findings of SR( 34 ). However, the improvement in outcomes reported in each SR as a result of dietary interventions in the workplace is relatively small and therefore it seems unlikely that results were skewed by this bias. The limitations of the individual interventions are also limiting the current SR of SR in its conclusions, such as self-reporting of diet outcomes, imprecise reporting of work-related outcomes, limited follow-up periods, missing information on intervention reach and lack of thorough evaluation (i.e. lack of process evaluation and use of qualitative as well as quantitative data collection). Osilla et al., for example, highlight that incentives are commonly used as part of workplace well-being programmes( 20 ); however, there is little information on their effectiveness.
Another limitation of the current SR is that scores for the quality of SR were given only when the SR clearly stated the required criterion and therefore some of the SR may have been judged inappropriately. It is hoped this will encourage researchers in future to clearly describe how quality criteria have been met to ensure researchers produce a good evidence base. The lack of rigorous study design, i.e. non-randomised and non-controlled trials, was commented on by a number of authors( 8 , 9 , 17 ); however, others argue that randomised controlled trials are not the most appropriate designs for public health interventions and that researchers should rather aim to increase efficacy, reach and uptake of interventions( 12 ). This argument was further explored by O’Donnell who argues that representative sampling, measures that appropriately assess the outcomes, correct use of statistical analysis and consideration of the elements of the programme are more important in a robust study methodology than a randomised controlled trial design( 35 ). Further, he argues that it is impossible to control the different factors of a comprehensive workplace programme and mentions key factors that are more important, including management support and a company-tailored programme, which agrees with SR discussed here( 3 , 11 , 19 ). Investors and business owners want to get the best return for their time and resource investment, which is another reason why randomised controlled trials may not be the most suitable design for these interventions and before-and-after designs are commonly implemented( 36 ). One way to evaluate non-controlled interventions would be to introduce intervention components in a staged manner( 9 ).
Comparison with the literature
A limited number of SR of SR reported findings on behaviour change in the workplace, including a change in eating habits. Greaves et al., for example, found that engaging in social support and targeting both diet and PA behaviour as well as building interventions on behaviour change techniques increased intervention effectiveness in type 2 diabetes patients( 37 ). Findings from another SR of SR suggested workplace settings are most effective in changing diet, as well as other health behaviours, compared with community-based settings or individual interventions( 38 ) and that environmental changes to the canteen environment, such as increased availability of healthier food and drink options, together with the labelling of healthier options, were effective in encouraging people to eat a healthier diet( 39 ). This is in agreement with the findings of the current SR of SR, as the majority of interventions recommended the inclusion of environmental changes when designing dietary interventions for workplaces. The most recent SR of SR in this area of research included SR on multiple health behaviours and only three SR reported dietary interventions( 40 ). It also lacked quality assessment of the SR and was therefore limited in its conclusions. By thoroughly assessing solely the dietary component of each SR under review, the outcomes of the present research have added valuable insight into the effectiveness of dietary studies alone on diet-, health- and economic-related outcomes.
Application of findings
The findings need to be considered with caution, as most SR have looked at well-being interventions that addressed multiple behaviours. Improvement in diet could be clearly linked to the dietary components; however, conclusions drawn with regards to health- and economic-related outcomes are limited. The reviewed interventions were mainly carried out in the USA or Western Europe and findings of the current SR may not be applicable elsewhere. However, two SR, excluded here, discussed initiatives in Latin America( 41 ) and New Zealand( 42 ). No recommendations can be made with regard to the type of work, age or gender, as these were not reported in the included SR, and the two SR that looked at interventions in health-care professionals were not able to draw conclusions( 9 , 13 ). Studies not included in the current SR also looked at blue-collar workers( 43 ), health-care professionals( 44 ), overweight and obese populations( 45 ), and groups at risk of CVD( 42 , 43 ).
Future research
While there is a small number of studies looking at different study populations, there is a need for further research to identify the effectiveness of dietary workplace interventions in different populations. Interventions and messages should be tailored to the study population and adapted to the requirements of each workplace to increase effectiveness. For intervention success, it is essential to make use of the unique opportunity that the workplace setting provides, i.e. nudge the environment, involve employees in intervention planning and delivery, and encourage effective leadership and management support. Intervention studies should also be set up over a longer period of time to assess long-term improvements. To improve comparability between study outcomes, gold standard measurements need to be developed to measure economic-related outcomes and a mixed-methods approach should be applied to assess the ‘how’ and ‘why’ as well as the ‘what’ has changed( 1 ).
