Abstract
Objective
Food pantries play a critical role in combating food insecurity. The objective of the present work was to systematically review and synthesize scientific evidence regarding the effectiveness of food pantry-based interventions in the USA.
Design
Keyword/reference search was conducted in PubMed, Web of Science, Scopus, Cochrane Library and CINAHL for peer-reviewed articles published until May 2018 that met the following criteria. Setting: food pantry and/or food bank in the USA; study design: randomized controlled trial (RCT) or pre–post study; outcomes: diet-related outcomes (e.g. nutrition knowledge, food choice, food security, diet quality); study subjects: food pantry/bank clients.
Results
Fourteen articles evaluating twelve distinct interventions identified from the keyword/reference search met the eligibility criteria and were included in the review. Five were RCT and the remaining seven were pre–post studies. All studies found that food pantry-based interventions were effective in improving participants’ diet-related outcomes. In particular, the nutrition education interventions and the client-choice intervention enhanced participants’ nutrition knowledge, cooking skills, food security status and fresh produce intake. The food display intervention helped pantry clients select healthier food items. The diabetes management intervention reduced participants’ glycaemic level.
Conclusions
Food pantry-based interventions were found to be effective in improving participants’ diet-related outcomes. Interventions were modest in scale and usually short in follow-up duration. Future studies are warranted to address the challenges of conducting interventions in food pantries, such as shortage in personnel and resources, to ensure intervention sustainability and long-term effectiveness.
Keywords: Food pantry, Food bank, Diet, Intervention, Systematic review
Food insecurity, a lack of reliable access to a sufficient quantity of affordable, nutritious food, impacts over one-eighth of American households, with highest rates among households with incomes below the federal poverty level( 1 ). Food insecurity is associated with poor dietary quality and elevated disease risks( 2 , 3 ). Food banks in the USA typically operate as warehouses that store a large quantity and variety of food items to be distributed by smaller front-line agencies, called food pantries, which directly serve the end users free of charge. Food banks and food pantries in the USA distribute free grocery items to over 46·5 million Americans in need annually( 4 , 5 ). Estimations of food insecurity among pantry clients in the USA range from 50 to 84%( 5 – 7 ). Food pantries are often used to augment the Supplemental Nutrition Assistance Program (SNAP) benefits( 7 , 8 ). However, some clients use food pantries as their primary or sole food source, partially due to SNAP ineligibility( 9 ). Food pantries play a critical role in addressing the needs of Americans at high risk of food insecurity( 10 ).
Besides emergency food provision, food pantries may serve as a natural setting and focal point where additional services can be delivered to improve the diet and health status of the highly vulnerable client population. Previous reviews on food pantries largely focused on cross-sectional studies that assessed the nutritional values of foods provided, service types and quality, and client characteristics (e.g. food security status, dietary intake, malnutrition status, health or disease status, and frequencies or reasons for food pantry use)( 6 , 11 , 12 ). One prospective review intends to survey outcomes of disease prevention and management interventions in food pantries, but the review does not assess health behaviour (e.g. food choice) and results have yet to be reported( 13 ). The purpose of the present study was to systematically review and synthesize scientific evidence regarding the effectiveness of food pantry-based interventions on diet-related outcomes in the USA. We focused on food pantries in the USA because the types and ways of operation of food banks and pantries differ substantially across countries, and they are also subject to different government regulations and serve diverse populations.
Methods
The systematic review was reported in accordance with the PRIMSA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement( 14 ). Analysis was conducted in May 2018.
Data sources
A keyword search was performed in five electronic bibliographic databases: (i) PubMed; (ii) Web of Science; (iii) Scopus; (iv) Cochrane Library; and (v) Cumulative Index to Nursing and Allied Health Literature (CINAHL). The search algorithm included all the following keywords: ‘food pantry’, ‘food pantries’, ‘food bank’, ‘food banks’, ‘food shelf’, ‘food shelves’, ‘food cupboard’, ‘food cupboards’ and ‘food assistance’. The MeSH (medical subject heading) term ‘food assistance’ was included in the PubMed search. All keywords in the PubMed were searched with the ‘(All fields)’ tag, which are processed using Automatic Term Mapping( 15 ). The Appendix documents the search algorithm in PubMed as an example. The search function ‘TS=Topic’ was used in Web of Science, which launches a search for topic terms in the fields of title, abstract, keywords and Keywords Plus®( 16 ). Titles and abstracts of the articles identified through the keyword search were screened against the study selection criteria. Potentially relevant articles were retrieved for evaluation of the full text. Two reviewers, J.W. and J.S., independently conducted title and abstract screening and identified potentially relevant articles. Inter-rater agreement was assessed using the Cohen’s kappa (κ=0·82). Discrepancies were resolved through face-to-face discussions between R.A., J.W. and J.S.
A reference list search (i.e. backward reference search) and a cited reference search (i.e. forward reference search) were conducted based on the full-text articles meeting the study selection criteria that were identified from the keyword search. Articles identified from the backward and forward reference search were further screened and evaluated using the same study selection criteria. The reference search was repeated on newly identified articles until no additional relevant article was found.
Study selection
Studies that met all of the following criteria were included in the review. (i) Setting: food pantry and/or food bank in the USA; (ii) exposure: any intervention that addresses food pantry clients’ diet-related outcomes (e.g. nutrition knowledge, food choice, food security, diet quality), except for the daily work routine of a food pantry (i.e. food service) or food bank (i.e. food storage and distribution); (iii) study design: randomized controlled trial (RCT) or pre–post study; (iv) study subjects: food pantry/bank clients; (v) article type: peer-reviewed publication; (vi) time window of search: from the inception of an electronic bibliographic database to 28 May 2018; and (vii) language: article written in English.
Studies that met any of the following criteria were excluded from the review: (i) food pantry/bank-related observational studies; (ii) non-peer-reviewed articles; (iii) articles not written in English; or (iv) letters, editorials, study/review protocols or review articles.
Data extraction
A standardized data extraction form was used to collect the following methodological and outcome variables from each included study: authors, publication year, study design, sample size, age range, percentage of women, duration of follow-up, setting, intervention type, intervention components, measures, outcomes, statistical models, covariates adjusted for and estimated intervention effectiveness.
