Abstract
Objective
To examine associations between grandmothers’ knowledge and infant and young child feeding (IYCF) practices and to test whether the associations are independent of or operate via maternal knowledge.
Design
Cross-sectional household survey data from households with a child under 5 years (n 4080). We used multivariate regression analyses, adjusted for child, maternal, grandmother and household characteristics, and district-level clustering, to test associations between grandmothers’ knowledge and IYCF practices for children aged 6–24 months living with a grandmother. We used causal mediation to formally test the direct effect of grandmothers’ knowledge on IYCF practices v. maternal knowledge mediating these associations.
Setting
Two hundred and forty rural communities, sixteen districts of Nepal.
Subjects
Children aged 6–24 months (n1399), including those living with grandmothers (n 748).
Results
We found that the odds of optimal breast-feeding practices were higher (early breast-feeding initiation: 2·2 times, P=0·002; colostrum feeding: 4·2 times, P<0·001) in households where grandmothers had correct knowledge v. those with incorrect knowledge. The same pattern was found for correct timing of introduction of water (2·6), milk (2·4), semi-solids (3·2), solids (2·9), eggs (2·6) and meat (2·5 times; all P<0·001). For the two pathways we were able to test, mothers’ correct knowledge mediated these associations between grandmothers’ knowledge and IYCF practices: colostrum feeding (b=10·91, P<0·001) and the introduction of complementary foods (b=5·18, P<0·001).
Conclusions
Grandmothers’ correct knowledge translated into mothers’ correct knowledge and, therefore, optimal IYCF practices. Given grandmothers’ influence in childcare, engagement of grandmothers in health and nutrition interventions could improve mothers’ knowledge and facilitate better child feeding.
Key words: Nepal, Child nutrition, Grandmothers, Infant and young child feeding
Nepal has experienced some of the fastest rates of reduction in child undernutrition globally: between 1996 and 2011, the prevalence of stunting (height-for-age Z-score <–2) among children under 2 years of age fell from 48 to 27 %. Improvements in health-service access and utilization, sanitation and education, coupled with reductions in poverty, drove this stunting reduction over time in Nepal( 1 – 3 ). However, child undernutrition remains a significant public health burden, with more than one in four Nepali children under 2 years of age being stunted( 1 , 2 ).
Infant and young child feeding (IYCF) practices, which did not improve between 1996 and 2011, might be a key contributor to persistent child undernutrition in Nepal( 1 – 5 ). IYCF practices are important for child survival, child growth and development( 6 , 7 ). The WHO-recommended IYCF practices cover both breast-feeding and complementary feeding of children under 2 years of age( 4 ). According to the 2011 Demographic and Health Survey, about 80 % of mothers reported to have exclusively breast-fed their children under 6 months of age. Complementary feeding practices continue to be suboptimal: not even one in three children aged 6–24 months consume foods from at least four of seven food groups, the standard for minimum dietary diversity. Also, contrary to the WHO recommendation of introducing children to complementary foods at 6 months of age, nearly one in four children 4–5 months of age are fed solid or semi-solid foods and at least 40 % of children 6–8 months of age still do not consume solid or semi-solid foods( 8 ). This highlights that complementary foods are sometimes introduced too late and other times, too early.
Maternal and household demographic and socio-economic factors likely drive poor IYCF practices. Prior studies in Nepal have found maternal employment, education, age and media exposure as determinants of IYCF practices( 3 , 6 , 7 ). Cultural beliefs, knowledge and perceptions have all been shown to influence complementary feeding, including which types of foods to introduce first, the timing of their introduction and who should feed young children( 9 ). Behaviour change interventions often target mothers with the aim of improving their IYCF-related beliefs, attitudes and knowledge and, ultimately, their IYCF practices. However, in much of South Asia, including Nepal, grandmothers are also childcare providers who influence maternal decisions regarding child feeding. Judi Aubel highlights the central role grandmothers play in child feeding in Bangladesh, Pakistan and Nepal: grandmothers advise mothers on caregiving, including child feeding, and they are often direct caregivers for young children( 10 , 11 ).
In South Asia, grandmothers are considered storehouses of knowledge and wisdom on a wide array of household topics. Given their revered status, grandmothers often serve as advisors and supervisors to the next generation, playing an influential role in child health and nutrition( 10 ). In a qualitative study about the role of Tamang mothers-in-law in Mwakanpur, Nepal, Masvie found that most mothers were assisted by their mothers-in-law for young child feeding( 12 ). Another qualitative study in Nepal reported that mothers were obliged to obey their mothers-in-law and follow local practices even when the mother wanted to follow a doctor’s recommendations: although mothers were responsible for food preparation, grandmothers had primary decision-making power over which foods the child would receive and when( 13 ). Furthermore, in Nepal, about four out of five women residing in rural areas are engaged in agricultural labour; many mothers depend on grandmothers to provide care for their young children while they work in the fields( 14 ). Locks et al. found that 55 % of mothers and 39 % of grandmothers are primary caregivers of children in Baitadi, Nepal( 14 ). In rural Nepal, grandmothers provide childcare in part because of the heavy workloads of mothers and the authoritative cultural space that grandmothers occupy in Nepali households, but also because of the drastic increase in labour emigration of both men and women. The number of labour permits issued to men increased from 211371 in 2008 to 492724 in 2014, a 133 % increase, but the number of labour permits issued to women grew even more drastically from 8594 in 2008 to 29154 in 2014, a steep incline of 239 %( 15 ). If this trend continues, grandmothers may play an increasingly significant role in child health and nutrition.
Studies on the role of grandmothers in IYCF practices in South Asia are limited; those conducted to date are primarily qualitative and the quantitative studies were based on small sample sizes. There are no prior quantitative studies on this topic in Nepal. In the present study, we investigate the associations between grandmothers’ correct knowledge and correct practices for the following IYCF indicators: breast-feeding initiation, colostrum feeding and timing of introduction of six types of complementary foods (water, milk (and milk products other than breast milk), semi-solid foods, solid foods, meat and eggs) for children 6–24 months of age residing in rural Nepal. We also investigate whether any found association is direct or whether maternal knowledge mediates the association.
