Abstract
Objective:
To assess the strength of correlation and agreement between mid-upper arm circumference (MUAC) and BMI, and determine suitable MUAC cut-offs, to detect wasting and severe wasting among non-pregnant adult women in India.
Design:
Cross-sectional studies were conducted in five high-burden pockets of four Indian states.
Setting:
Prevalence of malnutrition among women and children is very high in these pockets and the government plans to implement community-based pilot projects to address malnutrition in these areas.
Participants:
Anthropometric measurements were carried out on 1716 women with children <5 years of age. However, analyses were conducted on 1538 non-pregnant adult women.
Results:
The results showed a strong correlation between MUAC and BMI in the non-pregnant women, with correlation coefficient of 0·860 (95 % CI 0·831, 0·883; P < 0·001). Cohen’s κ of 0·812 and 0·884 also showed good agreement between MUAC and BMI in identifying maternal wasting and severe wasting, respectively. The univariate regression model between MUAC and BMI explained 0·734 or 73 % of the variation in BMI. The MUAC cut-offs for wasting (BMI < 18·5 kg/m2) and severe wasting (BMI < 16·0 kg/m2) were calculated as 232 and 214·5 mm, respectively.
Conclusions:
MUAC is a strong predictor of maternal BMI among non-pregnant women with children <5 years in high-burden pockets of four Indian states. In a resource-constrained setting where BMI may not be feasible, the MUAC cut-offs could reliably be used to screen wasting and severe wasting in non-pregnant women for providing appropriate care.
Keywords: BMI, Mid-upper arm circumference, Correlation, Malnutrition, Maternal wasting
Undernutrition due to deficiency of protein, energy, vitamins and minerals as well as poor health and socio-economic status is affecting millions of women across the globe. It is globally acknowledged that maternal undernutrition and anaemia, before and during pregnancy, adversely affect fetal growth (weight and length) and women’s own health and increase the risk of maternal mortality( 1 ). India’s fourth National Health Family Survey conducted in 2015–2016 shows that 23 % of India’s women of reproductive age are undernourished, with a BMI of less than 18·5 kg/m2 ( 2 ). This is the major factor why a child of an undernourished mother is born undernourished, maintaining an intergenerational cycle of undernutrition( 3 ). Women’s health and nutritional status are becoming worse due to the prevailing culture and traditional practices. It has also been observed that the dietary intake of rural Indian women is lower than the recommended quantity. The prevalence of anaemia is also found to be very high among Indian women at 53 %( 2 ). Nutritional deficiencies like iron and iodine and low intakes of essential nutrients could enhance the chances of having a low-birth-weight baby( 1 ).
Identification of malnourished women gives an opportunity to improve nutritional status and prevent adverse outcomes of future pregnancies and women’s own health. BMI is the most widely used measure of nutritional status of adult non-pregnant women in public health settings. However, it must also be taken into account that, in practice, it is difficult to measure height and skill is required for calculating BMI in a population setting. Also, in many low- and middle-income settings, stadiometers are not available for measuring height. Several practical difficulties and not having the proper skills set among our nutritional workers causes us to question the reliability of BMI to assess women’s nutritional status. Hence, it would be important to consider the need of having a surrogate marker which gives good results and, at the same time, is easier to measure in a population setting. Mid-upper arm circumference (MUAC) has been used for many years to assess nutritional status among children aged <5 years. Several studies have also shown a strong correlation between MUAC and BMI in adult women( 4 – 9 ). MUAC is a much simpler anthropometric measure than BMI, as its use eliminates the need for expensive equipment, such as height charts and scales, and for any mathematical calculation. It is also much easier to perform in a population setting and it is very easy to train nutritional workers on how to take MUAC measurements. The chances of errors are also less compared with height and weight measurements. However, globally recognized MUAC cut-offs have not been established to classify maternal nutritional status, with different countries using different MAUC cut-offs for classifying maternal malnutrition for their programme purposes( 10 ). Therefore, establishing standardized MUAC cut-offs for identifying cases of malnutrition among adult women would be of great help to effectively reach out to a larger community, so that women who are at increased risk of morbidity and mortality associated with malnutrition can be identified easily for timely and effective treatment.
