Abstract
Objectives
To categorize and assess all foods, beverages and ingredients provided over one week at Australian long day care (LDC) centres according to four levels of food processing and to assess the contribution of Na from each level of processing.
Design
Cross-sectional.
Setting
Menus for lunch, morning and afternoon snacks were collected from LDC centres. The level of food processing of all foods, beverages and ingredients was assessed utilizing a four-level food processing classification system: minimally processed (MP), processed culinary ingredients (PCI), processed (P) and ultra-processed (ULP).
Results
A total of thirty-five menus (lunch, n 35; snacks, n 70) provided to 1–5-year-old children were collected from seven LDC centres. Proportions of foodstuffs classified as MP, PCI, P and ULP were 54, 10, 15 and 21 %, respectively. All lunches were classified as MP. ULP foods accounted for 6 % of morning snacks; 41 % of afternoon snacks. Mean daily amount of Na provided per child across all centres was 633 (sd 151) mg. ULP foods provided 40 % of Na, followed by P (35 %), MP (23 %) and PCI (2 %).
Conclusions
Centres provided foods resulting in a mean total daily Na content that represented 63 % of the recommended Upper Level of Intake for Na in this age group. A significant proportion of ULP snack foods were included, which were the major contributor to total daily Na intake. Replacement of ULP snack foods with MP lower-Na alternatives is recommended.
Keywords: Sodium, Dietary, Child, Processed, Ultra-processed, Long day care, Australia
High dietary Na intakes that exceed recommendations are common in children aged 1–6 years in developed countries, with mean reported intake of >1000 mg/d (2·6 g salt equivalent/d)( 1 ). For example, in Australian children aged 2–3 years, dietary Na intake has been estimated at ~1500 mg/d (3·8 g salt/d)( 2 ) which exceeds the daily Upper Level (UL) of Intake of 1000 mg/d for 1–3-year-olds( 3 ). Excessive dietary Na consumption throughout childhood is associated with high blood pressure( 4 ), which tracks across the lifespan( 5 – 7 ) and is a risk factor for CVD in adulthood( 8 ). Moreover, early-life dietary habits tend to follow a trajectory from childhood and lay the foundations for eating patterns during adulthood( 9 , 10 ). This suggests that highly salted food exposure during childhood may increase the possibility of these dietary patterns continuing into adulthood. It is therefore important to establish healthy eating patterns that are low in salt early in life.
Ultra-processed (ULP) foods are industrially processed, highly palatable, habit forming, characteristically energy dense, high in added sugar, salt and saturated fat, and often contain artificial additives, flavours and colours( 11 ). There are growing health concerns about ULP foods as these types of foods have become increasingly dominant in the global food system( 12 – 15 ) and diets dominated by ULP foods have contributed to changes in childhood lipid profiles( 16 ), increased rates of obesity and weight gain( 17 , 18 ) and type 2 diabetes( 19 ) in adults and children.
In Australia, approximately 50 % of children aged 0–5 years attend long day care (LDC) where the majority spends on average 10–19 h/week( 20 ). In these settings, lunch and morning and afternoon snacks and drinks are usually provided( 21 ) and, according to nutritional recommendations, these meals together should contribute half of children’s total daily energy and nutrient requirements( 21 , 22 ). Hence LDC centres are likely important settings with regard to young children’s nutritional health.
The proportion of foods, beverages and ingredients provided at Australian LDC centres classified as ULP has not been assessed and there is no information on the contribution of ULP to the Na/salt content of foods and dishes provided on a daily basis in LDC. Therefore, the aims of the present study were to: (i) categorize individual foods based on the level of food processing using our NOVA-AUSNUT 2013 classification system( 23 ); (ii) calculate the proportions of minimally processed (MP), processed culinary ingredients (PCI), processed (P) and ULP among all foods and beverages and meals provided; and (iii) determine the contribution of Na from each of the four levels of food processing.
Methods
Study design
The present study used menus and recipes (which contained all foods, beverages and ingredients) collected over one week (Monday to Friday) as part of our previous cross-sectional study involving the assessment of foods consumed at lunch by pre-school children attending LDC centres within the Geelong area (regional city within the State of Victoria), Australia. Briefly, the study involved the recruitment of 100 children aged 3–4 years attending LDC. LDC centre managers in the region were approached and information about the centre cooking practices was collected over the telephone. Centres were eligible to participate if a cook worked on site, meals were provided to all children and a conventional food system (raw food purchased and transformed into the final product for service) was used. When one centre declined to participate another centre was approached. This continued until a sufficient number of centres was recruited to reach the target number of potentially 3–4-year-old children. Thirteen LDC centres (of a possible forty-two) were approached for study participation and seven agreed (response rate 54 %). Six centres (five privately operated, one local government operated) declined to participate. The reasons cited were: did not have time (n 2) and not interested (n 4). Centre managers provided further information on the use of menu planning guidelines, menu reviews and attendance of a menu planning workshop during a face-to-face meeting with the researcher.
Ethical approval was obtained from the Deakin University Human Research Ethics Committee (ID number: HEAG-H 90/2015).