Methods
Survey design and sampling
We use data collected for a baseline survey of a quasi-experimental impact evaluation of Suaahara, an integrated nutrition programme to improve maternal and child nutrition in rural Nepal. Data were collected from mid-June to early October (rainy season) of 2012 across Nepal’s three agro-ecological zones: mountains, hills and terai( 8 ). Households were selected through a multistage cluster design. First, sixteen districts were purposively selected to include eight intervention districts and eight comparison districts, matched based on various agro-ecological and sociodemographic characteristics. Second, five village development committees per district were selected and third, three wards per village development committee were selected; both village development committees and wards were selected using probability-proportional-to-size techniques. Lastly, within each ward, seventeen households with a child under 5 years of age were randomly selected from a census carried out by study enumerators. The total sample included 4080 households across 240 wards, including 1399 children between the ages of 6 and 24 months.
Ethics approval
Ethics approval was obtained from the Nepal Health Research Council (NHRC), Nepal’s ethical review board, and the internal review board of the International Food Policy Research Institute (IFPRI) in 2012. For the additional analysis in the present publication, ethics approval was also obtained from the London School of Hygiene and Tropical Medicine (LSHTM) in 2015.
Data collection
The baseline household survey involved interviewing three household members: (i) the mother of a randomly selected child under 5 years of age (the index child); (ii) a major adult economic decision maker (the mother’s husband or adult male, when available); and (iii) the child’s grandmother, if she resided in the same household. These household surveys included asking the primary female and male respondents a diverse set of questions regarding household sociodemographic characteristics and knowledge and practices relating to maternal and child health and nutrition; water, sanitation and hygiene; agriculture; family planning; and empowerment. The grandmothers’ questionnaire included questions regarding their knowledge and beliefs on key maternal and child health and nutrition topics, including IYCF.
Data analysis
All statistical analyses were performed using the statistical software package STATA version 13.0 (2013). For the present IYCF-focused study, we restricted our analysis to households with at least one child 6–24 months of age (n 1399) and for our regression analysis, we focused on index children in this age range residing with a grandmother (n 748).
The primary outcome variables were IYCF practices, as reported by mothers: whether or not the child was fed colostrum (yes/no); whether or not there was early initiation of breast-feeding, defined as the child receiving breast milk within the first hour of birth (yes/no); and whether or not the child was introduced to water, milk (and milk products other than breast milk), semi-solid foods, solid foods, eggs and meat at the appropriate age, defined as mothers who reported introducing each of the six types of complementary foods between 6 and 9 months of age (yes/no). These specific IYCF variables were selected based on both the research question and data availability from the grandmothers’ survey for construction of the parallel primary explanatory variables.
The primary explanatory variables were grandmothers’ knowledge and beliefs on these three IYCF practices. Grandmothers were asked whether or not a child should be given colostrum; when breast-feeding should start; and when (in months) they believed each of the six types of complementary foods should be introduced. Binary variables were created for both breast-feeding variables to denote correct knowledge: (i) child should be fed colostrum (yes/no); and (ii) child should receive breast milk within the first hour of birth (yes/no). Binary variables were also created for correct knowledge on the timing for introduction of complementary foods, defined as grandmothers who reported that each of the six types of complementary foods should be introduced between 6 and 9 months (yes/no).
We used ANOVA and χ 2 tests to explore characteristics of households with (n 748) and without (n 651) a grandmother in residence. Next, multivariate logistic regression models were used to test the associations between grandmothers’ IYCF knowledge and parallel IYCF practices. Lastly, we empirically tested the direct v. indirect effects for grandmothers’ correct knowledge and the actual practices, via mothers’ correct knowledge as the hypothesized mediator, for colostrum feeding and timely introduction of complementary foods. We were unable to test pathways for early initiation of breast-feeding, as the data set did not include a maternal knowledge variable for this. Given the binary nature of our child feeding outcome variables, we used generalized structural equation modelling for our mediation analysis.
In all adjusted models, we controlled for various potential confounding factors at the child, mother, grandmother and household levels, based on our knowledge of the local setting and prior studies regarding IYCF in Nepal( 13 , 14 , 16 – 19 ). Child variables included age in months, sex (male or female) and decision maker regarding child feeding (mother, grandmother or other). Maternal characteristics included age in years, level of education (years of formal schooling completed), whether participated in wage or salary employment in the year prior to the survey (yes or no), number of sources from which nutrition information was ever heard (newspaper/magazine, radio, television, brochure/banner/poster, billboard, flipchart, counseling card, announcements in loudspeakers, community/village gatherings, religious gathering/meetings, mother’s group, street drama, health facility, female community health volunteers) and residency with her own mother (yes or no). Grandmother characteristics included age in years and level of education (years of education completed). Household characteristics included the number of children <5 years of age residing in the household, the agro-ecological zone of residency (mountains, hills or terai), caste/ethnicity (Dalit, disadvantaged Janajatis, disadvantaged non-Dalit Terai, religious minorities, relatively advantaged Janajatis, Brahmin/Chhetri/Sanyasi), level of food security (food secure, mildly food insecure, moderately food insecure or severely food insecure) measured by the Household Food Insecurity Access Scale (HFIAS)( 20 ) and wealth quintile (poorest, second poorest, middle income, second wealthiest or wealthiest), calculated using principal component analysis. We also controlled for potential clustering at the district level and included a variable identifying whether the district was an intervention or comparison area, given the purposive selection of intervention areas by degree of need and how this may influence the results.
Results
Table 1 presents key descriptive statistics for the child, mother, grandmother and household; these statistics are presented for both types of household: those with (n 748) and without a grandmother (n 651) in residence. Among those living with a grandmother in the household, half of the children were male and the mean age was 14 months. Mothers were on average 24 years old, with age ranging from 15 to 42 years. Mean maternal education was 6 years of formal schooling. Among surveyed mothers, only 5 % resided with their own mothers and only 13 % claimed to participate in wage or salary employment in the past year. On average, women received nutrition information from only one source of a possible ten sources. Mean age of the grandmothers was 55 years, but their age ranged from 35 to 85 years. On average, these grandmothers had less than half a year of formal schooling. About half of the households resided in hill districts, with residency for the other half split fairly evenly between mountains and terai districts. About half of the households were from most advantaged ethnic group while 17 % were Dalit, the most disadvantaged caste group in Nepal. The average number of children <5 years of age per household was one. More than eight out of ten surveyed households were food secure.
