Abstract
Objective
Evidence suggests that improvements to the childcare nutrition environment can have a positive impact on child dietary intake. The primary aim of the present study was to assess, relative to usual care, the effectiveness of a multi-strategy implementation intervention in improving childcare compliance with nutrition guidelines. As a secondary aim, the impact on child dietary intake was assessed.
Design
Parallel-group, randomised controlled trial design. The 6-month intervention was designed to overcome barriers to implementation of the nutrition guidelines that had been identified by applying the theoretical domains framework.
Setting
Hunter New England region, New South Wales, Australia.
Subjects
Forty-five centre-based childcare services.
Results
There were no differences between groups in the proportion of services providing food servings (per child) compliant with nutrition guideline recommendations for all five (5/5) food groups at follow-up (i.e. full compliance). Relative to control services, intervention services were more likely to be compliant with guidelines (OR; 95 % CI) in provision of fruit (10·84; 1·19, 551·20; P=0·0024), meat and meat alternatives (8·83; 1·55, –; P=0·023), dairy (8·41; 1·60, 63·62; P=0·006) and discretionary foods (17·83; 2·15, 853·73; P=0·002). Children in intervention services consumed greater servings (adjusted difference; 95 % CI) of fruit (0·41; 0·09, 0·73; P=0·014) and vegetables (0·70; 0·33, 1·08; P<0·001).
Conclusions
Findings indicate that service-level changes to menus in line with dietary guidelines can result in improvements to children’s dietary intake. The study provides evidence to advance implementation research in the setting as a means of enhancing child public health nutrition.
Keywords: Childcare, Nutrition, Children, Diet, Implementation, Guidelines
Dietary risk factors, such as low fruit and vegetable intake and high sodium intake, are a primary cause of death and disability. In 2010, the Global Burden of Disease study reported that over 11 million deaths worldwide were due to dietary risk factors alone( 1 ). Dietary patterns and food preferences developed in childhood are known to track into adulthood and influence the risk of future chronic disease( 2 ). Therefore, developing healthy eating patterns in childhood is recommended by the WHO as a key chronic disease prevention strategy( 3 ).
Childcare services are an important setting for public health intervention. Systematic review evidence suggests that improvements to the childcare nutrition environment can have a positive impact on child dietary intake( 4 ). Australian childcare services are required to comply with licensing and accreditation standards as outlined in the National Quality Framework. There are seven National Quality Standards (NQS) which provide a national benchmark for services, allowing for assessment of the quality of each childcare service. Of particular relevance to the present study is NQS 2, ‘children’s health and safety’, which states that childcare services implement policies and practices to support children’s health and well-being, and makes specific reference to the provision of healthy foods( 5 ). Childcare services also provide access to a large number of children for prolonged periods of time at a critical stage of development( 4 ). In Australia, 52 % of children up to 6 years of age attend formal care at a pre-school or a long day care centre( 6 ) for on average 18 h/week and can consume a large proportion (50–67 %) of their daily dietary requirements during attendance( 7 , 8 ).
Many countries, including Australia, Canada and England, recommend that childcare services provide foods to children consistent with their national dietary guidelines( 9 , 10 ). International and Australian research, however, suggests that foods and beverages provided by services often do not meet dietary guideline recommendations. Assessment of menus from 118 nurseries in England found that all childcare service menus failed to comply with sector nutrition guidelines( 11 ). Furthermore, an analysis of lunch menus from eighty-three childcare centres in Oklahoma, USA concluded that the menus did not provide sufficient carbohydrates, dietary fibre, iron, vitamin D and vitamin E; and provided excessive sodium. Similarly, in Australia, a menu audit of forty-six long day care service menus found that no service provided food that was compliant with all sector nutrition guideline recommendations( 12 ).
Without implementation, childcare dietary guidelines cannot yield improvements in child health. Few trials, however, have been conducted to assess how to best support the implementation of nutrition guidelines in this setting. A recent Cochrane review (2017) found only two randomised trials of interventions targeting the implementation of dietary guidelines( 13 , 14 ). While both studies demonstrate that implementation strategies such as staff professional development and ongoing support may be effective at improving food provision, neither study measured the impact of improving food provision on child dietary intake.
Given the limited research available in this field, the primary aim of the present study was to assess, relative to usual care, the effectiveness of a multi-strategy implementation intervention in improving childcare compliance with nutrition guidelines. As a secondary aim, the impact on service-level child dietary intake was also assessed.
Methods
Ethical approval to conduct the study was obtained from the Hunter New England Human Research Ethics Committee (reference 06/07/26/4.04) and the University of Newcastle Human Research Ethics Committee (reference H-2012-0321). The trial was registered on the Australian New Zealand Clinical Trials Registry (ID: ACTRN12615001032549).
Design and setting
A detailed protocol has been published elsewhere( 15 ). A randomised controlled trial was conducted with childcare services, specifically long day care services in a single local health district in the state of New South Wales, Australia. There are currently 368 childcare services in the study region, of which the 106 long day care services that prepare and provide food onsite to children while in care served as the sampling frame.
Participants
Eligible childcare services were those that prepared and provided one main meal and two mid-meals to children while in care, and that were open for at least 8 h/d. Services that did not prepare and provide meals to children onsite or that did not have a cook with some responsibility for menu planning were excluded. Services catering exclusively for children requiring specialist care, mobile pre-schools and family day care centres were also excluded, given the different operational characteristics of these services compared with centre-based long day care services.
Recruitment procedures
Service managers were mailed information about the study approximately one week prior to recruitment. A random number function in Microsoft® Excel 2010 was used to determine the order at which services were approached to participate in the study. Services were telephoned and consent was obtained through the service manager agreeing to provide the service’s current two-week menu for baseline assessment.
Randomisation and allocation
When consent was obtained via telephone, consenting childcare services were immediately randomly allocated to an intervention or control group in a 1:1 ratio via block randomisation using a random number function in the statistical software package SAS version 9.3. Block size ranged between 2 and 6. All trial outcome data collectors were blinded; however, childcare service staff were aware of their group allocation.
Implementation intervention
The implementation intervention was delivered to participating childcare services over a 6-month period. Given their primary role in menu planning and the food preparation process in such services, long day care service managers and service cooks were the service personnel targeted by the intervention.