Data synthesis
A tabulation of extracted data revealed that no two interventions provided a quantitative estimate for the same outcome measure. This precluded a meta-analysis. We narratively summarized the common themes and findings of the included studies.
Study quality assessment
We used the National Institutes of Health’s Quality Assessment Tool of Controlled Intervention Studies to assess the quality of each included study( 17 ). This assessment tool rates each study based on fourteen criteria. For each criterion, a score of 1 was assigned if ‘yes’ was the response, whereas a score of 0 was assigned otherwise (i.e. an answer of ‘no’, ‘not applicable’, ‘not reported’ or ‘cannot determine’). Study quality assessment helped measure the strength of scientific evidence but was not used to determine the inclusion of studies.
Results
Study selection
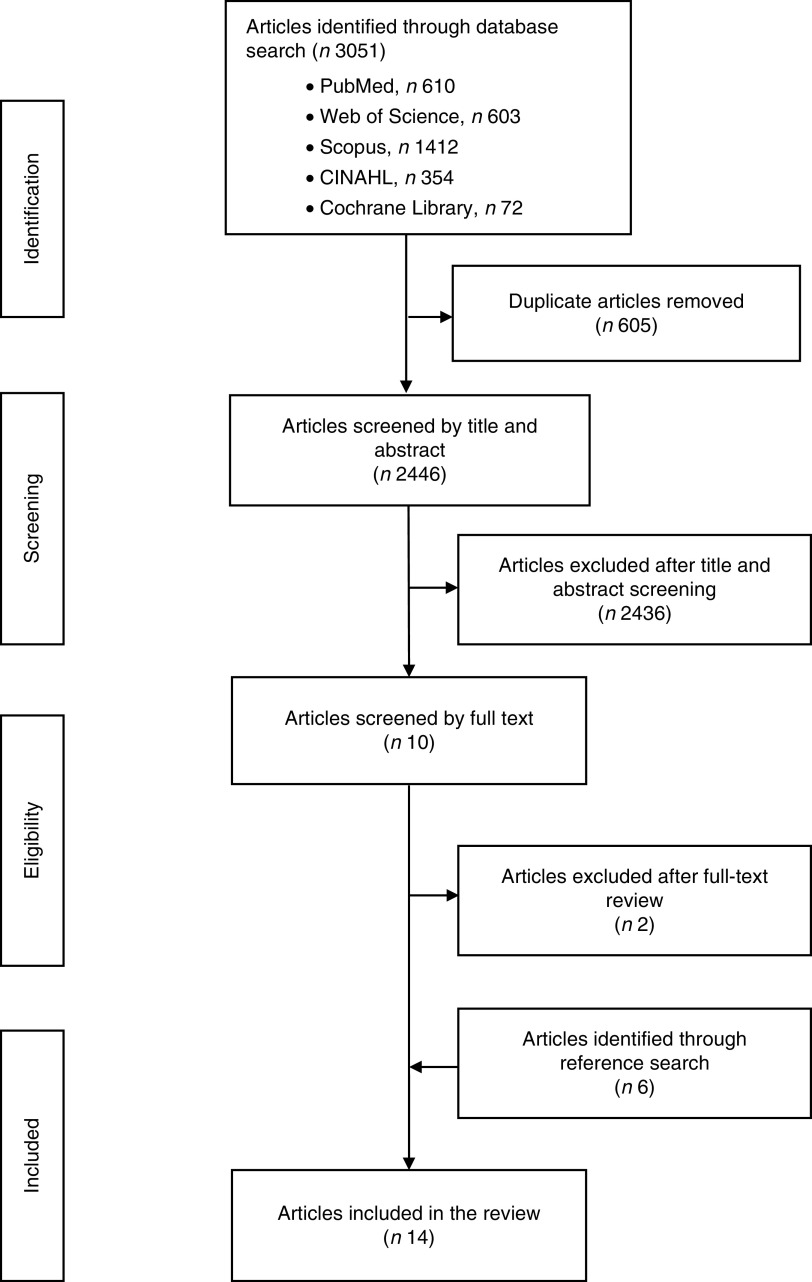
Figure 1 shows the study selection flowchart. We identified 3051 articles in total by the keyword search, including 610 articles from PubMed, 603 articles from Web of Science, 1412 from Scopus, 354 articles from CINAHL and seventy-two articles from Cochrane Library. After removing duplicates, 2446 unique articles entered title and abstract screening, of which 2436 articles were excluded. The full texts of the remaining ten articles were reviewed against the study selection criteria( 18 – 27 ) and two studies were excluded because they were other types of interventions (i.e. smoking cessation and medical referral) rather than diet-related interventions( 19 , 23 ). A forward and backward reference search was conducted based on these eight articles and six new articles were identified that met the study selection criteria( 28 – 33 ). Therefore, these fourteen articles consist of the final pool of studies included in the review( 18 , 20 – 22 , 24 – 33 ).
Fig. 1.
Flowchart showing study selection for the current review of food pantry-based interventions in the USA
Summary of the selected studies
Table 1 summarizes the basic characteristics of the fourteen articles evaluating twelve distinct interventions included in the review. All of them were published within the past 12 years. Seven studies adopted a pre–post study design and five adopted an RCT study design. Sample size varied substantially across studies. Two articles had a sample size between forty and 100 participants( 20 , 24 ), seven had a sample size between 100 and 500 participants( 18 , 22 , 25 , 29 – 32 ), three articles had a sample size between 500 and 1000 participants( 21 , 26 , 28 ), one had a sample size between 1000 and 2000 participants( 27 ), whereas the remaining one recruited 375 families( 33 ). The mean and median sample sizes were 429 and 236, respectively, except for one study that did not report its sample size in detail( 33 ). All studies but one( 33 ) focused exclusively on adults aged 18 years or above. Among the nine articles that reported sex distribution, women accounted for over half (53–100%) of the analytic sample( 20 – 22 , 24 , 25 , 28 , 29 , 31 , 32 ). Four articles recruited participants with diabetes( 21 , 22 , 25 , 28 ), three articles recruited participants with hypertension( 22 , 25 , 28 ), two articles recruited participants with obesity( 22 , 25 ) and one article recruited participants with heart disease( 28 ).
Table 1.