As the ultimate goal of research is to enhance practice and learn from previous findings, it is important to carefully evaluate each intervention and report in detail: (i) all intervention components, planned and delivered, so that future research may be able to replicate or tweak what has been done previously; (ii) participant as well as workplace characteristics (including management buy-in); and (iii) all relevant outcomes, including participant retention rate and fidelity of intervention delivery. MRC (Medical Research Council) guidelines should be followed to design and evaluate complex interventions( 46 ) and TREND (Transparent Reporting of Evaluations with Nonrandomized Designs) guidelines used for the accurate reporting of non-randomised trials( 47 ).
Conclusion
Dietary workplace interventions seem to have small positive effects, in the short term, on increasing FV intake, reducing fat intake, aiding weight loss and reducing cholesterol. There is no ‘one design fits all’; thus intervention designers should shift their focus from finding the ‘perfect’ design and apply some crucial criteria that have been repeatedly mentioned to improve the chances of intervention success, including tailoring the intervention to the workforce, aiming for high participation and low dropout rates, utilising the unique social and environmental assets of the workplace, ensuring management support and employee involvement, incorporating multiple components, considering eating habits at work and outside the workplace, carrying out mixed-methods process evaluation, and measuring health- and economic-related outcomes. More transparency in reporting of what did and did not work and what was well accepted by staff is encouraged, so that policy makers, employers and other researchers can learn from future efforts. Workplace dietary interventions seem to have the potential to improve some aspects of dietary behaviour and health outcomes, which is likely to save companies costs in the long term.
Acknowledgements
Financial support: This work was supported by the John Wilson Memorial Trust. The John Wilson Memorial Trust had no role in the design, analysis or writing of this article. Conflict of interest: The authors declare that there is no conflict of interest. Authorship: D.S. and J.V.W. formulated the research question. D.S. carried out the search and conducted the title screen. D.S. and J.V.W. conducted the abstract and full-text screens independently. D.S. extracted all information into predefined templates, which were checked by J.V.W. Both authors conducted the quality review independently and differences were resolved through discussion. D.S. wrote the manuscript, which was guided by J.V.W. Ethics of human subject participation: Not applicable.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980018003750.
click here to view supplementary material
References
- 1. Geaney F, Kelly C, Greiner BA et al. (2013) The effectiveness of workplace dietary modification interventions: a systematic review. Prev Med 57, 438–447. [DOI] [PubMed] [Google Scholar]
- 2. Jensen JD (2011) Can worksite nutritional interventions improve productivity and firm profitability? A literature review. Perspect Public Health 131, 184–192. [DOI] [PubMed] [Google Scholar]
- 3. Ni Mhurchu C, Aston LM & Jebb SA (2010) Effects of worksite health promotion interventions on employee diets: a systematic review. BMC Public Health 10, 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Glanz K, Sorensen G & Farmer A (1996) The health impact of worksite nutrition and cholesterol intervention programs. Sci Health Promot 10, 453–470. [DOI] [PubMed] [Google Scholar]
- 5. Pomerleau J, Lock K, Knai C et al. (2005) Interventions designed to increase adult fruit and vegetable intake can be effective: a systematic review of the literature. J Nutr 135, 2486–2495. [DOI] [PubMed] [Google Scholar]
- 6. Moher D, Liberati A, Tetzlaff J et al. (2009) Systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151, 264–269. [DOI] [PubMed] [Google Scholar]