Table 1.
Characteristics of the sample of households from 240 rural communities in sixteen districts of Nepal, 2012
| Households with grandmothers (n 748) | Households without grandmothers (n 651) | ||||
|---|---|---|---|---|---|
| % or Mean | sd | % or Mean | sd | P value† | |
| Child | |||||
| Sex: male (0/1) | 49·3 | – | 51·0 | – | 0·53 |
| Age (months; range 6–24) | 14·2 | 5·2 | 14·6 | 5·1 | 0·15 |
| Age group | |||||
| 6–8·9 months | 17·7 | – | 14·0 | – | |
| 9–11·9 months | 18·7 | – | 17·8 | – | |
| 12–14·9 months | 18·3 | – | 18·7 | – | |
| 15–17·9 months | 14·8 | – | 17·1 | – | |
| 18–20·9 months | 13·8 | – | 15·8 | – | |
| 21–23·9 months | 16·7 | – | 16·6 | – | 0·39 |
| Decision maker: child feeding | |||||
| Mother | 72·1 | – | 92·2 | – | |
| Grandmother | 10·3 | – | 0·3 | – | |
| Other | 17·6 | – | 7·5 | – | <0·001 |
| Mother | |||||
| Age (years; range 15–42) | 23·6 | 4·5 | 26·8 | 6·1 | <0·001 |
| Education (years of formal schooling completed; range 0–14) | 5·9 | 4·1 | 4·0 | 4·1 | <0·001 |
| Participation in wage/salary employment in past 12 months, yes (0/1) | 13·2 | – | 18·0 | – | 0·01 |
| Number of sources from which nutrition information ever heard (range 0–10) | 0·9 | 1·4 | 0·8 | 1·4 | 0·12 |
| Currently residing in own mother’s home, yes (0/1) | 4·7 | – | 1·8 | – | 0·003 |
| Grandmother | |||||
| Age (years; range 35–85) | 55·1 | 9·3 | NA | – | NA |
| Education (years of formal schooling; range 0–12)‡ | 0·3 | 1·2 | NA | – | NA |
| Household | |||||
| Number of children <5 years of age | 1·4 | 0·6 | 1·4 | 0·52 | 0·72 |
| Agro-ecological zone of residency | |||||
| Mountain | 23·5 | – | 27·0 | – | |
| Hill | 52·7 | – | 51·8 | – | |
| Terai | 23·8 | – | 21·2 | – | 0·25 |
| Caste/ethnicity | |||||
| Dalit | 17·4 | – | 21·8 | – | |
| Disadvantaged Janajatis | 21·9 | – | 24·0 | – | |
| Disadvantaged non-Dalit Terai | 5·2 | – | 3·2 | – | |
| Religious minorities (Muslim/Churoute) | 0·8 | – | 1·5 | – | |
| Relatively advantaged Janajatis | 5·2 | – | 4·8 | – | |
| Most advantaged (Brahmin/Chettri/Thakuri/Sanyasi) | 49·5 | – | 44·7 | – | 0·06 |
| Food security§ | |||||
| Severely food insecure | 0·9 | – | 3·2 | – | |
| Moderately food insecure | 5·8 | – | 13·1 | – | |
| Mildly food insecure | 11·2 | – | 19·1 | – | |
| Food secure | 82·1 | – | 64·7 | – | <0·001 |
| Wealth quintile | |||||
| Poorest | 20·1 | – | 20·0 | – | |
| Second poorest | 20·1 | – | 20·0 | – | |
| Middle income | 19·9 | – | 20·0 | – | |
| Second wealthiest | 20·1 | – | 20·0 | – | |
| Wealthiest | 19·9 | – | 20·0 | – | <0·001 |
NA, not available.
P values calculated using ANOVA for variables with mean values reported and χ 2 test for variables with prevalence.
Data missing for one or two individuals (n 747, n 746).
Measured with the Household Food Insecurity Access Scale (HFIAS)( 20 ).
Table 1 also presents some statistically significant differences we found between characteristics of households with and without grandmothers. Households with grandmothers tend to have mothers that are younger (P<0·001) and more highly educated (P<0·001); however, these mothers are less likely to have participated in wage/salary employment in the past 12 months (P=0·01). Compared with those households without a grandmother present, a higher proportion of households with grandmothers are from the Brahmin/Chettri/Thakuri/Sanyasi caste and ethnicity group and more have achieved food security, as measured by the HFIAS (P<0·001).
Table 2 summarizes both grandmothers’ and mothers’ IYCF knowledge and household IYCF practices included in the analysis. Most grandmothers had correct breast-feeding knowledge: breast-feeding should be initiated within an hour of birth (71 %) and colostrum should be given to the baby (83 %). While slightly less than half of the grandmothers had correct knowledge that water and meat products should be introduced at 6–9 months of age, a majority of the grandmothers had correct knowledge on when semi-solid foods and solid foods should be introduced (71 and 75 %, respectively). Half of the grandmothers had correct knowledge regarding timing of introduction of milk and eggs. Only 17 % of the grandmothers reported correctly (6–9 months of age) for when all six of these complementary foods should be introduced.
Table 2.