Basic characteristics of the studies included in the current review of food pantry-based interventions in the USA
| Study | Study design | Sample size | Age (years) | Sex | Disease status | Follow-up duration (weeks) | Setting | Type of intervention |
|---|---|---|---|---|---|---|---|---|
| Wilson et al. (2017)( 18 ) | RCT | 443 | Range: ≥18 | 3 | Food pantry | Food packaging intervention | ||
| Caspi et al. (2017)( 20 ) | Pre–post | 45 | Mean (sd): 42 (12·7) Range: 19–67 | M: 6 (13%) F: 39 (87%) | 6 | Food shelves | Cooking and nutrition education | |
| Martin et al. (2016)( 29 ) | RCT | 227 | Mean (sd): 51·4 (11·9) | M: 92 (40·5%) F: 135 (59·5%) | 72 | Food pantry | Freshplace intervention | |
| Clarke and Evans (2016)( 30 ) | RCT | 236 | Range: ≥18 | 1 | Food pantry | Vegetable, recipes and food-use tips | ||
| Seligman et al. (2015)( 21 ) | Pre–post | 687 | Mean: 56·6 | M: 179 (26%) F: 508 (74%) | Diabetes | 24 | Food bank | Diabetes-appropriate food intervention |
| Martin et al. (2013)( 22 ) | RCT | 228 | Control group: Mean (sd): 51·2 (11·8) Experiment group: Mean (sd): 51·8 (12·0) | M: 92 (40%) F: 136 (60%) | Control group: Diabetes: 28 (24%) High blood pressure: 72 (63%) Overweight/obesity: 83 (74%) Experimental group: Diabetes: 31 (27%) High blood pressure: 77 (68%) Overweight/obesity: 76 (68%) | 52 | Food pantry | Freshplace intervention |
| Flynn et al. (2013)( 24 ) | Pre–post | 63 | Mean (sd): 51·8 (16·6) | M: 10 (16%) F: 53 (84%) | 6 | Food pantry and low-income housing site | Cooking demonstration and nutrition education | |
| Yao et al. (2013)( 31 ) | Pre–post (with a control group) | 409 | Range: 18–91 Control group: Mean: 45 Experiment group: Mean: 41 | Control group: M: 4 (2%) F: 194 (98%) Experiment group: M: 4 (2%) F: 201 (98%) | 4 | Community cupboard pantry | Nutrition education | |
| Martin et al. (2012)( 25 ) | RCT | 233 | Range: ≥18 Mean: 51 | Control group (n 114): M: 48 (42%) F: 66 (58%) Experiment group (n 112): M: 44 (39%) F: 68 (61%) | Control group: Household member with diabetes: 30 (27%) Household member with high blood pressure: 76 (68%) Overweight: 25 (29%) Obesity: 31 (36%); Experiment group: Household member with diabetes: 28 (25%) Household member with high blood pressure: 71 (62%) Overweight: 32 (38%) Obesity: 31 (37%) | 72 | Food pantry | Freshplace intervention |
| Clarke et al. (2011)( 26 ) | RCT | 706 | Range: ≥18 | 6 | Food pantry | Nutrition education and recipe provision | ||
| Biel et al. (2009)( 27 ) | Pre–post | 1087 | Range: ≥18 | Urban food pantry: 83 (22%) require referral for care Rural food pantry: 196 (28%) require referral for care | One urban food pantry and one rural food pantry | Nutrition education and cooking demonstration | ||
| Eicher-Miller et al. (2009)( 32 ) | RCT | 219 | Range: ≥18 | F: 219 (100%) | 5 | Client homes and community locations | Food stamp nutrition education | |
| Greder et al. (2007)( 28 ) | Pre–post | 997 | Median: 41 | M: 469 (47%) F: 528 (53%) | Household member with diabetes: 239 (24%) Household member with heart disease: 70 (7%) Household member with high blood pressure: 329 (33%) Household member with asthma: 289 (29%) Household member with allergies: 339 (34%) | Food pantry | Nutrition education | |
| Miyamoto et al. (2006)( 33 ) | Pre–post | 375 families | Range: ≥4 | 8 | Food pantry | Nutrition education |
RCT, randomized controlled trial; M, male; F, female.
Table 2 summarizes intervention type, intervention components, outcome measures, statistical models and estimated intervention effectiveness on diet-related outcomes. Nutrition education (n 9) was the most common type of intervention( 20 , 24 – 28 , 31 – 33 ), followed by client-choice intervention (called ‘Freshplace’; n 3)( 22 , 25 , 29 ), food display intervention (n 1)( 18 ) and diabetes management intervention (n 1)( 21 ). The nutrition education interventions included nutrition knowledge dissemination (e.g. healthy eating plate, nutrition facts label use, nutritional implications of different fat types, relationship between nutrition and health, and healthy recipes using fresh produce)( 20 , 24 – 28 , 31 – 33 ) and cooking demonstrations( 24 , 27 ). In the nutrition education interventions, extension staff and local volunteers provided education pertaining to various nutrition-related facts and knowledge (e.g. read food labels, understand different types of fats) for low-income families( 20 ). Study investigators created a software to provide messages regarding tailored recipes and food-use tips for pantry clients( 26 , 33 ). Food pantry staff were trained about the relationship between nutrition and chronic diseases in order to provide healthier pantry food options( 28 ). A food safety-certified graduate assistant served whole-grain dish along with the recipe, informed clients regarding the whole-grain ingredients in the recipe and asked them to make half their grains whole on a daily basis( 31 ). In the cooking demonstration, study investigators provided cooking classes for low-income people who would like to try new recipes( 22 ). The staff did a cooking demonstration to show how one could prepare healthy recipes using the fresh produce offered and distributed the recipes to pantry clients( 27 ). The client-choice intervention (‘Freshplace’) included three major components: (i) participants chose their own foods (primarily fresh and perishable food items); (ii) met with a project manager once per month to develop and track personal goals for becoming food secure and self-sufficient; and (iii) received services tailored to their individual needs (e.g. a six-week cooking workshop)( 22 , 25 , 29 ). In the food display intervention, researchers manipulated the display of a targeted product (i.e. protein bar) in a food pantry – placing the product in the front or the back of the category line and presenting the product in its original box or unboxed – with the goal of encouraging the selection of targeted foods through ‘nudges’ but without restricting choices( 1 ). In the diabetes management intervention, food pantry clients with diabetes were provided with diabetes-appropriate foods, blood sugar monitoring, primary care referral and self-management support by project personnel who were registered dietitians or certified diabetes educators( 21 ).