Therefore, the present study was conducted to assess the strength of correlation and agreement between MUAC and BMI and to determine suitable MUAC cut-offs to detect wasting and severe wasting among adult females in India.
Materials and methods
Study design, sampling and data collection
The present study used anthropometric data, namely assessments of height, weight and MUAC, collected on mothers with children <5 years of age. Data were collected through five cross-sectional nutritional surveys, conducted between 2015 and 2017 by Kalawati Saran Children’s Hospital, New Delhi in collaboration with UNICEF India, in five districts of four Indian states: West Singhbhum (Jharkhand), Nabarangpur (Odisha), Koraput (Odisha), Banda (Uttar Pradesh) and Hosangabad (Madhya Pradesh). These high-burden pockets were identified by States for planning their community-based programme for addressing problems of maternal and child undernutrition. All five nutrition surveys in the five districts used two-stage cluster sampling with the probability of being sampled proportional to the population. In total, 1716 women were part of the survey; however, for the present analysis, pregnant women (n 148) were excluded as their BMI was not calculated. Hence the analytic sample was 1538 non-pregnant adult women.
In all five surveys, equipment of global standards was used for taking anthropometry. To obtain MUAC, a flexible, inelastic, white-coloured adult measuring tape (UNICEF supply catalogue code S0145630) was used. The values obtained were expressed in millimetres. For measuring height, wooden stadiometers were used; and for measuring weight, SECA 874 scales, equipped to weigh any person below 250 kg with highest precision, were used.
Statistical analysis
BMI (kg/m2) was calculated using the recorded height and weight using the formula: weight/height2. Pearson’s correlation coefficient (r) was used to calculate the correlation between BMI and MUAC and to assess the strength of their linear relationship. We also calculated Cohen’s κ coefficients to see the level of agreement between BMI and MUAC in diagnosing wasting and severe wasting. If κ = 1, then this implies perfect agreement between the two criteria to diagnose wasting and if κ = 0, this implies perfect disagreement. A univariate linear regression analysis was performed to derive the mathematical relationship between BMI and MUAC. The coefficient of determination (R 2) was calculated as a goodness-of-fit index. Receiver-operating characteristic curves were plotted for MUAC to obtain a global measure of the accuracy of the test for the combination of all possible cut-off points. The areas under the curves were calculated and, based on the coordinates of the curves, cut-off points were selected for the variable MUAC for classifying maternal wasting and severe wasting cases. Adequate cut-off points for MUAC were derived for classifying cases of maternal wasting and severe wasting that correlate to BMI of <18·5 and <16·0 kg/m2, respectively. All statistical analyses were performed using the statistical software package IBM SPSS Statistics version 20.
Results
Tables 1 and 2 provide descriptive statistics for the prevalence of nutritional status among the adult women as per WHO and Asian cut-offs for BMI( 11 ), respectively.
Table 1.
Distribution of maternal nutritional status, as per WHO classification, among non-pregnant adult women with children <5 years of age (n 1538) from five high-burden pockets of four Indian states, 2015–2017
| Category | Criterion | Cases | Prevalence (%) |
|---|---|---|---|
| Underweight | BMI < 18·5 kg/m2 | 624 | 40·6 |
| Normal | BMI = 18·5–24·9 kg/m2 | 813 | 52·9 |
| Overweight | BMI = 25·0–29·9 kg/m2 | 83 | 5·4 |
| Obese | BMI ≥ 30·0 kg/m2 | 18 | 1·2 |
| Total | 1538 | 100·0 |
Table 2.
Distribution of maternal nutritional status, as per Asian cut-offs, among non-pregnant adult women with children <5 years of age (n 1538) from five high-burden pockets of four Indian states, 2015–2017
| Category | Criterion | Cases | Prevalence (%) |
|---|---|---|---|
| Underweight | BMI < 18·5 kg/m2 | 624 | 40·6 |
| Normal | BMI = 18·5–22·9 kg/m2 | 730 | 47·5 |
| Overweight | BMI = 23·0–24·9 kg/m2 | 83 | 5·4 |
| Obese | BMI ≥ 25·0 kg/m2 | 101 | 6·5 |
| Total | 1538 | 100·0 |
Table 1 shows the distribution of nutritional status of the women as per the WHO classification using adult BMI. It shows that more than 40 % of the mothers surveyed were underweight and only 1·2 % were obese. Also, 5·4 % of mothers were classified as overweight and about 53 % of mothers had BMI within the normal range.