Infant and young child feeding (IYCF): grandmothers’ knowledge, maternal knowledge and household practices in the sample of households from 240 rural communities in sixteen districts of Nepal, 2012
| Households with grandmothers (n 748) | Households without grandmothers (n 651) | ||||
|---|---|---|---|---|---|
| n | % | n | % | P value | |
| Grandmothers’ knowledge | |||||
| Initial breast-feeding: should be within an hour of birth | 744 | 71·2 | NA | – | NA |
| Colostrum: should be given to child | 740 | 83·1 | NA | – | NA |
| Each complementary food should be introduced at 6–9 months of age: | |||||
| Water | 743 | 46·4 | NA | – | NA |
| Milk and milk products | 743 | 54·9 | NA | – | NA |
| Semi-solid foods | 743 | 70·7 | NA | – | NA |
| Solid foods | 743 | 74·2 | NA | – | NA |
| Eggs | 743 | 49·3 | NA | – | NA |
| Meat | 743 | 45·1 | NA | – | NA |
| All six complementary foods | 743 | 17·2 | NA | – | NA |
| Mothers’ knowledge | |||||
| Initial breast-feeding: should be within an hour of birth | NA | NA | NA | NA | NA |
| Colostrum: should be given to child | 744 | 92·9 | 647 | 90·4 | 0·17 |
| Each complementary food should be introduced at 6–9 months of age: | |||||
| Water | 748 | 54·8 | 651 | 54·5 | 0·92 |
| Milk and milk products | 747 | 66·0 | 651 | 63·6 | 0·35 |
| Semi-solid foods | 747 | 78·2 | 651 | 78·6 | 0·83 |
| Solid foods | 747 | 76·3 | 651 | 78·3 | 0·36 |
| Eggs | 747 | 56·4 | 651 | 56·4 | 0·99 |
| Meat | 747 | 53·5 | 651 | 53·3 | 0·93 |
| All six complementary foods | 747 | 27·7 | 651 | 27·6 | 0·98 |
| IYCF practices | |||||
| Initial breast-feeding: within an hour of birth | 748 | 64·2 | 651 | 67·4 | 0·20 |
| Colostrum: given to child | 740 | 90·1 | 649 | 91·1 | 0·54 |
| Each complementary food introduced at 6–9 months of age: | |||||
| Water | 748 | 36·9 | 651 | 35·8 | 0·67 |
| Milk and milk products | 748 | 36·6 | 651 | 37·6 | 0·70 |
| Semi-solid foods | 748 | 64·3 | 651 | 63·1 | 0·65 |
| Solid foods | 748 | 70·4 | 651 | 67·7 | 0·27 |
| Eggs | 748 | 51·6 | 651 | 51·1 | 0·87 |
| Meat | 748 | 51·3 | 651 | 52·4 | 0·70 |
| All six complementary foods | 748 | 12·6 | 651 | 11·5 | 0·55 |
NA, not available.
Mothers’ knowledge was higher than grandmothers’ knowledge for all IYCF variables analysed. Mothers reported that six of ten children were breast-fed within the first hour of birth and that about nine of ten children received colostrum. Thirty-seven per cent of the mothers, in households with grandmothers, reported feeding water and milk and milk products at the correct time, while 64 and 70 % of the mothers reported feeding semi-solid foods and solid foods at the correct time. Half of the mothers reported correct practice of introducing eggs and meat at 6–9 months of age. None of the differences in maternal knowledge or IYCF practices between households with and without grandmothers were statistically significant.
Table 3 shows results from the regression analysis of grandmothers’ correct knowledge and optimal household practices for breast-feeding initiation, colostrum feeding and timing of introduction of each of the six types of complementary foods. When adjusting only for district-level clustering, the odds of correct IYCF practices were about two to four times higher in households where grandmothers had correct knowledge compared with households where grandmothers had incorrect knowledge. In the adjusted models, the odds of appropriate breast-feeding initiation and colostrum feeding were 2·2 and 4·2 times higher (P=0·002 and P<0·001), respectively, in households where grandmothers had correct knowledge compared with households where grandmothers had incorrect knowledge. Similarly, in the adjusted models, correct household timing of introducing water, milk, semi-solid foods, solid foods, eggs and meat were all two to three times higher in households where grandmothers had appropriate knowledge compared with households where grandmothers did not have appropriate knowledge (all P<0·001). Results were also robust when checked for clustering at the ward level (results available upon request).
Table 3.
Associations between grandmothers’ correct knowledge and correct infant and young child feeding practices among children 6–24 months of age in the sample of households from 240 rural communities in sixteen districts of Nepal, 2012
| Household practices | |||||||
|---|---|---|---|---|---|---|---|
| Crude† | Adjusted‡ | ||||||
| n | OR | 95 % CI | P value§ | OR | 95 % CI | P value§ | |
| Breast-feeding initiation | 740 | 1·89 | 1·17, 3·06 | <0·001 | 2·16 | 1·33, 3·52 | 0·002 |
| Colostrum feeding | 740 | 3·84 | 2·94, 5·01 | <0·001 | 4·24 | 2·81, 6·40 | <0·001 |
| Timing of introduction of complementary foods | |||||||
| Water | 735 | 2·46 | 1·63, 3·72 | <0·001 | 2·60 | 1·64, 4·11 | <0·001 |
| Milk (other than breast milk) | 739 | 1·92 | 1·20, 3·06 | 0·007 | 2·38 | 1·49, 3·80 | <0·001 |
| Semi-solid foods | 741 | 3·30 | 1·98, 5·50 | <0·001 | 3·20 | 1·88, 5·44 | <0·001 |
| Solid foods | 739 | 3·07 | 2·23, 4·26 | <0·001 | 2·93 | 2·08, 4·13 | <0·001 |
| Eggs | 739 | 2·05 | 1·34, 3·11 | 0·001 | 2·64 | 1·57, 4·43 | <0·001 |
| Meat | 739 | 2·01 | 1·46, 2·77 | <0·001 | 2·46 | 1·67, 3·62 | <0·001 |
| All six complementary foods | 678 | 2·08 | 1·05, 4·12 | 0·035 | 2·55 | 1·42, 4·56 | 0·002 |
Controlled for district-level clustering.
Adjusted for district-level clustering, all child factors (age, sex and decision making on child feeding), maternal factors (age, education, participation in wage/salary employment, number of sources from which nutrition information ever heard and currently residing in own mother’s home), grandmother factors (age and education) and household factors (number of children <5 years of age, agro-ecological zone of residency, ethnicity, food security, wealth quintile) and whether the household belonged to the intervention area or not.
From Wald test.