- 7. Shea BJ, Grimshaw JM, Wells GA et al. (2007) Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 7, 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Anderson LM, Quinn TA, Glanz K et al. (2009) The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: a systematic review. Am J Prev Med 37, 340–357. [DOI] [PubMed] [Google Scholar]
- 9. Power BT, Kiezebrink K, Allan JL et al. (2014) Effects of workplace-based dietary and/or physical activity interventions for weight management targeting healthcare professionals: a systematic review of randomised controlled trials. BMC Obes 1, 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hutchinson AD & Wilson C (2011) Improving nutrition and physical activity in the workplace: a meta-analysis of intervention studies. Health Promot Int 27, 238–249. [DOI] [PubMed] [Google Scholar]
- 11. Steyn NP, Parker W, Lambert EV et al. (2009) Nutrition interventions in the workplace: evidence of best practice. S Afr J Clin Nutr 22, 111–117. [Google Scholar]
- 12. Maes L, Van Cauwenberghe E, Van Lippevelde W et al. (2011) Effectiveness of workplace interventions in Europe promoting healthy eating: a systematic review. Eur J Public Health 22, 1–6. [DOI] [PubMed] [Google Scholar]
- 13. Torquati L, Pavey T, Kolbe-Alexander T et al. (2016) Promoting diet and physical activity in nurses: a systematic review. Am J Health Promot 31, 19–27. [DOI] [PubMed] [Google Scholar]
- 14. Benedict MA & Arterburn D (2008) Worksite-based weight loss programs: a systematic review of recent literature. Sci Health Promot 22, 408–417. [DOI] [PubMed] [Google Scholar]
- 15. Matson-Koffman DM, Brownstein JN & Greaney ML (2005) A site-specific literature review of policy and environmental interventions that promote physical activity and nutrition for cardiovascular health: what works? Am J Health Promot 19, 167–193. [DOI] [PubMed] [Google Scholar]
- 16. Kahn-Marshall JL & Gallant MP (2012) Making healthy behaviors the easy choice for employees: a review of the literature on environmental and policy changes in worksite health promotion. Health Educ Behav 39, 752–776. [DOI] [PubMed] [Google Scholar]
- 17. Engbers LH, Van Poppel MNM, Chin A Paw MJM et al. (2005) Worksite health promotion programs with environmental changes: a systematic review. Am J Prev Med 29, 61–70. [DOI] [PubMed] [Google Scholar]
- 18. Allan JL, Querstret D, Banas K et al. (2017) Environmental interventions for altering eating behaviours of employees in the workplace: a systematic review. Obes Rev 18, 214–226. [DOI] [PubMed] [Google Scholar]
- 19. Janer G, Sala M & Kogevinas M (2002) Health promotion trials at worksites and risk factors for cancer. Scand J Work Environ Health 28, 141–157. [DOI] [PubMed] [Google Scholar]
- 20. Osilla KC, Van Busum K, Schnyer C et al. (2012) Systematic review of the impact of worksite wellness programs. Am J Manag Care 1, 68–81. [PubMed] [Google Scholar]
- 21. Aneni EC, Roberson LL, Maziak W et al. (2014) A systematic review of internet-based worksite wellness approaches for cardiovascular disease risk management: outcomes, challenges & opportunities. PLoS One 9, e83594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wilson MG (1996) A comprehensive review of the effects of worksite health promotion on health-related outcomes: an update. Am J Health Promot 11, 107–108. [DOI] [PubMed] [Google Scholar]
- 23. Riedel JE, Lynch W, Baase C et al. (2001) The effect of disease prevention and health promotion on workplace productivity: a literature review. Am J Health Promot 15, 167–190. [DOI] [PubMed] [Google Scholar]
- 24. Wilson MG, Holman PB & Hammock A (1996) A comprehensive review of the effect of worksite health promotion on health-related outcomes. Am J Health Promot 10, 429–435. [DOI] [PubMed] [Google Scholar]
- 25. Hooper L, Summerbell C, Thompson R et al. (2012) Reduced or modified dietary fat for preventing cardiovascular disease. Cochrane Database Syst Rev 16, CD002137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Department for Environment, Food & Rural Affairs (2016) Food Statistics Pocketbook 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/608426/foodpocketbook-2016report-rev-12apr17.pdf (accessed July 2017).