Table 2.
Intervention components, measures, statistical models and estimated effects on diet and health outcomes of the studies included in the current review of food pantry-based interventions in the USA
| Study | Intervention components | Data collection method | Outcomes | Statistical models | Covariates adjusted | Estimated effectiveness of food pantry-based interventions |
|---|---|---|---|---|---|---|
| Wilson et al. (2017)( 18 ) | Allocation of protein bar (front or back), boxed or unboxed (front–boxed, front–unboxed, back–boxed, back–unboxed) in relation to clients’ choice | Researchers’ observation | Take rate (the proportion of clients that selected the targeted item), binary choice ratios | Logistic regression | Order and packaging | Nudges increased uptake of the targeted food. The findings also hold when authors controlled for a potential confounder. Low-cost and unobtrusive nudges can be effective tools for food pantry organizers to encourage the selection of targeted foods (OR of intervention=4·739; 95% CI 2·269, 9·898; P<0·001) |
| Caspi et al. (2017)( 20 ) | 6-week cooking and nutrition education class | Telephone interview or face-to-face (e.g. 24 h dietary recall) | Cooking skills | Paired t test, intent-to-treat analysis | Participants demonstrated improved cooking skills scores post-intervention (P=0·002). This study provides some evidence that improvements in diet and skills can be demonstrated with minimal intervention | |
| Martin et al. (2016)( 29 ) | Providing fresh food (including fruits, vegetables, meat and dairy), assistance with housing, education, health care, employment and other basic needs; asking participants to attend the case management meeting | Questionnaire and measurement | Household food security, self-efficacy for food security scale | Hierarchical linear modelling, bivariate analyses, Cronbach α test | Age, gender, Freshplace participation | There was no significant difference in the rate of very low food security in the Freshplace intervention group (51·8%) compared with the controls (47·8%). Self-efficacy was significantly inversely associated with very low food security (P<0·05). Being in the Freshplace intervention (P=0·01) and higher self-efficacy (P=0·04) were independently associated with decreased very low food security |
| Clarke and Evans (2016)( 30 ) | All pantries received additional free vegetables; in addition, pantries in the other conditions received recipes and food-use tips | Telephone interview | Preparing vegetables, methods of cooks, uses of fats and salt | Among the experiment’s ten vegetables, some were used twice as often as others. Cooks practised a narrow repertoire of preparation methods, dominated by boiling and steaming, across most of the vegetables. Fats and salt were often added to boiled and steamed preparations | ||
| Seligman et al. (2015)( 21 ) | Diabetes-appropriate food, blood sugar monitoring, primary care referral, self-management support (recipes and cooking tips) | Blood glucose testing and HbA1c testing | HbA1c, diabetes self-management behaviours, diabetes self-efficacy, adherence, participants’ satisfaction with the food box | t test, χ 2 test | Age, sex, race/ethnicity, education, language, site | Improvements were seen in pre–post analyses of glycaemic control (HbA1c decreased from 8·11 to 7·96%; P<0·01), fruit and vegetable intake (which increased from 2·8 to 3·1 servings/d; P<0·01). Among participants with elevated HbA1c (at least 7·5%) at baseline, HbA1c improved from 9·52 to 9·04% (P<0·001). The proportion of participants with very poor glycaemic control (HbA1c>9%) declined from 28 to 25% (P<0·10) |
| Martin et al. (2013)( 22 ) | Client-choice pantry, monthly meetings with a project manager to receive motivational interviewing, targeted referrals to community services | Self-report and questionnaire (e.g. Block Food Frequency Screener) | Food security, self-sufficiency, fruit and vegetable consumption | Multivariate regression model, bivariate analysis, χ 2 test, t test, general linear mixed model | Gender, age, household size, income, presence of children in the household | At baseline, half of the sample experienced very low food security. Over 1 year, Freshplace members were less than half as likely to experience very low food security, increased self-sufficiency by 4·1 points, and increased fruits and vegetables by 1 serving/d compared with the control group (P<0·01 for all outcomes) |
| Flynn et al. (2013)( 24 ) | Provision of plant-based recipes that use extra virgin olive oil (6 weeks of cooking classes), consulting dietitians | Questionnaire and measurement | Grocery receipt for all foods purchased, BMI, waist circumference | t test, Wilcoxon signed-rank test | Total variety of vegetables and fruit intake increased (P<0·01 for both). Grocery receipts showed a decrease in purchases of meat, carbonated beverages, desserts, snacks and total groceries (all P<0·01). Food insecurity score decreased from baseline (P<0·01), as did BMI (P=0·05) | |
| Yao et al. (2013)( 31 ) | Trained volunteers shared whole-grain messages orally, then provided recipe with a bag of ingredients for clients | Telephone survey | Consumption of whole-grain foods, self-efficacy in choosing and preparing foods | Descriptive statistics, Cronbach’s α coefficient, logistic regression | Age, meal preparation experience, family size and number of children | Both perception of whole-grain consumption and self-efficacy improved significantly for the intervention group compared with the control group (P=0·001 and P<0·03, respectively). |
| Martin et al. (2012)( 25 ) | Client-choice pantry, monthly meetings with a project manager to receive motivational interviewing, and targeted referrals to community services, 6-week cooking class, nutrition education | Questionnaire | Food security, self-sufficiency, diet quality | t test, bivariate analysis, χ 2 test | Over 3 months, Freshplace members had larger change than the comparison group in food security scores (1·6 v. 0·7 points; P<0·01) and fruit and vegetable intake (1·9 v. –1·4 points; P<0·01) | |
| Clarke et al. (2011)( 26 ) | Recipes and food tips, vegetables | Questionnaire and telephone interview | Consumption of fresh vegetables, food-use booklet retention and use | χ 2 test, t test, ANOVA | Language preference, restaurant/fast-food places, household size, employment status | Results demonstrated benefits of tailoring over both generic and control conditions and uncovered the degree of tailoring that produced the largest effects (P<0·001). The intervention addressed recipients’ immediate and concrete decisions about healthy eating, instead of distant or abstract goals like prevention of illnesses. The study documented per-client costs of tailored information. Results also suggested that benefits from social capital at sites offering a health outreach may exceed the impact of message tailoring on outcomes of interest |
| Biel et al. (2009)( 27 ) | Display the message about the associations between diet and health, cooking demonstration, provision of fresh food | Staff registration | Number of clinic visits | Pantries and nearby clinics can be brought into collaboration to meet common goals in preventing diet-related illnesses and helping people with such conditions effectively access needed health care. Clinics can effectively partner with food pantries, an overlooked resource for health promotion | ||
| Eicher-Miller et al. (2009)( 32 ) | Food stamp nutrition education mainly including MyPyramid, food groups, food safety, shopping behaviours and resource management, and wellness | Questionnaire | Food insecurity, food insufficiency | χ 2 test, Satterthwaite t test | Food sufficiency pre-test score, employment | Food insecurity and food insufficiency in the experimental group compared with the control group were significantly improved (P=0·03 and P=0·04, respectively) |