Long day care food provision
Centre managers and/or cooks (who prepared the dishes on-site mostly from raw ingredients) were responsible for planning two-week menu cycles. All centres voluntarily followed dietary recommendations set out in the Healthy Eating Advisory Service (HEAS) menu planning guidelines from Nutrition Australia (Victorian State branch)( 22 ). According to these guidelines, LDC centres must provide meals that are diverse in tastes, colours, textures and flavours, main meals must not be repeated throughout the two-week menu cycle and key ingredients must not be repeated on the same day of the week (e.g. chicken served every Tuesday). In addition, all centre managers and cooks attended an interactive workshop with Nutrition Australia which provided information on developing menus that met Australia’s National Health and Medical Research Council’s Australian Dietary Guidelines( 24 ) and nutrition requirements for 1–5-year-olds( 22 ).
In keeping with the Australian Dietary Guidelines( 24 ) on salt usage and the consumption of salty foods, the HEAS guidelines for LDC centres also state: the addition of salt during cooking or at the table should be avoided and low/reduced-salt or no-added-salt packaged foods (e.g. sauces, stock or canned fish) should be used during cooking; processed foods such as ham or bacon (which are important contributors to dietary Na intake in children( 2 )) should be limited to once or twice per week; other processed meats such as sausages, frankfurters, salami, and commercial chicken and fish products (e.g. chicken nuggets or fish fingers) are not recommended; and discretionary food items (e.g. chips and savoury snacks), which are often high in fat, sugar and salt, should also be avoided( 22 , 24 ). For the present analysis, we used menus and recipes for lunch and morning and afternoon snacks that were prepared for all children aged 1–5 years attending LDC.
NOVA classification system and AUSNUT nutrient database
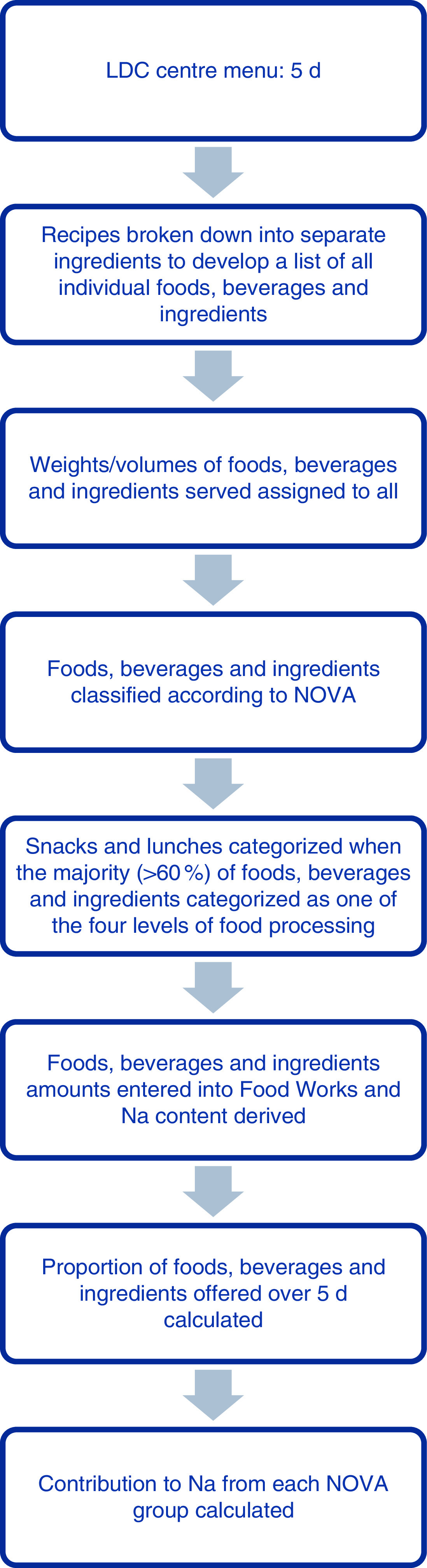
The NOVA-AUSNUT 2011–13 classification system( 23 ), a combination of the NOVA classification system( 25 ) and AUSNUT 2011–13 nutrient database( 26 ), was applied manually to all foods, beverages and ingredients within each menu at the AUSNUT 8-digit food level (Fig. 1).
Fig. 1.
Process for classifying all foods, beverages and ingredients provided, and for calculating the contribution to sodium over 5 d, at each long day care (LDC) centre
The NOVA system is the most studied food processing classification system and groups foods, beverages and ingredients according to the intention of use and degree of industrial food processing rather than in terms of nutrients and food types( 25 ). Criteria and examples of the NOVA system are described in detail in Table 1. The four food processing categories include: (i) minimally processed (MP) foods (e.g. fresh, dry, frozen fruits or vegetables, meat, milk, grains); (ii) processed culinary ingredients (PCI) (e.g. salt, sugar, oil, fat); (iii) processed (P) foods (e.g. cheese, bread, canned fish); and (iv) ultra-processed (ULP) foods (e.g. crisps, instant soups, confectionery)( 11 , 25 ).