Table 2 shows the distribution of nutritional status of the women as per the Asian cut-off using adult BMI criteria. It again shows that more than 40 % of the mothers surveyed were underweight. Also, 5·4 % of mothers were classified as overweight and 6·5 % of mothers were classified as obese, the latter being higher than with the WHO classification. About 48 % of the mothers had BMI within the normal range, which is lower than with the WHO classification.
The correlation coefficient of BMI and MUAC was calculated as r = 0·860 (95 % CI 0·831, 0·883; P < 0·001), which shows a strong relationship between the two. The univariate linear regression analysis showed that the relationship between MUAC and BMI by means of equation is BMI = −2·656 + 0·094 MUAC. This means on average, for each 1 mm unit of MUAC, BMI increases by 0·094 kg/m2 units. With a P value of <0·0001, this represents a very strong statistical significance: that is, the null hypothesis that there is no correlation between MUAC and BMI is rejected and we can state that there is a highly statistically significant correlation between MUAC and BMI. We found R 2 = 0·734 (i.e. regression model is a good fit) and the univariate model explained 73 % of the variation in BMI. We also found that Cohen’s κ between BMI and MUAC for diagnosing wasting and severe wasting was 0·812 (P = 0·00) and 0·884 (P = 0·00), respectively, showing that there is almost perfect agreement between the two criteria in diagnosing maternal wasting and severe wasting.
Receiver-operating characteristic curve analyses
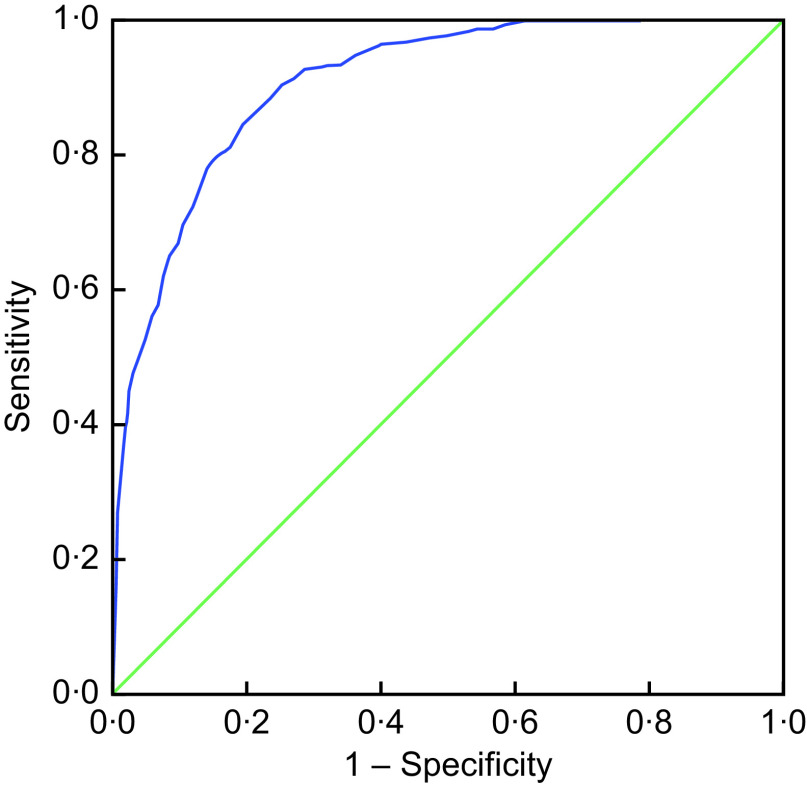
Mid-upper arm circumference to detect wasting among adult women
The area under the curve was 0·906 (95 % CI 0·892, 0·921; P < 0·001; Fig. 1). The higher the area under the curve (>0·5), the better the model is at distinguishing between mothers with wasting and no wasting.