| Greder et al. (2007)( 28 ) | Nutrition education programme | Questionnaire | Diabetes, heart disease, high blood pressure, asthma, allergies | A nutrition education programme designed to meet specific nutrition- and health-related needs of pantry participants was developed. Implications include training pantry staff about chronic disease and its relationship to nutrition, identifying pantry foods that provide positive health benefits, and developing consumer publications focused on selecting and preparing pantry foods when one has chronic disease | ||
| Miyamoto et al. (2006)( 33 ) | Nutrition education materials focusing on choosing nutritious foods and safe food handling | Oral survey | Food safety, proper hand washing | Of the adult participants, 50% reported preparing the dishes at home; 20% reported enjoying the food, did not prepare the recipe, but intended to do so in the future. Participants reported increasing the frequency of hand washing before preparing and consuming food |
HbA1c, glycated Hb.
Two of the fourteen articles adopted one or more biometric outcome measures (e.g. BMI calculated from measured height and weight, glycaemic level and blood pressure)( 21 , 24 ), and the remaining twelve articles adopted subjective outcome measures using questionnaires (n 5)( 22 , 25 , 28 , 29 , 32 ), face-to-face or telephone-based interviews (n 5, including a 24 h dietary recall( 20 ))( 20 , 26 , 30 , 31 , 33 ), staff registration (n 1)( 27 ) and researchers’ observation (n 1)( 18 ). One of the fourteen articles adopted both biometric and subjective measures (e.g. interview and biometric measures)( 24 ). Statistical tests and models applied included the t test, χ 2 test, Cronbach α test, Wilcoxon signed-rank test, linear regression, logistic regression, ANOVA, hierarchical linear modelling and generalized linear mixed model.
All twelve studies included in the review found improvements in diet, cooking skills, food security, nutrition knowledge and/or health outcomes attributable to food pantry-based interventions. Among these studies, four reported positive qualitative outcomes linking the food pantry-based intervention to improved cooking skills( 30 ), medical care( 27 ), nutrition knowledge( 28 ) and/or dietary quality among study participants( 33 ). The remaining eight studies that applied statistical tests and models reported a statistically significant positive association between the food pantry-based intervention and diet quality, cooking skills, food security, nutrition knowledge and/or health outcomes( 18 , 20 – 22 , 24 – 26 , 29 , 31 , 32 ). The nutrition education interventions and the client-choice intervention were found to improve participants’ nutrition knowledge, cooking skills, food security status and fresh produce intake( 20 , 22 , 24 – 29 , 31 – 33 ). The food display intervention was found to significantly help pantry clients select healthier food items( 18 ). The diabetes management intervention was found to significantly help participants better control their glycaemic level( 21 ). More specifically, the glycaemic control intervention was more effective among the subset of participants with glycated Hb (HbA1c) ≥7·5% at baseline (i.e. improved by 0·48 percentage points) than those with diabetes in general (i.e. improved by 0·15 percentage points)( 21 ). The only study that assessed BMI reported a reduction in BMI among food pantry clients following a six-week cooking programme of plant-based recipes, but the estimated intervention effect was only marginally significant (P=0·05)( 24 ).
Study quality assessment
Table 3 reports criterion-specific ratings from the study quality assessment. All fourteen articles included in the review clearly stated the research question/objective, clearly specified and defined the study population, recruited subjects from the same or similar populations during the same time period, pre-specified and uniformly applied inclusion and exclusion criteria to all participants, had a reasonably long follow-up period that was sufficient for changes in outcomes to be observed, and implemented valid and reliable exposure and outcome measures. On the other hand, none of them examined the dose–response effect of food pantry-based interventions, and few justified their sample size and/or conducted a power calculation( 18 , 26 ). Three articles had the outcome assessors blinded to the exposure status of the participants( 18 , 21 , 24 ). Four articles had an attrition rate less than 20%( 18 , 22 , 25 , 26 ). Seven articles had a participation rate above 50%( 22 , 25 , 26 , 29 – 32 ), assessed the exposures more than once during the study period( 20 – 22 , 24 – 26 , 29 ), and measured and statistically adjusted key potential confounding variables for their impact on the relationship between exposures and outcomes( 18 , 21 , 22 , 26 , 29 , 31 , 32 ).
Table 3.
Quality assessment* of the studies included in the current review of food pantry-based interventions in the USA
| Criterion | Wilson et al. (2017)( 18 ) | Caspi et al. (2017)( 20 ) | Martin et al. (2016)( 29 ) | Clarke and Evans (2016)( 30 ) | Seligman et al. (2015)( 21 ) | Martin et al. (2013)( 22 ) | Flynn et al. (2013)( 24 ) | Martin et al. (2012)( 25 ) | Yao et al. (2013)( 31 ) | Clarke et al. (2011)( 26 ) | Biel et al. (2009)( 27 ) | Eicher-Miller et al. (2009)( 32 ) | Greder et al. (2007)( 28 ) | Miyamoto et al. (2006)( 33 ) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Was the research question or objective in this paper clearly stated? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 2. Was the study population clearly specified and defined? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 3. Was the participation rate of eligible persons at least 50%? | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 |
| 4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study pre-specified and applied uniformly to all participants? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 5. Was a sample size justification, power description, or variance and effect estimates provided? | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| 6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 |
| 7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g. categories of exposure or exposure measured as continuous variable)? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 9. Were the exposure measures (independent variables) clearly defined, valid, reliable and implemented consistently across all study participants? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 10. Was the exposure(s) assessed more than once over time? | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 |
| 11. Were the outcome measures (dependent variables) clearly defined, valid, reliable and implemented consistently across all study participants? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 12. Were the outcome assessors blinded to the exposure status of participants? | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 13. Was loss to follow-up after baseline 20 % or less? | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 |
| 14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 |
The study quality assessment tool was adopted from the National Institutes of Health’s Quality Assessment Tool of Controlled Intervention Studies. For each criterion, a score of 1 was assigned if ‘yes’ was the response, whereas a score of 0 was assigned otherwise. Study quality assessment helped measure strength of scientific evidence but was not used to determine the inclusion of studies.