Table 1.
| Food group and definition | Examples |
|---|---|
| Group 1: Minimally processed (MP) and unprocessed foods | |
| Minimally processed foods include both unprocessed foods that are of plant origin and consumed shortly after harvesting (fruits, nuts, seeds) or of animal origin (meat, other flesh, tissue and organs, eggs, milk), and foods that have been modified by removing parts of the food, without the addition of any other substance. Minimally processed foods are unprocessed foods altered in ways that do not add or introduce any substance but may involve removing parts of the food. Minimal processes include washing, peeling, grinding, crushing, grating, roasting, boiling, carving, portioning, scaling, filleting; pressing, drying, pasteurizing; chilling, refrigerating, freezing. None of these processes add salt, sugar, oils or fats to the original foods. Malting is a minimal process, as also is fermenting, which adds living organisms, when alcohol is not produced. Also included are foods made from two or more items in this group, i.e. granola made from cereals, nuts and dried fruits with no added sugar; and foods with added vitamins and minerals such as wheat or corn flour fortified with iron or folic acid | Fresh, squeezed, chilled, frozen or dried fruits, leafy and root vegetables; grains, brown, parboiled or white rice; corn cob or kernel, wheat berry or grains; fresh, frozen and dried beans and other legumes (pulses), lentils, chickpeas; starchy roots and tubers such as potatoes and cassava; fungi such as fresh or dried mushrooms; freshly prepared or pasteurized non-reconstituted fruit and vegetable juices without added sugars, sweeteners or flavours; corn, wheat, oats or cassava unsalted, raw/dry roasted, ground nuts and seeds without added sugars; spices; fresh or dried herbs; fresh, chilled, frozen meats, poultry, fish and seafood, whole or in cuts; dried, fresh, pasteurized full-fat, low-fat, skimmed milk, fermented and plain yoghurt without added sugar or artificial sweeteners; eggs; pasta, couscous and polenta made from flour and water; teas, coffee, herbal infusions; tap, filtered, spring, mineral water |
| Group 2: Processed culinary ingredients (PCI) | |
| Substances extracted and purified by industry from food constituents or obtained from nature. Preservatives, stabilizing or additives may be added. Processes include pressing, refining, grinding, milling and spray drying. Group 2 products are rarely consumed in the absence of Group 1 foods. Also included are: products consisting of two groups, i.e. salted butter; Group 2 items with added vitamins or minerals, i.e. iodized salt | Plant oils; animal fats; starches from corn or other plants; sugars and molasses made from cane or beet; maple syrup, honey; butter and lard obtained from milk and pork; salt |
| Group 3: Processed (P) foods | |
| Manufactured by adding salt, sugar, oil or vinegar to foods to make them more durable or modify their palatability. Directly derived from foods and similar to the original foods. Most processed foods include two or three ingredients. Produced to be consumed as part of meals or dishes. Processes include canning and bottling, non-alcoholic fermentation, and methods of preservation such as salting, salt pickling and curing | Canned or bottled vegetables and legumes preserved in brine or pickled; fruits preserved in syrup; tinned whole or pieces of fish preserved in oil; salted or sugared nuts or seeds; non-reconstituted salted or cured processed meat and fish such as ham, bacon and dried fish; cheeses made from milk, salt and ferments; unpackaged freshly made breads made from flours, water, salt and ferments; beer, cider, wine |
| Group 4: Ultra-processed (ULP) foods | |
| Formulated mostly or entirely from substances derived from foods or other organic sources. Typically, they contain little or no whole foods, and are durable, convenient, packaged, highly or ultra-palatable. Often unrecognizable versions of foods. Many ingredients are not available in retail outlets. Some ingredients are directly derived from foods, such as oils, fats, starches, sugars or obtained from hydrogenated oils, hydrolysed proteins, high-fructose corn syrup, maltodextrin or synthesized from other organic sources such as casein, lactose, whey and gluten. The majority of ingredients are preservatives and other additives such as stabilizers, emulsifiers, solvents, binders, bulkers, sweeteners, sensory enhancers, colours and flavours, and processing aids. Designed to be consumed by themselves or in combination as snacks, or meals. Processes include fortification, hydrogenation, hydrolysis, extruding, moulding, reshaping, pre-processing by frying, baking. Included also are products made solely of Group 1 or Group 3 foods which also contain additives, i.e. plain yoghurt with added artificial sweeteners and breads with added emulsifiers | Chips (crisps) and many other types of sweet, fatty or salty packaged snack products; ice cream, chocolates, candy (confectionery); French fries (chips), burgers and hot dogs; poultry and fish nuggets or sticks (fingers); mass-produced packaged breads, buns, cookies (biscuits); sweetened breakfast cereals; pastries, cakes, cake mixes; energy bars; preserves (jams), margarines and spreads; packaged desserts; canned, bottled, dehydrated, packaged soups, powdered and packaged ‘instant’ soups, noodles, sauces and desserts; meat, chicken and yeast extracts (e.g. Vegemite™); carbonated drinks, energy drinks; sugar-sweetened milk drinks including fruit yoghurts; fruit and fruit nectar drinks; no-alcohol wine, beer; pre-prepared meat, fish, vegetable, processed cheese, pizza, pasta dishes; infant formulas, follow-on milks, other baby products; ‘health’ and ‘slimming’ products such as powdered or ‘fortified’ meal and dish substitutes; whisky, rum, gin, vodka |
The AUSNUT 2011–13 nutrient database, which was developed by Food Standards Australia and New Zealand to estimate nutrient intakes from the 2011–13 Australian Health Survey, groups foods according to a 2-digit, 3-digit or 5-digit food group( 26 ). The first two numbers refer to the major food group to which a food belongs, based on a key ingredient (e.g. cereals and cereal products). The 3-digit food group falls within the 2-digit food group (e.g. regular bread and bread rolls). The 5-digit food code represents foods which are divided based on nutritional or manufacturing factors, such as whether they contain saturated fat above or below a nominated value, are fortified or are produced in a particular way (e.g. white bread and bread rolls). The 5-digit group then forms the basis of the survey ID (8-digit) assigned to each food, beverage or ingredient (e.g. bread roll from white flour)( 26 ).