Fig. 1.
(colour online) Receiver-operating characteristic curve (----------) of mid-upper arm circumference to identify maternal wasting (BMI < 18·5 kg/m2) among non-pregnant adult women with children <5 years of age (n 1538) from five high-burden pockets of four Indian states, 2015–2017. Diagonal segments are produced by ties; ---------- represents the line of no discrimination
The receiver-operating characteristic curve analysis showed that MUAC cut-off of <232 mm has 84·4 % sensitivity and 80·7 % specificity. As per the Youden analysis, the best MUAC cut-off to detect wasting (BMI < 18·5 kg/m2) is <232 mm, with a Youden index of 0·652; however, for programmatic purposes, we can consider an MUAC cut-off of <235 mm or <23·5 cm for identifying cases of maternal wasting. Table 3 shows the sensitivity, specificity and Youden index of different MUAC cut-offs for identifying maternal wasting.
Table 3.
Sensitivity, specificity and Youden index of different mid-upper arm circumference (MUAC) cut-offs to identify maternal wasting (BMI < 18·5 kg/m2) among non-pregnant adult women with children <5 years of age (n 1538) from five high-burden pockets of four Indian states, 2015–2017
| MUAC cut-off (mm) | Sensitivity (%) | Specificity (%) | Youden index |
|---|---|---|---|
| <220 | 53·0 | 95·0 | 0·479 |
| <225 | 66·8 | 90·3 | 0·570 |
| <230 | 79·6 | 84·6 | 0·642 |
| <232 | 84·4 | 80·7 | 0·652 |
| <235 | 90·2 | 74·9 | 0·651 |
| <240 | 94·5 | 64·2 | 0·587 |
| <245 | 97·3 | 53·6 | 0·508 |
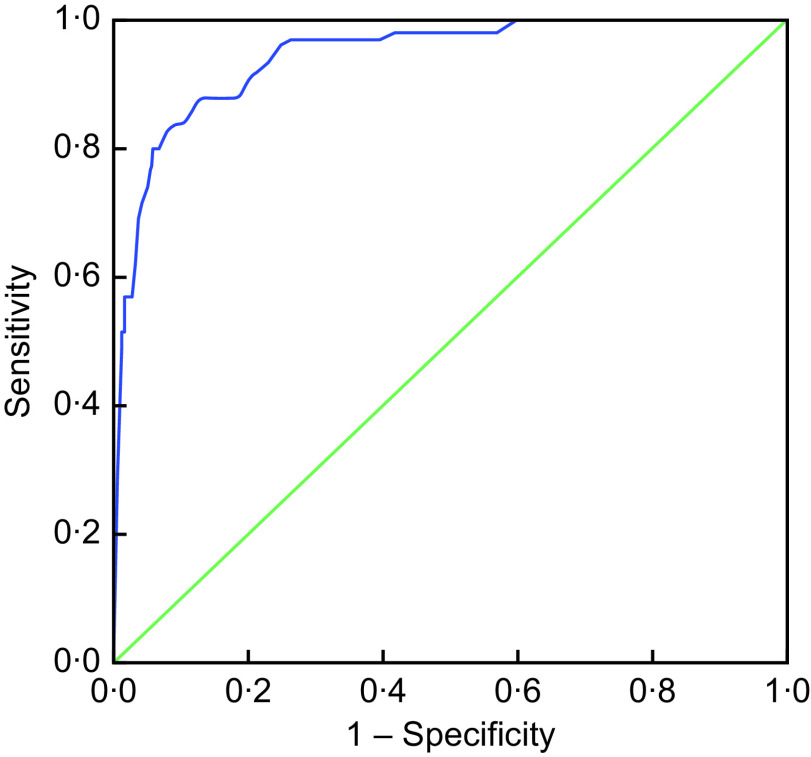
Mid-upper arm circumference cut-off to detect severe wasting among adult women
The area under the curve was 0·941 (95 % CI 0·920, 0·963; P < 0·001; Fig. 2), which again shows that the model is good at distinguishing between mothers with and without severe wasting.