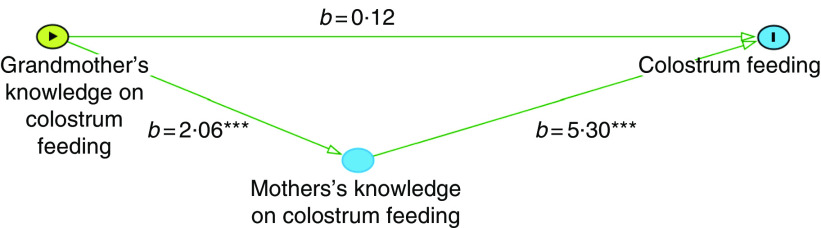
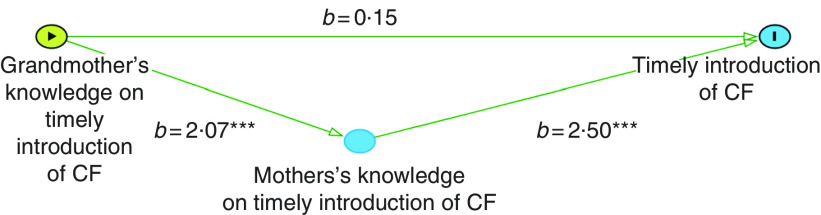
Tables 4 and 5 present results from our generalized structural equation modelling, based on our hypothesized models (Figs 1 and 2) of how grandmothers’ knowledge may influence IYCF practices directly as well as indirectly via maternal knowledge. Our results show that grandmother’s correct knowledge on feeding colostrum mostly influences the actual practice via influencing maternal knowledge. The direct effect is almost zero (Fig. 3), whereas there is a large, significant indirect effect: grandmothers’ correct knowledge improves the odds of mothers’ having correct knowledge by 2·1 times (P<0·001) and mothers’ correct knowledge improves the odds of colostrum being fed by 5·3 times (P<0·001). Similarly, grandmother’s correct knowledge on timely introduction of complementary foods has almost no direct effect (Fig. 4), but the indirect effect is positive and significant: the odds of maternal correct knowledge are 2·1 times higher in households where grandmothers have correct knowledge (P<0·001) and correct maternal knowledge improves the odds of complementary foods being introduced at the right time by 2·5 times (P<0·001).
Fig. 1.
Empirical model for direct and indirect effects of grandmothers’ knowledge on colostrum feeding and actual practice
Table 4.
Path analysis: exponentiated effects for grandmothers’ knowledge and colostrum feeding (n737) in the sample of households from 240 rural communities in sixteen districts of Nepal, 2012
| Colostrum feeding† | Maternal knowledge: colostrum feeding† | |
|---|---|---|
| Grandmothers’ correct knowledge | 0·12 | 2·06*** |
| Mothers’ correct knowledge | 5·30*** | NA |
| Child age | ||
| 9–11·9 months | −0·10 | 0·66 |
| 12–14·9 months | 0·30 | 0·45 |
| 15–17·9 months | 0·61 | −0·09 |
| 18–20·9 months | 0·77 | −0·07 |
| 21–23·9 months | 1·26 | 0·54 |
| Child sex | 0·67 | −0·57 |
| Decision maker: child feeding | ||
| Grandmother | 0·50 | −0·14 |
| Other | −0·68 | −0·09 |
| Maternal age | 0·01 | 0·10* |
| Maternal education | ||
| Some primary | −0·33 | 0·39 |
| Completed primary | −0·46 | 0·34 |
| Some secondary | −0·73(*) | 1·45** |
| Completed secondary | 0·85 | 0·98* |
| Higher level | −0·63 | 2·53* |
| Maternal employment | 0·24 | −0·68 |
| Maternal nutrition information: number of sources | 0·04 | −0·14 |
| Maternal residency with own mother | −1·03 | 1·27 |
| Grandmother’s age | 0·01 | 0·01 |
| Grandmother’s education | ||
| Some primary | −1·57* | −1·19 |
| Completed primary | 14·1*** | 14·4*** |
| Some secondary | 13·8*** | 13·7*** |
| Completed secondary | 13·6*** | 11·9*** |
| Higher level | 13·3*** | 14·5*** |
| Household agro-ecological zone of residency | ||
| Hill | 0·19 | −1·18(*) |
| Terai | 0·51 | −1·09 |
| Household caste/ethnicity | ||
| Disadvantaged Janajatis | −0·03 | 0·62 |
| Disadvantaged non-Dalit Terai | 0·64 | 0·00 |
| Religious minorities (Muslim/Churoute) | 17·1*** | −1·13 |
| Relatively advantaged Janajatis | 0·05 | −0·43 |
| Most advantaged (Brahmin/Chettri/Thakuri/Sanyasi) | 0·25 | 0·31 |
| Household food security | ||
| Mildly food insecure | −0·44 | 0·09 |
| Moderately food insecure | −1·13 | −0·43 |
| Severely food insecure | 1·61 | −1·07 |
| Household wealth quintile | ||
| Second poorest | 0·63 | −0·20 |
| Middle income | 0·01 | 0·17 |
| Second wealthiest | −0·25 | 0·86 |
| Wealthiest | 0·21 | 0·54 |
| Household number of children <5 years of age | ||
| 2 | 0·36 | 0·19 |
| 3 or more | 0·27 | 0·98 |
NA, not available.
(*)P<0·10, *P<0·05, **P<0·01, ***P<0·001.
Adjusted for clustering at district level.
Table 5.
Path analysis: exponentiated effects for grandmothers’ knowledge and introduction of complementary foods (n 741) in the sample of households from 240 rural communities in sixteen districts of Nepal, 2012
| Timely introduction of all complementary foods† | Maternal knowledge: introduction of complementary foods† | |
|---|---|---|
| Grandmothers’ correct knowledge | 0·15 | 2·07*** |
| Mothers’ correct knowledge | 2·50*** | NA |
| Child age | ||
| 9–11·9 months | −1·93*** | 0·62(*) |
| 12–14·9 months | −1·14*** | 0·33 |
| 15–17·9 months | −1·52*** | 0·67(*) |
| 18–20·9 months | −1·72** | 0·34 |
| 21–23·9 months | −1·22*** | 0·24 |
| Child sex | −0·63(*) | 0·01 |
| Decision maker: child feeding | ||
| Grandmother | −0·76 | −0·13 |
| Other | −0·54 | 0·42 |
| Maternal age | 0·03 | −0·02 |
| Maternal education | ||
| Some primary | −0·20 | 0·01 |
| Completed primary | 0·55 | 0·05 |
| Some secondary | −0·37 | 0·52 |
| Completed secondary | −0·32 | 0·34 |
| Higher level | −1·40(*) | 0·28 |
| Maternal employment | 0·18 | 0·32 |
| Maternal nutrition information: number of sources | 0·01 | −0·04 |
| Maternal residency with own mother | 0·84 | −0·81 |
| Grandmother’s age | 0·01 | 0·01 |
| Grandmother’s education | ||
| Some primary | 0·88 | −1·10* |
| Completed primary | −13·8*** | −0·69 |
| Some secondary | 3·01*** | 0·37 |
| Completed secondary | −10·4*** | −14·4*** |
| Higher level | −13·0*** | 0·94 |
| Household agro-ecological zone of residency | ||
| Hill | −0·39 | −0·07 |
| Terai | −1·52(*) | −0·41 |
| Household caste/ethnicity | ||
| Disadvantaged Janajatis | −0·53 | 0·02 |
| Disadvantaged non-Dalit Terai | −13·4*** | 0·63 |
| Religious minorities (Muslim/Churoute) | −12·0*** | −14·9*** |
| Relatively advantaged Janajatis | 0·03 | −0·28 |
| Most advantaged (Brahmin/Chettri/Thakuri/Sanyasi) | −0·17 | −0·51 |
| Household food security | ||
| Mildly food insecure | 0·15 | 0·09 |
| Moderately food insecure | −0·22 | 0·15 |
| Severely food insecure | −15·7*** | 0·20 |
| Household wealth quintile | ||
| Second poorest | −0·69(*) | 0·91** |
| Middle income | −0·37 | 0·18 |
| Second wealthiest | −0·72* | 0·44(*) |
| Wealthiest | −2·30** | 0·92* |
| Household number of children <5 years of age | ||
| 2 | 0·39 | 0·27 |
| 3 or more | −0·22 | 0·14 |
NA, not available.