The total number of foods, beverages and ingredients provided at all centres over one week (5 d) was calculated. Foods and beverages that appeared in more than one recipe were counted multiple times in the total. Regarding the provision of milk, an average volume of milk per child per morning snack (e.g. 100 ml per forty children=4 litres of milk for Centre 1 for Monday morning snack) was entered into the nutrient analysis software FoodWorks. Foods that were provided for desserts at lunchtime were combined with the lunches (e.g. spaghetti bolognaise and fruit and yoghurt) for analysis.
Sodium analysis
All foods, beverages and ingredients from the one week of recipes were entered into FoodWorks version 8 (Xyris Software, Brisbane Australia). The NOVA-AUSNUT 2011–13 classification system was applied to each food, beverage and ingredient and the Na contribution (per serving) from each processed food group was calculated.
Sodium intake recommendations
The mean total dietary Na provided to children for 1 d was calculated from the standard servings of foods and beverages provided and was compared with the National Health and Medical Research Council’s UL for Na of 1000 mg/d for children aged 1–3 years (e.g. lunch and two snacks to provide 50 % of UL for Na=500 mg Na/d)( 3 ).
Statistical analysis
All foods, beverages and ingredients were entered into a Microsoft® Office Excel 2013 spreadsheet and the proportions of MP, PCI, P and ULP were calculated. Descriptive statistics were used to describe the processed food group contributions to Na. ANOVA was used to assess differences in the mean daily amount of Na between LDC centres and in the mean Na content between the four types of processed foods. Sidak post hoc pairwise comparison was performed as a follow-up comparison test. Analyses were conducted using the statistical software package STATA/SE 13.1. A P value of <0·05 was considered significant.
Results
Centre menu characteristics
The total number of children aged 1–5 years across the seven LDC centres was 442. A total of thirty-five daily menus for 5 d (lunch, n 35; snacks, n 70) and recipes were assessed from the seven centres. Six of the seven centres provided pieces of fresh fruit (e.g. apples, bananas and pears) for morning snack, with one centre providing muffins, pancakes, crackers, sultana bread or ham and cheese rice cakes/biscuits for five mornings during the week. Afternoon snacks across the centres were either cooked from raw ingredients (e.g. scones; cookies; carrot cake) or consisted of processed foods (e.g. crackers and dips/cheese; raisin toast; bread and spreads); only one centre, on one occasion, served fruit for afternoon snack. All lunches provided were cooked mixed dishes (rather than sandwiches) and consisted of a combination of fresh (e.g. vegetables) and manufactured foods/ingredients (e.g. curry paste, stock powder). Desserts were provided as part of lunch and varied across the centres (e.g. fruit; yoghurt; apple pie; custard). At all centres, beverages consisted of full-cream plain/whole milk, which was served at morning snack every day, or water, which was available at all times. One-week menus for each centre are shown in the online supplementary material, Supplemental Table 1.
Sodium contribution from foods, beverages and ingredients
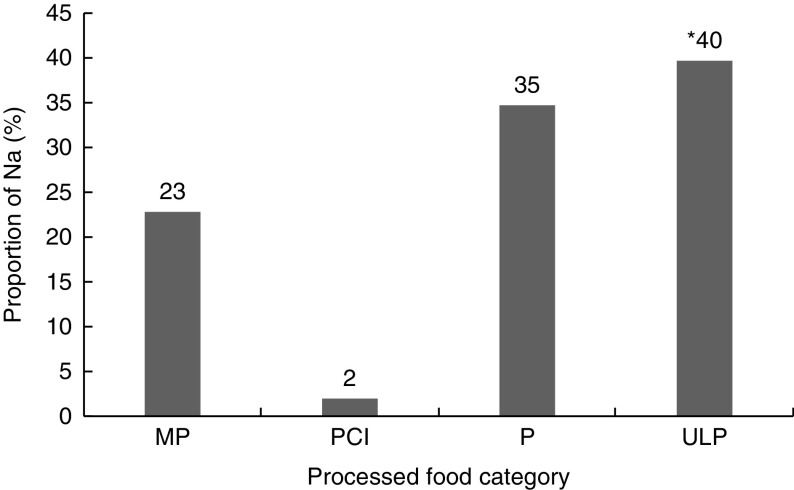
The mean amount of Na provided per child from all meals and snacks assessed from the recipe standard servings across all centres was 633 mg/d (Table 2). Overall, across the seven centres, ULP foods contributed significantly to the mean daily Na amount (Fig. 2).