The multi-strategy implementation intervention was developed by an experienced team of health promotion practitioners, implementation scientists, dietitians and behavioural scientists in consultation with childcare service cooks and service managers( 16 ). The intervention aimed to increase the implementation of the sector nutrition guidelines by addressing barriers and enablers to the implementation of such guidelines, and was developed based on the Caring for Children resource (which outlines the nutrition guidelines for childcare services in the state of New South Wales included in Table 1)( 17 ), the Theoretical Domains Framework (TDF) and previous research conducted in the childcare setting( 18 – 21 ).
Table 1.
Recommended daily servings of food groups to be provided to children aged 2–5 years who attend childcare for ≥8 h daily in New South Wales, Australia
| Food group | Recommended no. of daily servings to provide |
|---|---|
| Vegetables and legumes/beans | 2 |
| Fruit | 1 |
| Wholegrain cereal foods and breads | 2 |
| Lean meat and poultry, fish, eggs, tofu, seeds and legumes | 0·75 |
| Milk, yoghurt, cheese and alternatives | 1 |
Application of the Theoretical Domains Framework
The TDF( 21 – 24 ) is an integrative theoretical framework of factors considered to influence behaviour change and incorporates thirty-three theories of behaviour change. The framework includes fourteen health behaviour change domains thought to play a role in successful implementation of best practice guidelines and policies, and has been empirically validated in the childcare as well as health-care settings( 18 , 21 , 25 – 30 ). The TDF was used to develop a semi-structured interview, completed with a convenience sample of seven centre-based childcare service cooks, to identify factors (barriers and enablers) that influenced childcare services’ implementation of nutrition guidelines. The factors identified in these interviews informed the selection and design of the implementation intervention strategies.
Intervention strategies
The implementation intervention consisted of the following strategies:
-
1.
Securing executive support( 31 ). A memorandum of understanding outlining each party’s responsibilities to implement the nutrition guidelines was signed by the implementation support officer, the service manager and the service cook. Service managers were also asked to communicate support and endorsement of adhering to nutrition guidelines to other staff and update the service nutrition policy accordingly (if required).
-
2.
Provision of staff training( 32 – 35 ). A one-day face-to-face menu-planning workshop was provided to service managers and cooks aiming to improve their knowledge and skills in the application of nutrition guidelines to childcare food service. The workshop incorporated both didactic and interactive components including small group discussions, case studies, facilitator feedback and opportunities to practice new skills. Experienced implementation support staff and dietitians facilitated the workshop.
-
3.
Provision of resources( 17 ). All intervention services received a resource pack to support the implementation of the nutrition guidelines which included the Caring for Children resource, menu-planning checklists, recipe ideas and budgeting fact sheets.
-
4.
Audit and feedback( 36 ). Intervention services had a dietitian complete an audit of their two-week menus at two time points (baseline and mid-intervention), with written and verbal menu feedback provided at each time point.
-
5.
Implementation support( 37 , 38 ). Intervention services were each allocated an implementation support officer to provide expert advice and assistance to facilitate nutrition guideline implementation. Each implementation support officer offered two face-to-face contacts with the service following the menu-planning workshop. In addition to the support visits, two newsletters were also distributed to intervention services during the intervention period.
Control group
Services randomised to the control group were posted a hard copy of the Caring for Children resource and received usual care from the local health district health promotion staff. The control services did not receive any other implementation support from the research team.
Data collection procedures and measures
Service cook demographics and menu-planning practices
Service cooks were asked to complete a mailed pen-and-paper questionnaire at baseline and follow-up. Data collected by the questionnaire included data regarding the service cook (education level, years employed as a service cook, age, weekly hours worked) and information about their menu-planning processes and the provision of healthy foods (such as how frequently the service plans a menu) in their service. Questionnaire items were adapted from items previously used in a state-based survey of childcare service providers conducted by the research team( 39 ).
Childcare service operational characteristics, nutrition environment and menu-planning practices
Service managers were also asked to complete a pen-and-paper questionnaire mailed to them at baseline and follow-up. The questionnaire captured childcare service operational characteristics (including the hours of operation; the total number of children who are enrolled at the service; and the number of children who attend each day) and the service nutrition environment (including presence of a nutrition policy; role modelling behaviour of staff; and staff provision of positive comments and prompts to children during meal times). The items used in the questionnaire have been used in previous Australian surveys of childcare service managers conducted by the research team( 39 , 40 ).
Primary trial outcomes: compliance with nutrition guidelines
Services provided a copy of their current two-week menu to the research team. An independent dietitian, blinded to group allocation, assessed the menu and calculated servings of food groups per child based on the Australian Guide to Healthy Eating (AGHE) food groups. Menu compliance with nutrition guidelines was assessed via a comprehensive menu assessment undertaken by a dietitian in accordance with best practice protocols at baseline and follow-up( 15 , 41 ). Compliance to the nutrition guidelines was determined based on the calculations of servings of each food group provided per child each day. The calculated servings of each food group were rounded to the nearest 0·25 of a serving.
Two primary trial outcomes were assessed:
-
1.
Full compliance with nutrition guidelines. Guidelines for the sector indicate menus must provide 50 % of the recommended daily servings of the five food groups specified in the AGHE across a two-week menu cycle (ten days). Specifically, to be fully compliant, services must list on their menu each day for two weeks: (i) 2 servings of vegetables and legumes/beans; AND (ii) 1 serving of fruit; AND (iii) 2 servings of wholegrain cereal foods and breads; AND (iv) 0·75 servings of lean meat and poultry, fish, eggs, tofu, seeds and legumes; AND (v) 1 serving of milk, yoghurt, cheese and alternatives (see Table 1)( 16 ). Full compliance was defined as the proportion of services providing food servings (per child) compliant with nutrition guideline recommendations for all five food groups across all ten days of a two-week menu.
-
2.
Compliance with nutrition guidelines for individual AGHE food groups. Six measures were used to assess compliance with nutrition individual guideline recommendations for each of the five food groups specified above and discretionary foods. Discretionary foods are those which are high in kilojoules, saturated fat, added sugars and added salt, and are not recommended for provision in childcare services. Specifically, for this outcome, we assessed the proportion of services providing, across every day of a two-week menu, the recommended servings of each food group listed in Table 1, as well as discretionary foods( 17 ).