(*)P<0·10, *P<0·05, **P<0·01, ***P<0·001.
Adjusted for clustering at district level.
Fig. 2.
Empirical model for direct and indirect effects of grandmothers’ knowledge on timely introduction of complementary foods (CF) and actual practice
Fig. 3.
Exponentiated coefficients (b) for direct and indirect effects of grandmothers’ knowledge on colostrum feeding and actual practice in Nepal, 2012; ***P<0·001
Fig. 4.
Exponentiated coefficients (b) for direct and indirect effects of grandmothers’ knowledge on timely introduction of complementary foods (CF) and actual practice in Nepal, 2012; ***P<0·001
Discussion
The present study explored the association between grandmothers’ knowledge and selected IYCF practices of children under 2 years of age: initial breast-feeding, feeding colostrum, and the appropriate timing of introduction of water, milk, semi-solid foods, solid foods, meat and eggs as complementary foods. The results from the cross-sectional data set that included children 6–24 months of age (n 1399), of whom 748 lived with grandmothers and 651 did not live with grandmothers, showed that more than half initiated breast-feeding within the first hour of birth, nearly all were given colostrum, and the percentage of households with appropriate timing of introduction of complementary foods varied among the six types of food (water, milk, semi-solid foods, solid foods, meat and eggs). Using logistic regression models we found that, among households with grandmothers in residence, the odds of appropriate IYCF practice were at least two times or more likely in households where grandmothers had correct knowledge compared with households were grandmothers had incorrect knowledge and these results were statistically significant. Our mediation analyses showed that almost all of the association between grandmothers’ practice-specific IYCF knowledge and actual practice is mediated by maternal knowledge: grandmothers’ IYCF-related knowledge influences maternal IYCF knowledge and in turn household IYCF practices.
In the present study, the variation across IYCF practices even among the same population was substantial. Although more than 90 % of children in rural Nepal were given colostrum, initial breast-feeding in the first hour after birth happened only in about two-thirds of households. This prevalence was higher than in Nepal’s 2011 Demographic and Health Survey, which showed that less than 45 % of children in rural areas born in the previous 2 years were breast-fed within an hour of birth. Similarly, the timing of introduction of complementary foods varied substantially by type of food, with water and milk given too early and eggs and meat given too late, both in the present study and other studies in Nepal. A previous study noted that this is in part because of a belief that complementary foods should be soft to avoid diarrhoea and stomach aches and that animal-source foods should only be introduced once the child develops teeth and the ability to digest appropriately( 13 , 14 ). Attention to each of these IYCF practices is important given their importance for ensuring optimal child nutrition.
The present study highlights the potential role of other adult household members, specifically grandmothers, in child feeding and nutrition. The positive associations between grandmothers’ knowledge and IYCF practices are consistent with earlier, albeit scant, literature in South Asia. In a study in Vadodara, India, Sharma and Kanani found that households in which a grandmother resided, in comparison to households without a grandmother, delayed initiation of complementary feeding to beyond 6 months of age and called for future child nutrition interventions in South Asia to include all family members who are childcare providers( 21 ). In a mixed-methods study in rural Haryana, India, Kausal et al. found that grandmothers believed that complementary foods should only be introduced when the infant starts walking or asking for food, while the mothers believed complementary feeding should be introduced much earlier( 22 ). This is consistent with our findings, underscores that IYCF-related knowledge may differ among adult childcare providers in the same household and highlights the need for ensuring that grandmothers are also aware of optimal IYCF practices, given their influential role in child feeding in South Asia( 23 ). Analysing a cross-sectional data set from the Young Lives study in Andhra Pradesh, India, Moestue and Huttly found independent associations between maternal, paternal and grandmother characteristics and child nutritional status, further highlighting the need for programmes to target other family and community members, rather than just mothers( 24 ). Studies from outside South Asia have also emerged showing the important role of grandmothers for child health and nutrition and the need for targeting them with behaviour change communication interventions( 25 – 27 ).
As mentioned, commonly in South Asia and in Nepal, senior women are highly revered and hold the top position in the family hierarchy, often having power and authority over younger women, including relating to infant feeding( 27 , 28 ). A study in Maharashtra, India showed that grandmothers take care of infants and teach first-time, inexperienced mothers about breast-feeding, prelacteal feeding, complementary feeding and feeding during child illness. That study found that mothers often follow practices that their mothers and mothers-in-law suggest, perhaps due to their own inexperience or to avoid conflict and maintain tradition( 23 ). Mothers generally consult grandmothers regarding feeding of infants and young children and some grandmothers feel that it is their responsibility to teach mothers and pass on their knowledge, perceiving themselves as ‘providers of perinatal care’( 12 ), a perception strengthened by first-time mothers relying on them for expertise and knowledge regarding IYCF practices.