Table 2.
Proportion (%) of sodium from foods, beverages and ingredients, and the amount of sodium (mg) per child per day, provided to 1–5-year-old children attending seven long day care centres in the Geelong area, Victoria, Australia (August–October 2015), according to the four levels of food processing
| Over all centres | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Centre 1 | Centre 2 | Centre 3 | Centre 4 | Centre 5 | Centre 6 | Centre 7 | % Na* | Na mg† | ||||||||||
| % Na* | Na mg† | % Na* | Na mg† | % Na* | Na mg† | % Na* | Na mg† | % Na* | Na mg† | % Na* | Na mg† | % Na* | Na mg† | Mean | sd | Mean | sd | |
| MP | 54 | 113 | 57 | 162 | 49 | 109 | 54 | 204 | 56 | 152 | 57 | 105 | 52 | 165 | 54 | 3 | 144 | 37 |
| PCI | 11 | 6 | 8 | 2 | 9 | 0 | 18 | 71 | 2 | 5 | 7 | 2 | 13 | 3 | 10 | 5 | 13 | 26 |
| P | 18 | 307 | 18 | 268 | 17 | 200 | 8 | 121 | 10 | 166 | 18 | 218 | 20 | 275 | 15 | 5 | 222 | 66 |
| ULP | 17 | 254 | 17 | 211 | 25 | 600 | 20 | 81 | 32 | 362 | 18 | 143 | 15 | 126 | 21 | 6 | 254 | 179 |
| Total Na (mg/d) | 680 | 643 | 909 | 477 | 685 | 468 | 569 | 633 | 151 | |||||||||
MP, minimally processed; PCI, processed culinary ingredient; P, processed; ULP, ultra-processed.
Percentage of total Na (mg/d).
Na (mg/d) from individual standard servings of lunch and two snacks (morning and afternoon).
Fig. 2.
Contribution of sodium from foods, beverages and ingredients provided to 1–5-year-old children attending seven long day care centres in the Geelong area, Victoria, Australia (August–October 2015), according to the four food processing levels (MP, minimally processed; PCI, processed culinary ingredients; P, processed; ULP, ultra-processed). Significant contribution of ULP to mean daily sodium amount: *P<0·001
Level of food processing of foods, beverages and ingredients
Of all foods, beverages and ingredients provided at all centres over 5 d, 54 % were MP, 21 % were ULP, 15 % were P and 10 % were PCI. Across all centres the proportions of the four levels of processing and the mean Na served per child per day varied (Table 2). Centre 3 provided the greatest mean daily amount of Na, whereas Centre 6 provided the least (909 v. 468 mg, P<0·001). The difference in the mean daily amount of Na was due to the type of ULP foods provided on more than one day at Centre 3 (e.g. Vegemite™ (yeast extract), processed cheese and mass-manufactured breads/English muffins). Centre 7 provided a greater proportion of MP and the lowest proportion of ULP, which resulted in a low mean daily Na provision.
Level of processing of lunches and snacks
The proportions of foods, beverages and ingredients (within the morning snacks, lunches and afternoon snacks provided), categorized according to the four processed food groups, indicate that all lunches were classified as MP (Table 3). The majority of morning snacks provided were classified as MP (88 %) in contrast to the afternoon snacks where almost half were classified as ULP, with close to a quarter classified as P. Notably, afternoon snacks accounted for close to half of the total Na provided for the day, which was comparable to the proportion of daily Na provided by lunch: 48 v. 43 %.
Table 3.
Proportion (%) of snacks and lunches classified according to the four food processing levels and the mean amount of sodium (mg) provided during these meals to 1–5-year-old children attending seven long day care centres in the Geelong area, Victoria, Australia (August–October 2015)
| Morning snack | Lunch | Afternoon snack | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Na (mg) | Na (mg) | Na (mg) | |||||||
| % | Mean | sd | % | Mean | sd | % | Mean | sd | |
| MP | 88 | 61 | 55 | 100 | 265 | 118 | 30 | 86 | 51 |
| PCI | 3 | 2 | 0·5 | 6 | 17 | 12 | |||
| P | 3 | 2 | 0·6 | 23 | 66 | 45 | |||
| ULP | 6 | 4 | 0·1 | 41 | 117 | 96 | |||
| Total Na (mg/d) | 69 | 57 | 265 | 118 | 286 | 110 | |||
| % of total Na (mg/d) | 9 | 43 | 48 | ||||||
MP, minimally processed; PCI, processed culinary ingredient; P, processed; ULP, ultra-processed.