Secondary trial outcomes
Two secondary outcomes were also included to provide greater description of any changes occurring in the primary measures of menu compliance. These measures were not prospectively registered:
-
3.
Menu compliance score (mean number of compliant food groups). A score for menu compliance was generated by summing the number of food groups and discretionary foods provided in sufficient quantity to meet guideline recommendations for each service. Mean score could range between 0 and 6, with a score of 1 allocated for each of the food groups of (i) vegetables and legumes/beans; (ii) fruit; (iii) wholegrain cereal foods and breads; (iv) lean meat and poultry, fish, eggs, tofu, seeds and legumes; (v) milk, yoghurt, cheese and alternatives), as well as for ‘discretionary’ foods.
-
4.
Mean number of servings of each food group provided. The mean number of servings of each food group and discretionary foods listed on menus was also assessed.
Theoretical Domains Framework constructs
At post intervention, TDF constructs (knowledge, skills, professional role and identity, optimism, reinforcement, goals, environmental context and resources, social influences) targeted by the intervention were assessed via an online survey completed by service cooks for both intervention and control groups. The survey included sixty-one-items covering the fourteen TDF domains and was previously validated with long day care service cooks in Australia( 29 ). Cooks were asked to rate their barriers and enablers to implementing the sector nutrition guideline on a 7-point Likert scale from ‘strongly disagree’ to ‘strongly agree’. The study measured only the post-intervention difference in the TDF domains as awareness of the sector nutrition guidelines at baseline was low.
Service-level child food group consumption
Child consumption was assessed in a sub-sample of twenty-eight randomly selected (intervention, n 15; control, n 13) services. The aggregate servings of each of the core food groups and ‘discretionary’ foods consumed by children, for two mid-meals and one main meal while in care, was assessed at the service level at baseline and follow-up. Plate waste data were collected by two trained research assistants during a full-day data collection site visit at each time point. On the day of data collection, the research assistants collected the services’ menu and the pre- and post-serving weights of two mid-meals (morning and afternoon tea) and one main meal (lunch). The process for collecting plate waste measures was based on procedures previously reported in the literature( 42 ) and is detailed in the published protocol paper( 15 ).
Contamination, co-intervention and context
Intervention contamination and receipt of other interventions that may have influenced menu planning and food preparation was assessed in both intervention and control groups at follow-up via pen-and-paper questionnaires completed by service cooks and service managers.
A systematic search to identify any changes in government policy, standards, sector accreditation requirements and nutrition guidelines that may impact on the healthy eating environment and the provision of healthy foods within the childcare setting, was conducted to aid the assessment of the external validity of the trial findings and to describe the context in which the trial was conducted. The search was based on procedures applied in previous implementation trials in this setting( 19 ) and involved reviewing local news archives, websites of national and New South Wales health and education departments, accreditation standards and national healthy eating guidelines, to identify the existence of or changes in government policy, standards, funded programmes or guidelines that may influence the healthy eating environments of childcare services. The search included the 12 months prior to and during the 6-month intervention.
Adverse effects
Information on adverse effects was assessed via items included in the cooks’ pen-and-paper questionnaire completed at baseline and follow-up. Measures included: (i) receipt of negative feedback about the service menu in the last month (received from educators, children and/or parents); and (ii) the estimated average percentage of each meal not consumed by the children and classified as waste (morning tea, lunch, afternoon tea).
Intervention delivery
Project records maintained by implementation support staff were used to monitor the delivery of the intervention strategies.
Sample size and power calculations
Compliance with nutrition guidelines
Based on results of a preliminary study undertaken by the research team, the recruitment of twenty-nine services in the intervention group and twenty-nine services in the control group will enable the detection of an absolute difference of 32 % between groups in the primary outcome at follow-up, allowing for a 13 % overall compliance rate in the control group, with 80 % power, with a two-sided α of 0·05. If the intervention were made available to all services within New South Wales, approximately 1118 childcare services (~30 %) in the state would be compliant with the state guidelines, impacting on the diet of thousands of children who attend these services.
Statistical analyses
The SAS statistical software package (version 9.3 or later) was utilised for all statistical analyses. Socio-economic characteristics were determined using service postcodes, which were classified as being in the top or bottom 50 % of New South Wales according to the Socio-Economic Indexes for Areas( 43 ). All statistical tests were two-tailed with an α value of 0·05 and all available data were used for the analysis. All trial outcomes were analysed under an intention-to-treat framework using all available data with services analysed based on the groups to which they were allocated, regardless of the treatment type or exposure received. Logistic regression models, adjusted for baseline values of the outcome, were used to determine effectiveness of the intervention in improving full compliance with nutrition guidelines and compliance with nutrition guidelines for individual AGHE food groups. Linear regression models, adjusted for baseline values of all outcomes, were used to determine effectiveness of the intervention on modifying the mean number of compliant food groups, the mean number of servings of each food group planned on the service menu and the mean number of servings consumed for each AGHE food group and ‘discretionary’ foods. Analyses using multiple imputations for missing data were also performed.
Similar to previous studies, average scores for each TDF construct were calculated by summing all scores for all items within the domain (‘strongly disagree’=1 to ‘strongly agree’=7) and dividing by the total number of responses within the domain. The t test was used to assess between-group differences on TDF constructs at follow-up.
Results
Of the 106 long day care services in the study region that were eligible, ninety (85 %) nominated supervisors were eligible, seventy-nine (88 %) consented for their service to participate in the study and fifty-four were randomised into the study (intervention, n 26; control, n 28). The remaining twenty-five services were allocated to receive an alternative intervention consisting of training only due to service team resource availability (Fig. 1). Of the fifty-four services in the study, nine services (intervention, n 1; control, n 8) withdrew consent prior to baseline data collection and without knowledge of group allocation. Only one service did not complete follow-up data collection. The baseline characteristics of the long day care services are described in Table 2. There was a significant difference in cooks’ qualifications between the intervention and control services (52 % had university or TAFE qualification in the intervention services v. 90 % in the control; P ≤ 0·05).
Fig. 1.