- 27. Cancelliere C, Cassidy JD, Ammendolia C et al. (2011) Are workplace health promotion programs effective at improving presenteeism in workers? A systematic review and best evidence synthesis of the literature. BMC Public Health 11, 395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Baicker K, Cutler D & Song Z (2010) Workplace wellness programs can generate savings. Health Aff (Millwood) 29, 304–311. [DOI] [PubMed] [Google Scholar]
- 29. Baxter S, Sanderson K, Venn AJ et al. (2014) The relationship between return on investment and quality of study methodology in workplace health promotion programs. Am J Health Promot 28, 347–363. [DOI] [PubMed] [Google Scholar]
- 30. Sorensen G, Stoddard A, Peterson K et al. (1999) Increasing fruit and vegetable consumption through worksites and families in the Treatwell 5-a-day study. Am J Public Health 89, 54–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Beresford SAA, Thompson B, Feng Z et al. (2001) Seattle 5 a Day worksite program to increase fruit and vegetable consumption. Prev Med 32, 230–238. [DOI] [PubMed] [Google Scholar]
- 32. Dobbs R, Sawers C, Thompson F et al. (2014) Overcoming obesity: An initial economic analysis. https://www.mckinsey.com/~/media/McKinsey/Business%20Functions/Economic%20Studies%20TEMP/Our%20Insights/How%20the%20world%20could%20better%20fight%20obesity/MGI_Overcoming_obesity_Full_report.ashx (accessed October 2017).
- 33. Marteau T, Ogilvie D, Roland M et al. (2011) Judging nudging: can nudging improve population health? BMJ 342, 263–265. [DOI] [PubMed] [Google Scholar]
- 34. Van Dongen J, Proper K, Van Wier F et al. (2012) A systematic review of the cost-effectiveness of worksite physical activity and/or nutrition programs. Scand J Work Environ Health 38, 393–408. [DOI] [PubMed] [Google Scholar]
- 35. O’Donnell MP (2015) What is the ROI for workplace health promotion? It really does depend, and that’s the point. Am J Health Promot 29, v–viii. [DOI] [PubMed] [Google Scholar]
- 36. Pelletier K (1999) A review and analysis of the clinical and cost-effectiveness studies of comprehensive health promotion and disease management programs at the worksite: 1995–1998 update (IV). Am J Health Promot 13, 333–345. [DOI] [PubMed] [Google Scholar]
- 37. Greaves CJ, Sheppard KE, Abraham C et al. (2011) Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health 11, 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Jepson RG, Harris FM, Platt S et al. (2010) The effectiveness of interventions to change six health behaviours: a review of reviews. BMC Public Health 10, 538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mozaffarian D, Afshin A, Benowitz NL et al. (2012) Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation 126, 1514–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Schröer S, Haupt J & Pieper C (2014) Evidence-based lifestyle interventions in the workplace – an overview. Occup Med 64, 8–12. [DOI] [PubMed] [Google Scholar]
- 41. Mehta S, Dimsdale J, Nagle B et al. (2013) Worksite interventions – improving lifestyle habits among Latin American adults. Am J Prev Med 44, 538–542. [DOI] [PubMed] [Google Scholar]
- 42. Novak B, Bullen C, Howden-Chapman P et al. (2007) Blue-collar workplaces: a setting for reducing heart health inequalities in New Zealand? N Z Med J 120, U2704. [PubMed] [Google Scholar]
- 43. Groeneveld IF, Proper KI, Van Der Beek AJ et al. (2010) Lifestyle-focused interventions at the workplace to reduce the risk of cardiovascular disease – a systematic review. Scand J Work Environ Health 36, 202–215. [DOI] [PubMed] [Google Scholar]
- 44. Chan CW & Perry L (2012) Lifestyle health promotion interventions for the nursing workforce: a systematic review. J Clin Nurs 21, 2247–2261. [DOI] [PubMed] [Google Scholar]
- 45. Pearson ES (2012) Goal setting as a health behavior change strategy in overweight and obese adults: a systematic literature review examining intervention components. Patient Educ Couns 87, 32–42. [DOI] [PubMed] [Google Scholar]
- 46. Craig P, Dieppe P, Macintyre S et al. (2013) Developing and evaluating complex interventions: the new Medical Research Council guidance. Int J Nurs Stud 50, 587–592. [DOI] [PubMed] [Google Scholar]
- 47. Jarlais DCD, Lyles C, Crepaz N et al. (2004) Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health 94, 361–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980018003750.
click here to view supplementary material