Discussion
In this sample, the mean daily contribution of Na from all lunches and snacks provided at seven LDC centres was 633 mg, which represents 63 % of the UL of Na intake of 1000 mg/d for 1–3-year-olds( 3 ). Guidelines (HEAS) recommend that the two snacks and lunch served at LDC should provide approximately 50 % of daily nutrient requirements( 22 ). As Australian children have been found to be consuming Na in amounts well in excess of the UL( 2 ), it would seem that an appropriate, achievable target would be to ensure that the Na content of the foods provided on a daily basis at LDC centres does not exceed half the UL for Na, namely 500 mg Na/d( 3 , 22 ). Therefore, although the Na content of the food provided was on average 13 % more than desirable, the Na content of the foods was not excessive, particularly in context of results from the 2011–13 Australian Health Survey where children aged 2–3 years were found to be consuming an average daily intake of ~1500 mg Na/d (one-and-a-half times the UL)( 2 ). Finding a range of lower-salt foods, particularly mid-meal snacks, is challenging even for these centres which are utilizing the HEAS menu planning guidelines( 22 ) and using low-Na versions of different food products including canned vegetables and legumes.
When we assessed the level of processed foods and ingredients we found that overall only a small proportion of foods (21 %) were classified as ULP (e.g. crackers, tortillas, Asian sauces, mass-manufactured bread, processed cheese, Vegemite™). It was also evident that most of the ULP foods, such as crackers and dips and breads/crumpets/English muffins with spreads, were used in afternoon snacks rather than main meals. It is important to note that lunch, the main meal of the day, provided less than half of the daily Na (43 %), whereas afternoon snacks accounted for 48 % of the daily Na food provision. As such, more than 40 % of all afternoon snacks were classified as ULP (e.g. pita and bean salsa dip, muffins with spreads, apple muffins). Importantly these ULP foods made the greatest contribution to the total daily amount of dietary Na (40 %), which is perhaps not surprising given that in developed countries approximately three-quarters of dietary Na comes from salt added during the manufacture of these types of foods( 27 ). Findings from two recent cross-sectional studies have shown that ULP foods make a significant contribution to young children’s total dietary Na intake. We previously assessed the contribution from the level of processing to total daily Na intake in a sample of Australian children aged 3·5 years and found that ULP foods contributed 48 % of total daily Na intake compared with P (35 %) and MP (16 %) foods( 28 ). Similarly, utilizing 2 d of dietary data, Sparrenberger et al. found in 204 Brazilian children aged 2–10 years that ULP foods contributed 49 % of total Na, whereas MP foods contributed only 17 % and PCI 35 %( 29 ).
ULP foods are industrially formulated and tend to be energy dense, with high levels of added Na and/or sugars, and there is a growing body of epidemiological evidence in adults( 17 , 18 ) and children( 16 , 30 ) indicating an association between ULP foods and chronic disease. Cross-sectionally, the consumption of ULP foods has been associated with metabolic syndrome in Brazilian adolescents aged 12–19 years( 30 ). Furthermore, Rauber et al. colleagues found that ULP food consumption in Brazil at pre-school age (3–4 years) was a predictor of increased lipid concentrations at primary school (7–8 years)( 16 ). There is also some evidence in high-income countries that the consumption of ULP foods has displaced the consumption of meals/dishes prepared from MP foods( 31 ).
In our sample of seven LDC centres, across one week, the majority of morning snacks were classified as MP as a variety of fresh fruits and full-fat cow’s milk were served during these times, and as such contributed less than 10 % of the total daily Na provision. There was only one centre that provided ULP foods as morning snacks on three occasions, but most other times morning snacks were MP. More ULP foods (41 %) were provided as afternoon snacks across all centres. Therefore, there is scope for LDC centres to reduce exposure to high-salt foods on these occasions.
All lunches were classified as MP (e.g. lasagne, chicken and vegetable spaghetti, lamb and apricot chickpea curry) which were prepared from a majority (>60 %) of MP ingredients (e.g. fresh vegetables, meats, pasta, rice or couscous) and contributed less than a quarter of the total daily Na provision (23 %). According to the NOVA food processing classification system, which distinguishes freshly prepared dishes from manufactured products, MP foods are natural plant-based foods that do not contain added substances such as salts, fats oils or sugars and are altered by processes such as pasteurization, grinding or filtering which only remove inedible or unwanted parts( 11 , 25 ). It is the consumption of MP foods, such as fresh fruit and vegetables, throughout childhood that is important as higher intakes may reduce the risk of childhood obesity( 32 ), stroke( 33 ) and cancer later in life( 34 ). It is therefore encouraging that the main meals and morning snacks provided at LDC centres were based primarily on MP foods.
A key factor in keeping the total Na content of the meals low at these centres was the provision of cooked lunches rather than sandwiches, which, in Australia, are often provided in schoolchildren’s home-prepared packed lunches or are available for purchase at school canteens( 35 ). These lunchtime sandwiches are typically composed of processed foods such as bread, cheese and ham( 35 ), which according to the recent Australian Health Survey 2011–13 are key sources of Na in school-aged children, together contributing ~26 % of total daily Na( 2 ). Hence the transition from pre-school to primary school likely represents an important time when children are exposed to more Na-dense foods. It is therefore important to limit this shift from low to high Na-dense foods during this time. Effective strategies are likely to involve education programmes for parents on how to select low-Na food choices as well as food industry-led salt reduction policies to reduce Na in the food supply.