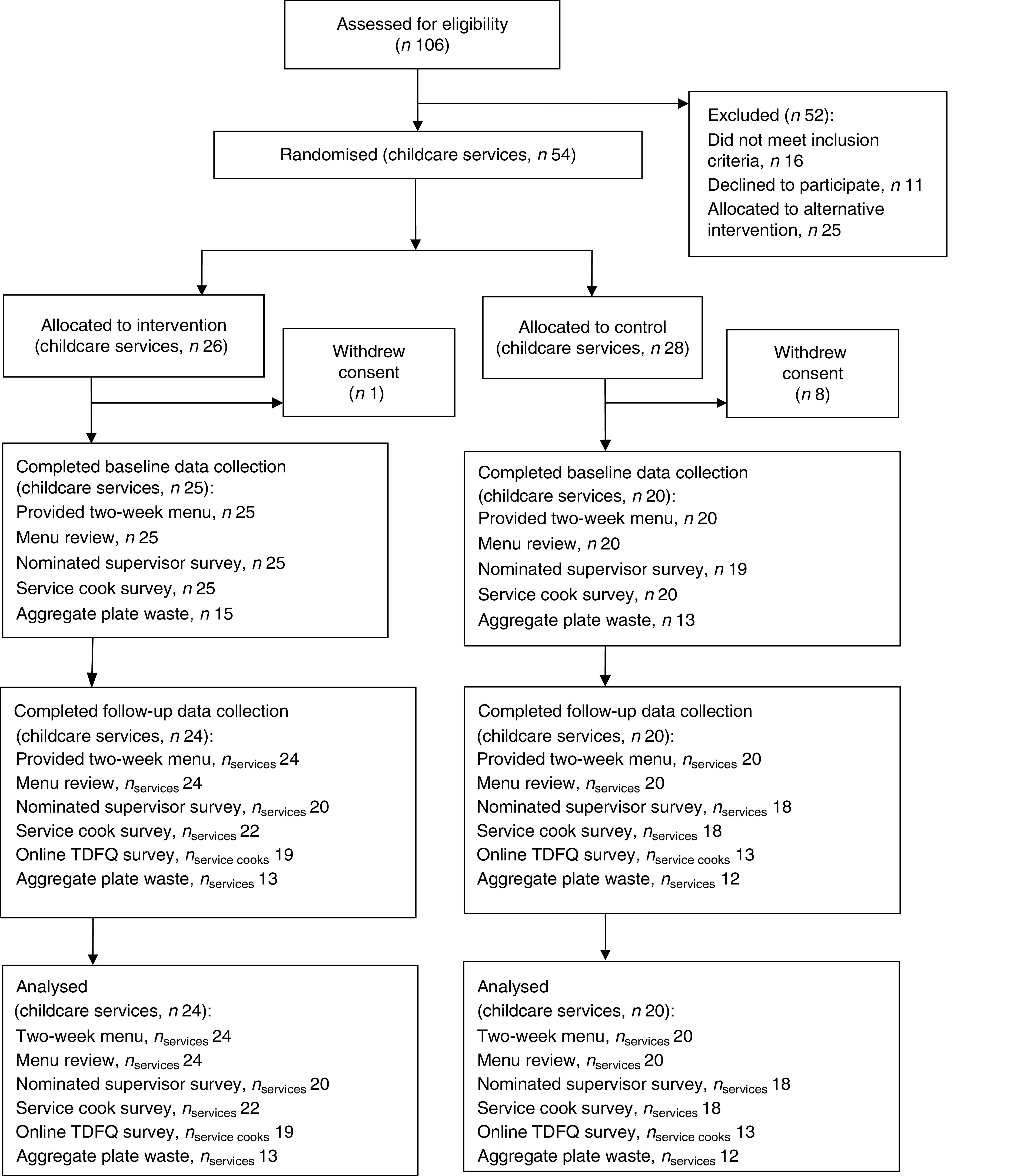
Retention of long day childcare services throughout the randomised controlled trial of a multi-strategy implementation intervention aimed to improve childcare compliance with nutrition guidelines (TDFQ, Theoretical Domains Framework questionnaire)
Table 2.
Baseline characteristics of long day childcare services and service cooks from Hunter New England region, New South Wales, Australia, participating in the randomised controlled trial of a multi-strategy implementation intervention aimed to improve childcare compliance with nutrition guidelines
| Intervention services (n 25) | Control services (n 20) | |||
|---|---|---|---|---|
| n | % | n | % | |
| Operational characteristics | ||||
| Total no. of children enrolled | 129 | 33·6 | 114 | 66·9 |
| No. of Aboriginal and Torres Strait Islander children enrolled | 5 | 6·5 | 8 | 17·5 |
| Daily budget allocated for food provision per child ($AU)*, mean and sd | 2·05 | 0·45 | 2·21 | 0·90 |
| Services in high socio-economic area | 14 | 56 | 8 | 40 |
| Services located (SEIFA) | ||||
| Major city+inner regional | 23 | 92 | 17 | 85 |
| Outer regional/remote Australia | 2 | 8 | 2 | 10 |
| Service cook demographic variable | ||||
| University or TAFE qualification | 13 | 52 | 18 | 90 |
| <40 years of age | 7† | 29 | 5‡ | 26 |
| >5 years as a cook in childcare services | 9† | 38 | 7‡ | 35 |
| Works ≤20 h/week | 2 | 8 | 5 | 25 |
| Nutrition environment | ||||
| Service has a nutrition policy | 25 | 100 | 19‡ | 100 |
| Menu is displayed in service for families to view | 25 | 100 | 19‡ | 100 |
| Menu-planning practices | ||||
| Service plans a menu every month or more frequently | 10 | 40 | 6† | 32 |
SEIFA, Socio-Economic Indexes for Areas.
Eleven intervention services and eleven control services completed the survey item.
Twenty-four intervention services completed the survey item.
Nineteen control services completed the survey item.
Primary trial outcomes
Full compliance with nutrition guidelines
At follow-up, one intervention service (4 %) and zero control services were fully compliant with the sector nutrition guidelines (all 5/5 food groups; see Table 3). Statistical analyses were not able to be performed given zero values across multiple cells.
Table 3.