Discussion
The present study systematically reviewed scientific evidence regarding food pantry-based interventions on participants’ diet-related outcomes in the USA. A total of fourteen articles evaluating twelve distinct interventions were identified. Seven studies adopted a pre–post study design and the remaining five adopted an RCT design. Nine studies focused on nutrition education interventions, one study focused on client-choice intervention, one study focused on food display intervention and the remaining one focused on diabetes management intervention. The review findings demonstrated the feasibility and preliminary effectiveness of these food pantry-based interventions in producing a wide range of positive outcomes such as improved nutrition and health literacy, food security, cooking skills, healthy food choices and intake, diabetes management and access to community resources.
Since the current review was conducted, Seligman et al. (2018)( 34 ) reported that food banks positively impacted food security, food stability and fruit/vegetable intake among participants. However, no differences in self-management (i.e. depressive symptoms, diabetes distress, self-care, hypoglycaemia and self-efficacy) or HbA1c were identified. On the one hand, findings from Seligman et al. (2018)( 34 ) help strengthen the evidence regarding the effectiveness of food pantry-based interventions on food security and dietary quality. On the other hand, the null findings contradicted previous positive findings pertaining to improved HbA1c reported in Seligman et al. (2015)( 21 ). Future studies should be conducted to assess this discrepancy.
Despite these initially promising results, food pantry-based interventions also face multiple challenges. Largely dependent upon donations and volunteer work, food pantries may have limited resources to provide additional services to clients in need( 6 , 11 , 12 , 35 ). Modifications of health behaviours and outcomes often require moderate to intensive interventions that last for a sustained period, but the shortage in personnel and funding may threaten the sustainability and suitability of food pantry-based interventions. Language and cultural barriers, lack of mutual trust and social stigma may prevent clients from fully engaging in the interventions offered at food pantries( 36 – 40 ). This situation could be further hampered by food pantry staff’s lack of professional training in intervention delivery. A close collaboration between food pantry and health or other professionals might be the key to a successful and sustainable intervention. A potential partnership for these interventions may exist between food pantries and agencies implementing SNAP-Ed (i.e. Supplemental Nutrition Assistance Program–Education), who have staff that specialize in assisting organizations serving low-income populations( 41 ). SNAP-Ed implementing agencies provide free technical assistance and may help bridge the gap between pantry staff or funding shortages and the desire to implement sustained food pantry interventions.
Food insecurity is merely one of the many challenges food pantry clients face on a daily basis. Malnutrition among food pantry users has been strongly correlated with lack of shelter, access barriers to health care and other social resources, unemployment, physical and mental disability, illiteracy, substance abuse and domestic conflict( 42 ). Findings of the current review revealed the potential of food pantry-based interventions in addressing some of the unmet needs of pantry users, especially in the domains of food insecurity and diet quality. The remaining questions are: what else could be done to support this highly vulnerable population, and how could we sustain interventions beyond the conclusion of research funding? Emerging research has explored non-diet related interventions at the food pantry setting, such as smoking cessation and medical referral programmes( 19 , 23 ), in an effort to meet other needs of pantry users beyond food access. In view of the close link between food insecurity and health, Feeding America has started to promote partnerships between food pantries/banks and health-care providers( 43 ). As a pilot programme, a food pantry in Indiana was established in a health clinic to address the health and nutrition needs of senior patients and the neighbouring community( 44 ). Sustainability of an intervention is largely determined by the abundance and stability of financial resources that cover the capital and labour cost of the intervention beyond the phase of scientific research. Demonstrating the intervention effectiveness and cost-effectiveness is of importance, but it alone may not be sufficient to attract and sustain long-term investment. Building a healthy partnership with other non-profit or for-profit institutes could help sustain the intervention in the long run if that is of their common interest. The Walmart Foundation has partnered with local food banks/pantries across the nation in a joint effort to improve the quantity and quality of food in the charitable meal system( 45 ). Resource and cost sharing based on partnerships can also play an important role in intervention sustainability. However, two recent studies assessed the network of agencies in local communities that promote healthy eating among populations with limited resources and found that those agencies were only loosely connected( 46 , 47 ).
The current review serves as the first attempt to synthesize scientific evidence regarding food pantry-based interventions on participants’ diet-related outcomes in the USA. Several limitations pertaining to the review and the included studies should be noted. The majority of the selected studies used subjective outcome measures (e.g. questionnaires and face-to-face or telephone-based interviews), which are subject to recall error and social desirability bias( 48 , 49 ). Half of the articles adopted a pre–post study design. In the absence of randomization, their estimated intervention effects could be prone to confounding bias. Research quality varied substantially across studies. Merely two articles justified their sample size and/or conducted a power calculation. It is possible that some studies were underpowered to detect a statistically significant effect. Only four articles had an attrition rate less than 20%, which could be partially explained by the high turnover rate of food pantry clients and the difficulty in tracking them over time. All articles reported positive findings only, whereas it is possible that non-positive and/or inconclusive results were not reported or published (i.e. presence of publication and/or reporting bias). No two articles provided a quantitative effect estimate for the same type of food pantry-based intervention on the same diet-related outcome, which precluded a meta-analysis. None of the included studies assessed the dose–response effect of food pantry-based interventions. The presence of an optimal intervention intensity remains to be tested. Most studies were small in scale and it remains unclear whether some of those interventions are suitable for scaling up to accommodate the population needs. The current review only included published literature. There might be useful and relevant unpublished studies that were missed by the review. Future work could explore grey literature to see whether it could build on the findings from the current review. Biel et al. (2009) explored a collaboration model between community clinics and local food pantries to jointly address the unmet needs of low-income residents( 27 ). However, such partnership is uncommon. Future work should incorporate larger sample sizes and diverse participants, examine the dose–response effect of the intervention, build collaboration with other public or private entities, and design innovative interventions to address other types of unmet needs of food pantry users.