The present study suffers from a few limitations. First, the study is based on a cross-sectional data set and thus our regression results cannot be interpreted as causal. Second, this was not a nationally representative sample; the sixteen districts of Nepal included in the survey were purposively selected for an impact evaluation baseline. Third, there may be residual unaccounted for confounders not available in the data set or biases which are inevitable in self-reported practices (e.g. IYCF). We asked mothers of children up to 2 years of age to remember child feeding practices since birth and acknowledge potential recall bias as a study limitation( 29 – 34 ). Finally, in this data set, the grandmother data are limited and certain interesting data points, such as whether the grandmothers had been exposed to nutrition-related counselling or other inputs, are unavailable.
Despite these limitations, the present study is the first empirical study in Nepal, and one of few globally, to investigate associations between grandmothers’ knowledge and IYCF practices. Our study adds to prior studies, which were mostly qualitative or had very small sample sizes, failed to adjust for potential confounding and clustering, and looked only at either breast-feeding or complementary feeding. Furthermore, our study disaggregates the complementary foods rather than lumping the various food types, which is important given variation in use of these foods for child feeding. The mediation analysis also allowed us to explore how grandmothers’ knowledge may influence nutritional practices compared with traditional regression analysis, which answers only whether associations exist or not. Therefore, our study suggests additional hypotheses around how household factors influence IYCF practices in South Asia.
Future research and programme and policy implications
Globally, most child nutrition policies and programmes target mothers of young children, aiming to increase their awareness and motivation to engage in optimal IYCF practices. In South Asia, grandmothers’ roles as decision makers and advisors on child health and nutrition suggest that they should be integrated into existing programmes or that interventions designed specifically for grandmothers and other adult household members could prove beneficial. One way of addressing knowledge gaps may be to improve health workers’ knowledge and their counselling skills for communicating accurate ICYF knowledge and ensure that health workers are reaching childcare providers at large with this information, rather than just mothers. Different child nutrition approaches and programmes may be needed to target households with and without grandmothers, since we observed differences in demographics between these two types of household.
Additional studies could analyse factors that may shape grandmothers’ knowledge, pathways and mechanisms for how this influences child feeding and the nutritional status of the child, and how these differ by various demographic (e.g. caste) and socio-economic (e.g. wealth) characteristics. Detailed attention should be given to which household member undertakes which specific childcare roles and how often to inform the design of future interventions. Rigorous experimental and quasi-experimental studies are needed to investigate how grandmothers, and other adult household members, effect change in IYCF practices. While the focus in the present study was on feeding infants and young children, a similar analysis for other nutrition-related practices, including diet for women during pregnancy and lactation, food hygiene, and water, sanitation and hygiene behaviours, would also be informative.
The Government of Nepal’s National Multi-sector Nutrition Plan and the various nutrition-sensitive and nutrition-specific interventions( 35 ), aiming to address the high prevalence of stunting, wasting and micronutrient deficiencies, are all important steps in the right direction. Our findings suggest these efforts may be more effective in improving IYCF practices and reducing undernutrition if other adult household members, such as grandmothers, are also explicitly targeted( 24 , 36 , 37 ). In rural Nepal, this is now particularly important in the light of increasing exit migration of women from Nepal and young children being left behind to be cared for by grandparents. Nepal’s present climate of commitment to nutrition and to addressing the burden of undernutrition, particularly among children in the first ‘1000 days’ of life, must be pushed forward. This is an ideal time to adopt innovative approaches to nutritional obstacles so that further reductions in child nutrition can be seen and to engage in rigorous research to assess the effectiveness of these approaches and build a stronger evidence base for how to address persistent undernutrition.
Acknowledgements
Acknowledgements: The authors would like to acknowledge various organizations within the Suaahara project, including the US Agency for International Development (USAID), Save the Children and Helen Keller International (HKI). They also thank Akriti Singh and Swetha Manohar for providing valuable feedback to this paper. They are particularly grateful to the thousands of households who participated in the Suaahara baseline study for their time and energy. C.K. would also like to thank Laura Brye, Pooja Pandey and Dale Davis for facilitating the internship at HKI Nepal so that this study could be carried out and Bishnu Dulal for assisting with data analysis. Financial support: Data collection and work on this manuscript was supported by Suaahara, funded by USAID. USAID had no role in the design, analysis or writing of this article. Conflict of interest: HKI, a Suaahara-implementing organization, provided an unpaid internship opportunity for C.K. to carry out this analysis in Nepal and funded a separate research consultancy for K.C. However, none of this analysis assesses the impact of Suaahara. Authorship: C.K., K.C. and S.K. designed the research; C.K., J.C. and K.C. analysed the data; C.K., K.C. and S.K. wrote the paper; C.K. had primary responsibility for final content; all authors read and approved the final manuscript. Ethics of human subject participation: Ethics approval was obtained from the NHRC and the internal review board of IFPRI (2012); and also from the LSHTM (2015) for the additional analysis presented herein.
References
- 1. Cunningham K, Headey D, Singh A et al. (2017) Maternal and child nutrition in Nepal: examining drivers of progress from the mid-1990s to 2010s. Glob Food Sec (Epublication ahead of print version).
- 2. Cunningham K, Singh A, Headey DD et al. (2016) Reaching new heights: 20 years of nutrition progress in Nepal. In Nourishing Millions: Stories of Change in Nutrition, pp. 115–123 [S Gillespie, J Hodge, S Yosef et al., editors]. Washington, DC: International Food Policy Research Institute. [Google Scholar]
- 3. Headey D & Hoddinott J (2015) Understanding the rapid reduction of undernutrition in Nepal, 2001–2011. PLoS One 10, e0145738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Devkota MD, Adikari RK & Upreti S (2016) Stunting in Nepal: looking back, looking ahead. Matern Child Nutr 12, 257–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Headey D, Hoddinott J & Park S (2016) Drivers of nutritional change in four South Asian countries: a dynamic observational analysis. Matern Child Nutr 12, Suppl. 1, 210–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pan American Health Organization & World Health Organization (2003) Guiding Principles for Complementary Feeding of the Breastfed Child. Washington, DC and Geneva: PAHO and WHO. [Google Scholar]
- 7. Black RE, Allen LH, Bhutta ZA et al. (2008) Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371, 243–260. [DOI] [PubMed] [Google Scholar]
- 8. Ministry of Health and Population (Nepal), New Era & ICF International (2011) Nepal Demographic and Health Survey. Kathmandu and Calverton, MD: Ministry of Health and Population, New Era and ICF International. [Google Scholar]
- 9. Stewart CP, Iannotti L, Dewey KG et al. (2013) Contextualising complementary feeding in a broader framework for stunting prevention. Matern Child Nutr 9, 27–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Aubel J & Alvarez M (2011) The Roles and Influence of Grandmothers and Men: Evidence Supporting a Family-Focused Approach to Optimal Infant and Young Child Nutrition. Washington, DC: US Agency for International Development. [Google Scholar]
- 11. Aubel J & Project TG (2005) Grandmothers: A Learning Institution. Washington, DC: US Agency for International Development. [Google Scholar]
- 12. Masvie H (2006) The role of Tamang mothers-in-law in promoting breast feeding in Makwanpur District, Nepal. Midwifery 22, 23–31. [DOI] [PubMed] [Google Scholar]
- 13. Seckel L (2011) Factors that Constrain or Prevent Optimal Infant and Young Child Feeding Practices in Rural Nepal: Findings from a Formative Research Study in Three Districts. Kathmandu: Nepal Family Health Program II, Johns Hopkins Bloomberg School of Public Health.