Baseline and follow-up results for the outcomes: full compliance with nutrition guidelines, compliance with nutrition guidelines for individual AGHE food groups and mean number of servings of each food group planned on the service menu, among long day childcare services from Hunter New England region, New South Wales, Australia, participating in the randomised controlled trial of a multi-strategy implementation intervention aimed to improve childcare compliance with nutrition guidelines
| Intervention services | Control services | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline (n 25) | Follow-up (n 24) | Baseline (n 20) | Follow-up (n 20) | Analysis using all available data (controlled for baseline) | Analysis using multiple imputation (controlled for baseline) | |||||||||
| n | % | n | % | n | % | n | % | OR | 95 % CI | Exact P value | OR | 95 % CI | Exact P value | |
| Primary trial outcomes | ||||||||||||||
| Full compliance with nutrition guidelines | 0 | 0 | 1 | 4 | 0 | 0 | 0 | 0 | – | – | – | – | – | – |
| Compliance with nutrition guidelines for individual AGHE food groups | ||||||||||||||
| Vegetables | 0 | 0 | 3 | 12·5 | 0 | 0 | 0 | 0 | 3·43 | 0·50, – | 0·239 | 3·28 | 0·48, – | 0·242 |
| Fruit | 4 | 16 | 9 | 37·5 | 5 | 25 | 2 | 10 | 10·84 | 1·19, 551·20 | 0·024 | 9·21 | 0·95, 488·40 | 0·049 |
| Breads and cereals | 3 | 12 | 3 | 12·5 | 2 | 10 | 2 | 10 | 1·19 | 0·11, 16·30 | 1·000 | 1·15 | 0·11, 15·79 | 1·000 |
| Meat and alternatives | 1 | 4 | 7 | 29·2 | 0 | 0 | 0 | 0 | 8·83 | 1·55, – | 0·023 | 8·37 | 1·48, – | 0·025 |
| Dairy | 10 | 40 | 15 | 62·5 | 5 | 25 | 3 | 15 | 8·41 | 1·60, 63·62 | 0·006 | 6·26 | 1·26, 43·40 | 0·020 |
| Discretionary | 0 | 0 | 12 | 50·0 | 0 | 0 | 1 | 5 | 17·83 | 2·15, 853·73 | 0·002 | 16·54 | 2·00, 788·10 | 0·002 |
| Mean | sd | Mean | sd | Mean | sd | Mean | sd | Estimate | 95 % CI | P value | Estimate | 95 % CI | P value | |
| Secondary trial outcome | ||||||||||||||
| Mean no. of servings of each food group planned on the service menu | ||||||||||||||
| Vegetables | 1·18 | 0·50 | 2·16 | 0·55 | 1·05 | 0·57 | 1·10 | 0·49 | 1·01 | 0·70, 1·31 | <0·001 | 0·96 | 0·65, 1·27 | <0·001 |
| Fruit | 0·83 | 0·51 | 1·10 | 0·35 | 0·91 | 0·45 | 0·78 | 0·40 | 0·35 | 0·15, 0·55 | <0·001 | 0·34 | 0·14, 0·54 | 0·002 |
| Breads and cereals | 2·00 | 0·65 | 2·34 | 0·57 | 2·13 | 0·72 | 2·09 | 0·61 | 0·31 | 0·01, 0·63 | 0·044 | 0·31 | 0·01, 0·61 | 0·045 |
| Meat and alternatives | 0·55 | 0·23 | 0·77 | 0·15 | 0·50 | 0·18 | 0·58 | 0·20 | 0·16 | 0·08, 0·25 | <0·001 | 0·15 | 0·06, 0·24 | 0·002 |
| Dairy | 1·19 | 0·43 | 1·40 | 0·42 | 1·13 | 0·54 | 1·04 | 0·50 | 0·35 | 0·07, 0·63 | 0·016 | 0·33 | 0·06, 0·61 | 0·019 |
| Discretionary | 0·63 | 0·44 | 0·08 | 0·19 | 0·65 | 0·35 | 0·58 | 0·41 | −0·47 | −0·66, −0·29 | <0·001 | −0·42 | −0·62, −0·21 | <0·001 |
AGHE, Australian Guide to Healthy Eating.
Compliance with nutrition guidelines for individual AGHE food groups
Relative to control, significantly greater compliance among services allocated to the intervention group was reported for four of the six food groups: fruit (OR=10·84; 95 % CI 1·19, 551·20; P=0·0024); meat and meat alternatives (OR=8·83; 95 % CI 1·55, –; P=0·023); dairy (OR=8·41; 95 % CI 1·60, 63·62; P=0·006); and discretionary foods (OR=17·83; 95 % CI 2·15, 853·73; P=0·002; see Table 3).
Secondary trial outcomes
Menu compliance score (mean number of compliant food groups)
There was a significant difference between groups at follow-up in the mean number of food groups compliant (mean difference=1·57; 95 % CI 0·82, 2·33; P ≤ 0·001) favouring the intervention services.
Mean number of servings of each food group provided
There were significant differences (Table 3) between groups at follow-up in the mean number of servings of each food group planned on the menu for all six of the food groups.
Theoretical Domains Framework constructs
At follow-up there was no significant difference between the intervention and control groups in the TDF domain scores that were targeted by the intervention: knowledge (P=0·45); skills (P=0·21); social/professional role and identity (P=0·12); reinforcement (P=0·99); goals (P=0·37); environmental context and resources (P=0·77); and social influences (P=0·75).
Service-level child food group servings consumption
Significant improvements in consumption in the intervention services, relative to control, were found for two out of the six food groups: vegetables (adjusted difference=0·70; 95 % CI 0·33, 1·08; P<0·001); and fruit (adjusted difference=0·41; 95 % CI 0·09, 0·73; P=0·014; see Table 4).
Table 4.