Fig. 2.
(colour online) Receiver-operating characteristic curve (----------) of mid-upper arm circumference to identify maternal severe wasting (BMI < 16·0 kg/m2) among non-pregnant adult women with children <5 years of age (n 1538) from five high-burden pockets of four Indian states, 2015–2017. Diagonal segments are produced by ties; ---------- represents the line of no discrimination
The receiver-operating characteristic curve analysis showed that MUAC cut-off of <214·5 mm has 88·0 % sensitivity and 86·8 % specificity. As per the Youden analysis, the best MUAC cut-off to detect severe wasting (BMI < 16·0 kg/m2) among women is <214·5 mm, with a Youden index of 0·748; however, from a programmatic perspective, an MUAC of <215 mm or <21·5 cm would be a good cut-off for identifying cases of severe wasting among women. Table 4 shows the sensitivity, specificity and Youden index of different MUAC cut-offs for identifying maternal severe wasting.
Table 4.
Sensitivity, specificity and Youden index of different mid-upper arm circumference (MUAC) cut-offs to identify maternal severe wasting (BMI < 16·0 kg/m2) among non-pregnant adult women with children <5 years of age (n 1538) from five high-burden pockets of four Indian states, 2015–2017
| MUAC cut-off (mm) | Sensitivity (%) | Specificity (%) | Youden index |
|---|---|---|---|
| <204·5 | 63·0 | 96·3 | 0·593 |
| <209·5 | 80·0 | 93·3 | 0·732 |
| <214·5 | 88·0 | 86·8 | 0·748 |
| <219·5 | 90·0 | 80·1 | 0·701 |
| <224·5 | 97·0 | 71·6 | 0·686 |
Discussion and conclusion
The results of the present study show that MUAC serves as significant predictor of BMI. The study concludes that, for non-pregnant adult women, MUAC cut-offs of <232 mm and <214·5 mm are good predictors to detect wasting (BMI < 18·5 kg/m2) and severe wasting (BMI < 16·0 kg/m2) respectively. In a population setting, where height and weight measurements of women are difficult to take due to non-availability of weight and height measurement scales and logistic challenges, as well as having high chance of measurement and calculation errors, MUAC measurement for identifying maternal wasting could serve as a practically viable alternative. It can also complement the identification of cases using BMI and work as a substitute if BMI measurement would be difficult in a particular situation. Several other studies have also shown a strong correlation between MUAC and BMI in different settings( 12 – 15 ). MUAC also proved to be a better predictor of mortality compared with BMI( 16 ). Our study was spread across five high-burden pockets of four Indian states and reflects true population characteristics of high-burden pockets of these states. Hence, we believe that introduction of MUAC as a criterion for identifying maternal wasting and severe wasting with the said cut-offs, similar to identifying child wasting, would be ideal in a low-resource setting for easy and quick identification and timely and effective treatment.
Acknowledgements
Acknowledgements: The authors are thankful to UNICEF India for providing financial and technical support to undertake the cross-sectional nutrition surveys. The authors are grateful to Dr Karanveer Singh and Dr Vani Sethi from UNICEF for providing technical inputs on the subject; and also thankful to Ms Vasundhara Bijalwan, SMART Consultant, Project Planning and Monitoring Unit at Kalawati Saran Children’s Hospital, for coordinating the SMART surveys and the SMART enumerators (Ms Shikha Sayal, Ms Sakshi Gupta, Ms Sangna Raybardhan, Ms Prachi Singh, Ms Romika Mehta, Ms Gauri Acharya and Mr Lekhchandra Tripathy) for collecting data. Financial support: This work was supported by UNICEF India. Conflict of interest: The authors declare no conflict of interest. Authorship: P.K. and V.K. conceived the study. R.S. and N.P. analysed the data. R.S. and P.K. wrote the manuscript and collated subsequent inputs. All authors reviewed and approved the manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and was done as part of a development project aimed at improving the nutritional status of mothers and children residing in the high-burden pockets of these districts and mostly belonging to marginalised sections. The study protocol was approved by all participating State officials. The study areas were selected with the respective State governments to implement a community-based programme to address maternal and child malnutrition. Written informed consent was obtained from all participants.