Within our sample, 15 % of the foods, beverages and ingredients were classified as P and contributed 35 % of total Na. The foods that fell into this category tended to be canned goods which were nutritionally rich and were low-Na varieties (e.g. canned tomatoes, fish and legumes). It should be noted that all surveyed centres had voluntarily implemented the policy of choosing these low/reduced-salt or no-added-salt packaged products and limited the use of ham or bacon to once or twice weekly( 24 ) as set out in the HEAS menu planning guidelines( 22 ) (which are informed by the Australian Dietary Guidelines)( 24 ). It is therefore likely that the contribution to Na from P foods would have been greater if the centres within our sample had not followed the HEAS guidelines recommending the provision of low-Na packaged products.
Strengths and limitations
We have used a previously tested NOVA-AUSNUT 2011–13 classification system which allows assessment of all foods, beverages and ingredients according to four levels of processing and the contribution of Na from each level in a sample of Australian pre-school children( 28 ). Furthermore, the analysis of 5 d of recipes from each centre allowed for the assessment of typical foods, beverages and ingredients provided to children at these settings on a regular basis. However, our analysis provides information only on the provision rather than the consumption of processed foods and beverages at these settings. We did not measure the actual Na content of food served and relied on food composition tables to determine the amounts of Na provided. In addition, our sample was subject to selection bias as all seven LDC centres participated in the workshop provided by Nutrition Australia and adhered to the HEAS menu planning guidelines( 22 ). Thus our findings cannot be generalized to other Australian LDC centres. Nevertheless, these data show the best-case scenario regarding the provision of ULP foods and their contribution to total Na. It would be interesting to assess the Na content of the foods provided in LDC centres that did not follow the guidelines, as they may provide less MP foods and a greater proportion of ULP foods.
Conclusion
We have categorized and assessed foodstuffs provided at Australian LDC centres according to four levels of food processing, determined the contribution of Na from each level of processing and found that all lunches were classified as MP. ULP foods contributed the greatest proportion of Na, despite accounting for only 20 % of foods and beverages provided. The mean amount of Na provided per child per day across all centres represented 63 % of the recommended UL of Na intake for this age group. However, a significant proportion of ULP snack foods were included, which were the major contributor to total daily Na intake. All centres followed the HEAS menu planning guidelines and used low/reduced-salt products which resulted in a relatively low level of use of P foods. A reduction in the use of ULP foods used to prepare afternoon snacks is recommended to help reduce the amount of dietary Na in young children’s diets.
Acknowledgements
Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sector. Conflict of interest: None. Authorship: S.A.O. was responsible for the study conception, wrote the manuscript and performed the data analysis. C.A.N. was responsible for the accuracy of the data analysis and together with K.E.L., J.W., C.A.G. and K.J.C., provided significant consultation and critically reviewed the manuscript. Each author has seen and approved the content of the submitted manuscript. Ethics of human subject participation: Not applicable.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S136898001700132X.
click here to view supplementary material
References
- 1. Brown IJ, Tzoulaki I, Candeias V et al. (2009) Salt intakes around the world: implications for public health. Int J Epidemiol 38, 791–813. [DOI] [PubMed] [Google Scholar]
- 2. Australian Bureau of Statistics (2014) 4364.0.55.007 – Australian Health Survey: Nutrition First Results – Food and Nutrients 2011–12. http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4364.0.55.0072011-12 (accessed September 2016).
- 3. Department of Health and Ageing, National Health and Medical Research Council (2006) Nutrient Reference Values for Australia and New Zealand. Canberra, ACT: NHMRC. [Google Scholar]
- 4. He FJ, Marrero NM & Macgregor GA (2008) Salt and blood pressure in children and adolescents. J Hum Hypertens 22, 4–11. [DOI] [PubMed] [Google Scholar]
- 5. Chen X & Wang Y (2008) Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation 117, 3171–3180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Toschke AM, Kohl L, Mansmann U et al. (2010) Meta-analysis of blood pressure tracking from childhood to adulthood and implications for the design of intervention trials. Acta Paediatr 99, 24–29. [DOI] [PubMed] [Google Scholar]
- 7. Tirosh A, Afek A, Rudich A et al. (2010) Progression of normotensive adolescents to hypertensive adults: a study of 26,980 teenagers. Hypertension 56, 203–209. [DOI] [PubMed] [Google Scholar]
- 8. Lauer RM, Clarke WR & Mahoney LT (1989) Childhood risk factors for high adult blood pressure. The Muscatine Study. Pediatrics 84, 633–641. [PubMed] [Google Scholar]
- 9. Nicklaus S & Remy E (2013) Early origins of overeating: tracking between early food habits and later eating patterns. Curr Obes Rep 2, 179–184. [Google Scholar]