Service-level child food group serving consumption at baseline and follow-up among long day childcare services from Hunter New England region, New South Wales, Australia, participating in the randomised controlled trial of a multi-strategy implementation intervention aimed to improve childcare compliance with nutrition guidelines
| Intervention services | Control services | Analysis using multiple | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline (n 15), servings | Follow-up (n 13), servings | Baseline (n 13), servings | Follow-up (n 12), servings | Analysis using all available data (controlled for baseline), difference in servings | imputation (controlled for baseline), difference in servings | |||||||||
| Mean | sd | Mean | sd | Mean | sd | Mean | sd | Estimate | 95 % CI | P value | Estimate | 95 % CI | P value | |
| Vegetables | 0·58 | 0·45 | 1·33 | 0·60 | 0·51 | 0·37 | 0·56 | 0·27 | 0·70 | 0·33, 1·08 | <0·001 | 0·56 | 0·19, 0·94 | 0·005 |
| Fruit | 0·39 | 0·36 | 0·87 | 0·44 | 0·42 | 0·29 | 0·46 | 0·30 | 0·41 | 0·09, 0·73 | 0·014 | 0·32 | 0·01, 0·63 | 0·042 |
| Breads and cereals | 1·19 | 0·78 | 1·85 | 0·74 | 1·45 | 0·48 | 1·66 | 1·44 | 0·26 | −0·67, 1·21 | 0·560 | 0·18 | −0·67, 1·04 | 0·661 |
| Meat | 0·47 | 0·38 | 0·66 | 0·27 | 0·38 | 0·37 | 0·53 | 0·31 | 0·13 | −0·12, 0·38 | 0·296 | 0·03 | −0·21, 0·27 | 0·816 |
| Dairy | 0·55 | 0·23 | 1·03 | 0·57 | 0·56 | 0·26 | 1·01 | 0·62 | −0·02 | −0·48, 0·43 | 0·902 | −0·05 | −0·46, 0·37 | 0·822 |
| Discretionary | 0·53 | 0·52 | 0·08 | 0·28 | 0·62 | 0·65 | 0·58 | 1·00 | −0·54 | −1·14, 0·05 | 0·073 | −0·42 | −0·98, 0·14 | 0·136 |
Contamination, co-intervention and context
At follow-up, no intervention and no control service cooks or service managers reported receiving any additional intervention or support beyond the prescribed intervention.
The systematic search undertaken did not identify any changes in childcare government policy, standards, sector accreditation requirements and nutrition guidelines related to healthy eating environment and the provision of healthy foods within the childcare setting. However, the trial was conducted concurrently with a state-wide childhood obesity prevention initiative where by services were eligible to receive training or support regarding healthy eating and physical activity, which may have included support or training to improve food provision( 44 ). Internal service records identified ten services (intervention, n 5; control, n 5) that had completed the state-wide training between the specified period (12 months prior to intervention delivery and during the 6-month intervention). For all except one service (intervention), the training was completed by service educators.
Adverse events
At follow-up there was no significant difference, after adjusting for baseline values, observed between groups for service cooks reporting negative feedback received about the service menu in the past month from educators (intervention 32 % (n 7/22) v. control 25 % (n 4/16); P=0·62), children (intervention 32 % (n 7/22) v. control 6 % (n 1/16); P=0·07) or parents (intervention 9 % (n 2/22) v. control 0 % (n 0/16); P=0·95).
At follow-up there was also no significant difference, after adjusting for baseline values, observed between groups for the estimated average percentage of food classified as waste for each meal: morning tea (adjusted difference=−0·41; 95 % CI −2·35, 1·52 %; P=0·66); lunch (adjusted difference=3·31; 95 % CI −2·64, 9·27 %; P=0·26); and afternoon tea (adjusted difference=−1·24; 95 % −3·77, 1·28 %; P=0·31).
Delivery of intervention strategies
All services were offered and accepted six months of implementation support via telephone contact from an implementation support staff member. Over 90 % of intervention services signed the memorandum of understanding, received all of the intervention resources and newsletters, participated in two service visits, completed the mid-point menu review and were provided with a feedback report. Eighty-eight per cent of nominated supervisors and 92 % of service cooks attended the one-day menu-planning workshop.
Discussion
The present study is one of the few randomised controlled trials measuring the effectiveness of a multicomponent implementation intervention on childcare service compliance with nutrition guidelines. The study found that the intervention improved compliance with individual core food groups (fruit; meat and meat alternatives; dairy; and discretionary foods) and that child intake of some core foods (vegetables and fruit) increased as a consequence. In addition, the intervention had no adverse effects on food wastage or the service receiving negative feedback about the menu. Such findings provide one approach for policy makers and service delivery organisations to enhance childcare service guideline compliance and children’s intake of healthy foods while in care.
The intervention did not improve full compliance with nutrition guidelines, however. This finding suggests that achieving a fully compliant two-week menu represents a considerable challenge for centre-based childcare services – even with comprehensive implementation support. The findings also support those of reviews of implementation practice guidelines which suggest that perfect compliance with guideline recommendations is rarely achieved( 45 ). In retrospect, the primary trial outcome selected for the trial may have been unrealistic, given the complexity of menu-planning processes and of the operating environments of childcare services. While the Caring for Children resource represents an attempt to develop guidelines that are acceptable and suitable for the childcare setting, the complexity with planning meals and beverages so that they meet the recommended servings for all core food groups is likely to represent a significant challenge for cooks who do not typically have any formal training in nutrition. Future updates to the guidelines should consider that full compliance is unlikely to be achievable in this context, Generally, this is a key finding for the formation and measurement of nutrition guideline compliance in the setting.
Nevertheless, improvements in food provision were achieved. The magnitudes of improvements in implementation of menus compliant with four of six individual food groups (fruit, meat and alternatives, dairy, discretionary) achieved by intervention services (21·5 % for fruit; 25·2 % for meat and alternatives; 22·5 % for dairy; 50·0 % for discretionary) were somewhat similar to yet slightly lower than those reported among trials using similar implementation strategies in childcare services to improve menus (40–68 %)( 13 , 14 , 46 , 47 ). The effect sizes were also similar to those reported in trials of implementation strategies in schools to improve the availability of healthy foods (25–42 %)( 46 , 48 ). The findings of the present study, therefore, reinforce the capacity to improve food provision in line with menu dietary guidelines in education settings as a potentially effective public health nutrition strategy.
Despite significant improvements among intervention services in the mean servings planned on the menu for all six food groups, changes in service-level child consumption improved significantly for vegetables (0·70 servings) and fruit (0·41 servings) only. The findings indicate that improvements in food availability do not uniformly translate into improvements in intake. Statistical significance aside, smaller improvements in consumption of foods relative to improvements reported in menu availability were also reported across other food groups. Additional strategies beyond targeting foods provided, such as the use of positive statements during meal times and educators’ role modelling healthy eating behaviours, and addressing other known determinants of child intake may be required to improve the effectiveness of the intervention on child diet.