References
- 1. Kowsalya R & Manoharan S (2017) Health status of Indian women – a brief report. MOJ Proteomics Bioinform 5, 00162. [Google Scholar]
- 2. Ministry of Health and Family Welfare (2016) National Health Family Survey 4 (2015–2016). http://rchiips.org/nfhs/pdf/NFHS4/India.pdf (accessed April 2018).
- 3. UNICEF India (2018) What we do Women Nutrition. http://unicef.in/Whatwedo/6/Women-Nutrition (accessed April 2018).
- 4. James WP, Mascie-Taylor GC, Norgan NG et al. (1994) The value of arm circumference measurements in assessing chronic energy deficiency in third world adults. Eur J Clin Nutr 48, 883–894. [PubMed] [Google Scholar]
- 5. Khadivzadeh T (2002) Mid upper arm and calf circumferences as indicators of nutritional status in women of reproductive age. East Mediterr Health J 8, 612–618. [PubMed] [Google Scholar]
- 6. Okereke C, Anyaehie U, Dim C et al. (2013) Evaluation of some anthropometric indices for the diagnosis of obesity in pregnancy in Nigeria: a cross-sectional study. Afr Health Sci 13, 1034–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sultana T, Karim MN, Ahmed T et al. (2015) Assessment of under nutrition of Bangladeshi adults using anthropometry: can body mass index be replaced by mid-upper-arm-circumference? PLoS One 10, e0121456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nguyen P, Ramakrishnan U, Katz B et al. (2014) Mid-upper-arm and calf circumferences are useful predictors of underweight in women of reproductive age in northern Vietnam. Food Nutr Bull 35, 301–311. [DOI] [PubMed] [Google Scholar]
- 9. Chakraborty R, Bose K & Koziel S (2011) Use of mid-upper arm circumference in determining undernutrition and illness in rural adult Oraon men of Gumla District, Jharkhand, India. Rural Remote Health 11, 1754. [PubMed] [Google Scholar]
- 10. Tang AM, Dong K, Deitchler M et al. (2013) Use of Cutoffs for Mid-Upper Arm Circumference (MUAC) as an Indicator or Predictor of Nutritional and Health-Related Outcomes in Adolescents and Adults: A Systematic Review. https://www.fantaproject.org/sites/default/files/resources/MUAC%20Systematic%20Review%20_Nov%2019.pdf (accessed February 2019).
- 11. Lim JU, Lee JH, Kim JS et al. (2017) Comparison of World Health Organization and Asia-Pacific body mass index classifications in COPD patients. Int J Chron Obstruct Pulmon Dis 12, 2465–2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bisai S & Bose K (2009) Undernutrition in the Kora Mudi tribal population, West Bengal, India: a comparison of body mass index and mid-upper-arm circumference. Food Nutr Bull 30, 63–67. [DOI] [PubMed] [Google Scholar]
- 13. Chakraborty R, Bose K & Bisai S (2009) Mid-upper arm circumference as a measure of nutritional status among adult Bengalee male slum dwellers of Kolkata, India: relationship with self-reported morbidity. Anthropol Anz 67, 129–137. [DOI] [PubMed] [Google Scholar]
- 14. Ferro-Luzzi A & James WP (1996) Adult malnutrition: simple assessment techniques for use in emergencies. Br J Nutr 75, 3–10. [DOI] [PubMed] [Google Scholar]
- 15. Gartner A, Maire B, Kameli Y et al. (2001) Body composition unaltered for African women classified as ‘normal but vulnerable’ by body mass index and mid-upper-arm-circumference criteria. Eur J Clin Nutr 55, 393–399. [DOI] [PubMed] [Google Scholar]
- 16. Tsai AC & Chang TL (2011) The effectiveness of BMI, calf circumference and mid-arm circumference in predicting subsequent mortality risk in elderly Taiwanese. Br J Nutr 105, 275–281. [DOI] [PubMed] [Google Scholar]