Conclusions
The present work systematically reviewed scientific evidence regarding food pantry-based interventions on clients’ diet-related outcomes. Fourteen articles evaluating twelve distinct interventions were identified from the keyword and reference search, including nine nutrition education interventions, a client-choice intervention, a food display intervention and a diabetes management intervention. All fourteen articles included in the review clearly stated the research question/objective, clearly specified and defined the study population, recruited subjects from the same or similar populations during the same time period, pre-specified and uniformly applied inclusion and exclusion criteria to all participants, had a reasonably long follow-up period that was sufficient for changes in outcomes to be observed, and implemented valid and reliable exposure and outcome measures. On the other hand, none of them examined the dose–response effect of food pantry-based interventions, only two justified their sample size and/or conducted a power calculation, three had the outcome assessors blinded to the exposure status of the participants and four had an attrition rate less than 20%. Findings from these studies demonstrated the feasibility and preliminary effectiveness of food pantry-based interventions in delivering a wide range of positive outcomes including improved nutrition and health literacy, food security, cooking skills, healthy food choices and intake, diabetes management and access to community resources. Future studies are warranted to address the challenges of conducting interventions in food pantries, such as shortage in personnel and resources, to ensure intervention sustainability and long-term effectiveness.
Acknowledgements
Financial support: This research is partially funded by Guangzhou Sport University. Guangzhou Sport University had no role in the design, analysis or writing of this article. Conflict of interest: The authors have no conflict of interest to declare. Authorship: R.A. conceived and designed the study and wrote the manuscript. J.W. and J.L. conducted the literature review and constructed the summary tables and figures. E.L. and J.M. contributed to manuscript drafting. J.S. contributed to manuscript revision. Ethics of human subject participation: This review is non-human subject research and exempt from institutional review board review.
Appendix
Search algorithm in PubMed
‘food pantry’(All Fields) OR ‘food pantries’(All Fields) OR ‘food bank’(All Fields) OR ‘food assistance’(MeSH) AND (‘humans’(MeSH Terms) AND English(lang))
References
- 1. US Department of Agriculture (2016) Household food security in the United States in 2015. Economic Research Report no. ERR-215. https://www.ers.usda.gov/webdocs/publications/79761/err-215.pdf?v=42636 (accessed July 2018).
- 2. Hanson KL & Connor LM (2014) Food insecurity and dietary quality in US adults and children: a systematic review. Am J Clin Nutr 100, 684–692. [DOI] [PubMed] [Google Scholar]
- 3. Laraia BA (2013) Food insecurity and chronic disease. Adv Nutr 4, 203–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rochester JS, Nanney M & Story M (2011) Assessing foodshelves’ ability to distribute healthy foods to foodshelf clients. J Hunger Environ Nutr 6, 10–26. [Google Scholar]
- 5. Feeding America (2018) Feeding America website. http://www.feedingamerica.org/hunger-in-america/ (accessed July 2018).
- 6. Bazerghi C, McKay FH & Dunn M (2016) The role of food banks in addressing food insecurity: a systematic review. J Community Health 41, 732–740. [DOI] [PubMed] [Google Scholar]
- 7. Robaina KA & Martin KS (2013) Food insecurity, poor diet quality, and obesity among food pantry participants in Hartford, CT. J Nutr Educ Behav 45, 159–164. [DOI] [PubMed] [Google Scholar]
- 8. Bhattarai GR, Duffy PA & Raymond J (2005) Use of food pantries and food stamps in low-income households in the United States. J Consum Aff 39, 276–298. [Google Scholar]
- 9. Dave JM, Thompson DI, Svendsen-Sanchez A et al. (2017) Perspectives on barriers to eating healthy among food pantry clients. Health Equity 1, 28–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. RTI International (2014) Current and prospective scope of hunger and food security in America: a review of current research. https://www.rti.org/sites/default/files/resources/full_hunger_report_final_07-24-14.pdf (accessed July 2018).
- 11. Simmet A, Depa J, Tinnemann P et al. (2017) The diet quality of food pantry users: a systematic review of existing literature. J Acad Nutr Diet 117, 563–576. [DOI] [PubMed] [Google Scholar]
- 12. Simmet A, Depa J, Tinnemann P et al. (2017) The nutritional quality of food provided from food pantries: a systematic review of existing literature. J Acad Nutr Diet 117, 577–588. [DOI] [PubMed] [Google Scholar]
- 13. Long CR, Rowland B, Steelman SC et al. (2017) Outcomes of disease prevention and management interventions in food pantries and food banks: protocol for a scoping review. BMJ Open 7, e018022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Moher D, Liberati A, Tetzlaff J et al. (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151, 264–269. [DOI] [PubMed] [Google Scholar]
- 15. US National Center for Biotechnology Information (2017) PubMed Help. https://www.ncbi.nlm.nih.gov/books/NBK3827/ (accessed July 2018).
- 16. Web of Science (2017) Web of Science® Help | Advanced Search Field Tags. https://images.webofknowledge.com/images/help/WOS/hs_advanced_fieldtags.html (accessed July 2018).
- 17. National Institutes of Health (2014) Quality assessment tool of controlled intervention studies. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed July 2018).