Interestingly, the implementation strategy did not change the TDF constructs that it targeted. The findings may suggest that the intervention exerts its effects in improving menu planning and food provision through other pathways. Future research to identify such pathways is warranted. Alternatively, the findings may reflect challenges in measurement of implementation constructs. While validated, and used in previous randomised trials, TDF scores for a number of constructs were high and skewed. Such ceiling effects may hinder the capacity of the measure to detect meaningful changes in hypothesised implementation mediators. Work to improve the TDF questionnaire tool in the childcare setting and the measurement of implementation constructs more broadly would be valuable for future research in the field.
Strengths of the study include the randomised controlled trial design, the application of theory for intervention design and the blinding of outcome assessors. However, the study findings should be considered in the context of its limitations. Previous studies have identified that time is a key determinant of implementation( 49 , 50 ). The short intervention period of 6 months may have not have provided sufficient time for the intervention services to reach full compliance, particularly considering the complexity of the menu-planning process. Second, with such a short intervention period, we do not know if the changes will be sustained long term. Future research is warranted to assess the sustainability of such interventions. Finally, the research was conducted in a region in which childcare services have been exposed to obesity prevention intervention and implementation support for more than a decade( 19 , 40 , 46 , 51 ). The effects of the implementation strategies on services operating under different contexts are unknown.
Conclusion
The present study is one of the few randomised controlled trials measuring the effectiveness of a multicomponent support intervention on the implementation of menu dietary guidelines in the childcare setting. The findings indicate that service-level changes to menus in line with dietary guidelines can result in improvements to children’s dietary intake. Despite the lack of effect on TDF constructs/outcomes, the chosen implementation strategies were effective in supporting practice change, despite a short intervention period. As such they should be considered for future programmes/interventions targeting dietary guideline implementation in the setting.
Acknowledgements
Acknowledgements: The authors wish to thank members of the ‘Good for Kids Good for Life’ Early Childhood Education and Care advisory group. Financial support: This project was funded by the Priority Research Centre for Health Behaviour and received infrastructure funding from Hunter New England Population Health and the University of Newcastle. L.W. is supported by a National Health and Medical Research Council Career Development Fellowship and a Heart Foundation Future Leaders Fellowship. Conflict of interest: The authors declare that they have no conflict of interests. Authorship: K.S. led the development of this manuscript. K.S., S.Y., L.W. and M.F. conceived the intervention concept. K.S., S.Y., L.W., M.F., J.W. and J.J. contributed to the research design and trial methodology. All authors contributed to and approved the final version of this manuscript. Ethics of human subject participation: Ethical approval to conduct the study was obtained from the Hunter New England Human Research Ethics Committee (reference 12/08/15/5.01) and the University of Newcastle Human Research Ethics Committee (reference H-2012-0321).
References
- 1. Institute for Health Metrics and Evaluation (2014) Global Burden of Disease Data. http://www.healthdata.org/gbd/data (accessed June 2017).
- 2. Shrestha R & Copenhaver M (2015) Long-term effects of childhood risk factors on cardiovascular health during adulthood. Clin Med Rev Vasc Health 7, 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Waxman A (2003) Prevention of chronic diseases: WHO Global Strategy on Diet, Physical Activity and Health. Food Nutr Bull 24, 281–284. [DOI] [PubMed] [Google Scholar]
- 4. Mikkelsen MV, Husby S, Skov LR et al. (2014) A systematic review of types of healthy eating interventions in preschools. Nutr J 13, 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Australian Children’s Education and Care Quality Assurance (2017) National Quality Standard. Quality Area 2 – Children’s health and safety 2017. http://www.acecqa.gov.au/Childrens-health-and-safety (accessed November 2017).
- 6. Australian Bureau of Statistics (2017) Australian Health Survey: First Results, 2011–12. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4364.0.55.001main+features12011-12 (accessed June 2017).
- 7. Radcliffe BC, Cameron CV & Baade PD (2002) Nutrient intakes of young children: implications for long-day child-care nutrition recommendations. Nutr Diet 59, 187–190. [Google Scholar]
- 8. Australian Bureau of Statistics (2016) Childhood Education and Care, Australia, June 2014. http://www.abs.gov.au/ausstats/abs@.nsf/mf/4402.0 (accessed June 2017).
- 9. Government of Australia (2013) Australian Dietary Guidelines. Canberra, ACT: National Health and Medical Research Council. [Google Scholar]
- 10. Benjamin Neelon SE & Briley ME; American Dietetic Association (2011) Position of the American Dietetic Association: benchmarks for nutrition in child care. J Am Diet Assoc 111, 607–615. [DOI] [PubMed] [Google Scholar]
- 11. Local Authorities Coordinators of Regulatory Services (2010) Nursery School Nutrition Survey Results. https://www.nottinghamcity.gov.uk/media/361919/healthy_eating-_regional_guidance.pdf (accessed November 2017).