- 14. Locks LM, Pandey PR, Osei AK et al. (2013) Using formative research to design a context-specific behaviour change strategy to improve infant and young child feeding practices and nutrition in Nepal. Matern Child Nutr 11, 882–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Government of Nepal (2014) Labour Migration for Employment A Status Report for Nepal: 2013/2014. Kathmandu: Government of Nepal. [Google Scholar]
- 16. Pandey S, Tiwari K, Senarath U et al. (2010) Determinants of infant and young child feeding practices in Nepal: secondary data analysis of Demographic and Health Survey 2000. Food Nutr Bull 31, 352–365. [DOI] [PubMed] [Google Scholar]
- 17. Pokhrel S & Sauerborn R (2004) Household decision-making on child health care in developing countries: the case of Nepal. Health Policy Plan 19, 218–233. [DOI] [PubMed] [Google Scholar]
- 18. Cunningham K, Ploubidis GB, Menon P et al. (2015) Women’s empowerment in agriculture and child nutritional status in rural Nepal. Public Health Nutr 18, 3134–3145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Joshi N, Kingsley EA, Dibley MJ et al. (2012) Determinants of inappropriate complementary feeding practices in young children in Nepal: secondary data analysis of Demographic and Health Survey 2006–2007. Matern Child Nutr 8, Suppl. 1, 60–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Coates J, Bilinsky P & Coates J (2007) Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide. Washington, DC: Food and Nutrition Technical Assistance, FHI 360. [Google Scholar]
- 21. Sharma M & Kanani S (2006) Grandmothers’ influence on child care. Indian J Pediatr 73, 295–298. [DOI] [PubMed] [Google Scholar]
- 22. Kaushal M, Aggarwal R, Singal A et al. (2005) Breastfeeding practices and health-seeking behavior for neonatal sickness in a rural community. J Trop Pediatr 51, 366–376. [DOI] [PubMed] [Google Scholar]
- 23. Aubel J (2012) The role and influence of grandmothers on child nutrition: culturally designated advisors and caregivers. Matern Child Nutr 8, 19–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Moestue H & Huttly S (2008) Adult education and child nutrition: the role of family and community. J Epidemiol Community Health 62, 153–159. [DOI] [PubMed] [Google Scholar]
- 25. Ahrari M, Houser RF, Yassin S et al. (2006) A positive deviance-based antenatal nutrition project improves birth-weight in Upper Egypt. J Health Popul Nutr 24, 498–507. [PMC free article] [PubMed] [Google Scholar]
- 26. Aubel J, Touré I & Diagne M (2004) Senegalese grandmothers promote improved maternal and child nutrition practices: the guardians of tradition are not averse to change. Soc Sci Med 59, 945–959. [DOI] [PubMed] [Google Scholar]
- 27. Aubel J & Alvarez M (2011) The Roles and Influence of Grandmothers and Men: Evidence Supporting a Family-Focused Approach to Optimal Infant and Young Child Nutrition: Literature Review. Washington, DC: US Agency for International Development. [Google Scholar]
- 28. Simkhada B, Porter MA & van Teijlingen ER (2010) The role of mothers-in-law in antenatal care decision-making in Nepal: a qualitative study. BMC Pregnancy Childbirth 10, 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Natland ST, Andersen LF, Nilsen TIL et al. (2012) Maternal recall of breastfeeding duration twenty years after delivery. BMC Med Res Methodol 12, 179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Li R, Scanlon KS & Serdula MK (2005) The validity and reliability of maternal recall of breastfeeding practice. Nutr Rev 63, 103–110. [DOI] [PubMed] [Google Scholar]
- 31. Karkee R, Lee AH, Khanal V et al. (2014) Infant feeding information, attitudes and practices: a longitudinal survey in central Nepal. Int Breastfeed J 9, 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bailey S & Hedlund K (2012) The Impact of Cash Transfers on Food Consumption in Humanitarian Settings: A Review of Evidence. London: Humanitarian Policy Group, Overseas Development Institute. [Google Scholar]
- 33. Bai DL, Fong DYT, Lok KYW et al. (2017) Practices, predictors and consequences of expressed breast-milk feeding in healthy full-term infants. Public Health Nutr 20, 492–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gibson RS (2005) Principles of Nutritional Assessment. Oxford: Oxford University Press. [Google Scholar]
- 35. Government of Nepal, National Planning Commission (2012) Multi-Sectoral Nutrition Plan for Accelerating the Reduction of Maternal and Child Undernutrition in Nepal. Kathmandu: Government of Nepal, National Planning Commission. [Google Scholar]
- 36. Moestue H, Huttly S, Sarella L et al. (2007) ‘The bigger the better’ – mothers’ social networks and child nutrition in Andhra Pradesh. Public Health Nutr 10, 1274–1282. [DOI] [PubMed] [Google Scholar]
- 37. Duffield A, Abdullah-Al-Harun, Hossain M et al. (2003) Thin on the Ground. Questioning the Evidence behind World Bank-Funded Community Nutrition Projects in Bangladesh, Ethiopia and Uganda. London: Save the Children. [Google Scholar]