- 10. Mikkila V, Rasanen L, Raitakari OT et al. (2004) Longitudinal changes in diet from childhood into adulthood with respect to risk of cardiovascular diseases: the Cardiovascular Risk in Young Finns Study. Eur J Clin Nutr 58, 1038–1045. [DOI] [PubMed] [Google Scholar]
- 11. Monteiro CA, Cannon G, Levy R et al. (2016) NOVA. The star shines bright. World Nutr 7, 28–38. [Google Scholar]
- 12. Moodie R, Stuckler D, Monteiro C et al. (2013) Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet 381, 670–679. [DOI] [PubMed] [Google Scholar]
- 13. Monteiro CA, Moubarac JC, Cannon G et al. (2013) Ultra-processed products are becoming dominant in the global food system. Obes Rev 14, Suppl. 2, S21–S28. [DOI] [PubMed] [Google Scholar]
- 14. Luiten CM, Steenhuis IH, Eyles H et al. (2016) Ultra-processed foods have the worst nutrient profile, yet they are the most available packaged products in a sample of New Zealand supermarkets. Public Health Nutr 19, 530–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moubarac JC, Martins AP, Claro RM et al. (2013) Consumption of ultra-processed foods and likely impact on human health. Evidence from Canada. Public Health Nutr 16, 2240–2248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rauber F, Campagnolo PD, Hoffman DJ et al. (2015) Consumption of ultra-processed food products and its effects on children’s lipid profiles: a longitudinal study. Nutr Metab Cardiovasc Dis 25, 116–122. [DOI] [PubMed] [Google Scholar]
- 17. Mozaffarian D, Hao T, Rimm EB et al. (2011) Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med 364, 2392–2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Romaguera D, Angquist L, Du H et al. (2011) Food composition of the diet in relation to changes in waist circumference adjusted for body mass index. PLoS One 6, e23384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Malik VS, Schulze MB & Hu FB (2006) Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr 84, 274–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Australian Bureau of Statistics (2014) 4402.0 – Childhood Education and Care, Australia, June 2014. http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4402.0June%202014?OpenDocument (accessed August 2016).
- 21. Benjamin Neelon SE & Briley ME (2011) Position of the American Dietetic Association: benchmarks for nutrition in child care. J Am Diet Assoc 111, 607–615. [DOI] [PubMed] [Google Scholar]
- 22. Healthy Eating Advisory Service (2016) Menu planning guidelines for long day care. http://heas.health.vic.gov.au/sites/default/files/ECS-Menu-planning-guidelines-LDC.pdf (accessed August 2016).
- 23. O’Halloran SA, Lacy KE, Grimes CA et al. (2017) A novel processed food classification system applied to Australian food composition databases. J Hum Nutr Diet (Epublication ahead of print version). [DOI] [PubMed]
- 24. Department of Health and Ageing, National Health and Medical Research (2013) Eat for Health Australian Dietary Guidelines. Canberra, ACT: Commonwealth of Australia. [Google Scholar]
- 25. Moubarac JC, Parra DC, Cannon G et al. (2014) Food classification systems based on food processing: significance and implications for policies and actions: a systematic literature review and assessment. Curr Obes Rep 3, 256–272. [DOI] [PubMed] [Google Scholar]
- 26. Food Standards Australia New Zealand (2015) AUSNUT 2011–13. http://www.foodstandards.gov.au/science/monitoringnutrients/ausnut/Pages/about.aspx (accessed August 2016).
- 27. James WP, Ralph A & Sanchez-Castillo CP (1987) The dominance of salt in manufactured food in the sodium intake of affluent societies. Lancet 329, 426–429. [DOI] [PubMed] [Google Scholar]
- 28. O’Halloran SA, Grimes CA, Lacy KE et al. (2016) Dietary sources and sodium intake in a sample of Australian preschool. BMJ Open 6, e008698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sparrenberger K, Friedrich RR, Schiffner MD et al. (2015) Ultra-processed food consumption in children from a Basic Health Unit. J Pediatr 91, 535–542. [DOI] [PubMed] [Google Scholar]
- 30. Tavares LF, Fonseca SC, Garcia Rosa ML et al. (2012) Relationship between ultra-processed foods and metabolic syndrome in adolescents from a Brazilian Family Doctor Program. Public Health Nutr 15, 82–87. [DOI] [PubMed] [Google Scholar]
- 31. Pan American Health Organization (2015) Ultra-Processed Food and Drink Products in Latin America: Trends, Impact on Obesity, Policy Implications. Washington, DC: PAHO; available at http://www.paho.org/hq/index.php?option=com_content&view=article&id=11153%3Aultra-processed-food-and-drink-products&catid=7587%3Ageneral&Itemid=40601&lang=en [Google Scholar]
- 32. Epstein LH, Paluch RA, Beecher MD et al. (2008) Increasing healthy eating vs. reducing high energy-dense foods to treat pediatric obesity. Obesity (Silver Spring) 16, 318–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ness AR, Maynard M, Frankel S et al. (2005) Diet in childhood and adult cardiovascular and all cause mortality: the Boyd Orr cohort. Heart 91, 894–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Maynard M, Gunnell D, Emmett P et al. (2003) Fruit, vegetables, and antioxidants in childhood and risk of adult cancer: the Boyd Orr cohort. J Epidemiol Community Health 57, 218–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sanigorski AM, Bell AC, Kremer PJ et al. (2005) Lunchbox contents of Australian school children: room for improvement. Eur J Clin Nutr 59, 1310–1316. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S136898001700132X.
click here to view supplementary material