- 12. Yoong SL, Skelton E, Jones J et al. (2014) Do childcare services provide foods in line with the 2013 Australian Dietary Guidelines? A cross-sectional study. Aust N Z J Public Health 38, 595–566. [DOI] [PubMed] [Google Scholar]
- 13. Gosliner WA, Paula J, Yancey AK et al. (2010) Impact of a worksite wellness program on the nutrition and physical activity environment of child care centers. Am J Health Promot 24, 186–189. [DOI] [PubMed] [Google Scholar]
- 14. Johnston Molloy C, Kearney J, Hayes N et al. (2014) Healthy incentive scheme in the Irish full-day-care pre-school setting. Proc Nutr Soc 73, 147–158. [DOI] [PubMed] [Google Scholar]
- 15. Seward K, Wolfenden L, Finch M et al. (2016) Multistrategy childcare-based intervention to improve compliance with nutrition guidelines versus usual care in long day care services: a study protocol for a randomised controlled trial. BMJ Open 6, e010786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wolfenden L, Yoong SL, Williams CM et al. (2017) Embedding researchers in health service organizations improves research translation and health service performance: the Australian Hunter New England Population Health example. J Clin Epidemiol 85, 3–11. [DOI] [PubMed] [Google Scholar]
- 17. NSW Ministry of Health (2014) Caring for Children: Birth to 5 years (Food, Nutrition and Learning Experiences). North Sydney, NSW: NSW Ministry of Health. [Google Scholar]
- 18. Cane J, O’Connor D & Michie S (2012) Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 7, 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jones J, Wyse R, Finch M et al. (2015) Effectiveness of an intervention to facilitate the implementation of healthy eating and physical activity policies and practices in childcare services: a randomised controlled trial. Implement Sci 10, 147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wolfenden L, Jones J, Williams C et al. (2016) Strategies to improve the implementation of healthy eating, physical activity and obesity prevention policies, practices or programmes within childcare services. Cochrane Database Syst Rev 10, CD011779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. French SD, Green SE, O’Connor DA et al. (2012) Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implement Sci 7, 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Michie SJ, Francis M, Hardeman J et al. (2008) From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Appl Psychol 57, 660–680. [Google Scholar]
- 23. Huijg JM, Gebhardt WA, Dusseldorp E et al. (2014) Measuring determinants of implementation behavior: psychometric properties of a questionnaire based on the theoretical domains framework. Implement Sci 9, 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hujg JM, Gebhardt WA, Crone MR et al. (2014) Discriminant content validity of a theoretical domains framework questionnaire for use in implementation research. Implement Sci 9, 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Phillips CJ, Marshall AP, Chaves NJ et al. (2015) Experiences of using the Theoretical Domains Framework across diverse clinical environments: a qualitative study. J Multidiscip Healthc 8, 139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sarmast H, Mosavianpour M, Collet J-P et al. (2014) TDF (Theoretical Domain Framework): how inclusive are TDF domains and constructs compared to other tools for assessing barriers to change? BMC Health Serv Res 14, Suppl. 2, P81. [Google Scholar]
- 27. Dyson J, Lawton R, Jackson C et al. (2013) Development of a theory-based instrument to identify barriers and levers to best hand hygiene practice among healthcare practitioners. Implement Sci 8, 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tavender EJ, Bosch M, Gruen RL et al. (2014) Understanding practice: the factors that influence management of mild traumatic brain injury in the emergency department – a qualitative study using the Theoretical Domains Framework. Implement Sci 9, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Seward K, Wolfenden L, Wiggers J et al. (2017) Measuring implementation behaviour of menu guidelines in the childcare setting: confirmatory factor analysis of a theoretical domains framework questionnaire (TDFQ). Int J Behav Nutr Phys Act 14, 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. French SD, McKenzie JE, O’Connor DA et al. (2013) Evaluation of a theory-informed implementation intervention for the management of acute low back pain in general medical practice: the IMPLEMENT cluster randomised trial. PLoS One 8, e65471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jones RA, Riethmuller A, Hesketh K et al. (2011) Promoting fundamental movement skill development and physical activity in early childhood settings: a cluster randomized controlled trial. Pediatr Exerc Sci 23, 600–615. [DOI] [PubMed] [Google Scholar]
- 32. Forsetlund L, Bjørndal A, Rashidian A et al. (2009) Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev issue 2, CD003030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Joyce B & Showers B (1980) Improving inservice training: the message of research. Educ Leadersh 37, 379. [Google Scholar]
- 34. Bero LA, Grilli R, Grimshaw JM et al. (1998) Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. BMJ 317, 465–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Read CW & Kleiner BH (1996) Which training methods are effective? Manage Dev Rev 9, 24–29. [Google Scholar]
- 36. Ivers N, Jamtvedt G, Flottorp S et al. (2012) Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev issue 6, CD000259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Abraham C & Michie S (2008) A taxonomy of behavior change techniques used in interventions. Health Psychol 27, 379–389. [DOI] [PubMed] [Google Scholar]
- 38. Soumerai SB & Avorn J (1990) Principles of educational outreach (‘academic detailing’) to improve clinical decision making. JAMA 263, 549–556. [PubMed] [Google Scholar]
- 39. Dodds P, Wyse R, Jones J et al. (2014) Validity of a measure to assess healthy eating and physical activity policies and practices in Australian childcare services. BMC Public Health 14, 572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Finch M, Wolfenden L, Falkiner M et al. (2012) Impact of a population based intervention to increase the adoption of multiple physical activity practices in centre based childcare services: a quasi experimental, effectiveness study. Int J Behav Nutr Phys Act 9, 101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ginani VC, Zandonadi RP, Araujo WMC et al. (2012) Methods, instruments, and parameters for analyzing the menu nutritionally and sensorially: a systematic review. J Culinary Sci Technol 10, 294–310. [Google Scholar]
- 42. Jacko CC, Dellava J, Ensle K et al. (2007) Use of the plate-waste method to measure food intake in children. J Extension 45, issue 6, 6RIB7. [Google Scholar]
- 43. Australian Bureau of Statistics (2011) Socio-Economic Indexes for Areas 2011. http://www.abs.gov.au/websitedbs/censushome.nsf/home/seifa (accessed November 2017).
- 44. NSW Department of Health (2017) About Munch & Move. http://www.healthykids.nsw.gov.au/campaigns-programs/about-munch-move.aspx (accessed May 2017).
- 45. Durlak JA & DuPre EP (2008) Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Community Psychol 41, 327–350. [DOI] [PubMed] [Google Scholar]
- 46. Bell CA, Davies L, Finch M et al. (2015) An implementation intervention to encourage healthy eating in centre-based childcare services: impact of the Good for Kids Good for Life programme. Public Health Nutr 18, 1610–1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Williams CL, Bollella MC, Strobino BA et al. (2002) ‘Healthy-Start’: outcome of an intervention to promote a heart healthy diet in preschool children. J Am Coll Nutr 21, 62–71. [DOI] [PubMed] [Google Scholar]
- 48. Nathan N, Wolfenden L & Bell AC (2012) Effectiveness of a multi-strategy intervention in increasing the implementation of vegetable and fruit breaks by Australian primary schools: a non-randomised controlled trial. BMC Public Health 12, 651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Gabor V, Mantinan K, Rudolph K et al. (2010) Challenges and Opportunities Related to Implementation of Child Care Nutrition and Physical Activity Policies in Delaware. Washington, DC: Altarum Institute. [Google Scholar]
- 50. Hughes CC, Gooze RA, Finkelstein DM et al. (2010) Barriers to obesity prevention in Head Start. Health Aff (Millwood) 29, 454–462. [DOI] [PubMed] [Google Scholar]
- 51. Bell LK, Hendrie GA, Hartley J et al. (2015) Impact of a nutrition award scheme on the food and nutrient intakes of 2- to 4-year-olds attending long day care. Public Health Nutr 18, 2634–2642. [DOI] [PMC free article] [PubMed] [Google Scholar]