- 18. Wilson N, Just DR, Swigert J et al. (2017) Food pantry selection solutions: a randomized controlled trial in client-choice food pantries to nudge clients to targeted foods. J Public Health (Oxf) 39, 366–372. [DOI] [PubMed] [Google Scholar]
- 19. Perkett M, Robson SM, Kripalu V et al. (2017) Characterizing cardiovascular health and evaluating a low-intensity intervention to promote smoking cessation in a food-assistance population. J Community Health 42, 605–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Caspi CE, Davey C, Friebur R et al. (2017) Results of a pilot intervention in food shelves to improve healthy eating and cooking skills among adults experiencing food insecurity. J Hunger Environ Nutr 12, 77–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Seligman HK, Lyles C, Marshall MB et al. (2015) A pilot food bank intervention featuring diabetes-appropriate food improved glycemic control among clients in three states. Health Aff (Millwood) 34, 1956–1963. [DOI] [PubMed] [Google Scholar]
- 22. Martin KS, Wu R, Wolff M et al. (2013) A novel food pantry program food security, self-sufficiency, and diet-quality outcomes. Am J Prev Med 45, 569–575. [DOI] [PubMed] [Google Scholar]
- 23. Larsson LS & Kuster E (2013) Nurse’s desk food bank-based outreach and screening to decrease unmet referral needs. Fam Community Health 36, 285–298. [DOI] [PubMed] [Google Scholar]
- 24. Flynn MM, Reinert S & Schiff AR (2013) A six-week cooking program of plant-based recipes improves food security, body weight, and food purchases for food pantry clients. J Hunger Environ Nutr 8, 73–84. [Google Scholar]
- 25. Martin K, Shuckerow M, O’Rourke C et al. (2012) changing the conversation about hunger: the process of developing Freshplace. Prog Community Health Partnersh 6, 429–434. [DOI] [PubMed] [Google Scholar]
- 26. Clarke P, Evans SH & Hovy EH (2011) Indigenous message tailoring increases consumption of fresh vegetables by clients of community pantries. Health Commun 26, 571–582. [DOI] [PubMed] [Google Scholar]
- 27. Biel M, Evans SH & Clarke P (2009) Forging links between nutrition and healthcare using community-based partnerships. Fam Community Health 32, 196–205. [DOI] [PubMed] [Google Scholar]
- 28. Greder K, Garasky S & Kleinet S (2007) Research to action: a campus-community partnership to address health issues of the food insecure. J Ext 45, issue 6, 6FEA4. [Google Scholar]
- 29. Martin KS, Colantonio AG, Picho K et al. (2016) Self-efficacy is associated with increased food security in novel food pantry program. SSM Popul Health 2, 62–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Clarke P & Evans SH (2016) How do cooks actually cook vegetables? A field experiment with low-income households. Health Promot Pract 17, 80–87. [DOI] [PubMed] [Google Scholar]
- 31. Yao P, Ozier A, Brasseur K et al. (2013) Food pantry nutrition education about whole grains and self-efficacy. Fam Consum Sci Res J 41, 426–437. [Google Scholar]
- 32. Eicher-Miller HA, Mason AC, Abbott AR et al. (2009) The effect of Food Stamp Nutrition Education on the food insecurity of low-income women participants. J Nutr Educ Behav 41, 161–168. [DOI] [PubMed] [Google Scholar]
- 33. Miyamoto A, Chun L, Kanehiro N et al. (2006) Food pantries: food and nutrition education in a non-traditional setting. J Ext 44, issue 1, 1IAW2. [Google Scholar]
- 34. Seligman HK, Smith M, Rosenmoss S et al. (2018) Comprehensive diabetes self-management support from food banks: a randomized controlled trial. Am J Public Health 108, 1227–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gany F, Bari S, Crist M et al. (2013) Food insecurity: limitations of emergency food resources for our patients. J Urban Health 90, 552–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chiu C, Brooks J & An R (2016) Beyond food insecurity. Br Food J 118, 2614–2631. [Google Scholar]
- 37. Algert SJ, Reibel M & Renvall MJ (2006) Barriers to participation in the food stamp program among food pantry clients in Los Angeles. Am J Public Health 96, 807–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lori LN, Elisabetta G & Peter AK (2013) Rural food pantry users’ stigma and safety net food programs. Contemp Rural Soc Work 5, 104–109. [Google Scholar]
- 39. University of Wisconsin–Madison (2013) The cost of free assistance: studying nonuse of food assistance in San Francisco. IRP Discussion Paper no. 1408-13. https://www.irp.wisc.edu/publications/dps/pdfs/dp140813.pdf (accessed July 2018).
- 40. Fuller-Thomson E & Redmond M (2008) Falling through the social safety net: food stamp use and nonuse among older impoverished Americans. Gerontologist 48, 235–244. [DOI] [PubMed] [Google Scholar]
- 41. US Department of Agriculture, Food and Nutrition Service (2016) The Supplemental Nutrition Assistance Program Education (SNAP-Ed) Evaluation Framework | Nutrition, Physical Activity, and Obesity Prevention Indicators | Interpretive Guide to the SNAP-Ed Evaluation Framework. https://snaped.fns.usda.gov/snap/EvaluationFramework/SNAP-EdEvaluationFrameworkInterpretiveGuide.pdf (accessed July 2018).
- 42. Greenberg M, Greenberg G & Mazza L (2010) Food pantries, poverty, and social justice. Am J Public Health 100, 2021–2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Feeding America (2018) Why should we think about food insecurity and health? https://hungerandhealth.feedingamerica.org/explore-our-work/community-health-care-partnerships/ (accessed July 2018).
- 44. Shockley S (2017) A food bank clinic partnership to support senior health. https://hungerandhealth.feedingamerica.org/2017/10/food-bank-clinic-partnership-support-senior-health/ (accessed July 2018).
- 45. Feeding America (2018) How Walmart and the Walmart Foundation are helping us solve hunger. http://www.feedingamerica.org/about-us/partners/food-and-fund-partners/visionary-partners/walmart-and-the-walmart.html (accessed July 2018).
- 46. An R, Loehmer E, Khan N et al. (2017) Community partnerships in healthy eating and lifestyle promotion: a network analysis. Prev Med Rep 6, 294–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. An R, Khan N, Loehmer E et al. (2016) Assessing the network of agencies in local communities that promote healthy eating and lifestyles among populations with limited resources. Am J Health Behav 41, 127–138. [DOI] [PubMed] [Google Scholar]
- 48. Bowling A (2005) Mode of questionnaire administration can have serious effects on data quality. J Public Health (Oxf) 27, 281–291. [DOI] [PubMed] [Google Scholar]
- 49. Kaushal K (2014) Social desirability bias in face to face interviews. J Postgrad Med 60, 415–416. [DOI] [PubMed] [Google Scholar]